Abstract
Objectives:
We aimed to describe recent technologic advances in the three domains of dementia care, falls, and home supports; summarize existing literature on usability; and identify knowledge gaps.
Methods:
A comprehensive search of five databases for recent peer-reviewed publications was conducted in May 2020. Independent reviewers performed title/abstract review, full-text screening, data extraction, and study characteristic summarization.
Results:
Out of 2,696 citations, 151 articles were retrieved for full-text evaluation, after which 54 studies were included in this scoping review. For each domain, different technologies are available to enhance the health and well-being of older adults; many users deemed them usable and useful. Technologies targeted improving function, psychosocial and cognitive status, home safety, and caregiver burden. Barriers to widespread uptake include privacy concerns, suboptimal user experience, and willingness to accept assistance.
Conclusion:
Technologic innovations directed towards dementia care, fall detection, and ambient assisted living can aid older adults ‘aging in place.’
Introduction
Gerontechnology — defined as technology designed to enable the health of older persons (Micera et al., 2008) — has become a key focus of biomedical research. Ideally, technology should assist older persons with “aging in place,” or living in their own homes independently, when disabilities such as cognitive impairment or mobility issues occur. Beyond living with a sense of independence, older adults may associate “aging in place” with the continuation of the social connections they developed with neighbors and friends as well as a reassuring sense of familiarity with the community they reside in — important biopsychosocial considerations that can be supported by technology (Wiles et al., 2012). Potential benefits also include lower healthcare costs (Aanesen et al., 2011) and improved quality of life and safety (Finch et al., 2017). Uptake of technology by older adults has been increasing (Anderson & Perrin, 2017), but remains dependent on the usability — or ease of using the devices. The three domains of dementia care, falls, and home supports are some of the greatest challenges faced by older adults in ‘aging in place.’ Connecting these domains and serving as the impetus for this review, persons with dementia (PWDs) have been shown to have an increased risk of falls in the home setting, highlighting the need for effective home support interventions to encourage ‘aging in place’ (Petersen et al., 2018).
Dementia care
According to the World Health Organization (WHO) (2019), an estimated 50 million people have dementia, with 5–8% of older adults affected worldwide. PWDs face unique challenges including loneliness, agitation, and wandering behaviors, with recent evidence identifying the importance of technology (e.g., smartphone applications) in supporting PWDs (Brown et al., 2019). Key areas in which technology can be used to benefit PWDs include assessment of cognitive impairment, assistance with activities of daily living (ADLs), facilitation of leisure activities, and support of caregivers (Astell et al., 2019).
Fall detection
Falls are the leading cause of fatal and non-fatal injuries among older adults over age 64 (Bergen et al., 2016). Globally, approximately one-third of older adults fall annually and 20–30% of older adults who fall experience injuries (WHO, 2008). In the United States, the estimated annual Medicare cost for older adult falls of $31.3 billion is expected to increase as the population ages (Burns et al., 2016). Automated alerts that passively detect falls and notify emergency staff are particularly important as injuries, a lack of home companions, and frailty can make it difficult for individuals to obtain assistance independently. Historically, research efforts have focused on refining technology to accurately detect falls, notify contacts of fall occurrences, and develop profiles of high-risk individuals (Baik, 2019).
Home supports
By 2030, only four caregivers will be available for each older adult to provide support, a marked decrease from 2010 when seven caregivers were available (AARP, 2019). As a result, we should anticipate a greater need for in-home nursing services, assisted living facilities, and long-term care facilities (Colombo et al., 2011). Because adults often prefer to ‘age in place’ in their familiar home environment rather than moving to facilities, unpaid caregivers and/or family members are often called upon to provide assistance. Because of the projected shortfall in caregivers, solutions such as ambient assisted living (AAL) could become more meaningful.
AAL is defined as “the use of information and communication technologies in a person’s daily living and working environment to enable them to stay active longer, remain socially connected and live independently into old age” (Monekosso et al., 2015). Generally, AAL includes smart devices, wireless networks, and medical sensors. These technologies can simplify and enhance safety for older persons by providing technological assistance with daily tasks and health and home monitoring (Kunnappilly et al., 2019).
Objectives
There is a growing body of gerontechnology literature, but no existing reviews focusing collectively on the three domains of dementia care, falls, and ambient assisted living and the usability of currently available technology. Additionally, recent reviews of these three individual domains (Astell et al., 2019; Pietrzak et al., 2014; Ganesan et al., 2019) neglect to report on the usability of technologies or address their relevance to ‘aging in place.’ Therefore, our aim was to highlight three growing areas of gerontechnology — dementia care, fall detection, and ambient assisted living — describe recent advances in the field, summarize existing usability studies, and identify knowledge gaps that should be addressed in future research.
Methods
To generate a summary of our three gerontechnology areas of interest, we performed a scoping review following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) (Liberati et al., 2009). We performed a scoping review because this design is especially useful to synthesize a topic with numerous interventions and outcomes. In this review, we aimed to examine interventions that could improve the quality of life for older persons.
Inclusion criteria
We selected studies based on a broad set of inclusion criteria to ensure inclusion of all relevant literature. We included articles on (1) dementia care, focusing on loneliness/social isolation, behavioral and psychological symptoms, wandering, care coordination, and fall detection; (2) fall detection via sensors or wearable devices; and (3) ambient assisted living, focusing on home monitoring. We only included articles focused on older adults, defined as individuals 65 years or older. We included interventional, observational, and pilot studies and excluded conference publications, published theses, and review articles. We also excluded articles that were not home-based, caregiver/provider-centric, not related to our three main concepts, not focused on independent living, and inappropriate study populations. Because the field of gerontechnology is rapidly evolving, we decided on a publication date cut point of studies published only in 2015 or later.
Literature search and article selection
We conducted a literature search in the following five databases: PubMed, CINAHL, EMBASE, PsycINFO, and MEDLINE. We used the following search strategy: (dementia or ‘cognitive impairment’ or ‘Alzheimer’s disease’ or ‘cognitive dysfunction’ or monitoring or ‘fall detection’ or ‘clinical alarms’ or ‘ambient intelligence’ or ‘ambient assisted living’ or ‘smart home’ or ‘AAL’) AND (‘older adults’ or aged or elderly or ‘older people’ or geriatric*) AND (technology or ‘assistive technology’ or sensor or camera or wearable) AND (‘randomized controlled trial’ or ‘controlled clinical trial’ or randomized or randomised or randomization or randomisation or placebo or randomly or trial or groups or ‘clinical trial’ or ‘clinical trials’ or ‘evaluation study’ or ‘intervention study’). Our keywords and search strategy are available in Table 1. We used the reference management software, EndNote version X9, to manage the identified articles and to check for duplicates. All database searches were concluded in May 2020.
