Abstract
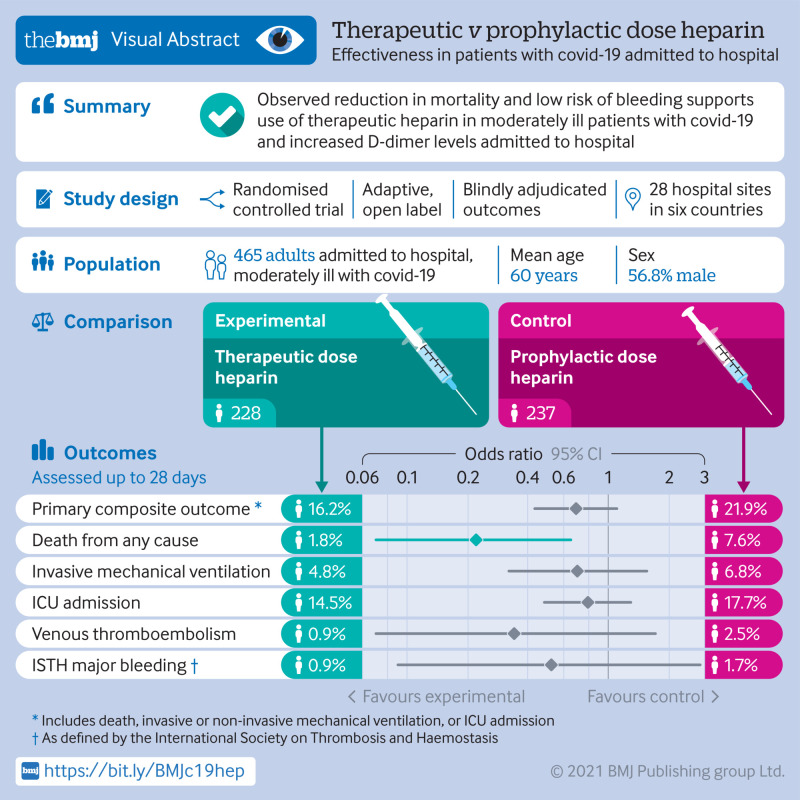
Objective
To evaluate the effects of therapeutic heparin compared with prophylactic heparin among moderately ill patients with covid-19 admitted to hospital wards.
Design
Randomised controlled, adaptive, open label clinical trial.
Setting
28 hospitals in Brazil, Canada, Ireland, Saudi Arabia, United Arab Emirates, and US.
Participants
465 adults admitted to hospital wards with covid-19 and increased D-dimer levels were recruited between 29 May 2020 and 12 April 2021 and were randomly assigned to therapeutic dose heparin (n=228) or prophylactic dose heparin (n=237).
Interventions
Therapeutic dose or prophylactic dose heparin (low molecular weight or unfractionated heparin), to be continued until hospital discharge, day 28, or death.
Main outcome measures
The primary outcome was a composite of death, invasive mechanical ventilation, non-invasive mechanical ventilation, or admission to an intensive care unit, assessed up to 28 days. The secondary outcomes included all cause death, the composite of all cause death or any mechanical ventilation, and venous thromboembolism. Safety outcomes included major bleeding. Outcomes were blindly adjudicated.
Results
The mean age of participants was 60 years; 264 (56.8%) were men and the mean body mass index was 30.3 kg/m2. At 28 days, the primary composite outcome had occurred in 37/228 patients (16.2%) assigned to therapeutic heparin and 52/237 (21.9%) assigned to prophylactic heparin (odds ratio 0.69, 95% confidence interval 0.43 to 1.10; P=0.12). Deaths occurred in four patients (1.8%) assigned to therapeutic heparin and 18 patients (7.6%) assigned to prophylactic heparin (0.22, 0.07 to 0.65; P=0.006). The composite of all cause death or any mechanical ventilation occurred in 23 patients (10.1%) assigned to therapeutic heparin and 38 (16.0%) assigned to prophylactic heparin (0.59, 0.34 to 1.02; P=0.06). Venous thromboembolism occurred in two patients (0.9%) assigned to therapeutic heparin and six (2.5%) assigned to prophylactic heparin (0.34, 0.07 to 1.71; P=0.19). Major bleeding occurred in two patients (0.9%) assigned to therapeutic heparin and four (1.7%) assigned to prophylactic heparin (0.52, 0.09 to 2.85; P=0.69).
Conclusions
In moderately ill patients with covid-19 and increased D-dimer levels admitted to hospital wards, therapeutic heparin was not significantly associated with a reduction in the primary outcome but the odds of death at 28 days was decreased. The risk of major bleeding appeared low in this trial.
Trial registration
ClinicalTrials.gov NCT04362085.
Introduction
The most common cause of clinical deterioration of patients admitted to hospital with covid-19 is hypoxaemic respiratory failure.1 Pulmonary endothelial injury and microvascular thrombosis probably contribute to respiratory compromise,2 3 4 5 6 which in turn might be caused by a thrombo-inflammatory state, also referred to as covid-19 coagulopathy.2 3 7 8 9 Increased D-dimer levels in the blood, as a marker of coagulopathy, and hypoxaemia are associated with poor prognosis.2 3 7 8 9 10
Heparin, in addition to its anticoagulant properties, has anti-inflammatory and potential antiviral effects and might improve endothelial function.2 11 12 13 14 15 Early initiation of therapeutic heparin could therefore decrease the thrombo-inflammatory process and reduce the risk of critical illness or death.2 4 16 17 18 Randomised trials indicated that anticoagulation using therapeutic heparin might be beneficial in moderately,19 but not critically20 ill patients with covid-19, suggesting that the time of initiation of therapeutic heparin is important. The Therapeutic Anticoagulation versus Standard Care as a Rapid Response to the COVID-19 Pandemic (RAPID) trial was designed to determine if therapeutic heparin is superior to prophylactic heparin in moderately ill patients with covid-19 and increased D-dimer levels admitted to hospital wards in decreasing the composite of admission to an intensive care unit (ICU), mechanical ventilation, or death.
Methods
Trial oversight
The RAPID trial was an investigator initiated randomised controlled trial. For administrative reasons, the protocol in Brazil was registered separately, but prospectively harmonised (see supplementary file). An independent data and safety monitoring board oversaw the trial (see supplementary file).
Design
The RAPID trial was an investigator initiated, parallel, pragmatic, adaptive multicentre, open label randomised controlled trial conducted at 28 hospitals in six countries. Its design has been described previously and the study protocol and statistical analysis plan are provided in the supplementary file.21 The trial evaluates the effects of therapeutic heparin compared with prophylactic heparin in moderately ill patients with covid-19 admitted to hospital.
Trial population
Patients were eligible if they were moderately ill and admitted to hospital wards for covid-19 with laboratory confirmed SARS-CoV-2 infection and had increased D-dimer levels within the first five days of admission. Moderate illness was defined as admission to hospital ward level of care (ie, not to ICU), not already mechanically ventilated, and not imminently requiring mechanical ventilation or critical care. D-dimer levels were required to be above the upper limit of normal of the local hospital in the presence of an oxygen saturation ≤93% on room air, or ≥2 times the upper limit of normal irrespective of oxygen saturation. Participants were excluded if they had substantial bleeding risks, an absolute indication for or any contraindication to heparin anticoagulation based on care team judgment, were pregnant, or if they had already experienced, or would imminently experience any component of the primary outcome (all cause death, non-invasive or invasive mechanical ventilation, or ICU admission). Full eligibility criteria are provided in the supplementary file. Written informed consent was obtained from all participants or their legal representatives.
Randomisation and study drugs
We used web based central randomisation with a computer generated random sequence of variable block sizes stratified by site and age (≤65 v >65 years) to assign patients in a 1:1 ratio to therapeutic heparin or prophylactic heparin. Throughout the paper heparin refers to either low molecular weight heparin or unfractionated heparin—both forms of heparin are within the same drug class and exert their anticoagulant effect by amplifying the activity of the coagulation inhibitor antithrombin. They both also have similar non-anticoagulant effects.22 Patients allocated to therapeutic heparin received therapeutic doses of low molecular weight heparin or unfractionated heparin as used for the treatment of venous thromboembolism.23 Unfractionated heparin was administered using a weight based nomogram (bolus plus continuous infusion) with activated partial thromboplastin time or unfractionated heparin anti-Xa titration according to the centre specific protocols (that is, high dose nomogram). Patients allocated to prophylactic heparin received dose capped prophylactic subcutaneous heparin (low molecular weight heparin or unfractionated heparin) adjusted for body mass index and creatinine clearance (see supplementary file for dosing). Prophylactic doses of heparin were thus restricted to evidence based protocols for the prevention of venous thromboembolism for medical patients admitted to hospital.24 Study treatment was started within 24 hours after randomisation and continued until the first of hospital discharge, day 28, study withdrawal, or death (supplementary fig S1). If a participant was admitted to ICU, continuation of the allocated treatment was recommended.
