Abstract
Background
The inclusion of pharmacists into general practices in Australia has expanded in recent years. This systematic review aimed to synthesise the literature of qualitative and quantitative studies, and identify the knowledge gaps, related to pharmacists working in general practice in Australia.
Methods
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. PubMed, EBSCOhost, EMBASE, and the Cochrane Library were searched from the inception of databases to January 2021. The search was focused on studies investigating general practice pharmacists in Australia. The quality of each study was appraised using the Mixed Method Appraisal Tool criteria. The narrative synthesis approach was utilised to describe data due to the heterogeneity among study designs and measures.
Results
Twenty-five studies were included in this review. General practice pharmacists engaged in various non-dispensing patient care services, with medication management reviews being the primary activity reported. General practice pharmacists’ characteristics and an environment with a willingness of collaboration were the notable influencing factors for successfully including pharmacists in general practices. Factors that posed a challenge to the adoption of general practice pharmacists were lack of funding and other resources, poorly defined roles, and absence of mentoring/training.
Conclusion
This review has summarised the characteristics, activities, benefits, barriers, and facilitators of including pharmacists in general practices in Australia. General practice pharmacists are well accepted by stakeholders, and they can engage in a range of patient-centred activities to benefit patients. There is a need for more robust research to explore the patient and economic outcomes related to clinical activities that a pharmacist can perform in general practice, as a foundation to developing an appropriate and sustainable funding model. The findings of this review will be beneficial for pharmacists, researchers, policymakers, and readers who wish to implement the role of general practice pharmacists in the future.
Introduction
With the expansion of pharmacists’ roles, pharmacists have been included in primary healthcare teams to provide collaborative patient care in many countries. The co-location of pharmacists within primary healthcare teams has been studied in the United States of America (USA), United Kingdom (UK), Canada, Australia, The Netherlands, Ireland, Brazil, New Zealand, and Malaysia [1–8]. Studies from the USA, UK, and Canada have reported that the inclusion of pharmacists into primary healthcare teams has improved patients’ health outcomes and benefited patients in other ways [9–11].
The primary purpose of co-locating pharmacists in primary care teams is to improve medicines optimisation and patient safety [2,12,13]. However, the characteristics of models for including pharmacists into primary care vary according to the challenges and policies of healthcare systems in individual countries. For example, in the USA, the Patient-Centred Medical Home (PCMH) model was introduced to improve the quality of patient-centred services in primary healthcare and to lower healthcare costs [14]. The PCMH model relies on critical structural components, such as the shared use of health information, advanced performance indicators, trust and good rapport among providers and patients, and adequate financial reimbursement [15]. The PCMH model has offered numerous opportunities for pharmacists to contribute through diverse clinical activities to improve patient outcomes [10,16,17].
Canadians have investigated the inclusion of pharmacists into family practices since 2003. The “Integrating Family Medicine and Pharmacy to Advance Primary Care Therapeutics (IMPACT)” project was one of the largest trials launched in Ontario, Canada to investigate the inclusion of pharmacists in family health teams [18]. The main aim was to improve collaborative practice between pharmacists, family physicians, and allied health professionals in managing medication therapy [18–21]. In Canada, the public health system has provided funding for pharmacists in family health teams and pharmacists have rights to prescribe in some states/provinces [22,23]. Canadian studies have reported positively on patient-centred activities as a result of including pharmacists as a part of the primary care team [9,12,21]. Furthermore, there is evidence for continued expansion of pharmacists in family health teams across the country [20].
National Health Service England launched the Clinical Pharmacists in General Practice model in 2015 to help overcome the expanding workforce crisis of general practitioners (GPs) [11]. The over-arching purpose of including pharmacists into general practices across the UK is to improve patient care [13,24,25]. This includes providing extra help to manage chronic health conditions, education to those on multiple medicines, and better access to health assessments [25]. UK studies have shown that general practice pharmacists’ consultations can benefit patients [11,24–27]. There are currently over 1000 full-time equivalent clinical pharmacists working across general practices in the UK [28]. Like in Canada, pharmacists in general practices in the UK are funded by the government, and they have rights to prescribe [29]. The “Pharmacotherapy Optimisation through Integration of a Non-dispensing pharmacist in a primary care Team (POINT)” study in The Netherlands [5] and the “General Practice Pharmacist (GPP)” study in Ireland [4] were another two projects launched to explore the general practice pharmacist model.
In Australia, general practices are the frontline healthcare service that act as a gateway to specialist services [30]. The inclusion of pharmacists in Australian general practices has been evolving gradually over the last decade to provide non-dispensing services such as medication management services, medication safety initiatives, and patient education. The role of general practice pharmacists has been supported by the Australian Medical Association (AMA), Pharmaceutical Society of Australia (PSA), and various Primary Health Networks in Australia since 2015 [31]. However, Australia lags well behind other countries, such as the UK and Canada, in widening the role of general practice pharmacists across the country [32]. The reasons may be due to unique challenges and policies in the Australian healthcare system, including the lack of an appropriate funding model, limitation of prescribing rights in the scope of practice of pharmacists, and the absence of focusing on overall patient health outcomes when considering the remuneration [33]. Australia has a growing burden of chronic diseases, an increased ageing population, health workforce pressures, unacceptable inequities in health outcomes and access to services, and escalating healthcare expenditure [34,35]. It is still unknown whether there is any impact on these healthcare system challenges with the inclusion of pharmacists in Australian general practice.
There have been systematic reviews conducted globally to explore the effectiveness of the activities of pharmacists in general practices [36]; to investigate how the degree of inclusion of a non-dispensing pharmacist impacts medication-related health outcomes in primary care [37]; and to assess the competencies of general practice pharmacists [38]. However, to date, there has not been a review to assess the overall impact of the inclusion of pharmacists in Australian general practices. Even though there have been studies conducted in Australia related to general practice pharmacists [32,39–62], the literature has not been summarised to describe the role of general practice pharmacists and to identify knowledge deficits related to pharmacists working in general practice in Australia.
The aim of this systematic review was to synthesise the literature related to general practice pharmacists in Australia, and attempt to answer the following research questions:
What are the clinical and non-clinical activities being conducted by pharmacists in general practices in Australia?
What are the benefits/outcomes from the inclusion of pharmacists in the Australian general practice setting?
What are the perspectives of stakeholders, and the barriers and facilitators of the inclusion of pharmacists in the general practice setting in Australia?
What are the characteristics, qualifications, and experience of the pharmacists in general practices in Australia?
What are the knowledge deficits relating to pharmacists working in general practice in Australia?
Methods
Research design
A systematic review for mixed methodologies was followed, informed by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) systematic review guidelines and checklist (S1 Checklist) [63,64]. A mixed-methods systematic review methodology was employed due to the relative paucity of research on the general practice pharmacist model in Australia. This approach provided the flexibility required to incorporate various study methodologies and offered a systematic design to conduct the literature review to meet the aims of the research. The review was registered with the international database of prospectively registered systematic reviews (PROSPERO: CRD42019109963).
Literature search strategy
A systematic literature search of PubMed, EBSCOhost, EMBASE, and the Cochrane Library was conducted from the inception of each database to January 2021. The search was focused on studies investigating general practice pharmacists in Australia. Full text peer-reviewed English language articles that involved qualitative, quantitative or mixed-method studies with any outcomes reported were included in the review. Search strategies for databases are provided in S1 Table. A manual search of the bibliography in the reference lists of identified articles was conducted and other related review articles were screened for additional relevant studies.
Eligibility criteria
Articles were included in the review if the following conditions were met: (a) tested an intervention of pharmacists in general practice and/or obtained views of stakeholders (pharmacists, GPs, practice staff and patients) related to pharmacist services/activities in general practice; and (b) a pharmacist was co-located within a general practice clinic to provide non-dispensing medication-related activities.
Articles were excluded if any of the following conditions were met: (a) conducted in secondary, tertiary or other care settings (hospitals, nursing homes); (b) conducted outside of Australia; or (c) presented as editorials, protocols, letters, commentaries, and reviews.
Data evaluation
Abstract and full-text screening was performed by two authors (TS, JT), who independently applied the eligibility criteria to 10% of the search results and checked inter-rater reliability. After finding 100% agreement, a single investigator (TS) rated the remaining 90% articles alone [65,66]. Full texts were reviewed where a decision could not be made on abstract and title alone. Title and abstract screening was conducted by using the software package Covidence for conducting systematic reviews [67]. Full-text screening involved using EndNote to manage and retrieve full-texts.
