Abstract
Background
This study aimed to assess the awareness and attitudes toward human papillomavirus (HPV) vaccination among female college freshmen and explore their willingness and associated factors to receive the HPV vaccine based on the information–motivation–behavior skills (IMB) model.
Methods
From February 21 to April 30, 2020, a cross-sectional survey was conducted among female freshmen in seven colleges in mainland China. Socio-demographic characteristics, health-related awareness, knowledge of HPV, motivation, and behavioral skills toward HPV vaccination were assessed using questionnaires. Univariate and multivariate logistic regression analyses were performed to identify the influencing factors of willingness to receive the HPV vaccine in the next 6 months.
Results
Among the 3867 students invited to participate in this study, 102 (2.64%) reported having taken the HPV vaccine. Among the unvaccinated participants, 59.89% had previously heard of HPV, and 32.08% were willing to take the HPV vaccine in the next 6 months. Willingness to get the HPV vaccine was associated with sexual experience(s) (AOR = 1.96, 95% CI: 1.25–3.08), family or friends with cancer (AOR = 1.24, 95% CI: 1.04–1.48), having heard of HPV (AOR = 1.23, 95% CI: 1.03–1.47), and having actively searched for or having consulted on issues concerning HPV vaccine (AOR = 1.22, 95% CI: 1.02–1.45). In the dimensions of the IMB model, “perceived susceptibility” (AOR = 1.20, 95% CI: 1.09–1.31), “perceived severity” (AOR = 1.24, 95% CI: 1.11–1.39), “subjective norms” (AOR = 2.09, 95% CI: 1.75–2.49), and “self-efficacy” (AOR: 2.95, 95% CI: 2.44–3.58) were positively associated with HPV vaccination acceptance, while “perceived barriers” (AOR = .60, 95% CI: .52–.69) negatively affected intention to get HPV vaccination.
Conclusion
HPV vaccination rates and willingness to receive the HPV vaccine in the next 6 months were found to be poor among female college freshmen in mainland China. Having a positive attitude toward HPV vaccination, creating vaccine-friendly social norms, and removing related barriers are important measures to promote HPV immunization.
Keywords: human papillomavirus vaccine, willingness, information–motivation–behavior skills, college female freshmen, China
Introduction
Cervical cancer has been a major public health problem for women for several decades. It is the fourth most diagnosed cancer among women worldwide, with 570 000 new cases and 311 000 deaths reported in 2018. In 2018, 106 000 new cases and 48 000 deaths due to cervical cancer were reported in China. 1 Similar to other sexually transmitted diseases, human papillomavirus (HPV) infection is a prerequisite for the development of cervical cancer.2,3 Among the high-risk types of HPV, HPV-16 and -18 are considered to account for approximately 70% of cervical cancers worldwide.4,5 The introduction of vaccines against high-risk HPV has proven to be an effective measure for the prevention and control of cervical cancer.6,7
As of October 2020, 110 countries around the world have introduced HPV vaccines into their national immunization programs. 8 The HPV vaccine was approved by the Chinese authorities in 2016, 10 years after the first HPV vaccine became available in the US. 9 As a public health prevention tool, the success of the HPV vaccine lies in its widespread use among the most appropriate target groups, such as teenage girls who have not had sex yet. 10 However, even though the efficacy and safety of vaccines have been widely recognized, the HPV vaccination rate among Chinese adolescents is still not satisfactory.11-13
Previous studies have found some reasons for HPV vaccine refusal in the ideal target population, including a comparatively conservative attitude toward sex, inability to afford the vaccine, lack of awareness due to low media coverage, low perceived susceptibility, and concerns about the safety, side effects, efficacy, and injection pain.11-15 This study focused on exploring the predictors of HPV vaccine willingness based on the information–motivation–behavioral skills (IMB) model among female Chinese university students. 16 In the context of HPV vaccination, the IMB model suggests that acceptance of HPV vaccines can be predicted by analyzing the respondents’ personal knowledge of HPV, the perceived susceptibility to HPV infection (risk of infection), the perceived severity of HPV infection (eg, progression to cervical cancer or death), their beliefs about the benefits of HPV vaccination (eg, prevention of HPV infection), and the barriers to HPV vaccination (eg, affordability issues).17-19 In addition, subjective norms (belief that people around them would support HPV vaccination and they would comply with their opinions), the ability to make decisions (individuals can make their own decisions to adopt healthy behaviors since health is valued), and self-efficacy (the belief that individual can overcome obstacles to get HPV vaccination) also influence the intention of HPV vaccination.17-19
In line with the need for knowledge about safe sex and the declining age of first sexual intercourse, female adolescents in China are vulnerable to sexually transmitted infections, especially HPV.20-22 In response to the World Health Organization’s initiative to eliminate cervical cancer by 2030, 23 the current cross-sectional study conducted in seven geographic regions in mainland China explored the predictors of willingness to receive the HPV vaccine among female college freshmen based on the IMB model. Our findings would be useful in identifying the key links to promote HPV vaccination among Chinese college girls, as well as target populations among neighboring Asian countries that share a similar cultural background.
Methods
Settings
The study participants were recruited from colleges from seven geographical territories in China, located in the eastern, southern, central, north, northwest, southwest, and northeast parts of China, namely, Jinan University, Sun Yat-sen University, Henan Institute of Engineering, Shanxi University of Finance and Economics, Xinjiang Agricultural University, Sichuan University, and Dalian University of Technology.
Study Population and Quality Control
This cross-sectional study was conducted between February 21 and April 30, 2020. An online self-administered questionnaire was disseminated and administered by university staff in each geographical territory. Female freshmen older than 18 years who had no vaccination contraindications and had mobile phone or computer access were invited to participate in the study. Medical students or those who were pregnant or were breastfeeding were excluded from the study.
On November 15, 2019, we conducted a pilot study among 28 female students at the University of Jinan in Shandong Province, China. Among them, 10 (35.71%) of them reported their willingness to undergo the HPV vaccination in the following 6 months. According to the minimum sample size formula, n = Z2 × P(1−P)/d2, the calculated sample size was 353 using an expected willingness of HPV vaccination of 35.71%, considering a 95% confidence interval (CI) and a 5% allowable error. Allowing for a 15% rate of non-response, 416 cases were required in each university, and a total of 2912 cases were required for the cross-sectional survey. To ensure the representativeness of the cross-sectional survey, and to meet the required sample size (calculated to be at least 3360 subjects) for a subsequent randomized controlled intervention study in the same population aimed at improving HPV vaccination rates (see the published protocol article for details), 19 we ended up recruiting 3968 female freshmen for the whole project.
In addition, two basic pieces of information would be collected for quality control: (1) ID number should conform to the coding rules and (2) the vaccination date must be after 2016 for those who self-reported that they had been vaccinated against HPV in mainland China. Only questionnaires that passed the above quality control were included in the statistical analysis.
Among the 3968 participants recruited in the study, 3867 (97.45%) met the quality control requirements. At the end of the study, each participant was given a notebook and pen with the research logo as compensation for his or her time and participation.
