Abstract
Inflammatory bowel disease (IBD) is a chronic condition that significantly affects the quality of life of its patients. Biologic drugs have been the mainstay treatment in the management of IBD patients but despite their significant contribution, there remains a proportion of patients that do not respond or lose response to treatment. Therapeutic drug monitoring (TDM) involves measuring levels of serum drug concentrations and anti-drug antibodies. TDM of biologic drugs initially emerged to understand treatment failure in other immune mediated inflammatory diseases. This was then introduced in IBD to rationalize primary non-response or secondary loss of response, given that low serum drug concentrations or the formation of anti-drug antibodies are variably associated with treatment failure. The aim of this narrative review is to provide an overview regarding the current use of TDM in clinical practice and to present the evidence available regarding its use in both proactive and reactive clinical settings in preventing and managing treatment failure. This review also presents the existing evidence regarding the association of various clinical outcomes with specific thresholds of drug concentrations, in everyday practice. A narrative review of published articles and conference abstracts regarding the use of TDM in IBD management, through an electronic search using PubMed and ScienceDirect. TDM has proven to be superior and more cost effective in guiding management of patients with treatment failure compared to empiric dose escalation or change in treatment. Despite a trend towards an association between clinical outcomes and drug concentrations, proactive TDM based strategies have not been shown to achieve clear benefit in long-term outcomes. In the clinical setting, TDM has proven to be useful in managing IBD patients, and its use in the reactive setting, as an additional tool to help manage patients with treatment failure, is being promoted as newer guidelines and consensus groups implement TDM as part of the management plan.
Keywords: Therapeutic drug monitoring, Inflammatory bowel disease, Biologic therapies, Loss of response, Reactive, Proactive
Core Tip: In this review, we discuss the existing studies that looked at both proactive and reactive therapeutic drug monitoring (TDM) and concluded that in current practice, reactive TDM has been shown to be useful. When used as an adjunct to clinical assessment and biomarkers in patients with treatment failure, TDM has proven to be a valuable tool for subsequent management.
INTRODUCTION
The management of patients with inflammatory bowel disease (IBD) has changed dramatically over the past decade, more so since the use of biologic agents[1]. Biologics such as anti-tumor necrosis factor (anti-TNF) agents have revolutionized the treatment of patients with IBD during this time in addition to newer classes of biologic agents, such as selective adhesion molecule and interleukin 12 and 23 inhibitors that are also being used. Furthermore, with advances in the treatment of IBD, goals of therapy have also changed as specialists worldwide have adopted the ‘treat to target’ approach in the management of IBD[2]. Despite these advances, treatment failure still occurs in a significant proportion of IBD patients[3], prompting a need in dose intensification or discontinuation of therapy with a change to another class of drug[4,5]. In the past, treatment failure in IBD, defined as either a primary non-response (PNR) or secondary loss of response (sLOR) to a drug, has been difficult to explain and predict. But as a result of a better understanding of the pharmacodynamics (PD) and pharmacokinetics (PK) of biologic drugs, the idea of therapeutic drug monitoring (TDM) emerged as an important tool. It plays a role in not only identifying the mechanism of loss of response but also in guiding clinicians in their treatment approach[6,7].
TDM is defined as the measurement of serum drug and/or anti-drug antibody (ADA) concentrations. ADAs refer to antibodies that are formed in response to the immune system’s recognition of biologic drugs. In several studies, ADAs have been found to be associated with treatment failure because of an up-regulated clearance of the drug[8,9]. Another mechanism of treatment failure relates to a non-immune mediated clearance, resulting in sub-therapeutic levels of the drug.
Over the years, TDM was initially used in the reactive setting for patients, when there was a suspected loss of response to a biologic drug, mainly the anti-TNF agents. Based on the serum drug levels and/or presence of ADAs, the management was changed with the aim of optimizing their current treatment, thus avoiding unnecessary dose intensification or targeted switching between anti-TNF agents or out of class. However, preliminary results from recently published data have shown that TDM used in the proactive setting, by preemptively targeting specific thresholds of serum drug levels, may in fact result in more favorable clinical outcomes[10-17]. Despite growing evidence supporting the use TDM in IBD, there still exist limitations of its use, such as when to use it and how best to apply it. This is evident in the fact that routine use of TDM in the management of IBD patients is not recommended in guidelines, but rather made as suggestions by organizations when faced with a patient with suspected treatment failure[18-22].
This review article summarizes the latest evidence with regards to the use of TDM in both the reactive and proactive settings in addition to its limitations and how it is currently being used in clinical practice.
BACKGROUND OF TDM
The idea of TDM involves measuring the serum concentration of a drug, to maintain an adequate dose that would ensure drug efficacy and to avoid drug toxicity[23]. Use of TDM in clinical practice has existed for many years, even before the development of biologics. In the past, TDM was used for a variety of medications, such as antibiotics and immunosuppressants. More recently, it has been applied to biologics mainly to monitor drug efficacy and to guide management in suspected treatment failure for IBD patients on biologics. In IBD, TDM involves the measurement serum drug levels, in addition to the measurement of ADAs, both of which are related to drug efficacy[8,9]. Although many studies have proved its utility, many issues exist such as timing of TDM, identification of target thresholds for serum drug levels and ADAs, and the practical application of the results. Data looking into this shows that there is considerable variability in target thresholds because of multiple factors that come to play, such as the different methods and assays used in TDM measurements, or the desired clinical outcome.
Lastly, given that the first class of biologics were anti-TNF agents, the use of TDM was first applied for patients who were treated with either infliximab or adalimumab, thus most studies looking into TDM revolved around anti-TNFs. With time, as newer classes of biologics emerged for their use in IBD, more studies were done regarding the application of TDM with vedolizumab or ustekinumab.
OVERVIEW OF TECHNICAL ASPECTS OF TDM
In TDM, the measurement of serum drug levels involves measuring the trough level (TL), meaning the lowest concentration of the drug just before the next dose. With the TL, the goal is to maintain a level sufficient enough for the drug to reach its maximal efficacy[24], and this is where the issue of target thresholds comes to play[25]. Before discussing the clinical relevance of these targets, it is important to know the technical aspects of TL and ADA measurements.
Assays used for TDM
Current tests for TL and ADA concentrations include various commercially available assays such as enzyme-linked immunoassay (ELISA), radioimmunoassay, high pressure liquid chromatography based homogeneous mobility assay, with ELISA being the most commonly used[26,27]. Drug assays use the drug as a calibrator while ADA assays use a monoclonal ADA as a calibrator, with titers often expressed as milligrams per liter. Several studies comparing various drug assays showed good correlation, however since assay methodologies and sensitivities differ, it is best to use the same assay when applying TDM[28]. Additionally, it is important to note that in the case of ELISA assays, the presence of the drug in the serum interferes with the detection of ADAs, thus not adequately quantifying ADA concentrations[29,30]. Various modified ELISA methods have been constructed to circumvent this problem, e.g., by improved puffer technologies, labeled ‘drug resistant’ assays for ADA detection.
Additionally, other factors that may influence results include human factors such as appropriate collection, handling, and storage. Newer studies looking into improving TDM have suggested the idea of point of care (POC) testing in the near future, where TDM measurements are made available on spot, without the need for a laboratory-based testing method[30].
MECHANISMS OF TREATMENT FAILURE IN IBD
To better comprehend the application of TDM in IBD, it is essential to understand the idea of drug PD and PK, as they are significant in understanding the mechanism of treatment failure[24]. Various factors affect a patient’s response to treatment, including low or sub-therapeutic drug levels related to increased clearance, whether it is immune or non-immune mediated in addition to the underlying pathway targeted by the drug.
PNR vs sLOR
Biologic agents, namely anti-TNF drugs, have significantly advanced the management of IBD patients. However, despite this, up to 30% of IBD patients fail to show an initial response after the induction period, also known as PNR, and up to 50% showing sLOR during the maintenance phase, especially during the first year 3-5]. Those with sLOR are patients who had initially responded after the induction phase, but then started to develop symptoms of disease activity, suggestive of treatment failure. Pharmacokinetic mechanisms underlining PNR and sLOR are thought to be due to inadequate serum drug concentrations as evidence has shown that those with low serum drug concentrations during induction or maintenance are less likely to achieve clinical response[31,32].
One study that signified this is the personalized anti-TNF therapy in Crohn’s disease (CD) study (PANTS), which was a prospective observational study carried out in the United Kingdom that included 955 patients with active luminal CD[33]. Results of the study revealed that anti-TNF failure is highly dependent on low drug concentration and that this was associated with immunogenicity and the development of ADAs, especially during induction[33]. This finding mimics other studies that also revealed that higher drug concentrations early on is associated with a reduced risk of PNR and in preventing sLOR[34,35].
Clinical relevance of ADAs
One important aspect of treatment failure in IBD revolves around the idea of immunogenicity, which is an important downside of biologics. Immunogenicity deals with the fact that the immune system recognizes protein aspects of the drug as foreign and forms antibodies in response. These antibodies then form complexes with the drug, resulting in increased drug clearance and lower concentrations of the drug, rendering it ineffective[30]. However, it is important to note that not all antibodies work in the same way. In fact, two types of antibodies exist, neutralizing (NAb) vs non-neutralizing antibodies (non-NAb). Although they both bind to the drug, each render it ineffective in a different way[36]. NAb inhibits the pharmacological function of the drug, thus preventing target binding, whereas non-NAb promotes increased clearance of the drug[37]. This is relevant to the understanding of TDM since there is evidence pointing to a correlation between ADA formation and low serum drug levels[38-40].