Quality appraisal
The Mixed Methods Appraisal Tool (MMAT) was used to appraise the quality of empirical studies, as it covers a variety of methodologies [68]. The MMAT includes five core quality criteria for each of the following five categories of study designs: qualitative research, randomised controlled trials, non-randomised studies, quantitative descriptive studies, and mixed-method studies [68]. Critical appraisal of methodological quality and risk of bias assessment of included papers were undertaken independently by two reviewers (TS, SK). A third reviewer (MN) was consulted in the case of disagreement without reaching consensus.
Data analysis
A narrative synthesis approach was used to synthesise the findings of the included articles, due to the heterogeneity of studies in the review with a range of methodologies [69,70]. First, a preliminary synthesis was conducted to search studies, and present results in a tabular form. Then the results were discussed by two reviewers (TS, SK) and structured into themes. The studies included in the narrative synthesis were then summarised within a framework to capture the features of each study with reference to the focus of this review: clinical and non-clinical activities of general practice pharmacists; benefits of general practice pharmacists; perspectives of stakeholders about general practice pharmacists; barriers and facilitators for the implementation of general practice pharmacists; and characteristics and training requirements of general practice pharmacists. Original investigators of the studies were contacted to obtain additional research information related to the framework [71].
Results
Literature retrieval
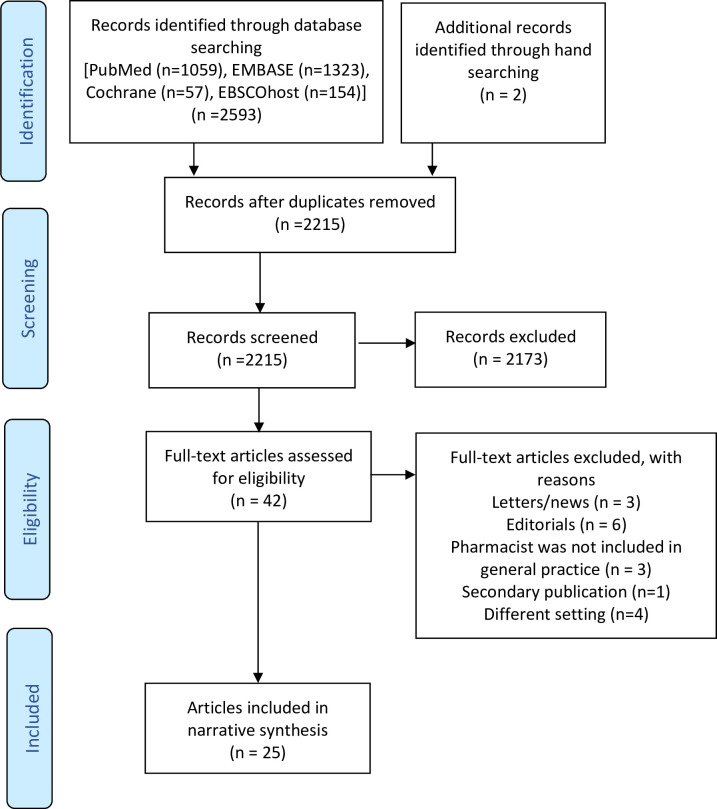
A search of the databases identified 2215 records once duplicates were removed. Twenty-five articles met the full inclusion criteria and were included in this review [32,39–62]. Fig 1 shows the flow diagram of the study selection.
Fig 1. Flowchart depicting inclusion/exclusion.
Article characteristics
Characteristics of the 25 articles included in this review are provided in S2 Table. The included articles aimed to: (i) characterise the clinical and non-clinical activities that a pharmacist can perform in general practice [32,39,42,44,46,51–53,55,56,62], (ii) explore the pharmacist recommendations and general practitioner acceptance rates regarding medication-related decision-making in general practice [43,49–51], and (iii) explain the stakeholders’ perspectives, barriers and facilitators of the inclusion of a pharmacist into general practice [40,41,45,47,48,51,54,57–59,61]. The included articles utilised designs that were qualitative (40%, n = 10) [40,42,45,47,48,55,58,59,61,62], quantitative non-randomised control (32%, n = 8) [39,43,46,49,50,52,56,60], quantitative descriptive (8%, n = 2) [32,41], and mixed-method (20%, n = 5) [44,51,53,54,57].
Risk of bias and quality assessment
All the included articles met the following screening criteria of MMAT: having clear research questions and addressing the research questions based on the collected data [65]. Almost all articles (92%, n = 23) were rated average or above average quality (S3 Table). Only 5 articles that utilised a qualitative design fulfilled all the criteria in the MMAT [44,46,47,58,60]. The articles which utilised a quantitative non-RCT design (32%, n = 8) or a mixed-method design (20%, n = 5) fulfilled 2–4 criteria [39,43,44,46,49–54,56,57,60], and quantitative descriptive design (8%, n = 2) fulfilled 3–4 criteria in the MMAT [31,40]. Overall, five articles (20%) fulfilled all criteria [44,46,47,59,61], eight articles (32%) fulfilled 4 criteria [32,40,42,46,49,50,54,62], ten articles (40%) fulfilled 3 criteria [39,41,52,52,54–58,60], and two articles (8%) fulfilled 2 criteria [42,43] for their particular research design using the MMAT. Details of the quality appraisal of the included articles are provided in S3 Table.
All the articles which utilised a qualitative design (n = 10, 40%) fulfilled 3 criteria or more in the MMAT. Among the ten qualitative studies, five studies used semi-structured interviews [45,46,58,59,61], two studies used a combination of semi‐structured and focus group interviews [40,47], two were case studies [55,62], and one study used an ethnographic approach [42]. Thematic analysis (6 out of 10, 60%) was the most widely used qualitative analysis method [45,47,48,58,59,61]. In the majority of non-randomised quantitative components and mixed-method studies, confounders and inconsistencies were not accounted for in the design and analysis. Small sample size/low response rate, lack of a control group, non-probability nature of sampling and researcher bias were the most notable limitations in the included articles [32,39–44,46,49–58,60,62].
Synthesis of results
Clinical/Non-clinical activities conducted by the pharmacists in general practices and outcomes
The general practice pharmacist role comprised a variety of activities including medication reviews and reconciliation; clinical audits; adherence counselling; patient education on medical conditions and medications; reviewing and ordering of laboratory tests; healthy lifestyle advice; chronic disease management; medication information provision; and administrative work [32,40,42,44,46,48–53,55–57]. Medication management reviews performed by general practice pharmacists has been the leading clinical activity investigated in most articles, reflecting its role as the primary source of funding for Australian general practice pharmacists at present [32,39,43,46,49–51,62].
The inclusion of pharmacists into general practices can facilitate the delivery of multiple patient-centred activities to manage chronic diseases; however, there were only five studies demonstrating clinical outcomes for patients [44,53,55,56,62]. Two articles reported general practice pharmacists’ activities related to osteoporosis and asthma management in general practice [44,53]. Pharmacist-led consultations made significant improvements to the prescription of anti-osteoporosis medicines, vitamin D and calcium supplements in general practice [44]. A pilot study demonstrated the feasibility, acceptability, and benefits of a general practice pharmacist in asthma management [53]. This study showed that general practice pharmacists engaged in the following activities to manage asthma: performing asthma control assessment, making recommendations to adjust medication or device, providing education on correct device use and avoidance of trigger factors, and developing an asthma action plan [53]. Case studies and qualitative data from the study indicated potential hospital admission avoidance and stakeholder acceptability of asthma management by a general practice pharmacist [53]. Two articles reported the perspectives of community pharmacists and GPs on collaborative asthma management with general practice pharmacists [58,59]. The articles indicated that community pharmacists and GPs supported collaborative asthma management with general practice pharmacists [58,59]. Furthermore, these two articles illustrated the challenges in asthma management, barriers and facilitators for collaborative asthma management, and possible collaborative asthma care models with general practice pharmacists [58,59].
