The number of persons living with dementia is expected to approximately double in Canada1 and around the world2 by 2030, making it a public health priority.2 In 2012, the World Health Organization recommended that governments develop plans to better tackle key issues related to dementia, such as awareness, timely diagnosis, health care service quality, and caregiver support, among others.2 As a result, many countries and other jurisdictions have put plans in place to address Alzheimer disease.3
There is ongoing debate as to which of primary care or specialty care should manage dementia. Some Alzheimer disease plans give the primary responsibility for managing patients with dementia to specialists, such as the plans for France, England, and Spain, countries in which family physicians do not diagnose or manage dementia.4-7 Other plans, such as those from Australia, Belgium, Finland, Denmark, and Canada (and from some of Canada’s provinces), recommend that in most cases the responsibility to manage the care of dementia patients, from diagnosis to treatment and follow-up, be given to primary care clinicians, with the support of specialized services.
While there is a growing interest in developing and implementing Alzheimer plans in primary care, we do not have a complete picture of their impact on the quality of care, partly because of the uncertainty surrounding the knowledge, attitudes, and practices (KAP) of primary health care professionals. More specifically, it remains unclear whether family physicians and nurses are prepared to manage patients with dementia.8,9 While the challenges of caring for patients with dementia in primary care are influenced by a variety of factors—setting, remuneration methods, and training being a few—there is a belief that many primary care clinicians are unprepared, not confident, and even reluctant to care for these patients in their practices,10,11 and that, depending on geographic differences in resources (eg, training, support, and remuneration), they prefer to refer patients to specialists immediately.
Evaluating the Quebec Alzheimer Plan’s implementation
In Canada, a national dementia strategy was launched in 2019 to meet the needs of persons living with dementia and their caregivers.12 This strategy is aligned with a series of Canadian recommendations that anchor dementia care in primary care.13-15 Before this report, several provinces had developed plans.16 Quebec, in 2009, was among the first to develop a comprehensive plan based in primary care.17 In 2014, the province’s Ministry of Health and Social Services launched a pilot phase in 42 interdisciplinary primary care clinics, known as family medicine groups. In 2016, this plan was implemented in all family medicine groups across the province, as described by Arsenault-Lapierre et al.18
Our research team, Research on Organization of Healthcare Services for Alzheimers, was mandated by the Ministry of Health and Social Services to evaluate the implementation of the Quebec Alzheimer Plan among the clinics that had piloted the plan and to assess its impact on quality of care for patients with dementia.19,20 This project offered an excellent opportunity to evaluate the KAP of primary care clinicians concerning dementia care and the Quebec Alzheimer Plan. As such, we developed and validated 2 questionnaires, one to assess the KAP of family physicians and the other to assess the KAP of nurses and other health professionals.21,22 Briefly, the responses to each questionnaire were scored on a Likert scale (where a higher number reflects more agreement) and grouped into 5 factors for family physicians and 4 factors for nurses and other health professionals. Each factor score is presented as the mean of the responses of the related questions and presented as a score out of 100. The results from these questionnaires, collected from the clinicians of 38 family medicine groups (2 of the 42 practices opted out of the Quebec Alzheimer Plan and 2 others refused to participate in research), allow us to challenge the preconceived notion that primary care clinicians are unprepared, not confident, and reluctant to care for persons in their practices living with dementia.