Table 1.
Search Outcomes
| Search Number | Search Words/Identifiers | Number of Results |
|---|---|---|
| S1 | dementia OR ‘cognitive impairment’ OR ‘alzheimer disease’ OR ‘cognitive dysfunction’ OR monitoring OR ‘fall detection’ OR ‘clinical alarms’ OR ‘ambient intelligence’ OR ‘ambient assisted living’ OR ‘smart home’ OR aal | 3,121,462 |
| S2 | ‘older adults’ OR aged OR elderly OR ‘older people’ OR geriatric* | 15,051,547 |
| S3 | technology OR ‘assistive technology’ OR sensor OR camera OR wearable | 3,505,133 |
| S4 | S1 AND S2 AND S3 | 35,098 |
| S5 | S1 AND S2 AND S3 (last 5 years) | 15,764 |
| S6 | ‘randomized controlled trial’ OR ‘controlled clinical trial’ OR randomized OR randomised OR randomization OR randomization OR placebo OR randomly OR trial OR groups OR ‘clinical trial’ OR ‘clinical trials’ OR ‘evaluation study’ OR ‘intervention study’ | 13,276,874 |
| S7 | S5 AND S6 | 2,696 |
| Duplicates removed | 697 | |
| For consideration | 1,999 | |
| Excluded | 1,945 | |
| Final articles included in review | 54 |
Data extraction
Two authors independently performed title and abstract screening. Full text articles of studies deemed potentially relevant from initial screening were further assessed for inclusion. Disagreements were managed through adjudication by the senior author. Data extraction of all data for the summary tables was performed, including: 1) study characteristics (i.e. author, year), 2) sample size, 3) average participant age (or range if not available), 4) intervention type or qualitative interview details, and 5) main results and findings. Due to the scoping review approach, as well as the volume and heterogeneity of included articles, a formal assessment of study quality or risk of bias was not completed.
Results
A multi-sourced database search returned a total of 2,696 articles, with 1,999 articles remaining after duplicate removal. Of those, 1,848 articles were excluded after screening titles and abstracts as their contents were unrelated to our three domains (dementia care, fall detection, and ambient assisted living) in older adults. Of the remaining 151 articles selected for full-text review, we identified 54 articles eligible for inclusion. The PRISMA flow diagram summarizes study identification and selection (Figure 1).
Figure 1.
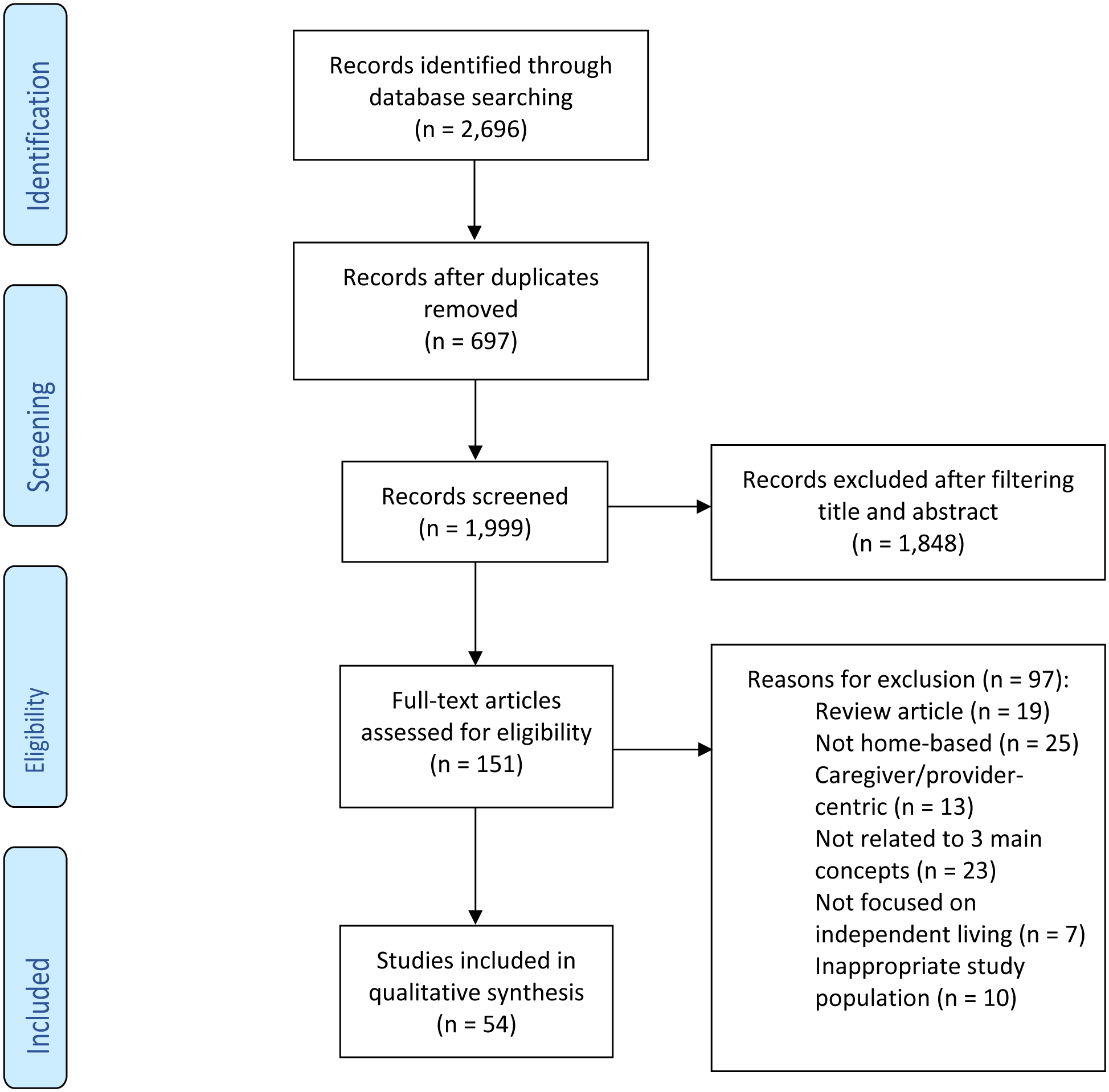
PRISMA flow diagram of studies included in the scoping review.
