Abstract
Purpose of review
To highlight artificial intelligence applications in ophthalmology during the COVID-19 pandemic that can be used to: describe ocular findings and changes correlated with COVID-19; extract information from scholarly articles on SARS-CoV-2 and COVID-19 specific to ophthalmology; and implement efficient patient triage and telemedicine care.
Recent findings
Ophthalmology has been leading in artificial intelligence and technology applications. With medical imaging analysis, pixel-annotated distinguishable features on COVID-19 patients may help with noninvasive diagnosis and severity outcome predictions. Using natural language processing (NLP) and data integration methods, topic modeling on more than 200 ophthalmology-related articles on COVID-19 can summarize ocular manifestations, viral transmission, treatment strategies, and patient care and practice management. Artificial intelligence for telemedicine applications can address the high demand, prioritize and triage patients, as well as improve at home-monitoring devices and secure data transfers.
Summary
COVID-19 is significantly impacting the way we are delivering healthcare. Given the already successful implementation of artificial intelligence applications and telemedicine in ophthalmology, we expect that these systems will be embraced more as tools for research, education, and patient care.
Keywords: artificial intelligence, COVID-19, ophthalmology, SARS-CoV-2, telemedicine
INTRODUCTION
Advances in artificial intelligence applications and digital tools for telemedicine have been changing patient care in ophthalmology over the past decade. The year 2020, heralded as ‘The Year of the Eye’ [1], is a particularly special year for ophthalmology; yet it will be undoubtedly remembered as the year of the unpredictable COVID-19 pandemic that has caused enormous morbidity and mortality, often exceeding the abilities of health-care systems to cope with its devastating impact. The worldwide precipitous shutdown efforts to contain viral transmission and the meager waves of reopening regional economies have resulted in unemployment, painful economic contraction, and major transformations of several sectors of the economy, including healthcare.
All aspects of medicine and ophthalmology, from clinical care and research to educational and public health activities have been irreversibly transformed by COVID-19. There is great hope that in the post COVID-19 era, artificial intelligence will have an ever-increasing positive impact on medicine and ophthalmology. Digital technology has provided platforms for adaptation and resources to continue essential operations for patients and healthcare workers during COVID-19. We also expect that in the future; there will be expanding central roles for artificial intelligence and telemedicine in ophthalmology.
COVID-19 has reoriented our day-to-day lives and challenged our healthcare system in unprecedented ways. During the pandemic, academic medical centers and hospitals have scrambled to adapt their systems, clinical workflows, and priorities to treat the most urgent and critical patients, all while minimizing exposure to their healthcare workers. Hospitals were built in convention centers in major cities to handle potential surges. Biomedical and technology industries shifted their focus and missions to generate products and therapies to help fight this disease. Artificial intelligence and telemedicine efforts were implemented to help mitigate the pandemic. We posit that experiences and data collected from the COVID-19 pandemic will help shape future solutions in the post COVID-19 era.
In this article, we present a brief review of artificial intelligence applications during the COVID-19 pandemic, as well as highlight artificial intelligence applications in ophthalmology that can be used to: describe ocular findings and changes correlated with COVID-19 diagnosis and severity; extract information from scholarly articles specific to ophthalmology diagnoses, manifestation of signs and symptoms, transmission, and patient management; and implement efficient patient triage and telemedicine applications.
ARTIFICIAL INTELLIGENCE APPLICATIONS DURING COVID-19
As more data becomes available, analytics, machine, and deep learning techniques are being developed for COVID-19 tracking and forecasting, diagnosis, contact tracing, vaccine and therapy development, and patient management [2–5,6▪▪,7–17]. Researchers from the United Nations Global Pulse and the Global Coordination Mechanism on NCDs World Health Organization reviewed recent studies using artificial intelligence to tackle many aspects of the COVID-19 crisis at the molecular, medical, and epidemiological scales [2]. Artificial intelligence applications can support the COVID-19 crisis through automating diagnosis from CT scans, providing ways to track disease evolution, and generating predictions on patient outcomes. From a therapeutic perspective, artificial intelligence is being used to estimate the structure of SARS-CoV-2-related proteins, to identify existing drugs, and to propose new compounds. Additionally, artificial intelligence modeling has been applied in several areas of epidemiological research, including forecasting the number of new confirmed cases given different public policy choices and modeling the rate of asymptomatic cases [2].
