Abstract
Background
External auditory canal (EAC) osteomas are rare, slow-growing benign neoplasms. Microscopic surgical excision had been reported for symptomatic osteomas. However, there was no study published on the feasibility of transcanal endoscopic ear surgery (TEES) for EAC osteoma. In this study, we propose two methods of TEES for symptomatic EAC osteomas and report the surgical outcomes of our patients.
Methods
Fifteen patients diagnosed with symptomatic EAC osteoma who underwent TEES were recruited at two otolaryngology referral centers. The extent of osteoma and degree of EAC stenosis was calculated based on high-resolution computed tomography (HRCT) imaging. We divided all the patients into two groups, solitary pedunculated osteoma or broad-based osteomas. The postoperative outcomes and complications were recorded for at least 6 months of outpatient follow-up.
Results
In this study, twelve patients with solitary osteoma underwent the first method, a direct transcanal removal procedure. In this approach, only a small bare bony area remained postoperatively, and it healed completely within 1 month. Three patients with broad based osteoma underwent the second method, a transcanal approach involving a skin flap. The degree of stenosis in all patients ranged from 29% to 90%. All of them could be treated completely through a transcanal endoscopic approach. No intraoperative or postoperative complications were noted during follow-up, and no canal stenosis and no recurrences were noted during at least 6 months of follow-up.
Conclusions
This endoscopic transcanal approach to EAC osteomas demonstrated good results for lesion removal without recurrence or intraoperative complications.
Keywords: Osteoma, External auditory canal, Endoscopic ear surgery
At a glance of commentary.
Scientific background on the subject
The external auditory canal osteomas were treated by microscopic surgical procedures with postauricular, transmeatal, and endaural pathways, rarely reported by the endoscopic approach. The present study reported the exclusive transcanal endoscopic approach to remove various-sized and location of the external auditory canal osteomas.
What this study adds to the field
The study demonstrated good results with endoscopic transcanal approach to the external auditory canal osteomas removal with both techniques, ie the direct method for a solitary pedunculated osteoma and a skin flap for a broad-based osteoma, which avoids retro-auricular approach by cutting the auricle.
External auditory canal (EAC) osteomas are rare, slow-growing benign neoplasms that are generally unilateral, solitary, and pedunculated [1]. They typically originate from the tympanomastoid or tympanosquamous suture lines adjacent to the bony–cartilaginous junction [2,3]. However, their etiology remains unknown. Histologically, osteoma is covered by periosteum and squamous epithelium and consists of discrete fibrovascular channels surrounded by dense lamellar bone with irregular direction [4,5]. Osteomas of the EAC often grow slowly and remain asymptomatic for many years. Symptoms can arise if the EAC becomes obstructed, narrowed by concurrent lesions such as cholesteatomas [6] and/or infected.
Several studies have been published discussing the management of EAC osteomas [1,2,[6], [7], [8], [9]]. Microscopic surgical procedures can be performed by different approaches, including postauricular, transcanal, and endaural pathways, which are chosen depending on the location and size of the EAC osteoma and the severity of the symptoms. When an osteoma is pedunculated and lateral to the isthmus, it can be removed easily by an osteotome or by drilling through the transmeatal approach. If an osteoma is very large, broad based and located medial to the isthmus, excision through the postauricular approach is recommended [1,6,8,9].
In recent years, with the advent of endoscopy for ear surgery and increasing experience using this technology, transcanal endoscopic ear surgery (TEES) has been applied to different ear surgeries to minimize invasive approaches and avoid the need for a postauricular incision [10,11]. To date, no study has been published on the feasibility of TEES for EAC osteoma. In this study, we present our experience in the endoscopic management of EAC osteoma using two methods and report the surgical outcomes of our patients.
Materials and methods
Participants
Fifteen patients who presented with obvious symptoms such as hearing loss and aural fullness and were diagnosed with EAC osteoma from January 2010 to June 2019 were enrolled from two otolaryngology referral centers. All of them underwent TEES procedures for the removal of EAC osteoma under general anesthesia. The preoperative symptoms, location, and size of the EAC osteoma were recorded. The extent of osteoma was calculated based on high-resolution computed tomography (HRCT) images. The degree of stenosis was the maximum measurement available of the lesion as a percentage of the maximum diameter of the EAC in axial and coronal view cuts. The preoperative HRCT was also carefully assessed to determine the morphology and comorbidity of the EAC osteoma and to judge whether the osteoma had a pedicle attached to the EAC.
