Key Points
Question
What are the patient perceptions and knowledge about ionizing radiation used for medical imaging?
Findings
In this survey study among 2866 patients undergoing radiological examinations in Italian hospitals, a substantial proportion of respondents perceived their medical radiation knowledge as inadequate and had misconceptions about basic aspects of radiation protection. Better knowledge was associated with receiving such information from medical staff and having a higher educational level.
Meaning
These findings suggest that interventions to improve patients’ knowledge about radiation protection risks would be beneficial, with communication from medical staff potentially playing a determinant role.
Abstract
Importance
Although imaging has become a standard tool of modern medicine, its widespread use has been paralleled by an increasing cumulative radiation dose to patients despite technological advancements and campaigns calling for better awareness and minimization of unnecessary exposures.
Objective
To assess patients’ knowledge about medical radiation and related risks.
Design, Setting, and Participants
A survey study of hospitals in Italy was conducted; all patients in waiting rooms for medical imaging procedures before undergoing imaging examinations at 16 teaching and nonteaching hospitals were approached to take the survey. The survey was performed from June 1, 2019, to May 31, 2020.
Main Outcomes and Measures
Survey respondents’ basic knowledge of ionizing radiation levels and health risks, earlier imaging tests performed, and information and communication about radiation protection issues.
Results
Among 3039 patients invited to participate, the response rate was 94.3% (n = 2866). Participants included 1531 women (53.4%); mean (SD) age was 44.9 (17.3) years. Of the 2866 participants, 1529 (53.3%) were aware of the existence of natural sources of ionizing radiation. Mammography (1101 [38.4%]) and magnetic resonance imaging (1231 [43.0%]) were categorized as radiation-based imaging modalities. More than half of the 2866 patients (1579 [55.1%]; P = .03) did not know that chest computed tomography delivers a larger dose of radiation than chest radiography, and only 1499 (52.3%) knew that radiation can be emitted after nuclear medicine examinations (P = .004). A total of 667 patients (23.3%) believed that radiation risks were unrelated to age, 1273 (44.4%) deemed their knowledge about radiation risks inadequate, and 2305 (80.4%) preferred to be informed about radiation risks by medical staff. A better knowledge of radiation issues was associated with receiving information from health care professionals (odds ratio [OR], 1.71; 95% CI, 1.43-2.03; P < .001) and having a higher educational level (intermediate vs low: OR, 1.48; 95% CI, 1.17-1.88; P < .001; high vs low: OR, 2.68; 95% CI, 2.09-3.43; P < .001).
Conclusions and Relevance
The results of this survey suggest that patients undergoing medical imaging procedures have overall limited knowledge about medical radiation. Intervention to achieve better patient awareness of radiation risks related to medical exposures may be beneficial.
This survey study examines patients’ knowledge of radiation used in imaging procedures.
Introduction
Owing to the development and widespread availability of cross-sectional imaging, in the last several decades, radiology has become pivotal in the diagnosis and management of many diseases. The use of medical imaging, including ionizing radiation-based modalities, continues to increase, raising concerns about patients’ radiation exposure,1,2,3,4 with reported cumulative effective doses exceeding 100 mSv for single procedures.5,6,7,8 Although accounting for only 17% of all medical examinations, multidetector computed tomography (CT) alone makes up approximately 50% of the total radiation burden for medical purposes, and a large multicenter trial by Rehani et al9 revealed that more than 1% of patients undergoing multiple CT examinations over 1 to 5 years received a cumulative effective dose above 100 mSv.
The European Council Directive 2013/59/Euratom has emphasized the need for “safety standards for protection against the dangers arising from exposure to ionizing radiation.”10 Technical advances aimed to optimize radiation dose use, and awareness campaigns for health care professionals (including general practitioners, clinicians, radiologists, nuclear medicine physicians, and radiographers) and patients are the main ways to minimize unnecessary radiation exposure. Several studies have reported a lack of knowledge about medical radiation and related risks among both health care professionals and patients.11,12,13,14,15,16 In particular, patients’ knowledge about medical radiation is limited, and the perception of radiation risks is variable depending on age and educational level.17,18,19
In Italy, this issue is of special interest owing to the European Council Directive 2013/59/Euratom having become effective starting on August 27, 2020.11,20 In this context, a nationwide survey might help to more thoroughly assess patients’ knowledge about medical radiation and its potential risks. Our purpose was to develop and validate a questionnaire aimed to assess such knowledge among Italian patients and identify any differences related to patient sex, age, educational level, information received, and radiological procedures performed.
Methods
Population and Data Collection
A multicenter, nationwide survey study with prospective data collection was performed between June 1, 2019, and May 31, 2020, with patients in waiting rooms for medical imaging examinations in 16 Italian academic and nonacademic hospitals. Radiography students were trained as interviewers to achieve more generalized respondent comprehension and avoid misunderstanding. A web platform containing an informative brochure, a user’s guide, and the online questionnaire was implemented for easier collection of the survey results. Inclusion criteria were provision of written and individually signed patient informed consent, patient ability and willingness to adhere to all study requirements, and age 18 years or older. Exclusion criteria were mental illness, physical inability to respond and/or no or limited legal capacity, and age younger than 18 years.
Our study was approved by the regional ethical committee for clinical trials (Comitato Etico di Area Vasta Nord Ovest), and all of the involved radiology departments agreed to participate in the study. All patients gave their written informed consent to take the survey and were assured about the anonymity of responses; participants did not receive compensation. The survey was anonymously completed only once by each volunteer.
