Abstract
Background:
As marijuana is legalized in more states, modes of administration that facilitate co-use with tobacco are growing in popularity among young adults. This study examines the prevalence, patterns, correlates, and reasons for co-use so that targeted interventions can be developed to prevent negative consequences associated with tobacco use and co-use.
Methods:
In Fall 2019, 1887 young adults, originally recruited in 2010 from 11 colleges in North Carolina and Virginia to participate in a cohort study, completed an online survey. Co-use was defined as self-reported use of marijuana and tobacco in the past month. Tobacco-only, marijuana-only and co-users were compared using regression modeling.
Results:
Overall, 9.3% of the sample were co-users, 7.1% tobacco-only, and 15.8% marijuana-only users. Tobacco use was associated with an increased likelihood of marijuana use and vice-versa. Co-users were more likely to use e-cigarettes and blunts to administer marijuana and less likely to use smokeless tobacco products. They were more likely to use cocaine, have less anxiety, and be heavier marijuana users than marijuana-only users. Co-users of e-cigarettes and marijuana were less likely to be daily e-cigarette users and make quit attempts than e-cigarette users that did not use marijuana. Experimentation was the primary reason for co-use of tobacco and marijuana.
Conclusions:
Co-users were more likely to use modes of administration that facilitate use of both substances and have patterns of use that may impact cessation efforts. These findings highlight the importance of surveillance of co-use and the development of interventions targeting experimentation with these substances by young adults.
Keywords: cannabis, co-use, marijuana, tobacco, young adults
1. Introduction
Rates of cigarette smoking are at an all-time low in the US. In 2019, 8.0% of young adults aged 18–24 were current cigarette smokers compared to 18.5% in 2014, representing a 57% decrease in smoking (Cornelius et al. 2020; Jamal et al. 2015). Rates of cigarette smoking also declined, but to a lesser degree, among adults aged 25–44, from 22.9% to 16.7%. Although cigarette smoking rates are at an all-time low, 18.2% of young adults aged 18–24 and 25.3% of adults aged 25–44 report current use of any tobacco product (Cornelius et al. 2020). Poly-tobacco use is also common (28.6% of 18–24 and 21.7% of 25–44-year-old tobacco users) with cigarettes and e-cigarettes the most prevalent tobacco product combination.
Co-use of tobacco with marijuana is also common. Among adults, 25.7% of tobacco users reported past-month use of marijuana compared to only 5.3% of non-tobacco users (Schauer et al. 2015). Data from the nationally representative Population Assessment of Tobacco and Health (PATH) study found that 21.3% of young adults ages 18–24 reported past-month use of marijuana and at least one tobacco product (Cohn et al. 2019). While rates of co-use are lower among those aged 26–34, national data show a significant increase from 6.6% to 8.0% between 2003–2012 (Schauer et al. 2015). While co-use typically refers to the use of both products within the past 30 days, it can also include co-administration (e.g., blunts, e-cigarettes/vaporizers) or sequential administration (e.g., ‘chasing’ marijuana with tobacco).
The development of new drug delivery systems for tetrahydrocannabinol (THC), the psychoactive component in marijuana, that parallel alternative drug delivery systems for nicotine (e.g., e-cigarettes) and facilitate the use of both products may explain these increases in co-use. For example, an e-cigarette may deliver nicotine on one occasion and THC on another or both simultaneously via the mixing of e-liquids. In fact, data from PATH found co-users are more likely to use e-cigarettes and little cigars and cigarillos (LCCs) (Cohn et al. 2019), and 80% of lifetime marijuana users reported using a tobacco product or device to administer marijuana (Seaman et al. 2020).
There is also increasing evidence that marijuana use increases the risk for tobacco initiation and nicotine dependence (Cornacchione-Ross et al. 2020; Weinberger et al. 2020; Cohn et al. 2018; Agrawal et al. 2011; Agrawal et al. 2008; Okoli et al. 2008; Patton et al. 2005). Recent studies find lower rates of sustained abstinence and fewer quit attempts among co-users (Strong et al. 2018; Vogel et al. 2018; Weinberger et al. 2020; Weinberger et al. 2018). Tobacco use has also been shown to be associated with an increased risk of marijuana use and dependence (Peters et al. 2012; Agrawal et al. 2009). A recent study found that daily marijuana use occurs almost exclusively among cigarette smokers (Goodwin et al. 2018). Additionally, co-use has been associated with greater prevalence of psychiatric and psychosocial problems (Seaman et al. 2020; Stewart et al. 2020; Peters et al. 2014; Ramo et al. 2012).
Despite these negative health effects, research on reasons for co-use to help inform interventions is limited. In one study, college students reported smoking to prolong the effects of marijuana (Ramo and Prochaska 2012). Others report tobacco and marijuana may be used in combination to attenuate each other’s undesirable effects, in particular withdrawal symptoms (Haney et al. 2013; Budney et al. 2008; Vandrey et al. 2008). Marijuana users in particular report using tobacco to attenuate cognitive impairment associated with marijuana use (Rabin and George 2015). Understanding the motives underlying co-use is critical for developing interventions but these have not been well-studied, especially for non-cigarette tobacco products and new modes of marijuana administration. The aims of this study are to examine the (1) prevalence and patterns of co-use by type of tobacco product and mode of marijuana administration, (2) demographic and psychosocial correlates, and (3) reasons for co-use in a sample of young adults to provide information that is needed for the development of targeted interventions in this population. We hypothesize that co-users will use products that facilitate co-use and have patterns of behavior that may impact cessation efforts.
2. Methods
2.1. Sample
Data are from a cohort of young adults who participated in the ACE (Assessment of the College Experience) and ACE II (Assessment of the Post-College Experience) studies. The goal of ACE was to assess smokeless tobacco (SLT) trajectories and their correlates in a cohort of college students (Wolfson et al. 2015). In Fall 2010, 3146 students were recruited as freshman from 11 colleges in the Southeast. Lifetime SLT users, past month cigarette smokers, and males were oversampled. More detail on initial study recruitment is described elsewhere (Spangler et al. 2018). ACE II focuses on the use of all tobacco products during the transition to adulthood following the same cohort. Data were collected at least annually from 2010 to 2020 using a web-based survey. The present study analyzes data from Fall 2019. The study protocol was approved by the study institutions’ Institutional Review Board and additional privacy protection was provided by obtaining a Certificate of Confidentiality from the U.S. Department of Health and Human Services.