One study that evaluated the clinical significance of ADAs was by Baert et al[32] that looked at a cohort of 125 CD patients receiving episodic infusions of infliximab. Results of this study revealed an association between the development of antibodies against infliximab response to treatment, as low trough infliximab level and high ADA level was found in 83% (10/12) with complete loss of response to infliximab. This finding reflects results of other studies that have also shown that ADA association was independently associated with LOR. There was also a large proportion of patients (61%) that had detectable ADAs and that there was an inverse relationship between ADA titers and duration of response (P < 0.0001)[32]. Moreover, they also noted that the median duration of clinical response was longer in patients with low ADA concentrations compared to those with higher ADA concentrations (71 d vs 35 d; P < 0.001). Similar conclusions were drawn in a study by Reinhold et al[41], where 16/104 (14%) patients had positive ADA titers and 15 of them had sub-therapeutic TLs, reflecting the increased drug clearance effect of ADAs[41].
As explained, ADAs play a significant role in treatment failure of IBD patients on biologics as antibodies neutralize the effect of the biologic agent, but the evidence linking ADA to LOR is not straightforward. This was demonstrated in a prospective study by Gonczi et al[42] that followed 112 IBD patients who were on therapy with adalimumab. Results of this study revealed that ADA positivity was significantly associated with LOR (P = 0.007), but the association between low TL and ADA positivity was not statistically significant (P = 0.054). They concluded that despite the development of ADA, low TL was not associated with LOR and that mainly ADA development should be considered a predictor for treatment failure[42]. This reiterates the significance of NAb in that they inhibit the pharmacological function of the drug resulting in clinical non-response. As opposed to non-NAb, which affect drug efficacy by increased drug clearance thus resulting in low drug levels. For this reason, interpretation of ADA and TL when dealing with LOR should be made with caution.
Another clinically relevant aspect involves patients who develop infusion reactions. These are often found in those with persistently low drug concentrations and a significant concentration of ADAs[32,43], and this was demonstrated in the same study by Reinhold et al[41]. In this retrospective study that followed 104 IBD patients treated with infliximab or adalimumab, the authors delineated a positive correlation between the presence of ADAs and the development of infusions reactions as 44% (7/13) of patients with infusion reactions had positive ADA titers[41].
In conclusion, it has become clear that different ADAs exist and that not all types of antibodies affect drug clearance. Available data suggests that the presence of ADAs has a potential negative impact on clinical outcomes. Additionally, the relationship between ADA and treatment failure is not clear cut and that the impact of ADAs, may be more relevant to certain biologics than others[44-46].
ASSOCIATION OF SERUM DRUG CONCENTRATIONS WITH CLINICAL OUTCOMES
Numerous studies have demonstrated an association between drug levels and favorable outcomes[33,47-50]. Additionally, recent data has shown that higher serum drug concentrations during induction especially, is strongly associated with positive outcomes[34]. However, it is important to note that serum drug concentrations of different biologics vary as a result of many factors, such as patient demographics (age and body size), degree of underlying inflammation, and severity of disease[51]. As a result, there exists a large variation in target thresholds of TLs for each biologic drug. Current thresholds for serum drug concentrations are determined from observational studies and post HOC analyses, by looking at a variety of drug concentrations that have been found to be associated with specific outcomes; these can be seen in Table 1[48,52-56].
Table 1.
Association between various thresholds for serum drug concentrations and clinical outcomes
|
Drug
|
Serum drug level
|
Clinical outcome
|
| Infliximab (IFX) | ||
| IFX | < 2 μg/mL for CD/UC at week 14 | Increased incidence of IFX antibodies[52] |
| IFX | > 2.1 μg/mL at week 14 in UC | Associated with mucosal healing[53] |
| IFX | ≥ 3 μg/mL during maintenance | Clinical remission[48] |
| IFX | > 3 μg/mL at week 14 or 22 in CD | Sustained response[54] |
| IFX | 3-7 μg/mL during maintenance | Remission[16] |
| IFX | ≥ 7 μg/mL during maintenance | Mucosal healing[48] |
| IFX | < 7 μg/mL at week 14 in luminal CD | Absence of primary response[53] |
| IFX | > 9.2 μg/mL at induction week 2 in CD | Fistula response at weeks 14 and 30[56] |
| IFX | ≥ 10 μg/mL at induction week 6 | Clinical response[48] |
| IFX | > 15 μg/mL at week 6 in UC | Associated with mucosal healing[53] |
| IFX | ≥ 20 μg/mL at induction week 2 | Clinical response[48] |
| IFX | ≥ 22 μg/mL at week 6 in UC | Clinical response at week 8[55] |
| IFX | ≥ 25 μg/mL at induction week 2 | Mucosal healing[48] |
| Adalimumab (Ada.) | ||
| Ada. | ≥ 3 μg/mL during maintenance | Clinical response[48] |
| Ada. | ≥ 5 μg/mL post induction (week 14) | Clinical response[48] |
| Ada. | ≥ 7 μg/mL post induction (week 14) | Mucosal healing[48] |
| Ada. | ≥ 8 μg/mL during maintenance | Mucosal healing[48] |
| Ada. | < 12 μg/mL at week 14 in luminal CD | Absence of primary response[53] |
| Ustekinumab (UST) | ||
| UST | ≥ 1 μg/mL during maintenance | Clinical response[48] |
| UST | ≥ 3.5 μg/mL post induction (week 8) | Clinical response[48] |
| UST | ≥ 4.5 μg/mL during maintenance | Mucosal healing[48] |
| Vedolizumab (VDZ) | ||
| VDZ | ≥ 12 μg/mL during maintenance | Clinical response[48] |
| VDZ | ≥ 14 μg/mL during maintenance | Mucosal healing[48] |
| VDZ | ≥ 15 μg/mL post induction (week 14) | Clinical response[48] |
| VDZ | ≥ 17 μg/mL post induction (week 14) | Mucosal healing[48] |
| VDZ | ≥ 24 μg/mL at induction (week 6) | Clinical response[48] |
| VDZ | ≥ 28 μg/mL at induction (week 2) | Clinical response[48] |
Many studies that looked at exposure response relationship studies of anti-tumor necrosis factor drugs have demonstrated that specific drug concentration thresholds are associated with certain clinical outcomes, such as clinical response, improvement in biochemical markers, endoscopic remission, and mucosal healing.
In a retrospective multi-center study carried out by Juncadella et al[47], 98 IBD patients on therapy with adalimumab, underwent TDM and were followed to determine factors associated with outcomes such as biochemical, endoscopic, and histological remission. Results revealed that higher drug concentration during maintenance associated with good clinical outcomes and drug concentration > 12 μg/mL were associated with endoscopic (P = 0.003) and histological remission (P = 0.012) in CD[47]. Similar results were found in another retrospective study by Ungar et al[57], where serum drug levels of both infliximab and adalimumab were significantly higher in patients with mucosal healing compared to those with active disease on endoscopy (P = 0.002 for infliximab and P = 0.01 for adalimumab)[57].
Moreover, results of the PANTS study, showed that the only factor independently associated with PNR was a low infliximab (IFX) concentration at week 14 and that drug concentrations values associated with remission at weeks 14 and 54 were > 7 μg/mL for infliximab and > 12 μg/mL for adalimumab[33].
In terms of disease severity, for CD patients with peri-anal fistula, current evidence supports the idea of targeting higher serum drug concentrations in those patients compared to those without fistulizing disease[56,58,59]. A study by Davidov et al[56], showed a positive association between infliximab TLs during induction and closure of perianal fistula in CD patients, further suggesting that those patients may benefit from a drug level guided treatment.
Interestingly, despite evidence that shows a positive association of higher serum drug levels with clinical outcomes, preliminary results from the SERENE CD and SERENE ulcerative colitis (UC) trials did not show an added benefit. In both trials, patients with CD and UC, were randomized to either induction by standard dosing (SIR) of adalimumab or by an intensified dosing regimen (HIR). Results of both trials revealed that there was no added benefit from those who underwent an intensified regimen even though that subset of patients had higher serum drug concentrations[60,61]. Additionally, in terms of primary endpoints, the rates of clinical and endoscopic remission were similar among both groups.
MANAGEMENT OF TREATMENT FAILURE IN IBD USING A TDM BASED STRATEGY-REACTIVE TDM
Prior to TDM, the standard of care for suspected treatment failure, after exclusion of secondary causes such as infections and non-compliance, was either by empiric dose escalation, change to an alternative anti-TNF, or change to a different class of biologic.
The empiric approach of managing loss of response is considered frequently suboptimal and may lead to additional costs. The TDM-based strategy, by applying measurements of anti-TNF drug levels and anti-drug antibodies at the time of treatment failure offers an alternative. With time, more studies looking into benefits of TDM emerged. These studies highlighted that TDM may be a useful adjunct to optimize the treatment of IBD patients, more cost effective than the standard of practice of empiric changes in management and can be useful in identifying patients who may be supra-therapeutic and instead, may benefit from dose reduction[6,62-64].
A multi-center study carried out by Guidi et al[65], was one of the first prospective studies carried out in a clinical practice setting that compared the management of sLOR by a TDM based algorithm to empiric dose escalations for IBD patients on infliximab. Results of their study demonstrated that the group of patients who underwent TDM based management of LOR resulted in lower rates of dose escalations with similar rates of clinical response, in addition to the fact that the TDM approach was more cost-effective[65]. Another study that reflected similar results was a randomized controlled study (RCT) carried out by Steenholdt et al[66], which recruited 69 Danish patients with CD on treatment with infliximab, who had developed sLOR. Patients were randomized to either routine infliximab dose or TDM based interventions. Rates of clinical response, measured by CD activity index were the same in both groups, 53% vs 58% (P = 0.81) respectively, however the costs per patients was 34% lower in TDM based group (P < 0.001)[66].
An important study that supported the use of reactive monitoring was by Afif et al[67], which looked at measurements of serum drug and ADA levels of 155 IBD patients who were on treatment with infliximab. Results of this study highlighted the importance of TDM in the management of partial or loss of response, as it provided insight into who might benefit from a change in drug or dose escalation. In this study, it can be seen that in ADA positive patients, the decision to change to another anti-TNF resulted in a complete or partial response in 92% of patients compared to 17% for those who underwent dose escalation. Additionally, with regards to drug levels, those who underwent dose escalation because of sub-therapeutic drug levels had a higher rate of complete or partial response compared to those who changed to an alternate drug[67]. Similarly, Yanai et al[6] demonstrated the utility of TDM in managing loss of response, as results from their study showed that patients with high ADA levels had longer duration to response when there was a drug change compared to dose escalation (P = 0.03) and that dose escalation was found to be more effective for those with low or undetectable ADA levels[6].