Clinicians’ responses regarding dementia care
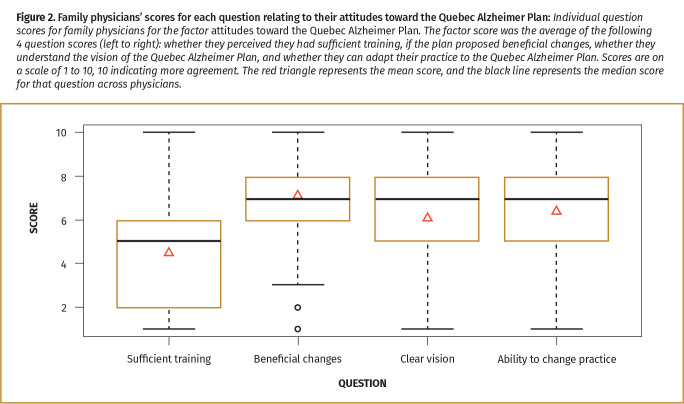
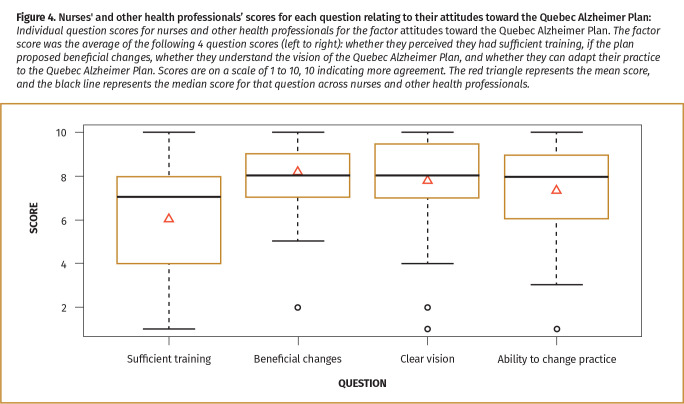
The questionnaires were sent to all clinicians in each practice, without knowing their eligibility (ie, working at least 1 day a week in that practice and seeing older patients). We estimated a response rate based on the questionnaires that were returned and known to be ineligible.21 A total of 369 eligible family physicians returned a completed questionnaire (68% estimated response rate). Family physicians reported positive attitudes toward dementia care (eg, “I think that, in the presence of symptoms, early diagnosis of dementia is important”), perceived competency and knowledge in dementia care (eg, “I believe that I have the skills to diagnose dementia”), positive attitudes toward collaboration with nurses and other health professionals in managing dementia care (eg, “I think that my collaboration with a nurse or other health professional in my team is essential to develop care plans for patients with dementia”), and good practices with regard to cognitive evaluation (eg, “I look for the presence of cognitive impairment in my patients when they complain about memory problems”) (Figure 1). However, family physicians reported a lower score in attitudes toward the Quebec Alzheimer Plan (eg, “I think that the changes proposed by the Alzheimer plan will benefit me: they will help me do my work better”) compared with scores for the other factors. When this score was looked at more closely, we observed a lower average score for the question related to sufficient training during the implementation of the plan (Figure 2).
Figure 1.
Questionnaire on knowledge, attitudes, and practices regarding dementia care and the Quebec Alzheimer Plan—scores for family physicians: The 5 factors starting from the top of the graph and going clockwise are practice with regard to cognitive evaluation; perceived competency and knowledge in dementia care; attitudes toward collaboration with nurses and other health professionals in managing dementia care; attitudes toward dementia care; and attitudes toward the Quebec Alzheimer Plan. Scores are presented as the average of family physicians’ responses to questions included in that factor, on a scale of 1 to 100.
Figure 2.
Family physicians’ scores for each question relating to their attitudes toward the Quebec Alzheimer Plan: Individual question scores for family physicians for the factor attitudes toward the Quebec Alzheimer Plan. The factor score was the average of the following 4 question scores (left to right): whether they perceived they had sufficient training, if the plan proposed beneficial changes, whether they understand the vision of the Quebec Alzheimer Plan, and whether they can adapt their practice to the Quebec Alzheimer Plan. Scores are on a scale of 1 to 10, 10 indicating more agreement. The red riangle represents the mean score, and the black line represents the median score for that question across physicians.