Representative surgical techniques: two surgical methods
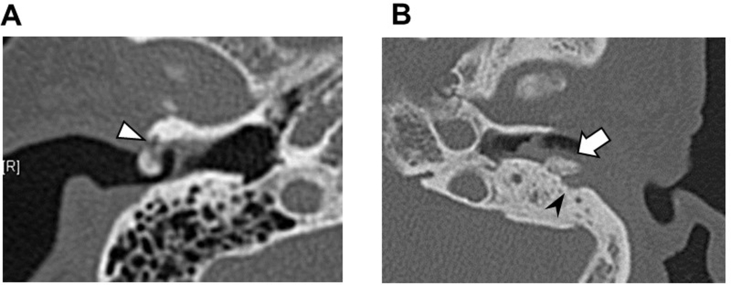
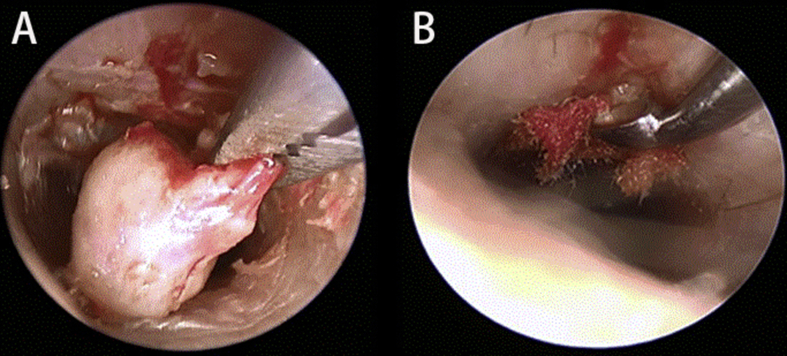
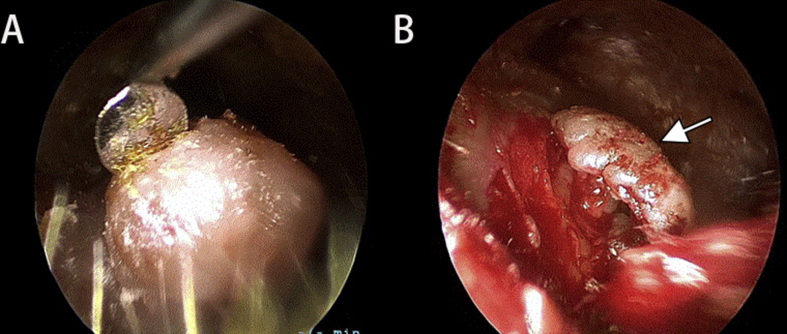
We performed all TEES procedures using a rigid endoscope with a 14-cm length, 3- or 4-mm diameter, and 0° viewing angle (Karl Storz, Tuttlingen, Germany). In addition to general anesthesia, local anesthetic agents containing a vasoconstrictor (e.g., a mixture of 1% lidocaine and 1:100,000 epinephrine) were infiltrated around the lesion to reduce intraoperative bleeding. To remove EAC osteomas through TEES, two surgical methods were designed depending on the characteristics and morphology of the osteoma. The first method was direct transcanal removal, which was suitable for osteomas connected to the EAC by a small stalk. If preoperative HRCT of the temporal bone revealed a small pedicle between the osteoma and EAC [Fig. 1A], the osteoma could be easily broken using a curette, followed by alligator forceps for taking out and lastly by a curette for removal of the residual bony stalk [Fig. 2]. In addition to preoperative imaging, we propose the use of curettes for perioperative mobility-dependent differentiation between pedunculated and broad-based osteomas. The second method used in this study was a transcanal removal involving a skin flap; this procedure was suitable for broad-based osteomas without an obvious stalk attached to the EAC [Fig. 1B]. Under a transcanal endoscope, a skin flap was made around the osteoma using a round knife until the tumor was completely exposed. The skin flap was then elevated and mobilized laterally, allowing the osteoma to be excised completely with a curette or a gauge blade. The skin flap was then returned to its original position [Fig. 3]. At the end of both procedures, the EACs were packed with Gelfoam, which was removed during outpatient follow-up.