Additionally, in a study carried out by Kelly et al[63], which followed primary responders on infliximab who initially presented with clinical disease activity, authors revealed that those who underwent TDM based escalation had significantly higher clinical response (P < 0.01) and lower rates of hospitalization (22% TDM vs 35% non-TDM, P = 0.025) compared to the non-TDM based group[63].
A study by Ungar and colleagues that looked at infliximab levels during induction, brought to light an important finding that may help better manage patients with acute severe UC. Results of their study indicated that at day 14, those with acute severe UC had lower serum drug levels compared to patients with moderately severe UC. This is significant as it suggests that patients with acute severe UC may benefit from an intensified regimen as drug efficacy may have been affected by the high degree of inflammation[68].
In terms of cost-effectiveness, Steenholdt et al[66] was able to demonstrate that an individualized approach using reactive TDM was in fact more effective[66]. Results of this multi-center RCT showed that the costs for the intention to treat patients were substantially lower in the TDM based group compared to various infliximab dosing regimens (€ 6038 vs € 9178, P < 0.001). Similar results were also replicated in a study by Velayos et al[62], again demonstrating that dose adjustments made based on a TDM based algorithmic approach is more cost effective than empiric dose escalation[62].
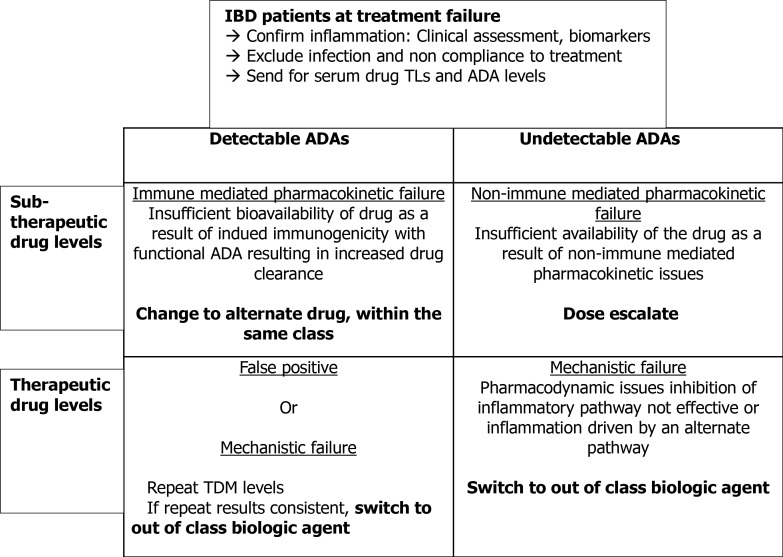
The key recommendations at sLOR regarding the clinical scenarios of different combinations of TL and ADA level results at TDM are consistent based on the above studies. The suggested therapeutic algorithm for the optimal management of anti-TNF treatment failure based on TDM results is summarized in Figure 1[69].
Figure 1.
Therapeutic drug monitoring based approach to treatment failure. IBD: Inflammatory bowel disease; ADA: Anti-drug antibody.
As mentioned earlier, TDM can be approached in one of two ways, either in the reactive or proactive setting. Although much debate exists around the many issues surrounding the use of TDM, in current practice, it is mainly used in the reactive setting. Prior to TDM, standard of practice for the management of treatment failure in IBD is through empiric dose escalation. But with growing evidence highlighting the utility of reactive TDM in guiding subsequent management and that it may in fact be more cost effective, more specialists are using it in their practice[62,66].
As a result of numerous exposure-response relationships linking target TLs to therapeutic outcomes, the idea of proactive approach emerged in the hopes of targeting a specific threshold to avoid PNR or sLOR.
PROACTIVE TDM
The idea of using a proactive approach stemmed from preliminary data revealing that targeting a specific drug concentration at various intervals is associated with better clinical outcomes, compared to empiric dose escalation and TDM done in the reactive setting[13,16,47-50]. A pivotal trial that demonstrated the potential benefits of proactive TDM is the landmark TAXIT trial (Trough Level Adapted Infliximab Treatment). This was a single center RCT of 263 IBD patients on infliximab, whose progress was followed to compare clinical benefit and cost effectiveness of concentration vs clinical based approach. As a result of the design study, the primary end point, of clinical and biochemical remission after 1 year, was not met. However, important findings included lower rates of undetectable drug levels and disease relapse in the proactive group[16].
More recently, Fernandes et al[15] carried out a prospective study of 205 IBD patients with results strongly supporting the proactive approach. Patients were randomized to two groups, those who were treated with IFX without TDM (data collected retrospectively) and those who underwent proactive TDM. In terms of outcomes, they looked at mucosal healing, need for hospitalization, and surgery. Results demonstrated that there were higher rates of treatment escalation in the TDM group (P < 0.001) with less need for surgery in addition to higher rates of mucosal healing (P < 0.0001), concluding that the proactive approach significantly decreased odds of reaching any unfavorable outcomes[15].
In a multi-center, retrospective cohort study of 102 IBD patients on infliximab, Papamichael and colleagues compared outcomes associated between those who underwent reactive vs proactive drug monitoring. The study demonstrated that those who underwent proactive testing after initial reactive testing was associated with greater drug persistence in addition to fewer IBD related hospitalizations (HR 0.18, CI 0.05-0.99; P = 0.007)[10].
Another multi-center study carried out by Papamichael et al[11], involving IBD patients on adalimumab also showed promising results with regards to the proactive approach as results also demonstrated that those who underwent proactive TDM had a reduced risk of treatment failure compared to the standard of care[11].
A recent study that strongly supports the proactive approach is the PAILOT study (Pediatric CD Adalimumab-Level based Optimization Treatment) by Assa et al[14]. This was a RCT of 78 children with CD who were on treatment with adalimumab and their primary end point was sustained steroid free remission. Authors of the study reached their primary endpoint with 82% in the proactive vs 48% in the reactive (P = 0.002) in addition to lower biochemical markers in the proactive group (P = 0.003)[14]. This study is considered a step forward supporting proactive TDM as this was the first proactive RCT whose primary endpoint was reached.
The TAILORIX trial (Tailored Treatment with Infliximab for Active CD) by D’Haens et al[12], was another important proactive trial carried out with the aim of promoting the treat to trough approach. This trial followed 122 biologic naïve patients with active CD who received induction with infliximab and were randomized to three different groups of maintenance infliximab. The three various groups comprised of various dose intensifications based on clinical assessment, biomarkers and/or serum infliximab levels with the primary outcome being sustained corticosteroid free clinical remission at one year. In the end, this trial failed to show the benefit of the proactive approach as results demonstrated that increasing infliximab dose based on combination of symptoms, biomarkers, and drug concentrations does not lead to increased rates of steroid free remission (P = 0.50) compared to dose escalation based on symptoms alone[12]. Interestingly, it is worth noting that less than 50% of patients in each group failed to reach the primary endpoint of corticosteroid free remission in addition to the fact that dose optimization was only carried out at week 14.
Interestingly, new evidence looking at proactive TDM was revealed through several studies including both the SERENE-CD and SERENE-UC trials. In the post induction phase of both trials, authors followed patients into the maintenance phase following induction with high dose vs standard dose adalimumab in the treatment of patients with moderate to severe CD and UC[60,70]. In the maintenance phase of SERENE-CD study, clinical responders from the induction phase were recruited and the authors explored outcomes after 44 wk on adalimumab using a clinical based assessment with the use of biomarkers or through proactive TDM with specified target thresholds. Preliminary results presented at United European Gastroenterology conference (UEG) showed that in terms of efficacy endpoints, the rates were the same in both arms and that the addition of TDM as a criteria showed no added benefit as the rates of clinical response, steroid free clinical remission, and endoscopic remission were similar[70]. A study by Bossuyt et al[71], presented at UEG 2020, showed similar results in terms of clinical endpoints, by comparing outcomes of two groups, ultra-proactive TDM vs reactive TDM. In this study, at the end of one year, there was no difference noted between both groups in terms of composite endpoints of: IBD related hospitalizations, IBD related surgeries, and change of treatment[71].
On the other hand, the SERENE-UC trial looked at outcomes of patients who were randomized to either a high dose or standard dose adalimumab maintenance regimen. Colombel et al[60], concluded that there was a higher number of patients who achieved clinical remission at week 52 in the high dose group, compared to the standard dose group. However, despite the clear numerical difference, it was not statistically significant. Here, the hypothesis was that with an intensified regimen, there would be higher drug bioavailability, which could result in positive outcomes. This theory was based on a previous trial that an intensive regimen in patients with severe UC resulted in lower rates of patients requiring colectomy[72]. Although drug levels were higher in the intensified regimen in both trials, the rates of clinical endpoints were the same.
Although more studies are demonstrating results in favor of proactive TDM, the range of studies remain limited in that the majority are retrospective in nature. Additionally, even with the current use of TDM, used by IBD specialists in the reactive setting, multiple factors are considered in the subsequent management of treatment failure, and not simply by a treat to trough concentration approach.
TDM IN CLINICAL PRACTICE
Despite the issues surrounding the application of TDM involving how and when it should be used, it has proven to be a valuable tool. The current use of TDM as one of many tools of clinical assessment has helped in advancing the care of these patients. As such, the use of TDM has been recommended in certain guidelines and by consensus groups as an adjunct to manage patients with suspected treatment failure. Furthermore, because of the lack of evidence from proactive trials to support the idea of improved clinical outcomes associated with this approach, many support the use of TDM in the reactive setting. For further information, refer to Table 2 for a list of the main TDM based trials including both reactive and proactive[6,10-12,14-16,66,67,70,71,73-77].
