Abstract
Rationale & Objective
There are many barriers to meeting the goal of increasing kidney transplants in the United States. It is important to understand dialysis and transplant center providers’ existing practices and identified barriers to increasing the number of dialysis patients who are evaluated for and get wait-listed for a transplant.
Study Design
Cross-sectional survey of dialysis unit and transplant center staff in End Stage Renal Disease Network 6 (Georgia, North Carolina, South Carolina).
Setting & Participants
Ninety-one transplant staff from all 9 transplant centers in the region and 421 dialysis staff from 421 facilities responded to the survey.
Predictors
N/A
Outcome
Provider perceptions of barriers faced by patients in the kidney transplant evaluation process and suggestions for improving care.
Analytical Approach
Mixed methods. Descriptive analyses of responses to multiple-choice questions and qualitative analysis of open-ended survey responses.
Results
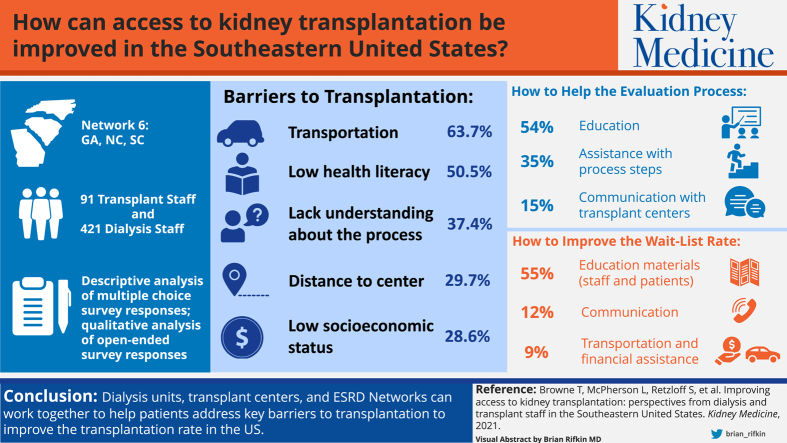
The top 5 barriers to kidney transplantation as reported by transplant staff were transportation (63.7%), low health literacy (50.5%), lack of understanding about the transplant process (37.4%), distance to transplant center (29.7%), and low socioeconomic status (28.6%). When asked how dialysis units can help patients complete the evaluation process, the most common responses from transplant center staff were educating patients about transplant (54%), helping patients through steps in the process (35%), and better communication with transplant centers (15%). When dialysis unit staff were asked what could be done to help the facility improve its transplant wait-list rate, the most common responses were educational materials for patients and staff (55%), better communication with transplant centers (12%), and transportation and financial assistance (9%).
Limitations
Survey responses are from 1 end stage renal disease network.
Conclusions
Dialysis units, transplant centers, and ESRD networks can work together to help patients address key barriers to transplantation to improve the country’s transplantation rate.
Index Words: Access, dialysis, interdisciplinary, transplant, wait-list
Graphical abstract
Plain-Language Summary.
Kidney transplantation is the recommended treatment for people with kidney failure, and there is national attention on improving patient access to transplant. There are many factors that affect a patient’s ability to pursue and receive a transplant, and it is important to understand what dialysis and transplant providers are doing and can do to help patients get a transplant. We surveyed transplant center and dialysis facility staff in the southeast to determine what difficulties patients experience in pursuit of a transplant. Transplant center staff reported that patients experience difficulties with transportation, low health literacy, lack of understanding about the transplant process, and low socioeconomic status. Dialysis facility staff reported needing more patient educational materials and improved communication with transplant centers.
Editorial, p. 696
Kidney transplantation is the recommended treatment for kidney failure due to the benefits of longer survival, better quality of life, and lower costs.1 Despite this, the majority of people with kidney failure remain on dialysis.1 Dialysis units play an important role in helping patients receive kidney transplants.2, 3, 4, 5 The Centers for Medicare & Medicaid Services (CMS) requires that dialysis units inform patients about transplantation and help patients pursue transplantation.6 Accordingly, CMS has mandated all end-stage renal disease (ESRD) networks increase transplant wait-listing among dialysis patients. The Advancing American Kidney Health initiative7 has also mandated an increase in the number of kidney transplants and in the percent of eligible patients on a transplant wait-list to 30% by 2023.8
To meet these federal goals and improve access to transplantation, it is important to understand dialysis and transplant providers’ existing practices and barriers to increasing the number of dialysis patients who are evaluated and get wait-listed for a transplant. Previous studies of dialysis unit staff highlighted opportunities for improved practices, such as using evidence-based patient education strategies.3,5,9, 10, 11 Our study builds on previous research with dialysis unit staff and, to our knowledge, is the first to also examine transplant center staff perspectives on patient-level barriers to transplantation in the United States.
