Abstract
Objectives:
This study examined the association between food insecurity status and healthcare access, utilization, and quality among adults aged 55 years and older.
Methods:
Data collected between 2011 and 2016 for the California Health Interview Survey were used. The sample included 72,212 individuals who were divided into three groups: food secure (FS), low food security (L-FS), and very low food security (VL-FS).
Results:
Logistic regression analyses controlled for demographics. Food insecurity was associated with decreased access to and quality of care and increased utilization. Specifically, VL-FS was more likely to delay care than FS. Additionally, VL-FS and L-FS had greater odds of visiting an emergency room than FS. Furthermore, VL-FS and L-FS were more likely to have a doctor who did not always explain aspects of care carefully compared to FS.
Discussion:
These findings suggest a need for increased screening for food insecurity in healthcare settings.
Keywords: California Health Interview Survey, food insecurity, healthcare access, healthcare quality, later life
Introduction
Food insecurity is a growing public health problem among midlife and older adults in America. It has been estimated that among those aged 50–59 years, the prevalence of those experiencing the most severe form of food insecurity increased by 80% between 2001 and 2017 (Ziliak & Gundersen, 2019a). Even more striking, the prevalence rate more than doubled among those older than 59 years, during this time (Ziliak & Gundersen, 2019b). In total, 26% of individuals aged older than 50 years experienced some form of food insecurity in 2017 (Ziliak & Gundersen, 2019a, 2019b).
A lack of food security occurs when a person does not have access “at all times to enough food for an active, healthy life” (Alisha et al., 2017). Food insecurity is associated with increased risk of chronic disease (Seligman & Schillinger, 2010). Additionally, those who are food insecure often struggle to purchase the food or medication needed to manage their illnesses, leading to exacerbation of both their illnesses and their food insecurity (Seligman & Schillinger, 2010). These poor health outcomes, in turn, can contribute to greater healthcare costs (Berkowitz et al., 2018).
The body of literature pertaining to healthcare access and utilization of healthcare services among food insecure adults suggests difficulty in obtaining care: these types of patients are more likely to delay care and utilize acute care services (Bhargava & Lee, 2017), perhaps due to a lack of resources to address both their nutritional and healthcare needs (Becker, 1965). The two studies that have assessed utilization of healthcare services among food insecure older adults only have produced conflicting results and do not comment on access to care among this population (Bhargava & Lee, 2016, 2017). For these reasons, additional research pertaining to healthcare access and utilization with a focus on middle and later life is warranted.
In explaining the association between food insecurity and healthcare utilization, two primary theories have been posited (Bhargava & Lee, 2017). The neoclassical household production framework postulates that utilization of healthcare is constrained by household resources, and thus implies a negative association between food insecurity and healthcare utilization (Becker, 1965; Bhargava & Lee, 2017). On the other hand, the Andersen framework proposes that healthcare utilization is influenced by three factors: a predisposing component, which speaks to an individual’s predisposition to utilizing healthcare services, an enabling component, which dictates an individual’s ability to utilize services, and an illness component, which relates to an individual’s health status and need to utilize services (Andersen & Newman, 1973). Food insecurity may be a predisposing factor that leads to a greater need for and utilization of healthcare due to the increased vulnerabilities of people who are food insecure (Bhargava & Lee, 2017). Taken together, these models can be used to construct differential predictions for the relationship between food insecurity and healthcare access and utilization. Specifically, as shown in Figure 1, we hypothesized decreased access to care, as supported by the neoclassical model, and increased utilization of care, as suggested by Andersen’s framework.
Figure 1.
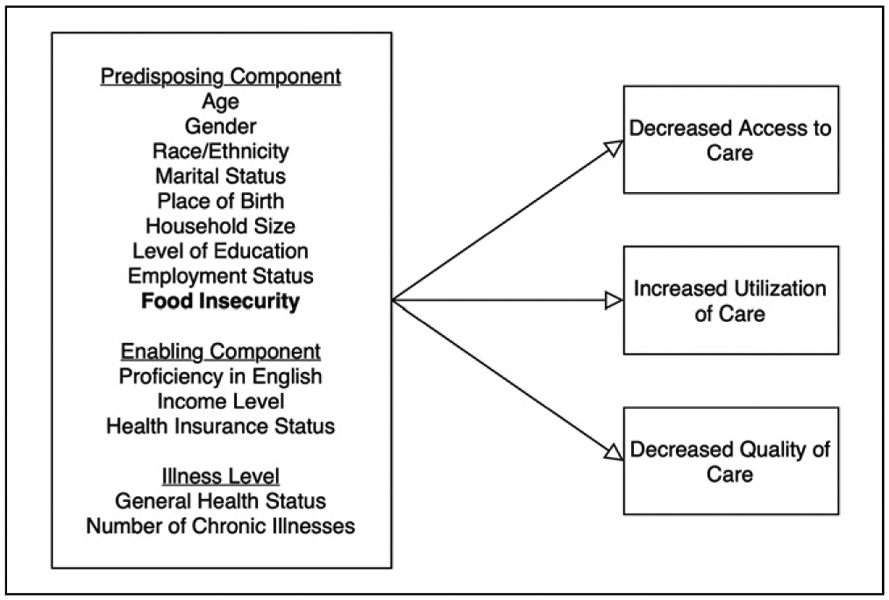
Application of the Andersen (Andersen & Newman, 1973) theory and the neoclassical household production framework (Becker, 1965): conceptual model displaying association between food insecurity and healthcare access, utilization, and quality.
The neoclassical household production framework (Becker, 1965) can also be used to understand the association between food insecurity and aspects of the quality of healthcare received, including communication. This framework suggests that those who are food insecure may have difficulty with uptake of physician-provided information, due to constrained resources, such as the mental “bandwidth” required for disease management (Seligman & Schillinger, 2010). Previous studies have assessed the association between aspects of socioeconomic status, such as education, income, employment status, and doctor–patient communication (Verlinde et al., 2012). In general, the literature suggests that there is room for physicians to better tailor the quality of their communication to meet the needs of vulnerable patients. For example, those of lower socioeconomic status report receiving less information pertaining to diagnosis and treatment and are less involved in medical decisions than are those of higher socioeconomic status (Verlinde et al., 2012). Food insecurity may measure other characteristics of a person’s social and economic standing that are not captured by these often -used indicators of a person’s risk status (Ma et al., 2008). In employing the neoclassical household production framework, it can be hypothesized that food insecurity is associated with decreased quality of doctor–patient communication, as shown in Figure 1.
Understanding the association between food security status and doctor–patient communication is necessary, as this aspect of quality of care has been shown to be related to treatment adherence and patient outcomes (Verlinde et al., 2012). To our knowledge, no study to date has examined the association between food insecurity and the quality of healthcare obtained in a population-based sample. In order to address this gap, this study focused on patient–provider communication, a core contributor to the Triple Aim dimension of patients’ experience of care (Berwick et al., 2008; Institute for Healthcare Improvement, 2020).
Therefore, the purpose of this study was to examine the association between food insecurity and healthcare access, utilization, and quality in a sample of middle and later life adults. As shown in Figure 1, we hypothesized that food insecurity would have an association with these outcomes, outside of the effects of traditional measures of socioeconomic status, such as income and insurance status. Additionally, given the heterogeneity among those in different age groups, we also sought to assess whether the associations between food insecurity and these aspects of healthcare differed across middle and late adulthood. In sum, this study was designed to expand upon previous studies pertaining to access and utilization, as well as to be the first to comment on the quality of care received by food insecure midlife adults and older adults.
Methods
Surveys
Data collected by the California Health Interview Survey (CHIS) were used. The CHIS is a telephone survey of noninstitutionalized individuals residing in California. The survey employs a random-digit-dial sample, which allowed for random selection of households. Within each household, one adult was randomly selected to complete the interview. Interviews were conducted in six different languages: English, Spanish, Chinese, Vietnamese, Korean, and Tagalog. Since 2011, the survey has been conducted continuously, on a two-year basis (“CHIS Methodology Documentation,” 2012).
Sample
Data were collected between June 2011 and December 2016 and included 125,264 individuals. The analytic sample was restricted to individuals who were over the age of 55 years and included 72,212 individuals. Of this group, 26,739 were between the ages of 55 and 64 years; 24,191 were between the ages of 65 and 74 years; and 21,282 were aged 75 years or older. The unweighted proportions of individuals in each age group were 37.0%, 33.5%, and 29.5%, respectively. Models assessing healthcare access and utilization included the full analytic sample. Models assessing quality of care received were restricted to individuals with a personal doctor (n = 64,213). Sample weights were employed to account for the sampling design and nonrespondents.
Measures
Independent variables.
Level of food security was measured using the CHIS-provided variable, derived from the United States Department of Agriculture six-item short form of the Food Security Survey Module (Supplementary Item 1; Blumberg et al., 1999). Only individuals with an income level less than 200% of the federal poverty level (FPL) who responded were divided into three categories: 1 = food secure (FS), 2 = low food security (L-FS), and 3 = very low food security (VL-FS). Those with income levels greater than or equal to 200% of the FPL were assumed to be food secure, as has been done previously (Walsemann et al., 2017). Age (1 = 55–64 years, 2 = 65–74 years, and 3 = 75+ years) was also assessed as an independent variable.
Outcomes.