Fig. 1.
Axial high-resolution computed tomography (HRCT) views of representative cases of osteoma. (A) Pedunculated osteoma (B) Broad-based osteoma. White arrowhead indicates that the osteoma had an obvious stalk attached to the ear canal. White arrow indicates that the osteoma had a broad base. Black arrowhead means concurrent cholesteatoma invaded the bony wall of external ear canal.
Fig. 2.
A representative case of an osteoma resected by direct removal in transcanal endoscopic ear surgery (TEES).
Fig. 3.
A representative case with the skin flap mobilized laterally and repositioned after removing the osteoma by transcanal endoscopic ear surgery (TEES).
The surgical outcomes, including the recurrence rate, the rate of postoperative complications and postoperative canal stenosis, were observed and recorded for at least 6 months of postoperative follow-up in the outpatient department.
Results
Fifteen patients (8 men and 7 women, aged between 27 and 71 years) who were diagnosed with EAC osteoma and underwent TEES were included in this study. The demographic characteristics of all patients with EAC osteoma are shown in [Table 1]. The most common symptoms of EAC osteoma are hearing impairment (47%, 7/15) and aural fullness (33%, 5/15). Most osteomas in our study originated lateral to the isthmus of EAC. The degree of stenosis in all patients ranged from 29% to 90%. Half of the patients had more than 50% EAC stenosis. Most of the patients (twelve patients) underwent the first TEES method of direct transcanal removal. The other three patients underwent a second surgical method involving a skin flap. All of them could be treated completely by TEES.
Table 1.
Patient demographics, surgical Procedures, and complications.
| No. | Gender | Age (y) | Location | Lesion Side |
Symptoms/signs | Operative finding | Degree of stenosis | Surgical method (TEES) | Complication |
|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 66 | Lateral | Left | Itching ear | Osteoma | 29% | First | None |
| 2 | M | 31 | Lateral | Left | Hearing impairment | Osteoma with cerumen | 74% | First | None |
| 3 | M | 55 | Lateral | Right | Hearing impairment | Osteoma with cerumen | 78% | First | None |
| 4 | F | 71 | Lateral | Left | Hearing impairment & aural fullness |
Osteoma with cholesteatoma | 65% | Second | None |
| 5 | F | 76 | Medial | Left | Hearing impairment | Osteoma with cholesteatoma | 37% | Second | None |
| 6 | F | 54 | Lateral | Right | Aural fullness | Osteoma with cerumen | 60% | First | None |
| 7 | M | 30 | Lateral | Right | Itching ear | Osteoma | 32% | First | None |
| 8 | M | 50 | Lateral | Left | Hearing impairment & Otalgia |
Osteoma with cholesteatoma | 42% | First | None |
| 9 | F | 45 | Lateral | Left | Otorrhea | Osteoma with cholesteatoma | 47% | First | None |
| 10 | M | 35 | Medial | Right | Otalgia | Osteoma with cerumen | 33% | First | None |
| 11 | M | 37 | Lateral | Right | Aural fullness | Osteoma | 80% | Second | None |
| 12 | M | 27 | Lateral | Left | Aural fullness | Osteoma with cerumen | 90% | First | None |
| 13 | F | 53 | Lateral | left | Hearing impairment | Osteoma with cerumen | 75% | First | None |
| 14 | M | 68 | Lateral | Left | Hearing impairment | Osteoma with cerumen | 68% | First | None |
| 15 | F | 43 | Lateral | Right | Aural fullness | Osteoma with cerumen | 73% | First | None |
Abbreviation: TEES: Transcanal endoscopic ear surgery. Surgical method: first, direct transcanal removal; second, transcanal removal with a skin flap.
