Highlights
-
•
Prolonged post-ictal Atrial fibrillation is a rare phenomenon.
-
•
Fluttering in the chest after seizures may be post-ictal cardiac arrhythmias.
-
•
Post-ictal Atrial fibrillation is captured on Video EEG in our case.
Keywords: Atrial fibrillation, Cardiac arrhythmias, Post-ictal atrial fibrillation, Seizures, SUDEP
Abstract
It is well known that several types of cardiac arrhythmias can occur after a seizure, with ictal sinus tachycardia being the most common. However, post-ictal atrial fibrillation (PIAF) is a rare phenomenon with significant clinical implications.
We describe the case of an epilepsy patient with prolonged PIAF. Our case is that of a 62-year-old female with seizure onset at 51 years of age. She had a left hemispheric meningioma that was resected with ongoing seizures. She described frequent episodes of chest fluttering lasting for several hours post-ictally. During video-EEG monitoring (VEEG), she had a typical seizure with staring and word finding difficulty. This was associated with the occurrence of atrial fibrillation with rapid ventricular rate that lasted 18 hours.
We discuss the relation between seizures and prolonged PIAF as it relates to the need for anticoagulation, use of appropriate antiseizure medications, and the possible association with SUDEP.
1. Introduction
The association between seizures and cardiac arrhythmias is well established. There are various kinds of cardiac arrhythmias that can occur after a seizure, the most common being sinus tachycardia. Though ictal sinus tachycardia is relatively benign, other cardiac arrhythmias can be potentially dangerous leading to significant morbidity and even death [1]. Several studies have suggested that peri-ictal cardiac arrhythmias may be implicated in the cause of sudden unexpected death in epilepsy (SUDEP). Post -ictal atrial fibrillation (PIAF) is potentially connected to SUDEP due to post-ictal generalized EEG suppression (PGES) and autonomic dysregulation [2].
Here we present a unique case with occurrence of prolonged PIAF documented on video-EEG monitoring (VEEG) and discuss its implications.
2. Case report
The case is a 62-year-old right-handed, overweight female patient referred for evaluation of seizures with onset at 51 years old. Her seizures consisted of a non-descript aura followed by staring with the inability to understand spoken language. Hence, it is likely a focal aware seizure followed by a focal impaired awareness seizure with aphasia. The patient also describes the sensation of hearing people speak in a foreign language. Occasionally, the patient would experience loss of consciousness with or without convulsions. The patient would also frequently describe a sensation of fluttering in her chest following a seizure and this sensation would last for several hours.
During her initial evaluation, she was diagnosed to have a meningioma of the left middle cranial fossa that was resected. Despite the resection, she continued to experience focal seizures. Preoperative MRI of brain with and without contrast in an outside facility showed a large extra-axial mass involving left middle cranial fossa with significant edema representing a meningioma with increased vascularity. She was initially prescribed levetiracetam, which was later discontinued due to increased agitation. Later, topiramate was prescribed to the patient and she was taking 150 mg twice daily at the time of evaluation.
When initially seen at our practice, the patient was experiencing about 3 to 5 seizures per month. A routine electroencephalogram (EEG) showed a left temporal breach rhythm, but was otherwise unremarkable. She was admitted for VEEG monitoring and topiramate was discontinued in order to capture her seizures. In the 72-hour recording of video EEG in the epilepsy-monitoring unit (EMU) the patient experienced one of her typical episodes, characterized by staring, lip smacking and word finding difficulty. Therefore, the seizure type was defined as a focal impaired awareness seizure with aphasia. VEEG demonstrated high voltage left temporal rhythmic theta activity lasting for more than 1 minute. About 12 seconds into the electrographic seizure, the patient developed atrial fibrillation with a rapid ventricular response of 150 beats per minute (bpm) (Fig. 1). The atrial fibrillation persisted after the end of the seizure (Fig. 2). She was given intravenous (IV) metoprolol 5 mg with improvement of her heart rate to 130 bpm followed by a second dose. The patient also received diltiazem 10 mg IV. A transthoracic echocardiogram did not demonstrate any structural heart disease. The cardiology service recommended a rhythm control strategy with flecainide, which she declined due to concerns for potential side effects. She was placed on metoprolol XL 25 mg and aspirin 81 mg daily. Anticoagulation therapy was not recommended due to low comorbid risk factors with a CHA2DS2 –VASc score of 1. After 18 hours, the patient converted to normal sinus rhythm (Fig. 3). The patient’s antiseizure medication, topiramate 150 mg twice daily was resumed for the seizure control and titrated up as outpatient.