Ethics
Ethical approval for the study was obtained from the Institutional Review Board of the Chinese Center for Disease Control and Prevention on October 24, 2019. Before enrollment in the study, participants were well informed of the purposes, methods, expected risks, and benefits of this research. A consent form was presented on the first page of the questionnaire, and participants who agreed to participate in the study clicked on the consent button to jump to the questionnaire page.
Data Collection
Data were collected using an anonymous questionnaire designed by a panel of the Peking Union Medical College. The structured questionnaire included demographic information, health-related perceptions, and the constructs of the IMB model, which included knowledge of HPV, motivation, behavioral skills, and willingness to take HPV vaccine.
Measurements
The intention of HPV vaccination was measured by asking the participants if they were willing to receive the HPV vaccine in the next 6 months (“Yes” or “No”). All the independent variables are described below.
Socio-demographic characteristics included age, major in school, ethnicity, place of residence for more than 1 year, monthly living expenses, education level of parents, previous sexual experience, current relationship, and whether they had relatives and/or friends with cancer.
Health-related variables included “agree that vaccines can effectively prevent diseases,” having received sexual education, attitude toward premarital sex, having previously heard of HPV, and had actively searched for or consulted on issues concerning HPV vaccination (“Yes” or “No”).
Knowledge concerning HPV was measured by asking participants eleven information-related items about HPV used in previous studies. The answers were “Agree,” “Disagree,” or “Do not know” (Table 2).24-28 Each correct answer was assigned one point, while incorrect or unknown answers were assigned zero points. The total score of the knowledge questions was derived by adding the number of correct responses. Higher scores indicate more information about HPV was known. Cronbach’s alpha for the 11 items was .78.
Table 2.
HPV-related knowledge and willingness to be vaccinated among participants (N = 3765).
| Question items | All | Willing to receive HPV vaccine | |||
|---|---|---|---|---|---|
| N (%) | Yes (%) | No (%) | Chi-square a | P | |
| HPV is related to the development of cervical cancer | |||||
| Agree b | 2635(69.99) | 906(75.00) | 1729(67.62) | 21.28 | .00 |
| Disagree | 73(1.94) | 23(1.90) | 50(1.96) | ||
| Do not know | 1057(28.07) | 279(23.10) | 778(30.43) | ||
| Males can be infected with HPV | |||||
| Agree b | 2434(64.65) | 93(7.70) | 194(7.59) | 9.43 | .00 |
| Disagree | 287(7.62) | 823(68.13) | 1611(63.00) | ||
| Do not know | 1044(27.73) | 292(24.17) | 752(29.41) | ||
| HPV is related to sexual behavior | |||||
| Agree b | 1994(52.96) | 696(57.62) | 1298(50.76) | 15.47 | .00 |
| Disagree | 351(9.32) | 121(10.02) | 230(8.99) | ||
| Do not know | 1420(37.72) | 391(32.37) | 1029(40.24) | ||
| Condoms can prevent HPV infection | |||||
| Agree b | 1408(37.40) | 534(44.21) | 874(34.18) | 35.22 | .00 |
| Disagree | 774(20.65) | 242(20.03) | 532(20.81) | ||
| Do not know | 1583(42.05) | 432(35.76) | 1151(45.01) | ||
| HPV is almost asymptomatic | |||||
| Agree b | 317(8.42) | 126(10.43) | 191(7.47) | 9.33 | .00 |
| Disagree | 2275(60.42) | 778(64.40) | 1497(58.55) | ||
| Do not know | 1173(31.16) | 304(25.17) | 869(33.99) | ||
| The HPV vaccine protects against all types of cervical cancer | |||||
| Agree | 140(3.72) | 64(5.30) | 76(2.97) | 4.18 | .04 |
| Disagree b | 2717(72.16) | 898(74.34) | 1819(71.14) | ||
| Do not know | 908(24.12) | 246(20.36) | 662(25.89) | ||
| HPV infection may result in oral cancer, condyloma acuminatum, and anal cancer | |||||
| Agree b | 2214(58.80) | 775(64.16) | 1439(56.28) | 21.02 | .00 |
| Disagree | 292(7.76) | 88(7.28) | 204(7.98) | ||
| Do not know | 1259(33.44) | 345(28.56) | 914(35.75) | ||
| Most HPV infections will disappear on their own | |||||
| Agree b | 354(9.40) | 143(11.84) | 211(8.25) | 12.38 | .00 |
| Disagree | 1652(43.88) | 578(47.85) | 1074(42.00) | ||
| Do not know | 1759(46.72) | 487(40.31) | 1272(49.75) | ||
| HPV infection is very common | |||||
| Agree b | 1025(27.22) | 405(33.53) | 620(24.25) | 35.66 | .00 |
| Disagree | 947(25.15) | 304(25.17) | 643(25.15) | ||
| Do not know | 1793(47.62) | 499(41.31) | 1294(50.61) | ||
| Regular cervical cancer screening is unnecessary after HPV vaccination | |||||
| Agree | 33(.88) | 16(1.32) | 17(.66) | 20.77 | .00 |
| Disagree b | 2872(76.28) | 977(80.88) | 1895(74.11) | ||
| Do not know | 860(22.84) | 215(17.8) | 645(25.22) | ||
| The best time for HPV vaccination is before any experience of sexual contact | |||||
| Agree b | 1697(45.07) | 690(57.12) | 1007(39.38) | 104.26 | .00 |
| Disagree | 191(5.07) | 62(5.13) | 129(5.04) | ||
| Do not know | 1877(49.85) | 456(37.75) | 1421(55.57) | ||
Abbreviation: HPV, human papillomavirus.
aChi-square test was used to test the difference of the distribution of “correct answer” and “incorrect answer or do not know” in the two groups of participants who were willing and not willing to receive HPV vaccine.
bAppropriate response.
Motivation for vaccination was measured in five dimensions: perceived susceptibility (perceptions of likelihood that they may get HPV infection), perceived severity (perceptions of the seriousness of the consequences related to HPV infection), perceived benefits and barriers (potential advantages and obstacles to participation in HPV vaccination), and subjective norms (perceived support from significant others toward HPV vaccination and the motivation to follow their recommendations) (Table A1).
Perceived susceptibility toward HPV infection was assessed by two items published in former studies: Cronbach’s alpha of the two items in our study was .92. 29 Perceived severity regarding HPV infection was assessed using four items, and Cronbach’s alpha in the present study was .80.25,30 Perceived benefits and barriers toward HPV vaccination were assessed using three and five items, respectively, and Cronbach’s alpha in the present study was .78 and .72, respectively.25,30,31 In addition, subjective norms regarding HPV vaccination were assessed by five items from previous studies, and Cronbach’s alpha in our study was .73. 27 Each item was assessed using a 5-point Likert scale (1 = strongly disagree, 2 = disagree, 3 = neither disagree nor agree, 4 = agree, and 5 = strongly agree). Except for the negative trend of perceived barriers, the higher scores of other items indicated stronger motivation of the participants to receive the HPV vaccine.