Three separate studies reported smoking cessation sessions, deprescribing in older persons, and reviewing medications in Human Immunodeficiency Virus (HIV)-infected patients utilising general practice pharmacists [55,56,62]. A pilot study reported that there was a smoking self-reported abstinence rate of 30% (20/66) and a verified abstinence rate of 20% (13/66) after at least 6 months, due to smoking cessation sessions conducted by a general practice pharmacist [56]. A case study report showed that deprescribing in older patients by general practice pharmacists could increase medication safety of elderly patients in general practices [55]. One case study demonstrated that review of medications by a general practice pharmacist could improve patient outcomes and prevent long-term consequences in patients with HIV [62]. Further, several studies have described other potential roles for general practice pharmacists: prescribing, managing insomnia, providing specialised medication information to GPs, screening for undiagnosed diseases, on-site dispensing, and optimising medication records [32,40–42,48,51,52,57,61].
Benefits of pharmacists in general practices
The inclusion of pharmacists in general practices can increase communication and collaboration between pharmacists and GPs [32,40,41,47,48,51,52,54,57,58]. The included articles reported that collaborative interventions by general practice pharmacists can identify and resolve medication-related problems [43,46,50,52,55,62]. For example, Benson et al in 2018 reported that general practice pharmacists identified 1124 medication-related problems from 15 general practices in Western Sydney over six months [50]. Tan et al reported that the median number of medication-related problems per patient identified by a general practice pharmacist at baseline was 2, decreasing to zero at six months after general practice pharmacists’ interventions [46]. Two studies have reported that general practice pharmacists’ consultations can improve the medication adherence of patients in general practices [46,49]. One study indicated that general practice pharmacist’s consultations improved adherence as rated by the Morisky Scale (44.1% to 62.7%, p = 0.023) and Tools for Adherence and Behaviour Screening (23.6% to 57.6%, p = 0.019) in patients who had one or more risk factors for medication-related problems [46].
It has been shown that a general practice pharmacist is effective at improving the timeliness of completion of Home Medicine Reviews (HMR) [39]. A complete HMR service includes the service provided by a GP, an accredited pharmacist (a pharmacist who is licensed to conduct medication management reviews, including HMRs and Residential Medicine Management Reviews (RMMR)), and input from a multidisciplinary team from the time the patient is identified through to the implementation and ongoing monitoring of the medication management plan and any follow-up service(s) as required [72]. In 2012, Freeman et al reported that a general practice pharmacist completed HMRs in a shorter time (within 20 days) than an accredited pharmacist who is external to general practice (within 56 days) [39]. The same study showed that the number of incomplete medication reviews that were not received by the medical centre, and HMR reports not reviewed or billed by GPs were significantly reduced from 56% to 6% after including a pharmacist into general practice [39]. Furthermore, this study demonstrated potential savings of AUD 17,374 per year for general practices from the completion of HMRs by a general practice pharmacist [39]. Kosari et al in 2020 reported that activities conducted by two general practice pharmacists saved time for GPs, potentially allowing for additional GP-patient consultations [60]. In this study, the time saved for GPs was estimated to be 23.9 hours per month for a full-time pharmacist working 37.5 hours per week [60]. This study reported that two part-time general practice pharmacists’ activities generated income of AUD 7000 for general practices over 19 weeks [60]. Furthermore, this study compared the cost of employing pharmacists against the income generated by them and reported that general practice pharmacists generated income between AUD 0.61–1.20 per AUD 1.00 of a pharmacist’s salary [60].
Several articles have shown that recommendations made by general practice pharmacists to GPs were frequently accepted (mean acceptance rate: 79.8±10.7%) [39,43,49,50]. It has been shown that general practice pharmacists’ involvement in clinical activities to support GPs increased with time working at the practice [52]. It was found that the addition of a general practice pharmacist improved liaison between the general practice and outreach services in two articles [57,58]. One article highlighted that the practice pharmacist’s role was intended to be complementary to and not competitive with that of community pharmacists [58], while the article by Baker et al highlighted that general practice pharmacists liaised more with hospitals and other outreach services than accredited pharmacists who worked in conjunction with GPs [57].
Included articles in this review have not stated any clinical disadvantages of the inclusion of general practice pharmacists. However, one article reported that the role of community pharmacists may be duplicated in general practice for smoking cessation and inhaler device education, with a subsequent loss of income for the community pharmacy [54]. Overall, the reported benefits of having a general practice pharmacist are summarised in Table 1.
Table 1. Benefits of the inclusion of general practice pharmacists.
| Benefits |
|---|
| Increase communication and collaboration with GPs [32,40,41,47,48,51,52,54,57,58] |
| Identify and resolve medication-related problems [43,46,50,52,55,62] |
| Improve medication adherence [46,49] |
| Reduce time to complete a medication review [39] |
| Potential savings in money and time [39,60] |
| Increase the acceptance of pharmacists’ recommendations by GPs [39,43,49,50] |
| Improve patient health outcomes [40,48,57,62] |
| Act as a conduit between the patient’s general practice and community pharmacies, hospitals, and other outreach services [57,58] |
*GP-General Practitioner.
Perspectives of stakeholders, barriers, and facilitators of the inclusion of pharmacists into general practices
There were eleven articles (44%) exploring the perspectives of stakeholders about including pharmacists in general practices [40,41,45,47,48,51,54,57–59,61]. The studies have indicated that general practice pharmacists were highly accepted into the general practices by stakeholders, including GPs, pharmacists (accredited and community pharmacists), patients, nurses, and practice managers. The main themes identified by the stakeholders were “benefits of general practice pharmacists”, “barriers and facilitators of the inclusion of general practice pharmacists”, “pharmacists’ attributes”, “collaboration”, “logistical challenges” and “sustainability” [40,41,45,47,48,51,54,57–59,61].
Barriers. There was a number of barriers identified for the inclusion of pharmacists into general practices in Australia. The main barrier for including pharmacists into general practices was funding/lack of government support [40,41,45,47,48,51,54,57–59,61]. Logistical challenges and role clarity were other general impediments identified by the pharmacists and GPs [40,41,45,47,48,51,54,57–59,61]. A lack of clinic space, lack of time for staff to engage with the practice pharmacist, and lack of patient time to attend multiple visits were the main logistical challenges described in the articles [40,47,51,57,59,61].
Medical culture, attitudes and perception of general practice staff and patients were mentioned as barriers to the implementation of general practice pharmacists in six articles [40,45,47,51,58,61]. Underutilisation of general practice pharmacists due to poor awareness of general practice staff towards the potential services that a practice pharmacist could offer was discussed in three articles [51,54,57]. The pharmacists have reported that absence of mentors to guide them in their roles and absence of programs to train them as a general practice pharmacist were barriers for implementing this practice model [51,54,59,61].
Facilitators. Stakeholders emphasised the GPs’ willingness for collaboration, rapport, communication and team support as the main facilitators for the inclusion of pharmacists in general practices [40,41,45,47,49,51,54,57,58]. Pharmacists’ characteristics including proactivity, good communication skills, clinical competency, credibility and adaptability were other facilitators identified in this review [45,47,51,54,57]. The benefit for patients through general practice pharmacists’ services, such as providing education, was an influencing factor reported by several articles [40,48,57,59,61]. Only two articles reported having a clearly defined scope of practice as a factor facilitating the inclusion of general practice pharmacists [40,57]. GPs who actively recommended the pharmacist to the patient were stated as important to facilitate the successful implementation of general practice pharmacists [51]. Not surprisingly, remuneration/external funding was another factor that can facilitate the inclusion of general practice pharmacists [40,45,61]. A study by Freeman et al in 2012 reported that stakeholders thought that a mix of government and private funding was an appropriate model of remuneration for pharmacists in general practice [40]. The barriers and facilitators for the inclusion of general practice pharmacists are summarised in Table 2.
Table 2. Barriers and facilitators for the inclusion of general practice pharmacists in Australia.
| Barriers | Facilitators |
|---|---|
| Funding/lack of government support [40,41,45,47,48,51,54,57–59,61] | Willingness of collaboration (rapport, communication, and team support) [40,41,45,47,49,51,54,57,58] |
| Role clarity [40,41,45,47,48,51,54,57–59] | |
| Logistical challenges (office space, lack of resources and time) [40,47,51,57,59,61] | Pharmacists’ characteristics [45,47,51,54,57] |
| Lack of awareness of pharmacists’ activities and underutilisation [51,54,57] | Clearly defined scope of practice [40,57] |
| Benefits for patients and better patient outcomes [40,48,57,59,61] | |
| Medical culture, perception, and attitudes [40,45,47,51,58,61] | Recommendation by GPs to patients [51] |
| Lack of mentors [51,54,59,61] | Remuneration/external funding [40,45,61] |
*GP-General Practitioner.
