Dear Editor,
In all age groups, presentation in the clinical setting with the complaint of shoulder pain is frequent. Common causes include local conditions such as rotator cuff disease, impingement syndrome, adhesive capsulitis, tendonitis, bursitis, acromioclavicular joint abnormalities, and cervical pathologies such as disc disease and spondylosis.[1]
A source of shoulder pain and dysfunction, which is often underestimated, is suprascapular nerve neuropathy. This may originate from entrapment of a ganglion or paralabral cyst at the spinoglenoid notch, which has led to weakness and atrophy of the infraspinatus muscle.[2] Suprascapular nerve entrapment accounts for 1%–2% of shoulder pain, and mainly affects patients younger than 40 years of age. There are various treatment options, such as ultrasound-guided aspiration, drainage, surgical excision, or arthroscopic decompression of the cyst. In cases where conservative management has not been successful, surgery may be considered.[3]
A 33-year-old, right-hand dominant, male patient presented with the complaints of posterolateral shoulder pain and nocturnal pain, which had been ongoing for 1 year. There was no history of trauma to the shoulder, and the pain increased with repetitive arm motions and exercises. The initial pain assessment was estimated as Visual Analog Scale 6. The patient had previously been unresponsive to physical therapy, medication, and subacromial corticosteroid injection. On examination, there was no restriction in the shoulder range of motion, but shoulder flexion and abduction were painful at 120°. There was no muscle atrophy, and the neurological examination was normal. Ultrasound examination showed a well–defined, homogeneously anechoic, noncompressible cystic lesion without vascularity at the spinoglenoid notch [Figure 1]. In the electromyography examination, fibrillation potentials and positive sharp waves were observed in the infraspinatus muscle. Magnetic resonance imaging of the right shoulder displayed a lobulated 2 cm × 3 cm × 4 cm ganglion cyst extending to the spinoglenoid notch [Figure 2]. The patient subsequently underwent ultrasonographic aspiration with a 23G needle of the ganglion cyst, and clinical improvement was seen [Figure 3].
Figure 1.
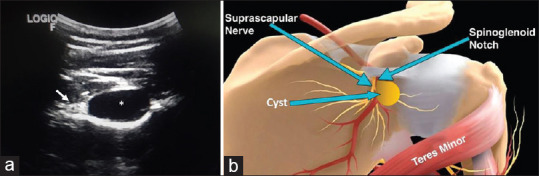
Cyst located at the spinoglenoid notch. (a) Ultrasonographic view, (b) Schematic illustration. *cyst; suprascapular nerve (arrow)
Figure 2.
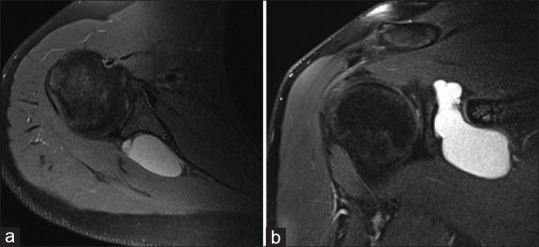
(a) Axial and (a) Coronal magnetic resonance imaging image showing a lobulated 2 cm × 3 cm × 4 cm ganglion cyst extending into the posterior spinoglenoid notch
Figure 3.

Ultrasound-guided aspiration of the cyst using an “in-plane approach”
As a branch of the upper trunk of the brachial plexus (a combination of C5 and C6 roots), the suprascapular nerve is a mixed sensorimotor nerve, which provides motor innervation to the supraspinatus and infraspinatus muscles. This nerve is also responsible for sensory innervation of the glenohumeral and acromioclavicular joints.[4] If the suprascapular nerve is compressed at the spinoglenoid notch, this will cause weakness in the infraspinatus muscle alone. However, injury or compression at the suprascapular notch may result in weakness of both the infraspinatus and supraspinatus muscles.[4] Shoulder pain caused by suprascapular nerve neuropathy as a result of cyst impingement may be easily confused with rotator cuff injury or cervical spondylosis. Compression at the spinoglenoid notch may be due to several etiologies, of which the most usual is a paralabral ganglion cyst. Paralabral ganglion cysts are thought to develop from the seepage of synovial fluid into the paralabral tissue as a result of a capsular defect.[5]
When a patient presents with nonspecific shoulder pain, there should be consideration of suprascapular nerve neuropathy. Although this is not a frequently seen condition, suprascapular notch entrapment is an easily treated with potentially good outcomes if diagnosed and treated early before the development of muscular atrophy.
Declaration of patient consent
The author certify that he has obtained all appropriate patient consent forms. In the form the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Linaker CH, Walker-Bone K. Shoulder disorders and occupation. Best Pract Res Clin Rheumatol. 2015;29:405–23. doi: 10.1016/j.berh.2015.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Romeo AA, Rotenberg DD, Bach BR., Jr Suprascapular neuropathy. J Am Acad Orthop Surg. 1999;7:358–67. doi: 10.5435/00124635-199911000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Zehetgruber H, Noske H, Lang T, Wurnig C. Suprascapular nerve entrapment.A meta-analysis. Int Orthop. 2002;26:339–43. doi: 10.1007/s00264-002-0392-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clavert P, Thomazeau H. Peri-articular suprascapular neuropathy. Orthop Traumatol Surg Res. 2014;100:S409–11. doi: 10.1016/j.otsr.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 5.Wee TC, Wu CH. Ultrasound-guided aspiration of a paralabral cyst at the spinoglenoid notch with suprascapular nerve compressive neuropathy. J Med Ultrasound. 2018;26:166–7. doi: 10.4103/JMU.JMU_39_18. [DOI] [PMC free article] [PubMed] [Google Scholar]