Behavioral skills: Two dimensions with a total of ten items were used to evaluate participants’ behavioral skills, including perceived control in decision-making about HPV vaccination, and perceived self-efficacy (beliefs that they can successfully take up the HPV vaccination).28,30 Answers for these items were measured on a 5-point Likert scale (1 = strongly disagree and 5 = strongly agree). Further details are presented in the appendix.
The ability of making decisions independently was evaluated by two items, while perceived self-efficacy to uptake the HPV vaccine was measured by eight items, and Cronbach’s alpha in the present study was .89 and .88, respectively. An average score was obtained by summing the responses of the ten items, and higher scores indicated more effective adoption of HPV vaccination.
Statistical Analysis
Statistical analysis was performed using SPSS 23.0. Descriptive analysis was performed to acquire socio-demographic characteristics, health awareness, and suitable understanding of HPV-related knowledge. To identify the different distribution of variables among groups that were willing and unwilling to take the vaccine, the chi-square test and Student’s t-test were used for categorical and continuous variables, respectively. The influencing factors of the intention of HPV vaccination were determined by logistic multivariate regression, and significant variables in the univariate analysis were further entered into the multivariate logistic regression model, where adjusted odds ratios (AORs) and their corresponding 95% CIs were calculated. Statistical significance was set at P < .05 (2-tailed test).
Results
Participants’ Background Characteristics
Of the 3867 verified respondents, 3765 were included in the final analysis as 102 respondents had been vaccinated before the questionnaire survey (the vaccination rate was 2.64%). The mean age of the participants was 19 years (standard deviation [SD] ±.82). As shown in Table 1, only 1208 (32.08%) participants were willing to take the HPV vaccine in the next 6 months. Of these, 47.30% majored in science, and the majority (87.78%) were Han Chinese. 64.25% had lived in urban areas for more than 1 year, 71.16% had monthly living expenses ranging from 1000 to 2000 yuan, and 25.21% of the participants’ parents had educational qualifications equaling a college degree or higher. Only 2.87% of the participants had prior sexual experience, 17.29% were in a romantic relationship, and 24.25% of the participants had relatives or friends with cancer.
Table 1.
Socio-demographics, health-related characteristics, and willingness to be vaccinated among participants (N = 3765).
| Variables | All | Willing to receive HPV vaccine | |||
|---|---|---|---|---|---|
| N (%) | Yes (%) | No (%) | Chi-square | P | |
| Socio-demographic | |||||
| Age (years) | |||||
| 18 | 693(18.41) | 206(17.05) | 487(19.05) | 2.74 | .26 |
| 19 | 2231(59.26) | 719(59.52) | 1512(59.13) | ||
| ≥20 | 841(22.34) | 283(23.43) | 558(21.82) | ||
| Mean ± SD | 19.12±.82 | 19.14±.72 | 19.11±.86 | ||
| Major in school | |||||
| Science | 1781(47.30) | 563(46.61) | 1218(47.63) | .35 | .56 |
| Liberal art | 1984(52.70) | 645(53.39) | 1339(52.37) | ||
| Ethnicity | |||||
| Han | 3305(87.78) | 1050(86.92) | 2255(88.19) | 1.23 | .27 |
| Other | 460(12.22) | 158(13.08) | 302(11.81) | ||
| Permanent residence (for more than one year) | |||||
| Rural | 1346(35.75) | 350(28.97) | 996(38.95) | 35.56 | .00 |
| Urban | 2419(64.25) | 858(71.03) | 1561(61.05) | ||
| Living Expenses (RMB/month) | |||||
| <1000 yuan | 771(20.48) | 196(16.23) | 575(22.49) | 59.38 | .00 |
| 1000–2000 yuan | 2679(71.16) | 859(71.11) | 1820(71.18) | ||
| 2001–3000 yuan | 279(7.41) | 130(10.76) | 149(5.83) | ||
| >3000 yuan | 36(.96) | 23(1.90) | 13(.51) | ||
| Education level of parents | |||||
| Junior high school or below | 1694(44.99) | 464(38.41) | 1230(48.1) | 38.18 | .00 |
| Senior high school ( including vocational high school) | 1122(29.80) | 375(31.04) | 747(29.21) | ||
| College (including technical college) and above | 949(25.21) | 369(30.55) | 580(22.68) | ||
| Previous sexual experience | |||||
| No | 3657(97.13) | 1149(95.12) | 2508(98.08) | 25.94 | .00 |
| Yes | 108(2.87) | 59(4.88) | 49(1.92) | ||
| Currently relationship | |||||
| No | 3114(82.71) | 956(79.14) | 2158(84.40) | 15.85 | .00 |
| Yes | 651(17.29) | 252(20.86) | 399(15.60) | ||
| Family/friends with any cancer (including cervical cancer) | |||||
| No | 2852(75.75) | 850(70.36) | 2002(78.29) | 28.09 | .00 |
| Yes | 913(24.25) | 358(29.64) | 555(21.71) | ||
| Health-related variables | |||||
| Believe vaccination is effective in preventing disease | |||||
| No | 266(7.07) | 68(5.63) | 198(7.74) | 5.59 | .02 |
| Yes | 3499(92.93) | 1140(94.37) | 2359(92.26) | ||
| Ever received sexual education | |||||
| No | 788(20.93) | 184(15.23) | 604(23.62) | 34.89 | .00 |
| Yes | 2977(79.07) | 1024(84.77) | 1953(76.38) | ||
| Attitude toward premarital sex | |||||
| Con | 2327(61.81) | 662(54.80) | 1665(65.12) | 36.97 | .00 |
| Pro | 1438(38.19) | 546(45.20) | 892(34.88) | ||
| Ever heard of HPV | |||||
| No | 1510(40.11) | 349(28.89) | 1161(45.40) | 93.14 | .00 |
| Yes | 2255(59.89) | 859(71.11) | 1396(54.60) | ||
| Ever actively searched for or consulted on HPV vaccine | |||||
| No | 2540(67.46) | 660(54.64) | 1880(73.52) | 133.34 | .00 |
| Yes | 1225(32.54) | 548(45.36) | 677(26.48) | ||
Abbreviation: HPV, human papillomavirus.
In terms of health-related variables, 92.93% agreed that vaccination was effective in preventing disease. Among the participants, 79.07% had received sexual education previously, while 38.19% said they could accept premarital sex. More than half of the participants (59.89%) had heard of HPV previously, while only 32.54% had actively searched for or consulted on issues concerning HPV vaccination. A statistically significant difference between groups that were willing and unwilling to undergo vaccination was identified using the chi-square test. The results showed that in addition to age, major in school, and ethnicity, other variables were related to the willingness to receive HPV vaccination (P < .05).