Characteristics, qualifications, and experience of pharmacists in general practice
Thirteen articles (52%) included in this review mentioned the general practice pharmacists’ characteristics, qualifications, and experience [32,40,42,43,45–47,49,52,54,56,57,60]. In eleven articles, the pharmacists recruited had accreditation to perform medication reviews [32,39,40,43,45–47,49,54,57,60]. Freeman et al in 2014 conducted a survey to explore the characteristics of general practice pharmacists Australia-wide and reported that 85% (n = 22) of general practice pharmacists were accredited to conduct medication management reviews, with 27% (n = 7) having been accredited for 13–15 years, 23% (n = 6) accredited for 1–3 years, and 19% (n = 5) accredited for 7–9 years [32]. General practice pharmacists’ experience varied in the included articles in this review. Two articles reported pharmacists’ experience ranged from 3–31 years [52,54], one article reported that pharmacists’ experience ranged from 3–14 years [60], two articles reported that pharmacists had experience of more than 8 years [46,47], and one article reported that pharmacists had experience of more than 10 years [49].
Only three articles included in this review reported the educational qualifications of general practice pharmacists [32,49,57]. One of these articles reported that general practice pharmacists had postgraduate qualifications related to clinical pharmacy (clinical pharmacy is a field in which pharmacists provide direct patient care to optimise medication use, often in the hospital setting) [49]. One quantitative descriptive study conducted Australia-wide reported that 58% (n = 15) of general practice pharmacists had postgraduate qualifications: coursework masters (27% (n = 7)), graduate diploma (23% (n = 6)) or a research doctorate (15% (n = 4)) [32]. Furthermore, one article reported accredited pharmacists’ opinions about desirable characteristics of pharmacists (qualifications, skills, experience, training) to work effectively in general practice: prior experience as a hospital pharmacist, communication skills, problem solving skills, Information Technology (IT) skills and understanding pharmacoeconomics [57]. The reported characteristics, qualifications, experience, skills, and desirable special training of general practice pharmacists are summarised in Table 3.
Table 3. Overview of general practice pharmacists’ characteristics described in the articles.
| Main characteristic/ requirement | Results/description |
|---|---|
| Accreditation | Accreditation to perform medication management reviews [32,39,40,43,45–47,49,54,57,60] |
| Experience | Minimum 3 years of experience [46,47,49,52,54,60], prior hospital experience (desirable) [57] |
| Educational qualifications | Postgraduate qualifications [32,49,57] |
| Special training | Desirable training: Introductory modules by PSA, GP software, spirometry, mental health, online asthma counselling, and motivational interviewing and health coaching [57] One article stated that pharmacist had completed training related to smoking cessation [56] |
| Skills | Communication skills, problem solving skills, IT skills, understanding pharmacoeconomics [57] |
*PSA-Pharmaceutical Society of Australia, GP-General Practitioner, IT-Information Technology.
Discussion
Over the past 20 years, the role of general practice pharmacists has been expanding worldwide. This review included articles with various methodologies, which explored factors related to the general practice pharmacist model in Australia. It adds a valuable insight on the overall view of pharmacists being embedded into general practices in Australia over the last decade.
Benefits and activities of general practice pharmacists
Overall, our findings indicated that the inclusion of pharmacists in Australian general practices benefited patients by improving medication safety, mainly through resolving medication-related problems [40,43,46,48–50,52,55,57,62]. Increasing communication between general practice pharmacists and GPs is critical in order to facilitate the effective functioning of primary care services in the context of growing demand [73]. Our findings indicated that the inclusion of pharmacists in general practices can increase communication with general practice team members [32,40,41,47,48,51,52,54,57,58]. Moreover, general practice pharmacists’ recommendations were highly accepted by GPs, which demonstrates rapport between these two professionals [39,43,49,50]. These findings are supported by international studies conducted in the UK and Canada [9,13,20,25].
There are mixed views on the liaison between community pharmacists and general practice pharmacists. In this review, it was shown that a key priority of the general practice pharmacist was to act as a conduit between community pharmacy, hospital pharmacy, and the general practice [57,58]. Community pharmacists appeared less enthusiastic towards pharmacists working in general practice according to one Australian article [54], while international studies have reported mixed views on the relationship between community pharmacists and general practice pharmacists: this includes a good rapport, and significant tensions stemming from professional hierarchy and competing business-related interests [9,74,75]. However, there is a knowledge gap in examining the impact of liaison between community pharmacists and general practice-based pharmacists, mainly around HMRs, smoking cessation, and lifestyle advice [54,76]. Therefore, further studies are required to explore collaboration between community pharmacists and general practice pharmacists.
The general practice pharmacist can engage in various activities, including medication safety initiatives such as clinical audits, medication management, education, and administrative work to improve patient health outcomes in general practices [32,40,42,44,46,48–53,55–57,62]. However, the primary function of general practice pharmacists reported by the majority of the articles was medication management reviews, in line with the stakeholders’ desired function of practice pharmacists [32,39,43,46,49–51,62]. This result is expected because HMRs and RMMRs are the only government-remunerated cognitive services that a pharmacist can conduct outside the community pharmacy in Australia [77]. Even though these activities are consistent with the international literature, general practice pharmacists’ activities are relatively limited by the scope of practice in Australia [9,13,78]. In particular, Australian pharmacists are unable to prescribe like general practice pharmacists in the UK and Canada, and are therefore very reliant on GPs adopting their recommendations [11,23,43,39,43,49,50,79]. Positively, however, the general practice pharmacists’ recommendations were highly accepted by GPs [39,43,49,50].
The activities that could be performed by a general practice pharmacist may save the time of GPs and generate income for the practice. A systematic review has reported that advanced pharmacy services appear to be cost-effective when delivered in community and primary care settings, but not in domiciliary settings [80]. A recent Irish study has reported that activities (medication reviews and involvement in the repeat prescribing process) by three general practice pharmacists working for 10 hours per week over 26 weeks saved approximately EUR 57 000 per year for general practices [81]. In Australia, as elsewhere, there is limited data on cost-benefits of the role of general practice pharmacists. The potential time saved for GPs by tasks being undertaken by part-time general practice pharmacists in one study was estimated to be 23.9 hours per month for a full-time pharmacist working 37.5 hours per week [60]. Based on the findings of this review, it is recommended to further evaluate clinical and non-clinical activities, and the cost-benefits of general practice pharmacists, with robust methodologies.
Barriers and facilitators of the inclusion of general practice pharmacists
The general practice pharmacist model has been well accepted by stakeholders [40,41,45,47,48,51,54,57–59,61]. This systematic review has highlighted several barriers, including lack of resources (funding/lack of government support, logistic challenges), lack of role definition, and lack of mentoring/training. Our results are broadly consistent with international studies regarding the barriers that pharmacists face when attempting to integrate into primary care teams [9,21,82,83]. Appropriate planning and preparation can be utilised to mitigate the identified barriers [82]. Identified factors that enhanced the inclusion of general practice pharmacists were willingness to collaborate, team support, pharmacists’ characteristics, recommendation by GPs to patients, a clearly defined scope of practice and proven benefits for patients [40,41,45,47,48,51,54,57–59,61]. Positive inclusion of pharmacists into general practices appeared to be greatly reliant on the individual characteristics of the pharmacists. Pharmacists who were pro-active, adaptive, and confident were more likely able to facilitate their inclusion in Australian general practices. These findings are compatible with studies conducted in Canada [9,21,82].
This review has revealed that there is sufficient evidence to explain barriers and facilitators for the inclusion of Australian general practice pharmacists [40,41,45,47,48,51,54,57–59,61]. Unfortunately, these barriers are persisting, and it suggests that actions made to minimise barriers are still lacking. The findings of the review provide a better understanding of the barriers and facilitators when developing strategies to ensure pharmacists are successfully included in general practice teams.