2.2. Measures
2.2.1. Tobacco use
The survey assessed ever use of six tobacco products: cigarettes, e-cigarettes or other vaping devices, smokeless tobacco (i.e., chew, dip, snuff, snus, dissolvables), waterpipe (also called a hookah), large cigars, and little cigars or cigarillos (LCCs). The question stem was “Have you ever used/smoked [product]?” For combustible products, the sentence ended with “even one or two puffs”. However, for cigarettes the question stem was “Have you ever smoked a whole cigarette?” Response options for each product were “Yes, in the past week”, “Yes in the past 30 days, but more than a week ago”, “Yes, in the past 6 months, but more than 30 days ago”, “Yes in the past year, but more than 6 months ago”, “Yes, more than a year ago”, and “No, never”. Young adults who reported “Yes, in the past week” and “Yes in the past 30 days, but more than a week ago” were considered current tobacco users for that product. Current users were asked “In the past 30 days, on how many days did you smoke/use [product]?” with response options of 1–2 days, 3–5 days, 6–9 days, 10–14 days, 15–19 days, 20–29 days, and all 30 days.
2.2.2. Marijuana use
Marijuana use was measured by asking respondents if they had used marijuana in the past six months. Respondents who responded yes were asked how many days out of the past 30 they used marijuana, with the following response options: 0 days, 1–2 days, 3–5 days, 6–9 days, 10–19 days, 20–29 days, and all 30 days. Participants were considered current marijuana users if they reported using marijuana at least once in the past 30 days. Current marijuana users were then asked, “In the past 30 days, how did you use marijuana? Please check all that apply.” Responses included “I smoked it in a rolling paper (joint), bowl or bong”, “I ate it in an edible, candy, tincture or other food”, “I smoked it in a blunt (i.e., marijuana in a cigar, little cigar or cigarillo wrapper)”, “I used an e-cigarette or vaporizer”, “I used dabs (i.e., heating a marijuana concentrate and inhaling the vapor)”, and “I smoked it in a waterpipe/hookah”.
2.2.2. Co-use, frequency of use, and quit behaviors.
Respondents who reported using any tobacco product in the past 30 days and using marijuana in the past 30 days were considered co-users of tobacco and marijuana. The mean number of days using a product was calculated by assigning the response to the midpoint of the response category. For each tobacco product separately, we defined daily use as using the product all 30 days. For marijuana, we defined daily or near-daily use as using marijuana on 20 or more days, consistent with national surveys. We did not collect data on days used marijuana separately for each mode of administration. For each tobacco product, current users were asked if they are seriously thinking of quitting and if they have tried to quit in the past 6 months. Cigarette users were asked if they considered themselves smokers. Respondents were asked the age when they first tried each product.
2.2.3. Reasons for co-use
Reasons for co-use of tobacco and marijuana were assessed using a scale developed by Berg et al. (2018). Respondents were asked about their reasons for co-use with response options ranging from 1=not at all true for me, to 6=extremely true for me. Responses were averaged to create four subscales: 1) Instrumentality, indicating that co-use was related to physical sensations (e.g. using tobacco increases the buzz I get from marijuana); 2) Displacement, indicating the use of one product to reduce or quit the use of another or using marijuana when tobacco is not available (e.g. I’ve tried to reduce my use of marijuana by replacing it with tobacco); 3) Social Context, indicating the use of different products in different social contexts (e.g. using marijuana or tobacco in different places or with different people); 4) Experimentation, indicating experimental use of these products but no specific link to their use (e.g. the use of one product has nothing to do with the use of the other).
2.2.4. Psychosocial factors
Stress was measured using the Perceived Stress Scale (Cohen et al. 1983). Scores were computed by summing 10 items on a scale from 0=never to 4=very often. Depressive symptoms were measured using the Center for Epidemiological Studies Depression (CESD) Iowa Short Form (Kohout et al. 1993). The scale includes 11 items with response options ranging from 1=rarely or none of the time (less than 1 day) to 4=most or all of the time (5–7 days). Scores were calculated for both scales by summing the items, reverse coding items where appropriate. If one or two items were missing responses, the mean of the other items was substituted in place of the missing item. Anxiety was measured using the PROMIS anxiety scale (Pilkonis et al. 2011). The scale includes 4 times with response options ranging from 1=never to 5=always. Scores were calculated by summing the items. If any item was missing, the score was not calculated. Higher scores on each scale indicate more symptoms of stress, depression, and anxiety.
2.2.5. Other substance use
Respondents were asked how many days out of the past 30 they used cocaine, and ADHD (e.g., Ritalin, Dexedrine, Adderall, Concerta, methylphenidate) or pain medication (e.g., Vicodin, Lortab, Percocet, OxyContin) without a doctor’s prescription or for reasons other than for what they were prescribed. Response options were 0 days, 1–2 days, 3–5 days, 6–9 days, 10–19 days, 20–29 days, and all 30 days. Participants were considered current users if they reported using a substance at least once in the past 30 days. They were also asked in the past 30 days, how many days they had five or more drinks in a row for males and four or more drinks for females. Reports of this behavior on one or more days were considered positive for binge drinking.
2.2.6. Demographics
Demographic characteristics included age, sex, race, ethnicity, sexual orientation, employment status, marital status, and mother’s education.