Under a call to action to the tech community issued on 16 March 2020, researchers and leaders in leading artificial intelligence institutes, Georgetown University’s Center for Security and Emerging Technology, the Allen Institute for AI and Microsoft, Chan Zuckerberg Initiative, and the National Library of Medicine, joined in the release of a new machine readable COVID-19 Open Research Dataset (CORD-19) [18]. The CORD-19 dataset consists of over 57 000 articles. All articles are related to the study of coronavirus, such as case reports, transmission routines, environmental factors, and treatment strategy explorations [19]. They have been transformed into machine-readable formats for researchers to mine and discover information that will help in understanding disease transmission and incubation, risk factors, virus genetics, origin and evolution, vaccines and therapeutics, and diagnosis and surveillance [19].
Other dedicated artificial intelligence-based search engines for scholarly research, such as DISCOVID.ai, have also been developed to compile data that will be useful in understanding this pandemic [20]. The National Institutes of Health have also established LitCovid, a curated literature hub for tracking up-to-date scientific information. It currently provides a central access to thousands of COVID-19 relevant articles in PubMed [21].
Given that artificial intelligence applications heavily rely on accurate data and training, it is still debatable how much they can help with the current pandemic. However, they will definitely play a role in upcoming potential waves and future public health crises.
ARTIFICIAL INTELLIGENCE APPLICATIONS IN OPHTHALMOLOGY DURING COVID-19
Ophthalmology has been leading in artificial intelligence and technology applications, from image processing and deep learning methods for classification and predicting progression, to natural language processing (NLP) methods on electronic health records. During COVID-19, ophthalmology can use artificial intelligence applications to: adapt image analysis and computational methods to describe ocular findings and changes correlated with COVID-19 diagnosis and severity; use NLP to extract scholarly articles specific to ocular manifestations, viral transmission, and patient/practice management; and implement patient triage and telemedicine applications.
Medical image analysis for ocular findings in COVID-19 patients
SARS-CoV-2 testing with reverse transcription PCR (RT-PCR) is limited in availability, speed, and accuracy. As such, there is a need to develop other diagnostic methodologies for screening and diagnosis of COVID-19 cases. Several studies have utilized machine learning and artificial intelligence systems on lung CT and X-ray scans of COVID-19 patients [5,6▪▪,7–9] (Table 1) with different approaches and architectures; such as training on raw CT scans or using labeled scans with regions of interest, and implementing a joint convolutional neural network for scans and clinical data [6▪▪]. Adapting from radiology studies, retinal images can potentially present COVID-19 specific features that can be extracted for classification and prediction tasks.
Table 1.
Artificial intelligence applications on lung computed tomography scans and chest X-rays for COVID-19 diagnosis
| Patient population | Task | Type/number of images | Methods | Results |
|---|---|---|---|---|
| 3322 patients from six medical centers in Wuhan, Shandong, Beijing, and Shenzhen, China [5] | Classification for detecting COVID-19-positive cases | 4356 3D chest CT scans | Deep learning model, COVID-19 detection neural network (COVNet) | AUC 0.96 (P- value < 0.001) |
| 905 patients from 18 medical centers in 13 provinces in China [6▪▪] | Rapidly diagnose patients who are COVID-19 positive by integrating chest CT findings with clinical symptoms, exposure history, and laboratory testing | Chest CT scans | Three AI algorithms: CNN for only CT scans; ML: SVM, Random forest for clinical data; joint CNN model combining CT scans and clinical data | AUC 0.92 AUC (95% CI 0.887–0.948) joint CNN model |
| 125 COVID-19-positive cases from open source chest X-ray dataset. Negative cases from another dataset (32717 unique patients with disease labels) [7] | Binary classification (COVID vs. no-findings) and multiclass classification (COVID vs. no-findings vs. pneumonia) | 1000 Chest X-ray images | Deep learning. DarkNet architecture | AUC 0.98 for (COVID vs. no-findings) and 0.87 for multiclass (COVID vs. no-findings vs. pneumonia) |
| 454 patients in the Netherlands (223 positive cases and 231 negative cases) [8] | Classification for detecting COVID-19 cases | 24678 Chest X-Ray images | AI system (CAD4COVID-Xray) | AUC 0.81 |
| 1186 patients: 521 COVID-19 positive cases from Rhode Island Hospital and 9 Hospitals in Hunan Province, China 665 with non-COVID-19 pneumonia from Rhode Island Hospital, University of Pennsylvania and Xiangya Hospital [9] | Classification of COVID-19 cases | 1186 CT scans 132583 CT slices |
EfficientNet B4 deep neural network architecture after lung segmentation, followed by two-layer fully connected neural network to pool slices together | AUC 0.96 (95% CI 0.9–0.98) |
AUC, Area Under the Curve; CNN, Convolutional Neural Network; CT, computed tomography; ML, Machine Learning; SVM, Support Vector Machine.