Study outcomes
The primary outcome was a composite of ICU admission, non-invasive (bilevel or continuous positive airway pressure) or invasive mechanical ventilation, or death up to 28 days. Secondary outcomes included all cause death; the composite of any mechanical ventilation or all cause death; ICU admission or all cause death; ventilator-free days alive; organ support-free days alive; ICU-free days alive; hospital-free days alive; renal replacement therapy; venous thromboembolism; arterial thromboembolism; and D-dimer level from blood samples taken at two days ±24 hours post-randomisation (see the supplementary file for detailed definitions). The following components of the primary composite were not included in the protocol but were prespecified as secondary outcomes in the statistical analysis plan: invasive mechanical ventilation; composite of invasive or non-invasive mechanical ventilation; and ICU admission. Prespecified safety outcomes included major bleeding as defined by the International Society on Thrombosis and Haemostasis,25 red blood cell transfusion (≥1 unit), transfusion of haemostatic blood components or products, and heparin induced thrombocytopenia. If a patient reached any defined clinical endpoint (that is, component of primary outcome or secondary outcome), other than events that required a change to clinical care, such as thromboembolism or bleeding, the protocol suggested ongoing treatment per allocated arm but left ultimate decisions about heparin anticoagulation to the discretion of the treating doctors. An independent event adjudication committee, which was unaware of treatment assignments, adjudicated the components of the primary outcome, bleeding, thrombotic events, and cause of death. The event adjudication was not prespecified in the protocol.
Statistical analysis
We estimated that 231 patients in each group would provide 90% power to detect a 15% absolute risk difference, from 50% in the control group to 35% in the experimental group, at a two sided α level of 0.048 accounting for two planned interim analyses at 25% and 75% of the originally planned sample size.2 16 21 At 75%, we performed a conditional power analysis. The protocol prespecified that the sample size would be increased if the conditional power was between 60% and 80%.21 As the conditional power was below 60%, the data safety and monitoring board recommended not to increase the sample size and complete recruitment as originally planned.
The primary analysis of the primary composite outcome was based on the intention-to-treat principle using logistic regression; a χ2 test of independence was conducted to obtain a two sided P value.26 Participants who did not have a 28 day assessment but were discharged from hospital alive before day 28, were assumed to be event-free up to day 28. Prespecified subgroup analyses of the primary outcome accompanied by tests of interaction were done for age, sex, body mass index, time from onset of covid-19 symptoms, diabetes mellitus, coronary artery disease, hypertension, race or ethnicity, D-dimer level, use of systemic corticosteroids, and geographical region. Post hoc subgroup analyses were repeated for all cause death. Prespecified sensitivity analyses of the primary outcome excluded participants who did not have a 28 day assessment and included only participants from the per protocol cohort. The per protocol cohort included all eligible participants who received their intervention as randomly allocated during the first 48 hours after randomisation, and excluded participants who did not satisfy all eligibility criteria, did not receive their allocated treatment, or did not have follow-up until day 28, death, or occurrence of a primary composite outcome component. Since randomisation was stratified by age, an additional logistic regression model was fit to analyse the primary outcome controlling for age.
Binary secondary outcomes were analysed using logistic regression. Ventilator-free days, organ support-free days, ICU-free days, and hospital-free days alive were analysed using ordinal logistic regression; death up to 28 days was assigned the worst outcome (a value of −1) in these analyses.27 We compared the post-treatment D-dimer level using linear regression adjusted for baseline. Since D-dimer assays differed across sites, D-dimer levels were expressed as multiples of the local laboratory assay upper limit of normal (D-dimer×upper limit of normal)—that is, the ratio of D-dimer values divided by the local upper limit of normal, and analysed as natural logarithm of this ratio: log(D-dimer/upper limit of normal). Analyses of secondary outcomes were considered exploratory so were not adjusted for multiple comparisons; the widths of 95% confidence intervals for secondary outcomes should not be used for inferences about treatment effects. The supplementary file provides an extended description of the statistical methods.
Patient and public involvement
Funding limitations and covid-19 restrictions interfered with our ability to involve patient partners in setting the research question and in developing plans for recruitment, design, and implementation of the results of this study.
Results
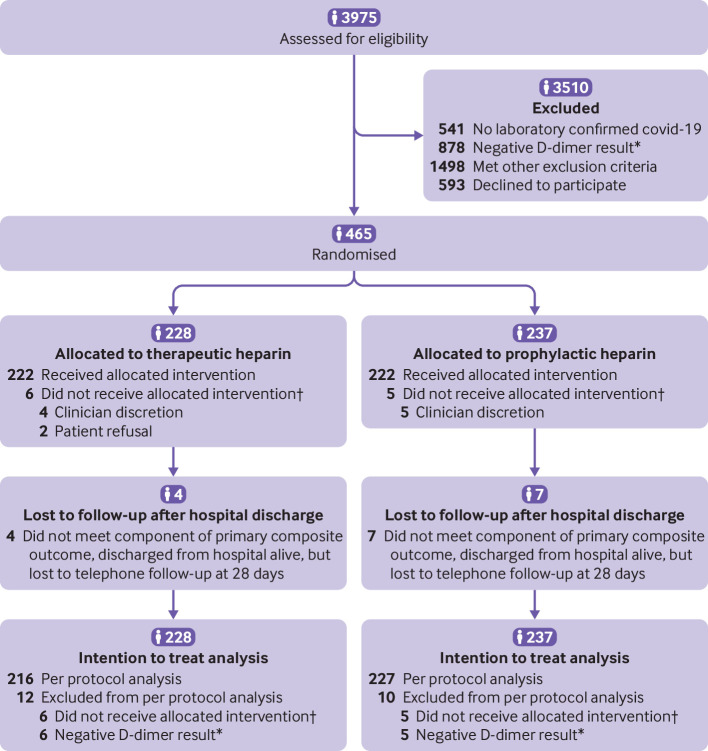
From 29 May 2020 to 12 April 2021, a total of 3975 patients were screened and 465 included in the study: 228 were randomly assigned to therapeutic heparin and 237 to prophylactic heparin. Overall, 224 (98.2%) in the therapeutic heparin group and 234 (98.7%) in the prophylactic heparin group received treatment as allocated within 24 hours after randomisation, and 222 (97.4%) and 232 (97.9%), respectively, continued to receive treatment as allocated up to 48 hours after randomisation (fig 1). The final follow-up date for the 28 day primary outcome was 10 May 2021.
Fig 1.
Screening, enrolment, randomisation, and inclusion in analysis. *Six patients in the therapeutic heparin group and five in the prophylactic heparin group had negative D-dimer values at the time of randomisation due to a delay in protocol harmonisation with Brazil. †Did not receive allocated intervention within the first 48 hours post-randomisation without clear clinical indication
The mean age of participants was 60 years; 264 (56.8%) were men and the mean body mass index was 30.3. Baseline D-dimer level was 2.3-fold above the upper limit of normal, and mean creatinine was 85.2 µmol/L. At baseline, six patients in the therapeutic heparin group and five in the prophylactic heparin group had D-dimer levels below the upper limit of normal. Baseline personal and clinical characteristics were similar between treatment arms (table 1, and supplementary tables S1-2). The mean duration from symptom onset to hospital admission was 7.1 days, and the mean duration from hospital admission to randomisation was 1.4 days. The mean treatment duration was 6.5 in the therapeutic heparin group and 6.3 days in the prophylactic heparin group (supplementary table S3). One patient in the therapeutic heparin group was admitted to hospital for more than 28 days post-randomisation compared with none in the prophylactic heparin group. Low molecular weight heparin was prescribed in 224 (98.2%) patients assigned to therapeutic heparin and 222 (93.7%) assigned to prophylactic heparin. Concomitant treatments (systemic corticosteroids, remdesivir, and tocilizumab) were balanced between treatment arms for pre-randomisation and post-randomisation periods combined (supplementary table S4).