2.3. Statistical analysis
Descriptive statistics characterized demographic characteristics of the sample and prevalence of tobacco and marijuana use and co-use. Types of tobacco products used, modes of marijuana administration, and demographic and other substance use behaviors were compared between co-users of tobacco and marijuana, marijuana-only, and tobacco-only users using chi-squared tests while continuous psychosocial factors were compared using F-tests. Multivariable generalized logistic regression examined the adjusted association between demographic characteristics, other substance use, and psychosocial factors and the likelihood of co-use of tobacco and marijuana relative to using tobacco or marijuana-only. Odds ratios and 95% confidence intervals and p-values from individual t-tests are presented. Next, we compared marijuana use behaviors between marijuana-only and co-users of marijuana and tobacco using t-tests for continuous variables and chi-square tests for binary variables. Tobacco use behaviors were examined for each tobacco product separately. For example, we compared cigarette smoking behaviors for past 30-day cigarette users (cigarette only) compared to past 30-day cigarette users that used marijuana in the past 30-days (co-users of cigarettes and marijuana). Tobacco product-specific analyses did not exclude users of other tobacco products, e.g., cigarette only users may also use e-cigarettes. Very few waterpipe, large cigar, and LCC users reported daily use, or thinking about or trying to quit the use of these products so these data are not shown. In the subsample of co-users of tobacco and marijuana, reasons for co-use were estimated for each subscale and linear regression models were fit separately for each subscale as a function of current tobacco product use. All analyses were performed using the survey sampling procedures in SAS V9.4 to account for the oversampling of males and tobacco users at baseline. All tests were two-sided with a 0.05 level of significance.
3. Results
3.1. Sample demographics
Of the 1908 young adults completing a survey in Fall 2019, 1887 had data on marijuana and tobacco use for analysis. The sample was 65% female, 84% White, 6% Hispanic, and 14% identified as lesbian, gay, or bisexual (LGB) with a mean age of 27.2 years (sd=0.5). More than 80% were employed full time and 31% were married.
3.2. Prevalence of tobacco and marijuana use and co-use
The prevalence of use of any tobacco product in the past month was 16.3%. Among current tobacco users, 26.1% reported the use of two or more tobacco products. The most common tobacco product used was e-cigarettes (49.0%) followed by cigarettes (38.9%), large cigars (13.7%), SLT (11.7%), waterpipe (11.6%) and LCCs (7.9%). Current marijuana use was reported by 25.0% of the sample with smoking marijuana in a joint, bowl, or bong the most common mode of administration (61.9%) followed by vaping (40.0%), ingesting edibles (33.2%), smoking blunts (15.0%), dabbing (9.5%) and using a waterpipe (4.5%). Co-use of tobacco and marijuana was reported by 9.3% of the sample while 7.1% used tobacco-only and 15.8% used marijuana-only. Among tobacco users, 57% reported using marijuana in the past 30 days compared to 18.9% of non-tobacco users (p<0.0001) while 37% of marijuana users reported using tobacco in the past 30 days compared to 9.4% of non-marijuana users (p<0.0001).
3.3. Tobacco product types and modes of marijuana administration
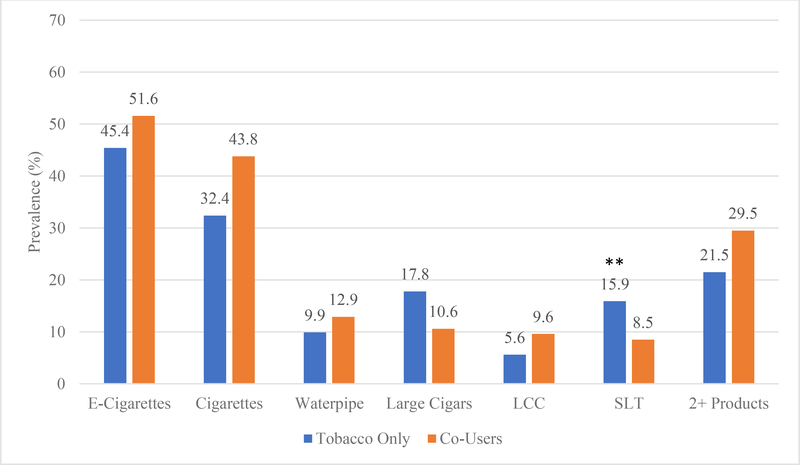
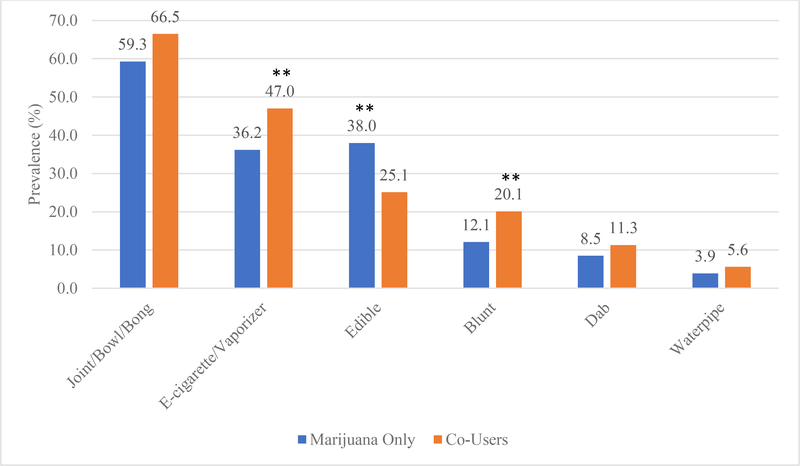
As shown in Figure 1, e-cigarettes were the most common tobacco product used by both tobacco-only and co-users of tobacco and marijuana followed by cigarettes. Although rates of e-cigarette use were higher among co-users of tobacco and marijuana compared to tobacco-only users (51.6% vs 45.4%) the differences were not statistically significant. Tobacco-only users, however, were significantly more likely to use SLT compared to tobacco and marijuana co-users (15.9% vs 8.5%; p=0.037). As shown in Figure 2, smoking marijuana in a joint, bowl or bong was the most prevalent mode of administration for co-users of tobacco and marijuana and marijuana-only users. Co-users of tobacco and marijuana were significantly more likely to vape marijuana (47.0% vs 36.2%; p=0.044) and smoke blunts (20.1% vs 12.1%; p=0.031) compared to marijuana-only users; marijuana-only users were significantly more likely to consume edibles compared to co-users of tobacco and marijuana (38.0% vs 25.1%; p=0.007).
Figure 1.