COVID-19 ophthalmological-related changes have been associated with ocular external diseases, such as conjunctivitis, including conjunctival hyperemia, chemosis, epiphora, or increased secretions [22▪]. Advanced imaging technology, such as Spectral Domain Coherence Tomography (SD-OCT), OCT-Angiography, and ultra-wide field fundus imaging, allow for noninvasive analyses of the microvasculature structure and the identification of subclinical retinal conditions. Various features can be extracted from the retina, such as vessel caliber bifurcation or tortuosity, microvascular changes, and vascular fractal dimensions, which may reflect the systemic health of patients. These features can then be used for classifying or predicting other systemic diseases, such as cardiovascular risk factors [23▪▪]. Similar methods can be applied in the diagnosis of COVID-19 and in predicting associated severe outcomes.
A recent study used OCT to evaluate patients infected by SARS-CoV-2 reporting identifying features [24▪]. All 12 patients diagnosed with COVID-19 showed hyper-reflective lesions at the level of ganglion cell and inner plexiform layers more prominently at the papillomacular bundle. Results of OCT-angiography and ganglionar cell complex analysis appeared normal [24▪]. Furthermore, four patients presented subtle cotton wool spots and microhaemorrhages along the retinal arcade, observed on fundus examination, color fundus photography, and red-free imaging [24▪]. Given the potential of COVID-19 identifiable features from retinal imaging, developing an artificial intelligence system may help with noninvasive diagnosis and predictions of severe outcomes, such as acute respiratory distress syndrome. These applications may allow for rapid clinical decision-making, such as aggressive treatments for high-risk patients; and assist in planning epidemiological studies on predicting severe outcomes of COVID-19 patients.
Despite the potential and promising performance, results of artificial intelligence applications on lung CT and X-ray scans, in order for these methods to be used as clinical decision support systems, they should undergo rigorous validation, clinical investigation, and regulatory approval.
Natural language processing for ophthalmic scholarly articles
Artificial intelligence researchers in informatics and data science, who work on ophthalmic applications, can also mine datasets, like the CORD-19, to extract information specific to ophthalmology diagnoses, manifestation of signs and symptoms, patient/practice management, and viral transmission. As an example, we utilized NLP techniques to extract articles from the CORD-19 dataset and integrated the results with COVID-19 ophthalmic-related articles in the LitCovid database.
Data preprocessing and topic modeling techniques were used to extract articles from the CORD-19 dataset. For topic modeling, we used a LatentDirichletAllocation (LDA) model to learn the distribution of ophthalmology topics across each document. We then selected reference documents that were used to highlight the most related articles by calculating similarity scores. Results were then merged with articles from the LitCovid database (last updated 5 June 2020).
To date, more than 200 ophthalmology COVID-19-related articles have been published. Figure 1 shows the distribution of topics by patient care and practice management (57.8%), transmission (19.4%), ocular manifestations (17.22%), treatment (3.9%), and diagnosis (1.7%). Combined, these articles stress two main findings: the potential presence of SARS-CoV-2 in ocular tissue or secretions and the risk of transmission; and the importance of adequate protection and strategies to prevent transmission in ophthalmic practices, with an increase for telemedicine applications.