Qualifications and training of general practice pharmacists
Accreditation to perform medication reviews, postgraduate qualifications, experience as a registered pharmacist, and specific skills such as communication and analytical skills, and training were the main desirable characteristics of general practice pharmacists in the articles included in this review [32,40,42,43,45–47,49,52,54,56,57,60]. The general practice pharmacists in Australia have not received formal training or guidelines before their employment. This contrasts with the inclusion of clinical pharmacists in general practices in the UK and Canada. In the UK, a government-funded general practice pharmacist training pathway was introduced for pharmacists employed in general practice. This consisted of an 18-month mandatory training program which provided a combination of study days, peer-learning groups, assessments, and access to three support functions—an education supervisor (offering individualised educational support), a GP clinical supervisor (based in practice, offering day-to-day clinical support), and a clinical mentor (an experienced clinical pharmacist) [10]. In Canada, the IMPACT training session was introduced as a transitional programme for pharmacists entering family practice to provide guidance and strategies. In addition, the “Adapting pharmacists’ skills and Approaches to maximize Patient’s drug Therapy effectiveness” (ADAPT) educational program was developed to provide a standard approach to medication assessment, team collaboration, patient assessment, evidence-based decision making and documentation, facilitated through an e-learning program for pharmacists in family health teams [20,84]. Similar models are desperately needed in Australia. Recently, the PSA has developed introductory modules for pharmacists wishing to work in general practices, focusing on the practical aspects of working as a general practice pharmacist [85]. However, the PSA training modules only provide an overview of the core knowledge and skills required by general practice pharmacists.
A Delphi study has reported 26 general practice pharmacist activities as educational needs in Australia, which was consistent with the themes in international studies [86]. This study has highlighted those activities related to medication management, chronic disease management, research, patient examination and screening, and audit and quality assurance were the major educational needs of general practice pharmacists [86]. By defining the core needs of the role, appropriate training and education programs can be developed for general practice pharmacists. Our findings support that comprehensive training programs are required for general practice pharmacists in Australia, as identified by Benson et al in [86].
Knowledge gap
Whilst the literature to date demonstrates several studies exploring the general practice pharmacist model in Australia, there is still limited evidence regarding certain areas. These include: awareness of stakeholders towards the activities that general practice pharmacists could perform, cost-benefits of including general practice pharmacists, interprofessional collaboration after including pharmacists into general practice teams, training and education needs of general practice pharmacists, guidelines/recommendations to utilise pharmacists in the general practice setting, and liaison of general practice pharmacists with community pharmacists and other out-reach services such as hospital pharmacies and aged-care facilities. While a limited number of studies indicated that general practice pharmacists’ activities improved patients’ health outcomes, evidence based on the use of robust methodologies is still lacking. Only one recent study, published outside of the search period of this review, utilised a randomised controlled trial [87]. This article reported that general practice pharmacists’ medication management services reduced the number of unplanned hospital admissions for patients recently discharged from hospitals who were prescribed five or more long-term medicines or had a primary discharge diagnosis of congestive heart failure or exacerbation of chronic obstructive pulmonary disease [87]. The estimated incremental net cost-benefit of the general practice pharmacist-led medication management services was AUD 5072 per patient, with a benefit-cost ratio of 31:1 [87]. As such, there is a need for more randomised controlled trials to explore the patient outcomes related to clinical activities that a pharmacist can perform in general practice.
Strengths and limitations
A strength of this systematic review was the inclusion of studies with various methodologies, including quantitative, qualitative and mixed-methods studies. This allowed a comprehensive and robust characterisation and evaluation of aspects of the implementation of general practice pharmacists in Australia. Moreover, abstract screening and data extraction were completed through compliance with best practice. Another strength of this review was contacting original investigators to obtain additional research information to improve the accuracy of the review.
The study has several limitations that constrain our conclusions. First, this review found a relatively small number of relevant studies. Only 25 studies were identified with various methodologies [32,39–62], which led to the choice of a narrative synthesis approach for data analysis. Second, there is the potential of researcher bias in the evaluation, although two reviewers independently assessed the articles. Third, the role of general practice pharmacists is relatively new in Australia; studies have been conducted in a limited number of general practices that believed in value of the inclusion of pharmacists in general practice. Therefore, the findings related to clinical disadvantages of the inclusion of general practice pharmacists may not be reported in the included articles in this review and the findings may not be generalisable to all Australian general practices if this model is rolled out in the future.
Study implications
The study has several implications. There is a need to:
Utilise robust methodologies to assess clinical/non-clinical activities of general practice pharmacists.
Act on the barriers and facilitators for the successful implementation of general practice pharmacists, especially those relating to funding and training.
Explore further in the areas where there are knowledge gaps related to the general practice pharmacist model identified through this review.
The findings of this systematic review will be useful for researchers, policy makers, and stakeholders to strengthen the role of general practice pharmacists in Australia. Furthermore, our findings will be beneficial for readers who wish to implement a team-based primary care model in their countries where the inclusion of pharmacists into primary care teams is not established yet.
Conclusion
This systematic review has summarised the characteristics, activities, benefits, barriers, and areas requiring further exploration relating to pharmacists working in general practice in Australia. General practice pharmacists are well accepted by stakeholders; they can engage in a range of clinical/non-clinical activities to benefit patients and general practices. This review has revealed that more actions are required on the factors that posed a challenge to the inclusion of pharmacists in general practice. Furthermore, this review has suggested more robust research to explore the patient and economic outcomes related to clinical activities that a pharmacist can perform in general practice, as a foundation to developing an appropriate and sustainable funding model.
Supporting information
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The author received no specific funding for this work.
References
- 1.Cardwell K, Smith SM. Clinical pharmacists working within family practice: what is the evidence? Fam Pract. 2018. Mar 27;35(2):120–121. doi: 10.1093/fampra/cmy003 . [DOI] [PubMed] [Google Scholar]