Tobacco Product Use for Co-Users and Tobacco Only Users
**p<0.05
Figure 2.
Modes of Marijuana Administration for Co-Users and Marijuana Only Users
**p<0.05
3.4. Demographic and psychosocial correlates
In fully adjusted models, co-users of tobacco and marijuana were significantly more likely to be male (aOR=1.68; 95% CI=1.02, 2.78), LGB (aOR=2.25; 95% CI=1.17, 4.34), binge drinkers (aOR=1.90; 95% CI=1.10, 3.31) and cocaine users (aOR=5.40; 95% CI=2.14, 13.6) and to have lower anxiety levels (aOR=0.88; 95% CI=0.77, 0.99) compared to marijuana-only users. Compared to tobacco-only users, co-users of tobacco and marijuana were significantly more likely to be cocaine users (aOR=5.24; 95% CI=1.91, 14.4). Tobacco-only users were significantly more likely to be male (aOR=2.63; 95%CI=1.57, 4.41) and less likely to be Hispanic (aOR=0.22; 95%CI=0.08, 0.64), and have marginally lower anxiety scores (aOR=0.88, 0.78, 1.00) compared to marijuana-only users (data not shown in table).
3.5. Tobacco and marijuana use behaviors
As shown in Table 2, co-users of tobacco and marijuana were more likely to be daily or near-daily marijuana users (30.6% vs 19.8%; p=0.015), use marijuana on more days (11.9 vs 9.3; p=0.023) and have a younger age of first use (18.1 vs 19.6; p<0.001) compared to marijuana-only users. In analyses of specific tobacco products, cigarette users that also used marijuana were significantly less likely to consider themselves smokers (27.4% vs 51.3%; p=0.009) compared to cigarette users that did not use marijuana. E-cigarette users that used marijuana were significantly less likely to be daily e-cigarette users (18.5% vs 37.0%, p=0.015), think about quitting e-cigarettes (26.8% vs 56.6%; p<0.001) and tried quitting e-cigarettes (10.6% vs 27.6%; p=0.006) compared to e-cigarettes users that did not use marijuana. Waterpipe users that used marijuana started using waterpipe at a significantly younger age than waterpipe users that did not use marijuana (18.5 vs 20.8, p=0.039), and LCC users that used marijuana used LCCs on significantly more days compared to LCC users that did not use marijuana (9.3 vs 3.0, p=0.040).
Table 2.
Marijuana and Tobacco Behaviors by Tobacco and Marijuana User Group.1
| Marijuana Behaviors | Marijuana Only N (%) or Mean (SE) N=307 |
Tobacco and Marijuana2 N (%) or Mean (SE) N=231 |
p-value |
| Days used marijuana | 9.3 (0.6) | 11.9 (0.9) | 0.023 |
| Daily or near-daily marijuana use | 74 (19.8) | 74 (30.6) | 0.015 |
| Age first used marijuana | 19.6 (0.2) | 18.1 (0.2) | <0.001 |
| Tobacco Behaviors by Tobacco Product Type | Tobacco Only3 N (%) or Mean (SE) |
Tobacco and Marijuana4 N (%) or Mean (SE) |
p-value |
| Cigarettes | N=65 | N=115 | |
| Days smoked cigarettes | 11.2 (1.7) | 8.9 (1.1) | 0.246 |
| Daily smoker | 15 (21.2) | 14 (10.5) | 0.086 |
| Consider self a smoker | 29 (51.3) | 34 (27.4) | 0.009 |
| Ever think about quitting | 36 (57.1) | 56 (50.5) | 0.491 |
| Ever tried to quit | 19 (37.5) | 40 (38.1) | 0.955 |
| Age first smoked cigarettes | 16.4 (0.5) | 17.1 (0.3) | 0.283 |
| E-cigarettes | N=81 | N=133 | |
| Days used e-cigarettes | 15.7 (1.8) | 11.6 (1.3) | 0.068 |
| Daily e-cigarette users | 25 (37.0) | 25 (18.8) | 0.015 |
| Ever think about quitting | 46 (56.6) | 45 (26.8) | <0.001 |
| Ever tried to quit | 21 (27.6) | 18 (10.6) | 0.006 |
| Age first tried e-cigarettes | 23.1 (0.4) | 22.3 (0.3) | 0.096 |
| Smokeless tobacco (SLT) | N=35 | N=22 | |
| Days used SLT | 11.8 (1.8) | 13.1 (3.3) | 0.727 |
| Daily SLT user | 5 (12.0) | 3 (24.1) | 0.301 |
| Ever think about quitting | 19 (55.7) | 13 (54.4) | 0.936 |
| Ever tried to quit | 12 (35.9) | 8 (32.5) | 0.817 |
| Age first tried SLT | 17.4 (0.4) | 17.9 (0.8) | 0.548 |
| Large Cigars5 | N=32 | N=28 | |
| Days used cigars | 1.5 (0.0) | 1.7 (0.2) | 0.336 |
| Age first tried large cigars | 19.4 (0.7) | 17.8 (0.7) | 0.123 |
| Waterpipe5 | N=15 | N=22 | |
| Days used waterpipe | 2.9 (0.7) | 2.4 (0.8) | 0.620 |
| Age first tried waterpipe | 20.8 (0.9) | 18.5 (0.5) | 0.039 |
| Little Cigarillos/Cigarillos (LCC)4 | N=12 | N=19 | |
| Days used LCCs | 3.0 (0.6) | 9.3 (2.9) | 0.040 |
| Age first tried LCC | 21.4 (1.1) | 19.2 (1.0) | 0.153 |
Ns are unweighted. Prevalences and means are weighted.
Co-use of marijuana with any tobacco product.
Use of the listed tobacco product does not exclude use of other tobacco products.
Co-use of marijuana with the listed tobacco product does not exclude use of other tobacco products.
None to few daily users, thinking of quitting or quit attempts reported for this tobacco product.
