Abstract
Background
The COVID-19 pandemic has resulted in the diversion of health resources away from routine primary care delivery. This disruption of health services has necessitated new approaches to providing care to ensure continuity.
Objectives
To summarize changes to the provision of routine primary care services during the pandemic.
Methods
Rapid literature review using PubMed/MEDLINE, SCOPUS, and Cochrane. Eligible studies were based in primary care and described practice-level changes in the provision of routine care in response to COVID-19. Relevant data addressing changes to routine primary care delivery, impact on primary care functions and challenges experienced in adjusting to new approaches to providing care, were obtained from included studies. A narrative summary was guided by Burns et al.’s framework for primary care provision in disasters.
Results
Seventeen of 1,699 identified papers were included. Studies reported on telehealth use and public health measures to maintain safe access to routine primary care, including providing COVID-19 screening, and establishing dedicated care pathways for non-COVID and COVID-related issues. Acute and urgent care were prioritized, causing disruptions to chronic disease management and preventive care. Challenges included telehealth use including disparities in access and practical difficulties in assessing patients, personal protective equipment shortages, and financial solvency of medical practices.
Conclusions
Substantial disruptions to routine primary care occurred due to the COVID-19 pandemic. Primary care practices’ rapid adaptation, often with limited resources and support, demonstrates agility and innovative capacity. Findings underscore the need for timely guidance and support from authorities to optimize the provision of comprehensive routine care during pandemics.
Keywords: COVID-19, general practice, models of care, pandemic, primary care, routine
Key Messages.
COVID-19 pandemic has necessitated new models of care.
Primary care providers adopted innovative, flexible, and integrated models of care.
Challenges included telehealth use and diversion of primary care resources to other settings.
Acute and urgent care were prioritized disrupting chronic disease management.
Greater efforts are needed to optimize comprehensive routine primary care.
Introduction
The COVID-19 pandemic has placed significant demands on health systems globally, resulting in the diversion of health resources away from routine primary care delivery to address the pandemic.1–5 This disruption of health services has necessitated new models of care to ensure continuity of regular care provision.6–8 Although several studies have examined primary care responses to COVID-19,9–11 there is limited evidence regarding adaptations to models of care and challenges associated with reconfiguring service delivery. This review aimed to identify and summarize practice-level strategies used to ensure the provision of routine primary care during the COVID-19 pandemic response in order to inform current and future practice.
Methods
We conducted a systematic search for relevant peer-reviewed literature to 15 December 2020 using PubMed/MEDLINE, SCOPUS, and Cochrane Library. A combination of key terms was used including the following: physicians, general practitioner (GP), family, registrar, doctor, primary, health, care, general, practice, usual, regular, routine, COVID, SARS-CoV-2, “model of care,” “models of care,” the MeSH term “organizational models,” “family practice,” “primary health care,” “primary care,” and “general practice.” Terms were grouped according to key concepts—primary care, COVID-19 pandemic, and models of care using truncation and Boolean operators “AND” and “OR.” The search string was developed and refined in PubMed and adapted for the other databases (refer to Supplementary Material). Searches were supplemented by hand searching of reference lists of eligible studies and by recommendations of additional articles from team members some of whom are primary care clinicians as well as primary care researchers. Gray literature sources and non-English publications were not included in the review.
Title and abstract screening was conducted by 2 independent reviewers (SM, ES) as was full text screening of relevant articles (JD, SM). Conflicts were resolved in consultation with a third reviewer (JD or ES). Peer-reviewed publications were included in the review if they were based in primary care and described practice-level changes to the provision of routine care in response to COVID-19. Publications were excluded if they were commentaries and guidelines on models of care, related to hospital or community care or allied health services, and specific to education and training. Publications that focused only on the use of telehealth without describing adaptations and strategies from a practice standpoint were also excluded.
Included papers were assessed for methodological quality or risk of bias (SM, JD, ES, SH, GD) using the Mixed Methods Appraisal Tool.12 Data were extracted from studies by all team members (ES, JD, SM, GD, SH) using a data extraction form that addressed changes to delivery models, impact on primary care functions, and challenges encountered in reorganizing services. Narrative synthesis, an approach used to summarize, compare, and integrate findings from included studies,13 was used to classify strategies adopted by primary care providers (PCPs) to facilitate provision of routine care, and identify challenges to adaptation. Results were framed and interpreted using Burns et al.’s framework for primary care provision in disasters,14 which compares characteristics of primary care response across disaster and nondisaster scenarios. We equated COVID-19 with Burns’ theory of disaster-related care and compared this with nondisaster usual or routine primary care (see Table 1).
Table 1.
Application of the findings to Burns et al.’s framework for disaster-related care.14
| Disaster health care: primary care surge | Disaster-related health conditions (acute distress and acute physical Injuries) | Disaster-related holistic needs (PCPs providing a safe place with trusted health care support for a broad range of needs) | Disaster-related medical needs (Deterioration of medical conditions, adjustment and supply of medications or medical supplies) | Disaster-related long-term care (Acute exacerbations of chronic conditions; delayed presentations) | Disaster-related preventive care (e.g. prevention, early intervention, health education and promotion) | Disaster-related coordination of care (across usual providers and emergency providers) | Disaster-related care within the local community context (contextually appropriate health care, health care for secondary community adversities and events) |
|---|---|---|---|---|---|---|---|
| • Telehealth (e.g. triage, screening of acute conditions) | • Telehealth—management of physical and psychosocial issues | • Telehealth management of chronic conditions | • Telehealth | • Telehealth | • Telehealth aiding coordination of referrals and care | • Telehealth | |
| • Limiting in-person care when possible including through home visits | • Limiting in-person care | • Limiting in-person care—cancellation or suspension of services | • Limiting in-person care | • Limiting in-person care—cancelling/deferring services including screening and immunization | • Enhancing surge capacity | • Proactively contacting high-risk individuals | |
| • Adopting public health measures (e.g. segregating care, PPE) | • Adopting public health measures | • Proactively contacting high-risk individuals with chronic disease | • Adopting public health measures | • Adopting public health measures to prevent the spread of COVID-19 | • Proactively contacting high-risk individuals in coordination with other health care providers and social support services | • Community outreach e.g. home delivery of medication and food, mobile COVID-19 testing and vaccination sites | |
| • Enhancing surge capacity to meet increased care needs (e.g. increasing staff and work hours) | • Proactively contacting high-risk individuals (e.g. elderly, homeless, minorities) | • Proactively contacting individuals with unstable chronic disease | • Proactively contacting high-risk individuals | ||||
| Usual non disaster primary care | Usual daily health care from usual primary care physician | Biopsychosocial health care from usual trusted health care provider | Management of existing medical conditions | Management of acute exacerbations of chronic conditions | Activities in public health, preventive care, and health promotion | Coordination across specialists, allied health, inpatient, and outpatient providers | Care within the context of the community population and health profile, cultures, and values |
| Routine primary care provision |
We defined primary care as the first point of health care access, with a focus on general practice, family practice, or office-based medical care. PCPs refer to medical or nursing practitioners who provide care in this setting including family doctors, GPs, family physicians, primary care physicians, nurses, and nurse practitioners.
