Introduction
Delays in routine cancer screening due to the covid-19 pandemic are being observed worldwide.1 , 3 , 4. Since the Spring of 2020, healthcare systems have been stressed beyond their capacity, and along with the devastating effects of the SARS-CoV-2 virus on the population itself, we are now beginning to see some of the deleterious effects it is having on patient care.
We set out to analyze the effect that the pandemic had on cancer screening in the veteran population. The Veterans Affairs (VA) healthcare system is one of the largest US healthcare systems and a high-volume provider of cancer care, accounting for approximately 3% of all U.S. cancer diagnoses annually.2 Veterans are a high-risk population due to harmful exposures incurred during their time in service, and patients seen at Veteran Affair clinics are a particularly vulnerable population to healthcare disparities.2
Methods
The goal of the project was to analyze the effect that the pandemic had on cancer screening and new diagnoses in the veteran population by evaluating rates of routine cancer screening with low dose CT, mammography, and colonoscopy and new diagnoses of lung, breast, and colon cancer between January 1- December 31 in 2019 and January 1- December 31 in 2020 at two VA outpatient primary care clinic sites in Connecticut. Number of new cancer diagnoses was collected through the VA CT Registry. Reports were run through electronic medical records to analyze number of screening tests completed in the calendar years of 2019 and 2020. This analysis was deemed exempt from Institutional Review Board (IRB) approval. The analyses for this report were conducted as part of a VA data quality assessment project approved by the VA State Healthcare System Research Office.
Results
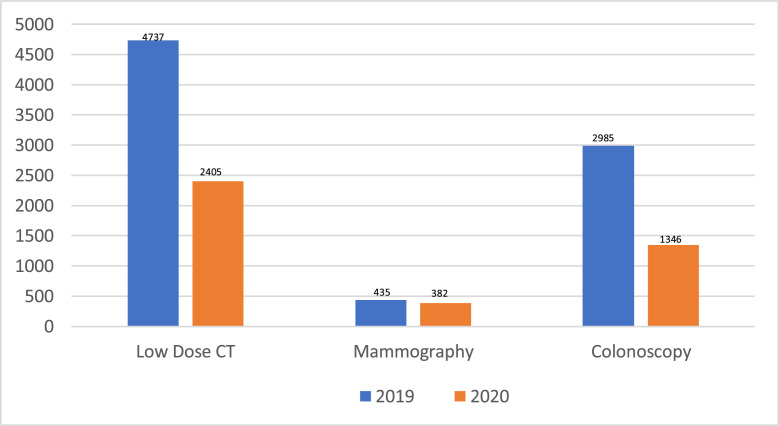
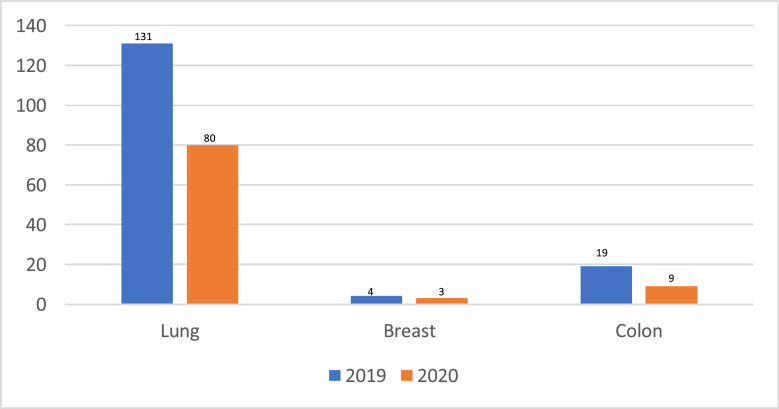
Data from a Veteran Affairs primary care clinic was analyzed to evaluate for evidence of decline in routine cancer screening. In 2019 and 2020, 4737 and 2405 low dose CT's, 435 and 382 mammograms, and 2985 and 1346 colonoscopies were completed. These numbers translate to a reduction in low dose CT's by 49%, mammograms by 12% and colonoscopies by 55% (Table 1 , Fig. 1 ). With regards to new diagnoses of malignancies in 2019, there were 4, 19, and 131 new cases of breast, colon, and lung cancer respectively between two primary care clinic sites in comparison to 3,9, and 80 recorded in 2020, 25%, 53%, and 39% less than the year prior (Table 2 , Fig. 2 ).
Table 1.
Cancer screenings 2019 and 2020
| Screening Test | 2019 | 2020 | Decrease |
|---|---|---|---|
| Low Dose CT | 4737 | 2405 | 49% |
| Mammography | 435 | 382 | 12% |
| Colonoscopy | 2985 | 1346 | 55% |
Number of low dose CT, mammography, and colonoscopy screenings in 2019 and 2020, and the percentage decrease in screenings between the two years.
Fig. 1.
Cancer Screenings 2019 and 2020.
Number of cancer screenings (low dose CT, mammography, colonoscopy) in 2019 and 2020.
Table 2.
New diagnoses cancer 2019 and 2020.
| New Cancer Diagnosis | 2019 | 2020 | Decrease |
|---|---|---|---|
| Lung | 131 | 80 | 39% |
| Breast | 4 | 3 | 25% |
| Colon | 19 | 9 | 53% |
Number of new diagnosis of lung, breast, and colon cancer in 2019 and 2020, and percentage decrease of new diagnoses between the two years.
Fig. 2.
New Cancer Diagnosis 2019 vs 2020.
Number of new lung, breast, and colon cancer diagnosis in 2019 and 2020.