3.6. Reasons for co-use
Finally, as seen in Table 3, among co-users of tobacco and marijuana, mean scores for reasons for co-use were greatest for experimentation (M=4.05, SE=0.11) followed by social context (M=2.73, SE=0.13), instrumentality (M=1.83, SE=0.08) and displacement (M=1.28, SE=0.05). Co-users of tobacco and marijuana who smoked cigarettes (β=0.51, p=0.001) and LCCs (β=0.85, p=0.049) reported significantly higher scores on the instrumentality subscale compared to co-users of tobacco and marijuana that did not use these specific tobacco products while co-users that smoked cigarettes also reported significantly higher scores on the displacement subscale (β=0.30, p=0.005). Co-users of tobacco and marijuana who used waterpipe reported significantly lower scores on the social context subscale compared to co-users of tobacco and marijuana that did not use waterpipe (β=−0.74, p=0.027).
Table 3.
Multivariable linear regression model of type of tobacco use on reasons for co-use with marijuana.
| Instrumentality | Displacement | Social Context | Experimentation | |
|---|---|---|---|---|
| Overall Mean (SE) | 1.83 (0.08) | 1.28 (0.05) | 2.73 (0.13) | 4.05 (0.11) |
| Tobacco Product Use | Beta (SD) p-value |
Beta (SD) p-value |
Beta (SD) p-value |
Beta (SD) p-value |
| Cigarettes |
0.51 (0.16)
0.001 |
0.30 (0.11)
0.005 |
0.50 (0.26) 0.058 |
−0.04 (0.20) 0.837 |
| E-Cigarettes | 0.07 (0.17) 0.677 |
−0.001 (0.13) 0.991 |
0.45 (0.26) 0.085 |
−0.02 (0.22) 0.907 |
| Waterpipe | −0.07 (0.28) 0.812 |
−0.09 (0.14) 0.513 |
−0.74 (0.33)
0.027 |
−0.24 (0.39) 0.536 |
| LCC |
0.85 (0.43)
0.049 |
0.32 (0.24) 0.168 |
0.89 (0.54) 0.102 |
0.16 (0.24) 0.499 |
| Large Cigar | −0.14 (0.19) 0.450 |
−0.05 (0.12) 0.648 |
−0.23 (0.34) 0.499 |
0.12 (0.28) 0.671 |
| SLT | −0.10 (0.21) 0.643 |
−0.05 (0.21) 0.800 |
−0.21 (0.43) 0.624 |
−0.22 (0.35) 0.531 |
4.0. Discussion
In this study of young adults, we found cross-sectional evidence that the use of tobacco or marijuana may increase the risk of use of the other product as well as evidence that co-users of tobacco and marijuana are more likely to use modes of administration that facilitate the use of both products and have patterns of use and other comorbidities that could impact cessation efforts.
More than half of tobacco users reported using marijuana in the past month and almost half of marijuana users reported using a tobacco product; rates more than twice that of non-users. Co-users of tobacco and marijuana had slightly higher rates of non-cigarette tobacco product use as found in other studies (Cohn et al. 2019; Masters et al. 2018) and tobacco-only users were significantly more likely to use traditional tobacco products like SLT and large cigars. There was some evidence that co-users of tobacco and marijuana were more likely to use multiple tobacco products as found in PATH (Osibogun et al. 2018), but the lack of significant findings may reflect increasing experimentation with multiple tobacco products among young adults regardless of the use of other products like marijuana. In terms of marijuana administration, co-users of tobacco and marijuana were significantly more likely to use e-cigarettes and blunts to deliver THC, devices that can also deliver nicotine, than marijuana-only users. However, only 5% of co-users that vaped marijuana reported mixing nicotine with THC, and approximately 20% that used blunts to smoke marijuana reported mixing it with tobacco (data not shown). Despite low rates of co-administration, the availability of products that can deliver both drugs raise concern about the use of one product increasing the risk of use of the other.
This study also provides insight into factors associated with the co-use of tobacco and marijuana that may inform both the development and target of intervention efforts. Co-users of tobacco and marijuana were significantly more likely to be male and LGB than marijuana-only users; characteristics previously shown to be associated with tobacco use. Demographic characteristics did not distinguish co-users and tobacco-only users. Co-users of tobacco and marijuana had significantly lower levels of anxiety than marijuana-only users providing support for the hypothesis that tobacco may counteract negative side effects like anxiety sometimes associated with marijuana use and may be a reason for co-use (Schauer et al. 2016). We also found higher rates of substance use among co-users consistent with other studies (Cohn et al. 2019; Seaman et al. 2019; Coleman-Cowger et al. 2017; Ramo et al. 2013; Ramo and Prochaska 2012); additional comorbidities that will need to be addressed when developing interventions.
Although these analyses are cross-sectional, data on the age of initiation provided some insight into whether the use of one product altered the course of initiation of the other product. The age of first use of cigarettes, e-cigarettes, SLT, large cigars, and LCCs did not differ between users of these products that also used marijuana and users of these products that did not use marijuana suggesting marijuana use does not alter the course of tobacco initiation for these products. The exception was waterpipe tobacco; users of waterpipe tobacco and marijuana first used waterpipe tobacco two years earlier than waterpipe users that did not use marijuana. Although we did not ask users of waterpipe and marijuana which product they used first, in comparing the age of initiation it was evenly split between those whose age of waterpipe tobacco preceded the age of first use of marijuana and vice versa (data not shown). In contrast, for co-users of e-cigarettes and marijuana, 91% reported the age of first marijuana use that preceded the age of first use of e-cigarettes, raising the possibility that legalization of marijuana could result in increases in vaping nicotine. For traditional tobacco products like SLT and large cigars, most co-users of these products with marijuana reported using the tobacco product at an earlier age than marijuana. Alternatively, tobacco product use seemed to alter the course of marijuana initiation consistent with other studies (Seaman et al. 2019). Co-users of any tobacco product and marijuana first used marijuana at an earlier age than marijuana users that did not use tobacco products. This could be related to the use of common modes of delivery and ease of use of both products. If tobacco enhances the effect of marijuana or reduces side effects, use of both products may also increase the frequency of use and risk for problematic use, highlighting the need for studies to collect data on the timing of use as well as reasons for co-use.