- 2.Freeman C, Rigby D, Aloizos J, Williams I. The practice pharmacist: a natural fit in the general practice team. Aust Prescr. 2016. Dec;39(6):211–214. doi: 10.18773/austprescr.2016.067 Epub 2016 Dec 5. ; PMCID: PMC5155053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stone MC, Williams HC. Clinical pharmacists in general practice: value for patients and the practice of a new role. Br J Gen Pract. 2015. May;65(634):262–3. doi: 10.3399/bjgp15X685033 ; PMCID: PMC4408499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cardwell K, Clyne B, Moriarty F, Wallace E, Fahey T, Boland F, et al. General Practice Pharmacist (GPP) Study Group. Supporting prescribing in Irish primary care: protocol for a non-randomised pilot study of a general practice pharmacist (GPP) intervention to optimise prescribing in primary care. Pilot Feasibility Stud. 2018. Jul 5;4:122. doi: 10.1186/s40814-018-0311-7 PMCID: PMC6034254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hazen AC, Sloeserwij VM, Zwart DL, de Bont AA, Bouvy ML, de Gier JJ, et al. Design of the POINT study: Pharmacotherapy Optimisation through Integration of a Non-dispensing pharmacist in a primary care Team (POINT). BMC Fam Pract. 2015. Jul 2;16:76. doi: 10.1186/s12875-015-0296-8 PMCID: PMC4489035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saw PS, Nissen L, Freeman C, Wong PS, Mak V. A qualitative study on pharmacists’ perception on integrating pharmacists into private general practitioner’s clinics in Malaysia. Pharm Pract (Granada). 2017. Jul-Sep;15(3):971. doi: 10.18549/PharmPract.2017.03.971 Epub 2017 Sep 2. ; PMCID: PMC5597807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barberato LC, Scherer MDDA, Lacourt RMC. The pharmacist in the Brazilian Primary Health Care: insertion under construction. Cien Saude Colet. 2019. Sep 26;24(10):3717–3726. Portuguese, English. doi: 10.1590/1413-812320182410.30772017 . [DOI] [PubMed] [Google Scholar]
- 8.Haua R, Harrison J, Aspden T. Pharmacist integration into general practice in New Zealand. J Prim Health Care. 2019. Jul;11(2):159–169. doi: 10.1071/HC18103 . [DOI] [PubMed] [Google Scholar]
- 9.Pottie K, Farrell B, Haydt S, Dolovich L, Sellors C, Kennie N, Hogg W, et al. Integrating pharmacists into family practice teams: physicians’ perspectives on collaborative care. Can Fam Physician. 2008. Dec;54(12):1714–1717.e5. ; PMCID: PMC2602632. [PMC free article] [PubMed] [Google Scholar]
- 10.Scott MA, Hitch B, Ray L, Colvin G. Integration of pharmacists into a patient-centered medical home. J Am Pharm Assoc (2003). 2011. Mar-Apr;51(2):161–6. doi: 10.1331/JAPhA.2011.10185 . [DOI] [PubMed] [Google Scholar]
- 11.Bradley F, Seston E, Mannall C, Cutts C. Evolution of the general practice pharmacist’s role in England: a longitudinal study. Br J Gen Pract. 2018 Oct;68(675):e727–e734. doi: 10.3399/bjgp18X698849 Epub 2018 Aug 28. ; PMCID: PMC6146003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dolovich L, Austin Z, Waite N, Chang F, Farrell B, Grindrod K, et al. Pharmacy in the 21st century: Enhancing the impact of the profession of pharmacy on people’s lives in the context of health care trends, evidence and policies. Can Pharm J (Ott). 2018. Dec 25;152(1):45–53. doi: 10.1177/1715163518815717 ; PMCID: PMC6346332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Avery AJ. Pharmacists working in general practice: can they help tackle the current workload crisis? Br J Gen Pract. 2017. Sep;67(662):390–391. doi: 10.3399/bjgp17X692201 ; PMCID: PMC5569715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Epperly T. The patient-centred medical home in the USA. J Eval Clin Pract. 2011. Apr;17(2):373–5. doi: 10.1111/j.1365-2753.2010.01607.x Epub 2011 Jan 11. . [DOI] [PubMed] [Google Scholar]
- 15.Lewis N, Shimp L, Rockafellow S, Tingen J, Choe HM, Marcelino M. The role of the pharmacist in patient-centered medical home practices: current perspectives. Integr Pharm Res Pract. 2014;3:29–38. doi: 10.2147/IPRP.S62670 [DOI] [Google Scholar]
- 16.American Pharmacists Association. Successful Integration of Pharmacists in Accountable Care Organizations and Medical Home Models: Case Studies [cited 6 Jan 2021]. Available from: https://www.pharmacist.com/sites/default/files/APhA%20Medical%20Home%20ACO%20Report%200320_6.pdf. [Google Scholar]
- 17.Phillips RS, Sullivan EE, Mayo-Smith MF. The Patient-Centered Medical Home and the Challenge of Evaluating Complex Interventions. JAMA Netw Open. 2020. Feb 5;3(2):e1920827. doi: 10.1001/jamanetworkopen.2019.20827 . [DOI] [PubMed] [Google Scholar]
- 18.Dolovich L, Pottie K, Kaczorowski J, Farrell B, Austin Z, Rodriguez C, et al. Integrating family medicine and pharmacy to advance primary care therapeutics. Clin Pharmacol Ther. 2008. Jun;83(6):913–7. doi: 10.1038/clpt.2008.29 Epub 2008 Mar 19. . [DOI] [PubMed] [Google Scholar]
- 19.The College of Family Physicians of Canada and the Canadian Pharmacists Association. Innovation in Primary Care: Integration of Pharmacists into Interprofessional Teams [cited 27 Sep 2020]. Available from: https://www.cfpc.ca/uploadedFiles/Health_Policy/IPC-2019-Pharmacist-Integration.pdf. [Google Scholar]
- 20.Khaira M, Mathers A, Benny Gerard N, Dolovich L. The Evolving Role and Impact of Integrating Pharmacists into Primary Care Teams: Experience from Ontario, Canada. Pharmacy (Basel). 2020. Dec 7;8(4):234. doi: 10.3390/pharmacy8040234 ; PMCID: PMC7768418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dolovich L. Ontario pharmacists practicing in family health teams and the patient-centered medical home. Ann Pharmacother. 2012. Apr;46(4):S33–9. doi: 10.1345/aph.1Q804 . [DOI] [PubMed] [Google Scholar]
- 22.Canadian Pharmacists Association. Pharmacists’ Expanded Scope of Practice [cited 16 Dec 2020]. Available from: https://www.pharmacists.ca/cpha-ca/assets/File/pharmacy-in-canada/Scope%20of%20Practice%20in%20Canada_June2020.pdf. [Google Scholar]
- 23.Emberley P. Canadian Pharmacists Scope 20/20: A vision for harmonized pharmacists’ scope in Canada. Can Pharm J (Ott). 2018. Oct 11;151(6):419–420. doi: 10.1177/1715163518804148 ; PMCID: PMC6293401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Butterworth J, Sansom A, Sims L, Healey M, Kingsland E, Campbell J. Pharmacists’ perceptions of their emerging general practice roles in UK primary care: a qualitative interview study. Br J Gen Pract. 2017. Sep;67(662):e650–e658. doi: 10.3399/bjgp17X691733 Epub 2017 Jul 3. ; PMCID: PMC5569745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Anderson C, Zhan K, Boyd M, Mann C. The role of pharmacists in general practice: A realist review. Res Social Adm Pharm. 2019. Apr;15(4):338–345. doi: 10.1016/j.sapharm.2018.06.001 Epub 2018 Jun 12. . [DOI] [PubMed] [Google Scholar]
- 26.Marques I, Gray NJ, Tsoneva J, Magirr P, Blenkinsopp A. Pharmacist joint-working with general practices: evaluating the Sheffield Primary Care Pharmacy Programme. A mixed-methods study. BJGP Open. 2018. Oct 17;2(4):bjgpopen18X101611. doi: 10.3399/bjgpopen18X101611 ; PMCID: PMC6348324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mann C, Anderson C, Avery AJ, Waring J, Boyd MJ. Clinical Pharmacists in General Practice: Pilot scheme Independent Evaluation Report: Full Report to NHS England June 2018. [cited 1 Mar 2021]. Available from: doi: 10.17639/re5w-wp5 [DOI] [Google Scholar]
- 28.The Pharmaceutical Journal. Pharmacists working in general practice increase by more than 40% in one year. Pharm. J. 2019. 303, doi: 10.1211/PJ.2019.20207405 [DOI] [Google Scholar]
- 29.National Health Services England. Clinical Pharmacists; NHS: London, UK: [cited 16 Dec 2020]. Available from: https://www.england.nhs.uk/gp/expanding-our-workforce/cp-gp/ [Google Scholar]
- 30.Swerissen H, Duckett S, Moran G. Mapping Primary Care in Australia; Grattan Institute Report No. 2018–09; Grattan Institute: Melbourne, Australia: [cited 14 Jun 2020]. Available from: https://grattan.edu.au/wp-content/uploads/2018/07/906-Mapping-primary-care.pdf. [Google Scholar]
- 31.Australian Medical Association. General Practice Pharmacists—Improving Patient Care [cited 14 Dec 2020]. Available from: https://ama.com.au/article/general-practice-pharmacists-improving-patient-care. [Google Scholar]
- 32.Freeman C, Cottrell N, Rigby D, Williams ID, Nissen L. The Australian practice pharmacist. J Pharm Pract Res. 2014;44:240–248. doi: 10.1002/jppr.1027 [DOI] [Google Scholar]
- 33.Pharmacy Guild of Australia. Review of Pharmacy Remuneration and Regulation [cited 22 Feb 2021]. Available from: https://www.guild.org.au/__data/assets/pdf_file/0024/12957/guild-submission-to-review-of-pharmacy-remuneration-and-regulation-2016.pdf. [Google Scholar]
- 34.Dixit SK, Sambasivan M. A review of the Australian healthcare system: A policy perspective. SAGE Open Med. 2018. Apr 12;6:2050312118769211. doi: 10.1177/2050312118769211 ; PMCID: PMC5900819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Calder R, Dunkin R, Rochford C, Nichols T. Australian Health Services: Too Complex to Navigate. A Review of the National Reviews of Australia’s Health Service Arrangements. Australian Health Policy Collaboration: Policy Issues Paper 1. 2019. [cited 16 Dec 2020]. Available from: https://apo.org.au/node/223011. [Google Scholar]