Measures of decreased healthcare access included delaying seeking care (0 = no and 1 = yes) and delaying filling a prescription (0 = no and 1 = yes) within the past 12 months. Decreased access was also indicated by not having a usual source of care other than the emergency department (0 = no and 1 = yes). Measures of increased healthcare utilization included seeing a physician within the past 12 months (0 = no and 1 = yes) and being admitted to an emergency department within the past 12 months (0 = no and 1 = yes). These measures have been utilized in previous studies (Vargas Bustamante et al., 2012). Decreased quality of healthcare specifically focused on doctor–patient communication and was assessed through two single items: having a doctor who did not always listen carefully (0 = no and 1 = yes) and having a doctor who did not always carefully explain aspects of medical care (0 = no and 1 = yes). Responses originally included never, usually, sometimes, or always, but were dichotomized for this study. These questions were similar to those asked on the Consumer Assessment of Healthcare Providers and Systems (CAHPS) Experience of Care and Health Outcomes Survey, which is a standardized measure used to assess the behavioral healthcare experiences of health insurance enrollees (“CAHPS Mental Health Care Surveys,” 2019; Eisen et al., 1999; Shaul et al., 2001).
Covariates.
Other covariates included gender (1 = male and 2 = female), race/ethnicity (1 = non-Hispanic white, 2 = Hispanic, 3 = Asian, 4 = Black/African American, and 5 = other), marital status (1 = married/living with a partner, 2 = widowed/divorced/separated, and 3 = never married), general health status (1 = excellent/very good and 2 = good/fair/poor), a summary score of the number of chronic conditions had, which included heart disease, asthma, and diabetes (0–3), level of education (1 = high school or less and 2 = more than high school), employment status (1 = full-time, 2 = unemployed and not seeking employment, 3 = unemployed and seeking employment, and 4 = part-time and other), insurance status (1 = uninsured, 2 = Medicare and Medicaid, 3 = Medicare and others, 4 = Medicare only, 5 = Medicaid, 6 = employment-based, 7 = privately purchased, and 8 = other public insurance), place of birth (1 = US born and 2 = not US born), English proficiency (1 = proficient and 2 = not proficient), household pretax annual income (1 = $0–29,999, 2 = $30,000–59,999, 3 = $60,000–89,999, 4 = $90,000–1199,999, 5 = $120,000–149,999, 6 = $150,000–179,999, and 7 = $180,000 or more), time (1 = 2011, 2 = 2012, 3 =2013, 4 = 2014, 5 = 2015, and 6 = 2016), and household size (1–10 people).
Statistical Analyses
All analyses were conducted in Stata 16 (StataCorp, 2019). Pearson chi-square tests, employing jackknife replicate weights, were used to assess differences in demographics among the three levels of food security. Results informed the covariates used in multivariable analysis. Logistic regression, employing jackknife replicate weights, was used to test the odds of experiencing each of the measures of healthcare access, utilization, and quality. Models first controlled only for level of food insecurity and age. Models then also controlled for gender, race/ethnicity, marital status, general health status, number of chronic conditions, level of education, employment status, insurance status, place of birth, English proficiency, income, year of survey administration, and household size. Odds ratios and 95% confidence intervals were reported. Finally, to examine whether the relationships between food security status and the measures of healthcare access, utilization, and quality varied across middle and late adulthood, models were run testing the interaction between food insecurity level and age. Models with and without the interaction terms were compared using Wald tests to assess how well they fit the data. Models with interaction terms that better fit the data were then subject to further analyses. Specifically, pairwise comparisons were conducted within each age group to compare the predicted probability of the outcome occurring between food security levels. All analyses employed a significance cutoff of p ≤ .05.
Results
Bivariate analysis revealed significant differences in the covariates among the food insecurity groups. Thus, each demographic variable (Table 1) was controlled for in the multivariable analyses.
Table 1.
Characteristics of Respondents According to Food Insecurity Level.
| Food secure,a % |
Low food security,b % |
Very low food security,c % |
|
|---|---|---|---|
| Age, years | |||
| 55–64 | 47.2 | 54.1 | 64.0 |
| 65–74 | 29.3 | 29.6 | 26.4 |
| 75+ | 23.5 | 16.3 | 9.6 |
| Gender | |||
| Male | 46.8 | 39.5 | 42.4 |
| Female | 53.2 | 60.5 | 57.6 |
| Race/ethnicity | |||
| non-Hispanic white | 62.2 | 21.9 | 37.6 |
| Hispanic | 18.9 | 51.6 | 38.9 |
| Asian | 11.1 | 17.0 | 5.7 |
| Black/African American | 5.5 | 7.3 | 12.2 |
| Other | 2.3 | 2.3 | 5.7 |
| Marital status | |||
| Married/partner | 66.7 | 52.7 | 35.5 |
| Widowed/divorced/separated | 27.8 | 37.9 | 51.2 |
| Never married | 5.5 | 9.3 | 13.3 |
| General health | |||
| Excellent/very good | 47.4 | 15.3 | 11.5 |
| Good/fair/poor | 52.6 | 84.7 | 88.5 |
| Number of chronic illnesses | |||
| 0 | 64.7 | 53.6 | 43.6 |
| 1 | 28.3 | 34.1 | 38.9 |
| 2 | 6.3 | 10.6 | 13.8 |
| 3 | .8 | 1.7 | 3.7 |
| Education level | |||
| High school or less | 35.6 | 71.0 | 62.2 |
| More than high school | 64.4 | 29.0 | 37.8 |
| Employment status | |||
| Full-time | 34.0 | 20.5 | 16.3 |
| Unemployed, not looking | 56.3 | 65.9 | 67.3 |
| Unemployed, looking | 2.5 | 6.8 | 8.1 |
| Part-time & other | 7.2 | 6.8 | 8.2 |
| Insurance status | |||
| Uninsured | 5.1 | 13.4 | 12.6 |
| Medicare & Medicaid | 9.0 | 32.8 | 33.7 |
| Medicare & others | 38.4 | 11.0 | 9.0 |
| Medicare only | 4.8 | 5.7 | 4.9 |
| Medicaid | 4.1 | 23.2 | 26.4 |
| Employment-based | 32.6 | 9.1 | 8.1 |
| Privately purchased | 4.9 | 2.8 | 2.4 |
| Other public | 1.1 | 2.0 | 2.9 |
| Place of birth | |||
| US born | 73.7 | 37.1 | 58.8 |
| Not US born | 26.4 | 62.9 | 41.2 |
| Proficiency in English | |||
| English proficient | 80.5 | 38.1 | 63.2 |
| Not English proficient | 19.5 | 61.9 | 36.8 |
| Income | |||
| 0–29,999 | 23.2 | 88.8 | 90.4 |
| 30,000–59,999 | 25.6 | 10.9 | 9.4 |
| 60,000–89,999 | 18.7 | .3 | .2 |
| 90,000–119,999 | 12.1 | .0 | .0 |
| 120,000–149,999 | 6.4 | .0 | .0 |
| 150,000–179,999 | 5.2 | .0 | .0 |
| 180,000 or more | 8.9 | .0 | .0 |
| Household size | |||
| 1 | 20.9 | 19.6 | 36.2 |
| 2 | 46.5 | 30.1 | 24.2 |
| 3 | 16.6 | 20.4 | 15.7 |
| 4 | 8.9 | 11.9 | 9.0 |
| 5 | 3.7 | 8.0 | 7.1 |
| 6 | 2.1 | 4.6 | 3.7 |
| 7 | .7 | 3.1 | 2.0 |
| 8 | .4 | 1.3 | .6 |
| 9 | .2 | .3 | .9 |
| 10 | .1 | .6 | .5 |
| Delay care in the past 12 months | |||
| Yes | 9.0 | 16.0 | 26.3 |
| No | 91.0 | 84.0 | 73.7 |
| Delay prescription in the past 12 months | |||
| Yes | 9.0 | 16.5 | 31.3 |
| No | 91.0 | 83.6 | 68.7 |
| Have a usual source of care | |||
| Yes | 93.9 | 81.8 | 85.0 |
| No | 6.1 | 18.3 | 15.0 |
| Doctor visit in the past 12 months | |||
| Yes | 89.8 | 85.0 | 84.6 |
| No | 10.2 | 15.0 | 15.4 |
| Emergency room visit in the past 12 months | |||
| Yes | 20.5 | 28.5 | 39.7 |
| No | 79.5 | 71.5 | 60.3 |
| Doctor always listens carefullyd | |||
| Yes | 74.7 | 66.2 | 65.5 |
| No | 25.3 | 33.8 | 34.5 |
| Doctor always explains carefullyd | |||
| Yes | 73.1 | 62.9 | 59.4 |
| No | 26.9 | 37.2 | 40.6 |
n = 65,805.
n = 4143.
n = 2264.
Questions pertaining to quality of care were asked only to those who reported having a personal doctor (n = 64,213).
Healthcare Access
Results from the unadjusted (Model 1) and adjusted (Model 2) models that regressed access to healthcare on food security status and age (n = 72,212) are shown in Table 2. VL-FS was most likely, followed by L-FS, to delay care (odds ratio (OR) [95% confidence interval (CI)] = 2.7, 95% CI = [2.1, 3.5] and OR = 1.9, 95% CI = [1.5, 2.5], respectively; analyses available on request) as compared to FS. Additionally, VL-FS was also most likely, followed by L-FS to delay filling a prescription (OR = 3.4, 95% CI = [2.5, 4.8] and OR = 1.9, 95% CI = [1.5, 2.4], respectively; analyses available on request) as compared to FS. Furthermore, compared to FS, VL-FS and L-FS were more likely not to have a usual source of care other than the emergency department (OR = 1.7, 95% CI = [1.3, 2.3] and OR = 1.5, 95% CI = [1.2, 2.0], respectively). Examination of the effect of age revealed that compared to those aged 55–64 years, those aged 75+ years were least likely, followed by those aged 65–74 years, to delay receiving care (OR = .3, 95% CI = [.3, .4] and OR = .6, 95% CI = [.4, .7], respectively; analyses available on request). Additionally, those aged 75+ years were least likely, followed by those aged 65–74 years, to delay filling a prescription (OR = .5, 95% CI = [.3, .6] and OR = .6, 95% CI = [.5, .8], respectively; analyses available on request), as compared to those aged 55–64 years. Age groups did not differ in regard to likelihood of having a usual source of care other than the emergency department (analyses available on request).