Co-users of e-cigarettes and marijuana were significantly less likely to think about or try to quit using e-cigarettes compared to e-cigarette users that did not use marijuana. They were also less likely to be daily e-cigarette users suggesting they do not perceive a need to quit. Similarly, cigarette and marijuana co-users were less likely to consider themselves smokers than cigarette users that did not use marijuana and were half as likely to be daily cigarette smokers. This is consistent with data on college students in which they consider themselves to be social smokers (Brown et al. 2011). Young adults that are not using tobacco products frequently may not perceive harm from use which will require effective communication efforts about the risks of infrequent tobacco use among co-users. In contrast, co-users of tobacco products and marijuana used marijuana on more days and were more likely to be daily or near-daily marijuana users compared to marijuana users that did not use tobacco products suggesting that tobacco use may be associated with more problematic marijuana use patterns.
Finally, this study provides preliminary insight into reasons for co-use. The highest score was on the experimentation subscale. This finding is not surprising given the age and demographics of this sample and their propensity to use alternative tobacco. It is also consistent with the second-highest score which was on the social context subscale which also supports the finding that young adults consider themselves social smokers. Although there was less support for using one product to increase the buzz of the other or using one product to reduce the use of the other product, cigarette users scored higher on these subscales than non-cigarette users and LCC users scored higher on instrumentality than non-LCC users. Interestingly, we did not find differences in these scores for e-cigarettes which may suggest a biological mechanism underlying co-use for combustible products which should be explored further.
There are limitations to our study. First, findings have limited generalizability and may not be representative of young adults who did not attend college. Further, although now living in other geographic areas, these young adults were recruited from colleges in two Southeastern states within the US. In addition, marijuana, tobacco, and other drug use was based on self-report and may be underreported. With the increasing legalization of marijuana, however, we expect this to be minimal for marijuana. Finally, the measurement of daily tobacco use was product-specific and could not be determined across all products. Despite these limitations, this is one of the few studies to examine both type of tobacco product used and modes of marijuana administration providing important information about patterns of co-use among young adults.
5.0. Conclusions
This study found cross-sectional evidence that the use of tobacco or marijuana among young adults increases the likelihood of use of the other product. Co-users of tobacco and marijuana were more likely to use modes of marijuana administration that facilitate co-use with tobacco, be daily or near-daily marijuana users, and use other substances while being less frequent tobacco users with little intention to quit using tobacco products. Reasons for co-use were primarily driven by a propensity for experimentation but potential biological mechanisms emerged for combustible tobacco product co-users. These findings highlight the importance of surveillance as marijuana becomes legalized in more states and drug delivery systems that facilitate co-use increase in popularity. It is possible that legalization of marijuana may have the unintended consequence of increasing tobacco use among young adults and may require targeted public health messaging to prevent negative outcomes among young adults.
Table 1.
Demographic Characteristics, Other Substance Use and Psychosocial Factors by Tobacco and Marijuana User Group.
| Univariate Descriptive Statistics1 N (%) or Mean (SE) |
Multivariable Generalized Logit Model Adjusted Odds Ratio (95% CI) p-value |
|||||
|---|---|---|---|---|---|---|
|
| ||||||
| Marijuana Only n=307 | Tobacco Only n=183 | Co-Users n=231 | p-value | Co-Users Vs. Tobacco Only | Co-Users Vs Marijuana Only | |
| Sex | ||||||
| Male | 149 (36.4) | 120 (60.6) | 131 (50.3) | <0.001 | 0.64 (0.35, 1.17) | 1.68 (1.02, 2.78) |
| Female | 158 (63.6) | 63 (39.4) | 100 (49.7) | 0.146 | 0.042 | |
|
| ||||||
| Ethnicity | ||||||
| Hispanic | 32 (8.9) | 5 (2.4) | 13 (6.8) | 0.055 | 2.44 (0.70, 8.55) | 0.53 (0.22, 1.30) |
| Non-Hispanic | 268 (91.1) | 178 (97.6) | 216 (93.2) | 0.163 | 0.165 | |
|
| ||||||
| Race | ||||||
| Nonwhite | 53 (18.4) | 21 (11.6) | 37 (17.7) | 0.256 | 1.75 (0.86, 3.57) | 0.98 (0.54, 1.80) |
| White | 250 (81.6) | 161 (88.4) | 189 (82.3) | 0.123 | 0.956 | |
|
| ||||||
| Employed Full Time | ||||||
| Yes | 256 (81.8) | 160 (88.2) | 195 (83.8) | 0.326 | 0.64 (0.30, 1.35) | 1.14 (0.58, 2.21) |
| No | 51 (18.2) | 22 (11.8) | 34 (16.1) | 0.240 | 0.708 | |
|
| ||||||
| Sexual Orientation | ||||||
| LGB | 61 (17.3) | 24 (13.7) | 50 (22.3) | 0.210 | 1.66 (0.79, 3.45) | 2.25 (1.17, 4.34) |
| Heterosexual | 244 (82.7) | 159 (86.3) | 181 (77.7) | 0.178 | 0.016 | |
|
| ||||||
| Married | ||||||
| Yes | 63 (22.4) | 44 (23.4) | 34 (13.3) | 0.069 | 0.56 (0.28, 1.12) | 0.66 (0.35, 1.22) |
| No | 244 (77.6) | 138 (76.6) | 196 (86.7) | 0.103 | 0.182 | |
|
| ||||||
| Binge Drinking | ||||||
| Yes | 195 (63.2) | 129 (71.3) | 188 (79.1) | 0.004 | 1.36 (0.75, 2.47) | 1.90 (1.10, 3.31) |
| No | 111 (36.8) | 54 (28.7) | 43 (20.9) | 0.315 | 0.023 | |
|
| ||||||
| Cocaine Use | ||||||
| Yes | 17 (3.2) | 8 (3.8) | 51 (19.4) | <0.001 | 5.24 (1.91, 14.4) | 5.40 (2.14, 13.6) |
| No | 290 (96.8) | 175 (96.2) | 180 (80.6) | 0.001 | <0.001 | |
|
| ||||||
| Prescription Meds | ||||||
| Yes | 39 (12.8) | 15 (7.2) | 43 (16.6) | 0.096 | 1.04 (0.30, 3.57) | 0.48 (0.17, 1.36) |
| No | 267 (87.2) | 168 (92.7) | 187 (83.4) | 0.954 | 0.166 | |
|
| ||||||
| ADHD Meds | ||||||
| Yes | 26 (8.1) | 8 (5.0) | 33 (13.8) | 0.069 | 1.86 (0.38, 9.14) | 2.10 (0.62, 7.11) |
| No | 281 (91.9) | 175 (95.0) | 198 (86.2) | 0.447 | 0.231 | |
|
| ||||||
| Stress Score | ||||||
| 16.8 (0.5) | 15.4 (0.7) | 16.8 (0.5) | 0.179 | 0.99 (0.92, 1.06) | 1.02 (0.96, 1.08) | |
| 0.743 | 0.500 | |||||
|
| ||||||
| Anxiety Score | ||||||
| 8.6 (0.2) | 7.6 (0.3) | 8.4 (0.3) | 0.038 | 0.99 (0.86, 1.15) | 0.88 (0.77, 0.99) | |
| 0.894 | 0.048 | |||||
|
| ||||||
| Depression Score | ||||||
| 8.8 (0.4) | 7.3 (0.6) | 8.4 (0.4) | 0.140 | 1.05 (0.96, 1.16) | 1.07 (1.00, 1.15) | |
| 0.281 | 0.065 | |||||
Ns are unweighted. Prevalences and means are weighted.