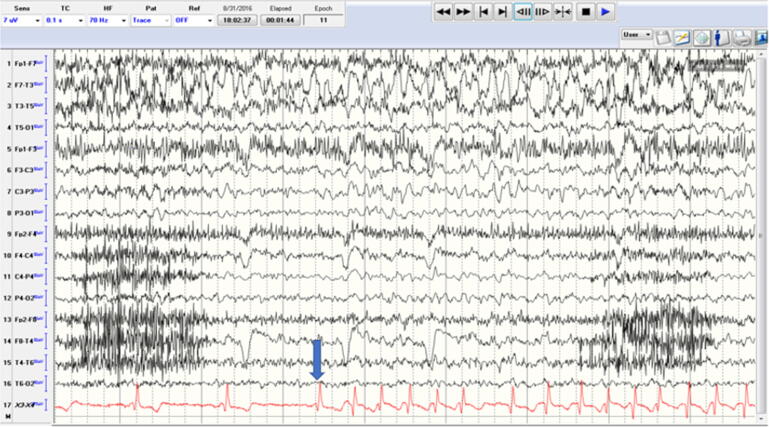
Fig. 1.
Left temporal electrographic seizure with EKG showing transition from normal sinus rhythm to atrial fibrillation indicated by an arrow.
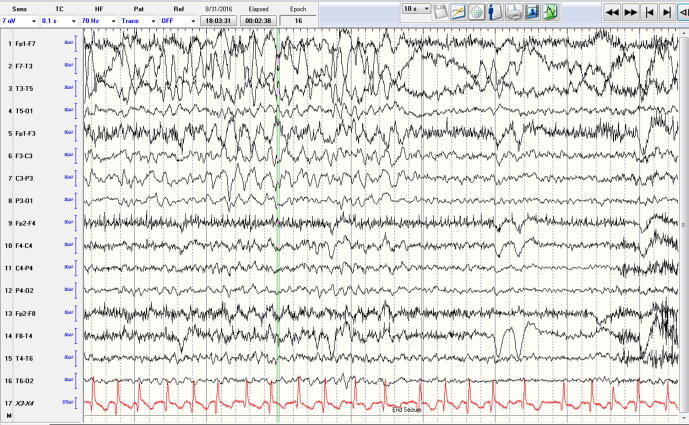
Fig. 2.
End of seizure with persistent atrial fibrillation.
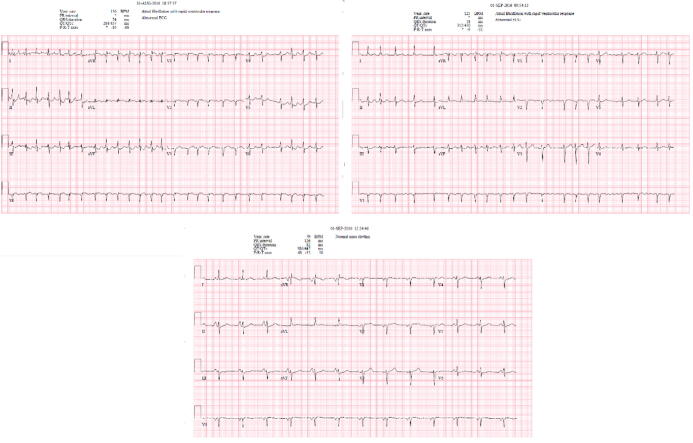
Fig. 3.
EKG in chronological order: the top 2 EKGs showing Atrial fibrillation followed by normal sinus rhythm in the 3rd EKG.