Table 2.
Food Insecurity and Age Differences in Access to Healthcare.
| Delay receiving carea | Delay filling a prescriptiona | No usual source of care other than the emergency departmenta |
|
|---|---|---|---|
| Model 1 (without covariates) | |||
| FS lvlb (FS)c | OR [95% CI] | OR [95% CI] | OR [95% CI] |
| Low FSc | 1.8 [1.5, 2.2]*** | 1.9 [1.6, 2.3]*** | 3.4 [2.7, 4.2]*** |
| Very low FSc | 3.2 [2.6, 3.9]*** | 4.3 [3.2, 5.7]*** | 2.9 [2.2, 3.7]*** |
| Age, years (55–64) | |||
| 65–74 | .5 [.4, .6]*** | .7 [.6, .8]*** | .5 [.5, .7]*** |
| 75+ | .3 [.3, .4]*** | .6 [.5, .7]*** | .6 [.5, .7]*** |
| Model 2 (adjusted models with covariates) | |||
| FS lvlb (FS)c | OR [95% CI] | OR [95% CI] | OR [95% CI] |
| Low FSc | 1.9 [1.5, 2.5]*** | 1.9 [1.5, 2.4]*** | 1.5 [1.2, 2.0]** |
| Very low FSc | 2.7 [2.1, 3.5]*** | 3.4 [2.5, 4.8]*** | 1.7 [1.3, 2.3]*** |
| Age, years (55–64) | |||
| 65–74 | .6 [.4, .7]*** | .6 [.5, .8]*** | 1.1 [.9, 1.4] |
| 75+ | .3 [.3, .4]*** | .5 [.3, .6]*** | 1.3 [1.0, 1.7] |
| Gender (male) | |||
| Female | 1.3 [1.1, 1.4]*** | 1.3 [1.2, 1.5]*** | .7 [.6, .9]*** |
| Race/ethnicity (non-Hispanic white) | |||
| Hispanic | .8 [.7, 1.0] | .9 [.8, 1.2] | 1.3 [1.0, 1.7]* |
| Asian | .6 [.5, .8]** | .7 [.5, .9]* | 1.2 [.9, 1.6] |
| Black/African American | .7 [.6, .9]* | 1.0 [.8, 1.2] | 1.1 [.8, 1.5] |
| Other | 1.1 [.8, 1.5] | 1.2 [.9, 1.5] | .9 [.6, 1.4] |
| Marital (married/partnerd) | |||
| Wid/div/sepe | 1.2 [1.0, 1.4]* | 1.4 [1.2, 1.7]*** | 1.1 [.9, 1.3] |
| Never married | 1.1 [.8, 1.4] | 1.4 [1.1, 1.8]* | 1.4 [1.0, 1.9]* |
| General health (excellent/very good) | |||
| Good/fair/poor | 2.0 [1.7, 2.3]*** | 2.0 [1.7, 2.3]*** | .7 [.6, .9]** |
| Number of chronic conditions (0) | |||
| 1 | 1.0 [.9, 1.1] | 1.4 [1.2, 1.7]*** | .8 [.7, .9]** |
| 2 | 1.1 [.9, 1.4] | 1.6 [1.3, 1.9]*** | .5 [.4, .7]*** |
| 3 | 1.0 [.6, 1.8] | 1.8 [1.0, 3.1]* | .5 [.2, 1.4] |
| Education level (HSf or less) | |||
| More than HSf | 1.5 [1.3, 1.7]*** | 1.2 [1.1, 1.4]** | .8 [.7, .9]** |
| Employment status (full-time) | |||
| Not lookingg | 1.0 [.8, 1.1] | .9 [.8, 1.1] | .8 [.7, 1.0] |
| Lookingh | 1.3 [.9, 1.8] | 1.3 [.9, 1.8] | 1.0 [.7, 1.3] |
| PT & otheri | 1.0 [.9, 1.3] | 1.1 [.8, 1.4] | .8 [.6, 1.1] |
| Insurance status (insured) | |||
| Medicare & Medicaid | .5 [.3, .6]*** | 1.1 [.8, 1.5] | .2 [.1, .2]*** |
| Medicare & others | .4 [.3, .6]*** | 1.1 [.8, 1.5] | .1 [.1, .1]*** |
| Medicare only | .5 [.3, .7]*** | 1.3 [.9, 1.8] | .3 [.2, .4]*** |
| Medicaid only | .5 [.4, .7]*** | .8 [.6, 1.1] | .3 [.2, .4]*** |
| Employment-based | .4 [.3, .6]*** | 1.0 [.7, 1.2] | .1 [.1, .2]*** |
| Privately purchased | .8 [.6, 1.1] | 1.4 [1.0, 2.0] | .3 [.2, .4]*** |
| Other public | .6 [.4, .9]** | .9 [.5, 1.4] | .2 [.1, .4]*** |
| Place of birth (US born) | |||
| Not US born | .8 [.6, 1.0]* | .8 [.6, 1.0]* | 1.3 [.9, 1.7] |
| English proficiency (proficient) | |||
| Not proficient | .8 [.6, 1.1] | .9 [.7, 1.2] | 1.4 [1.0, 1.9] |
| Income (0–29,999) | |||
| 30,000–59,999 | 1.1 [.9, 1.3] | 1.1 [1.0, 1.3] | .9 [.7, 1.0] |
| 60,000–89,999 | 1.1 [.9, 1.3] | 1.1 [.9, 1.3] | .6 [.4, .7]*** |
| 90,000–119,999 | 1.1 [.8, 1.4] | 1.2 [.9, 1.5] | .8 [.5, 1.1] |
| 120,000–149,999 | .8 [.6, 1.1] | 1.1 [.9, 1.5] | .5 [.3, 1.0]* |
| 150,000–179,999 | 1.0 [.7, 1.5] | 1.1 [.7, 1.6] | .8 [.5, 1.2] |
| 180,000 or more | 1.0 [.7, 1.3] | 1.1 [.8, 1.4] | .5 [.3, .7]*** |
| Time (2011) | |||
| 2012 | 1.0 [.8, 1.1] | 1.0 [.9, 1.2] | 1.0 [.8, 1.2] |
| 2013 | 1.0 [.8, 1.2] | .9 [.7, 1.0] | .8 [.6, 1.0]* |
| 2014 | 1.0 [.8, 1.1] | .8 [.7, 1.0] | 1.0 [.8, 1.3] |
| 2015 | .9 [.7, 1.0] | .9 [.7, 1.1] | 1.1 [.8, 1.3] |
| 2016 | .8 [.6, 1.0]* | .9 [.7, 1.1] | 1.2 [1.0, 1.6] |
| Household size (1) | |||
| 2 | .9 [.7, 1.1] | 1.0 [.8, 1.2] | .7 [.6, .9]** |
| 3 | .9 [.7, 1.1] | 1.2 [.9, 1.5] | .9 [.7, 1.2] |
| 4 | 1.1 [.9, 1.4] | 1.3 [1.0, 1.7]* | .8 [.6, 1.1] |
| 5 | .9 [.6, 1.2] | .9 [.6, 1.3] | .9 [.6, 1.3] |
| 6 | .7 [.5, 1.2] | 1.3 [.8, 2.0] | 1.2 [.7, 2.1] |
| 7 | .5 [.2, 1.5] | 1.4 [.6, 3.4] | .6 [.3, 1.2] |
| 8 | 1.1 [.4, 2.9] | .9 [.4, 2.2] | 2.7 [.9, 7.6] |
| 9 | 1.0 [.3, 3.6] | 2.0 [.8, 5.1] | 1.7 [.2, 2.1] |
| 10 | .6 [.2, 2.1] | 2.3 [.6, 9.6] | 1.4 [.4, 5.3] |
Note. OR = odds ratio; CI = confidence interval.
p ≤ .05
p < .01
p < .001.
n = 72,212
Food security level.
Food secure.
Living with partner.
Widowed/divorced/separated.
High school.
Unemployed and not looking for employment.
Unemployed and looking for employment.
Part-time and other.
Healthcare Utilization
The results from the unadjusted (Model 1) and adjusted (Model 2) regression models examining indicators of healthcare utilization as the dependent measures (n = 72,212) are shown in Table 3. Food insecurity groups did not differ in likelihood of having seen a doctor within the past 12 months (analyses available on request). However, VL-FS and L-FS had greater odds of visiting an emergency department within the past 12 months than did FS (OR = 1.6, 95% CI = [1.2, 2.1] and OR = 1.2, 95% CI = [1.0, 1.5], respectively). Assessment of the regression results pertaining to age group showed that compared to those aged 55–64 years, those aged 75+ years and 65–74 years were less likely to have seen a doctor in the past 12 months (OR = .6, 95% CI = [.5, .8] and OR = .7, 95% CI = [.6, .9], respectively). Those aged 65–74 years were less likely to have an emergency department admission within the past 12 months (OR = .7, 95% CI = [.6, .9]) than those aged 55–64 years. Those aged 75+ years were more likely to have an emergency department admission within the past 12 months than those aged 65–74 years (analyses available on request), but did not differ in likelihood from those aged 55–64 years.
Table 3.