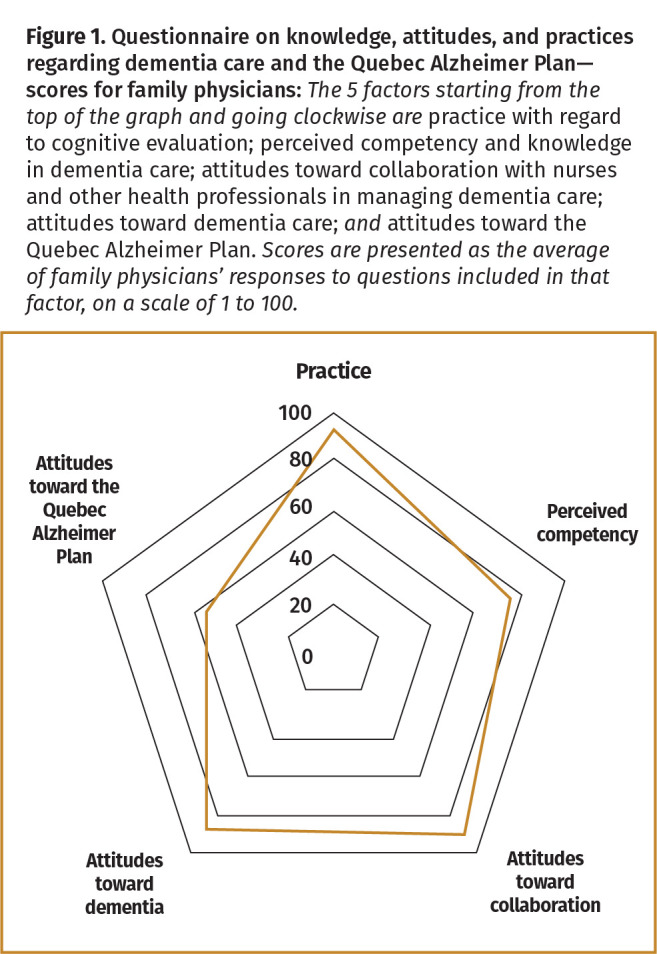
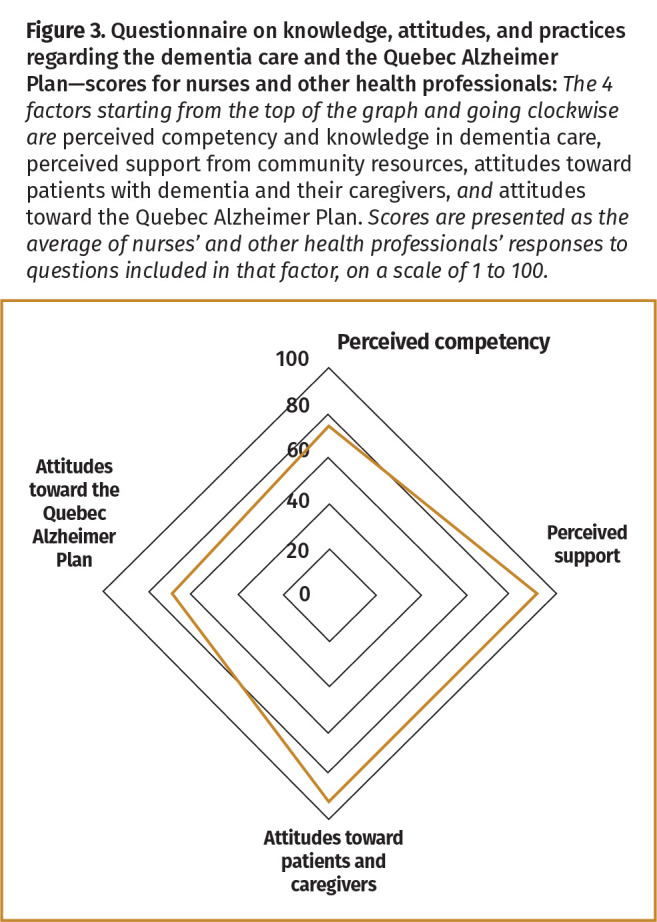
There were 144 completed questionnaires returned from nurses and other health professionals (of the 144, 83% of respondents were nurses, 9% were social workers, and 8% were other health professionals such as pharmacists, respiratory therapists, physiotherapists, social assistance technicians, and occupational therapists). The estimated response rate for nurses and other health professionals was 69.5%. They demonstrated positive attitudes toward patients with dementia and their caregivers (eg, “I think that several things can be done to improve the quality of life of a patient living with dementia”) and reported high levels of perceived support from community resources, such as the Alzheimer disease societies (Figure 3). However, compared with their scores on other factors, they reported lower levels of perceived competency and knowledge in dementia care (eg, “I believe that I have the skills to identify cognitive impairment”). Finally, they also scored lower on attitudes toward the Quebec Alzheimer Plan (eg, “I understand the vision and values of the Quebec Alzheimer Plan”) compared with the other factors. Similar to family physicians’ scores, nurses and other health professionals scored lower for the question on whether they received sufficient training during the implementation of the plan (Figure 4).
Figure 3.
Questionnaire on knowledge, attitudes, and practices regarding dementia care and the Quebec Alzheimer Plan—scores for nurses and other health professionals: The 4 factors starting from the top of the graph and going clockwise are perceived competency and knowledge in dementia care, perceived support from community resources, attitudes toward patients with dementia and their caregivers, and attitudes toward the Quebec Alzheimer Plan. Scores are presented as the average of nurses’ and other health professionals’ responses to questions included in that factor, on a scale of 1 to 100.
Figure 4.