We surveyed dialysis and kidney transplant center staff in 1 ESRD network (Georgia, North Carolina, and South Carolina)—a region with one of the lowest transplant rates in the nation12—about the current center practices that help patients receive transplants, the perceived barriers to transplantation, and suggestions for how to address these barriers.
Methods
We performed a cross-sectional analysis of survey data collected as part of the Reducing Disparities in Access to Kidney Transplantation (RaDIANT) Regional Study (clinicaltrials.gov NCT02389387).13 The data are derived from surveys administered to transplant and dialysis center staff. The Emory University (IRB00079596) and University of South Carolina (Pro00084060) institutional review boards approved this study, and informed consent was obtained for all participants. Members of the Southeastern Kidney Transplant Coalition (patients, providers, ESRD Network 6 staff, and researchers) created the surveys from January to September 2016. Notably, people with kidney disease were involved in this effort and provided feedback on the study design and survey items.
Study Design and Population
Transplant Center Staff Survey
From October 2016 to February 2017, research staff emailed a 56-item survey link (via compliant SurveyMonkey, which is compliant with the Health Insurance Portability and Accountability Act) to the medical directors of all 9 transplant centers in Network 6. Each medical director was instructed to forward the survey to staff members involved with transplant education. Responses were collected anonymously. A total of 106 staff from all 9 transplant centers completed the survey. Responses from 15 staff who were not involved with transplant education (as identified by a screening question) were excluded from the study population, leaving a final analytic cohort of N = 91. Responses to center-level survey questions were aggregated to the center level (n = 9).
Dialysis Unit Staff Survey
In January 2018, ESRD Network 6 staff emailed the link to a 36-item survey to the medical directors of the 440 dialysis units in the network participating in the RaDIANT Regional Study and Network 6’s Transplant Quality Improvement Project.14 Medical directors were instructed to have 1 staff person involved with transplant education complete the survey. Of the 440 dialysis facilities asked to complete the survey, 421 (95.7%) unique facilities had 1 staff member complete the survey and were included in the analytic cohort.
Primary Study Variables
Transplant Center Staff Survey
Transplant center staff roles were self-reported. The transplant center staff survey included questions on practices at the level of the transplant center and dialysis unit that may influence a patient’s success in being evaluated and listed for a transplant. The survey asked staff to identify the “top 5” barriers that prevent patients from completing the transplant evaluation process. The survey provided respondents 45 barriers to transplant evaluation identified by our coalition of experts, and the respondents could enter their answers for the top 5 barriers. Staff also responded to an open-ended question: “Briefly describe how dialysis facility staff can help your patients to start and complete the transplant evaluation process.”
Dialysis Staff Survey
The dialysis staff survey included questions about facility transplant education and referral practices, staff-perceived patient-level barriers to kidney transplant evaluation, and ways in which facility staff communicate with transplant center staff and assist patients with evaluation and wait-listing. Dialysis staff also answered an open-ended question: “What can the ESRD Network do to help your facility improve your transplant wait-listing rate?” Although this question asked about what the network could do, the answers provide insight into the general needs dialysis units have regarding kidney transplants.
Statistical Analyses
A mixed-methods approach was used to analyze survey responses. Descriptive analyses were conducted for all closed-ended survey questions using SAS version 9.4 (SAS Institute). Qualitative analyses were performed using MaxQDA software (VERBI GmbH). First-cycle coding of the qualitative data was performed by the first author, who individually examined the open-ended survey questions and initially coded the content for patterns. Major categories of responses were identified, and relevant themes in the responses were identified using a constant comparison method,15 reviewing all answers. After this initial analysis, the authors reviewed, discussed, and synthesized the findings and created a list of the final themes based on group consensus.
Results
Transplant Staff Survey
Among the 91 transplant center staff respondents, the majority were coordinators (49.5%), social workers (18.7%), or transplant nephrologists (12.1%). Respondents were 64.8% non-Hispanic white, 17.6% non-Hispanic black, and 4.4% Hispanic white; and 84.6% were female. Among the transplant centers, all 9 reported accepting patient referrals for transplant evaluation from nephrologists and from dialysis units, 4 transplant centers accepted self-referrals from patients, and 5 accepted referrals from social workers. All 9 transplant centers accepted responsibility for scheduling patients’ initial appointments for transplant evaluation. Five (55.6%) centers required that patients receive transplant education before scheduling a transplant evaluation appointment. Of these centers, the most common mechanism was via an in-person education session (4 of 5). Four centers indicated that only 1 visit was required to complete the transplant evaluation process; 5 centers reported that evaluation required more than 1 visit to be completed. All but 1 of the transplant centers did not require medical testing before being scheduled for transplant evaluation (Table 1).
Table 1.