Food Insecurity and Age Differences in Utilization and Quality of Healthcare.
| Seen doctor in past 12 monthsa | ED admission in past 12 monthsa |
Doctor does not always listenb |
Doctor does not always explain carefullyb |
|
|---|---|---|---|---|
| Model 1 (without covariates) | ||||
| FS lvlc (FS)d | OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] |
| Low FSd | .7 [.5, .8]** | 1.6 [1.4, 1.9]*** | 1.5 [1.2, 1.8]*** | 1.6 [1.3, 2.0]*** |
| Very low FSd | .7 [.4, 1.0] | 2.7 [2.2, 3.5]*** | 1.5 [1.1, 2.0]** | 1.9 [1.4, 2.5]*** |
| Age, years (55–64) | ||||
| 65–74 | 1.7 [1.5, 2.0]*** | 1.1 [1.0, 1.2]* | .8 [.8, .9]*** | .9 [.8, 1.0]** |
| 75+ | 1.7 [1.4, 2.0]*** | 1.5 [1.4, 1.7]*** | .8 [.7, .9]*** | 1.0 [.9, 1.1] |
| Model 2 (adjusted models with covariates) | ||||
| FS lvlc (FS)d | OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] |
| Low FSd | 1.0 [.7, 1.3] | 1.2 [1.0, 1.5]* | 1.2 [.9, 1.5] | 1.3 [1.0, 1.6]* |
| Very low FSd | .8 [.5, 1.3] | 1.6 [1.2, 2.1]** | 1.3 [1.0, 1.8] | 1.7 [1.3, 2.4]** |
| Age, years (55–64) | ||||
| 65–74 | .7 [.6, .9]** | .7 [.6, .9]** | 1.0 [.8, 1.2] | 1.0 [.8, 1.2] |
| 75+ | .6 [.5, .8]*** | .9 [.7, 1.0] | .9 [.8, 1.1] | 1.2 [1.0, 1.4] |
| Gender (male) | ||||
| Female | 1.2 [1.1, 1.4]** | .9 [.8, 1.0]** | 1.1 [1.0, 1.2] | 1.0 [1.0, 1.1] |
| Race/ethnicity (non-Hispanic white) | ||||
| Hispanic | 1.0 [.8, 1.3] | .9 [.7, 1.0] | .9 [.7, 1.0] | .8 [.6, .9]** |
| Asian | .7 [.5, .9]** | .7 [.5, .8]*** | 1.2 [1.0, 1.4] | 1.1 [.9, 1.3] |
| Black/African American | 1.1 [.8, 1.5] | 1.2 [1.0, 1.4] | .7 [.5, .8]*** | .6 [.5, .8]*** |
| Other | .7 [.5, 1.0]* | 1.4 [1.1, 1.7]* | .9 [.7, 1.2] | .8 [.6, 1.1] |
| Marital (married/partnere) | ||||
| Wid/div/sepf | 1.0 [.8, 1.1] | 1.2 [1.1, 1.4]*** | 1.0 [.9, 1.2] | 1.0 [.9, 1.2] |
| Never married | .8 [.6, 1.0] | .9 [.8, 1.1] | 1.0 [.8, 1.2] | 1.1 [.9, 1.3] |
| General health (excellent/very good) | ||||
| Good/fair/poor | 1.5 [1.3, 1.7]*** | 1.8 [1.7, 2.1]*** | 1.3 [1.2, 1.4]*** | 1.4 [1.3, 1.6]*** |
| Number of chronic conditions (0) | ||||
| 1 | 1.8 [1.5, 2.1]*** | 1.4 [1.3, 1.6]*** | .9 [.8, 1.0]* | .9 [.8, .9]** |
| 2 | 2.3 [1.8, 3.1]*** | 2.1 [1.8, 2.4]*** | .8 [.7, 1.0]* | .9 [.7, 1.0] |
| 3 | 3.0 [1.4, 6.2]** | 2.8 [1.9, 4.1]*** | .6 [.4, .8]** | .6 [.4, .9]* |
| Education level (HSg or less) | ||||
| More than HSg | 1.3 [1.1, 1.5]** | 1.1 [1.0, 1.2] | 1.1 [1.0, 1.3]** | 1.2 [1.1, 1.3]*** |
| Employment status (full-time) | ||||
| Not lookingh | 1.4 [1.2, 1.7]*** | 1.4 [1.2, 1.5]*** | .9 [.8, 1.0] | .9 [.8, 1.1] |
| Lookingi | 1.3 [.9, 1.8] | 1.1 [.8, 1.6] | 1.4 [1.0, 1.8]* | 1.3 [.9, 1.8] |
| PT & otherj | 1.3 [.9, 1.7] | 1.1 [.9, 1.4] | 1.0 [.8, 1.2] | 1.0 [.9, 1.2] |
| Insurance status (uninsured) | ||||
| Medicare & Medicaid | 6.0 [4.4, 8.2]*** | 2.1 [1.6, 2.8]*** | .8 [.6, 1.2] | .9 [.6, 1.2] |
| Medicare & others | 8.7 [6.4, 11.9]*** | 1.7 [1.3, 2.2]*** | .8 [.6, 1.2] | .9 [.6, 1.2] |
| Medicare only | 4.9 [3.5, 6.8]*** | 1.6 [1.2, 2.2]** | .8 [.6, 1.1] | .8 [.6, 1.2] |
| Medicaid only | 3.1 [2.3, 4.3]*** | 2.0 [1.5, 2.6]*** | 1.1 [.8, 1.5] | .9 [.6, 1.4] |
| Employment-based | 4.6 [3.6, 5.8]*** | 1.2 [1.0, 1.6] | 1.0 [.8, 1.4] | 1.0 [.7, 1.3] |
| Privately purchased | 2.6 [1.9, 3.5]*** | 1.2 [.8, 1.7] | 1.0 [.7, 1.5] | 1.1 [.8, 1.5] |
| Other public | 5.5 [3.6, 8.6]*** | 1.9 [1.3, 2.7]** | .8 [.5, 1.2] | .8 [.5, 1.2] |
| Place of birth (US born) | ||||
| Not US born | 1.0 [.8, 1.2] | 1.0 [.8, 1.2] | .9 [.8, 1.1] | 1.1 [.9, 1.3] |
| English proficiency (proficient) | ||||
| Not proficient | 1.0 [.8, 1.3] | .8 [.6, .9]* | 1.3 [1.1, 1.6]** | 1.5 [1.3, 1.8]*** |
| Income (0–29,999) | ||||
| 30,000–59,999 | 1.3 [1.1, 1.6]** | 1.1 [1.0, 1.3] | .9 [.8, 1.1] | .9 [.8, 1.1] |
| 60,000–89,999 | 1.3 [1.1, 1.6]* | 1.0 [.8, 1.1] | .9 [.8, 1.0] | .9 [.8, 1.0] |
| 90,000–119,999 | 1.4 [1.1, 1.9]** | 1.0 [.9, 1.3] | .8 [.7, 1.0]* | .9 [.7, 1.1] |
| 120,000–149,999 | 1.9 [1.3, 2.7]*** | 1.0 [.8, 1.3] | .7 [.6, .9]** | .8 [.7, 1.0] |
| 150,000–179,999 | 1.7 [1.2, 2.4]** | 1.0 [.8, 1.4] | .8 [.6, 1.1] | .9 [.7, 1.2] |
| 180,000 or more | 1.7 [1.3, 2.2]*** | 1.1 [.9, 1.3] | .7 [.6, .9]** | .8 [.6, .9]** |
| Time (2011) | ||||
| 2012 | 1.1 [1.0, 1.3] | 1.2 [1.0, 1.3]* | 1.1 [1.0, 1.3]* | 1.1 [1.0, 1.2] |
| 2013 | .9 [.8, 1.1] | 1.0 [.9, 1.2] | 1.0 [.9, 1.2] | 1.1 [.9, 1.2] |
| 2014 | 1.0 [.8, 1.2] | 1.0 [.8, 1.1] | .9 [.8, 1.1] | .9 [.8, 1.0] |
| 2015 | .9 [.7, 1.1] | 1.1 [1.0, 1.2] | 1.2 [1.0, 1.3]* | 1.0 [.9, 1.2] |
| 2016 | .9 [.7, 1.1] | 1.1 [.9, 1.3] | 1.1 [.9, 1.3] | 1.1 [.9, 1.2] |
| Household size (1) | ||||
| 2 | 1.1 [.9, 1.3] | 1.0 [.9, 1.2] | 1.0 [.9, 1.1] | 1.1 [.9, 1.2] |
| 3 | 1.0 [.8, 1.3] | 1.1 [.9, 1.3] | 1.0 [.9, 1.2] | 1.0 [.8, 1.1] |
| 4 | .9 [.7, 1.2] | 1.0 [.8, 1.2] | 1.1 [.9, 1.3] | 1.1 [.9, 1.3] |
| 5 | 1.1 [.8, 1.6] | 1.1 [.8, 1.4] | 1.1 [.9, 1.5] | 1.1 [.8, 1.4] |
| 6 | .9 [.5, 1.5] | 1.0 [.7, 1.5] | 1.4 [.9, 2.1] | 1.4 [.9, 2.0] |
| 7 | 1.2 [.6, 2.4] | 1.4 [.8, 2.4] | 1.7 [1.0, 2.9] | .9 [.5, 1.6] |
| 8 | 1.2 [.4, 3.5] | 1.5 [.7, 3.3] | 1.5 [.6, 3.7] | 1.5 [.6, 3.6] |
| 9 | .3 [.1, 1.4] | 1.4 [.6, 3.4] | 2.1 [.9, 5.3] | 2.0 [.8, 4.8] |
| 10 | 6.8 [1.3, 35]* | 4.2 [.7, 24.4] | 1.8 [.3, 9.1] | 1.0 [.2, 5.1] |
Note. OR = odds ratio; CI = confidence interval.
p ≤ .05
p <.01
p < .001.
n = 72,212.
n = 64,213.
Food security level.
Food secure.
Living with partner.
Widowed/divorced/separated.
High school.
Unemployed and not looking for employment.
Unemployed and looking for employment.
Part-time and other.