Table 1.
Baseline characteristics of moderately ill patients with covid-19 admitted to hospital wards, according to treatment assignment. Values are numbers (percentages) unless stated otherwise
| Characteristics | Therapeutic heparin (n=228) | Prophylactic heparin (n=237) |
|---|---|---|
| Mean (SD) age (years) | 60.4 (14.1) | 59.6 (15.5) |
| Women | 105 (46.1) | 96 (40.5) |
| Men | 123 (53.9) | 141 (59.5) |
| Race or ethnicity*: | ||
| White | ||
| European | 97 (43.7) | 96 (40.9) |
| Middle Eastern, North African | 65 (29.3) | 67 (28.5) |
| Asian | 27 (12.2) | 38 (16.2) |
| Black or African American | 18 (8.1) | 23 (9.8) |
| Hispanic or Latino | 14 (6.3) | 10 (4.3) |
| American Indian, Alaska Native, First Nations, Indigenous/Aboriginal, Metis | 0 (0.0) | 1 (0.4) |
| Native Hawaiian or Other Pacific Islander | 1 (0.5) | 0 (0.0) |
| Mean (SD) body mass index† | 30.3 (6.4) | 30.2 (7.0) |
| Mean (SD) duration of symptoms before hospital admission (days)‡ | 7.1 (5.1) | 7.1 (5.2) |
| Mean (SD) duration of hospital admission before randomisation (days) | 1.5 (1.1) | 1.4 (1.0) |
| Hypoxaemia at baseline§ | 190 (90.9) | 203 (93.1) |
| High flow nasal cannula oxygen use | 14 (6.2) | 13 (5.5) |
| Pre-existing conditions: | ||
| Hypertension | 108 (47.4) | 117 (49.4) |
| Diabetes mellitus | 83 (36.4) | 77 (32.5) |
| Coronary artery disease | 16 (7.0) | 18 (7.6) |
| Heart failure | 9 (3.9) | 6 (2.5) |
| Atrial fibrillation | 0 (0.0) | 2 (0.8) |
| Cerebrovascular disease | 10 (4.4) | 9 (3.8) |
| Peripheral vascular disease | 0 (0.0) | 1 (0.4) |
| History of venous thromboembolism | 3 (1.3) | 2 (0.8) |
| Chronic pulmonary disease¶ | 36 (15.8) | 27 (11.4) |
| Chronic kidney disease | 20 (8.8) | 13 (5.5) |
| Chronic liver disease | 5 (2.2) | 9 (3.8) |
| Cancer | 13 (5.7) | 19 (8.0) |
| Immunodeficiency | 1 (0.4) | 2 (0.8) |
| Autoimmune disease | 6 (2.6) | 11 (4.6) |
| Cognitive impairment | 12 (5.3) | 11 (4.6) |
| Mental illness | 18 (7.9) | 13 (5.5) |
| Active smoking | 5 (2.2) | 7 (3.0) |
| Drug history**: | ||
| Systemic corticosteroids | 161 (70.6) | 162 (68.4) |
| Antiplatelet agent | 24 (10.5) | 29 (12.2) |
| Previous covid-19 vaccine | 1 (0.4) | 2 (0.8) |
| Laboratory values: | ||
| D-dimer | ||
| D-dimer positivity†† | 222 (97.4) | 232 (97.9) |
| Geometric mean (SD) D-dimer ratio (D-dimer×ULN)‡‡ | 2.1 (0.7) | 2.5 (0.9) |
| D-dimer distribution: | ||
| <2×ULN | 115 (50.4) | 112 (47.3) |
| ≥2-3×ULN | 61 (26.8) | 55 (23.2) |
| ≥3-4×ULN | 25 (11.0) | 27 (11.4) |
| ≥4×ULN | 27 (11.8) | 43 (18.1) |
| Mean (SD) platelet count (109/L)§§ | 233.7 (95.7) | 237.8 (95.3) |
| Mean (SD) creatinine (μmol/L)¶¶ | 84.6 (44.1) | 85.9 (58.2) |
| Country: | ||
| Brazil | 54 (23.7) | 51 (21.5) |
| Canada | 72 (31.6) | 78 (32.9) |
| Ireland | 11 (4.8) | 12 (5.1) |
| Saudi Arabia | 71 (31.1) | 76 (32.1) |
| United Arab Emirates | 7 (3.1) | 6 (2.5) |
| USA | 13 (5.7) | 14 (5.9) |
| Enrolled in another covid-19 trial | 29 (12.7) | 31 (13.1) |
BMI=body mass index; SD=standard deviation; ULN=upper limit of normal.
Data were missing for six patients in the therapeutic heparin group and two in the prophylactic heparin group.
Data were missing for six participants in the therapeutic heparin group and four in the prophylactic heparin group.
Data were missing for one patient in the therapeutic heparin group and five patients in the prophylactic heparin group.
Hypoxaemia was defined as oxygen saturation <93% on room air. Data were missing for 19 patients in the therapeutic heparin group and 19 in the prophylactic heparin group.
Includes chronic restrictive pulmonary disease, chronic obstructive pulmonary disease, and asthma.
No patients were on remdesivir or tocilizumab at baseline.
Six patients in the therapeutic heparin group and five in the prophylactic heparin group had D-dimer levels below the ULN.
SD for the natural logarithm of D-dimer ratios (D-dimer levels×ULN).
Data were missing for 16 patients in the therapeutic heparin group and 24 in the prophylactic heparin group.
Data were missing for 14 patients in the therapeutic heparin group and 23 in the prophylactic heparin group.
Effectiveness outcomes
The primary outcome occurred in 37 patients (16.2%) in the therapeutic heparin group and 52 (21.9%) in the prophylactic heparin group (odds ratio 0.69, 95% confidence interval 0.43 to 1.10, P=0.12; table 2 and supplementary table S5). Death from any cause occurred in four patients (1.8%) in the therapeutic heparin group and 18 (7.6%) in the prophylactic heparin group (0.22, 0.07 to 0.65; P=0.006). Hypoxaemic respiratory failure was the most common cause of death (supplementary table S6). The composite of invasive or non-invasive mechanical ventilation occurred in 21 patients (9.2%) in the therapeutic heparin group and 26 (11.0%) in the prophylactic heparin group (0.82, 0.45 to 1.51; P=0.53). ICU admission occurred in 33 patients (14.5%) in the therapeutic heparin group and 42 (17.7%) in the prophylactic heparin group (0.79, 0.48 to 1.29; P=0.34). The composite of all cause death or invasive or non-invasive mechanical ventilation occurred in 23 patients (10.1%) in the therapeutic heparin group and 38 (16.0%) in the prophylactic heparin group (0.59, 0.34 to 1.02; P=0.06). No significant differences were found in time to the primary composite outcome, ICU admission, or mechanical ventilation between the groups (supplementary figs S2, S4, and S5). Differences in all cause death in favour of therapeutic heparin, however, emerged early during the first week of follow-up and continued to be apparent up to 28 days (supplementary fig S3).
Table 2.