- 36.Tan EC, Stewart K, Elliott RA, George J. Pharmacist services provided in general practice clinics: a systematic review and meta-analysis. Res Social Adm Pharm. 2014. Jul-Aug;10(4):608–22. doi: 10.1016/j.sapharm.2013.08.006 Epub 2013 Oct 23. . [DOI] [PubMed] [Google Scholar]
- 37.Hazen ACM, de Bont AA, Boelman L, Zwart DLM, de Gier JJ, de Wit NJ, et al. The degree of integration of non-dispensing pharmacists in primary care practice and the impact on health outcomes: A systematic review. Res Social Adm Pharm. 2018. Mar;14(3):228–240. doi: 10.1016/j.sapharm.2017.04.014 Epub 2017 Apr 22. . [DOI] [PubMed] [Google Scholar]
- 38.Benson H, Lucas C, Benrimoj SI, Williams KA. The development of a role description and competency map for pharmacists in an interprofessional care setting. Int J Clin Pharm. 2019. Apr;41(2):391–407. doi: 10.1007/s11096-019-00808-4 Epub 2019 Mar 16. . [DOI] [PubMed] [Google Scholar]
- 39.Freeman C, Cottrell WN, Kyle G, Williams I, Nissen L. Does a primary care practice pharmacist improve the timeliness and completion of medication management reviews? Int J Pharm Pract. 2012. Dec;20(6):395–401. doi: 10.1111/j.2042-7174.2012.00213.x Epub 2012 Jun 1. . [DOI] [PubMed] [Google Scholar]
- 40.Freeman C, Cottrell WN, Kyle G, Williams I, Nissen L. Integrating a pharmacist into the general practice environment: opinions of pharmacist’s, general practitioner’s, health care consumer’s, and practice manager’s. BMC Health Serv Res. 2012. Aug 1;12:229. doi: 10.1186/1472-6963-12-229 ; PMCID: PMC3444319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Freeman C, Cottrell WN, Kyle G, Williams ID, Nissen L. Pharmacists’, General Practitioners’ and Consumers’ Views on Integrating Pharmacists into General Practice. J Pharm Pract Res. 2012;42:184–188. doi: 10.1002/j.2055-2335.2012.tb00166.x [DOI] [Google Scholar]
- 42.Freeman C, Kyle G, Williams ID, Nissen L. Chronicles of a primary care practice pharmacist. Integr Pharm Res Pract. 2012;1:13–18. doi: 10.2147/IPRP.S38102 [DOI] [PubMed] [Google Scholar]
- 43.Freeman CR, Cottrell WN, Kyle G, Williams ID, Nissen L. An evaluation of medication review reports across different settings. Int J Clin Pharm. 2013. Feb;35(1):5–13. doi: 10.1007/s11096-012-9701-8 Epub 2012 Sep 26. . [DOI] [PubMed] [Google Scholar]
- 44.Tan EC, George J, Stewart K, Elliott RA. Improving osteoporosis management in general practice: a pharmacist-led drug use evaluation program. Drugs Aging. 2014. Sep;31(9):703–9. doi: 10.1007/s40266-014-0194-0 . [DOI] [PubMed] [Google Scholar]
- 45.Tan EC, Stewart K, Elliott RA, George J. Integration of pharmacists into general practice clinics in Australia: the views of general practitioners and pharmacists. Int J Pharm Pract. 2014. Feb;22(1):28–37. doi: 10.1111/ijpp.12047 Epub 2013 Jun 11. . [DOI] [PubMed] [Google Scholar]
- 46.Tan EC, Stewart K, Elliott RA, George J. Pharmacist consultations in general practice clinics: the Pharmacists in Practice Study (PIPS). Res Social Adm Pharm. 2014. Jul-Aug;10(4):623–32. doi: 10.1016/j.sapharm.2013.08.005 Epub 2013 Oct 2. . [DOI] [PubMed] [Google Scholar]
- 47.Tan EC, Stewart K, Elliott RA, George J. Stakeholder experiences with general practice pharmacist services: a qualitative study. BMJ Open. 2013. Sep 11;3(9):e003214. doi: 10.1136/bmjopen-2013-003214 ; PMCID: PMC3773653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bajorek B, LeMay K, Gunn K, Armour C. The potential role for a pharmacist in a multidisciplinary general practitioner super clinic. Australas Med J. 2015. Feb 28;8(2):52–63. doi: 10.4066/AMJ.2015.2278 ; PMCID: PMC4354025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Benson H, Lucas C, Benrimoj SI, Kmet W, Williams KA. Pharmacists in general practice: recommendations resulting from team-based collaborative care. Aust J Prim Health. 2018. Jan;24(6):448–454. doi: 10.1071/PY18022 . [DOI] [PubMed] [Google Scholar]
- 50.Benson H, Lucas C, Kmet W, Benrimoj SI, Williams K. Pharmacists in general practice: a focus on drug-related problems. Int J Clin Pharm. 2018. Jun;40(3):566–572. doi: 10.1007/s11096-018-0617-9 Epub 2018 Mar 14. . [DOI] [PubMed] [Google Scholar]
- 51.Benson H, Sabater-Hernández D, Benrimoj SI, Williams KA. Piloting the Integration of Non-Dispensing Pharmacists in the Australian General Practice Setting: A Process Evaluation. Int J Integr Care. 2018. Apr 18;18(2):4. doi: 10.5334/ijic.3293 ; PMCID: PMC6095080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Deeks LS, Naunton M, Tay GH, Peterson GM, Kyle G, Davey R, et al. What can pharmacists do in general practice? A pilot trial. Aust J Gen Pract. 2018. Aug;47(8):545–549. doi: 10.31128/AJGP-03-18-4520 . [DOI] [PubMed] [Google Scholar]
- 53.Deeks LS, Kosari S, Boom K, Peterson GM, Maina A, Sharma R, et al. The Role of Pharmacists in General Practice in Asthma Management: A Pilot Study. Pharmacy (Basel). 2018. Oct 15;6(4):114. doi: 10.3390/pharmacy6040114 ; PMCID: PMC6306779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Deeks LS, Kosari S, Naunton M, Cooper G, Porritt J, Davey R, et al. Stakeholder perspectives about general practice pharmacists in the Australian Capital Territory: a qualitative pilot study. Aust J Prim Health. 2018. Jul;24(3):263–272. doi: 10.1071/PY17086 . [DOI] [PubMed] [Google Scholar]
- 55.Peterson GM, Naunton M, Deeks LS, Kosari S, Jackson SL, Boom K. Practice pharmacists and the opportunity to support general practitioners in deprescribing in the older person. J Pharm Pract Res. 2018;48:183–185. doi: 10.1002/jppr.1427 [DOI] [Google Scholar]
- 56.Deeks LS, Kosari S, Develin A, Peterson GM, Naunton M. Smoking cessation and the general practice pharmacist. J Smok Cessat. 2019;14:186–189. doi: 10.1017/jsc.2019.3 [DOI] [Google Scholar]
- 57.Baker S, Lee YP, Hattingh HL. An evaluation of the role of practice pharmacists in Australia: a mixed methods study. Int J Clin Pharm. 2019. Apr;41(2):504–515. doi: 10.1007/s11096-019-00807-5 Epub 2019 Mar 16. . [DOI] [PubMed] [Google Scholar]
- 58.Qazi A, Saba M, Armour C, Saini B. Perspectives of pharmacists about collaborative asthma care model in primary care. Res Social Adm Pharm. 2021. Feb;17(2):388–397. doi: 10.1016/j.sapharm.2020.03.006 Epub 2020 Mar 16. . [DOI] [PubMed] [Google Scholar]
- 59.Qazi A, Armour C, Saini B. Perspectives of general practitioners about a collaborative asthma care model in primary care. J Asthma. 2020. Sep 26:1–13. doi: 10.1080/02770903.2020.1823408 Epub ahead of print. . [DOI] [PubMed] [Google Scholar]
- 60.Kosari S, Deeks LS, Naunton M, Dawda P, Postma MJ, Tay GH, et al. Funding pharmacists in general practice: A feasibility study to inform the design of future economic evaluations. Res Social Adm Pharm. 2021. May;17(5):1012–1016. doi: 10.1016/j.sapharm.2020.07.030 Epub 2020 Aug 10. . [DOI] [PubMed] [Google Scholar]
- 61.Sake FT, Wong K, Bartlett DJ, Saini B. Integrated primary care insomnia management in Australia. Res Social Adm Pharm. 2018. Feb;14(2):170–179. doi: 10.1016/j.sapharm.2017.02.013 Epub 2017 Feb 20. . [DOI] [PubMed] [Google Scholar]
- 62.Mackie KF, Duncan AJ, Fineberg D, Vujovic O. Specialist pharmacist in general practice coordinating HIV patient care to manage a complicated drug–drug interaction: case report. J Pharm Pract Res, 2019; 49:291–295. doi: 10.1002/jppr.1563 [DOI] [Google Scholar]
- 63.Lizarondo L, Stern C, Carrier J, Godfrey C, Rieger K, Salmond S, et al. Chapter 8: Mixed methods systematic reviews. In: Aromataris E, Munn Z (Editors). JBI Manual for Evidence Synthesis. JBI, 2020. [cited 6 May 2021]. Available from: https://synthesismanual.jbi.global. [Google Scholar]
- 64.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009. Jul 21;339:b2535. doi: 10.1136/bmj.b2535 ; PMCID: PMC2714657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Polanin JR, Pigott TD, Espelage DL, Grotpeter JK. Best practice guidelines for abstract screening large‐evidence systematic reviews and meta‐analyses. Res Synth Methods. 2019. Sep;10(3):330–42. doi: 10.1002/jrsm.1354 Epub 2019 Jun 24. PMCID: PMC6771536. [DOI] [Google Scholar]
- 66.Disalvo D, Luckett T, Agar M, Bennett A, Davidson PM. Systems to identify potentially inappropriate prescribing in people with advanced dementia: a systematic review. BMC Geriatr. 2016. May 31;16:114. doi: 10.1186/s12877-016-0289-z ; PMCID: PMC4888427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Covidence. Veritas Health Innovation; Melbourne, Australia. www.covidence.org.