Table 2.
A list of the main trials looking at both reactive and proactive therapeutic drug monitoring
|
Ref.
|
Study design; n
|
Population studied
|
Type of intervention
|
Primary outcome
|
Results
|
| Vande Casteele et al[16], 2015 (Proactive) | Prospective single center study RCT, n = 263 | Adults with mod to severe UC responders to infliximab (IFX) | IFX. Target 3-7 μg/mL during maintenance phase. Clinical vs concentration-based dose escalation | Clinical and biochemical remission | Fewer flares in concentration-based group. No difference in remission rates at 1 yr |
| Papamichael et al[73], 2017 (Proactive) | Retrospective multi-center RCT, n = 264 | Adults with CD + UC | IFX 5-10 μg/mL | Treatment failureNeed for IBD related hospitalization or surgery. Adverse events | Proactive was associated with better clinical outcomes, including greater drug durability, less need for IBD-related surgery or hospitalization |
| Perinbasekar et al[74], 2017 (Proactive) | Retrospective single center study, n = 127 | Adult IBD patients initiating treatment with either IFX or adalimumab (Ada) | IFX target ≥ 3 μg/mL; Ada target ≥ 5 μg/mL | Clinical response at 1 yr. Endoscopic response. Persistence with anti-TNF at 1 yr | Persistence with therapy and clinical and endoscopic response were superior for proactive compared to control patients treated with infliximab |
| Bernardo et al[75], 2017 (Proactive) | Retrospective single center study, n = 117 | Adult IBD patients on treatment with infliximab | Clinical based vs proactive TDM. (1) Target IFX CD 3-7 μg/mL; (2) Target IFX UC 5-10 μg/mL; (3) Target Ada CD 5-7 μg/mL; and (4) Target Ada UC 7-9 μg/mL | At 48 wk (1) Clinical remission; (2) Rates of hospitalizations; (3) Rates of surgery; and (4) Therapeutic failure | No difference noted in relation to outcomes. Higher rates of drug escalation in proactive group. Longer period of remission in proactive group |
| D’Haens et al[12], 2018 (Proactive) | Prospective multi-center RCT, n = 122 | Adults with mod to severe luminal CD biologic naïve on infliximab maintenance | Dose escalation using combined approach of clinical + TDM vs symptom-based approach. IFX target > 3 μg/mL during maintenance phase | Sustained steroid-free clinical remission at weeks 22-54 and mucosal healing at week 54 | No difference in terms of rates of steroid-free remission |
| Papamichael et al[10], 2018 (Proactive vs reactive) | Retrospective multicenter study, n = 102 | Adult IBD patients on infliximab | Reactive TDM followed by subsequent proactive TDM vs reactive testing IFX target 5-10 μg/mL | Treatment failure. IBD related hospitalization and surgery | Proactive monitoring after reactive testing associated with greater drug persistence and fever IBD related hospitalizations |
| Papamichael et al[11], 2019 (Proactive) | Retrospective multicenter study, n = 382 | IBD patients on maintenance therapy with adalimumab | Proactive vs reactive TDM. Ada > 10 μg/mL | Treatment failure | Proactive associated with lower risk of treatment failure |
| Assa et al[14], 2019 (Proactive) | Prospective multi-center RCT, n = 78 | Ages 6-17 yr with CD with response to adalimumab | Ada target trough levels ≥ 5 μg/mL | Sustained steroid-free clinical remission (weeks 8-72) | Higher rates of steroid free clinical remission in proactive group |
| Strik et al[76], 2019 (Proactive) | Retrospective multi-center RCT, n = 80 | UC + CD in clinical remission on infliximab maintenance therapy | Dashboard driven dose escalation with TDM vs non TDM. IFX level > 3 μg/mL | Clinical remission | Dashboard-guided dosing resulted in a significant higher proportion of patients who maintained clinical remission during 1 yr of treatment |
| Danese et al[70], 2020 (Proactive) | Prospective multi-center RCT, n = 184 | Clinical responders from induction phase of SERENE-CD | Clinical based group vs proactive TDM (TL 5-10 μg/mL) adalimumab every week or every other week | Clinical remission and endoscopic response and remission at 1 yr | No difference in terms of clinical end points |
| Fernandes et al[15], 2020 (Proactive) | Prospective study, n = 205 | IBD patients completing infliximab induction therapy | Prospective arm (TDM-based dose escalation) vs retrospective arm (non-TDM). IFX levels 3-7 μg/mL CD; IFX levels 5-10 μg/mL UC | Need for surgery, hospital admission, treatment endrates of mucosal healing at 2 yr of treatment | Proactive TDM associated with fewer surgeries and higher rates of mucosal healing |
| Bossuyt et al[71], 2020 (Proactive vs reactive) | Prospective multi-center RCT | All IBD patients on infliximab therapy > week 14 | Using point of care testing at the time of infusion > proactive vs reactive TDM | Clinical remissionDiscontinuation of infliximab. Composite end points of IBD related hospitalizations and surgeries, change of treatment | No difference in terms of rate of clinical remission or treatment discontinuationUltra-proactive not superior to reactive |
| Afif et al[67], 2010 (Reactive) | Retrospective study, n =155 | IBD patients who had infliximab | Measurements of human anti-chimeric antibodies (HACAs) and infliximab concentrations | Loss of response. Change in treatment | Measurement of both antibody and drug levels lead to improved response |
| Steenholdt et al[66], 2014 (Reactive) | Prospective RCT, n = 69 | CD patients failing on infliximab therapy | Infliximab intensification vs algorithm defined using TDM | Clinical and economic outcomes at week 20 | Lower healthcare costs in algorithm-based group. Similar rates of clinical response and remission |
| Kelly et al[63], 2017 (Reactive) | Retrospective study, n = 312 | Primary responders on infliximab who underwent dose escalation | TDM vs clinical based dose escalation of infliximab | Endoscopic remissionClinical response | Higher rates of endoscopic remission with TDM |
| Pouillon et al[77], 2018 (Reactive) | Retrospective single center study, n = 226 | IBD patients who completed maintenance phase of TAXIT | Clinical based vs trough concentration-based dosing of infliximab, infliximab level 3-7 μg/mL | IBD related hospitalization and surgery. Steroid use. Mucosal healing | Similar rates of mucosal healing in both groups. Higher rates of treatment discontinuation in clinic-based group |
TDM: Therapeutic drug monitoring; TNF: Tumor necrosis factor; IBD: Inflammatory bowel disease; RCT: Randomized controlled study; IFX: Infliximab; Ada: Adalimumab.
As evident, the debate over when to apply TDM is still ongoing because of limited prospective large trial studies. For this reason, TDM has not been fully incorporated into guidelines but rather hinted at as suggestions to help guide treatment in those with suspected treatment failure. One example is the guideline by the American Gastroenterological Association, in which the use of TDM is suggested for patients with active IBD on anti-TNFs but not recommended for those with quiescent IBD[18]. Table 3 lists the various recommendations and statements made by various gastroenterology guidelines and consensus groups[18-22].
Table 3.
Recommendations and statements made by various gastroenterology guidelines and consensus groups
|
Guideline/Consensus group
|
Recommendation
|
| AGA[18,19] | Active IBD with anti-TNF → suggest use of reactive TDM |
| Quiescent IBD with anti-TNF → not recommended | |
| Inflammatory bowel disease Sydney/Australian Inflammatory bowel disease consensus working group (2017)[20] | Use of TDM preferred in (1) Upon suspected treatment failure; (2) Following successful induction; and (3) When completed drug holiday |
| For those in clinical remission, consider TDM periodically only if it will change management | |
| British guidelines (2019)[21] | Good practice recommendation → ALL IBD patients should be reviewed 2-4 wk post loading dose to assess response and check drug levels and anti-drug antibodies |
| Use of serum drug trough & anti-drug antibody concentrations to be incorporated when deciding in change of therapy (dose escalation vs switch to other anti-TNF drug or out of class change) | |
| ECCO (2020)[22] | CD in remission on anti-TNF → insufficient evidence to recommend FOR or AGAINST TDM |
| CD patients who have lost response → insufficient evidence |
AGA: American Gastroenterology Association; ECCO: European Colitis & Crohn’s Organization; TDM: Therapeutic drug monitoring; TNF: Tumor necrosis factor; IBD: Inflammatory bowel disease.
PRACTICAL ASPECTS-HOW BEST TO APPLY TDM
Although much evidence exists supporting the use of TDM in the proactive setting, it has become clear that current evidence has not supported its use as routine practice in the management of IBD patients. Instead of dividing TDM into two separate entities, TDM should be considered as a useful tool in the management of IBD patients. As clinicians, we treat patients as a whole, in the sense that we treat their conditions by looking at various aspects including their clinical assessment in addition to biomarkers. Therefore, TDM should be considered as another adjunct that will help guide management as opposed to looking at it as the sole means of ensuring clinical response and remission.
Given the fact that various thresholds for serum drug levels and ADAs exist, it can be difficult to choose which one to target, especially since another variable that complicates this is the type of assay used for these measurements. However, despite the wide range, in current practice, certain thresholds have been followed to ensure clinical response in IBD patients who are on biologic agents. An example of these thresholds to target during maintenance therapy can be seen clearly in Table 4[16,41,78,79]. The values listed in the table have been determined by a panel of IBD specialists that have carefully looked at existing literature relating to TDM[79]. Interestingly, the cut-off values listed by this group differs from the suggestions put forth in the AGA 2017 guideline[18]. It is important to note that these cut-off values are not absolute and should always be made in context with the clinical picture and that higher values might be needed for more rigorous clinical outcomes[48]. In the end, optimal TLs are difficult to define because of the multiple factors discussed above and because of the limited data from observational studies and post HOC analyses, thus it is important to be aware that the idea of ‘one size’ fits all may not be appropriate.
Table 4.