Characteristics of included articles
The majority of the included studies were conducted in the United States (n=10, 18.5%), France (n=6, 11.1%), the United Kingdom (n=5, 9.3%), Italy (n=4, 7.4%), and Germany (n=3, 5.6%). Two-thirds of the studies focused exclusively on older adults (n=38), with the remaining one-third (n=16) additionally including caregivers and/or health professionals. Sample sizes varied widely among our included studies, with the smallest number of participants being four and the greatest number being 495. Twenty-three (42.6%) studies were pilot studies, ten (18.5%) were randomized trials, six (11.1%) were mixed-methods studies, five (9.3%) incorporated focus groups, four (7.4%) included a crossover design, three (5.6%) utilized semi-structured interviews, two (3.7%) were cost analyses, and one (1.9%) distributed a questionnaire. Supplemental Table 1 summarizes the characteristics of included studies.
Dementia care
A wide range of technologies were included in the 27 studies on dementia care: virtual reality (n=4, 14.8%), care robots (n=4, 14.8%), home monitoring systems (n=3, 11.1%), wearable cameras (n=2, 7.4%), apps (n=2, 7.4%), computer-based interventions (n=2, 7.4%), augmented reality (n=2, 7.4%), Xbox 360 Kinect (n=2, 7.4%), wearable activity monitor (n=1, 3.7%), active music therapy (n=1, 3.7%), electric calendar (n=1, 3.7%), and intelligent cognitive assistant (n=1, 3.7%). Two studies (7.4%) explored assistive technologies in general.
PWDs were generally receptive of the various technologies intended for dementia care and found them to be feasible (Appel et al., 2019; Dethlefs et al., 2017; Djabelkhir et al., 2017; Farina et al., 2019; Hattink et al., 2016). Many of these interventions led to improvements in cognitive, psychosocial, and motor functioning (Djabelkhir et al., 2017), including cognitive performance (Zając-Lamparska et al., 2019), ADL function (Liao et al., 2020; Nishiura et al., 2019; Silva et al., 2017), depressive symptomatology (Giovagnoli et al., 2018; Lazarou et al., 2016; Silva et al., 2017), appetite (Giovagnoli et al., 2018), sleep quality (Lazarou et al., 2016), MoCA scores (Amjad et al., 2019; Lazarou et al., 2016; Liao et al., 2020), Mini-Mental State Examination scores (Amjad et al., 2019; Lazarou et al., 2016; Nishiura et al., 2019), verbal memory (Liao et al., 2020), and long-term spatial memory (Serino et al., 2017). PWDs found these technologies to be more useful and had higher intention to use them than healthy controls (Pino et al., 2015). Additionally, separate studies addressed the positive effects of assistive robots regarding PWDs’ safety concerns (Darragh et al., 2017; Forsyth et al., 2019) and remote health monitoring (Darragh et al., 2017).
Several barriers to adoption and use were identified: lack of experience with technology (Pino et al., 2015), lack of desire for assistance by technology (Wu et al., 2016), difficulties learning how to use technology (Wu et al., 2016). PWDs also were noted to be concerned about privacy (Gelonch et al., 2019; Hattink et al., 2016) and suggested that assistive technologies may lead to social isolation (Asghar et al., 2018), with assistive robots lacking authenticity and the ‘human presence’ (Wu et al., 2016). Most of these barriers can be overcome with education and training (Megges et al., 2017).
Fall detection
The majority of the included studies on fall detection studied wearable sensors (n=5, 83.3%). Only one (n=1, 16.7%) study focused on environmental sensors, such as wall mounted devices. Older adults generally found fall detection devices to be acceptable and preferred wearable devices over environmental devices (Chaudhuri et al., 2017). The wearable devices examined had high sensitivity and specificity for fall detection (Di Rosa et al., 2017; Ejupi et al., 2017; Saadeh et al., 2019). Concerns regarding wearable devices included occasional false positives (Demiris et al., 2016) and insufficient battery life (Chaudhuri et al., 2017; Thilo et al., 2019). Some older adults failed to see the need for fall detection devices and were embarrassed by them (Demiris et al., 2016), but others reported that fall detection devices enhanced their independence (Chaudhuri et al., 2017).
Ambient assisted living
Studies addressing AAL focused on home monitoring systems (n=13, 61.9%), wearable devices (n=3, 14.3%), exergame/walking applications (n=2, 9.5%), care robots (n=1, 4.8%), and digital calendars (n=1, 4.8%). One study (n=1, 4.8%) focused on AAL technologies in general. Authors found that AAL improved inhibition and working memory (Adcock et al., 2020), increased physical activity and self-reported quality of life scores (Jang et al., 2018), a sense of safety and security (Halcomb et al., 2016; Pigini et al., 2017), assistance in health monitoring and management (Halcomb et al., 2016; Pigini et al., 2017), and improved ADL functioning (Baric et al., 2019).
Although most of the AAL interventions were found to be usable and acceptable, caregivers rated monitoring systems higher than older adults (Cohen et al., 2016), noting that AAL increased their sense of control (Epstein et al., 2016) and reduced their caregiving burden (Dupuy et al., 2017). Some older adults, however, felt that AAL technologies were not what they needed (Berridge et al., 2019) and they did not appreciate being monitored (Epstein et al., 2016; Macis et al., 2020). One study highlighted that older adults were concerned about privacy (Batsis et al., 2018), but other studies found that privacy was not a barrier to AAL technology adoption (Pigini et al., 2017; Pol et al., 2016). Studies examining AAL technologies identified a need for increased focus on user-centered design (Batsis et al., 2018) and greater individualization of interventions (Epstein et al., 2016). Although some older adults were concerned about the costs of the technology (Joe et al., 2018; Son & Kim, 2019), the two cost analyses included in this review indicated that remote monitoring could provide savings by reducing the use of medical services (Finch et al., 2017) and delaying entry into assisted living facilities (Rantz et al., 2015). Figure 2 identifies the technologic opportunities and barriers of the three key domains identified.
Figure 2.