Results
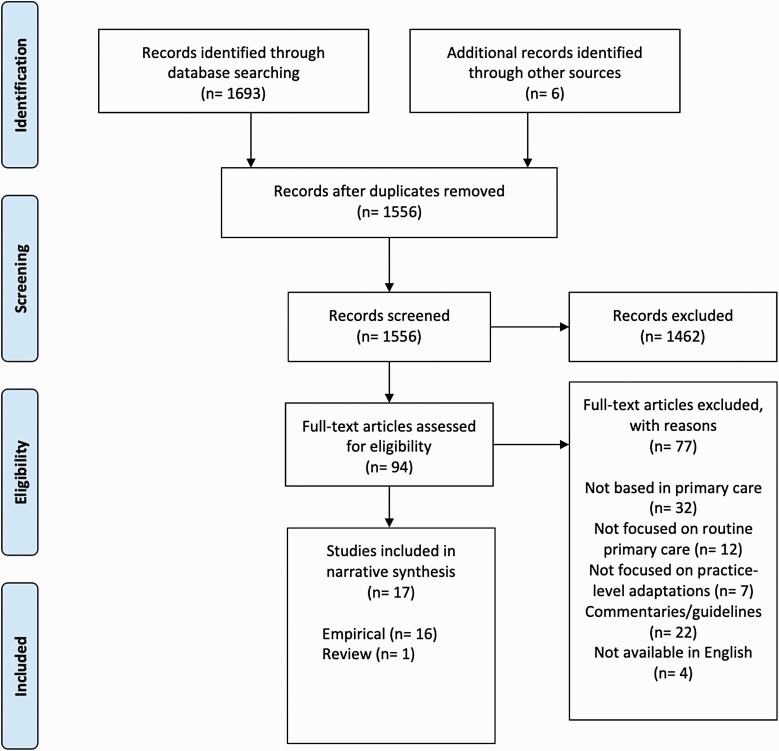
One thousand six hundred and ninety-nine publications were identified, of which 17 studies were included in the review (see Fig. 1). These included 16 empirical studies,15–30 including 8 case studies,23–30 and 1 review.31 The evidence base was generally low in quality with many studies having a high risk of bias based on study design and methodology. Tables 2 and 3 provide summaries of included studies and study characteristics respectively. A matrix of usual nondisaster care functions covered by the studies is provided in Table 4.14
Fig. 1.
PRISMA flow diagram of the study selection process.
Table 2.
Studies describing adaptations and challenges (published in 2020).
| Citation | Country | Study design | Population description | Specific health condition | Adaptations/strategies | Challenges |
|---|---|---|---|---|---|---|
| Al-Busaidi and Martin (2020) | New Zealand | Case study | PCPs (n = 12) | General primary care | Introduction of virtual/remote consultations (via email, texting, telephone, and videoconferencing); in-person visits only when appropriate; cancelation/suspension of usual procedures including admitting/enrolling new patients and online patient portal booking function (patients still able to request repeat prescriptions and communicate with their GP); screening appointment requests for COVID-19/triaging all “acute” consultations over the phone; establishing “infectious phone calls and clinic” (included drive through consultations and testing of symptomatic individuals who met testing criteria, with referral to local COVID center for further assessment where necessary); reduced working hours and number of staff onsite; suspending in-person collection of lab/imaging request forms, prescriptions, medical off work certificates and other forms; placing signage in the centre’s entrance and notifications online including website and social media accounts to inform patients of COVID-19 related policies; PPE use | Patients: Reported resistance to telehealth by some older adults due to preference of in-person consultations, aversion to technology, and perceived low value for cost; most patients found video consultations challenging due to technical issues resulting in low uptake of video consultations (majority of consults conducted by telephone) Practitioners: considerable reductions in financial revenue |
| Bhatti et al. (2020) | Canada | Qualitative | Community-governed primary health care organizations providing community-based care to at-risk populations (n > 70) | General primary care | Rapid adoption of virtual care (e.g. phone, online platforms such as Zoom, Facebook); in- person care and services; outreach and offsite in-person support; mental health and wellness checks to identify at-risk individuals; increased working hours, staffing for isolation centers to ensure safety and care of all; collaboration with community partner organizations to ensure basic needs met (e.g. housing, food); provision of temporary safe space/shelter for homeless or those at risk of domestic violence | Patients: Virtual care inaccessible for patients living in poverty if they did not have access to the internet or a device; safety concerns regarding homeless and precariously housed who had very little in terms of basic support |
| Brey (2020) | South Africa | Case study | Public sector primary care facilities providing care to at-risk populations (including those with chronic conditions and from a low-socioeconomic status) | General primary care | Home delivery system for delivering medications directly to patients homes to minimize potential exposure to COVID (key components included delivery of medications to primary care facility-based pharmacies from a central dispensing unit, verification of patient addresses, labeling of medication parcels, delivery of parcels by nonprofit organizations through a network of CHWs); increased workforce | Patients: Privacy concerns, i.e. home delivery associated with potential for inadvertent disclosure of HIV positive status to family members Practitioners: Many patients not contactable by phone and many addresses were incorrect; potentially increased workload for CHWs due to changing role |
| Danhieux et al. (2020) | Belgium | Qualitative | Primary care practices (n = 16) | General primary care | Telehealth (including telephone consultations in collaboration with COVID-19 triage posts); triage of patients with COVID-19 symptoms; risk stratification/needs assessment and proactive contacting of at-risk patients including those with chronic disease; support for self-management; planning for both patient exacerbation and epidemiological impact; multidisciplinary collaboration; cancelation of usual procedures including suspension of services considered non-essential, e.g. services provided by nurses and dieticians put on hold, also driven by loss of financial revenue | Patients: Perceived resistance due to patient preferences, lack of perceived need and time due to lengthy COVID-19 consultations; technology literacy (e.g. elderly unable to use telehealth) Practitioners: Resistance to telehealth use related to unfamiliarity with this mode of conducting consultations, ethical objections, and perceived inability to assess patients effectively; reduced capacity in some practices due to sidelining of health workers including dieticians and nurses which adversely impacted provision of robust chronic care; financial losses due to drop in consultations |
| Donohue (2020) | United States | Case study | Primary care practices providing services to community dwelling seniors | General Primary care | Telehealth use including remote patient monitoring for chronic conditions (e.g. BP, glucose, heart rate) and provision of care via smart phones and home monitoring devices | Patients: Difficulty accessing some IT equipment Providers: Financial losses |
| Falicov et al. (2020) | United States | Case study | Mental health professionals including primary care physicians providing services to vulnerable populations at a no-cost community Student Run Free Clinic | Mental health | Telehealth (phone and video consultations) adopted for the provision of health, mental health services and support, patient education/ health promotion and coordination of care; patient and practitioner training in IT use; cancelation of usual procedures including suspension of face-to-face special support group sessions; enhanced reliance on promotoras (lay health facilitators and advisors that serve as links between mental health team and the community) to facilitate setting up and confirming appointments/legitimizing mental health care needs; increased flexibility in convening and conducting psychotherapy sessions to overcome contextual constraints as a strategy to reduce inequitable access; delivery of medications and food to patients homes to minimize transmission risk; proactive contacting of clients/ patients | Patients: Suspension of in- person group therapy/educational sessions undermined clients’ sense of community and connectedness; technological barriers to accessing care for patients without computers, internet, cell phones/smartphones, computer literacy—potential for worsening inequities in access; other barriers included lack of time due to care giving duties, work commitments, privacy concerns (e.g. work/ housing situations with no privacy) Providers: Interpretation during phone or video consultations more taxing for providers and especially for interpreters due to lengthy sessions and lack of nonverbal cues; patients did not always answer or return phone calls from physicians although they did respond to calls from the promotoras who were known and trusted community members |