Healthcare Quality
Results from the unadjusted (Model 1) and adjusted (Model 2) models regressing the quality of care received among those with a personal doctor (n = 64,213) on food security status and age are shown in Table 3. The likelihood of having a doctor who did not always listen carefully did not differ by food security level. However, VL-FS and L-FS were more likely than FS to lack a doctor who always explained aspects of care carefully (OR = 1.7, 95% CI = [1.3, 2.4] and OR = 1.3, 95% CI = [1.0, 1.6], respectively). In regard to regression results pertaining to the effects of age, age groups did not differ in likelihood of having a doctor who did not always listen carefully (analyses available on request). Those aged 75+ years and 65–74 years did not differ from those aged 55–64 years in likelihood of having a doctor who did not always explain aspects of care carefully. However, those aged 75+ years were more likely than those aged 65–74 years to have a doctor who did not always explain aspects of care carefully (analyses available on request).
Testing the Interaction of Food Security Status and Age
Analyses testing whether the relationship between food security status and healthcare access and utilization varied across adulthood and late adulthood found no evidence of a significant interaction between food security status and age (results shown in Tables 4 and 5). In regard to quality of care, there was a significant interaction within the model assessing the likelihood of not having a physician who always explained aspects of care carefully. However, a Wald test confirmed that the interaction terms did not significantly improve the fit of the model, however; thus, the interactions were not subject to further analysis. There was one significant interaction that did improve model fit: the interaction between food security status and age was significantly associated with the likelihood of having a physician who always listened carefully (results shown in Table 5). Specifically, among those aged 65–74 years, VL-FS was more likely than FS to have a doctor who did not always listen carefully (Predicted Probability (Pr) = .4, 95% CI = [.3, .5] and Pr = .2, 95% CI = [.2, .3], respectively; analyses available on request). Additionally, among those aged 75+ years and older, VL-FS were less likely to have a doctor who did not always listen carefully than L-FS and FS (Pr = .1, 95% CI = [.01, .2], Pr = .3, 95% CI = [.2, .4], and Pr = .2, 95% CI = [.2, .2], respectively; analyses available on request). These interactions are graphed in Figure 2.
Table 4.
Food Insecurity and Age Differences in Access to Healthcare Adjusted for the Interaction Between Food Insecurity Level and Age.
| Delay receiving carea | Delay filling a prescriptiona | No usual source of care other than the emergency departmenta |
|
|---|---|---|---|
| FS lvlb (FS)c | OR [95% CI] | OR [95% CI] | OR [95% CI] |
| Low FSc | 1.6 [1.2, 2.2]** | 1.7 [1.2, 2.3]** | 1.3 [1.0, 1.9] |
| Very low FSc | 2.4 [1.8, 3.2]*** | 3.2 [2.3, 4.5]*** | 1.9 [1.3, 2.6]** |
| Age, years (55–64) | |||
| 65–74 | .5 [.4, .7]*** | .6 [.4, .7]*** | 1.1 [.8, 1.4] |
| 75+ | .3 [.2, .4]*** | .4 [.3, .5]*** | 1.2 [.9, 1.6] |
| Interaction | |||
| 65–74 × low FSc | 1.7 [.9, 3.0] | 1.3 [.8, 2.2] | 1.4 [.8, 2.4] |
| 65–74 × very low FSc | 1.3 [.7, 2.5] | 1.3 [.6, 2.6] | 1.5 [.7, 3.0] |
| 75+ × low FSc | 1.7 [.9, 3.0] | 1.1 [.6, 1.8] | .6 [.2, 1.5] |
| 75+ × very low FSc | .9 [.3, 2.9] | 1.8 [.2, 14.0] | 1.2 [.4, 3.3] |
| Gender (male) | |||
| Female | 1.3 [1.1, 1.4]*** | 1.3 [1.2, 1.5]*** | .7 [.6, .9]*** |
| Race/ethnicity (non-Hispanic white) | |||
| Hispanic | .8 [.7, 1.0] | 1.0 [.8, 1.2] | 1.3 [1.0, 1.7]* |
| Asian | .6 [.5, .8]** | .7 [.5, .9]* | 1.2 [.9, 1.6] |
| Black/African American | .7 [.6, 1.0]* | 1.0 [.8, 1.2] | 1.1 [.8, 1.5] |
| Other | 1.1 [.8, 1.5] | 1.2 [.9, 1.5] | .9 [.6, 1.4] |
| Marital (married/partnerd) | |||
| Wid/div/sepe | 1.2 [1.0, 1.4]* | 1.4 [1.2, 1.7]*** | 1.1 [.9, 1.3] |
| Never married | 1.1 [.8, 1.4] | 1.4 [1.1, 1.8]* | 1.4 [1.0, 1.9]* |
| General health (excellent/very good) | |||
| Good/fair/poor | 2.0 [1.7, 2.3]*** | 2.0 [1.7, 2.3]*** | .7 [.6, .9]** |
| Number of chronic conditions (0) | |||
| 1 | 1.0 [.9, 1.1] | 1.4 [1.2, 1.7]*** | .8 [.7, .9]** |
| 2 | 1.1 [.9, 1.4] | 1.6 [1.3, 1.9]*** | .5 [.4, .7]*** |
| 3 | 1.0 [.6, 1.8] | 1.8 [1.0, 3.2]* | .5 [.2, 1.4] |
| Education level (HSf or less) | |||
| More than HSf | 1.5 [1.3, 1.7]*** | 1.3 [1.1, 1.4]** | .8 [.7, .9]** |
| Employment status (full-time) | |||
| Not lookingg | 1.0 [.8, 1.1] | .9 [.8, 1.1] | .8 [.7, 1.0] |
| Lookingh | 1.3 [.9, 1.8] | 1.3 [.9, 1.8] | 1.0 [.7, 1.3] |
| PT & otheri | 1.1 [.9, 1.3] | 1.1 [.8, 1.4] | .8 [.6, 1.1] |
| Insurance status (uninsured) | |||
| Medicare & Medicaid | .5 [.3, .6]*** | 1.0 [.7, 1.5] | .2 [.1, .2]*** |
| Medicare & others | .5 [.3, .7]*** | 1.1 [.8, 1.6] | .1 [.1, .1]*** |
| Medicare only | .5 [.3, .7]*** | 1.3 [.9, 1.8] | .3 [.2, .4]*** |
| Medicaid only | .6 [.4, .7]*** | .8 [.6, 1.1] | .3 [.2, .4]*** |
| Employment-based | .4 [.3, .5]*** | .9 [.7, 1.2] | .1 [.1, .2]*** |
| Privately purchased | .8 [.6, 1.1] | 1.4 [1.0, 2.0] | .3 [.2, .4]*** |
| Other public | .6 [.4, .9]** | .9 [.5, 1.4] | .2 [.1, .3]*** |
| Place of birth (US born) | |||
| Not US born | .8 [.6, 1.0]* | .8 [.6, 1.0]* | 1.3 [.9, 1.7] |
| English proficiency (proficient) | |||
| Not proficient | .8 [.6,1.1] | .9 [.7, 1.2] | 1.4 [1.0, 1.9] |
| Income (0–29,999) | |||
| 30,000–59,999 | 1.1 [.9, 1.3] | 1.1 [1.0, 1.3] | .9 [.7, 1.0] |
| 60,000–89,999 | 1.1 [.9, 1.3] | 1.1 [.9, 1.3] | .6 [.4, .7]*** |
| 90,000–119,999 | 1.1 [.8, 1.4] | 1.2 [.9, 1.5] | .8 [.5, 1.1] |
| 120,000–149,999 | .8 [.6, 1.1] | 1.1 [.9, 1.5] | .5 [.3, 1.0]* |
| 150,000–179,999 | 1.0 [.7, 1.5] | 1.1 [.7, 1.6] | .8 [.5, 1.2] |
| 180,000 or more | 1.0 [.7, 1.3] | 1.1 [.8, 1.4] | .5 [.3, .7]*** |
| Time (2011) | |||
| 2012 | 1.0 [.8, 1.1] | 1.0 [.9, 1.2] | 1.0 [.8, 1.2] |
| 2013 | 1.0 [.8, 1.2] | .9 [.7, 1.0] | .8 [.6, 1.0]* |
| 2014 | 1.0 [.8, 1.1] | .8 [.7, 1.0] | 1.0 [.8, 1.3] |
| 2015 | .9 [.7, 1.0] | .9 [.7, 1.1] | 1.1 [.8, 1.3] |
| 2016 | .8 [.6, 1.0]* | .9 [.7, 1.1] | 1.2 [1.0, 1.5] |
| Household size (1) | |||
| 2 | .9 [.7, 1.1] | 1.0 [.8, 1.2] | .7 [.6, .9]** |
| 3 | .9 [.7, 1.1] | 1.2 [.9, 1.5] | .9 [.7, 1.1] |
| 4 | 1.1 [.9, 1.5] | 1.3 [1.0, 1.7]* | .8 [.6, 1.1] |
| 5 | .9 [.6, 1.2] | .9 [.6, 1.3] | .9 [.6, 1.3] |
| 6 | .8 [.5, 1.2] | 1.3 [.8, 2.0] | 1.2 [.7, 2.1] |
| 7 | .5 [.2, 1.5] | 1.4 [.6, 3.5] | .6 [.3, 1.2] |
| 8 | 1.1 [.4, 2.9] | .9 [.4, 2.2] | 2.7 [1.0, 7.6] |
| 9 | 1.0 [.3, 3.7] | 2.0 [.8, 5.1] | 1.8 [.2, 20.1] |
| 10 | .5 [.1, 2.0] | 2.3 [.6, 9.2] | 1.5 [.4, 5.7] |
Note. OR: odds ratio; CI: confidence interval.
p ≤ .05
p < .01
p < .001.
n = 72,212.
Food security level.
Food secure.
Living with partner.
Widowed/divorced/separated.
High school.
Unemployed and not looking for employment.
Unemployed and looking for employment.
Part-time and other.
Table 5.