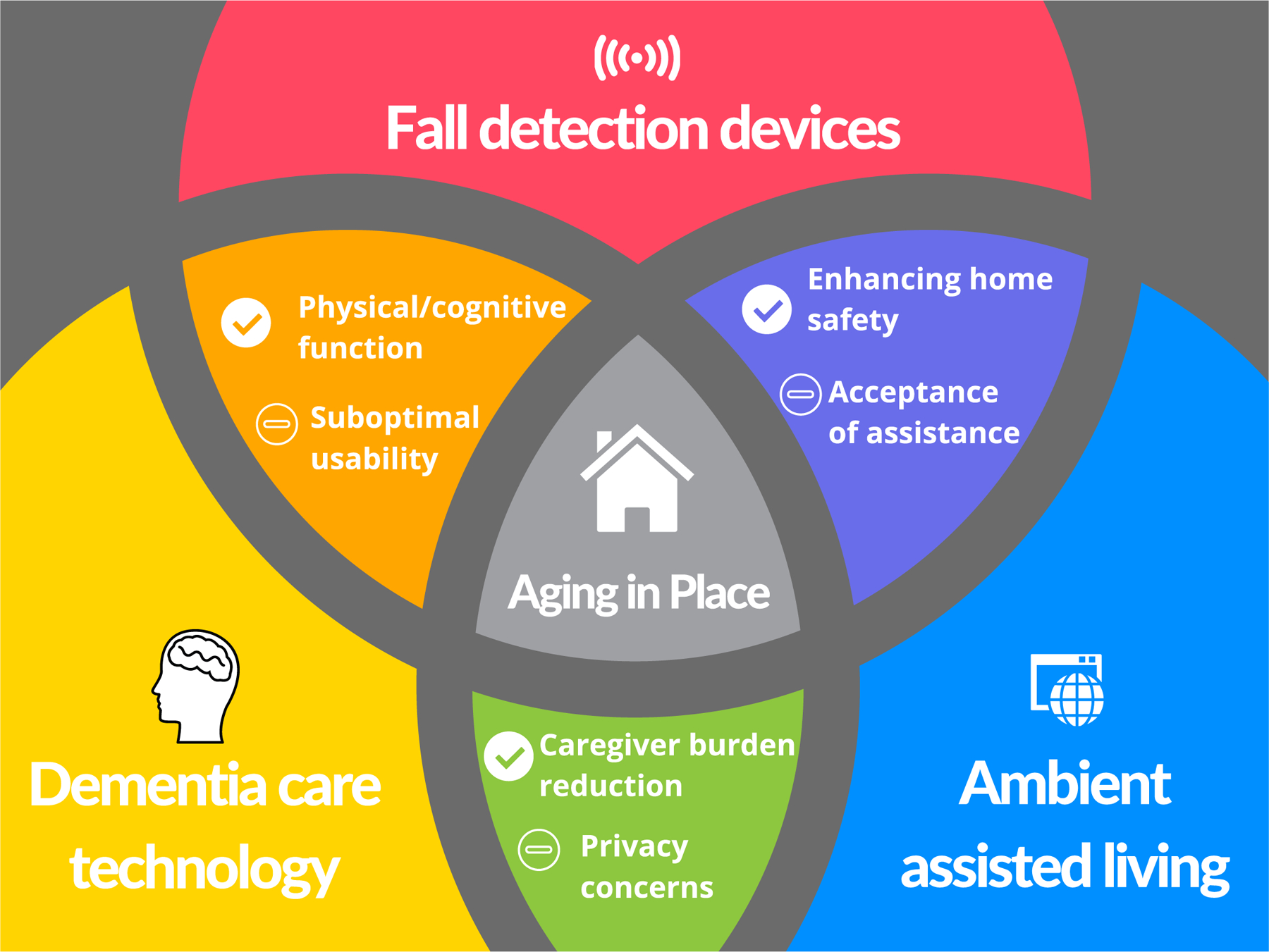
Opportunities and barriers of dementia care, fall detection devices, and ambient assisted living technologies.
Discussion
In this scoping review we examined the current evidence base on gerontechnology in dementia care, fall detection, and ambient assisted living and found that individuals and caregivers found most technologies usable and useful. Benefits included improved cognitive and psychosocial functioning for the individual and a greater sense of security for caregivers of PWDs. If accepted by older individuals, AAL has the potential to reduce the need for long-term care facilities and offset expensive home care, empowering individuals to remain in their communities and live independently longer. In turn, this could improve the lives of caregivers, who could feel more confident leaving their loved one at home and potentially retain employment out of the house instead of being available to provide care full-time.
We found several concerns about adopting technology for health still exist. Privacy concerns remain particularly among older adults who may not feel monitoring is necessary. Although some older adults benefit from having continuous monitoring, the intrusiveness of these devices may prove to be uncomfortable or even unacceptable for some populations. This finding is in line with a previously published review of the literature (van Boekel et al., 2019), and future work on digital interventions for older adults must ensure the desire for privacy is respected and not infringed upon.
Affordability is another barrier to adoption. Although the cost analyses included in this review demonstrate the cost-effectiveness of the studied interventions, relatively high up-front costs of many of these technologies often preclude their widespread adoption. In the absence of insurance coverage of these interventions, older adults may not be able to access these devices. As such, device manufacturers and insurers should work to provide older adults with reasonably priced technologies to ensure equitable access. In the United States, public and private funding sources offer coverage of some mainstream assistive technologies. Continued expansion of the range of covered technologies is a necessary step in ensuring older adults do not have to worry about affordability of assistive technologies.
Finally, many of the devices we covered are designed for specific purposes, such as fall detection, cognitive training, and remote monitoring. Because of this, older adults will likely have to use multiple health technologies to address their wide range of health concerns, which increases cost and complexity. Streamlining and consolidating these devices into the fewest number possible would reduce the amount of training necessary and could simplify the user experience. Newer consumer devices, such as the Apple Watch (2020 Apple Inc., Cupertino, CA), may be able to serve as a model of integrated health monitoring devices for older adults, as it combines fall detection and reporting with heart rate monitoring, a pedometer, and other health applications.