Questionnaire Development
This study followed the American Association for Public Opinion Research (AAPOR) reporting guideline for survey studies. The survey consisted of 23 items grouped into 3 sections (eAppendix in the Supplement). The first section of the survey contained questions on factors such as sex, age, marital status, and educational level. The second section contained questions aimed to explore the patient’s knowledge about ionizing radiation risks (Knowledge About Ionizing Radiation Questionnaire [KIRQ]) and was divided into 3 steps. The first step identified survey questions (items generation) based on a review of current biomedical and life sciences literature (eTable 1 in the Supplement), which resulted in creation of the first KIRQ version. In the second step, semantic structure and content of each item in terms of statement relevance, clarity, and appropriateness were assessed by 5 radiologists with more than 10 years of experience in radiation protection policies (first questionnaire version). After modification and optimization of the selected items, 10 questions were included in the second version and validated by an independent panel of radiology educators. The third step involved pretesting the questionnaire on 20 nonmedical volunteers to assess its comprehensibility (pilot test). A reliability test-retest was performed on 50 volunteers and reapplied 2 weeks later to ensure the stability of questionnaire scores over time.21 The third section of the survey contained questions aimed to explore expectations and communication gaps between health care professionals and survey respondents The full survey questions are reported in the eAppendix in the Supplement.
Statistical Analysis
Sample characteristics from the 3 questionnaire sections are assessed using descriptive statistics, whereas categorical variables are expressed as percentages and continuous variables are reported as mean (SD). The Italian regions were grouped into 3 territorial subareas: north, center, and south/islands.22 The educational level of the survey respondents was classified as low (ie, unschooled, primary school, or middle school), intermediate (ie, technical college [3 years] or high school/diploma), or high (ie, bachelor [3 years], master, or PhD degree).
We performed exploratory factor analysis and confirmatory factor analysis via structural equation modeling to identify latent factors underlying the psychometric properties of the 10-item KIRQ.23 To quantify the reliability of the questionnaire, we calculated the Cronbach index (α) as a measure of internal consistency. Several goodness-of-fit criteria were used, including the standardized root mean square residual, root mean square error of approximation (cutoff ≤0.10), comparative fit index, and Tucker-Lewis index (cutoff >0.90).24,25
Respondents’ scores were recorded using a binary classification of the KIRQ score with a 75th-percentile threshold separating high knowledge (≥75th percentile, binary value 1) from low to moderate knowledge (<75th percentile, binary value 0). Binary logistic models were applied to evaluate the association between personal data, communication, and information aspects and respondents’ knowledge. Setting the binary KIRQ score as the dependent variable and personal data, communication, and information items as independent variables, we performed univariable logistic regression as a first step to identify predictive variables and subsequently performed a multivariable logistic regression to simultaneously test the combinations of variables selected by univariable multinomial logistic regression (adjusted for sex and age). Results are reported as odds ratios (ORs) and their 95% CIs.
Statistical analysis was performed using Stata/SE, version 15 (StataCorp LLC) and SPSS, version 24 (IBM Corp). All P values were 2-sided, and P < .05 was set as the threshold for statistical significance.
Results
Our survey was conducted among 3039 individuals, with a response rate of 94.3% (n = 2866). The sample population included 1531 women (53.4%) and 1335 men (46.6%); mean (SD) age was 44.9 (17.3) years. The survey had a homogeneous geographic distribution (north, 1139 [39.7%], center, 889 [31.0%], and south/islands, 838 [29.2%]; P = .06).
The educational level of survey respondents was low in 661 respondents (23.1%), intermediate in 1367 (47.7%), and high in 838 (29.2%). Most respondents were married (1404 [49.0%]). Surveyed women had a higher level of education (491 [32.1%]) than men (347 [26.0%]) (Table 1).
Table 1. Personal Data of Survey Respondents.
| Variable | No. (%) | P value | ||
|---|---|---|---|---|
| Men (n = 1335) | Women (n = 1531) | Total (n = 2866) | ||
| Age, mean (SD), y | 45.44 (17.4) | 44.35 (17.2) | 44.90 (17.3) | .10 |
| Geographic area | ||||
| North | 520 (29.7) | 619 (32.2) | 1139 (39.7) | .06 |
| Center | 396 (39.0) | 493 (40.4) | 889 (31.0) | |
| South/islands | 419 (31.4) | 419 (27.4) | 838 (29.2) | |
| Nationality | ||||
| Italian | 1283 (96.1) | 1466 (95.8) | 2749 (95.9) | .71 |
| Other | 52 (3.9) | 65 (4.2) | 117 (4.1) | |