Primary and secondary outcomes of moderately ill patients with covid-19 admitted to hospital wards, according to treatment assignment
| Outcomes | No (%) of patients | Odds ratio or geometric mean ratio (95% CI) | P value | |
|---|---|---|---|---|
| Therapeutic heparin (n=228) | Prophylactic heparin (n=237) | |||
| Primary outcome | ||||
| Primary composite outcome* | 37 (16.2) | 52 (21.9) | 0.69 (0.43 to 1.10) | 0.12 |
| Secondary outcomes | ||||
| Death from any cause | 4 (1.8) | 18 (7.6) | 0.22 (0.07 to 0.65) | 0.006 |
| Invasive mechanical ventilation | 11 (4.8) | 16 (6.8) | 0.70 (0.32 to 1.55) | 0.38 |
| Any mechanical ventilation† | 21 (9.2) | 26 (11.0) | 0.82 (0.45 to 1.51) | 0.53 |
| ICU admission | 33 (14.5) | 42 (17.7) | 0.79 (0.48 to 1.29) | 0.34 |
| Death or any mechanical ventilation | 23 (10.1) | 38 (16.0) | 0.59 (0.34 to 1.02) | 0.06 |
| Death or ICU admission | 36 (15.8) | 50 (21.1) | 0.70 (0.44 to 1.13) | 0.14 |
| Mean (SD) ventilator-free days | 26.5 (5.6) | 24.7 (8.5) | 1.77 (1.02 to 3.08) | 0.042 |
| Mean (SD) organ support-free days | 25.8 (6.2) | 24.1 (8.8) | 1.41 (0.90 to 2.21) | 0.13 |
| Mean (SD) ICU-free days | 26.0 (6.1) | 24.2 (8.8) | 1.51 (0.94 to 2.41) | 0.087 |
| Mean (SD) hospital-free days | 19.8 (7.3) | 18.4 (9.2) | 1.09 (0.79 to 1.50) | 0.59 |
| Renal replacement therapy‡ | 2 (0.9) | 5 (2.1) | 0.41 (0.08 to 2.15) | 0.29 |
| Thromboembolism§: | ||||
| Venous | 2 (0.9) | 6 (2.5) | 0.34 (0.07 to 1.71) | 0.19 |
| Arterial | 0 (0.0) | 1 (0.4) | - | - |
| Bleeding: | ||||
| ISTH major bleeding¶ | 2 (0.9) | 4 (1.7) | 0.52 (0.09 to 2.85) | 0.69 |
| Red blood cell transfusion (≥1 unit) | 3 (1.3) | 9 (3.8) | 0.34 (0.09 to 1.27) | 0.14 |
| Transfusion of other blood components or products** | 1 (0.4) | 0 (0.0) | - | - |
| Heparin induced thrombocytopenia | 0 (0.0) | 0 (0.0) | - | - |
| Geometric mean (SD) D-dimer ratio (D-dimer×ULN)†† | 1.9 (0.7) | 2.4 (0.9) | 0.88 (0.78 to 0.99) | 0.032 |
ICU=intensive care unit; SD=standard deviation; ISTH=International Society on Thrombosis and Haemostasis.
All clinical outcomes were assessed up to 28 days post-randomisation. Analyses of all outcomes with exception of D-dimer ratio (D-dimer×ULN), ventilator-free, organ support-free, ICU-free, and hospital-free days alive were repeated for the timeframe up to hospital discharge and are shown in supplementary table S20.
Defined as death, invasive mechanical ventilation, non-invasive mechanical ventilation, or ICU admission.
Invasive or non-invasive (bilevel or continuous positive airway pressure) mechanical ventilation.
Continuous renal replacement therapy or intermittent haemodialysis.
All diagnostically confirmed except for one symptomatic deep vein thrombosis event in the prophylactic heparin group, which could not be definitively confirmed because diagnostic imaging was not done during acute symptomatic period.
Major bleeding defined by the ISTH Scientific and Standardization Committee.
Transfusion of platelets, frozen plasma, prothrombin complex concentrate, cryoprecipitate and/or fibrinogen concentrate; 17 patients received convalescent plasma and were not included in the count.
Geometric mean ratio defined as ratio of geometric means of D-dimer ratios (D-dimer×ULN) of day 2 ±24 hours post-randomisation, adjusted for baseline geometric means of D-dimer ratios using analysis of covariance. SD for the natural logarithm of D-dimer ratios at day 2 ±24 hours. Data for day 2 ±24 hours D-dimer were missing for 66 patients in the therapeutic heparin group and 64 in the prophylactic heparin group.
The mean number of ventilator-free days was 26.5 (standard deviation 5.6) in the therapeutic heparin group and 24.7 (SD 8.5) in the prophylactic heparin group (odds ratio from ordinal logistic regression 1.77, 95% confidence interval 1.02 to 3.08; P=0.042). The mean number of organ support-free days was 25.8 (SD 6.2) in the therapeutic heparin group and 24.1 (SD 8.8) in the prophylactic heparin group (odds ratio 1.41, 95% confidence interval 0.90 to 2.21; P=0.13). The mean number of ICU-free days was 26.0 (SD 6.1) in the therapeutic heparin group and 24.2 (SD 8.8) in the prophylactic heparin group (1.51, 0.94 to 2.41; P=0.087). No relevant between group difference in hospital-free days was found (table 2).
Venous thromboembolism occurred in two patients (0.9%) in the therapeutic heparin group and six (2.5%) in the prophylactic heparin group (0.34, 0.07 to 1.71; P=0.19; table 2 and supplementary table S7). No fatal thromboembolic events occurred. D-dimer levels, assessed a median of 1.5 days (interquartile range 1-2 days) after randomisation in 162 patients (71.1%) assigned to therapeutic heparin and 173 (73.0%) assigned to prophylactic heparin, were lower in the therapeutic heparin group (geometric mean ratio 0.88, 95% confidence interval 0.78 to 0.99; P=0.03).
Safety outcomes
Major bleeding events occurred in two patients (0.9%) in the therapeutic heparin group and four (1.7%) in the prophylactic heparin group (odds ratio 0.52, 95% confidence interval 0.09 to 2.85; P=0.69, table 2). No fatal bleeding events or cases of intracranial haemorrhage occurred (supplementary tables S8 and S9).
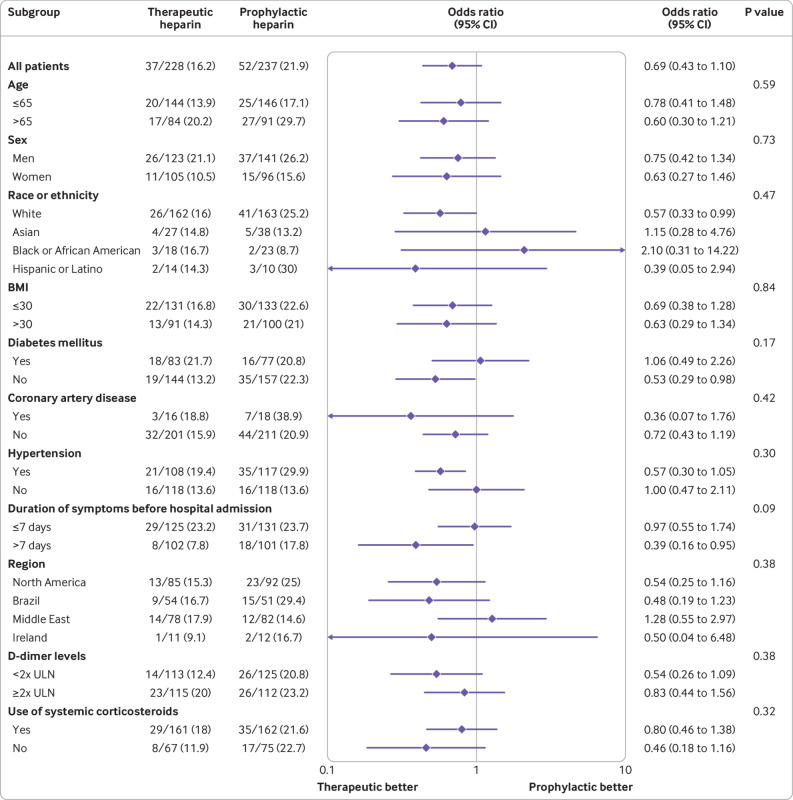
Subgroup and sensitivity analyses
Prespecified subgroup analyses of the primary outcome and post hoc subgroup analyses of all cause death did not provide evidence for differences in treatment effect between subgroups (fig 2 and supplementary fig S6). Findings from the per protocol analyses and other sensitivity analyses, including an intention-to-treat analysis of the primary outcome with time-by-treatment interaction, were similar to those from the primary analysis (supplementary tables S10-S17).
Fig 2.
Subgroup analysis of the primary outcome (a composite of death, invasive mechanical ventilation, non-invasive mechanical ventilation, or admission to an intensive care unit). Subgroup specific odds ratios derived from logistic regression. Circles represent point estimates and whiskers represent 95% confidence intervals. Odds ratio <1.0 favours therapeutic heparin. BMI=body mass index; ULN=upper limit of normal
Discussion
In this randomised trial of moderately ill patients with covid-19 and increased D-dimer levels admitted to hospital wards, therapeutic heparin was not associated with a significantly lower incidence of the primary composite of death, mechanical ventilation, or ICU admission compared with prophylactic heparin. The odds of all cause death in the group allocated to therapeutic heparin was, however, significantly reduced by 78%. Between group differences were smaller and non-significant for mechanical ventilation and ICU admission.