There were two patients with solitary pedunculated osteomas without concurrent cerumen or cholesteatoma patients number 1 and 7 in [Table 1]. The degree of stenosis of the osteoma was 29% and 32%, respectively. Because the osteoma was attached to the EAC by fibrotic connective tissue and a small bony stalk, we removed it directly using a curette and a large round knife. Eight patients were diagnosed with osteomas with concurrent cerumen numbers 2, 3, 6, 10, 12, 13, 14 and 15 in [Table 1]; in these cases, the degree of stenosis ranged from 33% to 90%. The osteomas were excised through the direct transcanal approach of the first method. The accompanying cerumen could be easily cleaned up after excision of the osteoma. Two other patients were diagnosed with osteoma plus EAC cholesteatoma and entrapped cerumen and debris numbers 8 and 9 in [Table 1]. Preoperative HRCT revealed that EAC cholesteatoma involved the floor of EAC. The cerumen and debris were removed first to define the border and dimension of the osteoma. Next, we excised the sac of cholesteatoma completely because the cholesteatoma could invade local neighboring soft tissues, such as the mastoid cavity mucosa and facial nerve [12]. Finally, the osteoma was separated from the EAC using a curette. The aforementioned twelve patients underwent the first operative method, direct transcanal removal, and the small bare bony region that remained postoperatively healed completely within 1 month.
A total of three patients underwent the second surgical method, excision of osteoma with a skin flap. A 71-year-old female patient number 4 in [Table 1] initially presented with hearing impairment and aural fullness that had not improved with outpatient treatment by ENT clinics. Examination of left ear revealed a hard mass connected to the posterior-inferior wall of her EAC with a broad base. Besides, concurrent cholesteatoma involved the floor of EAC and the sclerotic bone of the mastoid [Fig. 1B]. Thus, direct transcanal removal would cause a large, exposed skin defect; hence, surgery was performed using the second method, transcanal removal involving a skin flap, to limit the exposure of the bare bony region and decrease the risk of complications involving postoperative canal stenosis. Cholesteatomas were treated by limited canalplasty and the defect was covered with tragal perichondrium/cartilage postoperatively.
None of the 15 patients demonstrated intraoperative complications, such as sensorineural hearing loss, vertigo, and facial palsy. There were no postoperative complications, such as canal stenosis, and no recurrences of osteoma or EAC cholesteatoma were found during 6-month follow-up.
Discussion
This study is the first to discuss the endoscopic removal of EAC osteoma. We proposed two methods of endoscopic transcanal removal of fifteen EAC osteomas. Twelve patients were diagnosed with a solitary osteoma with a pedicle, and they underwent the first surgical method of direct endoscopic transcanal removal. The other three patients, who had broad-based osteomas, underwent the second surgical method of endoscopic transcanal removal with a skin flap. No perioperative or postoperative complications were found in our series. In addition, no recurrences and no postoperative canal stenosis were found in our patients during 6-month follow-up.
The typical clinical features of EAC osteomas overlap those of EAC exostosis externa; therefore, the distinction between these two conditions has been frequently overlooked. However, they have different radiological and histopathological characteristics. Histologically, osteomas have internal fibrovascular channels surrounded by irregularly oriented lamellated bone. Radiologically, EAC osteomas usually appear as solitary, pedunculated, well-circumscribed lesions with high attenuation, equivalent to that of bone density, in CT images [13,14]. However, exostoses externa are generally multiple, bilateral, symmetrical bony elevations attached to the EAC with a broad base. They are relatively close to the tympanic membrane and are characterized by parallel concentric layers of subperiosteal bone [7,15]. CT is also usually useful for defining the association between lesion size and the surrounding tissue [16]. Therefore, preoperative imaging is valuable for the differential diagnosis of osteoma and exostosis.
EAC osteomas are typically asymptomatic and can be monitored without any treatment. However, surgery remains the choice of treatment when symptoms, such as conductive hearing loss, recurrent infection secondary to cerumen impaction or a cholesteatoma, become prominent. Microscopic ear surgery has been the conventional procedure used to treat EAC osteomas. The size and location of the osteoma determine the surgical approach. Sheehy et al. [9] reported that EAC osteomas could be surgically removed through two microscopic approaches, the choice of which depended on their location. When EAC osteomas originated lateral to the isthmus of the EAC, they could be removed under local anesthesia using a transmeatal approach. The postauricular approach under general anesthesia was recommended if the osteomas originated medial to the isthmus. Grinblat at al. [8]. also proposed two surgical approaches in canalplasty for exostosis and osteoma of the EAC depending on the size of the lesion. A simple transcanal approach was applicable if the size was less than 50% stenosis, whereas a retroauricular-transcanal approach was advised if the stenosis was greater than 50%. In 2015, Dr. Kozin et al. [17] reported four cases of EAC exostosis and all of them were successfully removed with osteotome and facial nerve monitor through endoscopic transcanal approach. Besides, skin graft was not necessary in two cases (2/4, 50%) because of the skin saving technique. In the present study, we reported 15 cases with EAC osteoma which were treated endoscopically by two kinds of methods. Because of skin preservation, all patients did not need skin graft after the surgery. There was no intraoperative or postoperative complications found and shorten the operation time with endoscopic canalplasty.