Strengths and limitations
Although our search strategy followed best practices for scoping reviews it focused on topics of chief concern to older persons and their caregivers — dementia care, fall detection, and ambient assisted living — and findings are therefore not generalizable to all gerontechnologies. Although this review highlights knowledge gaps regarding technology and ‘aging in place,’ which will help guide future research, our findings are limited by the methodological quality of the included studies. Given the heterogeneity of the included studies and a lack of side-by-side comparisons, we were unable to suggest some technologies as superior to others. Although efforts were made to follow scoping review guidelines, readers should note that there is not one accepted and universally followed methodology for these reviews (Pham et al., 2014). Finally, many studies did not assess long-term outcomes, and therefore readers will need to ascertain on their own whether the reported short-term benefits outweigh the potential downsides of cost.
Future directions
This scoping review contributes important new information regarding the use of gerontechnology in older adults ‘aging in place’ and highlights several notable gaps in the literature. Because most included studies were pilot, observational, or qualitative studies focusing on feasibility and acceptability and short-term outcomes, more randomized controlled trials and studies comparing technologies are needed. Additionally, although this review included two cost analyses, additional investigations should prioritize analyzing the cost-effectiveness of these innovations for older adults, their caregivers, and healthcare systems. Once a technology is found to be beneficial, studies examining implementation techniques to enhance the uptake of technology among older adults who may benefit will be critical.
In the area of dementia care, more studies should focus on how assistive technologies can foster or maintain a sense of human connection. Many of the studies we have examined highlighted the measurable benefits to cognitive and physical functioning, but only two (Hattink et al., 2016; Silva et al., 2017) evaluated their impact on PWDs’ quality of life. Additionally, further research is needed on how best to orient PWDs to new technologies and ease their adoption.
In this review, we identified a shortage of user-centered fall detection devices research. Although the devices tested were able to detect falls with high levels of sensitivity, individuals cited concerns about usability, poor battery life, obtrusiveness, and unacceptably high false positive rates. Consequently, future fall detection research should focus on understanding the user experience, incorporating user feedback into device designs, and minimizing false positives.
AAL technologies have great potential as they can detect abnormal and potentially dangerous activity and can monitor the physical and cognitive health of older adults. This could open research horizons in telemedicine if the data can be efficiently summarized, routed to the necessary parties, and synthesized into a treatment plan. AAL technologies could also offer a more reliable method to detect cognitive decline or a decrease in the ability to perform ADLs without depending on self-report, which can be burdensome for individuals and their families. Research progress in these key domains could ensure that technologies that monitor and enhance health for older adults is made available and is a necessary step before clinicians endorse them as health devices.
Conclusion
As the population of older adults increases and caregivers become less available, technology could enable ‘aging in place.’ Progress has been made in dementia care, fall detection, and home supports. We found that technology can improve ADLs, cognitive and psychosocial status, home safety, and caregiver burden. Wearable sensor data could be used by clinicians for disease prevention, diagnosis, and treatment in addition to use for self-monitoring. Future gerontechnology research must focus on addressing privacy concerns, enhancing usability for older adults with varying abilities, and addressing drawbacks of the currently available technology such as poor battery life and insufficient accuracy. If these concerns are addressed, technology could be a valuable tool to promote independence into late life.
Supplementary Material
Funding:
CG’s role in this publication was made possible by the Yale National Clinician Scholars Program and by CTSA Grant Number TL1 TR001864 from the National Center for Advancing Translational Science (NCATS), a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH. EG received support from the National Institute on Aging (K76AG059983). The funders had no role in the design or conduct of the study; collection, management, analysis, and interpretation of the data; and preparation or approval of the manuscript.
Footnotes
Declaration of Conflicting Interests:
The authors declare that there is no conflict of interest.
References
- Aanesen M, Lotherington AT, & Olsen F (2011). Smarter elder care? A cost-effectiveness analysis of implementing technology in elder care. Health Informatics Journal, 17(3), 161–172. 10.1177/1460458211409716 [DOI] [PubMed] [Google Scholar]
- AARP. (2019). AARP family caregiving consumer insights guide 2019. https://www.aarp.org/content/dam/aarp/caregiving/2019/09/aarp-price-of-caring-resource-guide.pdf
- Adcock M, Fankhauser M, Post J, Lutz K, Zizlsperger L, Luft AR, …de Bruin ED (2020). Effects of an in-home multicomponent exergame training on physical functions, cognition, and brain volume of older adults: A randomized controlled trial. Frontiers in Medicine, 6. 10.3389/fmed.2019.00321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amjad I, Toor H, Niazi IK, Pervaiz S, Jochumsen M, Shafique M, …Ahmed T (2019). Xbox 360 kinect cognitive games improve slowness, complexity of EEG, and cognitive functions in subjects with mild cognitive impairment: A randomized control trial. Games for Health Journal, 8(2), 144–152. 10.1089/g4h.2018.0029 [DOI] [PubMed] [Google Scholar]
- Anderson M, & Perrin A (2017). Tech adoption climbs among older adults. https://www.pewresearch.org/internet/2017/05/17/tech-adoption-climbs-among-older-adults/