| Franzosa et al. (2020) | United States | Qualitative | Practices providing home-based primary care (n = 6) | General primary care | Patient facing adaptations included adoption of telehealth which was balanced with in-person care provided in patients homes; proactive assessments and screening of high-risk patients including for social determinants of health (e.g. housing, food, security, loneliness); maintaining patient trust (transparency, honesty, active listening); cancelation of usual procedures including ceasing admission of patients. Practice facing adaptions included fostering supportive multidisciplinary team environments (daily huddles, education, workflow/ operational changes, case review); providing emotional support for staff (acknowledging patient deaths, modifying staff schedules, peer support) |
Patients: Video consultations were challenging for patients with cognitive and physical limitations and they often required provider or caregiver assistance; some patients preferred continued in- person care and needed support to understand why this was no longer possible. Providers: Staff grief due to deaths of many long-term patients; stress associated with intensified workload |
| Hinchman et al. (2020) | United States | Review | PCPs (n > 500) | General primary care | Virtual care to minimize in-person visits (e.g. remote management of preexisting conditions); measures to minimize health care disparities during the pandemic including waiving of patient co-payment fees to remove financial barriers to care for high-risk individuals, improved access to testing, outreach programs; cancelation of usual procedure including suspension of routine checks and new patient intakes; increased workforce | Patients: Inequities in accessing telemedicine (particularly amongst racial minorities with low income, patients with no internet and lack of access to smart devices); usability barriers (lack of training and knowledge on how to use telemedicine) Providers: Infrastructural challenges to dissemination or optimization of virtual care; lack of proper training in use of telemedicine; reimbursement, licensure and credentialing restrictions; limited capacity for testing, PPE shortages, and challenges minimizing exposure of healthy patients compounded by stress of tackling an abundance of patient concerns; staff absence due to quarantine |
| Kumar et al. (2020) | United Kingdom | Case study | GPs and other primary care clinicians requiring respiratory specialist advice | Respiratory conditions | Establishment of a respiratory specialist telephone hotline to support GPs in the provision of COVID-19 specific and non-COVID-19 respiratory care; regular educational webinars for GPs to facilitate sharing of lessons learnt (entailed discussions of key themes emerging from calls to the hotline; regular updating of local guidelines on the management of COVID-19 in the community (based on key themes) | Providers: Availability of respiratory specialists to staff the hotline; challenges streamlining information flow and managing time during high service usage; ensuring appropriate governance of the system, risk reporting and record keeping; uncertainties when providing advice related to COVID-19 due to the rapidly evolving evidence |
| Lemire and Slade (2020) | Canada | Quantitative | Family physicians (n > 4,000) | General primary care | Shift to telehealth (telephone mostly); enhanced IPC measures (e.g. PPE use, environmental cleaning, reconfiguring patient waiting areas); working in new settings (in addition to their offices) to meet care demands; screening for COVID-19; reduced work hours | Providers: Loss of revenue due to adjustments (shift to telehealth and fewer inpatient visits); inadequate PPE, practitioners concern regarding neglected care |
| Pierce and Pierce (2020) | United States | Case study | PCPs | General primary care | Expansion of telehealth consultations (phone, video, online, secure texting); home visits (initially increased due to more requests for home visits) and in-person/office consultations; staff training in point-of-care ultrasound for COVID-19 cases; dedicated areas for nasopharyngeal swab testing, point-of-care coagulation tests and nebulizer treatments | Patients: Limited availability of vendors to expand telemedicine consultation to reduce long waits, travel and out-of- pocket costs; virtual group counseling for substance use disorders not compatible with mutual support and camaraderie with fellow patients when compared with in-person sessions Providers: loss of social primary care rounds in local hospital due to transmission risk |
| Rawaf et al. (2020) | International | Qualitative | Members of the Global Forum on Universal Health Coverage and Primary Care (n = 54) | General primary care | Adoption/expansion of virtual care (telephone, online, email, patient apps) for patient consultations and monitoring to minimize COVID-19 transmission risk whilst ensuring continuity of care; screening/ triaging of suspected cases of COVID-19; specific care pathways for non-COVID-19 patients, and COVID-19 suspects (e.g. dedicated practice hours and spaces/entrances; direction of suspects to COVID-19 community clinics staffed by primary care professionals for further assessment thus relieving pressure from regular primary care clinics and enabling them to see lower-risk patients); cancelation/suspension of usual procedures including postponement of “regular” chronic care (potential risk for increased health problems due to delayed access) | Patients: Limited options to adoption of virtual care in resource limited settings (e.g. LMICs) Providers: Shortages of PPE and testing capacity- some family physicians withdrew services due to inadequate PPE |