Responses to Selected Questions From an Electronic Survey 91 Respondents From All 9 Transplant Centers in Georgia, North Carolina, and South Carolina Examining Perceived Barriers to Kidney Transplantation, 2017
| Question | No. of Transplant Centers (%) |
|---|---|
| From whom does your center accept referrals for transplant evaluation? (Choose all that apply.) | |
| Nephrologist | 9 (100) |
| Dialysis facility | 9 (100) |
| Patient (self-referral) | 4 (44.4) |
| Social worker | 5 (55.6) |
| Whose responsibility is it to initiate scheduling of the kidney transplant evaluation? | |
| Transplant center | 9 (100) |
| Does your center require patients to read/view education materials prior to being scheduled for a kidney transplant evaluation? | |
| Yes | 5 (55.6) |
| In-person education session | 4 (80.0) |
| Online education program | 1 (20.0) |
| No | 4 (44.4) |
| Number of visits to complete evaluation process: | |
| 1 visit | 4 (44.4) |
| 2 visits | 2 (22.2) |
| 3 or more visits | 3 (33.3) |
| How is medical testing scheduled at your transplant center? | |
| Patients are given option to have transplant center schedule | 4 (44.4) |
| Transplant center | 3 (33.3) |
| Split between patient and transplant center | 2 (22.2) |
| Methods center uses to remind patients of their upcoming medical testing appointments (choose all that apply): | |
| Telephone call | 9 (100) |
| Mailed letter | 8 (88.9) |
| Number of missed appointments before closing referral: | |
| Eventually, but not after a specific number of times | 4 (44.4) |
| 3 times | 4 (44.4) |
| 1 time | 1 (11.1) |
| Does your center offer any free transportation services? | |
| No | 9 (100) |
| Does your center offer any free park and ride shuttle services? | |
| No | 9 (100) |
| Does your center assist patients with parking costs? | |
| Yes | 4 (44.4) |
| No | 5 (55.6) |
| Does your center have a transplant telemedicine program? | |
| Yes | 2 (22.2) |
| No | 7 (77.8) |
| Does your center have satellite clinics? | |
| No | 5 (55.6) |
| Yes | 4 (44.4) |
| Number of satellite clinics | |
| 4 | 2 (50.0) |
| 5 | 1 (25.0) |
| 6 | 1 (25.0) |
| Required medical tests within 12 months prior to evaluation start: | |
| Mammogram for females > 40 years old | 1 (11.1) |
| Pap smear for females > 18 years old | 1 (11.1) |
| Colonoscopy for patients > 50 | 1 (11.1) |
| Echocardiogram | 1 (11.1) |
| Stress test | 1 (11.1) |
| Immunizations | 1 (11.1) |
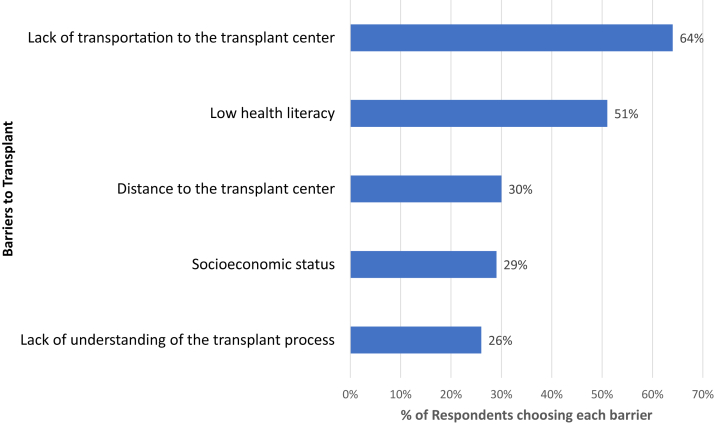
The most common methods of reminding patients of their transplant evaluation appointments were telephone calls (100%) and letters (88.9%). Four transplant centers closed out transplant referrals after a patient missed 3 scheduled transplant evaluation appointments. One transplant center closed a patient referral if the patient did not attend their first scheduled visit. None of the centers provided free patient transportation services. Two centers offered transplant telemedicine services for evaluations. Four centers assisted with parking costs, and 4 centers had satellite clinics where patients could be evaluated locally. When asked about the top 5 patient-level barriers to kidney transplantation, transplant center staff most often included transportation, low health literacy, lack of understanding about the transplant process, distance to the transplant center, and socioeconomic status (Fig 1).
Figure 1.
The top 5 transplant center-staff perceived patient-level barriers to evaluation for kidney transplantation (n = 91). Survey participants were asked to select common barriers to kidney transplantation from each of 6 categories (logistical barriers, emotional/motivation barriers, knowledge barriers, health condition barriers, financial barriers, and demographic barriers) and from among those selections, they were asked to choose the top 5 barriers to being evaluated for transplant at their center.
Eighty-six transplant staff provided answers to the open-ended question, “Please briefly describe how dialysis facility staff can help your patients to start and complete the transplant evaluation process.” The 3 main themes of these responses were educating patients about transplantation, helping patients with the steps to transplant, and better communication with transplant centers.