Therapeutic drug monitoring thresholds used in current practice (Using enzyme-linked immunoassay)
|
Drug
|
Cut-off for serum drug concentration
|
Cut-off for detectable ADA
|
| Infliximab | > 3 μg/mL | Present if > 10 μg/mL |
| Adalimumab | > 5 μg/mL | Present if > 10 μg/mL |
| Certolizumab | > 15 μg/mL | - |
| Ustekinumab | Insufficient evidence to make a suggestion | - |
| Vedolizumab | Insufficient evidence to make a suggestion | - |
ADA: Anti-drug antibody.
LIMITATIONS OF TDM
In research, RCTs are considered the gold standard in providing evidence for causal relationships and to support changes to clinical practice, and this seems to be lacking with regards to TDM. Thus, the majority of data available regarding TDM has been based mainly on prospective and retrospective observational studies or post HOC analyses. In addition to the timing of TDM and how often it should be carried out, other issues around TDM have to do with how to best interpret the results given the difficulty in obtaining results in a timely manner and being able to implement changes immediately[79]. Also, the bulk of evidence supporting TDM revolves mainly around anti-TNF and less so with the other biologics such as vedolizumab and ustekinumab[80-82]. These newer biologics are now being used more in IBD thus it is imperative that well designed studies are done looking into outcomes associated with TDM based approach using these drugs.
Nonetheless, results from recent trials are promising and provide hope that more guidance may come soon. One example of such trials, is the PRECISION trial by Strik et al[76], which was the first prospective trial that demonstrated clinical benefit of a more personalized approach involving a dashboard system that incorporates patient features and TDM[76]. The ultra-proactive trial put forth by Bossuyt et al[71] is another example, making it one of the first studies to involve the use of POC testing, suggesting that this technology may be feasible to facilitate future research and the application of TDM. Lastly, the NOR-DRUM study also brings hope as this will be the first large sized RCT looking at the safety and effectiveness of TDM in patients receiving anti-TNF for a range of immune-mediated diseases, including IBD[83].
CONCLUSION
In the end, despite its issues, TDM has evolved the management of IBD patients and is being used more in clinical practice in the hopes of preventing loss of response and to ensure maximal use of biologic drugs. Even though more studies are showing results that support proactive TDM usage, many of them have methodological issues, making their data less reliable to be able to implement changes in clinical practice. Hence making it difficult to prove that proactive TDM is associated with better therapeutic outcomes. At present, TDM has been shown to be a useful tool in managing patients suspected of loss of response and although it has not been fully implemented in guidelines, its usefulness in current practice brings hope that this might soon change.
Footnotes
Conflict-of-interest statement: Authors declare no conflict of interest.
Manuscript source: Invited manuscript
Corresponding Author's Membership in Professional Societies: Canadian Association of Gastroenterology; American Gastroenterological Association; European Crohn's and Colitis Organisation.
Peer-review started: March 19, 2021
First decision: May 1, 2021
Article in press: August 31, 2021
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Canada
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Schoenenberger-Arnaiz JA S-Editor: Fan JR L-Editor: A P-Editor: Xing YX
Contributor Information
Farah Albader, Department of Internal Medicine, McGill University, Montreal H3G1A4, Quebec, Canada.
Petra Anna Golovics, Division of Gastroenterology, Hungarian Defence Forces, Medical Centre, Budapest H-1062, Hungary; Division of Gastroenterology, McGill University, Montreal H3G 1A4, Quebec, Canada.
Lorant Gonczi, First Department of Medicine, Semmelweis University, Budapest H-1083, Hungary.
Talat Bessissow, Division of Gastroenterology, McGill University Health Centre, Montreal H3G 1A4, Quebec, Canada.
Waqqas Afif, Division of Gastroenterology, McGill University, Montreal H3G 1A4, Quebec, Canada.
Peter Laszlo Lakatos, Division of Gastroenterology, McGill University, Montreal H3G 1A4, Quebec, Canada. kislakpet99@gmail.com.
References
- 1.Akobeng AA, Sandborn WJ, Bickston SJ, Chande N, Shackelton LM, Nelson S, Feagan BG. Tumor necrosis factor-alpha antagonists twenty years later: what do Cochrane reviews tell us? Inflamm Bowel Dis. 2014;20:2132–2141. doi: 10.1097/MIB.0000000000000218. [DOI] [PubMed] [Google Scholar]
- 2.Peyrin-Biroulet L, Sandborn W, Sands BE, Reinisch W, Bemelman W, Bryant RV, D'Haens G, Dotan I, Dubinsky M, Feagan B, Fiorino G, Gearry R, Krishnareddy S, Lakatos PL, Loftus EV Jr, Marteau P, Munkholm P, Murdoch TB, Ordás I, Panaccione R, Riddell RH, Ruel J, Rubin DT, Samaan M, Siegel CA, Silverberg MS, Stoker J, Schreiber S, Travis S, Van Assche G, Danese S, Panes J, Bouguen G, O'Donnell S, Pariente B, Winer S, Hanauer S, Colombel JF. Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE): Determining Therapeutic Goals for Treat-to-Target. Am J Gastroenterol. 2015;110:1324–1338. doi: 10.1038/ajg.2015.233. [DOI] [PubMed] [Google Scholar]
- 3.Ben-Horin S, Chowers Y. Review article: loss of response to anti-TNF treatments in Crohn's disease. Aliment Pharmacol Ther. 2011;33:987–995. doi: 10.1111/j.1365-2036.2011.04612.x. [DOI] [PubMed] [Google Scholar]
- 4.Gisbert JP, Panés J. Loss of response and requirement of infliximab dose intensification in Crohn's disease: a review. Am J Gastroenterol. 2009;104:760–767. doi: 10.1038/ajg.2008.88. [DOI] [PubMed] [Google Scholar]
- 5.Billioud V, Sandborn WJ, Peyrin-Biroulet L. Loss of response and need for adalimumab dose intensification in Crohn's disease: a systematic review. Am J Gastroenterol. 2011;106:674–684. doi: 10.1038/ajg.2011.60. [DOI] [PubMed] [Google Scholar]
- 6.Yanai H, Lichtenstein L, Assa A, Mazor Y, Weiss B, Levine A, Ron Y, Kopylov U, Bujanover Y, Rosenbach Y, Ungar B, Eliakim R, Chowers Y, Shamir R, Fraser G, Dotan I, Ben-Horin S. Levels of drug and antidrug antibodies are associated with outcome of interventions after loss of response to infliximab or adalimumab. Clin Gastroenterol Hepatol. 2015;13:522–530.e2. doi: 10.1016/j.cgh.2014.07.029. [DOI] [PubMed] [Google Scholar]
- 7.Volk N, Siegel CA. Defining Failure of Medical Therapy for Inflammatory Bowel Disease. Inflamm Bowel Dis. 2019;25:74–77. doi: 10.1093/ibd/izy238. [DOI] [PubMed] [Google Scholar]
- 8.Seow CH, Newman A, Irwin SP, Steinhart AH, Silverberg MS, Greenberg GR. Trough serum infliximab: a predictive factor of clinical outcome for infliximab treatment in acute ulcerative colitis. Gut. 2010;59:49–54. doi: 10.1136/gut.2009.183095. [DOI] [PubMed] [Google Scholar]
- 9.Karmiris K, Paintaud G, Noman M, Magdelaine-Beuzelin C, Ferrante M, Degenne D, Claes K, Coopman T, Van Schuerbeek N, Van Assche G, Vermeire S, Rutgeerts P. Influence of trough serum levels and immunogenicity on long-term outcome of adalimumab therapy in Crohn's disease. Gastroenterology. 2009;137:1628–1640. doi: 10.1053/j.gastro.2009.07.062. [DOI] [PubMed] [Google Scholar]
- 10.Papamichael K, Vajravelu RK, Vaughn BP, Osterman MT, Cheifetz AS. Proactive Infliximab Monitoring Following Reactive Testing is Associated With Better Clinical Outcomes Than Reactive Testing Alone in Patients With Inflammatory Bowel Disease. J Crohns Colitis. 2018;12:804–810. doi: 10.1093/ecco-jcc/jjy039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Papamichael K, Juncadella A, Wong D, Rakowsky S, Sattler LA, Campbell JP, Vaughn BP, Cheifetz AS. Proactive Therapeutic Drug Monitoring of Adalimumab Is Associated With Better Long-term Outcomes Compared With Standard of Care in Patients With Inflammatory Bowel Disease. J Crohns Colitis. 2019;13:976–981. doi: 10.1093/ecco-jcc/jjz018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.D'Haens G, Vermeire S, Lambrecht G, Baert F, Bossuyt P, Pariente B, Buisson A, Bouhnik Y, Filippi J, Vander Woude J, Van Hootegem P, Moreau J, Louis E, Franchimont D, De Vos M, Mana F, Peyrin-Biroulet L, Brixi H, Allez M, Caenepeel P, Aubourg A, Oldenburg B, Pierik M, Gils A, Chevret S, Laharie D GETAID. Increasing Infliximab Dose Based on Symptoms, Biomarkers, and Serum Drug Concentrations Does Not Increase Clinical, Endoscopic, and Corticosteroid-Free Remission in Patients With Active Luminal Crohn's Disease. Gastroenterology. 2018;154:1343–1351.e1. doi: 10.1053/j.gastro.2018.01.004. [DOI] [PubMed] [Google Scholar]