| Rossi et al. (2020) | United States | Case study | PCPs from the Veteran’s Health Administration (VHA) | Intimate partner violence (IPV) | Telehealth use for IPV screening, safety planning and provision of resources/support (telephone, video, online); provision of IPV guidance and resources e.g. virtual care considerations such as environmental safety check for IPV screening to enable safe opportunities to discuss IPV-related information, whilst reducing risk of danger for affected women; use of a | Patients: challenges related to limited space for privacy and safety with use of virtual platforms- potential for reductions in patient disclosure opportunities and difficulty obtaining information on IPV resources and services by affected women Providers: privacy and safety concerns with telemedicine (unlike in-person office visits) |
| multimethod approach to raise awareness and enable access to services through social media, internal emails, staff, and veteran specific fact sheets; provision of links to external stakeholders with COVID-19-specific information and risk reduction strategies; regular updating of resources and referral information (e.g. for shelters) and dissemination of information to interprofessional staff who may screen for IPV or provide resources and support | ||||||
| Saint-Lary et al. (2020) | France | Quantitative | GPs (n = 5,425) | General primary care | Digital health (telephone, video consultations, email); cancelation of unscheduled consultations; adoption of public health functions i.e. prevention/mitigation measures (screening of symptomatic patients, specific pathways for COVID-19 suspected patients including a dedicated waiting area, home visits and reorganization of work duties, PPE use, hygiene and protective measures); staff training (receptionists) to identify COVID-19 suspected patients | Providers: PPE shortages |
| Saso et al. (2020) | International | Mixed method | Members of the Immunizing Pregnant Women and Infants Network (n = 48) | Routine immunization (maternal and infant vaccines) | Use of telemedicine for care delivery (particularly in high income countries, e.g. telephone or virtual consultations); suspension/cancelation of services(in low- and middle-income countries [LMICs]); adoption of public health functions e.g. social distancing and appropriate hygiene at immunization sessions, scheduling of sessions with few individuals, environmental cleaning and widespread use of masks; sensitization and awareness raising for care givers to report suspected cases of COVID-19 in their communities to enable detailed investigation and prevention of spread of disease; communication with parents to inform them on the importance of attending routine vaccinations; other measures including mobile/ drive-through vaccine schemes and repurposing of existing locations to facilitate vaccine delivery (e.g. use of local football grounds for maternity outpatient clinics) | Providers: Disruptions to clinics including canceled clinics specifically in LMICs; shortages in staffing, PPE, and vaccines |
| Spelman et al. (2020) | United States | Case study | PCPs from the VHA (n = 80) | General primary care | Expansion of virtual care (telephone, video consultations, secure messaging); establishment of home telework rotations (clinics staffed by those onsite with maintenance of adequate personnel to address health care needs); in-person visits where appropriate, e.g. critical needs; mandatory staff training in use of virtual platforms, and peer-to-peer informatics support; establishment of virtual respiratory urgent clinics to support increased demand for care (staffed by licensed independent primary care providers); increased working hours including increase in access to clinics from 1 to 3 clinics/day, and adoption of an afterhours service to ensure COVID-19-positive test results were responded to quickly; development of new COVID-19 note templates to standardize and guide virtual assessment and medical decision-making, inform patients of test results and give advice regarding isolation and return to work; awareness raising campaign emphasizing importance of virtual care; provision of frequent messaging around COVID-19 to veterans | Patients: Barriers to virtual care included software that required many steps to schedule video consultations; non- intuitive interface for patients; many lacked access to smartphone devices/ ability to easily use the VA’s platform; practical challenges re: obtaining vital signs as some patients did not have access to thermometers, blood pressure monitors and pulse oximeters Providers: Limited ability to conduct physical assessments with virtual care which may have resulted in missed diagnoses; practical challenges obtaining vital signs due to limited access to home monitoring devices; challenges communicating with patients with hearing and vision impairment |
| Verhoeven et al. (2020) | Belgium | Qualitative | GPs | General primary care | including separate patient flows for COVID-19 and non-COVID (both individual practices and specialized “corona” centers); establishment of GP run corona centers for management of COVID-related conditions; transition to telehealth (telephone triage and consultations for both COVID and non-COVID-related conditions, digital prescriptions/issuance of sick leave certificates etc); cancelation/restructuring of usual procedures including online booking function, diagnostics, screening for non-COVID conditions; increased opening hours; regular updating of practice websites to reflect advice or guidance by local/national authorities; adoption of more structured work schedules (agreements regarding division/reallocation of jobs for virtual and in-person consultations and work in the specialized centers); proactive contacting of vulnerable or high-risk patients; collaboration with other GPs, specialists, allied | Patients: Challenges with telemedicine including limited ability for some patients to communicate their needs, limited intercultural communications and associated language barriers; communication also affected because of PPE- masks made it challenging to understand providers Providers: Challenges with telemedicine including loss of nonverbal communication, limited intercultural communications and associated language barriers, less information obtainable through phone consults making clinical decision-making more difficult—generated concerns about missing important diagnoses; difficulty organizing acute psychological care (telephone consults usual not sufficient); challenges differentiating urgent from non-urgent problems by phone; PPE use made consultations less |
| health, public health; COVID-19 prevention/mitigation measures e.g. social distancing, environmental cleaning, removal of non-essential materials to limit contamination; use of PPE | smooth and longer and affected communication during physical assessments (i.e. patients sometimes did not understanding what was said, and masks made it difficult to show empathy); PPE shortages; increase in administrative tasks (considerable time spent providing sick leave certificate, digital prescriptions, writing emails etc); financial loss due to reductions in-person consultations |
Table 3.