Nurses’ and other health professionals’ scores for each question relating to their attitudes toward the Quebec Alzheimer Plan: Individual question scores for the nurses and other health professionals for the factor attitudes toward the Quebec Alzheimer Plan. The factor score was the average of the following 4 question scores (left to right): whether they perceived they had sufficient training, if the plan proposed beneficial changes, whether they understand the vision of the Quebec Alzheimer Plan, and whether they can adapt their practice to the Quebec Alzheimer Plan. Scores are on a scale of 1 to 10, 10 indicating more agreement. The red triangle represents the mean score, and the black line represents the median score for that question across nurses and other health professionals.
Discussion
The responses from primary care clinicians to our questionnaires showed that family physicians, nurses, and other health professionals who had participated in the implementation of the Quebec Alzheimer Plan had high or positive KAP toward dementia care and the Quebec Alzheimer Plan. These scores suggest that primary care clinicians are interested in and have positive attitudes toward diagnosing and managing dementia care in their practices. This not only aligns with Canadian recommendations13,14 but also with the evidence that patients generally value continuity of care23 and might prefer being diagnosed and treated by their family physicians.24-26
The Quebec Alzheimer Plan employed a multifaceted strategy to address primary dementia care,27 including clinical, change management, and financial resources; making use of multidisciplinary teams; and training and coaching in dementia care. This comprehensive approach was successful in improving dementia care.28 Our results suggest that the success of the plan might have been driven by the positive attitudes of clinicians toward dementia care. However, positive attitudes are not sufficient, as clinicians indicated they believed they needed more training and coaching to change their practices in the long run.
The responses that we received from clinicians suggest that decision makers need to invest more in training when they are implementing a dementia strategy. This is not a new idea; several studies have supported that training is important for quality-of-care improvement.29-31 When developing and implementing Alzheimer plans, health organizations and decision makers need to step up and provide more dementia-specific training for clinicians, to ensure that they are not only willing to undertake the care of persons with dementia in their practices, but are also fully prepared. Primary care clinicians must perceive that they have been given sufficient training to undertake most of the care for their patients with dementia. To determine how much and what kind of training is needed, decision makers and health authorities should work in close collaboration with primary care clinicians to develop the curriculum and to ensure that clinicians will participate in training.32
The results of our study assessing the KAP of clinicians participating in the Quebec Alzheimer Plan suggest that their attitudes toward providing dementia care are positive and willing but that they would benefit from more support and training, as has been expressed in previous studies.33 These results are important because several national and provincial plans are focusing on primary care tackling dementia care. Indeed, Canadian recommendations have put forward primary care as the foundation on which to further improve dementia care.34
Acknowledgment
This work was supported by the Fonds de recherche du Quebec—Santé and the Canadian Consortium on Neurodegeneration in Aging. The Canadian Consortium on Neurodegeneration in Aging is supported by a grant from the Canadian Institutes of Health Research with funding from several partners.
Footnotes
Competing interests
None declared
The opinions expressed in commentaries are those of the authors. Publication does not imply endorsement by the College of Family Physicians of Canada.
This article has been peer reviewed.
La traduction en français de cet article se trouve à www.cfp.ca dans la table des matières du numéro d’octobre 2021 à la page e275.