FIGURE 1.
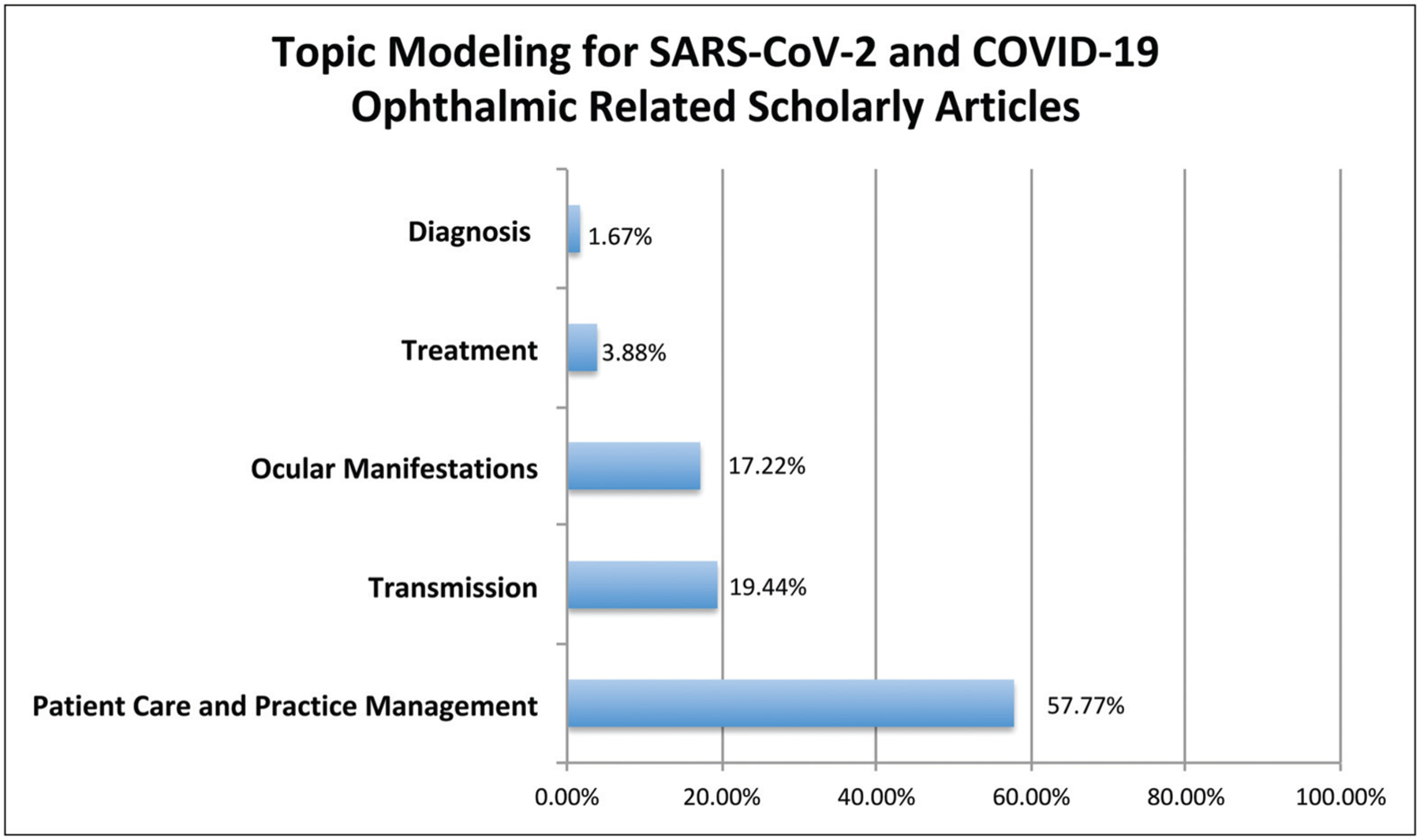
Distribution of SARS-Cov-2 and COVID-19 topics in ophthalmology scholarly related articles.