| Educational level | ||||
| Low | 330 (24.7) | 331 (21.6) | 661 (23.1) | <.001 |
| Intermediate | 658 (49.3) | 709 (46.3) | 1367 (47.7) | |
| High | 347 (26.0) | 491 (32.1) | 838 (29.2) | |
| Marital status | ||||
| Unmarried/civil partnership | 506 (37.9) | 580 (37.9) | 1086 (37.9) | .46 |
| Married | 665 (49.8) | 739 (48.3) | 1404 (49.0) | |
| Separated/divorced | 116 (8.7) | 117 (7.6) | 233 (8.1) | |
| Widowed | 48 (3.6) | 95 (6.2) | 143 (5.0) | |
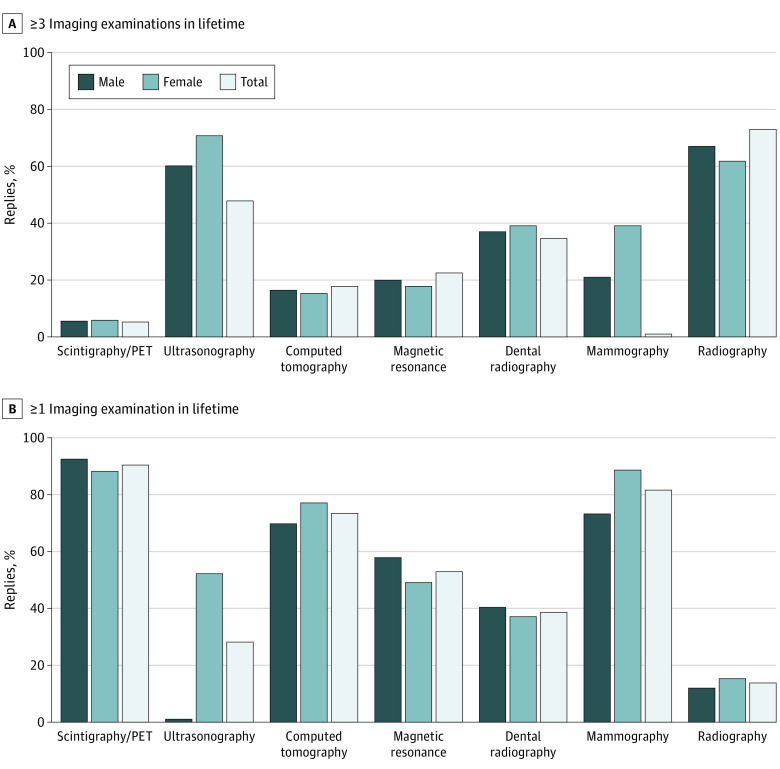
Almost all 2866 survey respondents (2823 [98.5%]) reported having undergone at least 1 radiological test in their lifetime. Of the 42 respondents (1.5%) undergoing an imaging examination for the first time, 1.3% were women (20/1531) and 1.6% were men (22/1335) (mean [SD] age, 32.1 [14.5 years]). Most of them had undergone examinations involving ionizing radiation at least once (Figure 1), including radiography (1244 men [93.2%], 1358 women [88.7%], 2602 combined [90.8%]), dental radiography (936 men [70.1%], 1185 women [77.4%], 2021 combined [74%]), CT (545 men [40.8%], 574 women [37.5%], 1119 combined [39%]), mammography (17 men [1.3%], 804 women [52.5%], 821 combined [28.6%]), and nuclear medicine imaging (164 men [12.3%], 237 women [15.5%], 401 combined [14%]). At least 3 exposures to radiography examinations had been performed in 1916 (66.8%) respondents (973 men [72.9%], 943 women [61.6%]); dental radiography, 1058 respondents (36.9%) (462 men [34.6%], 596 women [38.9%]); CT, 468 respondents (16.3%) (235 men [17.6%], 233 women [15.2%]); mammography, 601 respondents (21%) (11 men [0.8%], 594 women [38.8%]); and nuclear medicine, 158 respondents (5.5%) (69 men [5.2%], 89 women [5.8%]). Among radiation-free imaging tests, ultrasonography had been performed at least once in 2345 respondents (81.9%) (984 men [73.7%], 1361 women [88.9%]), whereas magnetic resonance imaging (MRI) had been performed at least once in 1532 respondents (53.4%) (776 men [58.1%]; 756 women [49.4%]). The mean (SD) overall number of lifetime imaging tests was slightly higher in women (4.31 [1.8]; median, 4; IQR, 3-6) than men (3.8 [1.7]; median, 4; IQR, 3-5) (P<.001).
Figure 1. Lifetime Imaging Tests of Survey Respondents.
Responses of individuals who had received 3 or more imaging examinations (A) and 1 or more imaging examinations (B). PET indicates positron emission tomography.
In the KIRQ survey section, 1529 of the 2866 respondents (53.3%) were aware of the existence of natural sources of ionizing radiation, with no statistically significant difference between men and women (Table 2). Computed tomography was correctly categorized as radiation-based imaging by 2035 respondents (71.0%), and mammography was correctly categorized by 1101 respondents (38.4%). Although no statistically significant difference was found in the rate of correct answers about CT between men and women, correct answers regarding mammography were provided by women (711 of 1531 [46.4%]) more frequently than men (390 of 1335 [29.2%]) (P < .001).
Table 2. Respondents’ Replies to the Second and Third Survey Sectionsa.
| Survey question | No. (%) | P value | ||
|---|---|---|---|---|
| Men (n = 1335) | Women (n = 1531) | Total (N = 2866) | ||
| Category B: Knowledge | ||||
| B4. Is there a natural source of ionizing radiation to which we are all exposed? | ||||
| Yes/no | 721 (54.0) | 808 (52.8) | 1529 (53.3) | .51 |
| B5. Which of these radiological examinations involve exposure to ionizing radiation? (multiple choices allowed) | ||||
| Ultrasonography | 1096 (82.1) | 1340 (87.5) | 2436 (85.0) | <.001 |
| CTb | 964 (72.2) | 1071 (70.0) | 2035 (71.0) | .18 |
| Magnetic resonanceb | 581 (43.5) | 650 (42.5) | 1231 (43.0) | .57 |
| Mammography | 390 (29.2) | 711 (46.4) | 1101 (38.4) | <.001 |
| B6. Which of the following imaging tests delivers a higher radiation dose? | ||||
| Chest CTb | 568 (42.5) | 719 (47.0) | 1287 (44.9) | <.05 |
| Chest radiograph | 395 (29.6) | 393 (25.7) | 788 (27.5) | |
| The amount of radiation is the same | 372 (27.9) | 419 (27.4) | 791 (27.6) | |
| B7. Following which radiological tests can one emit radiation (even some time after it)? | ||||
| Contrast-enhanced ultrasonography | 62 (4.6) | 63 (4.1) | 125 (4.4) | <.01 |
| Contrast-enhanced CT | 230 (17.2) | 243 (15.9) | 473 (16.5) | |
| Scintigraphyb | 648 (48.5) | 851 (55.6) | 1499 (52.3) | |
| All of the above | 226 (16.9) | 208 (13.6) | 434 (15.1) | |
| None of the above | 169 (12.7 | 166 (10.8) | 335 (11.7) | |
| B8. For an abdominal CT scan, how does the amount of radiation dose delivered to a thinner patient (60 kg) compare with that delivered to a heavier one (100 kg)? | ||||
| Higher in a thin patient | 186 (13.9) | 225 (14.7) | 411 (14.3) | .24 |
| Higher in a heavy patientb | 444 (33.3) | 464 (30.3) | 908 (31.7) | |
| It is comparable | 705 (52.8) | 842 (55.0) | 1547 (54.0) | |
| B9. How dangerous is it to undergo radiological tests using ionizing radiation? | ||||
| Not very dangerousb | 552 (41.3) | 471 (30.8) | 1023 (35.7) | <.001 |
| Quite dangerous | 639 (47.9) | 865 (56.5) | 1504 (52.5) | |