- Appel L, Appel E, Bogler O, Wiseman M, Cohen L, Ein N, …Campos JL (2019). Older adults with cognitive and/or physical impairments can benefit from immersive virtual reality experiences: A feasibility study. Frontiers in Medicine, 6, 329. 10.3389/fmed.2019.00329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asghar I, Cang S, & Yu H (2018). Usability evaluation of assistive technologies through qualitative research focusing on people with mild dementia. Computers in Human Behavior, 79, 192–201. 10.1016/j.chb.2017.08.034 [DOI] [Google Scholar]
- Astell AJ, Bouranis N, Hoey J, Lindauer A, Mihailidis A, Nugent C, & Robillard JM Technology and dementia: the future is now. Dement Geriatr Cogn Disord. 2019;47(3):131–139. 10.1159/000497800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baik G (2019). How AI is helping predict and prevent senior falls. https://healthtechmagazine.net/article/2019/08/how-ai-helping-predict-and-prevent-senior-falls
- Baric V, Andreassen M, Ohman A, & Hemmingsson H (2019). Using an interactive digital calendar with mobile phone reminders by senior people - A focus group study. BMC Geriatrics, 19(1), 116. 10.1186/s12877-019-1128-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batsis JA, Zagaria A, Kotz DF, Bartels SJ, Boateng GG, Proctor PO, …Carpenter-Song EA (2018). Usability evaluation for the Amulet Wearable Device in rural older adults with obesity. Gerontechnology, 17(3), 151–159. 10.4017/gt.2018.17.3.003.00 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Sadoun G, Sacco G, Manera V, Bourgeois J, König A, Foulon P, …Robert P (2016). Physical and cognitive stimulation using an exergame in subjects with normal aging, mild and moderate cognitive impairment. Journal of Alzheimer’s Disease, 53(4), 1299–1314. 10.3233/JAD-160268 [DOI] [PubMed] [Google Scholar]
- Bergen G, Stevens MR, & Burns ER (2016). Falls and fall injuries among adults aged ≥65 years — United States, 2014. Morbidity and Mortality Weekly Report, 65(37), 993–998. 10.15585/mmwr.mm6537a2 [DOI] [PubMed] [Google Scholar]
- Berridge C, Chan KT, & Choi Y (2019). Sensor-based passive remote monitoring and discordant values: Qualitative study of the experiences of low-income immigrant elders in the United States. JMIR mHealth uHealth, 7(3), e11516. 10.2196/11516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown EL, Ruggiano N, Li J, Clarke PJ, Kay ES, & Hristidis V (2019). Smartphone-based health technologies for dementia care: opportunities, challenges, and current practices. J Appl Gerontol, 38(1), 73–91. 10.1177/0733464817723088 [DOI] [PubMed] [Google Scholar]
- Burns ER, Stevens JA, & Lee R (2016). The direct costs of fatal and non-fatal falls among older adults - United States. J Safety Res, 58, 99–103. 10.1016/j.jsr.2016.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudhuri S, Kneale L, Le T, Phelan E, Rosenberg D, Thompson H, & Demiris G (2017). Older adults’ perceptions of fall detection devices. J Appl Gerontol, 36(8), 915–930. 10.1177/0733464815591211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen C, Kampel T, & Verloo H (2016). Acceptability of an intelligent wireless sensor system for the rapid detection of health issues: Findings among home-dwelling older adults and their informal caregivers. Patient Preference and Adherence, 10, 1687–1695. 10.2147/PPA.S113805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colombo F, Llena-Nozal A, Mercier J, & Tjadens F (2011). Help wanted? 10.1787/9789264097759-en [DOI]
- Costa SE, Rodrigues JJ, Silva BM, Isento JN, & Corchado JM (2015). Integration of wearable solutions in AAL environments with mobility support. J Med Syst, 39(12), 184. 10.1007/s10916-015-0342-z [DOI] [PubMed] [Google Scholar]
- Croff RL, Witter PIV, Walker ML, Francois E, Quinn C, Riley TC, …Kaye JA (2019). Things are changing so fast: Integrative technology for preserving cognitive health and community history. The Gerontologist, 59(1), 147–157. 10.1093/geront/gny069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darragh M, Ahn HS, MacDonald B, Liang A, Peri K, Kerse N, & Broadbent E (2017). Homecare robots to improve health and well-being in mild cognitive impairment and early stage dementia: Results from a scoping study. J Am Med Dir Assoc, 18(12), 1099.e1091–1099.e1094. 10.1016/j.jamda.2017.08.019 [DOI] [PubMed] [Google Scholar]
- Demiris G, Chaudhuri S, & Thompson HJ (2016). Older adults’ experience with a novel fall detection device. Telemed J E Health, 22(9), 726–732. 10.1089/tmj.2015.0218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dethlefs N, Milders M, Cuayáhuitl H, Al-Salkini T, & Douglas L (2017). A natural language-based presentation of cognitive stimulation to people with dementia in assistive technology: A pilot study. Inform Health Soc Care, 42(4), 349–360. 10.1080/17538157.2016.1255627 [DOI] [PubMed] [Google Scholar]
- Di Rosa M, Hausdorff JM, Stara V, Rossi L, Glynn L, Casey M, …Cherubini A (2017). Concurrent validation of an index to estimate fall risk in community dwelling seniors through a wireless sensor insole system: A pilot study. Gait Posture, 55, 6–11. 10.1016/j.gaitpost.2017.03.037 [DOI] [PubMed] [Google Scholar]
- Djabelkhir L, Wu YH, Vidal JS, Cristancho-Lacroix V, Marlats F, Lenoir H, …Rigaud AS (2017). Computerized cognitive stimulation and engagement programs in older adults with mild cognitive impairment: Comparing feasibility, acceptability, and cognitive and psychosocial effects. Clin Interv Aging, 12, 1967–1975. 10.2147/cia.S145769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupuy L, Froger C, Consel C, & Sauzéon H (2017). Everyday functioning benefits from an assisted living platform amongst frail older adults and their caregivers. Frontiers in Aging Neuroscience, 9. 10.3389/fnagi.2017.00302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ejupi A, Brodie M, Lord SR, Annegarn J, Redmond SJ, & Delbaere K (2017). Wavelet-based sit-to-stand detection and assessment of fall risk in older people using a wearable pendant device. IEEE Trans Biomed Eng, 64(7), 1602–1607. 10.1109/tbme.2016.2614230 [DOI] [PubMed] [Google Scholar]
- Epstein I, Aligato A, Krimmel T, & Mihailidis A (2016). Older adults’ and caregivers’ perspectives on in-home monitoring technology. Journal of Gerontological Nursing, 42(6), 43–50. 10.3928/00989134-20160308-02 [DOI] [PubMed] [Google Scholar]