Knowledge of HPV
There were 11 questions about HPV, HPV-associated diseases, and HPV vaccine. About 70% of participants knew that “HPV is related to the development of cervical cancer” (69.99%) and “Males can be infected with HPV” (64.65%). In addition, 76.28% and 72.16% of respondents knew that the statements “Regular cervical cancer screening is unnecessary after HPV vaccination” and “The HPV vaccine protects against all types of cervical cancer” were false, respectively. However, less than 10% of the study participants correctly answered the questions “HPV is almost asymptomatic” (8.42%) and “A majority of HPV infections will disappear on their own” (9.40%). In addition, 52.96% and 58.80% of the students correctly answered the questions that “HPV is related to sexual contact” and “HPV infection may cause condyloma acuminatum, oral cancer, and other diseases,” respectively. Furthermore, 45.07%, 37.40%, and 27.22% of the participants correctly answered the questions that “The best time for HPV vaccination is before any experience of sexual contact,” “Condoms prevent HPV infection,” and “HPV infection is very common.” As shown in Table 2, a statistically significant difference between the groups that were willing and unwilling to receive the HPV vaccine was observed using the chi-square test. Further, greater awareness concerning HPV-related knowledge was observed in the group willing to receive the HPV vaccine (P < .05).
Dimensions of the IMB Model
As shown in Table 3, the mean score of HPV-related information was 5.22 ± 2.74. For the motivation of HPV vaccination, the average perceived susceptibility score was 2.44 ± .89, the average perceived severity score was 3.45 ± .74, the mean perceived benefits level was 3.93 ± .60, the mean perceived barriers level was 2.94 ± .61, and the average score of perceived norms was 3.15 ± .51. In terms of objective skills for HPV vaccination, the average score of perceived decision-making was 4.27 ± .57, and the mean self-efficacy level was 3.50 ± .59. A statistically significant difference between the groups that were willing and unwilling to receive the HPV vaccine was observed using the Student’s t-test, with a higher level of information, motivation, and behavioral skills toward HPV vaccination observed in the group willing to receive the HPV vaccine (P < .05).
Table 3.
Dimensions of the IMB model and willingness to be vaccinated among participants (N = 3765).
| Dimensions of the IMB model | All | Willing to receive HPV vaccine | |||
|---|---|---|---|---|---|
| Mean(SD) | Yes (mean[SD]) | No (mean[SD]) | t-value | P | |
| Information (knowledge of HPV) | 5.22(2.74) | 5.77(2.65) | 4.96(2.74) | 8.53 | .00 |
| Motivation | |||||
| Perceived susceptibility | 2.44(.89) | 2.59(.91) | 2.38(.87) | 6.91 | .00 |
| Perceived severity | 3.45(.74) | 3.49(.76) | 3.43(.73) | 2.11 | .04 |
| Perceived benefits | 3.93(.60) | 4.07(.60) | 3.86(.59) | 9.89 | .00 |
| Perceived barriers | 2.94(.61) | 2.75(.63) | 3.03(.58) | -12.97 | .00 |
| Subjective norms | 3.15(.51) | 3.37(.52) | 3.05(.47) | 17.71 | .00 |
| Behavioral skills | |||||
| Decision-making | 4.27(.57) | 4.36(.57) | 4.22(.56) | 7.05 | .00 |
| Self-efficacy | 3.50(.59) | 3.81(.57) | 3.35(.53) | 23.55 | .00 |
Abbreviations: HPV, human papillomavirus; IMB, information–motivation–behavior.
Multivariate Correlates of HPV Vaccination Intention
Table 4 presents the univariate and multivariate correlates of HPV vaccination intention with significant variables (P < .05) in Tables 1 and 3. After adjusting for all other covariates, participants who had prior sexual intercourse (AOR = 1.96, 95% CI: 1.25–3.08) and had family or friends with cancer (AOR = 1.24, 95% CI: 1.04–1.48) were more likely to be vaccinated. Also, individuals who had heard of HPV (AOR = 1.23, 95% CI: 1.03–1.47) and had ever actively searched for or consulted on HPV vaccine issues (AOR = 1.22, 95% CI: 1.02–1.45) were more likely to be vaccinated.
Table 4.
Influencing factors of HPV vaccination intention among participants (N = 3765).
| Variables | Willing to receive HPV vaccine | ||
|---|---|---|---|
| Unadjusted OR (95% CI) | Adjusted OR (95% CI) | P | |
| Permanent residence (for more than one year) | |||
| Rural | 1 | 1 | |
| Urban | 1.56(1.35–1.81) | 1.08(.89–1.30) | .44 |
| Living expenses (RMB/month) | |||
| <1000 yuan | 1 | 1 | |
| 1000–2000 yuan | 1.39(1.16–1.66) | .90(.73–1.11) | .32 |
| 2001–3000 yuan | 2.56(1.92–3.41) | .93(.66–1.32) | .70 |
| >3000 yuan | 5.19(2.58–10.44) | 2.18(.97–4.92) | .06 |
| Education level of parents | |||
| Junior high school or below | 1 | 1 | |
| Senior high school ( including vocational high school) | 1.33(1.13–1.57) | .96(.79–1.16) | .66 |
| College (including technical college) and above | 1.69(1.43–2.00) | .87(.69–1.09) | .21 |
| Previous sexual experience | |||
| No | 1 | 1 | |
| Yes | 2.63(1.79–3.86) | 1.96(1.25–3.08) | .00** |
| Currently relationship | |||
| No | 1 | 1 | |
| Yes | 1.43(1.20–1.70) | 1.10(.90–1.35) | .35 |
| Family or friends with any cancer (including cervical cancer) | |||
| No | 1 | 1 | |
| Yes | 1.52(1.30–1.77) | 1.24(1.04–1.48) | .02* |
| Vaccination is effective in preventing disease | |||
| No | 1 | 1 | |
| Yes | 1.41(1.06–1.87) | .91(.66–1.25) | .55 |
| Ever received sexual education | |||
| No | 1 | 1 | |
| Yes | 1.72(1.44–2.06) | 1.14(.93–1.39) | .22 |
| Attitude toward premarital sex | |||
| Con | 1 | 1 | |
| Pro | 1.54(1.34–1.77) | 1.06(.90–1.25) | .51 |
| Ever heard of HPV | |||
| No | 1 | 1 | |
| Yes | 2.05(1.77–2.37) | 1.23(1.03–1.47) | .03* |
| Ever actively searched for or consulted on HPV vaccination | |||
| No | 1 | 1 | |
| Yes | 2.31(2.00–2.66) | 1.22(1.02–1.45) | .03* |
| Information | 1.12(1.09–1.15) | 1.01(.97–1.04) | .73 |
| Motivation | 1.01(.97–1.04) | .73 | |
| Perceived susceptibility | 1.31(1.22–1.42) | 1.20(1.09–1.31) | .00** |
| Perceived severity | 1.11(1.01–1.21) | 1.24(1.11–1.39) | .00** |
| Perceived benefits | 1.82(1.61–2.06) | .86(.73–1.00) | .05 |
| Perceived barriers | .46(.41–.52) | .60(.52–.69) | .00** |
| Subjective norms | 3.90(3.32–4.57) | 2.09(1.75–2.49) | .00** |
| Behavioral skills | |||
| Decision-making | 1.56(1.38–1.77) | .86(.74–1.01) | .06 |
| Self-efficacy | 4.54(3.94–5.24) | 2.95(2.44–3.58) | .00** |
*P < .05; **P < .01. Abbreviation: HPV, human papillomavirus.