| Very dangerous | 144 (10.8) | 195 (12.7) | 339 (11.8) | |
| B10. For which of the following is it riskier to undergo a radiological test using ionizing radiation? | ||||
| A childb | 766 (57.4) | 913 (59.6) | 1679 (58.6) | <.01 |
| A 25-y-old man | 22 (1.6) | 23 (1.5) | 45 (1.6) | |
| A 25-y-old woman | 90 (6.7) | 97 (6.3) | 187 (6.5) | |
| A middle-aged adult | 38 (2.8) | 34 (2.2) | 72 (2.5) | |
| An older individual | 128 (9.6) | 88 (5.7) | 216 (7.5) | |
| No difference (the risk is comparable) | 291 (21.8) | 376 (24.6) | 667 (23.3) | |
| Category C: Communication | ||||
| C1. How do you evaluate your knowledge about the risks associated with the use of ionizing radiation for medical purposes? | ||||
| Fair/good/excellent | 338 (25.3) | 377 (24.6) | 715 (24.9) | .52 |
| Sufficient | 419 (31.4) | 459 (30.0) | 878 (30.6) | |
| Inadequate | 578 (43.3) | 695 (45.4) | 1273 (44.4) | |
| C2. From which communication channels have you usually received information about the risks associated with the use of ionizing radiation for medical purposes? | ||||
| Television/radio | 395 (29.6) | 395 (25.8) | 790 (27.6) | .02 |
| Magazines/newspapers | 201 (15.1) | 245 (16.0) | 446 (15.6) | .49 |
| Internet or social media (eg, Facebook) | 344 (25.8) | 382 (25.0) | 726 (25.3) | .62 |
| Booklets | 194 (14.5) | 283 (18.5) | 477 (16.6) | <.01 |
| School, university | 217 (16.3) | 319 (20.8) | 536 (18.7) | <.01 |
| I have never received any information about ionizing radiation | 488 (36.6) | 514 (33.6) | 1002 (35.0) | .10 |
| C3. If you underwent a diagnostic examination with ionizing radiation, did you receive information about the risks associated with the use of ionizing radiation for that examination? | ||||
| Yes | 551 (41.3) | 671 (43.8) | 1222 (42.6) | .21 |
| I have never received any information about ionizing radiation | 784 (58.7) | 860 (56.2) | 1644 (57.4) | |
| C4. From which of the following sources would you like to receive information regarding the risks associated with the use of ionizing radiation for medical purposes? | ||||
| Television/radio | 581 (43.5) | 597 (39.0) | 1178 (41.1) | .01 |
| Newspapers | 325 (24.3) | 346 (22.6) | 671 (23.4) | .27 |
| Internet or social media (eg, Facebook) | 386 (28.9) | 438 (28.6) | 824 (28.8) | .86 |
| Booklets | 351 (26.3) | 464 (30.3) | 815 (28.4) | .02 |
| School | 407 (30.5) | 513 (33.5) | 920 (32.1) | .08 |
| Health care staff | 1057 (79.2) | 1248 (81.5) | 2305 (80.4) | .12 |
| C5. In the health care environment, from which professional would you prefer to receive information about the risks associated with the use of ionizing radiation? | ||||
| Radiologist | 905 (67.8) | 1061 (69.3) | 1966 (68.6) | .39 |
| Medical physicist | 183 (13.7) | 177 (11.6) | 360 (12.6) | .08 |
| Radiographer | 675 (50.6) | 830 (54.2) | 1505 (52.5) | .06 |
| General practitioner | 759 (56.9) | 854 (55.8) | 1613 (56.3) | .56 |
| C6. At the end of a radiological examination, in which terms would you prefer to be informed about the amount of radiation received? | ||||
| The radiation value expressed in terms of radiation units | 513 (38.4) | 502 (32.7) | 1015 (35.4) | .002 |
| The equivalent risk to that of a No. of smoked cigarettes | 515 (38.6) | 448 (29.3) | 963 (33.6) | <.001 |
| The equivalent risk to that of a No. of days of background radiation exposure | 427 (32.0) | 555 (36.3) | 982 (34.3) | .02 |
| The equivalent risk to a No. of kilometers traveled by car | 193 (14.5) | 250 (16.3) | 443 (15.5) | .17 |
| I don’t want to be informed | 142 (10.6) | 199 (13.0) | 341 (11.9) | .05 |
Abbreviations: CT, computed tomography; KIRQ, Knowledge About Ionizing Radiation Questionnaire.
Second section, KIRQ; third section, communication and information.
Correct answer for the KIRQ questions.
Ultrasonography was correctly classified as a radiation-free examination by 2436 respondents (85.0%), and MRI was correctly classified by 1231 respondents (43.0%). Women (1340 of 1531 [87.5%]) replied correctly to questions about ultrasonography more frequently than men (1096 of 1335 [82.1%]) (P < .001), whereas no statistically significant difference between men and women was found related to questions about MRI.
More than half of the 2866 respondents (1579 [55.1%]; P = .03) did not know that chest CT delivers more radiation compared with chest radiography, and slightly more than half knew that patients can emit radiation after nuclear medicine examinations (1499 of 2866 [52.3%]; P = .004). The question about the association between CT dose and patient’s body weight was correctly answered by only 31.7% (908) of the respondents, whereas 58.6% (1679) of respondents correctly replied to the question about radiation risks and age. Few respondents (667 [23.3%]) believed that radiation exposure risks were not affected by age.
In the third survey section, 1273 of the 2866 respondents (44.4%) deemed their knowledge about radiation risks as inadequate. They had been informed about radiation risks by radio and television (790 [27.6%]) exposure and from the internet, including Facebook or other social media (726 [25.3%]).