Food Insecurity and Age Differences in Utilization and Quality of Healthcare Adjusted for the Interaction Between Food Insecurity Level and Age.
| Seen doctor in past 12 monthsa |
ED admission in past 12 monthsa |
Doctor does not always listenb |
Doctor does not always explain carefullyb |
|
|---|---|---|---|---|
| FS lvlc (FS)d | OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] |
| Low FSd | 1.1 [.8, 1.5] | 1.2 [.9, 1.6] | 1.1 [.8, 1.4] | 1.1 [.8, 1.5] |
| Very low FSd | 1.1 [.7, 1.5] | 1.7 [1.2, 2.4]** | 1.3 [.9, 1.8] | 1.4 [1.0, 1.9] |
| Age, years (55–64) | ||||
| 65–74 | .7 [.6, .9]* | .7 [.6, .9]** | .9 [.8, 1.1] | .9 [.7, 1.1] |
| 75+ | .7 [.5, .9]* | .9 [.7, 1.1] | .9 [.8, 1.1] | 1.1 [.9, 1.3] |
| Interaction | ||||
| 65–74 × low FSd | 1.0 [.6, 1.8] | 1.1 [.7, 1.6] | 1.3 [.8, 2.1] | 1.4 [.9, 2.2] |
| 65–74 × very low FSd | .5 [.3, 1.1] | .9 [.5, 1.4] | 1.1 [.7, 1.9] | 1.3 [.8, 2.3] |
| 75+ × low FSd | .7 [.4, 1.5] | .9 [.5, 1.6] | 1.6 [.9, 3.0] | 1.9 [1.0, 3.4]* |
| 75+ × very low FSd | .2 [.0, 2.6] | .6 [.2, 2.1] | .2 [.1, .7]** | 1.3 [.2, 8.4] |
| Gender (male) | ||||
| Female | 1.2 [1.1, 1.4]** | .9 [.8, 1.0]** | 1.1 [1.0, 1.2] | 1.0 [1.0, 1.1] |
| Race/ethnicity (non-Hispanic white) | ||||
| Hispanic | 1.0 [.8, 1.3] | .9 [.7, 1.0] | .9 [.7, 1.0]* | .8 [.6, .9]** |
| Asian | .7 [.5, .9]** | .7 [.5, .8]*** | 1.2 [1.0, 1.4] | 1.1 [.9, 1.3] |
| Black/African American | 1.1 [.8, 1.5] | 1.2 [1.0, 1.4] | .7 [.5, .8]*** | .6 [.5, .8]*** |
| Other | .7 [.5, .9]* | 1.4 [1.1, 1.7]* | .9 [.7, 1.2] | .8 [.6, 1.1] |
| Marital (married/partnere) | ||||
| Wid/div/sepf | 1.0 [.8, 1.1] | 1.2 [1.1, 1.4]*** | 1.0 [.9, 1.2] | 1.0 [.9, 1.1] |
| Never married | .8 [.6, 1.0] | .9 [.8, 1.1] | 1.0 [.8, 1.2] | 1.1 [.9, 1.3] |
| General health (excellent/very good) | ||||
| Good/fair/poor | 1.5 [1.3, 1.7]*** | 1.8 [1.7, 2.1]*** | 1.3 [1.2, 1.4]*** | 1.4 [1.3, 1.6]*** |
| Number of chronic conditions (0) | ||||
| 1 | 1.8 [1.5, 2.1]*** | 1.4 [1.3, 1.6]*** | .9 [.8, 1.0]* | .9 [.8, .9]** |
| 2 | 2.3 [1.8, 3.1]*** | 2.1 [1.8, 2.4]*** | .8 [.7, 1.0]* | .9 [.7, 1.0] |
| 3 | 3.0 [1.4, 6.4]** | 2.8 [1.9, 4.2]*** | .6 [.4, .8]** | .6 [.4, .9]* |
| Education level (HSg or less) | ||||
| More than HSg | 1.3 [1.1, 1.5]** | 1.1 [1.0, 1.2] | 1.1 [1.0, 1.2]** | 1.2 [1.1, 1.3]*** |
| Employment status (full-time) | ||||
| Not lookingh | 1.4 [1.2, 1.6]*** | 1.3 [1.2, 1.5]*** | .9 [.8, 1.0] | .9 [.8, 1.0] |
| Lookingi | 1.3 [.9, 1.8] | 1.1 [.8, 1.6] | 1.3 [1.0, 1.8]* | 1.3 [.9, 1.8] |
| PT & otherj | 1.3 [.9, 1.7] | 1.1 [.9, 1.4] | 1.0 [.8, 1.2] | 1.0 [.9, 1.2] |
| Insurance status (uninsured) | ||||
| Medicare & Medicaid | 6.1 [4.4, 8.4]*** | 2.1 [1.6, 2.8]*** | .8 [.6, 1.2] | .9 [.6, 1.2] |
| Medicare & others | 8.5 [6.2, 11.7]*** | 1.7 [1.3, 2.2]*** | .9 [.6, 1.2] | .9 [.6, 1.3] |
| Medicare only | 4.8 [3.4, 6.8]*** | 1.6 [1.2, 2.2]** | .8 [.6, 1.1] | .9 [.6, 1.3] |
| Medicaid only | 3.1 [2.2, 4.2]*** | 2.0 [1.5, 2.6]*** | 1.1 [.8, 1.5] | 1.0 [.7, 1.4] |
| Employment-based | 4.7 [3.7, 5.9]*** | 1.2 [1, 1.6] | 1.0 [.8, 1.3] | 1.0 [.7, 1.3] |
| Privately purchased | 2.6 [1.9, 3.6]*** | 1.2 [.8, 1.8] | 1.0 [.7, 1.5] | 1.1 [.7, 1.5] |
| Other public | 5.5 [3.5, 8.6]*** | 1.9 [1.3, 2.7]** | .8 [.5, 1.2] | .8 [.5, 1.2] |
| Place of birth (US born) | ||||
| Not US born | 1.0 [.8, 1.2] | 1.0 [.8, 1.2] | .9 [.8, 1.1] | 1.1 [.9, 1.3] |
| English proficiency (proficient) | ||||
| Not proficient | 1.0 [.8, 1.3] | .8 [.6, .9]* | 1.3 [1.1, 1.6]** | 1.5 [1.3, 1.8]*** |
| Income (0–29,999) | ||||
| 30,000–59,999 | 1.3 [1.1, 1.6]** | 1.1 [1.0, 1.3] | .9 [.8, 1.1] | .9 [.8, 1.1] |
| 60,000–89,999 | 1.3 [1.1, 1.7]** | 1.0 [.8, 1.1] | .9 [.8, 1.0] | .9 [.8, 1.0] |
| 90,000–119,999 | 1.5 [1.1, 1.9]** | 1.1 [.9, 1.3] | .8 [.7, 1.0]* | .9 [.7, 1.1] |
| 120,000–149,999 | 1.9 [1.3, 2.8]*** | 1.0 [.8, 1.3] | .7 [.6, .9]** | .8 [.7, 1.0] |
| 150,000–179,999 | 1.7 [1.3, 2.4]** | 1.0 [.8, 1.4] | .8 [.6, 1.1] | .9 [.7, 1.2] |
| 180,000 or more | 1.7 [1.3, 2.3]*** | 1.1 [.9, 1.3] | .7 [.6, .9]** | .8 [.6, .9]** |
| Time (2011) | ||||
| 2012 | 1.1 [1.0, 1.3] | 1.2 [1.0, 1.3]* | 1.1 [1.0, 1.3]* | 1.1 [1.0, 1.2] |
| 2013 | .9 [.7, 1.1] | 1.0 [.9, 1.2] | 1.0 [.9, 1.2] | 1.1 [.9, 1.2] |
| 2014 | 1.0 [.8, 1.2] | 1.0 [.8, 1.1] | .9 [.8, 1.1] | .9 [.8, 1.0] |
| 2015 | .9 [.7, 1.1] | 1.1 [1.0, 1.2] | 1.2 [1.0, 1.3]* | 1.0 [.9, 1.2] |
| 2016 | .9 [.7, 1.1] | 1.1 [.9, 1.3] | 1.1 [.9, 1.3] | 1.1 [.9, 1.2] |
| Household size (1) | ||||
| 2 | 1.1 [.9, 1.3] | 1.0 [.9, 1.2] | 1.0 [.9, 1.1] | 1.1 [.9, 1.2] |
| 3 | 1.0 [.8, 1.3] | 1.1 [.9, 1.3] | 1.0 [.9, 1.2] | 1.0 [.8, 1.1] |
| 4 | .9 [.7, 1.2] | 1.0 [.8, 1.2] | 1.1 [.9, 1.3] | 1.1 [.9, 1.3] |
| 5 | 1.1 [.8, 1.6] | 1.1 [.8, 1.4] | 1.1 [.9, 1.5] | 1.1 [.8, 1.4] |
| 6 | .9 [.5, 1.4] | 1.0 [.7, 1.5] | 1.4 [.9, 2.1] | 1.4 [1.0, 2.0] |
| 7 | 1.2 [.6, 2.4] | 1.4 [.8, 2.4] | 1.7 [1.0, 2.9] | 1.0 [.6, 1.7] |
| 8 | 1.2 [.4, 3.5] | 1.5 [.7, 3.3] | 1.5 [.6, 3.7] | 1.5 [.6, 3.6] |
| 9 | .3 [.1, 1.3] | 1.4 [.6, 3.4] | 2.1 [.8, 5.4] | 2.0 [.8, 5.0] |
| 10 | 6.5 [1.3, 32.8]* | 4.2 [.7, 24.2] | 1.7 [.3, 8.1] | 1.0 [.2, 4.7] |
Note: OR: odds ratio; CI: confidence interval.
p ≤ .05
p < .01
p < .001.
n = 72,212.
n = 64,213
Food security level.