Prior to VEEG monitoring, the patient reported frequent chest palpitations lasting several hours following seizures indicating possible pre-existing episodes of PIAF. The patient denied having any interictal palpitations. The nature of these palpitations was undiagnosed prior to VEEG. She also denied having history of hypertension, thyroid dysfunction, illicit drug use or a family history of cardiovascular disease. However, a baseline EKG prior to video-EEG monitoring was not available.
3. Discussion
There is a well-known association between seizures and the occurrence of peri-ictal and post-ictal cardiac arrhythmias. It is hypothesized that this may be due to autonomic dysregulation following seizures, which is characterized by sympathetic overactivity and parasympathetic suppression [2]. Early tachycardia in right temporal seizures can be explained by sympathetic cardiovascular regulation activated by seizures. Hemispheric lateralization of autonomic cardiovascular control has been demonstrated by animal studies. These studies indicated that the right posterior insular cortex was critical to heart rate increase. Heart rate increase is inevitable in right mesial temporal lobe epilepsy but not in left. It is unclear if the same mechanism applies to atrial fibrillation. Studies indicated that the right posterior insular cortex and the dorso medial hypothalamic nucleus were critical to heart rate increase [3]. Sodium-channel blockers such as lacosamide may alter the threshold to develop cardiac arrhythmias by increasing the PR interval.
The most commonly seen peri-ictal cardiac arrhythmia is sinus tachycardia. This accounts for about 90% of cardiac abnormalities, with other arrhythmias such as bradycardia being less common [4]. The more commonly seen life threatening arrhythmias following seizures include ventricular fibrillation and asystole.
Post-ictal atrial fibrillation is among the less-frequently encountered cardiac arrhythmias. There is one case of PIAF being associated with marijuana use [5]. PIAF typically lasts for a few minutes [6]. The longest recorded PIAF reported in literature is 25 hours. However, the onset of that episode was not captured and not definitively time-locked to ictal EEG data [7]. There are 21 documented cases of PIAF in the literature, 19 being associated with generalized tonic clonic seizures and 2 with focal seizures [8].
Our patient had a focal seizure leading to PIAF that lasted 18 hours. To our knowledge, our case is the third in the literature of PIAF after focal impaired awareness seizure without evolving to a bilateral tonic-clonic seizure. The two prior cases of PIAF after focal seizures were also of left temporal onset. This case is unique however, as we were able to capture on video and EEG, the moment of conversion from normal sinus rhythm to PIAF and demonstrate conclusively that episodes of PIAF can last for a protracted period. In addition, our patient experienced frequent and prolonged palpitations following seizures prior to VEEG, indicating that there likely were pre-existing episodes of PIAF that were undiagnosed. She denied any palpitation in the absence of seizures. A 48-hour holter monitoring was done which did not reveal any cardiac arrhythmias. However, a prolonged holter monitoring to capture an event was not performed and may be a limitation of this case.
Atrial fibrillation is known to be a significant risk factor for stroke. Given the transient nature of most cases of PIAF, anticoagulation is rarely prescribed. However, our case indicates that PIAF can be prolonged and recurrent, and presents a dilemma as to whether anticoagulation is required. Anticoagulation must be considered weighing against the potential risk of head injury in patients with epilepsy [9].
In our case, the decision was made not to anticoagulate as the patient had a CHA2DS2-VASc score of one. However, our patient was advised to undergo long-term cardiac monitoring and close follow up with a cardiologist as well.
Cardiac arrhythmias are also of major clinical significance in the setting of seizures due to its potential association with SUDEP. This is because the majority of seizure-associated cardiac arrhythmias occur after generalized tonic-clonic seizures, likely during PGES [8]. It has been established that the likelihood of SUDEP increases with prolonged PGES [10]. Patients with drug-resistant epilepsy and genetic abnormalities such as sodium and potassium channelopathies are particularly susceptible to SUDEP [2]. Our case illustrates the importance of inquiring about history of palpitations following seizures and the regular use of cardiac telemetry during VEEG as a potential means of detecting arrhythmias and potentially intervening to decrease the occurrence of SUDEP.