Approximately one-third (1002 [35.0%]) of the respondents had never been informed about ionizing radiation from mass media. However, most respondents (2305 [80.4%]) expressed the preference to receive such information from health care professionals.
Only 1224 respondents (42.7%) had been informed about radiation risks during an imaging examination. Most patients would like to be informed by a radiologist (1966 [68.6%]), followed by their general practitioner (1613 [56.3%]), a radiographer (1505 [52.5%]), and a medical physicist (360 [12.6%]).
A total of 2525 of the 2866 respondents (88.1%) wanted to be informed about the amount of radiation received after the radiological examination was completed. The most appreciated methods of communication were via a quantitative dose measurement using a specific radiation unit (eg, millisieverts) (1015 [35.4%]) and by expressing the radiation hazard in terms of equivalent cancer risk from a given number of smoked cigarettes (963 [33.6%]) (Table 2).
Psychometric Properties of the 10-Item KIRQ
Exploratory factor analysis highlighted the presence of 1 latent factor underlying the 10-item questionnaire on ionizing radiation knowledge. The questionnaire showed acceptable internal consistency (Cronbach α, 0.742) (eTable 2 in the Supplement).
Confirmatory factor analysis revealed that the items related to ionizing radiation exposure from specific imaging modalities (question B5) were the most important variables, with a value equal to 0.478 for CT and 0.382 for MRI. Other variables with optimal specific validity index values were those related to the amount of radiation in association with specific imaging examinations (question B6; 0.374), natural sources of ionizing radiation (question B4; 0.342), and radiation emission after radiological tests (question B7; 0.313).
Factors Associated With Knowledge of Radiation Protection
The KIRQ score greater than or equal to the 75th percentile was equal or above 7 points and the median was 5 points. The KIRQ score was significantly lower in patients older than 65 years (median, 4; IQR, 3-6 years) than in those aged 18 to 64 years (median, 5; IQR, 4-7) (P < .001).
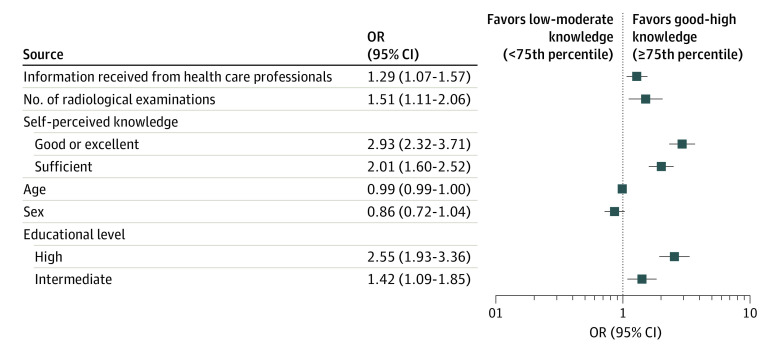
Univariable analysis (Table 3) showed a significant positive association between ionizing radiation knowledge (KIRQ score ≥75th percentile) and age (OR, 0.99; 95% CI, 0.989-0.998; P = .01). A higher level of knowledge was associated with higher levels of education (intermediate vs low: OR, 1.48; 95% CI, 1.168-1.881; P < .001; high vs low: OR, 2.68; 95% CI, 2.091-3.426; P < .001). Respondents with high levels of self-perceived knowledge had greater knowledge about ionizing radiation (good or excellent vs inadequate self-perception knowledge: OR, 3.46; 95% CI, 2.789-4.279; P < .001). Respondents who had received information from health care professionals (OR, 1.71; 95% CI, 1.431-2.034; P < .001) or those who had sought information from brochures, radio, internet, or other mass media (OR, 1.36; 95% CI, 1.212-1.518; P < .001) were more knowledgeable about ionizing radiation. No significant association was found between ionizing radiation knowledge and respondents’ sex (OR, 0.91; 95% CI, 0.771-1.079; P = .28), lifetime number of radiological examinations (OR, 1.72; 95% CI, 0.762-3.898; P = .19), and geographic location (center vs south/islands: OR, 1.14; 95% CI, 0.923-1.407; P = .22; north vs south/islands: OR, 0.77; 95% CI, 0.623-1.045; P = .06).
Table 3. Univariable and Multivariable Logistic Regression .
| Variable | Univariable | Multivariable | ||
|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | |
| Sex | 0.91 (0.771-1.079) | .28 | 0.86 (0.718-1.035) | .11 |
| Age | 0.99 (0.989-0.998) | <.01 | 0.99 (0.987-0.999) | .02 |
| Educational level | ||||
| Low | 1 [Reference] | 1 [Reference] | ||
| Intermediate | 1.48 (1.168-1.881) | <.001 | 1.42 (1.085-1.846) | .01 |
| High | 2.68 (2.091-3.426) | <.001 | 2.55 (1.933-3.359) | <.001 |
| Self-perceived knowledge | ||||
| Inadequate | 1 [Reference] | 1 [Reference] | ||
| Sufficient | 2.30 (1.863-2.837) | <.001 | 2.01 (1.602-2.516) | <.001 |
| Good or excellent | 3.46 (2.789-4.279) | <.001 | 2.93 (2.315-3.708) | <.001 |
| KIRQ informationa | ||||
| B1. No. of imaging examinations (at least 1 in lifetime) | 1.72 (0.762-3.898) | .19 | 1.51 (1.110-2.061) | .009 |
| C3. Information received from health care professionals | 1.71 (1.431-2.034) | <.001 | 1.30 (1.072-1.565) | .007 |
| B2. No. of imaging examinations (≥3 in lifetime) | 1.30 (1.002-1.691) | <.05 | NA | NA |
| C2. Information about ionizing radiation received | 1.36 (1.212-1.518) | <.001 | NA | NA |
| C4. Information about ionizing radiation desired | 1.07 (1.015-1.133) | .01 | NA | NA |
| Geographic area | NA | NA | ||
| South/islands | 1 [Reference] | NA | NA | |
| Center | 1.14 (0.923-1.407) | .22 | NA | NA |
| North | 0.77 (0.623-1.045) | .06 | NA | NA |
Abbreviations: KIRQ, Knowledge About Ionizing Radiation Questionnaire; NA, not applicable; OR, odds ratio.