Study characteristics.
| Characteristics | Number (n = 17) |
|---|---|
| Country | |
| South Africa | 1 |
| New Zealand | 1 |
| United States | 7 |
| Canada | 2 |
| United Kingdom | 1 |
| France | 1 |
| Belgium | 2 |
| International | 2 |
| Study design | |
| Qualitative | 5 |
| Quantitative | 2 |
| Mixed method | 1 |
| Review | 1 |
| Case study | 8 |
| Focus | |
| General primary care | 13 |
| Specific health condition | 4 |
Table 4.
Usual nondisaster primary care functions covered by included studies.
| Studies | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Functions | Al-Busiadi 2020 (New Zealand) |
Bhatti 2020 (Canada) |
Brey 2020 (South Africa) |
Danhieux 2020 (Belgium) |
Donohue 2020 (United States) |
Falicov 2020 (United States) |
Franzosa 2020 (United States) |
Hinchman 2020 (United States) |
Kumar 2020 (United Kingdom) |
Lemire 2020 (Canada) |
Pierce 2020 (United States) |
Rawaf 2020 (International) |
Rossi 2020 (United States) |
Saint-Lary 2020 (France) |
Saso 2020 (International) |
Spelman 2020 (United States) |
Verhoeven 2020 (Belgium) |
| First-contact care (acute presentations) | X | X | X | X | X | X | X | X | X | X | |||||||
| Biopsychosocial care | X | X | X | X | X | X | X | X | X | ||||||||
| Management of existing conditions | X | X | X | X | X | X | X | X | X | X | X | X | X | ||||
| Management of acute exacerbations of chronic conditions | X | X | X | X | X | X | X | ||||||||||
| Preventative care and health promotion | X | X | X | X | X | X | X | ||||||||||
| Coordination across specialists, allied health, in and outpatient providers | X | X | X | X | X | X | X | X | X | X | X | ||||||
| Community- based care | X | X | X | X | X | X | X | X | X | X | X | X | X |
X denotes functions covered by studies (functions adapted from Burns et al.’s framework for disaster-related care14).
Adaptations to models of care
Five key strategies were adopted to facilitate provision of regular health care: (i) Integrating telehealth; (ii) Limiting in-person care; (iii) Adopting public health measures; (iv) Enhancing surge capacity; and (v) Proactively contacting vulnerable patients.
Integrating telehealth
The shift to remote care was necessitated by the need to prevent the spread of COVID-19 and to ensure continuity of care while protecting providers and patients, especially vulnerable individuals such as the elderly, and those with chronic illness.15–17,19,20,22,23,25,28–31 Telehealth was widely used to facilitate this, with most studies (n = 15) describing its integration into routine care.15–23,25,26,28–31
For many primary care settings, the transition to telehealth occurred rapidly, aided by legislative changes in response to the pandemic.19,20,22,25,28,31 In the United States, for example, the temporary easing by most states of regulations governing telehealth licensing and reimbursement requirements for health care providers accelerated its adoption and expansion.25,28,31 Similar payment mechanisms were provided in the Netherlands, France, and Belgium to promote telehealth services.19,20,22 Other facilitators included technical and organizational factors such as existing telehealth infrastructure (e.g. internet access, digital platforms, and devices),20,23,26,28,30 training of providers and patients in the use of telehealth,26,30,31 enabling organizational funding models, and provider incentives for telehealth adoption (e.g. pay for performance).15,30
Telehealth was provided through a variety of ways including telephone,15–23,25,26,28–31 video consultations,15–23,26,28–30 email,18–20,22,23,29 text messaging,23,28,30 online patient portals,22,23,28 and smart phone apps.19,25,29 Telephone was the primary means of care delivery in many practices and reportedly constituted the majority of remote consultations.18,20,22,23,30
Telehealth was adapted to support the provision of a range of routine care functions including disease management15–17,19,22,23,25,26,28,30,31 and coordination of care.15–17,19,22,26,28–30 Telephone and video consultations were commonly used for triaging patients and treating acute and chronic conditions that did not require in-person management including nonurgent presentations and stable chronic conditions.15–19,22,23,25,26,28–31 Two studies described the use of medical home monitoring devices such as Bluetooth-enabled blood pressure monitors, pulse oximeters, and glucose meters to support chronic disease management.25,30 Telehealth enabled care coordination between PCPs and other health care providers including allied health and hospital-based specialists.15–17,19,22,26,28–30
Telehealth facilitated the screening, triage, and management of suspected cases of COVID-19,16,19,22,23,30 and in certain contexts such as in Belgium, this was done in collaboration with designated COVID centers or triage posts so as to maintain safe access to routine primary care.16,22 Other reported uses of telehealth included aiding the provision of essential services (e.g. immunization and abortion services),21 assessing and addressing patient needs,15–17,22,29 electronic prescribing,22,23 and issuance of medical certificates or laboratory and imaging requests.22,23
Limiting in-person care
Practices balanced remote and in-person care in response to the pandemic, limiting the latter to help contain the spread of COVID-19. Nine studies from Canada,15 United States,17,26,28,30,31 New Zealand,23 South Africa,24 and Belgium22 reported measures taken (other than telehealth) to limit direct patient care. These included canceling or deferring appointments,22,23,31 suspending intake of new patients,17 advising patients against in-person care when possible,23,30 and avoiding in-person group activities including social support programs.15,24,26,28 In-person consultations were undertaken either onsite,23,30 or through home visits,17,24,26 or both15,22,28 and were usually reserved for acute and urgent presentations15,22,23,28,30 and management of at-risk patients.15,17,22,24
Adopting public health measures
As part of promoting safe access to routine care, PCPs adopted public health measures, which commonly included screening patients for symptoms of COVID-19 and establishing dedicated care pathways for non-COVID- and COVID-related problems.16,18–20,22,23,25,30 Patient screening was usually conducted remotely, and in some of the practices examined, this was aided by receptionists trained in identifying suspected cases of COVID-19.20,23 Other infection control measures taken included having dedicated clinic hours19,20 and onsite areas for symptomatic patients,19,20,23,28 reorganizing patient waiting areas to make them safer (e.g. limiting number of patients, removing unnecessary material to prevent contamination),18,21,22 personal protective equipment (PPE) use by staff,18–23,28,31 widespread wearing of masks and maintaining appropriate hygiene,20–22 and environmental cleaning.18,21,22
Enhancing surge capacity
Practices took steps to strengthen their capacity to meet increased care needs during the pandemic. Experiences from the United States,17,26,28,30,31 South Africa,24 Belgium,22 and Canada15,18 described a range of strategies, which included expanding staffing (e.g. recruiting temporary employees or retired physicians),18,24,30,31 increasing work hours,15,22,30 staff training and prioritizing PPE,16,22,26,28,31 as well as redeploying staff to meet the increased demand in care.15,17,18
Proactively contacting high-risk individuals
Some primary care practices took a proactive approach to identify and engage with high-risk individuals.15–17,22,26,31 These included the elderly, individuals with chronic diseases, the homeless and those of lower socioeconomic status, essential workers, as well as racial and ethnic minorities.15–17,22,26,31 Risk stratification and active follow-up of vulnerable patients was aided by electronic medical records,15,16 assessments for socioeconomic challenges including housing and food insecurity,15,17,26 and by practitioners’ intimate knowledge of such persons.16,26 Proactive care was provided through various means including telehealth15–17,22,26 and in-person visits,16,17 in coordination with other health care providers and social support services.