Educating Patients About Transplants
Just over half of transplant staff respondents (54%) suggested that dialysis staff could improve their kidney transplantation rates through effective patient education about transplants. One respondent’s answer to this question was “Education, education, education.” Another respondent replied, “Many patients are unaware that transplant is even a possibility.” Suggestions included having dialysis staff explain the transplant process, how to obtain a transplant, and the benefits of transplantation.
Helping Patients With Steps to Transplant
About one-third of staff (35%) thought that dialysis units should help patients navigate the steps to transplant. This included helping patients with referrals to a kidney transplant center, completing necessary paperwork, and reminding patients about appointments and tests. One respondent referred to this as helping patients “problem shoot” issues with attending appointments needed to be listed for a transplant. Many respondents used the term “follow up” or “monitor” to answer this question—that is, dialysis units needed to follow up with patients and actively inquire about how they could help patients.
Communication
Thirteen respondents (15%) suggested ways that dialysis units could communicate better with transplant centers to improve kidney transplant rates. Transplant staff wanted more frequent communication with dialysis units and wanted dialysis units to inform transplant centers of changes that could potentially impact a patient’s candidacy for transplantation.
Dialysis Staff Survey
Among the 421 dialysis staff survey respondents representing 421 facilities, most reported that their dialysis unit had a designated transplant coordinator (79.1%) (Table 2), and most indicated awareness of all of their patients’ status in the transplant process (82.2%). Social workers were the primary professionals in dialysis units helping patients move through the steps to transplantation (as reported by 56% of respondents), followed by nephrologists (12.6%) and nurses (11.9%). Almost all respondents reported that dialysis facility staff discussed kidney transplants with patients upon admission (92.6%), and a majority reported that these discussions were repeated whenever a patient asked (71.2%) or annually (66.2%). Most dialysis units (84.1%) used printed educational materials. Some had transplant coordinators visit their units (39.8%), some offered other transplant education sessions (25.5%), some hosted a transplant “education station” in their facility (20.5%), and a few presented transplant videos (16.2%).
Table 2.
Responses to Selected Questions From an Electronic Survey of 1 Respondent From 421 Selected Dialysis Facilities in Georgia, North Carolina, and South Carolina Examining Perceived Barriers to Kidney Transplantation, 2018
| Question | No. of Dialysis Facilities (%) |
|---|---|
| Does your facility have a designated transplant coordinator? | |
| Yes | 333 (79.1) |
| No | 74 (17.6) |
| Unknown | 14 (3.3) |
| Are staff aware of patients’ status in the transplant process (eg, date of medical evaluation at a transplant centers, wait-listing status, etc.)?a | |
| Yes | 346 (82.2) |
| No | 43 (10.2) |
| Unknown | 31 (7.4) |
| When does your facility discuss kidney transplant with your patients? (Please select all that apply.)a | |
| When a patient is new to our facility | 389 (92.6) |
| Whenever they ask | 299 (71.2) |
| Once a year | 278 (66.2) |
| Every 6 months | 84 (20.0) |
| Every 2 years | 4 (1.0) |
| Not discussed | 1 (0.2) |
| Other | 109 (26.0) |
| Unknown | 4 (1.0) |
| Who is the main person in your facility that helps patients get transplants?a | |
| Social worker | 235 (56.0) |
| Nephrologist | 53 (12.6) |
| Dialysis nurse | 50 (11.9) |
| Facility manager | 23 (5.5) |
| Patients do it themselves | 6 (1.4) |
| Patient care technician | 4 (1.0) |
| Other | 47 (11.2) |
| Unknown | 2 (0.5) |
| What transplant education methods are routinely administered to patients at your dialysis facility? (Please select all that apply.)a | |
| Printed transplant educational material | 353 (84.1) |
| Transplant coordinator lobby days | 167 (39.8) |
| Patient transplant education session at your facility | 107 (25.5) |
| Education station where general transplant information is available to patients | 86 (20.5) |
| Transplant educational video | 68 (16.2) |
| Transplant center open house at your facility | 24 (5.7) |
| Patient transplant navigator or peer mentor | 21 (5.0) |
| Unknown | 11 (2.6) |
| Other | 75 (17.9) |
| Do you feel confident that the transplant center received all the information they need to process the referral?a | |
| Very confident | 295 (70.1) |
| Moderately confident | 103 (24.5) |
| Slightly confident | 17 (4.0) |
| Not confident | 5 (1.2) |
| Primary way you communicate with transplant center staff about your patients?a | |
| Phone | 243 (57.7) |
| Fax | 108 (25.7) |
| 33 (7.8) | |
| We do not communicate | 1 (0.2) |
| Other | 31 (7.4) |
| Unknown | 4 (1.0) |
| If your patient misses an appointment with a kidney transplant center, what does your facility do? (Please select all that apply.)a | |
| We encourage the patient to reschedule the appointment. | 343 (81.7) |
| We help the patient reschedule the appointment. | 219 (52.1) |
| We help the patient remove barriers to making the appointment (eg, transportation, schedule, fear). | 136 (32.4) |
| We don’t know if a patient misses an appointment with transplant centers. | 46 (11.0) |
| We don’t help patients with their appointment at transplant centers. | 6 (1.4) |
| Other | 19 (4.5) |
One participant did not respond to this question.