The use of TEES in otologic surgery has recently gained popularity, and it could be feasibly applied to the treatment of EAC osteomas in this study. By using a curette, EAC osteomas with a pedicle could be easily removed by the first method. However, it is difficult to mobilize a broad-based osteoma, and the second method with a skin flap is recommended. All osteomas in our cases were removed through a transcanal endoscopic approach, regardless of the size of the lesion.
Compared with a microscopic approach of EAC osteomas, endoscopic approach has some advantages. First, it can reduce the operative time, including set-up and procedural time [17]. In the second place, TEES promises better tissue preservation and avoid extra postauricular skin incision and tissue damage. Third, TEES provides a wider view of the surgical field, increased visibility around the corner of the target objects, and less hidden space [10]. Thus, osteomas and concomitant lesions such as cerumen and cholesteatomas can be removed simultaneously with limited canalplasty or without canalplasty In contrast, microscopy provides a straight-line view and may result in a blind corner during surgery. Sometimes canalplasty may be considered to widen the external ear canal. Therefore, it is a less time-intensive procedure for the treatment of concurrent lesions in patients with EAC osteomas. However, if the cholesteatoma involves large area of mastoid cavity/ossicles, retroauricular approach with microscope is suggested with bimanual techniques and benefit to reconstruct after canalplasty/ossiculoplasty. However, there are still some drawbacks of endoscopic approach, such as one-handed surgery, the need to fit instruments around the endoscope, and the potential injuries by heat of the tip of the endoscope. Sometimes, the endoscope holder is needed to allow two-handed surgery to overcome the limitation of one-handed surgery, [18]. Besides, an assistant to hold the endoscope is another option. Because of the characteristics of EAC osteomas, one-handed endoscopic surgery was feasible, and the osteomas could be easily removed using appropriate instruments. Loss of stereoscopic vision is also an issue. Move the endoscope slowly during the operation can overcome this problem. If osteoma is complicated with ossicular chain disruption, 3D endoscopic imaging system may be a good choice to manage delicate and complicated structures [19].
There are some limitations of this study. This study included only 15 patients of EAC osteoma. It is too small sample size and two referral centers only. In the future, large series of case study is suggested for comparison the surgical outcomes of EAC osteoma with microscopic and endoscopic approaches.
Conclusion
In this study, we have proposed two TEES procedures as alternatives to a conventional microscopic approach for EAC osteomas: direct transcanal removal and transcanal removal involving a skin flap. TEES for EAC osteoma demonstrated good results, including lesion removal with no eventful recurrences or intraoperative complications such as sensorineural hearing loss, vertigo, and facial palsy. TEES may provide a wider-angled view of the surgical field and increase tissue preservation, avoiding the postauricular approach regardless of the size of the osteoma.
Funding
The authors disclose receipt of the following financial support for the research, authorship, and/or publication of this article. This work was supported, in part, by the Ministry of Science and Technology (MOST 108-2314-B-182A-109) and Chang Gung Memorial Hospital, Taiwan (CMRPG3J0701 and CORPG3F0851).
Conflicts of interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Footnotes
Peer review under responsibility of Chang Gung University.