Proactive care comprised an holistic, integrated, and community-based approach to the provision of routine care during the pandemic. Providers engaged in community outreach to provide services and support, with an emphasis on vulnerable and underserved patients, through traditional and innovative strategies including home delivery of medications and food15,24,26; provision of addiction and harm reduction services as part of outreach15; drive through vaccine schemes21; and mobile COVID-19 testing and vaccination sites to overcome barriers to access.21,31
Challenges encountered in adapting new practice models of care delivery
A range of challenges experienced by patients and practitioners were reported across the studies. Difficulties encountered by patients mostly related to the shift to telehealth.15–17,19,22,23,25,26,28–31 These included barriers to access due to low-technology literacy,17,23,26,30,31 aversion to telehealth,23 and inadequate internet connectivity or access to devices such as smartphones and laptops, especially among under-resourced and underserved patients.15,26,30,31 This raised concerns about disparities in access to care during the pandemic.15,26,31 Other issues related to the use of telehealth included language and cognitive barriers,17,22,30 privacy and safety concerns,26,29 lack of access to home monitoring medical devices such as thermometers, blood pressure monitors and pulse oximeters,25,30 and loss of a sense of community and connectedness with fellow patients which in-person group activities engendered.26,28
Similarly, practitioner challenges revolved around the adoption of telehealth.16–18,22,23,25,26,29–31 These included infrastructure limitations (e.g. internet connectivity),23,25,28,31 regulatory barriers,17,26,31 concerns regarding patient confidentiality and safety,26,29 digital literacy issues,16,30 reluctance to provide care virtually,16 practical limitations on the ability to examine patients,16,22,23,30 communication barriers,22,26,30 and loss of financial revenue due to reductions in in-person consultations.16,18,22,23,25
Other challenges included staff shortages or redeployment to other settings, including acute and hospital-level care,15–19,21,31 and shortages of products including PPE,18–22,31 logistical challenges providing respiratory specialist support to PCPs such as availability of specialists,27 increased workload and work-related stress,16–19,22,31 and limited support and guidance from authorities on response measures.17,19,20,22
Discussion
This review identified key strategies adopted by PCPs to cope with changes in routine care during the pandemic. Providers were quick to adopt innovative, flexible, and integrated models of care delivery to ensure continuity and safe access to care. Burns et al.’s framework for primary care provision in disasters comprehensively covers the functions of primary care and served as a useful lens to study and reflect on the changes to routine primary care during the COVID-19 pandemic.14
Practices examined in the included studies considered these functions to varying degrees, giving greater consideration to aspects such as acute and chronic disease management, biopsychosocial or holistic care, and coordinated care within the community context, while there was less consideration of functions such as preventive care and health promotion (refer to Table 4). Primary care remained the first point of contact, supported by the use of telehealth to address acute non-COVID and COVID-related presentations that did not require in-person management. Similarly, a holistic, coordinated, and community-based approach to the delivery of care was maintained with an emphasis on vulnerable patient groups. Practitioners collaborated among themselves and leveraged existing partnerships with other providers, such as COVID centers, hospital-based specialists, and community services to coordinate care. However, there was little evidence on linkages with public health or government entities, with some studies suggesting suboptimal coordination and guidance on response measures. Previous research32–36 has similarly highlighted the lack of collaboration between public health and primary care in planning and response, which has important implications for maintaining safe access to regular care during a pandemic.
Disruptions to chronic care delivery during the pandemic are well recognized and were highlighted across some of the studies covering this function of routine care.16,17,19,22,31 A combination of factors contributed to this including prioritization of acute services by providers to meet an increased demand for care and a reduced capacity to reorganize chronic care.16,19,22 Disruptions to chronic disease management were worsened by public health containment measures (e.g. lockdowns and physical distancing), and the reluctance of some patients to seek care due to fears of becoming infected.16,19,22 Consequently, these conditions were often dealt with inadequately, which is concerning given the potential for increased illness and death due to delayed care. Equally concerning was the lack of attention given to preventive care and health promotion (such as screening activities and immunizations), which were substantially impacted due to the cancelation or suspension of services in certain contexts including low- and middle-income countries.21,22,31 As with chronic care, disruption to these lifesaving activities has important health implications including avoidable illness and potential resurgence in vaccine-preventable diseases.5,37–39 Interruptions to routine care during the pandemic have been reported by other studies,1,4,40 which underscores the need to strengthen primary care capacity to promote access to a broader range of regular health services during pandemics, and to reduce the potential harmful effects of delayed care on patients, providers, and primary care systems.
Strengths and limitations
The limitations of this review include a focus only on peer-reviewed literature and exclusion of non-English publications; as such we may have missed relevant adaptations and strategies discussed in the gray literature and in languages other than English. Due to time constraints, we excluded telehealth publications that did not discuss adaptations from a practice standpoint and consequently did not explore its use beyond these changes. The strength of our study lies in demonstrating the application of the framework by Burns et al. to reflect on practice-level adaptions and impacts on functions of routine care during the COVID-19 pandemic.