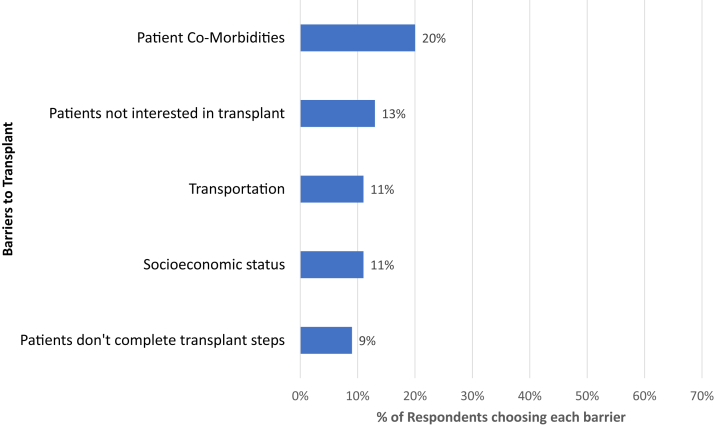
A majority of dialysis staff respondents reported that they felt confident that transplant centers received all the information they needed to process transplant referrals (70.1%). Just over half of dialysis staff respondents reported communicating with transplant center staff primarily by phone (57.7%), a quarter communicated by fax (25.7%), and 7.8% communicated by email. When asked to list their own responses for the top barriers in response to the question “Why do you think your facility has a low transplant wait-listing rate?” dialysis center staff most often included patient comorbidities, patients not interested in transplant, transportation, socioeconomic status, and patients not completing transplant steps (ie, patients do not follow up with transplant centers, or patients miss appointments for testing; Fig 2).
Figure 2.
The top 5 dialysis center-staff perceived barriers to kidney transplant wait-listing (n = 209). Survey participants were asked to list their own responses for the top barriers in response to the question “Why do you think your facility has a low transplant wait-listing rate?”
According to respondents, when dialysis units became aware of a patients’ missed transplant evaluation appointments, most (81.7%) encouraged patients to reschedule their appointments, over half helped the patients reschedule the appointment (52.1%), one-third (32.4%) helped patients with barriers to making the appointment (eg, transportation, schedule, fear), and six dialysis units (1.4%) did not help patients with these appointments. Eleven percent reported they “do not know if their patients miss appointments with transplant centers.”
Almost three-quarters of the dialysis staff respondents (n = 285, 70%) provided a qualitative response to the open-ended question, “What can the ESRD Network do to help your facility improve your transplant wait-listing rate?” The main themes from these qualitative responses were educational materials for patients and staff, help from transplant centers, transportation, and financial assistance.
Educational Materials for Patients and Staff
More than half (55%) of the respondents indicated they would like to receive educational materials about transplant that they could give to patients. No dialysis staff member asked for electronic versions of patient education materials; among all responses that mentioned a specific medium, only printed materials were mentioned.
Help From Transplant Centers
Thirty-four respondents requested better communication and follow-up from transplant centers to improve their patients’ success in being wait-listed for a kidney transplant. These professionals expressed concern that neither they nor their patients were aware of the patients’ status in the evaluation process, and they would like more frequent communication from the transplant centers about patient status. One of the respondents stated, “One of the ways in which they can improve the transplant waiting list is to be proactive and aggressive with information regarding the status of applicants. Referrals are made, but unsure of time frame of the evaluation process.” Another respondent suggested that ESRD Networks should “develop an easier way of communicating between dialysis facilities and transplant centers.” Some respondents (n = 13) also suggested that transplant center outreach staff or transplant recipients could visit dialysis units to talk with patients and inform patients about kidney transplantation.
Transportation and Financial Assistance
The third most-mentioned type of assistance that dialysis units needed to help patients obtain transplants was transportation (n = 25 respondents). Fifteen additional respondents suggested that their patients needed financial assistance to be wait-listed for a kidney transplant.
Discussion
Previous studies have discussed health care providers’ perceptions of patient barriers to transplantation, especially among members of racial and ethnic minority groups.10,11,16,17 However, barriers in the transplant evaluation process as perceived by transplant and dialysis staff are understudied, as are potential avenues of coordination between them to reduce these barriers. This study explored transplant and dialysis center practices that help patients obtain transplants, the perceived barriers to transplantation, and suggestions for how to address these barriers and improve access to transplantation.