- Farina N, Sherlock G, Thomas S, Lowry RG, & Banerjee S (2019). Acceptability and feasibility of wearing activity monitors in community-dwelling older adults with dementia. International Journal of Geriatric Psychiatry, 34(4), 617–624. 10.1002/gps.5064 [DOI] [PubMed] [Google Scholar]
- Finch M, Griffin K, & Pacala JT (2017). Reduced healthcare use and apparent savings with passive home monitoring technology: A pilot study. J Am Geriatr Soc, 65(6), 1301–1305. 10.1111/jgs.14892 [DOI] [PubMed] [Google Scholar]
- Fischinger D, Einramhof P, Papoutsakis K, Wohlkinger W, Mayer P, Panek P, …Vincze M (2016). Hobbit, a care robot supporting independent living at home: First prototype and lessons learned. Robotics and Autonomous Systems, 75(Part A), 60–78. 10.1016/j.robot.2014.09.029 [DOI] [Google Scholar]
- Forsyth K, Henderson C, Davis L, Singh Roy A, Dunk B, Curnow E, …Howard R (2019). Assessment of need and practice for assistive technology and telecare for people with dementia—The ATTILA (assistive technology and telecare to maintain independent living at home for people with dementia) trial. Alzheimer’s and Dementia: Translational Research and Clinical Interventions, 5, 420–430. 10.1016/j.trci.2019.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganesan B, Gowda T, Al-Juamily A, Fong KNK, Meena SK, & Tong RKY Ambient assisted living technologies for older adults with cognitive and physical impairments: a review. Eur Rev Med Pharmacol Sci. 2019;23(23):10470–0481. 10.26355/eurrev_201912_19686 [DOI] [PubMed] [Google Scholar]
- Gelonch O, Ribera M, Codern-Bové N, Ramos S, Quintana M, Chico G, …Garolera M (2019). Acceptability of a lifelogging wearable camera in older adults with mild cognitive impairment: A mixed-method study. BMC Geriatrics, 19(1), 1–10. 10.1186/s12877-019-1132-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giovagnoli AR, Manfredi V, Schifano L, Paterlini C, Parente A, & Tagliavini F (2018). Combining drug and music therapy in patients with moderate Alzheimer’s disease: A randomized study. Neurological Sciences, 39(6), 1021–1028. 10.1007/s10072-018-3316-3 [DOI] [PubMed] [Google Scholar]
- Halcomb E, Purcell R, Hickman L, & Smyth E (2016). Telemonitoring is acceptable amongst community dwelling older Australians with chronic conditions. Collegian, 23(4), 383–390. 10.1016/j.colegn.2015.09.007 [DOI] [PubMed] [Google Scholar]
- Hattink BJ, Meiland FJ, Overmars-Marx T, de Boer M, Ebben PW, van Blanken M, …Dröes RM (2016). The electronic, personalizable Rosetta system for dementia care: Exploring the user-friendliness, usefulness and impact. Disabil Rehabil Assist Technol, 11(1), 61–71. 10.3109/17483107.2014.932022 [DOI] [PubMed] [Google Scholar]
- Jang I-Y, Kim HR, Lee E, Jung H-W, Park H, Cheon S-H, …Park YR (2018). Impact of a wearable device-based walking programs in rural older adults on physical activity and health outcomes: Cohort study. JMIR mHealth and uHealth, 6(11), e11335. 10.2196/11335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joe J, Hall A, Chi N-C, Thompson H, & Demiris G (2018). IT-based wellness tools for older adults: Design concepts and feedback. Informatics for Health & Social Care, 43(2), 142–158. 10.1080/17538157.2017.1290637 [DOI] [PubMed] [Google Scholar]
- Kunnappilly A, Marinescu R, & Seceleanu C (2019). A model-checking-based framework for analyzing ambient assisted living solutions. Sensors (Basel), 19(22). 10.3390/s19225057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lach HW, Lorenz RA, Palmer JL, Koedbangkham J, & Noimontree W (2019). Home monitoring to track activity and sleep patterns among older adults: A feasibility study. Comput Inform Nurs, 37(12), 628–637. 10.1097/cin.0000000000000569 [DOI] [PubMed] [Google Scholar]
- Lazarou I, Karakostas A, Stavropoulos TG, Tsompanidis T, Meditskos G, Kompatsiaris I, & Tsolaki M (2016). A novel and intelligent home monitoring system for care support of elders with cognitive impairment. Journal of Alzheimer’s disease : JAD, 54(4), 1561–1591. 10.3233/JAD-160348 [DOI] [PubMed] [Google Scholar]
- Liao YY, Tseng HY, Lin YJ, Wang CJ, & Hsu WC (2020). Using virtual reality-based training to improve cognitive function, instrumental activities of daily living and neural efficiency in older adults with mild cognitive impairment. Eur J Phys Rehabil Med, 56(1), 47–57. 10.23736/s1973-9087.19.05899-4 [DOI] [PubMed] [Google Scholar]
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, …Moher D (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ, 339, b2700. 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lie MLS, Lindsay S, & Brittain K (2016). Technology and trust: Older people’s perspectives of a home monitoring system. Ageing & Society, 36(7), 1501–1525. 10.1017/S0144686X15000501 [DOI] [Google Scholar]
- Macis S, Loi D, Ulgheri A, Pani D, Solinas G, Manna S, …Raffo L (2020). Design and usability assessment of a multi-device SOA-based telecare framework for the elderly. IEEE J Biomed Health Inform, 24(1), 268–279. 10.1109/jbhi.2019.2894552 [DOI] [PubMed] [Google Scholar]
- Megges H, Freiesleben SD, Jankowski N, Haas B, & Peters O (2017). Technology for home dementia care: A prototype locating system put to the test. Alzheimer’s and Dementia: Translational Research and Clinical Interventions, 3(3), 332–338. 10.1016/j.trci.2017.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Micera S, Bonato P, & Tamura T (2008). Gerontechnology. IEEE Engineering in Medicine and Biology Magazine, 27(4), 10–14. 10.1109/MEMB.2008.925213 [DOI] [PubMed] [Google Scholar]
- Mitchell LL, Peterson CM, Rud SR, Jutkowitz E, Sarkinen A, Trost S, …Gaugler JE (2020). “It’s like a cyber-security blanket”: The utility of remote activity monitoring in family dementia care. Journal of Applied Gerontology, 39(1), 86–98. 10.1177/0733464818760238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monekosso D, Florez-Revuelta F, & Remagnino P (2015). Ambient assisted living [Guest editors’ introduction]. IEEE Intelligent Systems, 30(4), 2–6. 10.1109/MIS.2015.63 [DOI] [Google Scholar]
- Moyle W, Jones C, Dwan T, Ownsworth T, & Sung B (2019). Using telepresence for social connection: Views of older people with dementia, families, and health professionals from a mixed methods pilot study. Aging & Mental Health, 23(12), 1643–1650. 10.1080/13607863.2018.1509297 [DOI] [PubMed] [Google Scholar]