Comparison with other studies
The mortality reduction was more pronounced in RAPID than in a multiplatform trial of moderately ill patients with covid-19 admitted to hospital, integrating the Antithrombotic Therapy to Ameliorate Complications of COVID-19 (ATTACC), Accelerating COVID-19 Therapeutic Interventions and Vaccines-4 Antithrombotics Inpatient Platform Trial (ACTIV-4a), and the Randomized, Embedded, Multifactorial Adaptive Platform Trial for Community-Acquired Pneumonia (REMAP-CAP).19 Potential explanations include chance and a stronger contrast between treatment arms in RAPID compared with the multiplatform trial.19 28 The multiplatform trial allowed intermediate dose heparin in the control group, and 28.3% of participants received higher than prophylactic doses.19 In addition, 20.4% participants in the experimental group received lower than therapeutic heparin doses.19 RAPID only allowed prophylactic heparin doses in the control group, and only 1.7% of participants received higher doses with no clear clinical indication. Similarly, only 2.6% received lower than therapeutic heparin doses in the experimental group (supplementary tables S18 and S19). It is unlikely that the difference in eligibility criteria for increased D-dimer levels between RAPID and the multiplatform trial account for the larger reduction in deaths in RAPID. The multiplatform trial did not find a treatment-by-subgroup interaction for any of the outcomes, including all cause death, when distinguishing between patients who were D-dimer positive, D-dimer negative, or had unknown D-dimer levels.19 Both trials excluded patients at higher risk of bleeding and thrombosis, and those who were receiving mechanical ventilation at screening.21 29 The effectiveness of anticoagulation seems to depend on the type of anticoagulant: the Anticoagulation Coronavirus (ACTION) trial used 15-20 mg of rivaroxaban in 94% of patients assigned to therapeutic anticoagulation, and found no benefit.30 Rivaroxaban is unlikely to have the anti-inflammatory and antiviral properties attributed to heparin.2 11 12 13 14 15 In addition, ACTION allowed intermediate doses of enoxaparin in the control group. Nevertheless, given variation in findings from published trials, prospective meta-analyses will be important to determine the effects of different types and doses of anticoagulants in different patient subgroups.31 32
The trial was conducted during a 12 month period between May 2020 and May 2021. During this time, management strategies for covid-19 have evolved, which in turn could have influenced the effect of therapeutic heparin on clinical outcomes. However, we found no time-by-treatment interaction in a sensitivity analysis (supplementary table S15). In RAPID and the multiplatform trials, lower rates of major bleeding compared with those in cohort studies were observed, suggesting that investigators were able to exclude patients with higher risks of bleeding.19 20 A numerical increase in bleeding risk with prophylactic heparin in this trial is most probably a chance finding; 95% confidence intervals are wide and compatible with the increased risk of bleeding associated with therapeutic heparin in the multiplatform trial by Lawler et al.19 In fact, one of the patients in the prophylactic heparin group experienced a major bleed after hospital discharge while not receiving any form of anticoagulation. The event was reported, as it occurred within the 28 day observation period. The reason for low venous thromboembolic events in this and other trials is unclear (2.2% overall in RAPID, 1.9% in the multiplatform trial in moderately ill patients,19 4.7% in ACTION),30 but could reflect eligibility criteria or improvements in therapies addressing inflammatory and thrombotic processes, compared with earlier studies.17 19 30 33
Limitations of this study
Our trial has several limitations. RAPID had an adaptive design. The protocol prespecified that the sample size would be increased if the conditional power at 75% of the original sample size was between 60% and 80%.21 The conditional power was, however, below 60%, therefore the sample size was not increased and RAPID remained underpowered for the analysis of the primary outcome. Despite encouraging early observational data from Wuhan, China,2 we did not consider all cause death as a primary outcome, as the sample size required to appropriately power the trial for this outcome would not have been feasible. Rather, we developed a primary composite outcome that would capture death, severe disease, and relevant health care utilisation irrespective of setting and available resources across geographical locations and pandemic waves. At the time of trial design in March and April 2020, covid-19 was essentially an unknown entity with no known effective treatments. At this time, about 25% of patients admitted to the hospital in Ontario, Canada, were subsequently admitted to the ICU and an additional 10% of patients died in-hospital without previous ICU admission.34 35 Taken together, this would have resulted in an average risk of the composite of death or ICU admission of 35%. Based on early data from Wuhan, China,2 we anticipated that the event rate in the control group could reach 50% if D-dimer levels were used for enrichment. To account for the uncertainty at the time of trial design, we additionally used an adaptive design with conditional power analysis.
Given the potential for overburdening resource limited healthcare systems during the pandemic, it was not considered feasible to conduct a double blind trial. However, ICU admission and non-invasive mechanical ventilation as components of the primary composite outcome might have been too subjective and open to performance bias or random variation. Performance bias36 could have occurred if clinicians had been influenced in their decision to admit patients to ICU or treat them with non-invasive mechanical ventilation by their knowledge of the allocated treatment; random variation could have been caused by the pandemic’s variable impact on hospital resources over time and across regions. Detection bias36 could have occurred if investigation or reporting of potential events (especially incidental deep vein thromboses) in patients receiving therapeutic heparin was less likely than events in patients receiving prophylactic heparin. The converse could have been true for bleeding events. Biased reporting is unlikely to have occurred for the components of the primary outcome as admission to ICU and mechanical ventilation are unambiguously supported by medical source documents and all cause death is objective. Also, an independent clinical events committee blindly adjudicated all relevant outcomes. As in other anticoagulation trials in patients with covid-19,19 20 30 37 many screened patients were not deemed eligible or did not consent to participate. Our findings might therefore not be generalisable to all moderately ill patients with covid-19 admitted to hospital wards.
Conclusions
The RAPID trial did not find a significant reduction in the primary composite outcome of death, mechanical ventilation, or ICU admission with therapeutic heparin. However, therapeutic heparin was associated with a substantially decreased odds of all cause death and low risk of major bleeding. In conjunction with the recently published multiplatform trial,19 the RAPID trial therefore suggests that therapeutic heparin is beneficial in moderately ill patients with covid-19 admitted to hospital wards.
What is already known on this topic
Randomised trials suggest that therapeutic heparin is beneficial in moderately ill patients with covid-19 admitted to hospital, but of no benefit and potential harm when provided to critically ill patients
Given the disparate findings in these two patient populations, there is hesitancy to adopt therapeutic heparin as standard care in moderately ill patients with covid-19
What this study adds
Use of therapeutic heparin in moderately ill patients with covid-19 and increased D-dimer levels admitted to hospital wards was not associated with a significant reduction in the primary composite outcome of death, non-invasive or invasive mechanical ventilation, or ICU admission
Although the difference in the primary outcome was not statistically significant, a noticeable reduction in mortality and low risk of bleeding was observed with therapeutic heparin
Acknowledgments
Details of the trial can also be found at ClinicalTrials.gov NCT04444700.
We thank the patients and hospital staff who contributed to this trial, the donors who contributed to RAPID crowd funding, hospital sites that donated research infrastructure in kind, and the data and safety monitoring board.