Transplant staff respondents focused significantly on patient education deficits and geographic barriers (eg, lack of transportation) as key to improving transplant access. Dialysis staff respondents also identified patient comorbidities, patient interest in transplant, and patient ability to complete transplant steps as barriers to kidney transplantation. These findings provide insight into how dialysis units and transplant centers can work together to help patients obtain kidney transplants and address the barriers to this effort identified in our surveys. Dialysis units clearly play an important role in the transplant process, with all 9 transplant centers in 3 states accepting referrals from dialysis units (100%).
Patient education emerged as a focal strategy for increasing access to transplantation in both survey responses. The fact that 5 out of the 9 transplant centers required patients to have some sort of education before being scheduled for an evaluation suggests that dialysis unit staff can assist by asking patients if they have completed this requirement and keep track of this for patients. Transplant centers should be mindful that educational materials must accommodate patients with low health literacy; low health literacy was highlighted as a top barrier to transplantation by transplant staff and has been shown to be a critical barrier to kidney disease outcomes, including the pursuit of transplantation.18,19
CMS requires that patients on dialysis receive education on kidney transplantation; accordingly, nearly all dialysis unit survey respondents reported that transplantation was discussed with patients upon admission (92.6%). However, these discussions may not be sufficient, as a lack of education was reported as a top barrier to transplant by transplant staff. These initial conversations with dialysis patients could be augmented with increased and longitudinal patient education about transplant.
Although types of transplant education provided to patients varied among facilities, most surveyed units reportedly used printed education materials (84.1%), and over half of dialysis facility respondents requested assistance from the ESRD network in providing additional updated materials. Transplant centers, dialysis companies, and ESRD networks can create and provide such materials and distribute them to dialysis units, especially in the preferred paper format. Given the high need for patient transplant education identified by transplant center staff, printed education materials may not be sufficient to adequately inform patients about this treatment option, and dialysis centers may want to train all staff to discuss transplant with their patients.
This study reveals how transplant centers can better coordinate with dialysis units to improve patient completion of the steps to the transplant wait-list. According to respondents, none of the transplant centers in the Network 6 region communicated with dialysis units to notify them of upcoming patient appointments. Four of the 9 transplant centers reportedly closed patient transplant referrals after 3 evaluation appointments were missed. Dialysis units, which see most patients 3 times a week, could remind patients of their upcoming transplant clinic appointments and help them navigate any barriers to keeping them. Providing education to patients about transplantation is not enough: patients also need encouragement—with dialysis unit staff acting as a “cheerleader” 17—and assistance with completing steps to being wait-listed. Dialysis staff recognize this as a barrier to transplant, with 9 percent (n = 49) reporting “patients don’t complete transplant steps” as a top-5 barrier to transplant. This is consistent with previous evidence that patients recognize the value of dialysis unit staff being active in these roles.17
Improved communication between transplant centers and dialysis units can potentially help to enhance patient engagement and awareness. Almost 20% of responding dialysis staff said they did not know their patients’ status in the transplant process, and 28.5% were only moderately or slightly confident that transplant centers received all of the information they needed to process patient referrals for transplants. As dialysis patients may not be aware of their kidney transplant wait-listing status,20 many dialysis units must rely on transplant centers to provide this information.
Communication between dialysis and transplant centers could also be more effective and engaging, as a quarter of dialysis staff (25.7%) reported that fax was their primary way to communicate with transplant staff. Transplant centers may want to implement interactive methods for communicating with dialysis units, such as phone or email conversations to help improve collaboration. Many dialysis staff also requested that transplant center staff communicate with them more frequently about their patients’ status in the evaluation process. Transplant centers can explore ways to enhance this communication, and ESRD networks may consider exploring database systems that can help facilitate needed information exchange.
Encouragingly, almost all dialysis units in the 3-state region routinely had discussions with patients about kidney transplant. However, only about half of dialysis units (52%) reported helping patients with rescheduling missed appointments with transplant centers, and even fewer (32.4%) reported helping patients navigate the barriers to making these appointments. Respondents from 46 dialysis units (11%) reported not being informed if their patients missed appointments with transplant centers; improved communication between transplant centers and dialysis units can help address this disconnect. ESRD networks can also remind all dialysis units that they are mandated by CMS to help patients get transplants: respondents from 6 dialysis units in our survey reported that their units provided no assistance to patients with their transplant center appointments, and 81.7% of dialysis units reported relying on patients to reschedule missed appointments.
Some of our findings reflect those of other research highlighting the need for transportation to facilitate patients’ completion of the transplant evaluation process.21, 22, 23, 24 None of the 3-state region’s 9 transplant centers facilitated transportation to transplant evaluation appointments, although some assisted patients with parking costs. Dialysis and transplant centers might consider working with ride-share companies to provide these services for patients without access to transportation. In addition, providers, professionals, and kidney disease stakeholder organizations could advocate for policy changes that would require insurers to pay for transportation to transplant centers.