- 13.Vaughn BP, Martinez-Vazquez M, Patwardhan VR, Moss AC, Sandborn WJ, Cheifetz AS. Proactive therapeutic concentration monitoring of infliximab may improve outcomes for patients with inflammatory bowel disease: results from a pilot observational study. Inflamm Bowel Dis. 2014;20:1996–2003. doi: 10.1097/MIB.0000000000000156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Assa A, Matar M, Turner D, Broide E, Weiss B, Ledder O, Guz-Mark A, Rinawi F, Cohen S, Topf-Olivestone C, Shaoul R, Yerushalmi B, Shamir R. Proactive Monitoring of Adalimumab Trough Concentration Associated With Increased Clinical Remission in Children With Crohn's Disease Compared With Reactive Monitoring. Gastroenterology. 2019;157:985–996.e2. doi: 10.1053/j.gastro.2019.06.003. [DOI] [PubMed] [Google Scholar]
- 15.Fernandes SR, Bernardo S, Simões C, Gonçalves AR, Valente A, Baldaia C, Moura Santos P, Correia LA, Tato Marinho R. Proactive Infliximab Drug Monitoring Is Superior to Conventional Management in Inflammatory Bowel Disease. Inflamm Bowel Dis. 2020;26:263–270. doi: 10.1093/ibd/izz131. [DOI] [PubMed] [Google Scholar]
- 16.Vande Casteele N, Ferrante M, Van Assche G, Ballet V, Compernolle G, Van Steen K, Simoens S, Rutgeerts P, Gils A, Vermeire S. Trough concentrations of infliximab guide dosing for patients with inflammatory bowel disease. Gastroenterology. 2015;148:1320–9.e3. doi: 10.1053/j.gastro.2015.02.031. [DOI] [PubMed] [Google Scholar]
- 17.Martins CdA, Moss AC, Sobrado CW, Queiroz NSF. Practical Aspects of Proactive TDM for Anti-TNF Agents in IBD: Defining Time Points and Thresholds to Target. Crohns Colitis 360. 2019:1. [Google Scholar]
- 18.Feuerstein JD, Nguyen GC, Kupfer SS, Falck-Ytter Y, Singh S American Gastroenterological Association Institute Clinical Guidelines Committee. American Gastroenterological Association Institute Guideline on Therapeutic Drug Monitoring in Inflammatory Bowel Disease. Gastroenterology. 2017;153:827–834. doi: 10.1053/j.gastro.2017.07.032. [DOI] [PubMed] [Google Scholar]
- 19.Vande Casteele N, Herfarth H, Katz J, Falck-Ytter Y, Singh S. American Gastroenterological Association Institute Technical Review on the Role of Therapeutic Drug Monitoring in the Management of Inflammatory Bowel Diseases. Gastroenterology. 2017;153:835–857.e6. doi: 10.1053/j.gastro.2017.07.031. [DOI] [PubMed] [Google Scholar]
- 20.Mitrev N, Vande Casteele N, Seow CH, Andrews JM, Connor SJ, Moore GT, Barclay M, Begun J, Bryant R, Chan W, Corte C, Ghaly S, Lemberg DA, Kariyawasam V, Lewindon P, Martin J, Mountifield R, Radford-Smith G, Slobodian P, Sparrow M, Toong C, van Langenberg D, Ward MG, Leong RW IBD Sydney Organisation and the Australian Inflammatory Bowel Diseases Consensus Working Group. Review article: consensus statements on therapeutic drug monitoring of anti-tumour necrosis factor therapy in inflammatory bowel diseases. Aliment Pharmacol Ther. 2017;46:1037–1053. doi: 10.1111/apt.14368. [DOI] [PubMed] [Google Scholar]
- 21.Lamb CA, Kennedy NA, Raine T, Hendy PA, Smith PJ, Limdi JK, Hayee B, Lomer MCE, Parkes GC, Selinger C, Barrett KJ, Davies RJ, Bennett C, Gittens S, Dunlop MG, Faiz O, Fraser A, Garrick V, Johnston PD, Parkes M, Sanderson J, Terry H IBD guidelines eDelphi consensus group, Gaya DR, Iqbal TH, Taylor SA, Smith M, Brookes M, Hansen R, Hawthorne AB. British Society of Gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults. Gut. 2019;68:s1–s106. doi: 10.1136/gutjnl-2019-318484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Torres J, Bonovas S, Doherty G, Kucharzik T, Gisbert JP, Raine T, Adamina M, Armuzzi A, Bachmann O, Bager P, Biancone L, Bokemeyer B, Bossuyt P, Burisch J, Collins P, El-Hussuna A, Ellul P, Frei-Lanter C, Furfaro F, Gingert C, Gionchetti P, Gomollon F, González-Lorenzo M, Gordon H, Hlavaty T, Juillerat P, Katsanos K, Kopylov U, Krustins E, Lytras T, Maaser C, Magro F, Marshall JK, Myrelid P, Pellino G, Rosa I, Sabino J, Savarino E, Spinelli A, Stassen L, Uzzan M, Vavricka S, Verstockt B, Warusavitarne J, Zmora O, Fiorino G. ECCO Guidelines on Therapeutics in Crohn's Disease: Medical Treatment. J Crohns Colitis. 2020;14:4–22. doi: 10.1093/ecco-jcc/jjz180. [DOI] [PubMed] [Google Scholar]
- 23.Cheifetz A. Overview of Therapeutic Drug Monitoring of Biologic Agents in Patients With Inflammatory Bowel Disease. Gastroenterol Hepatol (N Y) 2017;13:556–559. [PMC free article] [PubMed] [Google Scholar]
- 24.Lobo ED, Hansen RJ, Balthasar JP. Antibody pharmacokinetics and pharmacodynamics. J Pharm Sci. 2004;93:2645–2668. doi: 10.1002/jps.20178. [DOI] [PubMed] [Google Scholar]
- 25.Vaughn BP, Sandborn WJ, Cheifetz AS. Biologic concentration testing in inflammatory bowel disease. Inflamm Bowel Dis. 2015;21:1435–1442. doi: 10.1097/MIB.0000000000000312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gils A, Vande Casteele N, Poppe R, Van de Wouwer M, Compernolle G, Peeters M, Brouwers E, Vermeire S, Geukens N, Declerck PJ. Development of a universal anti-adalimumab antibody standard for interlaboratory harmonization. Ther Drug Monit. 2014;36:669–673. doi: 10.1097/FTD.0000000000000074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bendtzen K, Ainsworth M, Steenholdt C, Thomsen OØ, Brynskov J. Individual medicine in inflammatory bowel disease: monitoring bioavailability, pharmacokinetics and immunogenicity of anti-tumour necrosis factor-alpha antibodies. Scand J Gastroenterol. 2009;44:774–781. doi: 10.1080/00365520802699278. [DOI] [PubMed] [Google Scholar]
- 28.Dreesen E, Bossuyt P, Mulleman D, Gils A, Pascual-Salcedo D. Practical recommendations for the use of therapeutic drug monitoring of biopharmaceuticals in inflammatory diseases. Clin Pharmacol. 2017;9:101–111. doi: 10.2147/CPAA.S138414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cassinotti A, Travis S. Incidence and clinical significance of immunogenicity to infliximab in Crohn's disease: a critical systematic review. Inflamm Bowel Dis. 2009;15:1264–1275. doi: 10.1002/ibd.20899. [DOI] [PubMed] [Google Scholar]
- 30.Vermeire S, Dreesen E, Papamichael K, Dubinsky MC. How, When, and for Whom Should We Perform Therapeutic Drug Monitoring? Clin Gastroenterol Hepatol. 2020;18:1291–1299. doi: 10.1016/j.cgh.2019.09.041. [DOI] [PubMed] [Google Scholar]
- 31.Nanda KS, Cheifetz AS, Moss AC. Impact of antibodies to infliximab on clinical outcomes and serum infliximab levels in patients with inflammatory bowel disease (IBD): a meta-analysis. Am J Gastroenterol. 2013;108:40–47; quiz 48. doi: 10.1038/ajg.2012.363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baert F, Noman M, Vermeire S, Van Assche G, D' Haens G, Carbonez A, Rutgeerts P. Influence of immunogenicity on the long-term efficacy of infliximab in Crohn's disease. N Engl J Med. 2003;348:601–608. doi: 10.1056/NEJMoa020888. [DOI] [PubMed] [Google Scholar]
- 33.Kennedy NA, Heap GA, Green HD, Hamilton B, Bewshea C, Walker GJ, Thomas A, Nice R, Perry MH, Bouri S, Chanchlani N, Heerasing NM, Hendy P, Lin S, Gaya DR, Cummings JRF, Selinger CP, Lees CW, Hart AL, Parkes M, Sebastian S, Mansfield JC, Irving PM, Lindsay J, Russell RK, McDonald TJ, McGovern D, Goodhand JR, Ahmad T UK Inflammatory Bowel Disease Pharmacogenetics Study Group. Predictors of anti-TNF treatment failure in anti-TNF-naive patients with active luminal Crohn's disease: a prospective, multicentre, cohort study. Lancet Gastroenterol Hepatol. 2019;4:341–353. doi: 10.1016/S2468-1253(19)30012-3. [DOI] [PubMed] [Google Scholar]
- 34.Brandse JF, Mathôt RA, van der Kleij D, Rispens T, Ashruf Y, Jansen JM, Rietdijk S, Löwenberg M, Ponsioen CY, Singh S, van den Brink GR, D'Haens GR. Pharmacokinetic Features and Presence of Antidrug Antibodies Associate With Response to Infliximab Induction Therapy in Patients With Moderate to Severe Ulcerative Colitis. Clin Gastroenterol Hepatol. 2016;14:251–8.e1. doi: 10.1016/j.cgh.2015.10.029. [DOI] [PubMed] [Google Scholar]