Food secure.
Living with partner.
Widowed/divorced/separated.
High school.
Unemployed and not looking for employment.
Unemployed and looking for employment.
Part-time and other.
Figure 2.
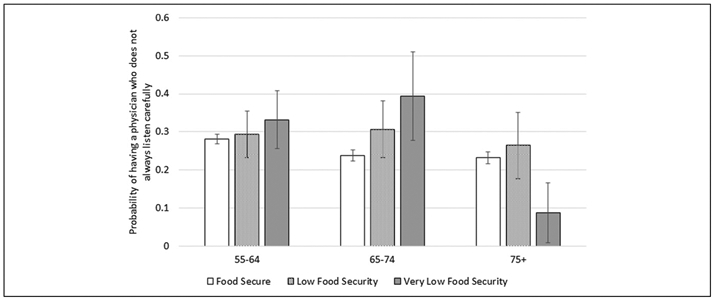
Predicted probability of having a physician who does not always listen carefully by age group and food insecurity level.
Discussion
It has been well established that food insecure adults are more likely to delay care than those who are FS (Bhargava & Lee, 2017). However, to the best of our knowledge, this is the first study to examine the relationship between food insecurity and healthcare access in a state-wide representative sample of midlife and older adults. The present study mirrors and extends upon previous research by being the first to find that among midlife and older adults, those who were food insecure reported decreased access to healthcare. Specifically, food insecurity was associated with delaying care and delaying filling a prescription. Food insecurity was also associated with a lack of a usual source of care, other than the emergency department. These findings remained even after controlling for other social and economic factors that have been linked to healthcare access. This suggests that providers can gain additional information regarding a patient’s risk status by knowing whether or not they are food insecure. Perhaps this is because food security status may capture other processes that impact access to care (Ma et al., 2008). For example, food insecure individuals struggle to meet all of their basic needs. If they prioritize addressing their need for food, they may do so at the expense of seeking care or obtaining medications (Ma et al., 2008). This may differentiate them from other populations that lack health-promoting resources, such as adequate income or health insurance, but are food secure.
In regard to healthcare utilization, previous research shows that food insecure adults are more likely to utilize acute sources of care and engage in a greater number of encounters with physicians. However, studies pertaining to older adults have produced mixed findings (Bhargava & Lee, 2016, 2017). The ambiguous results by Bhargava and Lee may have resulted from the use of two different populations: in one case, survey data from a nationally representative sample were used and found that those who were food insecure had a greater number of outpatient office visits, hospital stays, and emergency room encounters (Bhargava & Lee, 2016). The other study employed Medicare claims data from a low-income population and did not find differences in the number of emergency room, inpatient, or outpatient encounters (Bhargava & Lee, 2017). Findings from this present study, which employed a state-wide representative sample, showed that older adults experiencing food insecurity do not differ in likelihood of having a physician visit. However, here we assessed the presence or absence of a visit, whereas the previous study by Bhargava and Lee utilized the number of physician visits as the outcome (Bhargava & Lee, 2016), which may account for this discrepancy. Our findings do mirror those of Bhargava and Lee (2016), by similarly showing that older adults who were food insecure experienced increased utilization of sources of acute care as compared to those who were food secure. Specifically, those who were food insecure were more likely to visit an emergency department than those who were food secure. Similar to those results pertaining to access, these findings remained even after considering demographic characteristics, which suggests that those who are food insecure may experience unique factors prompting their utilization of acute care. For example, older adults experience a high prevalence of chronic conditions (Piccirillo et al., 2008), including those dependent on diet, such as hypertension and diabetes (Seligman & Schillinger, 2010). Exacerbation of these conditions due to the inability to afford both adequate food and medication may contribute to emergency department admissions (Kersey et al., 1999).
Whereas previous studies have focused solely on healthcare access and utilization among those who are food insecure, this is the first study to also assess the relationship between food security status and quality of care received. After considering social and economic factors, those who were food insecure were equally likely to have a physician who always listened carefully, but less likely to have a physician who always explained aspects of care carefully. There exist previous studies that have not found a difference in physician nonverbal communication, according to the socioeconomic characteristics of the patient (Verlinde et al., 2012), which may account for a lack of difference in perceptions of how carefully physicians listen to those of different food security levels. Evidence suggests that individuals with low socioeconomic status tend to receive less information pertaining to diagnosis or treatment and have less control over their conversations with their physicians (Verlinde et al., 2012), which may translate to perceptions of not receiving careful explanations, in the present study. Taken together, this suggests a need for doctors to adjust their explanations to better suit those who are vulnerable. This may include encouraging patients to express their concerns and queries (Verlinde et al., 2012).
Socioeconomic status encompasses a number of different characteristics, and thus, in the adult population, may allow for an accurate understanding of the association between these traits and the quality of care received. However, older adults may be relatively homogenous in regard to a number of their socioeconomic characteristics. Thus, understanding the socioeconomic impact on healthcare quality must extend beyond considerations of income or insurance status alone. For example, many older adults are retired or no longer working, and live with fixed incomes, which may overestimate or underestimate their total wealth. In 2018, it was reported that more than half of all individuals receiving supplemental security income (SSI) did not have any additional income (“SSI Annual Statistical Report, 2018,” 2019). Furthermore, as most individuals aged 65 years and older are entitled to Medicare (“An Overview of Medicare Characteristics of People on Medicare,” 2019), there may be little variation in regard to insurance status. Thus, food insecurity may be a more accurate representation of the socioeconomic status of individuals within this population than income, employment status, or insurance status alone.
While the main effects of age are not the focus of this study, the consideration of the impact of age on healthcare access, utilization, and quality, beyond other sociodemographic characteristics, is important to note. In regard to the association between age and healthcare access, those who were older were less likely to delay receiving care or filling a prescription. Despite the increased access to care, those who were older also experienced decreased utilization of care. Specifically, they were less likely to have seen a physician within the past 12 months. Those aged 65–74 years were also less likely than those who were younger to utilize the emergency department. Thus, this sample of older adults possessed both increased healthcare access and decreased use. This may be explained by the propensity that older adults have to utilize the emergency department only when appropriate as compared to those who are younger (Gruneir et al., 2011), which may also account for a lower likelihood of visiting a physician in general.
While the oldest age group in our sample also reported increased access to care and fewer physician encounters, they were more likely to use the emergency department than those aged 65–74 years. Individuals in this oldest age group are disproportionally represented in emergency department admissions (Gruneir et al., 2011). This may be due to factors not controlled for in our analyses, including a greater number of falls among this population (Gruneir et al., 2011). Thus, while those who are older may be more likely to seek care when appropriate than those who are younger, those in the oldest age group may be forced to utilize acute care services.
Last, in regard to quality of care, age groups differed only in that those aged 75+ years were less likely to have a physician who always explained aspects of care carefully than those aged 65–74 years. These findings may be explained by characteristics of older adults, such as poor health literacy and difficulty in processing new information (Chesser et al., 2016), which may translate to perceptions of poor physician communication and a need for physicians to adjust their communication accordingly.
In general, among middle and later life adults, the odds of having a physician who always listened carefully decreased with greater food insecurity. However, interestingly, among those who were aged 75+ years and older, VL-FS experienced greater odds of having a physician who always listened carefully than FS and L-FS. Older patients generally report a greater satisfaction with their care (Greene et al., 1994), which may be attributed to a higher number of interactions with the same physician (Spooner et al., 2016). Additionally, physicians who have a commitment to those who are vulnerable may practice in areas where socioeconomically-disadvantaged patients seek care (Piette et al., 2003). It may be that these physicians are more likely to spend additional time counseling patients they perceive to be in greater need (Piette et al., 2003). Thus, perhaps it is the dual vulnerability of these patients, being both older and socioeconomically-disadvantaged that alerts doctors to listen more attentively to these patients. Interestingly, this did not translate to these same individuals reporting an increased likelihood of having a physician who always explained aspects of care carefully. Thus, doctors may be practicing in ways that make these vulnerable older adults feel like they are being listened to more carefully; however, it does not appear that the benefit extends to communicating more clearly around aspects of care.
Several limitations should be noted. The first is that the CHIS does not assess the food insecurity level of individuals whose income levels are greater than or equal to 200% of the FPL. In California, 24% of individuals who are food insecure live above 200% of the FPL (Feeding America, 2018). In this study, it was assumed that these individuals were food secure, which may underestimate the prevalence of food insecurity in this sample (Bickel et al., 2000; Walsemann et al., 2017). Although it is possible that individuals in this income bracket may experience barriers around accessing food (e.g., due to lack of access due to transportation barriers or isolation), the cause for these barriers is likely due to other factors beyond income. Second, all variables were measured by self-report. Future studies would benefit from employing objective measures, such as the use of claims data or electronic health record data to measure access, utilization, and quality. Third, the analyses pertaining to healthcare quality do not consider the number of times a person sees the same doctor. It is likely that patients who have a longer length relationship with their physicians have higher quality communications than those who do not (Parchman & Burge, 2004). Fourth, these data are only representative of California’s noninstitutionalized population and may not be generalizable to populations from other states. One reason this may be the case is that up until June 2019, California was the only state preventing SSI recipients from applying for benefits from the Supplemental Nutrition Assistance Program (SNAP) (Hammond et al., 2020). Thus, the effects of food insecurity on older adults in California may be different than those among older adults from other states, who have had access to SNAP. The last limitation is that food insecurity is a cyclic phenomenon, with most food insecure households experiencing periods of security and insecurity throughout the year (Seligman & Schillinger, 2010). Healthcare access, utilization, and quality may change in tandem with this cycle. For this reason, a longitudinal study may be better equipped to assess these complex interrelationships. Nevertheless, this study provides an important snapshot in time of the association between food insecurity and healthcare access, utilization, and quality of care.