- 68.Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, et al. The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Educ Inf. 2018;34: 285–291. doi: 10.3233/EFI-180221 [DOI] [Google Scholar]
- 69.Evans D. Systematic reviews of interpretive research: interpretive data synthesis of processed data. Aust J Adv Nurs. 2002. Dec-2003 Feb;20(2):22–6. . [PubMed] [Google Scholar]
- 70.Ryan R. Cochrane Consumers and Communication Review Group. ‘Cochrane Consumers and Communication Review Group: data synthesis and analysis’ [cited 11 Oct 2020]. Available from: http://cccrg.cochrane.org. [Google Scholar]
- 71.Higgins JPT, Lasserson T, Chandler J, Tovey D, Churchill R. Methodological Expectations of Cochrane Intervention Reviews (MECIR). Standards for the conduct and reporting of new Cochrane Intervention Reviews, reporting of protocols and the planning, conduct and reporting of updates [cited 18 Mar 2021]. Available from: http://methods.cochrane.org/sites/default/files/public/uploads/mecir_printed_booklet_final.pdf. [Google Scholar]
- 72.Buss VH, Shield A, Kosari S, Naunton M. Quality Use of the Pathology Data in Home Medicines Reviews: A Retrospective Evaluation. Ann Pharmacother. 2018. Oct;52(10):992–999. doi: 10.1177/1060028018777547 Epub 2018 May 17. . [DOI] [PubMed] [Google Scholar]
- 73.The Deloitte Access Economics Commissioned by Cornerstone Health. General Practitioner Workforce Report 2019. [cited 6 Aug 2020]. Available from: https://www2.deloitte.com/au/en/pages/economics/articles/general-practitioner-workforce-report-2019.html. [Google Scholar]
- 74.Karampatakis GD, Patel N, Stretch G, Ryan K. Community pharmacy teams’ experiences of general practice-based pharmacists: an exploratory qualitative study. BMC Health Serv Res. 2020. May 18;20(1):431. doi: 10.1186/s12913-020-05245-y ; PMCID: PMC7236450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nabhani-Gebara S, Fletcher S, Shamim A, May L, Butt N, Chagger S, et al. General practice pharmacists in England: Integration, mediation and professional dynamics. Res Social Adm Pharm. 2020. Jan;16(1):17–24. doi: 10.1016/j.sapharm.2019.01.014 Epub 2019 Feb 1. . [DOI] [PubMed] [Google Scholar]
- 76.King R. Unintended consequences of pharmacists working in GP practices. Pharm J. 2015. [cited 8 Jan 2021]. Available from: https://www.pharmaceutical-journal.com/opinion/comment/unintended-consequences-of-pharmacists-working-in-gp-practices/20068159.article. [Google Scholar]
- 77.Australian Government Department of Health. Medicare Benefits Schedule Online [cited 20 Sep 2020]. Available from: http://www.mbsonline.gov.au/internet/mbsonline/publishing.nsf/Content/Home. [Google Scholar]
- 78.Cresswell KM, Sadler S, Rodgers S, Avery A, Cantrill J, Murray SA, et al. ; PINCER Evaluation Team. An embedded longitudinal multi-faceted qualitative evaluation of a complex cluster randomized controlled trial aiming to reduce clinically important errors in medicines management in general practice. Trials. 2012. Jun 8;13:78. doi: 10.1186/1745-6215-13-78 ; PMCID: PMC3503703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zhou M, Desborough J, Parkinson A, Douglas K, McDonald D, Boom K. Barriers to pharmacist prescribing: a scoping review comparing the UK, New Zealand, Canadian and Australian experiences. Int J Pharm Pract. 2019. Dec;27(6):479–489. doi: 10.1111/ijpp.12557 Epub 2019 Jul 9. . [DOI] [PubMed] [Google Scholar]
- 80.Dawoud DM, Haines A, Wonderling D, Ashe J, Hill J, Varia M, et al. Cost Effectiveness of Advanced Pharmacy Services Provided in the Community and Primary Care Settings: A Systematic Review. Pharmacoeconomics. 2019. Oct;37(10):1241–1260. doi: 10.1007/s40273-019-00814-4 . [DOI] [PubMed] [Google Scholar]
- 81.Cardwell K, Smith SM, Clyne B, McCullagh L, Wallace E, Kirke C, et al. ; General Practice Pharmacist (GPP) Study Group. Evaluation of the General Practice Pharmacist (GPP) intervention to optimise prescribing in Irish primary care: a non-randomised pilot study. BMJ Open. 2020. Jun 28;10(6):e035087. doi: 10.1136/bmjopen-2019-035087 ; PMCID: PMC7322285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jorgenson D, Laubscher T, Lyons B, Palmer R. Integrating pharmacists into primary care teams: barriers and facilitators. Int J Pharm Pract. 2014. Aug;22(4):292–9. doi: 10.1111/ijpp.12080 Epub 2013 Nov 27. . [DOI] [PubMed] [Google Scholar]
- 83.Ryan K, Patel N, Lau WM, Abu-Elmagd H, Stretch G, Pinney H. Pharmacists in general practice: a qualitative interview case study of stakeholders’ experiences in a West London GP federation. BMC Health Serv Res. 2018. Apr 2;18(1):234. doi: 10.1186/s12913-018-3056-3 ; PMCID: PMC5879559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Farrell B, Ward N, Jennings B, Jones C, Jorgenson D, Gubbels-Smith A, et al. Participation in online continuing education. Int J Pharm Pract. 2016. Feb;24(1):60–71. doi: 10.1111/ijpp.12202 Epub 2015 Jul 15. . [DOI] [PubMed] [Google Scholar]
- 85.Pharmaceutical Society of Australia. General Practice Pharmacist Training [cited 29 Jun 2020]. Available from: https://www.psa.org.au/career-and-support/career-pathways/general-practice-pharmacist/gpp-training/. [Google Scholar]
- 86.Benson H, Lucas C, Williams KA. Establishing consensus for general practice pharmacist education: A Delphi study. Curr Pharm Teach Learn. 2020. Jan;12(1):8–13. doi: 10.1016/j.cptl.2019.10.010 Epub 2019 Nov 19. . [DOI] [PubMed] [Google Scholar]
- 87.Freeman CR, Scott IA, Hemming K, Connelly LB, Kirkpatrick CM, Coombes I, et al. Reducing Medical Admissions and Presentations Into Hospital through Optimising Medicines (REMAIN HOME): a stepped wedge, cluster randomised controlled trial. Med J Aust. 2021. Mar;214(5):212–217. doi: 10.5694/mja2.50942 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.