The RAPID Trial Investigators:
Andreas Laupacis, Yulia Lin, Andrew Day, Bram Rochwerg, Jameel Abdulrehman, Mansour Gergi, Rodrigo Hidd Kondo, Bruna Mamprim Piloto, Guilherme de Abreu Pereira, Fernando Salvetti Valente, Ariel Fernando Villarroel Agreda, Pablo Andres Munoz Torres, Maíra Oliveira Moraes, Claudia de Lucena Moreira, Fernando Galassi Stocco Neto, Fabíola Vieira Duarte Baptista, Joanne Alves Moreira, Augusto Séttemo Ferreira, Paula Frudit, Gabriel Martinez, Heraldo Possolo Souza, Rodrigo Antônio Brandão Neto, Elbio Antonio d'Amico, Eduardo Messias Hirano Padrão, Fernando Sarin da Mota e Albuquerque, Giovanna Villela Zangrossi, Alberto Kendy Kanasiro, Alissom Vitti Cincoto, Hugo de Souza Reis, Vitor Miyashiro Arias da Silva, Arthur Petrillo Bellintani, Vivian dos Santos Pereira, Yohan Washington de Oliveira, Bárbara Justo Carvalho, Mariana de Souza Novaes, Henrique Brito Silveira, Gabriel César Alves de Avelar, Lara Bonanni Mota, Karina Caciola, Matheus de Arêa Leão Freire Marim, Tales Cabral Monsalvarga, Alexandre Salgado Blanco Santos, Ahmed Haydar, Gabriella Seixas Sampaio Saraiva, Sabrina Correa da Costa Ribeiro, Julio Flavio Meirelles Marchini, Julio Cesar Garcia de Alencar, Ana Catharina de Seixas Santos, Caroline Millette, Mathieu Lebeau, Céline Devaux, Mélina Boutin, Trung Nghia Nguyen, Line Srour, Flavia de Angelis, Mariane Fugulin, Alexandra Binnie, Shayna A.D. Bejaimal, Andrew Binding, Rosa M. Marticorena, Galo Ginocchio, Eric Kaplovitch, Klaudia Rymaszewski, Afsaneh Raissi, Marcelo Falappa, Blair Ernst, Amna Ali, Martin Romano, Mobina Khurram, Christie Kim, Ajay Kapur, Michelle Edwards, Vidushi Swarup, Bruna Camilotti, Jiten Jani, Jeff Carter, Mark R. Gillrie, Davinder Sidhu, Traci Robinson, Krystina Stutely, Irene Watpool, Rebecca Porteous, Kevin Jao, Jean-Samuel Boudreault-Pedneault, Christopher Kandel, Maureen T. Taylor, Wei En Enoch Choo, Laura Parsons, Ann Dowbenka, Gitana Ramonas, Sergey Nikitin, Jeffery Patterson, Mark Hnatiuk, Anca Tapardel, Sarah Takach- Lapner, Thirza Carpenter, Lori Rackel, Rebecca Cairns, Jessica Pinder, Peter Anglin, Catherine McPherson, Liselle Chiverton, David Barbosa, Shany Loukiantchenko, Yana Shamiss, Danaë Tassy, Sudeep Shivakumar, Mary-Margaret Keating, Sue Pleasance, Barry Kevane, Sarah Cullivan, Nick Power, Peter Doran, Kelly Leamy, Aoife Kelly, Conor Moran, Mairead O'Connor, Aoife McDonnell, Roseanne Boyce, Faiza Sefroun, Rabia Hussain, Patrick Murray, Anna Malara, Brenda Molloy, Meadbh O’Halloran, Emer Cunningham, Jack Lambert, Aoife Cotter, Brian Marsh, Gerard Sheehan, Eavan Muldoon, James Woo, Sean Gaine, Deirdre Morley, Farjah H AlGahtani, Ibrahim Almaghlouth, Sondus Ata, Fai Alkhathlan, Najma Khalil, Israa Mohamed Hussein, Mohammed Bashir, Ahmed S. BaHammam, Abdulrahman Alsultan, Hadeel Alkofide, Tariq M Alhawassi, Abdulhadi M. Alqahtani, Emad K. Zayed, Ammar AlSughayir, Yacoub Abuzied, Hazzaa AlZahrani, Jawaher Al-Otaibi, Haya Alothaimeen, Noura Alzannan, Amer Al Homssi, Haisam Abid, Stephanie Jones, Shannon Broaddrick, Neha Jain, Roz King, Mohit Jindal, Kristen Sanfilippo, Patty Nieters, Muhammad Hammad, Aleeswa Francis Benny, Tariq A. Hamdan, Suhaib Kamal Ahmed Elobaid, Ibrahim Khafagi, Saima Saeed Ahmed, AbduleRehman AlEssaie, Shamma AlAlawi, Khloud Bashir, Aysha Abdulla Salem Al Suwaidi, Hiba Ibrahim Khogali Ahmed, Mohamed Milad Ismail, El Mutasim Ahmed El Faki, Mercy Charles, Alice Dang, Gurpreet Lakhanpal, Dominic Lee, Prachi Ray, Maria Naydenova, Kosma Wysocki, Aziz Jiwajee, Greg Wendling, Rebekah Boyle, Elaine Cornell, Debora Kamin Mukaz.
Web extra.
Extra material supplied by authors
Web appendix: Supplementary material
Contributors: MS and PJü conceived the trial. MS, GHT, BRDC, KET, MCu, and PJü designed the trial. MS, MAH, LBK, FNA, PDJ, DL, AB, MCa, CC, ERA, MCu, and PJü obtained funding. MS, GHT, HR, MAH, LBK, FNA, FA, KA, MAls, FAS, CP, CS, ST, TT, PJak, DS, MAlm, LC, CC, JJ, MAr, CW, KD, ERA, VD, ET, GL, MF, EN, and PJü collected the data. FZ, BRDC, KET, and PJü did the statistical analysis and interpreted it in collaboration with the other authors. MS, GHT, MCu, and PJü drafted the manuscript. All authors critically revised the manuscript for important intellectual content. MS and PJü are the guarantors. They had full access to the final data and had final responsibility for the decision to submit for publication. The corresponding author attests that all listed authors meet authorship criteria and no others meeting the criteria have been omitted.
Funding: This study was funded by Task 54, Defense Research Development Canada, Department of National Defense, Ottawa, Canada; St Michael’s Hospital Foundation, Toronto, Canada; St Joseph’s Health Centre Foundation, Toronto, Canada; 2020 TD Community Health Solutions Fund – COVID-19 research grant; Michael Garron Hospital, Toronto, Canada; The Ottawa Hospital Foundation COVID-19 Emergency Response Fund, Ottawa, Canada; International Network of Venous Thromboembolism Clinical Research Networks (INVENT) Kickstarter Award; Science Foundation Ireland, Enterprise Ireland, IDA Ireland COVID-19 Rapid Response Funding Call 20/COV/0157; SEAMO (South-eastern Ontario Academic Medical Organization) COVID-19 Innovation Fund; P20 GM135007 from the National Institute of General Medical Sciences, National Institutes of Health; University of Vermont Medical Center Fund Grant; College of Medicine Research Center, and Deanship of Scientific Research, King Saud University, Riyadh, Saudi Arabia. The funders had no role in the trial design; conduct, collection, management, analysis, or interpretation of data; or in preparation or review of the manuscript or the approval of the manuscript for submission.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/disclosure-of-interest/ and declare: MS reports receiving funding from Task 54, Defense Research Development Canada, Department of National Defense, Ottawa, Canada (to institution), St Michael’s Hospital Foundation, Toronto, Canada (to institution), St Joseph’s Health Centre Foundation, Toronto, Canada (to institution), International Network of Venous Thromboembolism Clinical Research Networks (INVENT) Kickstarter Award (to institution) during the conduct of this study. LBK reports receiving funding from the INVENT Kickstarter Award during the conduct of the study. FNA reports receiving Science Foundation Ireland, Enterprise Ireland, IDA Ireland COVID-19 Rapid Response Funding Call 20/COV/0157 (to Institution; University College Dublin) during the conduct of this study; and grants or contracts from Sanofi, Daiichi-Sankyo, Irish Health Research Board (a state agency under the Department of Health, supporting and funding health and social care research), and Bayer; and reports patent submitted (European Application No 20166826.6) outside of the submitted work. LAC reports receiving honorariums for lectures and presentations for Bristol Meyers Squibb, Pfizer, Bayer, Boehringer Ingelheim, Leo Pharma, Sanofi, The Academy for Continued Advancement in Healthcare Education outside of the submitted work. PDJ reports receiving research grant funding from Bayer, Takeda, CSL Behring outside of the submitted work and reports receiving funding from SEAMO (South-eastern Ontario Academic Medical Organization) COIVD-19 Innovation Fund during the conduct of this study. DL reports receiving research support from Bayer, Biomarin, CSL-Behring, Octapharma, Sanofi; and serving on Data Safety Monitoring and Advisory Boards for Biomarin, CSL Behring, Takeda, Sanofi, and Spark outside of the submitted work. MCa reports grant or contracts from Bristol Meyers Squibb, Leo Pharma, Pfizer (to institution); consulting fees from Bayer, Pfizer, Bristol Meyers Squibb, Sanofi, Servier, Leo Pharma (to institution) outside of the submitted work. CC reports stock options from BioCogniv, Burlington, Vermont, USA outside of the submitted work. CW reports receiving payment or honorariums for speaking engagements from Leo Pharma, Pfizer, Bristol Meyers Squibb-Pfizer, and Servier and serving on advisory board meetings for LEO Pharma, Pfizer, Bristol Meyers Squibb-Pfizer, Servier outside of the submitted work. KD reports receiving honorariums from LEO Pharma and Pfizer outside of the submitted work. ERA reports receiving funding from 2020 TD Community Health Solutions Fund COVID-19 research grant (to institution) during the conduct of this study; honorariums from Pfizer and Bayer; support for attending meetings and/or travel from Pfizer, and participation in advisory board for Tavalisse outside of the submitted work. MF reports consulting fees from Pine Trees Health outside of the submitted work. SM reports grants and personal fees from Daiichy Sankyo, grants and personal fees from Bayer, Pfizer, and Boehringer-Ingelheim, personal fees from Portola, Abbvie, Bristol Meyers Squibb-Pfizer, and Sanofi, outside the submitted work. AYYL reports receiving consulting fees from LEO Pharma; payment or honorariums for speaking engagements and/or consulting from LEO Pharma and Pfizer, and serving on a data safety monitoring board or advisory board for CONNECTS program (COVID-19 clinical trials involving anticoagulation) outside of the submitted work. MC reports receiving an honorarium from the International Society on Thrombosis and Haemostasis outside of the submitted work. PJü reports receiving funding from Task 54, Defense Research Development Canada, Department of National Defense, Ottawa, Canada (to institution), St Michael’s Hospital Foundation, Toronto, Canada (to institution), St Joseph’s Health Centre Foundation, Toronto, Canada (to institution), International Network of Venous Thromboembolism Clinical Research Networks (INVENT) Kickstarter Award (to institution) during the conduct of this study; receiving a grant from Appili Therapeutics (to the institution); payment for participation in advisory boards and/or consulting for Amgen and Fresenius (to the institution); honorariums and travel reimbursement from Amgen, Ava, and Fresenius (to the institution); participation in advisory boards and/or consulting for Amgen and Fresenius; and serves as unpaid member of the steering group of trials funded by Appili Therapeutics, Terumo, and Abbott Vascular outside of the submitted work.