Among the dimensions of the IMB model, participants who had high scores of “perceived susceptibility” (AOR = 1.20, 95% CI: 1.09–1.31), “perceived severity” (AOR = 1.24, 95% CI: 1.11–1.39), “subjective norms” (AOR = 2.09, 95% CI: 1.75–2.49), and “self-efficacy” (AOR: 2.95, 95% CI: 2.44–3.58) were more likely to be vaccinated. On the other hand, those who had a high score of “perceived barriers” (AOR = .60, 95% CI: .52–.69) were less likely to receive the HPV vaccine in the next 6 months.
Reasons for Unwilling to Get HPV Vaccine
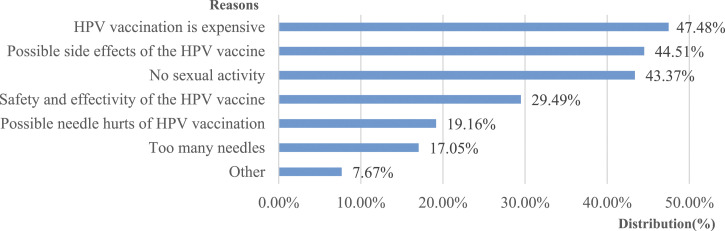
Among the students unwilling to get the HPV vaccine in the following 6 months, the top three common reasons reported were as follows: “HPV vaccination is expensive” (47.48%), “Worry about the possible side effects of the HPV vaccine” (44.51%), and “No sexual activity” (43.37%). In addition, 7.67% of participants chose the “other” option, and the reasons for self-reported group that was unwilling to receive the HPV vaccine in the near future included “Not enough information to make a decision about HPV vaccination,” “Not yet, preferring to wait until I’m a little older or after college,” “Family conditions do not support vaccination in the short term, I should be vaccinated in the future,” “Parents do not know about the HPV vaccine, and my friends aren’t vaccinated yet,” and “Hesitation to get vaccinated in general, not specifically for HPV” (Figure 1).
Figure 1.
Reasons for unwilling to get human papillomavirus vaccine.
Discussion
In China, cervical cancer remains one of the most common cancers among women despite advances in HPV vaccines and cancer screening. The HPV vaccination rate was 2.64% among female freshmen in our study, which was lower than that of the three previous studies with all “female college students,” which were 3.57%, 11.00%, and 9.50%, respectively.11-13 In addition, only 32.08% of participants were willing to receive the HPV vaccine in the next 6 months, and few had in-depth knowledge of HPV-related diseases and the corresponding prevention and control measures. It is worth noting that participants with sexual experience were more willing to take the HPV vaccine. Since HPV infection is a common sexually transmitted disease and people are concerned about the risk of infection from existing sexual behaviors, those who had prior sexual experience were more willing to take preventive measures such as HPV vaccination. 22 Additionally, only 2.87% of participants in our study had sexual experience(s), which may be a major reason for the low vaccination rate and willingness to be vaccinated against HPV. With a decrease in the age of individuals at their first sexual intercourse and the greater odds of sexual intercourse as their age increases, it is particularly important to improve vaccination rates and intention for vaccination among populations who have not yet had sex.20,22
The reasons behind low vaccination rates and willingness to receive HPV vaccines are worth considering. First, the health education provided by the government and schools is not sufficient in terms of both content and frequency, leading to a lack of in-depth understanding of the vaccine among the target population. Second, HPV vaccination is relatively expensive for most university students, which results in various affordability issues with the increasing demand for HIV vaccination.11-13,32 Students with better social and economic status (SES) have a higher chance of being vaccinated, and the accessibility of the HPV vaccine is reduced to a certain population in China. In addition, there is a need to consider the supply and accessibility issues of HPV vaccines since HPV vaccines are not yet available in many rural areas in China. 33 However, most of the burden of cervical cancer comes from low- and middle-income countries and populations with lower SES; hence, it is essential to provide HPV immunization among these vulnerable populations. 1
Traditional health education focuses on knowledge, believing that enhanced knowledge will lead to behavioral action. However, it is worth noting that the relationship between knowledge scores and HPV vaccination intention is controversial. While significant positive correlations were found in some previous studies, some others, including the current study, showed that knowledge concerning HPV infection, HPV-associated diseases, and vaccines was not a predictor of HPV vaccine acceptance.12,13,34,35 It is not rare to find people with a medical background who believe that they are at a low risk of HPV infection and are hence reluctant to get vaccinated. On the contrary, people tend to rely heavily on their own or experience and knowledge from those close to them to make health decisions. 36 When a person realizes the health benefits of the vaccine, even though she may have only heard of the HPV vaccine, she will actively search for information about the HPV vaccine and consult professionals about making an appointment for vaccination. This scenario suggests a possible way of guiding health interventions to improve HPV vaccination among female freshmen, and the benefit of receiving the HPV vaccination should be specially addressed, rather than focusing only on HPV-related knowledge.
In line with other studies, in this study, participants who believed they were at risk for HPV infection and had a higher perceived severity of developing cervical cancer were more likely to receive the HPV vaccine.12,30,31 However, the low percentage of premarital sex among freshman women leads to insufficient awareness of the risk of HPV infection among them and their families. The cognitive gap between the actual age group at the peak of HPV infection and the belief that there is no risk warrants considerable attention. 37 This misconception about HPV prevention may come from cultural beliefs about sexuality and result in widespread vaccine hesitancy and rejection among Chinese individuals.38,39 Therefore, comprehensive understanding of the actual risks and possible consequences of HPV infection will help increase the willingness of the target population to receive HPV vaccination. Furthermore, subjective norms were also a significant predictor of vaccine acceptance, as has been discussed in other similar studies.40,41 While the influence of self-made decisions was small in magnitude, it would lose significance when subjective norms were considered.40,41 University youngsters are in the process of forming their own thoughts and identity as well as developing a sense of direction in their life. Compared to their own decisions, they are sometimes more likely to comply with the social norms surrounding them. Moreover, young people are mostly in good health and usually ignore the role of disease prevention as a whole. In such circumstances, advice from family, friends, and their schools, together with their own positive attitude toward HPV vaccination, would be an effective way to promote HPV vaccination.
Similar to other studies, in this study, “perceived barriers” played a key negative role in young female students’ willingness for HPV vaccination.13,30,31 There were three main barriers that hindered vaccination. The first was the vaccine itself. Some participants refused to be vaccinated because of concerns about safety and effectiveness. The second was the vaccination process, such as the possibility that the needle might hurt and the occurrence of adverse reactions due to HPV vaccination. Furthermore, in terms of the realistic conditions necessary for vaccination, some were unwilling to be vaccinated because they could not make their own decisions or afford the relatively high price of the vaccination. In the meantime, positive associations have been found between self-efficacy and performance of health behaviors (eg, vaccination) through engagement and motivation, and this always resulted in persistence. 17 Although self-efficacy beliefs can be developed by creating positive experience of success, it needs professional guidance and skills. 42 Therefore, reducing the target population’s concerns about vaccine safety, possible needle injuries, and vaccination costs would be a cost-effective and practical way to promote HPV vaccination in Chinese youth. In addition, exploring the gap of willingness toward HPV vaccination and acceptance of the HPV vaccine and formulating targeted measures to remove this gap should be prioritized. 43 Recently, as the first Chinese domestic-made 2-valent HPV vaccine (Cecolin, Innovax, Xiamen, China) was approved by Chinese FDA, additional efforts should be taken to relieve hesitation regarding the vaccine and use the opportunity to expand vaccine supply and reduce vaccine prices.44,45 If feasible, HPV vaccines for young girls should be guaranteed initially, followed by a “catch-up” vaccination program for young women, and the government should finally integrate HPV vaccination into the national immunization program.