References
- 1.Manuel DG, Garner R, Finès P, Bancej C, Flanagan W, Tu K, et al. Alzheimer’s and other dementias in Canada, 2011 to 2031: a microsimulation population health modeling (POHEM) study of projected prevalence, health burden, health services, and caregiving use. Popul Health Metr 2016;14:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dementia: a public health priority. Geneva, Switz: World Health Organization; 2012. Available from: https://extranet.who.int/agefriendlyworld/wp-content/uploads/2014/06/WHO-Dementia-English.pdf. Accessed 2021 May 24. [Google Scholar]
- 3.From plan to impact: progress towards targets of the Global Action Plan on Dementia. London, UK: Alzheimer’s Disease International; 2018. Available from: https://www.alz.co.uk/adi/pdf/from-plan-to-impact-2018.pdf. Accessed 2021 May 24. [Google Scholar]
- 4.Living well with dementia: a national dementia strategy. London, UK: Department of Health; 2009. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/168220/dh_094051.pdf. Accessed 2019 Nov 28. [Google Scholar]
- 5.Banerjee S. Living well with dementia—development of the national dementia strategy for England. Int J Geriatr Psychiatry 2010;25(9):917-22. [DOI] [PubMed] [Google Scholar]
- 6.Ministerio de Sanidad, Servicios Sociales e Igualdad . Estrategia en Enfermedades Neurodegenerativas del Sistema Nacional de Salud. 2016. Madrid, Spain: Government of Spain; 2016. Available from: https://www.mscbs.gob.es/organizacion/sns/planCalidadSNS/pdf/Est_Neurodegenerativas_APROBADA_C_INTERTERRITORIAL.pdf. Accessed 2021 May 24. [Google Scholar]
- 7.Plan « Alzheimer et maladies apparentées » 2008-2012. Paris, France: Government of France; 2008. Available from: https://www.cnsa.fr/documentation/plan_alzheimer_2008-2012-2.pdf. Accessed 2019 Dec 3. [Google Scholar]
- 8.Harris DP, Chodosh J, Vassar SD, Vickrey BG, Shapiro MF.. Primary care providers’ views of challenges and rewards of dementia care relative to other conditions. J Am Geriatr Soc 2009;57(12):2209-16. Epub 2009 Nov 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Millard F, Baune B.. Dementia—who cares?: a comparison of community needs and primary care services. Aust Fam Physician 2009;38(8):642-9. [PubMed] [Google Scholar]
- 10.Fox C, Maidment I, Moniz-Cook E, White J, Thyrian JR, Young J, et al. Optimising primary care for people with dementia. Ment Health Fam Med 2013;10(3):143-51. [PMC free article] [PubMed] [Google Scholar]
- 11.Parmar J, Dobbs B, McKay R, Kirwan C, Cooper T, Marin A, et al. Diagnosis and management of dementia in primary care. Exploratory study. Can Fam Physician 2014;60:457-65. [PMC free article] [PubMed] [Google Scholar]
- 12.A dementia strategy for Canada: together we aspire. Ottawa, ON: Public Health Agency of Canada; 2019. Available from: https://www.canada.ca/content/dam/phac-aspc/images/services/publications/diseases-conditions/dementia-strategy/National%20Dementia%20Strategy_ENG.pdf. Accessed 2019 Dec 4. [Google Scholar]
- 13.Moore A, Frank C, Chambers LW.. Role of the family physician in dementia care. Can Fam Physician 2018;64:717-9 (Eng), e418-21 (Fr). [PMC free article] [PubMed] [Google Scholar]
- 14.Gauthier S, Patterson C, Chertkow H, Gordon M, Herrmann N, Rockwood K, et al. Recommendations of the 4th Canadian Consensus Conference on the Diagnosis and Treatment of Dementia (CCCDTD4). Can Geriatr J 2012;15(4):120-6. Epub 2012 Dec 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Third Canadian Consensus Conference on Diagnosis and Treatment of Dementia. March 9-11, 2006. Montreal, Quebec. 146 Approved recommendations. Final—July 2007. Toronto, ON: Mount Sinai Hospital. Available from: https://sinaigeriatrics.ca/wp-content/uploads/2017/05/2007-CCCDFinal.pdf. Accessed 2021 Aug 31. [Google Scholar]
- 16.Teper MH, Godard-Sebillotte C, Vedel I.. Achieving the goals of dementia plans: a review of evidence-informed implementation strategies. World Health Popul 2019;18(1):37-46. [DOI] [PubMed] [Google Scholar]
- 17.Bergman H, Arcand M, Bureau C, Chertkow H, Ducharme F, Joanette Y, et al. Report of the Committee of Experts for the Development of an Action Plan on Alzheimer’s Disease and Related Disorders. Meeting the challenge of Alzheimer’s disease and related disorders: a vision focused on the individual, humanism, and excellence. Quebec, QC: Ministère de la Santé et des Services sociaux; 2009. [Google Scholar]