Telemedicine ophthalmology applications during COVID-19
With the lack of a cure or vaccine, the only way to slow and contain the transmission of COVID-19 is through isolation, shelter-in-place, and lockdown orders. Telemedicine systems are ideal for mitigating overcrowding of hospitals and clinics by triaging low-risk patients to decrease exposure and promote delivery of care. These systems can also help in addressing the depletion of medical supplies and resources, like personal protective equipment.
With COVID-19, video consultations have been promoted and scaled up to reduce the risk of transmission. On 6 March 2020, the Centers for Medicare and Medicaid services broadened access to Medicare telehealth services [25]. This expansion allowed for services to be rendered nationally, and visits could be provided with the patient presenting from home. This opened doors to millions of new patients who can utilize telemedicine for the first time. Since this modification, there has been an exponential increase in telemedicine visits. Telehealth companies are scrambling to upgrade their systems to handle the influx. Healthcare systems have become overburdened with administrative challenges to train and onboard practitioners in telemedicine procedures. Systems without any telemedicine capabilities are trying to adopt technology from third-party companies without the time to test new platforms.
Ophthalmology has been at the forefront of international telemedicine healthcare delivery before COVID-19. In 2018, the American Academy of Ophthalmology (AAO) released a telemedicine statement to provide an overview highlighting issues that we anticipate will shape the development and implementation of telemedicine for ophthalmology in the near future [26]. Four primary domains for telemedicine were highlighted with different technologies: live audio–video (synchronous) telemedicine; store-and-forward (asynchronous) telemedicine: electronic transmission of healthcare data; remote patient monitoring; and mobile Health. Telemedicine has been successfully established for two ophthalmic diseases: diabetic retinopathy [27,28] and retinopathy of prematurity (ROP) [29,30], especially for remote surveillance, and has demonstrated clinical, public health, and economic benefits. Telemedicine for ROP has improved access to eye care globally for premature infants at high risk of ROP. Similarly, diabetic retinopathy telemedicine programs have improved patient access to retinal examinations through retinal imaging in primary care settings, allowing for urgent cases to be streamlined directly to a retina specialist for evaluation and treatment.
Saleem et al. [31▪] described guidelines to help ophthalmic practices implement telemedicine during COVID-19. The New York-based authors conclude that the technology for remote ophthalmic monitoring in the United States is not fully scalable or ready, however, patients are willing to adopt these applications [31▪]. Specialties, such as oculo-plastics, neuro-ophthalmology, and pediatrics can adapt faster to telemedicine, whereas anterior segment presentations are more challenging. For glaucoma, telemedicine applications are helpful for medicine reconciliation and assessment of glaucoma medication tolerance; and retinal telehealth is best supported by store-and-forward asynchronous models [31▪].
The transition to telemedicine during COVID-19 has been swift, with practitioners leaning on this technology for continuity of care and saving face-to-face visits for those who require urgent evaluation and treatment. However, there are organizational and technological limitations for telemedicine applications. These include lack of hardware within hospitals to implement specialized remote care, limited home monitoring devices, reimbursement, cost, tailored training modules, and confidentiality and privacy issues. CMS has committed to relaxing restrictions for reimbursement during the COVID-19 pandemic. Also, federal rules were lessened to allow physicians to work across state lines, encouraging remote consultations. If these rules continue post COVID-19, then telemedicine applications may increase across healthcare systems with future investments in artificial intelligence, technology, and training.
Artificial intelligence within telemedicine is an emerging field [32]. The main drivers for using artificial intelligence applications in telemedicine are to address the high demand and prioritize patients who need immediate care [32]. Algorithms can be developed to match the availability of practitioners to patients immediately and within close locations. Additionally, increasing discoveries for personalized care are making care provisions more complex, beyond the scope of one single provider. Artificial intelligence can also support the development of knowledge of clinical processes with more than one provider to address care for patients who need it in more than one specialty. For interpretation of images and text data from electronic health records, the use of decision analytics and artificial intelligence would allow for data integration and interpretation pipelines.