4. Conclusion
Peri-ictal and post ictal atrial fibrillation (PIAF) is a rare cardiac arrhythmia in patients with seizures. As this case illustrates, PIAF can persist for many hours and in certain cases, may remain undiagnosed for years. We propose that patients with epilepsy be routinely queried on whether they experience palpitations accompanying their seizures and that those undergoing VEEG monitoring also have cardiac telemetry monitoring to improve the diagnosis of PIAF. Doing so may increase the likelihood of diagnosing PIAF, leading to appropriate therapy and possibly decreasing the occurrence of SUDEP.
Ethical statement
As referenced by Epilepsy and Behavior Case Reports, all authors report that they have conformed to the principles of ethics in publishing and ethical guidelines for journal publication.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Barot N, Nei M. Autonomic aspects of sudden unexpected death in epilepsy (SUDEP). Clin Auton Res 2019 Apr; 29(2):151-160. doi: 10.1007/s10286-018-0576-1. Epub 2018 Nov 19. Review. PubMed PMID: 30456432. [DOI] [PubMed]
- 2.Sanchez-Larsen A., Aznar-Lain G., Benito B., Principe A., Ley M., Tauste Campo A. Post-ictal atrial fibrillation detected during video-EEG monitoring: Case report, proposed physiopathologic mechanism and therapeutic considerations. Epilepsy Behav Case Rep. 2017;8:40–43. doi: 10.1016/j.ebcr.2017.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kazuhiro Kato, Kazutaka Jin, Hisashi Itabashi, Masaki Iwasaki, Yosuke Kakisaka, Masashi Aoki, Nobukazu Nakasato. Earlier tachycardia onset in right than left mesial temporal lobe seizures. PMID: 25194011. doi 10.1212/WNL.0000000000000864. [DOI] [PubMed]
- 4.Herskovitz M., Schiller Y. Atrial fibrillation associated with epileptic seizures. Arch Neurol. 2012;69(9):1197–1199. doi: 10.1001/archneurol.2011.3647. PubMed PMID: 22637287. [DOI] [PubMed] [Google Scholar]
- 5.Singh D., Huntwork M., Shetty V., Sequeira G., Akingbola O. Prolonged atrial fibrillation precipitated by new-onset seizures and marijuana abuse. Pediatrics. 2014 Feb;133(2):e443–e446. doi: 10.1542/peds.2013-1831. Epub 2014 Jan 13 PubMed PMID: 24420812. [DOI] [PubMed] [Google Scholar]
- 6.Vedovello M., Baldacci F., Nuti A., Cipriani G., Ulivi M., Vergallo A. Peri-ictal prolonged atrial fibrillation after generalized seizures: description of a case and etiopathological considerations. Epilepsy Behav. 2012;23(3):377–378. doi: 10.1016/j.yebeh.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 7.Surges R, Moskau S, Viebahn B, Schoene-Bake JC, Schwab JO, Elger CE. Prolonged atrial fibrillation following generalized tonic-clonic seizures. Seizure. 2012 Oct; 21(8):643-5. doi: 10.1016/j.seizure.2012.05.012. Epub 2012 Jun 12. PubMed PMID: 22698381; PubMed Central PMCID: PMC4104675. [DOI] [PMC free article] [PubMed]
- 8.Basili L.M., Morano A., Fattouch J., Fanella M., Albini M., Avorio F. Ictal atrial fibrillation during focal seizures: a case report and literature review. Epileptic Disord. 2019;21(3):295–301. doi: 10.1684/epd.2019.1070. Review. PubMed PMID: 31225804. [DOI] [PubMed] [Google Scholar]
- 9.Singh Dangol GM, Hoffman DA. Post-Ictal Transient Atrial Fibrillation as a Rare Manifestation of Grand Mal Seizure. J Atr Fibrillation. 2017 Aug-Sep; 10(2):1643. doi: 10.4022/jafib.1643. eCollection 2017 Aug-Sep. PubMed PMID: 29250236; PubMed Central PMCID: PMC5673295. [DOI] [PMC free article] [PubMed]
- 10.Lhatoo S.D., Faulkner H.J., Dembny K., Trippick K., Johnson C., Bird J.M. An electroclinical case-control study of sudden unexpected death in epilepsy. Ann Neurol. 2010;68(6):787–796. doi: 10.1002/ana.22101. PubMed PMID: 20882604. [DOI] [PubMed] [Google Scholar]