- Nishiura Y, Nihei M, Nakamura-Thomas H, & Inoue T (2019). Effectiveness of using assistive technology for time orientation and memory, in older adults with or without dementia. Disabil Rehabil Assist Technol, 1–7. 10.1080/17483107.2019.1650299 [DOI] [PubMed] [Google Scholar]
- Petersen JD, Siersma VD, Christensen RD, Storsveen MM, Nielsen CT, & Waldorff FB The risk of fall accidents for home dwellers with dementia - a register- and population-based case-control study. Alzheimers Dement (Amst). 2018;10:421–428. 10.1016/j.dadm.2018.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pham MT, Rajić A, Greig JD, Sargeant JM, Papadopoulos A, & McEwen SA A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Synth Methods. 2014;5(4):371–385. 10.1002/jrsm.1123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzak E, Cotea C, & Pullman S Does smart home technology prevent falls in community-dwelling older adults: a literature review. Inform Prim Care. 2014;21(3):105–112. 10.14236/jhi.v21i3.64 [DOI] [PubMed] [Google Scholar]
- Pigini L, Bovi G, Panzarino C, Gower V, Ferratini M, Andreoni G, …Ferrarin M (2017). Pilot test of a new personal health system integrating environmental and wearable sensors for telemonitoring and care of elderly people at home (SMARTA Project). Gerontology, 63(3), 281–286. 10.1159/000455168 [DOI] [PubMed] [Google Scholar]
- Pino M, Boulay M, Jouen F, & Rigaud AS (2015). “Are we ready for robots that care for us?” Attitudes and opinions of older adults toward socially assistive robots. Front Aging Neurosci, 7, 141. 10.3389/fnagi.2015.00141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pol M, van Nes F, van Hartingsveldt M, Buurman B, de Rooij S, & Kröse B (2016). Older people’s perspectives regarding the use of sensor monitoring in their home. The Gerontologist, 56(3), 485–493. 10.1093/geront/gnu104 [DOI] [PubMed] [Google Scholar]
- Rantz M, Lane K, Phillips LJ, Despins LA, Galambos C, Alexander GL, …Miller SJ (2015). Enhanced registered nurse care coordination with sensor technology: Impact on length of stay and cost in aging in place housing. Nurs Outlook, 63(6), 650–655. 10.1016/j.outlook.2015.08.004 [DOI] [PubMed] [Google Scholar]
- Robert P, Manera V, Derreumaux A, Montesino MFY, Leone E, Fabre R, & Bourgeois J (2020). Efficacy of a web app for cognitive training (MeMo) regarding cognitive and behavioral performance in people with neurocognitive disorders: Randomized controlled trial. Journal of Medical Internet Research, 22(3). 10.2196/17167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohrbach N, Gulde P, Armstrong AR, Hartig L, Abdelrazeq A, Schröder S, …Hermsdörfer J (2019). An augmented reality approach for ADL support in Alzheimer’s disease: A crossover trial. J Neuroeng Rehabil, 16(1), 66. 10.1186/s12984-019-0530-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saadeh W, Butt SA, & Altaf MAB (2019). A patient-specific single sensor IoT-based wearable fall prediction and detection system. IEEE Trans Neural Syst Rehabil Eng, 27(5), 995–1003. 10.1109/tnsre.2019.2911602 [DOI] [PubMed] [Google Scholar]
- Sejunaite K, Lanza C, Ganders S, Iljaitsch A, & Riepe MW (2017). Augmented reality: Sustaining autonomous way-finding in the community for older persons with cognitive impairment. J Frailty Aging, 6(4), 206–211. 10.14283/jfa.2017.25 [DOI] [PubMed] [Google Scholar]
- Serino S, Pedroli E, Tuena C, De Leo G, Stramba-Badiale M, Goulene K, …Riva G (2017). A novel virtual reality-based training protocol for the enhancement of the “mental frame syncing” in individuals with Alzheimer’s disease: A development-of-concept trial. Frontiers in Aging Neuroscience, 9(JUL). 10.3389/fnagi.2017.00240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva AR, Pinho MS, Macedo L, Moulin C, Caldeira S, & Firmino H (2017). It is not only memory: Effects of sensecam on improving well-being in patients with mild Alzheimer disease. Int Psychogeriatr, 29(5), 741–754. 10.1017/s104161021600243x [DOI] [PubMed] [Google Scholar]
- Son H, & Kim H (2019). A pilot study to test the feasibility of a home mobility monitoring system in community-dwelling older adults. Int J Environ Res Public Health, 16(9). 10.3390/ijerph16091512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thilo FJS, Hahn S, Halfens RJG, & Schols J (2019). Usability of a wearable fall detection prototype from the perspective of older people-A real field testing approach. J Clin Nurs, 28(1–2), 310–320. 10.1111/jocn.14599 [DOI] [PubMed] [Google Scholar]
- van Boekel LC, Wouters EJM, Grimberg BM, van der Meer NJM, & Luijkx KG (2019). Perspectives of stakeholders on technology use in the care of community-living older adults with dementia: A systematic literature review. Healthcare (Basel, Switzerland), 7(2), 73. 10.3390/healthcare7020073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. (2008). WHO global report on falls prevention in older age. World Health Organization. https://www.who.int/ageing/publications/Falls_prevention7March.pdf [Google Scholar]
- WHO. (2019). Dementia. World Health Organization. Retrieved April 26 from https://www.who.int/news-room/fact-sheets/detail/dementia [Google Scholar]
- Wiles JL, Leibing A, Guberman N, Reeve J, & Allen RE (2012). The meaning of “aging in place” to older people. Gerontologist, 52(3), 357–366. 10.1093/geront/gnr098 [DOI] [PubMed] [Google Scholar]
- Wolters MK, Kelly F, & Kilgour J (2016). Designing a spoken dialogue interface to an intelligent cognitive assistant for people with dementia. Health Informatics J, 22(4), 854–866. 10.1177/1460458215593329 [DOI] [PubMed] [Google Scholar]
- Wu Y-H, Cristancho-Lacroix V, Fassert C, Faucounau V, de Rotrou J, & Rigaud AS (2016). The attitudes and perceptions of older adults with mild cognitive impairment toward an assistive robot. Journal of Applied Gerontology, 35(1), 3–17. 10.1177/0733464813515092 [DOI] [PubMed] [Google Scholar]
- Zając-Lamparska L, Wiłkość-Dębczyńska M, Wojciechowski A, Podhorecka M, Polak-Szabela A, Warchoł Ł, …Izdebski P (2019). Effects of virtual reality-based cognitive training in older adults living without and with mild dementia: A pretest-posttest design pilot study. BMC Res Notes, 12(1), 776. 10.1186/s13104-019-4810-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