Our survey findings reflect the importance of an interdisciplinary team effort to help patients obtain kidney transplants, with physicians, social workers, and nurses playing large roles. Likewise, addressing the barriers to transplant should be a team effort involving both transplant and dialysis centers. A key member of this team should be a designated transplant coordinator, as almost one-fifth (17.6%) of the 421 dialysis units surveyed reportedly did not have such a person identified.
One limitation of this study is that the dialysis unit survey was created as part of a CMS quality improvement initiative,7 and the transplant center survey was created for the RaDIANT study. Although the survey questions were not identical, both surveys addressed barriers to the transplantation process that need resolution to improve patient access. The surveys used were not pretested, but the surveys were co-created with patients and patient stakeholder groups to enhance face validity. Our findings also may be affected by response bias, which was addressed by making the surveys anonymous.
Another limitation of this study is that these surveys were completed in 1 ESRD network’s coverage area. Future research is needed beyond this 3-state region. An additional limitation is that because facilities chose who to send the surveys to, the total possible number of respondents is not known. The dialysis center staff survey did not explore whether centers used an interdisciplinary approach to help patients get transplants; future research could examine this care model.
A final limitation is that these surveys were conducted before the COVID-19 pandemic and did not account for COVID-19 practice changes. The recent increase of telehealth may have helped address some of the barriers identified in this and other research, such as transportation. Future research on the impact of COVID-19 on transplant access is needed.
Our survey findings suggest recommendations for improving transplant and dialysis center coordination to increase kidney transplantation. With the Advancing American Kidney Health initiative and broad CMS-mandated quality improvement goals, there has been increased national attention on expanding access to kidney transplantation, and dialysis units are tasked with helping patients obtain transplants.8,9 Achieving these goals requires that we leverage both dialysis and transplant professionals’ expertise to improve patient outcomes. Further research, particularly patient-centered outcomes research, is needed on how dialysis and transplant staff can facilitate patients’ access to kidney transplants. Transplant and dialysis centers must coordinate efforts to collectively help patients get kidney transplants.
Article Information
Authors’ Full Names and Academic Degrees
Teri Browne, PhD, Laura McPherson, MPH, Samantha Retzloff, MPH, Amandha Darius, BS, Adam S. Wilk, PhD, Alexandra Cruz, Shannon Wright, Stephen O. Pastan, MD, Jennifer C. Gander, PhD, Alexander A. Berlin, and Rachel E. Patzer, PhD, on behalf of the Southeastern Kidney Transplant Coalition.
Authors’ Contributions
Research idea and study design: TB, LM, JCG, AAB, SOP, REP; data acquisition: LM, SR, SW AC; data analysis/interpretation: TB, AD, LM, SR, SW, AW, SOP, AC, REP; statistical analysis: LM, SR, REP. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Support
The Reducing Disparities in Access to Kidney Transplantation Regional Study was funded by the National Institute on Minority Health and Health Disparities (U01MD010611). The funder had no role in the study design, analysis, reporting, or decision to submit the manuscript for publication.
Financial Disclosure
The authors declare that they have no relevant financial interests.
Acknowledgements
The authors acknowledge the assistance of the Southeastern Kidney Transplant Coalition in participating with data collection and survey design. The authors would like to specifically acknowledge the Coalition members who heavily contributed to these tasks: Randy Detwiler (University of North Carolina Center for Transplant), Derek DuBay (Medical University of South Carolina), Matthew Ellis (Duke University Transplant Center), Chris Fotiadis (Carolinas Health), Erica Hartmann (Piedmont Transplant Institute), Heather Jones (Vidant Medical Center), Laura Mulloy (Augusta University Health Transplant Center), Amber Reeves-Daniel (Wake Forest Health), and Carlos Zayas (Augusta University Health Transplant Center). All authors have approved the final manuscript and certify that this manuscript represents valid work and has not been previously published.
Disclaimer
The analyses upon which this publication is based were performed under contract number HHSM-500-2016-00006C entitled End Stage Renal Disease Networks Organization for the State (Commonwealth) of Georgia, North Carolina, and South Carolina, sponsored by the Centers for Medicare & Medicaid Services, Department of Health and Human Services. The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the US government. The author assumes full responsibility for the accuracy and completeness of the ideas presented.
Peer Review
Received December 3, 2020. Evaluated by 2 external peer reviewers, with direct editorial input by an Associate Editor and the Editor-in-Chief. Accepted in revised form April 14, 2021.
Footnotes
Complete author and article information provided before references.