The survey consisted of 23 items grouped into 3 sections. Items labeled as “B” indicate knowledge, and items labeled as “C” indicate communication.
Multivariable logistic regression (Figure 2) showed that higher educational level (intermediate vs low: OR, 1.42; 95% CI, 1.085-1.846; P < .01; high vs low: OR, 2.55; 95% CI, 1.933-3.359; P < .001) and sufficient or good self-perception of knowledge (sufficient vs inadequate: OR, 2.01; 95% CI, 1.602-2.516; P < .001; good or excellent vs inadequate: OR, 2.93; 95% CI, 2.315-3.708; P < .001) were associated with greater knowledge of ionizing radiation issues (KIRQ score ≥75th percentile). Statistically significant associations were also observed for lifetime number of radiological examinations (OR, 1.51; 95% CI, 1.110-2.061; P < .01) and information received from health care professionals (OR, 1.30; 95% CI, 1.072-1.565; P < .01). No statistically significant association was observed for sex, whereas younger age was associated with a greater knowledge level (OR, 0.99; 95% CI, 0.987-0.999; P = .02).
Figure 2. Multivariable Logistic Regression Analysis .
The reference category for educational level was low level, and the reference category for self-perceived knowledge was inadequate knowledge. OR indicates odds ratio.
Overall, multivariable analysis showed that the most relevant factors associated with ionizing radiation knowledge were a higher educational level, an adequate self-perception of radiation knowledge, a higher number of imaging examinations performed, and having received radiation information from a health care professional. Although exposure to radiation information from various news sources (eg, television, radio, and newspapers) was also associated with a higher radiation knowledge on univariate analysis, such association was not confirmed by multivariate analysis.
Discussion
Despite the fact that 98.5% of the respondents had undergone imaging, few had an understanding of radiation dose or risk and had gained their knowledge from outside the health care system, and most requested more information. These results suggest the need for new strategies even with the presence of many public radiation protection and awareness campaigns for more than a decade.
This study was designed to be a national-level survey of adults undergoing medical imaging procedures aimed to evaluate their knowledge and awareness about ionizing radiation, with the dual purpose of understanding their concerns and informing policy makers and radiation protection professionals about gaps in education and training of all stakeholders. To our knowledge, this is the first multicenter survey on this topic performed on a large population, as studies published so far have included a limited number of patients and/or single imaging centers.17,18,26
Our results revealed a lack of knowledge in the general population about radiation doses associated with common radiological examinations and basic radiation protection issues. In particular, the existence of natural background radiation and the dose burden of the most frequent imaging examinations were largely unknown by our surveyed patients. This lack of information was not due to having no experience with radiological procedures. In fact, nearly all of the respondents had previously received at least 1 imaging examination, including radiation-free imaging modalities, and about two-thirds of the patients had undergone at least 3 imaging tests; there was a prevalence of men in the number of total radiological examinations (72.9%), whereas women had undergone ultrasonographic examinations more frequently than other imaging tests, including mammography. Such a female prevalence of ultrasonographic examinations could be due to breast screening and follow-up testing for urogynecological concerns.
Although most patients had undergone an ultrasonographic or MRI examination at least once, most were unaware of the absence of ionizing radiation in MRI (57%), and to a lesser extent, this finding also applied to ultrasonography (15%). Moreover, 71.0% of surveyed patients knew that CT relies on ionizing radiation, whereas only 38.4% (men and women combined) knew that mammography uses ionizing radiation, with women knowing that mammography is radiation based more frequently than men (46.4% vs 29.2%; P < .001). To this latter point, a questionnaire-based study conducted by Hollada et al27 on 1725 patients presenting for a mammogram showed that, although 65% of the patients responded that they had been informed of the risks and benefits of the examination, 60% overestimated the amount of radiation in a mammogram, suggesting that targeted patient education for those undergoing any type of imaging procedure should be heightened. More generally, our findings are in line with those from previous studies, revealing an unmet need for awareness campaigns about medical radiation addressed to the general population.26,27,28,29,30 Efforts to improve patient awareness about CT and radiation protection have yielded some results,28 yet much remains to be done. In addition, our findings highlighted patients’ limited knowledge about the association between body mass index and delivered CT radiation dose, with more than half believing that radiation dose is unrelated to body size, and about the association between patient age and radiation risk.
Furthermore, most surveyed patients were unaware of the potential radiation risks to which they may have been exposed if their imaging had required ionizing radiation, with more than half of the respondents receiving no radiation information before, during, or after imaging examinations despite more stringent legal requirements about delivering patient information and recording and reporting of doses on medical procedures. Improved communication between medical staff and patients may be useful if it is the main and mandatory focus of further informative campaigns because more than 40% of the respondents had received information about ionizing radiation mainly from mass media and deemed the knowledge received from those sources to be inadequate. Approximately 80% of the respondents stated they would like to receive information from medical staff, attesting to their willingness to be properly informed about the potential risks of radiological procedures.
In particular, most patients (68.6%) would like to be given information on this topic by radiologists. This preference could be explained by assuming that patients prefer to be informed by physicians who, owing to the medical and technological skills that pertain to their professional specialty, will supervise their imaging procedures and interpret the findings in combination with their clinical history to reach a diagnosis, hence being directly involved in clinical management and communication with other medical specialists. Although to a lesser extent, patients would also like to be informed by their general practitioners, with whom they usually have a closer relationship than with other health care professionals, or by radiographers, probably owing to their specific technical expertise. Nonetheless, several factors may align to prevent satisfactory communication between health care professionals and patients in a busy radiology setting.26,31 It could be hypothesized that this communication gap may partly result from a heavy workload in radiological departments, often making it difficult for the radiological staff to provide patients with exhaustive information about radiation exposure. Several studies have highlighted patients’ preference to speak directly with imaging experts about their imaging findings,19,32,33,34,35 further emphasizing the need for improved direct communication between radiological staff and patients.