Conclusion
The COVID-19 pandemic resulted in substantial disruptions to the provision of routine primary care. This review demonstrates the agility and innovative capacity of PCPs, who rapidly adopted new models of care delivery to ensure continuity and safe access to care. While practitioners rose to the occasion, they encountered substantial challenges, not least being limited guidance and support with adaptations. Our findings underscore the need for enhanced efforts including timely and adequate investment by authorities to optimize the provision of comprehensive routine care during pandemics. These lessons are also important as many PCPs again shift their model of care delivery to support national COVID-19 vaccination programs. Changes to routine primary care delivery are likely to continue as the pandemic evolves; supporting primary care practices with response measures and in maintaining new models of care, including telehealth integration, is critical to ensure care continuity. While our review identified key strategies used to maintain the provision of routine primary care during the pandemic, further research is needed to evaluate the effectiveness of new models of service delivery, including PCPs’ experiences and perceptions, patient reported outcomes, and costs. In addition to determining best practices to ensuring continuity of routine care during the COVID-19 pandemic, such research will help broaden the evidence based on primary care response to infectious disease outbreaks for future reference.
Supplementary Material
Contributor Information
Sethunya Matenge, Department of Health Services Research and Policy, College of Health and Medicine, Australian National University, Canberra, ACT, Australia.
Elizabeth Sturgiss, School of Primary and Allied Health Care, Monash University, Melbourne, VIC, Australia.
Jane Desborough, Department of Health Services Research and Policy, College of Health and Medicine, Australian National University, Canberra, ACT, Australia.
Sally Hall Dykgraaf, Rural Clinical School, ANU Medical School, College of Health and Medicine, Australian National University, Canberra, ACT, Australia.
Garang Dut, ANU Medical School, College of Health and Medicine, Australian National University, Canberra, ACT, Australia.
Michael Kidd, ANU Medical School, College of Health and Medicine, Australian National University, Canberra, ACT, Australia; Australian Government Department of Health, Canberra, ACT, Australia; Department of Family and Community Medicine, The University of Toronto, Toronto, Canada; Department of General Practice, The University of Melbourne, Melbourne, VIC, Australia; Southgate Institute for Equity, Health and Society, Flinders University, Adelaide, SA, Australia.
Funding
No funding to declare.
Conflict of interest
The authors are employed by or seconded to the Australian Government Department of Health. There are no additional interests to declare.
References
- 1. Levene LS, Seidu S, Greenhalgh T, Khunti K. Pandemic threatens primary care for long term conditions. BMJ. 2020;371:m3793. [DOI] [PubMed] [Google Scholar]
- 2. Haldane V, Zhang Z, Abbas RF, Dodd W, Lau LL, Kidd MR, Rouleau K, Zou G, Chao Z, Upshur RE, et al. National primary care responses to COVID-19: a rapid review of the literature. BMJ Open. 2020;10(12):e041622. doi: 10.1136/bmjopen-2020-041622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Garg S, Basu S, Rustagi R, Borle A. Primary health care facility preparedness for outpatient service provision during the COVID-19 pandemic in India: cross-sectional study. JMIR Public Health Surveill. 2020;6(2):e19927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organisation. Pulse survey on continuity of essential health services during the COVID-19 pandemic – interim report. Geneva, Switzerland: WHO. [accessed 2021 April 1]. https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS_continuity-survey-2020.1. [Google Scholar]
- 5. Blanchet K, Alwan A, Antoine C, Cros MJ, Feroz F, Guracha TA, Haaland O, Hailu A, Hangoma P, Jamison D, et al. Protecting essential health services in low-income and middle-income countries and humanitarian settings while responding to the COVID-19 pandemic. BMJ Glob Health. 2020;5(10):e003675. doi:10/1136/bmjgh-2020–003675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Duckett S. What should primary care look like after the COVID-19 pandemic? Aust J Prim Health. 2020;26(3):207–211. [DOI] [PubMed] [Google Scholar]
- 7. Levis M, Shadwick L, Levison J, Matousek S. Primary care transformation in a COVID-19 world. Boston, MA: Center for Primary Care, Harvard Medical School. [accessed 1 April 2021]. http://info.primarycare.hms.harvard.edu/blog/primary-care-transformation-covid. [Google Scholar]
- 8. Webb E, Hernández-Quevedo C, Edwards N, Reed S, Gandré C, Or Z, Cascini F, Winkelmann J, Kroneman M, De Jong J, et al. How have countries restarted more routine ambulatory care activities during the COVID-19 pandemic? Brussels, Belgium: COVID-19 Health System Response Monitor. [accessed 1 April 2021]. https://analysis.covid19healthsystem.org/index.php/2020/11/24/how-have-countries-restarted-more-routine-ambulatory-care-activities-during-the-covid-19-pandemic/. [Google Scholar]
- 9. Desborough J, Hall Dykgraaf S, de Toca L, Davis S, Roberts L, Kelaher C, Kidd M. Australia’s national COVID-19 primary care response. Med J Aust. 2020;213(3):104–106.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kidd M. Australia’s primary care COVID-19 response. Aust J Gen Pract. 2020;49. doi: 10.31128/AJGP-COVID-02 [DOI] [PubMed] [Google Scholar]
- 11. Kidd M. Five principles for pandemic preparedness: lessons from the Australian COVID-19 primary care response. Br J Gen Pract. 2020;70(69):316–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, Gagnon MP, Griffiths F, Nicolau B, et al. Mixed Methods Appraisal Tool (MMAT) version 2018. Montreal, Canada: Department of Family Medicine, McGill University. [accessed 20 February 2021]. http://mixedmethodsappraisaltoolpublic.pbworks.com/w/file/fetch/127916259/MMAT_2018_criteria-manual_2018-08-01_ENG.pdf. [Google Scholar]
- 13. Lisy K, Porritt K. Narrative synthesis: considerations and challenges. Int J Evid Based Healthc. 2016;14(4):201. doi: 10.1097/01.XEB.0000511348.97198.8c [DOI] [Google Scholar]
- 14. Burns P, Douglas K, Hu W, Aitken P, Raphael B. General practitioners in the field – a qualitative study of general practitioners’ experiences in disaster healthcare. Aust J Gen Pract. 2020;49. doi: 10.31128/AJGP-08-19-5054 [DOI] [PubMed] [Google Scholar]