References
- 1.Ebelhar A.J., Gadre A.K. Osteoma of the external auditory canal. Ear Nose Throat J. 2012;91:96–100. doi: 10.1177/014556131209100304. [DOI] [PubMed] [Google Scholar]
- 2.Hsiao S.H., Liu T.C. Osteoma of the external ear canal. Otol Neurotol. 2003;24:960. doi: 10.1097/00129492-200311000-00025. [DOI] [PubMed] [Google Scholar]
- 3.Yuen H.W., Chen J.M. External auditory canal osteoma. Otol Neurotol. 2008;29:875–876. doi: 10.1097/mao.0b013e318161aaf8. [DOI] [PubMed] [Google Scholar]
- 4.Fenton J.E., Turner J., Fagan P.A. A histopathologic review of temporal bone exostoses and osteomata. Laryngoscope. 1996;106:624–628. doi: 10.1097/00005537-199605000-00020. [DOI] [PubMed] [Google Scholar]
- 5.Lizuka T., Haruyama T., Nagaya K. Large osteoma of the external auditory canal. Ear Nose Throat J. 2013;92:286–290. doi: 10.1177/014556131309200703. [DOI] [PubMed] [Google Scholar]
- 6.Lee D.H., Jun B.C., Park C.S., Cho K.J. A case of osteoma with cholesteatoma in the external auditory canal. Auris Nasus Larynx. 2005;32:281–284. doi: 10.1016/j.anl.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 7.Kemink J.L., Graham M.D. Osteomas and exostoses of the external auditory canal - medical and surgical management. J Otolaryngol. 1982;11:101–106. [PubMed] [Google Scholar]
- 8.Grinblat G., Prasad S.C., Piras G., He J., Taibah A., Russo A. Outcomes of drill canalplasty in exostoses and osteoma: analysis of 256 cases and literature review. Otol Neurotol. 2016;37:1565–1572. doi: 10.1097/MAO.0000000000001239. [DOI] [PubMed] [Google Scholar]
- 9.Sheehy J.L. Diffuse exostoses and osteomata of the external auditory canal: a report of 100 operations. Otolaryngol Head Neck Surg. 1982;90:337–342. [PubMed] [Google Scholar]
- 10.Marchioni D., Alicandri-Ciufelli M., Mattioli F., Nogeira J.F., Tarabichi M., Villari D. From external to internal auditory canal: surgical anatomy by an exclusive endoscopic approach. Eur Arch Oto-Rhino-Laryngol. 2013;270:1267–1275. doi: 10.1007/s00405-012-2137-x. [DOI] [PubMed] [Google Scholar]
- 11.Chen C.K., Hsieh L.C. Clinical outcomes of exclusive transcanal endoscopic tympanoplasty with tragal perichondrium in 129 patients. Clin Otolaryngol. 2018;43:1624–1628. doi: 10.1111/coa.13197. [DOI] [PubMed] [Google Scholar]
- 12.Kuo C.L., Shiao A.S., Yung M., Sakagami M., Sudhoff H., Wang C.H. Updates and knowledge gaps in cholesteatoma research. BioMed Res Int. 2015;2015:854024. doi: 10.1155/2015/854024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ramirez-Camacho R., Vicente J., Garcia Berrocal J.R., Ramon Y., Cajal S. Fibro-osseous lesions of the external auditory canal. Laryngoscope. 1999;109:488–491. doi: 10.1097/00005537-199903000-00027. [DOI] [PubMed] [Google Scholar]
- 14.Brea B., Roldan Fidalgo A. Imaging diagnosis of benign lesions of the external auditory canal. Acta Otorrinolaringol Esp. 2013;64:6–11. doi: 10.1016/j.otorri.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 15.Carbone P.N., Nelson B.L. External auditory osteoma. Head Neck Pathol. 2012;6:244–246. doi: 10.1007/s12105-011-0314-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen C.Y., Ying S.H., Yao M.S., Chiu W.T., Chan W.P. Sphenoid sinus osteoma at the sella turcica associated with empty sella: CT and MR imaging findings. Am J Neuroradiol. 2008;29:550–551. doi: 10.3174/ajnr.A0935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kozin E.D., Remenschneider A.K., Shah P.V., Reardon E., Lee D.J. Endoscopic transcanal removal of symptomatic external auditory canal exostoses. Am J Otolaryngol. 2015;36:283–286. doi: 10.1016/j.amjoto.2014.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khan M.M., Parab S.R. Endoscopic cartilage tympanoplasty: a two-handed technique using an endoscope holder. Laryngoscope. 2016;126:1893–1898. doi: 10.1002/lary.25760. [DOI] [PubMed] [Google Scholar]
- 19.Chen C.K., Hsieh L.C., Hsu T.H. Novel three-dimensional image system for endoscopic ear surgery. Eur Arch Otorhinolaryngol. 2018;275:2933–2939. doi: 10.1007/s00405-018-5153-7. [DOI] [PubMed] [Google Scholar]