- 18.Arsenault-Lapierre G, Godard-Sebillotte C, Sourial N, Couturier Y, Bouchard P, Rozo LR, et al. Le Plan Alzheimer québécois, un plan basé sur les soins primaires. Santé Publique 2020;32(4):375-80. [DOI] [PubMed] [Google Scholar]
- 19.Guillette M, Couturier Y, Moreau O, Gagnon G, Bergman H, Vedel I.. Gouvernance et accompagnement du changement: le cas de la phase expérimentale du Plan Alzheimer du Québec. Innovations 2019;60(3):145-68. [Google Scholar]
- 20.Guillette M. De la politique aux changements de pratiques: la traduction du Plan Alzheimer du Québec dans ses formes locales. Sherbrooke, QC: University of Sherbrooke; 2016. Available from: https://savoirs.usherbrooke.ca/handle/11143/9734. Accessed 2021 May 26. [Google Scholar]
- 21.Arsenault-Lapierre G, Sourial N, Pakzad S, Hardouin M, Couturier Y, Bergman H, et al. Validation of a questionnaire for family physicians: knowledge, attitude, practice on dementia care. Can J Aging 2021;40(2):238-47. Epub 2020 May 5. [DOI] [PubMed] [Google Scholar]
- 22.Arsenault-Lapierre G, Sourial N, Vedel I.. Measuring knowledge, practice, and attitudes toward dementia in nurses and other allied health professionals: questionnaire development and validation. McGill Fam Med Stud Online 2020;15:e02. [Google Scholar]
- 23.Low LF, White F, Jeon YH, Gresham M, Brodaty H.. Desired characteristics and outcomes of community care services for persons with dementia: what is important according to clients, service providers and policy? Australas J Ageing 2013;32(2):91-6. Epub 2012 Aug 23. [DOI] [PubMed] [Google Scholar]
- 24.Frank C, Forbes RF.. A patient’s experience in dementia care. Using the “lived experience” to improve care. Can Fam Physician 2017;63:22-6 (Eng), e3-8 (Fr). [PMC free article] [PubMed] [Google Scholar]
- 25.Forbes D, Finkelstein S, Blake CM, Gibson M, Morgan DG, Markle-Reid M, et al. Knowledge exchange throughout the dementia care journey by Canadian rural community-based health care practitioners, persons with dementia, and their care partners: an interpretive descriptive study. Rural Remote Health 2012;12(4):2201. Epub 2012 Nov 26. [PubMed] [Google Scholar]
- 26.Di Gregorio D, Ferguson S, Wiersma E.. From beginning to end: perspectives of the dementia journey in northern Ontario. Can J Aging 2015;34(1):100-12. [DOI] [PubMed] [Google Scholar]
- 27.Ministère de la Santé et des Services sociaux . Relever le défi de la maladie d’Alzheimer et des maladies apparentées. Une vision centrée sur la personne, l’humanisme et l’excellence. Rapport du comité d’experts en vue de l’élaboration d’un plan d’action pour la maladie d’Alzheimer. Quebec, QC: Gouvernement du Québec; 2009. Available from: http://publications.msss.gouv.qc.ca/msss/document-000869/. Accessed 2021 May 24. [Google Scholar]
- 28.Vedel I, Sourial N, Arsenault-Lapierre G, Godard-Sebillotte C, Bergman H.. Impact of the Quebec Alzheimer Plan on the detection and management of Alzheimer disease and other neurocognitive disorders in primary health care: a retrospective study. CMAJ Open 2019;7(2):E391-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Koch T, Iliffe S.. Dementia diagnosis and management: a narrative review of changing practice. Br J Gen Pract 2011;61(589):e513-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Perry M, Drašković I, Lucassen P, Vernooij-Dassen M, van Achterberg T, Rikkert MO.. Effects of educational interventions on primary dementia care: a systematic review. Int J Geriatr Psychiatry 2011;26(1):1-11. [DOI] [PubMed] [Google Scholar]
- 31.Lee L, Weston WW, Hillier LM.. Developing memory clinics in primary care: an evidence-based interprofessional program of continuing professional development. J Contin Educ Health Prof 2013;33(1):24-32. [DOI] [PubMed] [Google Scholar]
- 32.Pimlott NJG, Persaud M, Drummond N, Cohen CA, Silvius JL, Seigel K, et al. Family physicians and dementia in Canada: part 2. Understanding the challenges of dementia care. Can Fam Physician 2009;55:508-9.e1-7. Available from: https://www.cfp.ca/content/cfp/55/5/508.full.pdf. Accessed 2021 May 26. [PMC free article] [PubMed] [Google Scholar]
- 33.Yaffe MJ, Orzeck P, Barylak L.. Family physicians’ perspectives on care of dementia patients and family caregivers. Can Fam Physician 2008;54:1008-15. [PMC free article] [PubMed] [Google Scholar]
- 34.Moore A, Patterson C, Lee L, Vedel I, Bergman H.. Fourth Canadian Consensus Conference on the Diagnosis and Treatment of Dementia. Recommendations for family physicians. Can Fam Physician 2014;60:433-8 (Eng), e244-50 (Fr). [PMC free article] [PubMed] [Google Scholar]