- 35.Brandse JF, Mould D, Smeekes O, Ashruf Y, Kuin S, Strik A, van den Brink GR, DʼHaens GR. A Real-life Population Pharmacokinetic Study Reveals Factors Associated with Clearance and Immunogenicity of Infliximab in Inflammatory Bowel Disease. Inflamm Bowel Dis. 2017;23:650–660. doi: 10.1097/MIB.0000000000001043. [DOI] [PubMed] [Google Scholar]
- 36.Gunn GR 3rd, Sealey DC, Jamali F, Meibohm B, Ghosh S, Shankar G. From the bench to clinical practice: understanding the challenges and uncertainties in immunogenicity testing for biopharmaceuticals. Clin Exp Immunol. 2016;184:137–146. doi: 10.1111/cei.12742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shankar G, Arkin S, Cocea L, Devanarayan V, Kirshner S, Kromminga A, Quarmby V, Richards S, Schneider CK, Subramanyam M, Swanson S, Verthelyi D, Yim S American Association of Pharmaceutical Scientists. Assessment and reporting of the clinical immunogenicity of therapeutic proteins and peptides-harmonized terminology and tactical recommendations. AAPS J. 2014;16:658–673. doi: 10.1208/s12248-014-9599-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ainsworth MA, Bendtzen K, Brynskov J. Tumor necrosis factor-alpha binding capacity and anti-infliximab antibodies measured by fluid-phase radioimmunoassays as predictors of clinical efficacy of infliximab in Crohn's disease. Am J Gastroenterol. 2008;103:944–948. doi: 10.1111/j.1572-0241.2007.01638.x. [DOI] [PubMed] [Google Scholar]
- 39.Allez M, Karmiris K, Louis E, Van Assche G, Ben-Horin S, Klein A, Van der Woude J, Baert F, Eliakim R, Katsanos K, Brynskov J, Steinwurz F, Danese S, Vermeire S, Teillaud JL, Lémann M, Chowers Y. Report of the ECCO pathogenesis workshop on anti-TNF therapy failures in inflammatory bowel diseases: definitions, frequency and pharmacological aspects. J Crohns Colitis. 2010;4:355–366. doi: 10.1016/j.crohns.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 40.Weisshof R, Ungar B, Blatt A, Dahan A, Pressman S, Waterman M, Kopylov U, Ben-Horin S, Chowers Y. Anti-infliximab Antibodies with Neutralizing Capacity in Patients with Inflammatory Bowel Disease: Distinct Clinical Implications Revealed by a Novel Assay. Inflamm Bowel Dis. 2016;22:1655–1661. doi: 10.1097/MIB.0000000000000797. [DOI] [PubMed] [Google Scholar]
- 41.Reinhold I, Blümel S, Schreiner J, Boyman O, Bögeholz J, Cheetham M, Rogler G, Biedermann L, Scharl M. Clinical Relevance of Anti-TNF Antibody Trough Levels and Anti-Drug Antibodies in Treating Inflammatory Bowel Disease Patients. Inflamm Intest Dis. 2021;6:38–47. doi: 10.1159/000511296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gonczi L, Kurti Z, Rutka M, Vegh Z, Farkas K, Lovasz BD, Golovics PA, Gecse KB, Szalay B, Molnar T, Lakatos PL. Drug persistence and need for dose intensification to adalimumab therapy; the importance of therapeutic drug monitoring in inflammatory bowel diseases. BMC Gastroenterol. 2017;17:97. doi: 10.1186/s12876-017-0654-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ben-Horin S, Chowers Y. Tailoring anti-TNF therapy in IBD: drug levels and disease activity. Nat Rev Gastroenterol Hepatol. 2014;11:243–255. doi: 10.1038/nrgastro.2013.253. [DOI] [PubMed] [Google Scholar]
- 44.Bian S, Dreesen E, Tang HT, Compernolle G, Peeters M, Van Assche G, Ferrante M, Vermeire S, Gils A. Antibodies Toward Vedolizumab Appear from the First Infusion Onward and Disappear Over Time. Inflamm Bowel Dis. 2017;23:2202–2208. doi: 10.1097/MIB.0000000000001255. [DOI] [PubMed] [Google Scholar]
- 45.Chiu HY, Chu TW, Cheng YP, Tsai TF. The Association between Clinical Response to Ustekinumab and Immunogenicity to Ustekinumab and Prior Adalimumab. PLoS One. 2015;10:e0142930. doi: 10.1371/journal.pone.0142930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Strand V, Balsa A, Al-Saleh J, Barile-Fabris L, Horiuchi T, Takeuchi T, Lula S, Hawes C, Kola B, Marshall L. Immunogenicity of Biologics in Chronic Inflammatory Diseases: A Systematic Review. BioDrugs. 2017;31:299–316. doi: 10.1007/s40259-017-0231-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Juncadella A, Papamichael K, Vaughn BP, Cheifetz AS. Maintenance Adalimumab Concentrations Are Associated with Biochemical, Endoscopic, and Histologic Remission in Inflammatory Bowel Disease. Dig Dis Sci. 2018;63:3067–3073. doi: 10.1007/s10620-018-5202-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Papamichael K, Cheifetz AS. Therapeutic drug monitoring in inflammatory bowel disease: for every patient and every drug? Curr Opin Gastroenterol. 2019;35:302–310. doi: 10.1097/MOG.0000000000000536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Roblin X, Marotte H, Rinaudo M, Del Tedesco E, Moreau A, Phelip JM, Genin C, Peyrin-Biroulet L, Paul S. Association between pharmacokinetics of adalimumab and mucosal healing in patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol. 2014;12:80–84.e2. doi: 10.1016/j.cgh.2013.07.010. [DOI] [PubMed] [Google Scholar]
- 50.Paul S, Moreau AC, Del Tedesco E, Rinaudo M, Phelip JM, Genin C, Peyrin-Biroulet L, Roblin X. Pharmacokinetics of adalimumab in inflammatory bowel diseases: a systematic review and meta-analysis. Inflamm Bowel Dis. 2014;20:1288–1295. doi: 10.1097/MIB.0000000000000037. [DOI] [PubMed] [Google Scholar]
- 51.Dirks NL, Meibohm B. Population pharmacokinetics of therapeutic monoclonal antibodies. Clin Pharmacokinet. 2010;49:633–659. doi: 10.2165/11535960-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 52.Vande Casteele N, Gils A, Singh S, Ohrmund L, Hauenstein S, Rutgeerts P, Vermeire S. Antibody response to infliximab and its impact on pharmacokinetics can be transient. Am J Gastroenterol. 2013;108:962–971. doi: 10.1038/ajg.2013.12. [DOI] [PubMed] [Google Scholar]
- 53.Papamichael K, Van Stappen T, Vande Casteele N, Gils A, Billiet T, Tops S, Claes K, Van Assche G, Rutgeerts P, Vermeire S, Ferrante M. Infliximab Concentration Thresholds During Induction Therapy Are Associated With Short-term Mucosal Healing in Patients With Ulcerative Colitis. Clin Gastroenterol Hepatol. 2016;14:543–549. doi: 10.1016/j.cgh.2015.11.014. [DOI] [PubMed] [Google Scholar]
- 54.Bortlik M, Duricova D, Malickova K, Machkova N, Bouzkova E, Hrdlicka L, Komarek A, Lukas M. Infliximab trough levels may predict sustained response to infliximab in patients with Crohn's disease. J Crohns Colitis. 2013;7:736–743. doi: 10.1016/j.crohns.2012.10.019. [DOI] [PubMed] [Google Scholar]
- 55.Adedokun OJ, Sandborn WJ, Feagan BG, Rutgeerts P, Xu Z, Marano CW, Johanns J, Zhou H, Davis HM, Cornillie F, Reinisch W. Association between serum concentration of infliximab and efficacy in adult patients with ulcerative colitis. Gastroenterology. 2014;147:1296–1307.e5. doi: 10.1053/j.gastro.2014.08.035. [DOI] [PubMed] [Google Scholar]
- 56.Davidov Y, Ungar B, Bar-Yoseph H, Carter D, Haj-Natour O, Yavzori M, Chowers Y, Eliakim R, Ben-Horin S, Kopylov U. Association of Induction Infliximab Levels With Clinical Response in Perianal Crohn's Disease. J Crohns Colitis. 2017;11:549–555. doi: 10.1093/ecco-jcc/jjw182. [DOI] [PubMed] [Google Scholar]
- 57.Ungar B, Levy I, Yavne Y, Yavzori M, Picard O, Fudim E, Loebstein R, Chowers Y, Eliakim R, Kopylov U, Ben-Horin S. Optimizing Anti-TNF-α Therapy: Serum Levels of Infliximab and Adalimumab Are Associated With Mucosal Healing in Patients With Inflammatory Bowel Diseases. Clin Gastroenterol Hepatol. 2016;14:550–557.e2. doi: 10.1016/j.cgh.2015.10.025. [DOI] [PubMed] [Google Scholar]
- 58.Strik AS, Löwenberg M, Buskens CJ, B Gecse K, I Ponsioen C, Bemelman WA, D'Haens GR. Higher anti-TNF serum levels are associated with perianal fistula closure in Crohn's disease patients. Scand J Gastroenterol. 2019;54:453–458. doi: 10.1080/00365521.2019.1600014. [DOI] [PubMed] [Google Scholar]
- 59.Bouguen G, Siproudhis L, Gizard E, Wallenhorst T, Billioud V, Bretagne JF, Bigard MA, Peyrin-Biroulet L. Long-term outcome of perianal fistulizing Crohn's disease treated with infliximab. Clin Gastroenterol Hepatol. 2013;11:975–81.e1. doi: 10.1016/j.cgh.2012.12.042. [DOI] [PubMed] [Google Scholar]
- 60.Colombel F, Panés J, D’Haens G, Schreiber S, Panaccione R, Peyrin-Biroulet L, Loftus E, Danese S, Louis E, Armuzzi A, Ferrante M, Vogelsang H, Lefebvre J, Doan T, Xie W, Huang B, Petersson J, Kalabic J, Robinson A, Sandborn W. OP01 Higher vs. standard adalimumab maintenance regimens in patients with moderately to severely active ulcerative colitis: Results from the SERENE-UC maintenance study. J Crohns Colitis. 2020;14:S001–S001. [Google Scholar]