In conclusion, the findings from this study suggest that food insecurity is strongly associated with poorer access to and quality of care, as well as increased utilization of acute sources of care. These findings support both the neoclassical household production framework and the Andersen model of healthcare utilization. Specifically, those who were resource-constrained or food insecure experienced decreased access to and quality of care, which is consistent with the neoclassical household production framework. Additionally, while food insecurity level was not associated with the likelihood of having seen a physician, those who were food insecure were more likely to visit an emergency department, thus supporting the Andersen model. It is important that these associations remained even after controlling for traditional measures of socioeconomic status, including income, education level, employment status, and health insurance status. In summary, knowing patients’ food insecurity status can provide physicians with additional information about patients’ risk profiles beyond that known by assessing traditional socioeconomic characteristics alone, such as a person’s education or income level. Additionally, screening for food insecurity can allow for subsequent referral to social programs, such as SNAP, which has been shown to reduce food insecurity (Ratcliffe et al., 2011). However, physicians experience barriers to screening, including a lack of tools or resources to offer patients who are food insecure (Makelarski et al., 2017). For these reasons, systematic changes within healthcare settings are necessary to promote food insecurity screening by physicians.
Supplementary Material
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was partially supported by the grant UL1 TR0001414 from the National Center for Advancing Translational Sciences, through the University of California, Irvine Biostatistics, Epidemiology and Research Design and Community-Engagement Units.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplemental Material
Supplemental material for this article is available online.
References
- Alisha C-J, Rabbitt M, Gregory C, & Singh A (2017). Household food security in the United States in 2016. US Department of Agriculture and Economic Research Service. [Google Scholar]
- Andersen R, & Newman JF (1973). Societal and individual determinants of medical care utilization in the United States. Milbank Mem.Fd Quart, 51, 95. doi: 10.2307/3349613 [DOI] [PubMed] [Google Scholar]
- An Overview of Medicare Characteristics of People on Medicare. (2019). Kaiser family foundation. Retrieved from https://www.kff.org/medicare/issue-brief/an-overview-of-medicare/
- Becker GS (1965). A theory of the allocation of time. The Economic Journal, 75(299), 493–517. doi: 10.2307/2228949 [DOI] [Google Scholar]
- Berkowitz SA, Basu S, Meigs JB, & Seligman HK (2018). Food insecurity and health care expenditures in the United States, 2011–2013. Health Services Research, 53(3), 1600. doi: 10.1111/1475-6773.12730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berwick DM, Nolan TW, & Whittington J (2008). The triple aim: Care, health, and cost. Health Affairs. doi: 10.1377/hlthaff.27.3.759 [DOI] [PubMed] [Google Scholar]
- Bhargava V, & Lee JS (2016). Food insecurity and health care utilization among older adults in the United States. Journal of Nutrition in Gerontology and Geriatrics, 35(3), 177–192. doi: 10.1080/21551197.2016.1200334 [DOI] [PubMed] [Google Scholar]
- Bhargava V, & Lee JS (2017). Food insecurity and health care utilization among older adults. Journal of Applied Gerontology, 36(12), 1415–1432. doi: 10.1177/0733464815625835 [DOI] [PubMed] [Google Scholar]
- Bickel G, Nord M, Price C, Hamilton W, & Cook J (2000). Measuring food security in the United States Guide to measuring household food security revised 2000. United States Department of Agriculture. [Google Scholar]
- Blumberg SJ, Bialostosky K, Hamilton WL, & Briefel RR (1999). The effectiveness of a short form of the household food security scale. American Journal of Public Health, 89(8), 1231–1234. doi: 10.2105/AJPH.89.8.1231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- CAHPS Mental Health Care Surveys. (2019). Retrieved June 19, 2020, from https://www.ahrq.gov/cahps/surveys-guidance/echo/index.html
- Chesser A, Keene Woods N, Smothers K, & Rogers N (2016). Health literacy and older adults: A systematic review. Gerontology and Geriatric Medicine, 2(1), 1–13. doi: 10.1177/2333721416630492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- CHIS Methodology Documentation. (2012). Retrieved April 29, 2020, from https://healthpolicy.ucla.edu/chis/design/Pages/methodology.aspx
- Eisen S, Shaul J, Clarridge B, Nelson D, Spink J, & Cleary P (1999). Development of a consumer survey for behavioral health services. Psychiatric Services, 50(6), 793–798. [DOI] [PubMed] [Google Scholar]
- Feeding America. (2018). Food insecurity in California. Retrieved August 12, 2020, from https://map.feedingamerica.org/county/2018/overall/california
- Greene MG, Adelman RD, Friedmann E, & Charon R (1994). Older patient satisfaction with communication during an initial medical encounter. Social Science and Medicine, 38(9), 1279–1288. doi: 10.1016/0277-9536(94)90191-0 [DOI] [PubMed] [Google Scholar]
- Gruneir A, Silver MJ, & Rochon PA (2011). Review: Emergency department use by older adults: A literature review on trends, appropriateness, and consequences of unmet health care needs. Medical Care Research and Review, 68(2), 131–155. doi: 10.1177/1077558710379422 [DOI] [PubMed] [Google Scholar]
- Hammond R, Li J, McKinnon R, & Munoz J (2020). Calfresh expansion to SSI recipients: A case study on SNAP accessibility. University of California and Berkeley Goldman School of Public Policy. [Google Scholar]
- Institute for Healthcare Improvement. (2020). Triple aim for populations. Retrieved from http://www.ihi.org/Topics/TripleAim/Pages/Overview.aspx
- Kersey MA, Beran MS, McGovern PG, Biros MH, & Lurie N (1999). The prevalence and effects of hunger in an emergency department patient population. Academic Emergency Medicine, 6(11), 1109–1114. doi: 10.1111/j.1553-2712.1999.tb00112.x [DOI] [PubMed] [Google Scholar]
- Ma CT, Gee L, & Kushel MB (2008). Associations between housing instability and food insecurity with health care access in low-income children. Ambulatory Pediatrics, 8(1), 50–57. doi: 10.1016/j.ambp.2007.08.004 [DOI] [PubMed] [Google Scholar]
- Makelarski JA, Abramsohn E, Benjamin JH, Du S, & Lindau ST (2017). Diagnostic accuracy of two food insecurity screeners recommended for use in health care settings. American Journal of Public Health, 107(11), 1812–1817. doi: 10.2105/AJPH.2017.304033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parchman ML, & Burge SK (2004). The patient-physician relationship, primary care attributes, and preventive services. Family Medicine, 36(1), 22–27. [PubMed] [Google Scholar]
- Piccirillo JF, Vlahiotis A, Barrett LB, Flood KL, Spitznagel EL, & Steyerberg EW (2008). The changing prevalence of comorbidity across the age spectrum. Critical Reviews in Oncology/Hematology, 67(2), 124–132. doi: 10.1016/j.critrevonc.2008.01.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piette JD, Schillinger D, Potter MB, & Heisler M (2003). Dimensions of patient-provider communication and diabetes self-care in an ethnically diverse population. Journal of General Internal Medicine, 18(8), 624–633. doi: 10.1046/j.1525-1497.2003.31968.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ratcliffe C, McKernan SM, & Zhang S (2011). How much does the supplemental nutrition assistance program reduce food insecurity? American Journal of Agricultural Economics, 93(4), 1082–1098. doi: 10.1093/ajae/aar026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seligman HK, & Schillinger D (2010). Hunger and socioeconomic disparities in chronic disease. New England Journal of Medicine, 363(1), 6–9. doi: 10.1056/NEJMp1000072 [DOI] [PubMed] [Google Scholar]
- Shaul J, Eisen S, Clarridge B, Stringfellow V, Fowler F, & Cleary P (2001). Experience of Care and Health Outcomes (ECHO) survey field test report: Survey evaluation. Harvard Medical School and Department of Health Care Policy. [Google Scholar]
- Spooner KK, Salemi JL, Salihu HM, & Zoorob RJ (2016). Disparities in perceived patient-provider communication quality in the United States: Trends and correlates. Patient Education and Counseling, 99(5), 844–854. doi: 10.1016/j.pec.2015.12.007 [DOI] [PubMed] [Google Scholar]
- SSI Annual Statistical Report, 2018. (2019). Retrieved April 29, 2020, from https://www.ssa.gov/policy/docs/statcomps/ssi_asr/2018/ssi_asr18.pdf
- StataCorp. (2019). Stata statistical software: Release 16. College Station. [Google Scholar]
- Vargas Bustamante A, Fang H, Garza J, Carter-Pokras O, Wallace SP, Rizzo JA, & Ortega AN (2012). Variations in healthcare access and utilization among Mexican immigrants: The role of documentation status. Journal of Immigrant and Minority Health, 14(1), 146–155. doi: 10.1007/s10903-010-9406-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verlinde E, De Laender N, De Maesschalck S, Deveugele M, & Willems S (2012). The social gradient in doctor-patient communication. International Journal for Equity in Health, 11(1), 12. doi: 10.1186/1475-9276-11-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsemann KM, Ro A, & Gee GC (2017). Trends in food insecurity among California residents from 2001 to 2011: Inequities at the intersection of immigration status and ethnicity. Preventive Medicine, 105, 142–148. doi: 10.1016/j.ypmed.2017.09.007 [DOI] [PubMed] [Google Scholar]
- Ziliak J, & Gundersen C (2019a). Hunger among adults age 50-59 in 2017. Retrieved April 29, 2020, from https://www.feedingamerica.org/sites/default/files/2019-06/HungerAmongAdultsAge50-59in2017_F2.pdf [Google Scholar]
- Ziliak J, & Gundersen C (2019b). The state of senior hunger in America in 2017. Retrieved April 29, 2020, from https://www.feedingamerica.org/sites/default/files/2019-06/TheStateofSeniorHungerin2017_F2.pdf [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