A number of studies around the world have explored the factors influencing HPV vaccination among female college students.12,13,27,30,31,34,35,40 However, it is important to understand the factors that affect or improve HPV vaccination rates among female college students in China as this population remains an important target group for HPV vaccination, especially after the vaccine is officially approved. Our research had some strengths. First, it was a multi-center study with a representative sample size. In addition, we used the IMB model to comprehensively analyze the factors influencing HPV vaccination, including personal background information, health-related awareness, and knowledge of HPV and HPV vaccines, to obtain persuasive results. Finally, the items in the IMB model were obtained from relevant high-quality research to ensure study quality.
This study examined women who had just entered college and were old enough to provide informed consent. Although the questionnaire survey was conducted in seven universities over the country and had certain representativeness, it was convenience sampling and the number of recruits might not be sufficient to cover heterogeneity in the target populations. In addition, most of the participants who volunteered to join the study may have been those who demonstrated greater interest in the HPV vaccination. Further, the proportion of students from urban areas and those with Han ethnicity was large. Hence, the study results might not be suitable to be generalized for all-age women or the whole “college female” population. Therefore, when applying the results and conclusions of this study, we should be careful in expanding representativeness. In addition, this was a cross-sectional survey based on self-reported information; hence, causality inference can hardly be drawn, and the possible overestimated influence of personal perceptions should be taken into consideration. In addition, 83 potential participants did not participate in the research, even after invitation and eligibility screening. Without the right to obtain the information of these non-respondents, it was difficult for us to understand whether the information provided by the respondents and non-respondents was balanced, and whether the research results can be inferred to the non-respondents. Furthermore, conclusions about the intention of HPV vaccination and associated factors should be interpreted with caution since these factors may have changed due to different research backgrounds. Finally, the study was conducted during a Public Health Emergency of International Concern, the COVID-19 pandemic. There might have been an increase in the perceived barriers reported by participants in the study due to the overlapping period, and hence, there is scope for further research concerning this issue. 46
Conclusion
This study was based on the IMB model with a large sample size to explore factors influencing female college students’ intention to receive the HPV vaccine since the vaccine became available in mainland China. Only a small proportion of the female freshmen had been vaccinated against HPV about three years after the HPV vaccines were approved in China, and the willingness of the vaccine among the unvaccinated remained low. Participants who had sex, had relatives or friends suffering from cancer, had heard of HPV, and actively consulted about HPV vaccines were more likely to receive the HPV vaccine in the next 6 months. Most importantly, our study found associations between vaccination acceptance and IMB constructs, such as perceived susceptibility, perceived severity, perceived barriers, subjective norms, and self-efficacy. The evaluation and strengthening of the positive attitude of female freshmen toward HPV vaccination, reducing barriers to vaccination, and creating vaccine-friendly social norms can be crucial for the promotion of HPV vaccination among college freshmen in mainland China.
Appendix A.
Table A1.
Items and distribution of perceptions based on the IMB model dimensions included in the questionnaire (N = 3765).
| IMB dimensions | Items | Willing to receive HPV vaccine (%) | Unwilling to receive HPV vaccine (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Strongly disagree | Disagree | Neither disagree nor agree | Agree | Strongly agree | Strongly disagree | Disagree | Neither disagree nor agree | Agree | Strongly agree | ||
| Perceived susceptibility | I believe i am at risk for getting HPV | 201(16.64) | 312(25.83) | 525(43.46) | 156(12.91) | 14(1.16) | 536(20.96) | 832(32.54) | 999(39.07) | 165(6.45) | 25(.98) |
| I believe i am at risk for developing cervical cancer | 180(14.90) | 296(24.50) | 553(45.78) | 166(13.74) | 13(1.08) | 475(18.58) | 773(30.23) | 1111(43.45) | 177(6.92) | 21(.82) | |
| Perceived severity | The thought of HPV infection scares me | 38(3.15) | 218(18.05) | 341(28.23) | 515(42.63) | 96(7.95) | 62(2.42) | 470(18.38) | 862(33.71) | 993(38.83) | 170(6.65) |
| HPV infection is a serious disease that can disturb my school life | 34(2.81) | 172(14.24) | 348(28.81) | 509(42.14) | 145(12.00) | 51(1.99) | 399(15.60) | 799(31.25) | 1039(40.63) | 269(10.52) | |
| Having cervical cancer would be devastating for me | 37(3.06) | 233(19.29) | 375(31.04) | 415(34.35) | 148(12.25) | 78(3.05) | 486(19.01) | 900(35.20) | 838(32.77) | 255(9.97) | |
| Having cervical cancer would have major consequences on my life | 18(1.49) | 81(6.71) | 240(19.87) | 650(53.81) | 219(18.13) | 35(1.37) | 159(6.22) | 617(24.13) | 1372(53.66) | 374(14.63) | |
| Perceived benefits | It is necessary to vaccinate against HPV even if you are in a committed relationship | 14(1.16) | 8(.66) | 250(20.70) | 642(53.15) | 294(24.34) | 28(1.10) | 39(1.53) | 788(30.82) | 1303(50.96) | 399(15.60) |