- 15. Bhatti S, Commisso E, Rayner J. A rapid primary healthcare response to COVID-19: an equity-based and systems-thinking approach to care ensuring that no one is left behind. Healthc Q. 2020;23(3):29–33. [DOI] [PubMed] [Google Scholar]
- 16. Danhieux K, Buffel V, Pairon A, Benkheil A, Remmen R, Wouters E, van Olmen J. The impact of COVID-19 on chronic care according to providers: a qualitative study among primary care practices in Belgium. BMC Fam Pract. 2020;21(1):255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Franzosa E, Gorbenko K, Brody A, Leff B, Ritchie C, Kinosian B, Ornstein K, Federman A. “At home with, with care”: lessons from New York City home-based primary care practices managing COVID-19. J Am Geriatr Soc. 2020;69(2):300–306. doi: 10.1111/jgs.16952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lemire F, Slade S. Reflections on family practice and the pandemic first wave. Can Fam Phys. 2020;66(6):468. [PMC free article] [PubMed] [Google Scholar]
- 19. Rawaf S, Allen LN, Stigler FL, Kringos D, Quezada Yamamoto H, van Weel C; Global Forum on Universal Health Coverage and Primary Health Care . Lessons on the COVID-19 pandemic, for and by primary care professionals worldwide. Eur J Gen Pract. 2020;26(1):129–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Saint-Lary O, Gautier S, Le Breton J, Gilberg S, Frappé P, Scheurs M, Bourgueil Y, Renard V. How GPs adapted their practices and organisations at the beginning of COVID-19 outbreak: a French national observational survey. BMJ Open. 2020;10(12):e042119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Saso A, Skirrow H, Kampmann B. Impact of COVID-19 on immunization services for maternal and infant vaccines: results of a survey conducted by imprint-the immunising pregnant women and infants network. Vaccines. 2020;8(3). doi: 10.3390/vaccines8030556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Verhoeven V, Tsakitzidis G, Philips H, Van Royen P. Impact of the COVID-19 pandemic on the core functions of primary care: will the cure be worse than the disease? A qualitative interview study in Flemish GPs. BMJ Open. 2020;10(6):e039674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Al-Busaidi IS, Martin M. The transition to a “virtual practice” in primary care during the COVID-19 pandemic: experience from one medical centre in New Zealand. N Z Med J. 2020;133(1520):91–98. [PubMed] [Google Scholar]
- 24. Brey Z, Mash R, Goliath C, Roman D. Home delivery of medication during Coronavirus disease 2019, Cape Town, South Africa: short report. Afr J Prim Health Care Fam Med. 2020;12(1):e1–e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Donohue D. A primary care answer to a pandemic: keeping a population of patients safe at home through chronic care management and remote patient monitoring. Am J Lifestyle Med. 2020;14(6):595–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Falicov C, Niño A, D’Urso S. Expanding possibilities: flexibility and solidarity with under-resourced immigrant families during the COVID-19 pandemic. Fam Process. 2020;59(3):865–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kumar K, Mak V, Groom K, Razak Y, Brown JL, Hyde T, Bokobza A, Coker RK, Parmar M, Wong E, et al. Respiratory specialists working in different ways: development of a GP hotline and respiratory support service during the COVID-19 pandemic. Future Healthc J. 2020;7(3):e88–e92. doi: 10.786/fhj.2020-0082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Pierce BR, Pierce C. Pandemic notes from a Maine direct primary care practice. J Ambul Care Manage. 2020;43(4):290–293. [DOI] [PubMed] [Google Scholar]
- 29. Rossi FS, Shankar M, Buckholdt K, Bailey Y, Israni ST, Iverson KM. Trying times and trying out solutions: intimate partner violence screening and support for women veterans during COVID-19. J Gen Intern Med. 2020;35(9):2728–2731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Spelman JF, Brienza R, Walsh RF, Drost P, Schwartz AR, Kravetz JD, Pitkin P, Ruser C. A model for rapid transition to virtual care, VA Connecticut primary care response to COVID-19. J Gen Intern Med. 2020;35(10):3073–3076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hinchman A, Ali D, Goodwin BW, Gillie M, Boudreaux J, Laborde Y. Global health is local health: a multidisciplinary perspective of COVID-19. Ochsner J. 2020;20(2):123–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Desborough J, Hall Dykgraaf S, Phillips C, Wright M, Maddox R, Davis S, Kidd M. Lessons for the global primary care response to COVID-19: a rapid review of evidence from past epidemics. Fam Pract. 2021;1–15. doi: 10.1093/fampra/cmaa142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kort R, Stuart AJ, Bontovics E. Ensuring a broad and inclusive approach: a provincial perspective on pandemic preparedness. Can J Public Health. 2005;96(6):409–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kunin M, Engelhard D, Piterman L, Thomas S. Response of general practitioners to infectious disease public health crises: an integrative systematic review of the literature. Disaster Med Public Health Prep. 2013;7(5):522–533. [DOI] [PubMed] [Google Scholar]
- 35. Patel MS, Phillips CB, Pearce C, Kljakovic M, Dugdale P, Glasgow N. General practice and pandemic influenza: a framework for planning and comparison of plans in five countries. PLoS One. 2008;3(5): e2269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tomizuka T, Kanatani Y, Kawahara K. Insufficient preparedness of primary care practices for pandemic influenza and the effect of a preparedness plan in Japan: a prefecture-wide cross-sectional study. BMC Fam Pract. 2013;14:174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Chandir S, Siddiqi DA, Setayesh H, Khan AJ. Impact of COVID-19 lockdown on routine immunisation in Karachi, Pakistan. Lancet Glob Health. 2020;8(9):e1118–e1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. van Weert H. After the first wave: what effects did the COVID-19 measures have on regular care and how can general practitioners respond to this? Eur J Gen Pract. 2020;26(1):126–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wright A, Salazar A, Mirica M, Volk LA, Schiff GD. The invisible epidemic: neglected chronic disease management during COVID-19. J Gen Intern Med. 2020;35(9):2816–2817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Chudasama YV, Gillies CL, Zaccardi F, Coles B, Davies MJ, Seidu S, Khunti K. Impact of COVID-19 on routine care for chronic diseases: a global survey of views from healthcare professionals. Diabetes Metab Syndr. 2020;14(5):965–967. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.