- 61.D’Haens G SW, Loftus Jr E, Hanauer SB, Peyrin-Biroulet L, Panaccione R, Panes J, Colombel JF, Ferrante M, Louis E, Armuzzi A, Zhou Q, Huang B, Kwatra NV, Mostafa NM, Doan T, Petersson J, Song A, Anne M. High vs standard adalimumab induction dosing regimens in patients with moderately to severely active Crohn’s disease: results from the SERENE-CD induction study. United European Gastroenterol J. 2019;7 [Google Scholar]
- 62.Velayos FS, Kahn JG, Sandborn WJ, Feagan BG. A test-based strategy is more cost effective than empiric dose escalation for patients with Crohn's disease who lose responsiveness to infliximab. Clin Gastroenterol Hepatol. 2013;11:654–666. doi: 10.1016/j.cgh.2012.12.035. [DOI] [PubMed] [Google Scholar]
- 63.Kelly OB, Donnell SO, Stempak JM, Steinhart AH, Silverberg MS. Therapeutic Drug Monitoring to Guide Infliximab Dose Adjustment is Associated with Better Endoscopic Outcomes than Clinical Decision Making Alone in Active Inflammatory Bowel Disease. Inflamm Bowel Dis. 2017;23:1202–1209. doi: 10.1097/MIB.0000000000001126. [DOI] [PubMed] [Google Scholar]
- 64.Restellini S, Chao CY, Lakatos PL, Aruljothy A, Aziz H, Kherad O, Bitton A, Wild G, Afif W, Bessissow T. Therapeutic Drug Monitoring Guides the Management of Crohn's Patients with Secondary Loss of Response to Adalimumab. Inflamm Bowel Dis. 2018;24:1531–1538. doi: 10.1093/ibd/izy044. [DOI] [PubMed] [Google Scholar]
- 65.Guidi L, Pugliese D, Panici Tonucci T, Berrino A, Tolusso B, Basile M, Cantoro L, Balestrieri P, Civitelli F, Bertani L, Marzo M, Felice C, Gremese E, Costa F, Viola F, Cicala M, Kohn A, Gasbarrini A, Rapaccini GL, Ruggeri M, Armuzzi A. Therapeutic Drug Monitoring is More Cost-Effective than a Clinically Based Approach in the Management of Loss of Response to Infliximab in Inflammatory Bowel Disease: An Observational Multicentre Study. J Crohns Colitis. 2018;12:1079–1088. doi: 10.1093/ecco-jcc/jjy076. [DOI] [PubMed] [Google Scholar]
- 66.Steenholdt C, Brynskov J, Thomsen OØ, Munck LK, Fallingborg J, Christensen LA, Pedersen G, Kjeldsen J, Jacobsen BA, Oxholm AS, Kjellberg J, Bendtzen K, Ainsworth MA. Individualised therapy is more cost-effective than dose intensification in patients with Crohn's disease who lose response to anti-TNF treatment: a randomised, controlled trial. Gut. 2014;63:919–927. doi: 10.1136/gutjnl-2013-305279. [DOI] [PubMed] [Google Scholar]
- 67.Afif W, Loftus EV Jr, Faubion WA, Kane SV, Bruining DH, Hanson KA, Sandborn WJ. Clinical utility of measuring infliximab and human anti-chimeric antibody concentrations in patients with inflammatory bowel disease. Am J Gastroenterol. 2010;105:1133–1139. doi: 10.1038/ajg.2010.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ungar B, Mazor Y, Weisshof R, Yanai H, Ron Y, Goren I, Waizbard A, Yavzori M, Fudim E, Picard O, Loebstein R, Kopylov U, Dotan I, Chowers Y, Eliakim R, Ben-Horin S. Induction infliximab levels among patients with acute severe ulcerative colitis compared with patients with moderately severe ulcerative colitis. Aliment Pharmacol Ther. 2016;43:1293–1299. doi: 10.1111/apt.13631. [DOI] [PubMed] [Google Scholar]
- 69.Ma C, Battat R, Jairath V, Vande Casteele N. Advances in Therapeutic Drug Monitoring for Small-Molecule and Biologic Therapies in Inflammatory Bowel Disease. Curr Treat Options Gastroenterol. 2019;17:127–145. doi: 10.1007/s11938-019-00222-9. [DOI] [PubMed] [Google Scholar]
- 70.Danese S SW, Loftus EV, Hanauer S, Schreiber S, Peyrin-Biroulet L, Panaccione R, Panes J, Baert F, Colombel JF, Ferrante M, Louis E, Armuzzi A, Goteti VS, Mostafa N, Doan T, Petersson J, Robinson A, Song A, D’Haens GR. Clinically Adjusted vs Therapeutic Drug Monitoring Dosing Regimens With Adalimumab in Patients With Moderately to Severely Active Crohn’s Disease: Results From the SERENE-CD Maintenance Study. United European Gastroenterol. 2020 [Google Scholar]
- 71.Bossuyt P, Pouillon L, Claeys S, D'Haens S, Hoefkens E, Strubbe B, Marichal D, Peeters H. Ultra-proactive therapeutic drug monitoring of infliximab based on point-of-care-testing in inflammatory bowel disease: results of a pragmatic trial. J Crohns Colitis. 2021;23:jjab127. doi: 10.1093/ecco-jcc/jjab127. [DOI] [PubMed] [Google Scholar]
- 72.Govani S, Waljee A, Stidham R, Higgins P, Hardiman K. 516 Accelerated Dosing of Infliximab Prevents Colectomy Within 90 Days in Only Half of Patients With Severe Ulcerative Colitis. Gastroenterology. 2016;150:S106. [Google Scholar]
- 73.Papamichael K, Chachu KA, Vajravelu RK, Vaughn BP, Ni J, Osterman MT, Cheifetz AS. Improved Long-term Outcomes of Patients With Inflammatory Bowel Disease Receiving Proactive Compared With Reactive Monitoring of Serum Concentrations of Infliximab. Clin Gastroenterol Hepatol. 2017;15:1580–1588.e3. doi: 10.1016/j.cgh.2017.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Perinbasekar R, Brown S, Syed N, Lonsako S, Cross R. Proactive Monitoring of Infliximab (IFX) and Adalimumab (ADA) Using LabCorp's Electrochemiluminescence Assay (ECLIA) in Inflammatory Bowel Disease Patients: 719. Official J the Am College Gastroenterol. 2017;112:S397. [Google Scholar]
- 75.Bernardo S, Fernandes S, Gonçalves AR, Baldaia C, Valente A, Santos P, Araújo-Correia L, Velosa J. P453 Efficacy of therapeutic drug monitoring of anti-TNF therapy in the control of patients with inflammatory bowel disease. J Crohns Colitis. 2017;11:S308–S309. [Google Scholar]
- 76.Strik A, Berends S, Mould D, Mathôt R, Ponsioen C, van den Brande J, Jansen J, Hoekman D, Brandse J, Löwenberg M, D'Haens G. DOP56 Dashboard driven vs. conventional dosing of infliximab in inflammatory bowel disease patients: the PRECISION trial. J Crohns Colitis. 2019;13(Supplement_1):S063–S063. [Google Scholar]
- 77.Pouillon L, Ferrante M, Van Assche G, Rutgeerts P, Noman M, Sabino J, Vande Casteele N, Gils A, Vermeire S. Mucosal Healing and Long-term Outcomes of Patients With Inflammatory Bowel Diseases Receiving Clinic-Based vs Trough Concentration-Based Dosing of Infliximab. Clin Gastroenterol Hepatol. 2018;16:1276–1283.e1. doi: 10.1016/j.cgh.2017.11.046. [DOI] [PubMed] [Google Scholar]
- 78.Roblin X, Rinaudo M, Del Tedesco E, Phelip JM, Genin C, Peyrin-Biroulet L, Paul S. Development of an algorithm incorporating pharmacokinetics of adalimumab in inflammatory bowel diseases. Am J Gastroenterol. 2014;109:1250–1256. doi: 10.1038/ajg.2014.146. [DOI] [PubMed] [Google Scholar]
- 79.Papamichael K, Cheifetz AS, Melmed GY, Irving PM, Vande Casteele N, Kozuch PL, Raffals LE, Baidoo L, Bressler B, Devlin SM, Jones J, Kaplan GG, Sparrow MP, Velayos FS, Ullman T, Siegel CA. Appropriate Therapeutic Drug Monitoring of Biologic Agents for Patients With Inflammatory Bowel Diseases. Clin Gastroenterol Hepatol. 2019;17:1655–1668.e3. doi: 10.1016/j.cgh.2019.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ward MG, Sparrow MP, Roblin X. Therapeutic drug monitoring of vedolizumab in inflammatory bowel disease: current data and future directions. Therap Adv Gastroenterol. 2018;11:1756284818772786. doi: 10.1177/1756284818772786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Berends S, Löwenberg M, Baert F, Mathôt R, Clasquin E, Woude C, Hoentjen F, Bossuyt P, Franchimont D, Rispens T, de Vries A, Vermeire S, D'Haens G. DOP046 Higher serum concentrations of vedolizumab are associated with superior endoscopic outcomes in Crohn’s disease: data from the LOVE-CD trial. J Crohns Colitis. 2018;12:S063–S063. [Google Scholar]
- 82.Löwenberg M, Vermeire S, Mostafavi N, Hoentjen F, Franchimont D, Bossuyt P, Hindryckx P, Rispens T, de Vries A, van der Woude CJ, Berends S, Ambarus CA, Mathot R, Clasquin E, Baert F, D'Haens G. Vedolizumab Induces Endoscopic and Histologic Remission in Patients With Crohn's Disease. Gastroenterology. 2019;157:997–1006.e6. doi: 10.1053/j.gastro.2019.05.067. [DOI] [PubMed] [Google Scholar]
- 83.Syversen SW, Goll GL, Jørgensen KK, Olsen IC, Sandanger Ø, Gehin JE, Warren DJ, Sexton J, Mørk C, Jahnsen J, Kvien TK, Bolstad N, Haavardsholm EA. Therapeutic drug monitoring of infliximab compared to standard clinical treatment with infliximab: study protocol for a randomised, controlled, open, parallel-group, phase IV study (the NOR-DRUM study) Trials. 2020;21:13. doi: 10.1186/s13063-019-3734-4. [DOI] [PMC free article] [PubMed] [Google Scholar]