The manuscript’s guarantors (MS and PJü) affirm that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as originally planned (and, if relevant, registered) have been explained.
Dissemination to participants and related patient and public communities: Funding limitations and covid-19 restrictions interfered with our ability to involve patient partners in dissemination of the results of this study. The authors will disseminate the study results through their social media outlets (Twitter). They will run dedicated #hashtag campaigns (#RAPIDTrial) to promote the main findings. The results will be also disseminated through scientific meetings, guideline committee presentations, and webinars. Press releases will be prepared for public engagement via general medicine and haematology blogs and websites on request.
Provenance and peer review: Not commissioned; externally peer reviewed.
Contributor Information
Collaborators: RAPID trial investigators, Andreas Laupacis, Yulia Lin, Andrew Day, Bram Rochwerg, Jameel Abdulrehman, Mansour Gergi, Rodrigo Hidd Kondo, Bruna Mamprim Piloto, Guilherme de Abreu Pereira, Fernando Salvetti Valente, Ariel Fernando Villarroel Agreda, Pablo Andres Munoz Torres, Maíra Oliveira Moraes, Claudia de Lucena Moreira, Fernando Galassi Stocco Neto, Fabíola Vieira Duarte Baptista, Joanne Alves Moreira, Augusto Séttemo Ferreira, Paula Frudit, Gabriel Martinez, Heraldo Possolo Souza, Rodrigo Antônio Brandão Neto, Elbio Antonio d'Amico, Eduardo Messias Hirano Padrão, Fernando Sarin da Mota e Albuquerque, Giovanna Villela Zangrossi, Alberto Kendy Kanasiro, Alissom Vitti Cincoto, Hugo de Souza Reis, Vitor Miyashiro Arias da Silva, Arthur Petrillo Bellintani, Vivian dos Santos Pereira, Yohan Washington de Oliveira, Bárbara Justo Carvalho, Mariana de Souza Novaes, Henrique Brito Silveira, Gabriel César Alves de Avelar, Lara Bonanni Mota, Karina Caciola, Matheus de Arêa Leão Freire Marim, Tales Cabral Monsalvarga, Alexandre Salgado Blanco Santos, Ahmed Haydar, Gabriella Seixas Sampaio Saraiva, Sabrina Correa da Costa Ribeiro, Julio Flavio Meirelles Marchini, Julio Cesar Garcia de Alencar, Ana Catharina de Seixas Santos, Caroline Millette, Mathieu Lebeau, Céline Devaux, Mélina Boutin, Trung Nghia Nguyen, Line Srour, Flavia de Angelis, Mariane Fugulin, Alexandra Binnie, Shayna A.D. Bejaimal, Andrew Binding, Rosa M. Marticorena, Galo Ginocchio, Eric Kaplovitch, Klaudia Rymaszewski, Afsaneh Raissi, Marcelo Falappa, Blair Ernst, Amna Ali, Martin Romano, Mobina Khurram, Christie Kim, Ajay Kapur, Michelle Edwards, Vidushi Swarup, Bruna Camilotti, Jiten Jani, Jeff Carter, Mark R. Gillrie, Davinder Sidhu, Traci Robinson, Krystina Stutely, Irene Watpool, Rebecca Porteous, Kevin Jao, Jean-Samuel Boudreault-Pedneault, Christopher Kandel, Maureen T. Taylor, Wei En Enoch Choo, Laura Parsons, Ann Dowbenka, Gitana Ramonas, Sergey Nikitin, Jeffery Patterson, Mark Hnatiuk, Anca Tapardel, Sarah Takach Lapner, Thirza Carpenter, Lori Rackel, Rebecca Cairns, Jessica Pinder, Peter Anglin, Catherine McPherson, Liselle Chiverton, David Barbosa, Shany Loukiantchenko, Yana Shamiss, Danaë Tassy, Sudeep Shivakumar, Mary-Margaret Keating, Sue Pleasance, Barry Kevane, Sarah Cullivan, Nick Power, Peter Doran, Kelly Leamy, Aoife Kelly, Conor Moran, Mairead O'Connor, Aoife McDonnell, Roseanne Boyce, Faiza Sefroun, Rabia Hussain, Patrick Murray, Anna Malara, Brenda Molloy, Meadbh O’Halloran, Emer Cunningham, Jack Lambert, Aoife Cotter, Brian Marsh, Gerard Sheehan, Eavan Muldoon, James Woo, Sean Gaine, Deirdre Morley, Farjah H AlGahtani, Ibrahim Almaghlouth, Sondus Ata, Fai Alkhathlan, Najma Khalil, Israa Mohamed Hussein, Mohammed Bashir, Ahmed S BaHammam, Abdulrahman Alsultan, Hadeel Alkofide, Tariq M Alhawassi, Abdulhadi M. Alqahtani, Emad K. Zayed, Ammar AlSughayir, Yacoub Abuzied, Hazzaa AlZahrani, Jawaher Al-Otaibi, Haya Alothaimeen, Noura Alzannan, Amer Al Homssi, Haisam Abid, Stephanie Jones, Shannon Broaddrick, Neha Jain, Roz King, Mohit Jindal, Kristen Sanfilippo, Patty Nieters, Muhammad Hammad, Aleeswa Francis Benny, Tariq A. Hamdan, Suhaib Kamal Ahmed Elobaid, Ibrahim Khafagi, Saima Saeed Ahmed, AbduleRehman AlEssaie, Shamma AlAlawi, Khloud Bashir, Aysha Abdulla Salem Al Suwaidi, Hiba Ibrahim Khogali Ahmed, Mohamed Milad Ismail, El Mutasim Ahmed El Faki, Mercy Charles, Alice Dang, Gurpreet Lakhanpal, Dominic Lee, Prachi Ray, Maria Naydenova, Kosma Wysocki, Aziz Jiwajee, Greg Wendling, Rebekah Boyle, Elaine Cornell, and Debora Kamin Mukaz
Ethics statements
Ethical approval
Ethical and regulatory approval were obtained from each of the participating centres. Ethical oversight and approval for the entire study was provided by the institutional review boards of Clinical Trials Ontario, St Michael’s Hospital, Toronto, Canada, and Comissão Nacional de Ética em Pesquisa and Comitê de Ética em Pesquisa, Sao Paulo, Brazil.
Data availability statement
Requests for data sharing should be sent to the corresponding author at michelle.sholzberg@unityhealth.to.