| Getting vaccinated for HPV will help protect me from HPV infection | 9(.75) | 27(2.24) | 166(13.74) | 668(55.30) | 338(27.98) | 19(.74) | 64(2.50) | 558(21.82) | 1485(58.08) | 431(16.86) | |
| If i get vaccinated for HPV, i can reduce my risk of cervical cancer | 4(.33) | 4(.33) | 126(10.43) | 758(62.75) | 316(26.16) | 9(.35) | 25(.98) | 508(19.87) | 1616(63.2) | 399(15.60) | |
| Perceived barriers | I doubt the safety and efficacy of the vaccine | 105(8.69) | 489(40.48) | 450(37.25) | 149(12.33) | 15(1.24) | 135(5.28) | 817(31.95) | 1150(44.97) | 402(15.72) | 53(2.07) |
| I have difficulty deciding HPV vaccination | 193(15.98) | 527(43.63) | 395(32.70) | 82(6.79) | 11(.91) | 147(5.75) | 702(27.45) | 1289(50.41) | 366(14.31) | 53(2.07) | |
| Possible needle hurts of HPV vaccination make me worry | 206(17.05) | 463(38.33) | 321(26.57) | 183(15.15) | 35(2.90) | 224(8.76) | 797(31.17) | 910(35.59) | 544(21.27) | 82(3.21) | |
| HPV vaccination is expensive | 58(4.80) | 190(15.73) | 534(44.21) | 326(26.99) | 100(8.28) | 52(2.03) | 195(7.63) | 1329(51.97) | 771(30.15) | 210(8.21) | |
| Possible side effects of HPV vaccination make me worry | 56(4.64) | 188(15.56) | 496(41.06) | 415(34.35) | 53(4.39) | 35(1.37) | 205(8.02) | 1097(42.9) | 1062(41.53) | 158(6.18) | |
| Social norms | Other girls like me are considering getting the HPV vaccine | 9(.75) | 45(3.73) | 593(49.09) | 447(37) | 114(9.44) | 41(1.60) | 216(8.45) | 1651(64.57) | 580(22.68) | 69(2.70) |
| My family thinks I should get vaccinated against HPV | 14(1.16) | 61(5.05) | 571(47.27) | 423(35.02) | 139(11.51) | 63(2.46) | 339(13.26) | 1710(66.88) | 391(15.29) | 54(2.11) | |
| In general, I want to do what my family members think I should do | 11(.91) | 106(8.77) | 447(37.00) | 564(46.69) | 80(6.62) | 26(1.02) | 279(10.91) | 1108(43.33) | 1090(42.63) | 54(2.11) | |
| My friends thinks I should get vaccinated against HPV | 15(1.24) | 78(6.46) | 704(58.28) | 351(29.06) | 60(4.97) | 78(3.05) | 421(16.46) | 1710(66.88) | 314(12.28) | 34(1.33) | |
| In general, I want to do what my FF thinks I should do | 28(2.32) | 228(18.87) | 675(55.88) | 243(20.12) | 34(2.81) | 71(2.78) | 661(25.85) | 1497(58.55) | 306(11.97) | 22(.86) | |
| Decision-making | I strongly value my health | 1(.08) | 3(.25) | 65(5.38) | 629(52.07) | 510(42.22) | 4(.16) | 9(.35) | 183(7.16) | 1534(59.99) | 827(32.34) |
| Prevention of disease and infections is important to me | 1(.08) | 0(.00) | 55(4.55) | 651(53.89) | 501(41.47) | 3(.12) | 4(.16) | 198(7.74) | 1602(62.65) | 750(29.33) | |
| Self-efficacy | I feel confident in my ability to get vaccinated for HPV, even if it is expensive | 5(.41) | 33(2.73) | 379(31.37) | 532(44.04) | 259(21.44) | 33(1.29) | 187(7.31) | 1488(58.19) | 675(26.40) | 174(6.80) |
| I feel confident in my ability to get vaccinated for HPV, even if getting the shot hurts a little | 3(.25) | 4(.33) | 195(16.14) | 704(58.28) | 302(25.00) | 17(.66) | 82(3.21) | 997(38.99) | 1215(47.52) | 246(9.62) | |
| I feel confident in my ability to get vaccinated for HPV, even if you are worried about the possible side effects | 3(.25) | 26(2.15) | 387(32.04) | 590(48.84) | 202(16.72) | 30(1.17) | 200(7.82) | 1482(57.96) | 725(28.35) | 120(4.69) | |
| I feel confident in my ability to get vaccinated for HPV, even if it means finding the time to go to the doctor three times | 3(.25) | 7(.58) | 279(23.10) | 674(55.79) | 245(20.28) | 24(.94) | 128(5.01) | 1294(50.61) | 937(36.64) | 174(6.80) | |
| I can talk to my parents/guardians/nurses/doctors about whether to get HPV vaccine at will | 10(.83) | 48(3.97) | 354(29.30) | 552(45.7) | 244(20.20) | 26(1.02) | 270(10.56) | 1174(45.91) | 927(36.25) | 160(6.26) | |
| I know the location of vaccination, or I will find out the location through online search or telephone consultation | 15(1.24) | 144(11.92) | 447(37.00) | 455(37.67) | 147(12.17) | 51(1.99) | 550(21.51) | 1202(47.01) | 663(25.93) | 91(3.56) | |
| I know that the HPV vaccine is a self-funded vaccine and the price is affordable | 11(.91) | 105(8.69) | 494(40.89) | 461(38.16) | 137(11.34) | 63(2.46) | 441(17.25) | 1471(57.53) | 514(20.1) | 68(2.66) | |
| If I want to vaccinate, I will set a reminder calendar and so on to complete 3 shots regularly | 1(.08) | 4(.33) | 213(17.63) | 725(60.02) | 265(21.94) | 14(.55) | 84(3.29) | 839(32.81) | 1361(53.23) | 259(10.13) | |
Abbreviations: HPV, human papillomavirus; IMB, information–motivation–behavior skills.
Footnotes
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval; COVID-19, coronavirus disease 2019; HPV, human papillomavirus; IMB, information–motivation–behavior skills; OR, odds ratio; P, probability; SD, standard deviation; SES, socioeconomic status; WHO, World Health Organization.
Author Contributions: Mingyu Si and Xiaoyou Su prepared the first draft. Yu Jiang, Xiaoyou Su, and Ming-Yu Si managed the overall project. Xi Zhang, Wenjun Wang, Xiaofen Gu, Li Ma, Jing Li, Shaokai Zhang, and Zefang Ren were responsible for the questionnaire survey in seven geographical regions of China. Yu Jiang and Yuanli Liu finalized the manuscript on the basis of comments from other authors. Youlin Qiao provided overall guidance.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Asian Regional Special Cooperation Fund of National Health Commission of the People’s Republic of China (BLXM01) and Innovation Fund for Medical Sciences sponsored by Chinese Academy of Medical Sciences (2019-I2M-2-005, 2017-I2M-B&R-17).
Ethical Approval and Consent to Participate: This study has been approved by the Institutional Review Board of Chinese Center for Disease Control and Prevention on October 24, 2019 (approval number: 201918-01).
Availability of Data and Materials: The original data generated from this study and the analyzed results will be available from the corresponding author upon reasonable request.