Highlights.
Use of tobacco or marijuana increases the likelihood of use of the other product
Co-users were more likely to use modes of marijuana administration that facilitate co-use
Co-use was associated with different use patterns that may impact cessation efforts
Funding:
This grant was supported by the National Cancer Institute Award R01CA141643. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The study sponsor did not have any role in study design; data collection, analysis, or interpretation; writing the report; or the decision to submit the manuscript for publication.
Footnotes
Declarations of Interest: none
Conflict of Interest: No conflict declared.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agrawal A, Lynskey MT, Pergadia ML, Bucholz KK, Heath AC, Martin NG, Madden PA, 2008. ‘Early cannabis use and DSM-IV nicotine dependence: a twin study’, Addiction, 103(11): 1896–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agrawal A, Lynskey MT Madden PA, Pergadia ML, Bucholz KK, Heath, A.C., 2009. ‘Simultaneous cannabis and tobacco use and cannabis-related outcomes in young women’, Drug and Alcohol Dependence, 101(1–2): 8–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agrawal A, Scherrer JF, Lynskey MT, Sartor CE, Grant JD, Haber JR, Madden PA, Jacob T, Bucholz KK, Xian. H., 2011. ‘Patterns of use, sequence of onsets and correlates of tobacco and cannabis’, Addict Behav, 36(12): 1141–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg CJ, Payne J, Henriksen L, Cavazos-Regh P, Getachew B, Schaeur GL, Haardorfer R, 2018. ‘Reasons for marijuana and tobacco co-use among young adults: a mixed methods scale development study”, Subst Use Misuse, 53(3): 357–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown AE, Carpenter MJ, Sutfin EL, 2011. ‘Occasional smoking in college: who, what, when and why?’, Addict Behav, 36(12):1199–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budney AJ, Vandrey RG, Hughes JR, Thostenson JD, Bursac Z, 2008. ‘Comparison of cannabis and tobacco withdrawal: severity and contribution to relapse’, J Subst Abuse Treat, 35(4): 362–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R, 1983. ‘A global measure of perceived stress’, Journal of Health and Social Behavior, 24(4): 386–96. [PubMed] [Google Scholar]
- Cohn AM, Johnson AL, Rose SW, Pearson JL, Villanti AC, Stanton C, 2018. ‘Population-level patterns and mental health and substance use correlates of alcohol, marijuana, and tobacco use and co-use in US young adults and adults: Results from the population assessment for tobacco and health’, Am J Addict, 27(6): 491–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohn AM, Abudayyeh H, Perreras L, Peters EN, 2019. ‘Patterns and correlates of the co-use of marijuana with any tobacco and individual tobacco products in young adults from Wave 2 of the PATH Study’, Addict Behav, 92: 122–27. [DOI] [PubMed] [Google Scholar]
- Coleman-Cowger VH, Schauer GL, Peters EN, 2017. ‘Marijuana and tobacco co-use among a nationally representative sample of US pregnant and non-pregnant women: 2005–2014 National Survey on Drug Use and Health findings’, Drug Alcohol Depend, 177: 130–35. [DOI] [PubMed] [Google Scholar]
- Cornacchione-Ross J, Sutfin EL, Suerken C, Walker S, Wolfson M, Reboussin BA, 2020. ‘Longitudinal associations between marijuana and cigar use in young adults’, Drug Alcohol Depend, 211: 107964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornelius ME, Wang TW, Jamal A, Loretan CG, Neff LJ, 2020. ‘Tobacco product use among adults - United States, 2019’, MMWR Morb Mortal Wkly Rep, 69(46): 1736–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin RD, Pacek LR, Copeland J, Moeller SJ, Dierker L, Weinberger A, Gbedemah M, Zvolensky MJ, Wall MM, Hasin DS, 2018. ‘Trends in daily cannabis use among cigarette smokers: United States, 2002–2014’, Am J Public Health, 108(1): 137–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haney M, Bedi G, Cooper ZD, Glass A, Vosburg SK, Comer SD, Foltin RW, 2013. ‘Predictors of marijuana relapse in the human laboratory: robust impact of tobacco cigarette smoking status’, Biol Psychiatry, 73(3): 242–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamal A, Homa DM, O’Connor E, Babb SD, Caraballo RS, Singh T, Hu SS, King BA. 2015. ‘Current cigarette smoking among adults - United States, 2005–2014’, MMWR Morb Mortal Wkly Rep, 64(44): 1233–40. [DOI] [PubMed] [Google Scholar]
- Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J, 1993. ‘Two shorter forms of the CES-D (Center for Epidemiological Studies Depression) depression symptoms index’, J Aging Health, 5(2): 179–93. [DOI] [PubMed] [Google Scholar]
- Masters MN, Haardörfer R, Windle M, Berg C, 2018. ‘Psychosocial and cessation-related differences between tobacco-marijuana co-users and single product users in a college student population’, Addictive Behaviors, 77: 21–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okoli CTC, Richardson CG, Ratner PA, Johnson JL, 2008. ‘Adolescents’ self-defined tobacco use status, marijuana use, and tobacco dependence’, Addict Behav, 33(11): 1491–9. [DOI] [PubMed] [Google Scholar]