Discussion
In evaluating the number of completed cancer screening tests and new diagnoses of malignancy in 2019 versus 2020, we can surmise that this decline was due to the covid-19 pandemic. This phenomenon we have observed at these VA clinic sites is not unlike what is being observed across the nation. This trend has been seen in studies evaluating delays in New England, with a reported significant decline in cancer screenings including pap smears, mammography, prostate specific antigen, colonoscopy, and low dose CT scans during the first peak of the pandemic from March to June 2020.1 A larger scale study evaluating the Medicare fee for service population between March and July of 2020 also reported a substantial decrease in cancer screenings, visits, therapy, surgeries, with decline in breast, colon, prostate, and lung cancer screenings by 85%, 75%, 74%, and 56%, respectively.3 Similarly, findings released in May 2020 by the Epic Health Research Network showed a drop between 86% to 94% in preventive cancer screenings performed nationwide to date in 2020 compared with equivalent weeks from 2017 to 2019.4 Due to stay-at-home orders and clinic closures during the Spring of 2020, these observations were not unexpected, however, they may be potentially more consequential to the veteran population.
Military personnel are a particularly high-risk population to development of malignancy due to exposures incurred during their time in service. While the implications of various deployment-related exposures continue to be elucidated, many have already been identified as carcinogenic including agent orange, asbestos, benzene, and chromium exposure. While rates of the most common cancers in males in the VA system are identified to be similar to those of the general population based on comparison of national cancer registries, prostate and breast cancer are reportedly higher in the VA population.5 Additionally, by virtue of the eligibility criteria to receive care at the Veteran Affairs, including financial and service-related disability, this is a more vulnerable population due to healthcare disparities. This demographic of patients is more likely to be of a minority race, have poorer health status, lower level of income as well as education, and cancer screening is already reportedly lower in this group than the general population.2
Cancer screening has resulted in significant decline in death rates from cancer over the last several years, with a steady observed decline in cancer-related mortality since 1991.2 Delay of screening by even 12 months could possibly translate to significant progression of disease. The implications of these declines in cancer screening can be consequential; cancers will be diagnosed later, possibly at a more advanced stage, which will ultimately translate to poorer outcomes and lower survival.
Next steps
Though screening rates are lower in the VA population, according to a comprehensive review of the VA Cancer Registry, patients in the VA were found to be diagnosed with commonly occurring cancers at earlier stages than observed in the general population.2 This observation can be attributed to the number of efforts implemented by facilities to improve cancer screening compliance. Most notably, in 2005, The Colorectal Care Collaborative was conducted in an effort to improve timeliness in follow up colonoscopies after positive FIT testing by identifying and addressing gaps in care. This model has been similarly adapted at facilities such as the ones evaluated in this study with positive outcomes on reduction of overdue colon cancer screenings. Additionally, VA providers are educated on identified malignancy-associated exposures and incorporate deployment-specific screenings to ensure appropriate management of high-risk individuals. Quality improvement initiatives such as these will be important in the months to follow to ensure that this vulnerable population is not adversely effected by the inevitable healthcare access delays brought on by the covid-19 pandemic.
Limitations
There were several limitations identified with this quality assessment. The Veteran Affairs population is predominantly male, leaving a small sample size that may not accurately reflect the changes that occurred with female-specific cancer screenings.
The number of low dose lung CT's assessed did not distinguish between those performed as lung node follow up versus those that were done for screening purposes. We acknowledge that this may skew the true decline in screenings, however delays in lung nodule follow up bare the similar if not more significant consequence as delayed surveillance imaging on cancer-related mortality. Similarly, a distinction between screening and surveillance colonoscopies was not made in the reported data. Colonoscopy screening intervals are patient-specific and in assessing only two years, this assessment may have overestimated decline in screen not accounting for patients who may have tested out of screening by age, sought alternate screening modalities (fecal immunochemical test (FIT) testing, sigmoidoscopy, etc).
Patients who receive care at the VA often receive additional care outside the community. This assessment did not account for patients who may have sought cancer screening outside of the VA healthcare system.
Conclusion
The covid pandemic reduced access for patients to routine healthcare, leading to a disruption in healthcare delivery and a notable impact on cancer screenings. Despite adaptations healthcare facilities have made, barriers to access to care will likely remain a problem for the foreseeable future due to covid-related demands on providers and clinical staff. This phenomenon can be particularly detrimental to high-risk populations such as patients receiving care at Veteran Affairs Facilities. In the months to follow, providers will need to be diligent in ensuring these delays in healthcare delivery are addressed and are not consequential to patient care.
Footnotes
Financial disclosures: None.
Support: None reported.
Ethics approval: This report received QI determination and IRB exemption by the VACHS Research Office.
References
- 1.Bakouny Z, Paciotti M, Schmidt AL, Lipsitz SR, Choueiri TK, Trinh Q. Cancer screening tests and cancer diagnoses during the COVID-19 pandemic. JAMA Oncol. January 14, 2021 doi: 10.1001/jamaoncol.2020.7600. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zullig LL, Jackson GL, Dorn RA, et al. Cancer incidence among patients of the U.S. veterans affairs health care system. Mil Med. 2012;177(6):693–701. doi: 10.7205/milmed-d-11-00434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DOI:10.1200/CCI.20.00134 JCO Clinical Cancer Informatics no. 4 (2020) 1059–1071. Published online November 30, 2020.
- 4.Epic Health Research Network. Preventive cancer screenings during COVID-19 pandemic. Published 2020. Accessed July 1, 2020. https://ehrn.org/wp-content/uploads/Preventive-Cancer-Screenings-during-COVID-19-Pandemic.pdf
- 5.U.S. Department of Veterans Affairs [Internet] Washington, D.C: VA Health Care Eligibility & Enrollment Ratings and Evaluations; Service Connection 3.303-1 [updated 2009 Sept 15; cited 2011 Nov 12].