References
- 1. Richardson S, Hirsch JS, Narasimhan M, et al. the Northwell COVID-19 Research Consortium . Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA 2020;323:2052-9. 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost 2020;18:1094-9. 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Guan WJ, Ni ZY, Hu Y, et al. China Medical Treatment Expert Group for Covid-19 . Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med 2020;382:1708-20. 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McGonagle D, O’Donnell JS, Sharif K, Emery P, Bridgewood C. Immune mechanisms of pulmonary intravascular coagulopathy in COVID-19 pneumonia. Lancet Rheumatol 2020;2:e437-45. 10.1016/S2665-9913(20)30121-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wichmann D, Sperhake J-P, Lütgehetmann M, et al. Autopsy Findings and Venous Thromboembolism in Patients With COVID-19: A Prospective Cohort Study. Ann Intern Med 2020;173:268-77. 10.7326/M20-2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Negri EM, Piloto BM, Morinaga LK, et al. Heparin Therapy Improving Hypoxia in COVID-19 Patients - A Case Series. Front Physiol 2020;11:573044. 10.3389/fphys.2020.573044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost 2020;18:844-7. 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Petrilli CM, Jones SA, Yang J, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ 2020;369:m1966. 10.1136/bmj.m1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Thachil J, Cushman M, Srivastava A. A proposal for staging COVID-19 coagulopathy. Res Pract Thromb Haemost 2020;4:731-6. 10.1002/rth2.12372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Iba T, Levy JH, Levi M, Connors JM, Thachil J. Coagulopathy of Coronavirus Disease 2019. Crit Care Med 2020;48:1358-64. 10.1097/CCM.0000000000004458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mu S, Liu Y, Jiang J, et al. Unfractionated heparin ameliorates pulmonary microvascular endothelial barrier dysfunction via microtubule stabilization in acute lung injury. Respir Res 2018;19:220. 10.1186/s12931-018-0925-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Li L, Ma X, Li X. [Effect of heparin on histone-mediated the expression of von Willebrand factor and fibrinogen in lung tissue]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue 2019;31:1363-7. 10.3760/cma.j.issn.2095-4352.2019.11.010. [DOI] [PubMed] [Google Scholar]
- 13. Liu J, Li J, Arnold K, Pawlinski R, Key NS. Using heparin molecules to manage COVID-2019. Res Pract Thromb Haemost 2020;4:518-23. 10.1002/rth2.12353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Helms J, Tacquard C, Severac F, et al. CRICS TRIGGERSEP Group (Clinical Research in Intensive Care and Sepsis Trial Group for Global Evaluation and Research in Sepsis) . High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med 2020;46:1089-98. 10.1007/s00134-020-06062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wang C, Chi C, Guo L, et al. Heparin therapy reduces 28-day mortality in adult severe sepsis patients: a systematic review and meta-analysis. Crit Care 2014;18:563. 10.1186/s13054-014-0563-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054-62. 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Nopp S, Moik F, Jilma B, Pabinger I, Ay C. Risk of venous thromboembolism in patients with COVID-19: A systematic review and meta-analysis. Res Pract Thromb Haemost 2020;4:1178-91. 10.1002/rth2.12439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Paranjpe I, Fuster V, Lala A, et al. Association of Treatment Dose Anticoagulation With In-Hospital Survival Among Hospitalized Patients With COVID-19. J Am Coll Cardiol 2020;76:122-4. 10.1016/j.jacc.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lawler PR, Goligher EC, Berger JS, et al. ATTACC Investigators. ACTIV-4a Investigators. REMAP-CAP Investigators . Therapeutic Anticoagulation with Heparin in Noncritically Ill Patients with Covid-19. N Engl J Med 2021;385:790-802. 10.1056/NEJMoa2105911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Goligher EC, Bradbury CA, McVerry BJ, et al. REMAP-CAP Investigators. ACTIV-4a Investigators. ATTACC Investigators . Therapeutic Anticoagulation with Heparin in Critically Ill Patients with Covid-19. N Engl J Med 2021;385:777-89. 10.1056/NEJMoa2103417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sholzberg M, Tang GH, Negri E, et al. Coagulopathy of hospitalised COVID-19: A Pragmatic Randomised Controlled Trial of Therapeutic Anticoagulation versus Standard Care as a Rapid Response to the COVID-19 Pandemic (RAPID COVID COAG - RAPID Trial): A structured summary of a study protocol for a randomised controlled trial. Trials 2021;22:202. 10.1186/s13063-021-05076-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Page C. Heparin and related drugs: beyond anticoagulant activity. ISRN Pharmacol 2013;2013:910743. 10.1155/2013/910743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kearon C, Akl EA, Ornelas J, et al. Antithrombotic Therapy for VTE Disease: CHEST Guideline and Expert Panel Report. Chest 2016;149:315-52. 10.1016/j.chest.2015.11.026. [DOI] [PubMed] [Google Scholar]
- 24. Schünemann HJ, Cushman M, Burnett AE, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: prophylaxis for hospitalized and nonhospitalized medical patients. Blood Adv 2018;2:3198-225. 10.1182/bloodadvances.2018022954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Schulman S, Kearon C, Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis . Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost 2005;3:692-4. 10.1111/j.1538-7836.2005.01204.x. [DOI] [PubMed] [Google Scholar]
- 26. Doi SA, Furuya-Kanamori L, Xu C, Lin L, Chivese T, Thalib L. Questionable utility of the relative risk in clinical research: a call for change to practice. J Clin Epidemiol 2020;S0895-4356(20)31171-9. 10.1016/j.jclinepi.2020.08.019. [DOI] [PubMed] [Google Scholar]
- 27. Gordon AC, Mouncey PR, Al-Beidh F, et al. REMAP-CAP Investigators . Interleukin-6 Receptor Antagonists in Critically Ill Patients with Covid-19. N Engl J Med 2021;384:1491-502. 10.1056/NEJMoa2100433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ten Cate H. Surviving Covid-19 with Heparin? N Engl J Med 2021;385:845-6. 10.1056/NEJMe2111151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Houston BL, Lawler PR, Goligher EC, et al. Anti-Thrombotic Therapy to Ameliorate Complications of COVID-19 (ATTACC): Study design and methodology for an international, adaptive Bayesian randomized controlled trial. Clin Trials 2020;17:491-500. 10.1177/1740774520943846. [DOI] [PubMed] [Google Scholar]
- 30. Lopes RD, de Barros E Silva PGM, Furtado RHM, et al. ACTION Coalition COVID-19 Brazil IV Investigators . Therapeutic versus prophylactic anticoagulation for patients admitted to hospital with COVID-19 and elevated D-dimer concentration (ACTION): an open-label, multicentre, randomised, controlled trial. Lancet 2021;397:2253-63. 10.1016/S0140-6736(21)01203-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Talasaz AH, Sadeghipour P, Kakavand H, et al. Recent Randomized Trials of Antithrombotic Therapy for Patients With COVID-19: JACC State-of-the-Art Review. J Am Coll Cardiol 2021;77:1903-21. 10.1016/j.jacc.2021.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Tritschler T, Mathieu M-E, Skeith L, et al. International Network of VENous Thromboembolism Clinical Research Networks INVENT-VTE . Anticoagulant interventions in hospitalized patients with COVID-19: A scoping review of randomized controlled trials and call for international collaboration. J Thromb Haemost 2020;18:2958-67. 10.1111/jth.15094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Middeldorp S, Coppens M, van Haaps TF, et al. Incidence of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost 2020;18:1995-2002. 10.1111/jth.14888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Government of Ontario. Hospitalizations. COVID-19 (coronavirus) in Ontario. https://covid-19.ontario.ca/data/hospitalizations
- 35.Government of Ontario. Case numbers and spread. COVID-19 (coronavirus) in Ontario. https://covid-19.ontario.ca/data/case-numbers-and-spread
- 36. Jüni P, Altman DG, Egger M. Systematic reviews in health care: Assessing the quality of controlled clinical trials. BMJ 2001;323:42-6. 10.1136/bmj.323.7303.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Sadeghipour P, Talasaz AH, Rashidi F, et al. INSPIRATION Investigators . Effect of Intermediate-Dose vs Standard-Dose Prophylactic Anticoagulation on Thrombotic Events, Extracorporeal Membrane Oxygenation Treatment, or Mortality Among Patients With COVID-19 Admitted to the Intensive Care Unit: The INSPIRATION Randomized Clinical Trial. JAMA 2021;325:1620-30. 10.1001/jama.2021.4152. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Web appendix: Supplementary material
Data Availability Statement
Requests for data sharing should be sent to the corresponding author at michelle.sholzberg@unityhealth.to.