FUTURE DIRECTIONS IN THE POST COVID-19 ERA
COVID-19 is significantly impacting the way we are delivering healthcare. The lessons learned during this crisis are going to shape future clinical care, research, and education missions in academic medical centers and healthcare systems. We expect that telemedicine will be embraced more as a tool for healthcare delivery, data sharing mechanisms, and HIPPAA regulations will be adjusted to validate and help with implementation of artificial intelligence applications, and new healthcare delivery models will be adopted.
COVID-19 brought telemedicine into a new light, and it may motivate further measures that will increase its adoption. Post COVID-19, telemedicine usage may increase for elective, routine and outpatient visits, and for infectious diseases. Health systems will need to adopt or build their own digital platforms compatible with their environment, healthcare workers, and patient population. Home monitors, smart devices, and their connectivity need to overcome the hurdle of affordability and data privacy. Additionally, telemedicine needs to be less sophisticated and accessible to all patient demographics. Data efficiencies can also be improved with artificial intelligence applications within telemedicine, assisting in integration and analyses.
The COVID-19 pandemic has brought artificial intelligence researchers together. For any artificial intelligence system to perform well, it relies on the quality of data inputted and trained on. Generaliz-ability is also improved when these systems learn characteristics from diverse populations. The post COVID-19 era may witness more data-sharing mechanisms with new HIPPAA guidelines. This will allow artificial intelligence researchers to develop systems that will make more accurate predictions, simulate results for different economic decisions, and help with better preparation for the next crises.
CONCLUSION
Ophthalmology is a leader in technological innovations and telemedicine. Given the already successful implementation of telemedicine systems, we expect the expansion of these systems post COVID-19. Innovations in artificial intelligence systems and hardware for prevention and monitoring will serve as promising tools in ophthalmic care. Clinical, research, and educational operations in academic settings during COVID-19 will also continue to evolve post this pandemic. To be better prepared for the next crisis, it is important to consider the lessons learned and develop solutions with digital technology in providing accessible care.
KEY POINTS.
COVID-19 is significantly impacting medicine and ophthalmology. As more data becomes available, analytics, machine and deep learning techniques are being developed for COVID-19 tracking and forecasting, diagnosis, contact tracing, vaccine and therapy development, and patient management.
Adapting from artificial intelligence radiology studies that use lung computed tomography (CT) and X-ray scans, retinal images can present with COVID-19-specific ocular features that can be extracted for classification and prediction tasks.
Natural language processing methods (NLP) can be utilized to analyze the increasing influx of COVID-19 scholarly articles to improve our understanding in ophthalmology patient care and practice management, viral transmission, ocular manifestation and treatment. To date, COVID-19 ophthalmology-related articles stress two main findings: the potential presence of SARS-CoV-2 in ocular tissue or secretions and the risk of transmission; and the importance of adequate protection and strategies to prevent transmission in ophthalmic practices.
The transition to telemedicine during COVID-19 has been swift. Artificial intelligence for telemedicine applications can address the high demand, prioritize and triage patients, improve at home monitoring devices, as well as secure data-sharing mechanisms.
Digital technology has provided platforms for adaptation and resources to continue essential operations for patients and healthcare workers during COVID-19. We expect that in the post COVID-19 era, there will be expanding central roles for artificial intelligence and telemedicine in ophthalmology.
Acknowledgements
Manoj Nallabothula, MS and Abdullah Aleem, MS for their help in topic modeling.
Financial support and sponsorship
J.A.H., support by BrightFocus Foundation Grant; D.T.A, support by grant R01 EY010101 24 (National Eye Institute), Verily Life Sciences (Employee), Verb Surgical (Board Member); R.V.P.C., support by grants P30EY001792 and R01EY029673 from the National Institutes of Health (Bethesda, MD), by grants SCH-1622679, SCH-1622542, and SCH-1622536 from the National Science Foundation (Arlington, VA), and unrestricted departmental funding from Research to Prevent Blindness (New York, NY). Alcon, Novartis, Phoenix Technologies.