In line with Hartwig et al,31 who found an association between patients’ educational level and awareness of potential negative effects from medical imaging, our study found that educational level, self-perceived knowledge about ionizing radiation, and number of imaging examinations performed were associated with a higher degree of awareness and knowledge about the risks of radiation exposure. Moreover, the fact that these patients were more likely to seek radiation protection information through mass media might suggest that proper information given by the radiological staff at imaging appointments could trigger patients’ interest about radiation protection issues. This practice could possibly improve patient knowledge and awareness and, in the long run, ease the educational tasks of radiology personnel.
Limitations
The study has limitations. The first limitation of our survey is that it was administered in waiting rooms of different hospitals without any differentiation based on imaging modality, potentially introducing a selection bias in the recruitment of survey respondents. Second, the sample selection and total number of respondents were not representative of the general patient population. Third, although our survey included a question on whether respondents who had undergone prior imaging examinations had been informed about radiation risks, it lacked more specific questions to assess whether such information was adequate. Fourth, although the survey had been tested and validated before being distributed to our final patient population, it cannot be considered as a standardized tool. Further studies with larger samples are needed, possibly via a nationwide or, even better, international standardized questionnaire, to get a more accurate representation of the general population’s radiation knowledge and awareness.
Conclusions
The findings of our survey suggest a substantial lack of knowledge about medical radiation among Italian patients. This scenario calls for improved communication between medical staff and patients to provide them with adequate awareness about medical radiation and the risks related to cumulative radiation exposure.
eAppendix. Survey Questions
eTable 1. Literature References Used for Generation of the Survey Items
eTable 2. Psychometric Properties of the 10-Item KIRQ
References
- 1.Mettler FA Jr, Bhargavan M, Faulkner K, et al. Radiologic and nuclear medicine studies in the United States and worldwide: frequency, radiation dose, and comparison with other radiation sources—1950-2007. Radiology. 2009;253(2):520-531. doi: 10.1148/radiol.2532082010 [DOI] [PubMed] [Google Scholar]
- 2.Brenner DJ. Should we be concerned about the rapid increase in CT usage? Rev Environ Health. 2010;25(1):63-68. doi: 10.1515/REVEH.2010.25.1.63 [DOI] [PubMed] [Google Scholar]
- 3.Smith-Bindman R, Lipson J, Marcus R, et al. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med. 2009;169(22):2078-2086. doi: 10.1001/archinternmed.2009.427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miglioretti DL, Johnson E, Williams A, et al. The use of computed tomography in pediatrics and the associated radiation exposure and estimated cancer risk. JAMA Pediatr. 2013;167(8):700-707. doi: 10.1001/jamapediatrics.2013.311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li X, Hirsch JA, Rehani MM, Ganguli S, Yang K, Liu B. Radiation effective dose above 100 mSv from fluoroscopically guided intervention: frequency and patient medical condition. AJR Am J Roentgenol. 2020;215(2):433-440. doi: 10.2214/AJR.19.22227 [DOI] [PubMed] [Google Scholar]
- 6.Arellano RS, Yang K, Rehani MM. Analysis of patients receiving ≥100 mSv during a computed tomography intervention. Eur Radiol. 2021;31(5):3065-3070. doi: 10.1007/s00330-020-07458-5 [DOI] [PubMed] [Google Scholar]
- 7.Rehani MM, Nacouzi D. Higher patient doses through X-ray imaging procedures. Phys Med. 2020;79:80-86. doi: 10.1016/j.ejmp.2020.10.017 [DOI] [PubMed] [Google Scholar]
- 8.Rehani MM, Melick ER, Alvi RM, et al. Patients undergoing recurrent CT exams: assessment of patients with non-malignant diseases, reasons for imaging and imaging appropriateness. Eur Radiol. 2020;30(4):1839-1846. doi: 10.1007/s00330-019-06551-8 [DOI] [PubMed] [Google Scholar]
- 9.Rehani MM, Yang K, Melick ER, et al. Patients undergoing recurrent CT scans: assessing the magnitude. Eur Radiol. 2020;30(4):1828-1836. doi: 10.1007/s00330-019-06523-y [DOI] [PubMed] [Google Scholar]
- 10.European Agency for Health and Safety at Work. Directive 2013/59/Euratom—protection against ionising radiation. July 7, 2019. Accessed July 27, 2021. https://osha.europa.eu/en/legislation/directives/directive-2013-59-euratom-protection-against-ionising-radiation
- 11.Günalp M, Gülünay B, Polat O, et al. Ionising radiation awareness among resident doctors, interns, and radiographers in a university hospital emergency department. Radiol Med. 2014;119(6):440-447. doi: 10.1007/s11547-013-0374-8 [DOI] [PubMed] [Google Scholar]
- 12.Lee RKL, Chu WCW, Graham CA, Rainer TH, Ahuja AT. Knowledge of radiation exposure in common radiological investigations: a comparison between radiologists and non-radiologists. Emerg Med J. 2012;29(4):306-308. doi: 10.1136/emermed-2011-200481 [DOI] [PubMed] [Google Scholar]
- 13.Singh RK, McCoubrie P, Burney K, Miles JA. Teaching medical students about radiation protection—what do they need to know? Clin Radiol. 2008;63(12):1344-1349. doi: 10.1016/j.crad.2008.06.010 [DOI] [PubMed] [Google Scholar]