References
- 1.U.S. Renal Data System . National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2018. 2018 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. [Google Scholar]
- 2.Plantinga L.C., Pastan S.O., Wilk A.S. Referral for kidney transplantation and indicators of quality of dialysis care: a cross-sectional study. Am J Kidney Dis. 2017;69(2):257–265. doi: 10.1053/j.ajkd.2016.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Browne T., Patzer R.E., Gander J. Kidney transplant referral practices in southeastern dialysis units. Clin Transplant. 2016;30(4):365–371. doi: 10.1111/ctr.12693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gander J., Browne T., Plantinga L. Dialysis facility transplant philosophy and access to kidney transplantation in the southeast. Am J Nephrol. 2015;41(6):504–511. doi: 10.1159/000438463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Waterman A.D., Peipert J.D., Xiao H. Education strategies in dialysis centers associated with increased transplant wait-listing rates. Transplantation. 2020;104(2):335–342. doi: 10.1097/TP.0000000000002781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Conditions for coverage for end-stage renal disease facilities; final rule. Fed Regist. 2008;73:20369–20484. [PubMed] [Google Scholar]
- 7.US Department of Health and Human Services Advancing American Kidney Health. 2019, July 10. https://aspe.hhs.gov/sites/default/files/private/aspe-files/262056/advancingamericankidneyhealth.pdf
- 8.ESRD National Coordinating Center Welcome to the Quality Improvement Learning and Action Networks (LANs) https://esrdncc.org/en/qia/
- 9.Patzer R.E., Basu M., Smith K.D. Awareness of the new kidney allocation system among United States dialysis providers with low waitlisting. Am J Nephrol. 2018;47(2):115–119. doi: 10.1159/000486648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim J.J., Basu M., Plantinga L. Awareness of racial disparities in kidney transplantation among health care providers in dialysis facilities. Clin J Am Soc Nephrol. 2018;13(5):772–781. doi: 10.2215/CJN.09920917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lipford K.J., McPherson L., Hamoda R. Dialysis facility staff perceptions of racial, gender, and age disparities in access to renal transplantation. BMC Nephrol. 2018;19(1) doi: 10.1186/s12882-017-0800-6. 5-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patzer R.E., Plantinga L., Krisher J., Pastan S.O. Dialysis facility and network factors associated with low kidney transplantation rates among United States dialysis facilities. Am J Transplant. 2014;14(7):1562–1572. doi: 10.1111/ajt.12749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Patzer R.E., Gander J., Sauls L. The RaDIANT community study protocol: community-based participatory research for reducing disparities in access to kidney transplantation. BMC Nephrol. 2014;15:171. doi: 10.1186/1471-2369-15-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Medicare and Medicaid Services ESRD Network Organizations, 2017. https://www.cms.gov/Medicare/End-Stage-Renal-Disease/ESRDNetworkOrganizations/index.html
- 15.Saldana J. 3rd ed. SAGE; 2015. The Coding Manual for Qualitative Researchers. [Google Scholar]
- 16.Alexander G.C., Sehgal A.R. Barriers to cadaveric renal transplantation among blacks, women, and the poor. JAMA. 1998;280(13):1148–1152. doi: 10.1001/jama.280.13.1148. [DOI] [PubMed] [Google Scholar]
- 17.Browne T., Amamoo A., Patzer R.E. Everybody needs a cheerleader to get a kidney transplant: a qualitative study of the patient barriers and facilitators to kidney transplantation in the Southeastern United States. BMC Nephrol. 2016;17(1):108. doi: 10.1186/s12882-016-0326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dageforde L.A., Cavanaugh K.L. Health literacy: emerging evidence and applications in kidney disease care. Adv Chronic Kidney Dis. 2013;20(4):311–319. doi: 10.1053/j.ackd.2013.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grubbs V., Gregorich S.E., Perez-Stable E.J., Hsu C.Y. Health literacy and access to kidney transplantation. Clin J Am Soc Nephrol. 2009;4(1):195–200. doi: 10.2215/CJN.03290708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gillespie A., Hammer H., Lee J., Nnewihe C., Gordon J., Silva P. Lack of listing status awareness: results of a single-center survey of hemodialysis patients. Am J Transplant. 2011;11(7):1522–1526. doi: 10.1111/j.1600-6143.2011.03524.x. [DOI] [PubMed] [Google Scholar]
- 21.Dageforde L.A., Box A., Feurer I.D., Cavanaugh K.L. Understanding patient barriers to kidney transplant evaluation. Transplantation. 2015;99(7):1463–1469. doi: 10.1097/TP.0000000000000543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kazley A.S., Simpson K.N., Chavin K.D., Baliga P. Barriers facing patients referred for kidney transplant cause loss to follow-up. Kidney Int. 2012;82(9):1018–1023. doi: 10.1038/ki.2012.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lockwood M.B., Saunders M.R., Nass R. Patient-reported barriers to the prekidney transplant evaluation in an at-risk population in the United States. Prog Transpl. 2017;27(2):131–138. doi: 10.1177/1526924817699957. [DOI] [PubMed] [Google Scholar]
- 24.Hamoda R.E., McPherson L.J., Lipford K. Association of sociocultural factors with initiation of the kidney transplant evaluation process. Am J Transplant. 2020;20(1):190–203. doi: 10.1111/ajt.15526. [DOI] [PMC free article] [PubMed] [Google Scholar]