Footnotes
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
- 1.American Academy of Ophthalmology. 2020 is the #YearOfTheEye.Available at: https://www.aao.org/2020-year-of-the-eye. (Accessed 8 June 2020)
- 2.Bullock J, Luccioni A, Pham KH, et al. Mapping the landscape of artificial intelligence applications against COVID-19. arXi 2003; 11336v1. https://arxiv.org/pdf/2003.11336.pdf (last accessed June 6, 2020). [Google Scholar]
- 3.Weissman GE, Crane-Droesch A, Chivers C, et al. Locally informed simulation to predict hospital capacity needs during the COVID-19 pandemic. Ann Intern Med 2020; M20–1260; doi: 10.7326/M20-1260. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 4.COVID-19 Statistics. Illinois Department of Public Health. Available at: https://www.dph.illinois.gov/covid19/covid19-statistics. (Accessed 7 June 2020)
- 5.Li L, Qin L, Xu Z, et al. Artificial intelligence distinguishes COVID-19 from community acquired pneumonia on chest CT. Radiology 2020; 200905; doi: 10.1148/radiol.2020200905 [Epub ahead of print] [DOI] [Google Scholar]
- 6▪▪.Mei X, Lee HC, Diao KY, et al. Artificial intelligence-enabled rapid diagnosis of patients with COVID-19. Nat Med 2020; doi: 10.1038/s41591-020-0931-3 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]; This study shows artificial intelligence algorithms to integrate chest CT findings with clinical symptoms, exposure history and laboratory testing to rapidly diagnose patients who are positive for COVID-19. It provides the reader with an example of how artificial intelligence systems can be used to rapidly diagnose COVID-19 patients.
- 7.Ozturk T, Talo M, Yildirim EZ, et al. Automated detection of COVID-19 cases using deep neural networks with X-ray images. Comput Biol Med 2020; 121:103792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murphy K, Smits H, Knoops AJG, et al. COVID-19 on the chest radiograph: a multi-reader evaluation of an AI system. Radiology 2020; 201874; doi: 10.1148/radiol.2020201874 [Epub ahead of print] [DOI] [Google Scholar]
- 9.Bai HX, Wang R, Xiong Z, et al. AI augmentation of radiologist performance in distinguishing COVID-19 from pneumonia of other etiology on chest CT. Radiology 2020; 201491; doi: 10.1148/radiol.2020201491 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ong E, Wong MU, Huffman A, et al. COVID-19 coronavirus vaccine design using reverse vaccinology and machine learning. bioRxiv 2020; 2020.03. 20.000141. Published 2020. March 21. doi: 10.1101/2020.03.20.000141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Institute for Protein Design, University of Washington, Coronavirus. Available at: https://www.ipd.uw.edu/2020/02/rosettas-role-in-fighting-coronavirus/. (Accessed 7 June 2020).
- 12.Senior AW, Evans R, Jumper J, et al. Improved protein structure prediction using potentials from deep learning. Nature 2020; 577:706–710. [DOI] [PubMed] [Google Scholar]
- 13.Richardson P, Griffin I, Tucker C, et al. Baricitinib as potential treatment for 2019-nCoV acute respiratory disease. Lancet 2020; 395:e30–e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hong L, Lin J, Tao J, et al. BERE: an accurate distantly supervised biomedical entity relation extraction network. 2019. arXiv preprint arXiv:1906.06916. [Google Scholar]
- 15.Hu F, Jiang J, Yin P, et al. Prediction of potential commercially inhibitors against SARS- CoV-2 by multitask deep model.2020. arXiv preprint arXiv:2003.00728. [Google Scholar]
- 16.Zhavoronkov A, Aladinskiy V, Zhebrak A, et al. Potential COVID-2019 3C-like AQ10 protease inhibitors designed using generative deep learning approaches. 2020. ChemRxiv. Preprint. Available at https://chemrxiv.org/articles/Potential_2019-nCoV_3C-like_Protease_Inhibitors_Designed_Using_Generative_Deep_Learning_Approaches/11829102 (Accessed July 1, 2020) [Google Scholar]
- 17.Foy K Bluetooth signals from your smartphone could automate Covid-19 contact tracing while preserving privacy. Available at: http://news.mit.edu/2020/bluetooth-covid-19-contact-tracing-0409. (Accessed 4 June 2020)
- 18.Call to Action to the Tech community on new machine readable COVID-19 dataset. Available at: https://www.whitehouse.gov/briefings-statements/call-action-tech-community-new-machine-readable-covid-19-dataset/. (Accessed 8 June 2020)
- 19.CORD-19: COVID-19 Open Research Dataset. Available at: https://pages.semanticscholar.org/coronavirus-research. (Accessed 7 June 2020)
- 20.Discover COVID: unraveling scientific knowledge to fight COVID-19. https://discovid.ai/search.(Accessed 7 June 2020)
- 21.LitCovid. NIH NLM. Available at: https://www.ncbi.nlm.nih.gov/research/coronavirus/(Accessed 8 June 2020)
- 22▪.Wu P, Duan F, Luo C. Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol 2020; 138:575–578. [DOI] [PMC free article] [PubMed] [Google Scholar]; This publication describes the ocular manifestations and viral prevalence in the conjunctiva of patients with COVID-19. It provides the reader with information to understand ocular manifestations of COVID-19 to improve diagnosis and prevent disease transmission.