- 14.Paolicchi F, Miniati F, Bastiani L, et al. Assessment of radiation protection awareness and knowledge about radiological examination doses among Italian radiographers. Insights Imaging. 2016;7:233-242. doi: 10.1007/s13244-015-0445-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Faggioni L, Paolicchi F, Bastiani L, Guido D, Caramella D. Awareness of radiation protection and dose levels of imaging procedures among medical students, radiography students, and radiology residents at an academic hospital: results of a comprehensive survey. Eur J Radiol. 2017;86:135-142. doi: 10.1016/j.ejrad.2016.10.033 [DOI] [PubMed] [Google Scholar]
- 16.Hobbs JB, Goldstein N, Lind KE, Elder D, Dodd GD III, Borgstede JP. Physician knowledge of radiation exposure and risk in medical imaging. J Am Coll Radiol. 2018;15(1, pt A):34-43. doi: 10.1016/j.jacr.2017.08.034 [DOI] [PubMed] [Google Scholar]
- 17.Lambertova A, Harsa P, Lambert L, Kuchynka P, Briza J, Burgetova A. Patient awareness, perception and attitude to contrast-enhanced CT examination: implications for communication and compliance with patients’ preferences. Adv Clin Exp Med. 2019;28(7):923-929. doi: 10.17219/acem/94146 [DOI] [PubMed] [Google Scholar]
- 18.Ria F, Bergantin A, Vai A, et al. Awareness of medical radiation exposure among patients: a patient survey as a first step for effective communication of ionizing radiation risks. Phys Med. 2017;43:57-62. doi: 10.1016/j.ejmp.2017.10.014 [DOI] [PubMed] [Google Scholar]
- 19.Salerno S, Nardi C, Tudisca C, et al. Complete written/oral information about dose exposure in CT: is it really useful to guarantee the patients’ awareness about radiation risks? Radiol Med. 2018;123(10):788-798. doi: 10.1007/s11547-018-0909-0 [DOI] [PubMed] [Google Scholar]
- 20.Legislative decree: directive 2013/59/Euratom. 31 July 2020, n. 101, Law of the Italian Republic. Accessed July 27, 2021. https://www.gazzettaufficiale.it/eli/id/2020/08/12/20G00121/sg
- 21.Polit DF, Beck CT. Is there gender bias in nursing research? Res Nurs Health. 2008;31(5):417-427. doi: 10.1002/nur.20276 [DOI] [PubMed] [Google Scholar]
- 22.National Institute of Statistics . Istat. Accessed January 4, 2021. https://www.istat.it/en/archivio/regional+accounts
- 23.Bartholomew DJ, Knott M. Latent Variable Models and Factor Analysis. 2nd ed. Oxford University Press; 1999. [Google Scholar]
- 24.Kline RB. Methodology in the Social Sciences: Principles and Practice of Structural Equation Modeling. 2nd ed. Guilford Press; 2005. [Google Scholar]
- 25.Steiger JH. Understanding the limitations of global fit assessment in structural equation modeling. Pers Individ Dif. 2007;42(5):893-898. doi: 10.1016/j.paid.2006.09.017 [DOI] [Google Scholar]
- 26.Schuster AL, Forman HP, Strassle PD, Meyer LT, Connelly SV, Lee CI. Awareness of radiation risks from CT scans among patients and providers and obstacles for informed decision-making. Emerg Radiol. 2018;25(1):41-49. doi: 10.1007/s10140-017-1557-8 [DOI] [PubMed] [Google Scholar]
- 27.Hollada J, Speier W, Oshiro T, et al. Patients’ perceptions of radiation exposure associated with mammography. AJR Am J Roentgenol. 2015;205(1):215-221. doi: 10.2214/AJR.14.13650 [DOI] [PubMed] [Google Scholar]
- 28.Zwank MD, Leow M, Anderson CP. Emergency department patient knowledge and physician communication regarding CT scans. Emerg Med J. 2014;31(10):824-826. doi: 10.1136/emermed-2012-202294 [DOI] [PubMed] [Google Scholar]
- 29.Sin HK, Wong CS, Huang B, Yiu KL, Wong WL, Chu YCT. Assessing local patients’ knowledge and awareness of radiation dose and risks associated with medical imaging: a questionnaire study. J Med Imaging Radiat Oncol. 2013;57(1):38-44. doi: 10.1111/j.1754-9485.2012.02471.x [DOI] [PubMed] [Google Scholar]
- 30.Singh N, Mohacsy A, Connell DA, Schneider ME. A snapshot of patients’ awareness of radiation dose and risks associated with medical imaging examinations at an Australian radiology clinic. Radiography (Lond). 2017;23(2):94-102. doi: 10.1016/j.radi.2016.10.011 [DOI] [PubMed] [Google Scholar]
- 31.Hartwig HDR, Clingenpeel J, Perkins AM, Rose W, Abdullah-Anyiwo J. Parental knowledge of radiation exposure in medical imaging used in the pediatric emergency department. Pediatr Emerg Care. 2013;29(6):705-709. doi: 10.1097/PEC.0b013e3182949066 [DOI] [PubMed] [Google Scholar]
- 32.Shyu JY, Sodickson AD. Communicating radiation risk to patients and referring physicians in the emergency department setting. Br J Radiol. 2016;89(1061):20150868. doi: 10.1259/bjr.20150868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mangano MD, Rahman A, Choy G, Sahani DV, Boland GW, Gunn AJ. Radiologists’ role in the communication of imaging examination results to patients: perceptions and preferences of patients. AJR Am J Roentgenol. 2014;203(5):1034-1039. doi: 10.2214/AJR.14.12470 [DOI] [PubMed] [Google Scholar]
- 34.Basu PA, Ruiz-Wibbelsmann JA, Spielman SB, Van Dalsem VF III, Rosenberg JK, Glazer GM. Creating a patient-centered imaging service: determining what patients want. AJR Am J Roentgenol. 2011;196(3):605-610. doi: 10.2214/AJR.10.5333 [DOI] [PubMed] [Google Scholar]
- 35.Koney N, Roudenko A, Ro M, Bahl S, Kagen A. Patients want to meet with imaging experts. J Am Coll Radiol. 2016;13(4):465-470. doi: 10.1016/j.jacr.2015.11.011 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Survey Questions
eTable 1. Literature References Used for Generation of the Survey Items
eTable 2. Psychometric Properties of the 10-Item KIRQ