- Osibogun O, Taleb ZB, Bahelah R, Salloum RB, Maziak W, 2018. ‘Correlates of poly-tobacco use among youth and young adults: Findings from the Population Assessment of Tobacco and Health study, 2013–2014’, Drug Alcohol Depend, 187: 160–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton GC, Coffey C, Carlin JB, Sawyer SM, Lynskey M, 2005. ‘Reverse gateways? Frequent cannabis use as a predictor of tobacco initiation and nicotine dependence’, Addiction, 100(10): 1518–25. [DOI] [PubMed] [Google Scholar]
- Peters EN, Budney AJ, Carroll KM, 2012. ‘Clinical correlates of co-occurring cannabis and tobacco use: a systematic review’, Addiction, 107(8): 1404–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters EN, Schwartz RP, Wang S, O’Grady KE, Blanco C,. 2014. ‘Psychiatric, psychosocial, and physical health correlates of co-occurring cannabis use disorders and nicotine dependence’, Drug Alcohol Depend, 134: 228–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D, PROMIS Cooperative Group, 2011. ‘Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS®): depression, anxiety, and anger’, Assessment, 18(3): 263–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabin RA, George TP, 2015. ‘A review of co-morbid tobacco and cannabis use disorders: possible mechanisms to explain high rates of co-use’, Am J Addict, 24(2): 105–16. [DOI] [PubMed] [Google Scholar]
- Ramo DE, Liu H, Prochaska JJ, 2012. ‘Tobacco and marijuana use among adolescents and young adults: a systematic review of their co-use’, Clin Psychol Rev, 32(2): 105–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramo DE, Prochaska JJ, 2012. ‘Prevalence and co-use of marijuana among young adult cigarette smokers: An anonymous online national survey’, Addict Sci Clin Pract, 7(1): 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramo DE, Delucchi KL, Hall SL, Liu H, Prochaska JJ, 2013. ‘Marijuana and tobacco co-use in young adults: patterns and thoughts about use’, J Stud Alcohol Drugs, 74(2): 301–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schauer GL, Berg CJ, Kegler MC, Donovan DM, Windle M, 2015. ‘Assessing the overlap between tobacco and marijuana: Trends in patterns of co-use of tobacco and marijuana in adults from 2003–2012’, Addict Behav, 49: 26–32. [DOI] [PubMed] [Google Scholar]
- Schauer GL, Hall CD, Berg CJ, Donovan DM, Windle M, Kegler MC, 2016. ‘Differences in the relationship of marijuana and tobacco by frequency of use: A qualitative study with adults aged 18–34 years’, Psychology of Addictive Behaviors, 30(3): 406–14. [DOI] [PubMed] [Google Scholar]
- Seaman EL, Green KM, Wang MQ, Quinn SC, Fryer CS, 2019. ‘Examining prevalence and correlates of cigarette and marijuana co-use among young adults using ten years of NHANES data’, Addict Behav, 96: 140–47. [DOI] [PubMed] [Google Scholar]
- Seaman EL, Stanton CA, Edwards KC, Halenar MJ, 2020. ‘Use of tobacco products/devices for marijuana consumption and association with substance use problems among U.S. young adults (2015-2016)’, Addict Behav, 102: 106133. [DOI] [PubMed] [Google Scholar]
- s JG, Song EY, Egan KL, Wagoner KG, Reboussin BA, Wolfson M, Sutfin EL, 2018. ‘Correlates of Alcohol Mixed with Energy Drink Use Among First Year College Students: Clinical and Research Implications’, J Caffeine Adenosine Res, 8(3): 107–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart SB, Bhatia D, Burns EK, Sakai JT, Martin LF, Levinson AH, Vaughn AM, Li Y, James KA, 2020. ‘Association of Marijuana, Mental Health, and Tobacco in Colorado’, J Addict Med, 14(1): 48–55. [DOI] [PubMed] [Google Scholar]
- Strong DR, Myers MG, Pulvers K, Noble M, Brikmanis K, Doran N, 2018. ‘Marijuana use among US tobacco users: Findings from wave 1 of the population assessment of tobacco health (PATH) study’, Drug Alcohol Depend, 186: 16–22. [DOI] [PubMed] [Google Scholar]
- Vandrey RG, Budney AJ, Hughes JR, Liguori A, 2008. ‘A within-subject comparison of withdrawal symptoms during abstinence from cannabis, tobacco, and both substances’, Drug Alcohol Depend, 92(1–3): 48–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel EA, Rubinstein ML, Prochaska JJ, Ramo DE, 2018. ‘Associations between marijuana use and tobacco cessation outcomes in young adults’, J Subst Abuse Treat, 94: 69–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberger AH, Platt J, Copeland J, Goodwin RD, 2018. ‘Is Cannabis use associated with increased risk of cigarette smoking initiation, persistence, and relapse? Longitudinal data from a representative sample of US adults’, J Clin Psychiatry, 79(2):17m11522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberger AH, Delnevo CD, Wyka K, Gbedemah M, Lee J, Copeland J, Goodwin RD, 2020. ‘Cannabis use is associated with increased risk of cigarette smoking initiation, persistence, and relapse among adults in the US’, Nicotine Tob Res, 22(8):1404–08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfson M, Suerken CK, Egan KL, Sutfin EL, Reboussin BA, Wagoner KG, Spangler J, 2015. ‘The role of smokeless tobacco use in smoking persistence among male college students’, Am J Drug Alcohol Abuse, 41(6): 541–6. [DOI] [PMC free article] [PubMed] [Google Scholar]