- 23▪▪.Poplin R, Varadarajan AV, Blumer K, et al. Prediction of cardiovascular risk factors from retinal fundus photographs via deep learning. Nat Biomed Eng 2018; 2:158–164. [DOI] [PubMed] [Google Scholar]; This publication shows how deep learning models can be applied on retinal images to predict cardiovascular risk factors not previously thought to be present or quantifiable. It provides the reader with an example of how potential artificial intelligence applications on retinal images can be used to predict systemic diseases and/or associated risk factors.
- 24▪.Marinho PM, Marcos AAA, Romano AC, et al. Retinal findings in patients with COVID-19. Lancet 2020; 395:1610. [DOI] [PMC free article] [PubMed] [Google Scholar]; This report presents retinal and OCT changes in 12 adults, examined 11–33 days after COVID-19 symptom onset. It provides the reader with information on how advanced ophthalmic imaging can be used to identify features in COVID-19 patients.
- 25.Medicare Telemedicine Healthcare provider fact Sheet. Available at: https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet. (Accessed 18 April 2020)
- 26.AAO Telemedicine Task Force. Telemedicine for Ophthalmology Statement-2018. American Academy of Ophthalmology (AAO) released a telemedicine statement. (Accessed 18 April 2020) [Google Scholar]
- 27.Horton MB, Silva PS, Cavallerano JD, Aiello LP. Clinical components of telemedicine programs for diabetic retinopathy. Curr Diab Rep 2016; 16:129. [DOI] [PubMed] [Google Scholar]
- 28.Horton MB, Silva PS, Cavallerano JD, Aiello LP. Operational components of telemedicine programs for diabetic retinopathy. Curr Diab Rep 2016; 16:128. [DOI] [PubMed] [Google Scholar]
- 29.Quinn GE, Ying GS, Repka MX, et al. Timely implementation of a retinopathy of prematurity telemedicine system. J AAPOS 2016; 20:425.e1–430.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang SK, Callaway NF, Wallenstein MB, et al. SUNDROP: six years of screening for retinopathy of prematurity with telemedicine. Can J Ophthalmol 2015; 50:101–106. [DOI] [PubMed] [Google Scholar]
- 31▪.Saleem SM, Pasquale LR, Sidoti PA, et al. Virtual ophthalmology: telemedicine in a covid-19 era. Am J Ophthalmol 2020; doi: 10.1016/j.ajo.2020.04.029 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]; This publication provides a review of recent trends in telehealth and governmental recommendations for healthcare delivery during the COVID-19 pandemic. It also provides the reader with the current state of telemedicine in ophthalmology or teleophthalmology, along with a comprehensive experience in telemedicine design and implementation.
- 32.Kuziemsky C, Maeder AJ, John O, et al. Role of artificial intelligence within the telehealth domain. Yearb Med Inform 2019; 28:035–040. [DOI] [PMC free article] [PubMed] [Google Scholar]