ORCID iDs
Mingyu Si https://orcid.org/0000-0002-8372-9301
References
- 1.Arbyn M, Weiderpass E, Bruni L, et al. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Glob Health. 2020;8(2):e191-e203. doi: 10.1016/S2214-109X(19)30482-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Walboomers JMM, Jacobs MV, Manos MM, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189(1):12-19. doi: [DOI] [PubMed] [Google Scholar]
- 3.Schiffman MH, Bauer HM, Hoover RN, et al. Epidemiologic evidence showing that human papillomavirus infection causes most cervical intraepithelial neoplasia. J Natl Cancer Inst. 1993;85(12):958-964. doi: 10.1093/jnci/85.12.958 [DOI] [PubMed] [Google Scholar]
- 4.Clifford G, Franceschi S, Diaz M, Muñoz N, Villa LL. HPV type-distribution in women with and without cervical neoplastic diseases. Vaccine. 2006;24(suppl 3):S26-S34. doi: 10.1016/j.vaccine.2006.05.026 [DOI] [PubMed] [Google Scholar]
- 5.Sotlar K, Stubner A, Diemer D, et al. Detection of high-risk human papillomavirus E6 and E7 oncogene transcripts in cervical scrapes by nested RT-polymerase chain reaction. J Med Virol. 2004;74(1):107-116. doi: 10.1002/jmv.20153 [DOI] [PubMed] [Google Scholar]
- 6.Villa LL, Costa RL, Petta CA, et al. Prophylactic quadrivalent human papillomavirus (types 6, 11, 16, and 18) L1 virus-like particle vaccine in young women: a randomised double-blind placebo-controlled multicentre phase II efficacy trial. Lancet Oncol. 2005;6(5):271-278. doi: 10.1016/S1470-2045(05)70101-7 [DOI] [PubMed] [Google Scholar]
- 7.Harper DM, Franco EL, Wheeler C, et al. Efficacy of a bivalent L1 virus-like particle vaccine in prevention of infection with human papillomavirus types 16 and 18 in young women: a randomised controlled trial. Lancet. 2004;364(9447):1757-1765. doi: 10.1016/S0140-6736(04)17398-4 [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization . Immunization, vaccines and biologicals-data, statistics and graphics, 2020. https://www.who.int/teams/immunization-vaccines-and-biologicals/data-statistics-and-graphics
- 9.Markowitz LE, Dunne EF, Saraiya M, et al. Quadrivalent human papillomavirus vaccine: recommendations of the Advisory Committee on Immunization practices (ACIP). MMWR Recomm Rep. 2007;56(RR-2):1-24. [PubMed] [Google Scholar]
- 10.World Health Organization . Human papillomavirus (HPV) position paper. https://www.who.int/immunization/policy/position_papers/hpv/en/
- 11.Deng C, Chen X, Liu Y. Human papillomavirus vaccination: coverage rate, knowledge, acceptance, and associated factors in college students in mainland China. Hum Vaccines Immunother. 2021;17(3):828-835. doi: 10.1080/21645515.2020.1797368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu Y, Di N, Tao X. Knowledge, practice and attitude towards HPV vaccination among college students in Beijing, China. Hum Vaccines Immunother. 2020;16(1):116-123. doi: 10.1080/21645515.2019.1638727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.You D, Han L, Li L, et al. Human papillomavirus (HPV) vaccine uptake and the willingness to receive the HPV vaccination among female college students in China: a multicenter study. Vaccines. 2020;8(1):31. doi: 10.3390/vaccines8010031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang X, Wang Z, Ren Z, et al. HPV vaccine acceptability and willingness-related factors among Chinese adolescents: a nation-wide study. Hum Vaccines Immunother. 2020;17:1025-1032. doi: 10.1080/21645515.2020.1812314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang Y, Wang Y, Liu L, et al. Awareness and knowledge about human papillomavirus vaccination and its acceptance in China: a meta-analysis of 58 observational studies. BMC Publ Health. 2016;16:216. doi: 10.1186/s12889-016-2873-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull 1992;111:455-474. [DOI] [PubMed] [Google Scholar]
- 17.Fisher WA. Understanding human papillomavirus vaccine uptake. Vaccine. 2012;30(suppl 5):F149-F156. doi: 10.1016/j.vaccine.2012.04.107 [DOI] [PubMed] [Google Scholar]
- 18.Perez G, Cruess DG, Strauss N. A brief information-motivation-behavioral skills intervention to promote human papillomavirus vaccination among college-aged women. Psychol Res Behav Manag. 2016;9:285-296. doi: 10.2147/PRBM.S112504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Si M, Su X, Jiang Y, Qiao Y, Liu Y. Interventions to improve human papillomavirus vaccination among Chinese female college students: study protocol for a randomized controlled trial. BMC Publ Health. 2019;19(1):1546. doi: 10.1186/s12889-019-7903-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang R, Guo XL, Wisman GBA, et al. Nationwide prevalence of human papillomavirus infection and viral genotype distribution in 37 cities in China. BMC Infect Dis. 2015;15:257. doi: 10.1186/s12879-015-0998-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhou HL, Zhang W, Zhang CJ, et al. Prevalence and distribution of human papillomavirus genotypes in Chinese women between 1991 and 2016: a systematic review. J Infect. 2018;76(6):522-528. doi: 10.1016/j.jinf.2018.02.008 [DOI] [PubMed] [Google Scholar]
- 22.Zhao FH, Tiggelaar SM, Hu SY, et al. A multi-center survey of age of sexual debut and sexual behavior in Chinese women: suggestions for optimal age of human papillomavirus vaccination in China. Cancer Epidemiology. 2012;36(4):384-390. doi: 10.1016/j.canep.2012.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.World Health Organization . Accelerate cervical cancer elimination initiative. https://www.who.int/reproductivehealth/publications/update-screening-treatment-cervical-cancer/en/
- 24.Chen PU, Chun-rong LIU, Zhang X, Jing LI. Knowledge and attitudes toward HPV and its vaccines among parents of middle school students in Chengdu. Mod Prev Med. 2018;45(02):299-302. [Google Scholar]
- 25.Kim HW. Knowledge about human papillomavirus (HPV), and health beliefs and intention to recommend HPV vaccination for girls and boys among Korean health teachers. Vaccine. 2012;30(36):5327-5334. doi: 10.1016/j.vaccine.2012.06.040 [DOI] [PubMed] [Google Scholar]
- 26.Kahn JA, Rosenthal SL, Hamann T, Bernstein DI. Attitudes about human papillomavirus vaccine in young women. Int J STD & AIDS. 2003;14(5):300-306. doi: 10.1258/095646203321605486 [DOI] [PubMed] [Google Scholar]
- 27.Yun-xia C, Wu Ds, Shi-qun C, et al. Investigation on college students’ knowledge of human papilloma virus and HPV vaccine. Chinese J School Doctor. 2018;32(06):401-404. [Google Scholar]
- 28.Forster AS, McBride KA, Davies C, et al. Development and validation of measures to evaluate adolescents’ knowledge about human papillomavirus (HPV), involvement in HPV vaccine decision-making, self-efficacy to receive the vaccine and fear and anxiety. Publ Health. 2017;147:77-83. doi: 10.1016/j.puhe.2017.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DiClemente RJ, Murray CC, Graham T, Still J. Overcoming barriers to HPV vaccination: a randomized clinical trial of a culturally-tailored, media intervention among African American girls. Hum Vaccines Immunother. 2015;11(12):2883-2894. doi: 10.1080/21645515.2015.1070996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gerend MA, Shepherd JE. Predicting human papillomavirus vaccine uptake in young adult women: comparing the health belief model and theory of planned behavior. Ann Behav Med. 2012;44(2):171-180. doi: 10.1007/s12160-012-9366-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guvenc G, Seven M, Akyuz A. Health belief model scale for human papilloma virus and its vaccination: adaptation and psychometric testing. J Pediatr Adolesc Gynecol. 2016;29(3):252-258. doi: 10.1016/j.jpag.2015.09.007 [DOI] [PubMed] [Google Scholar]
- 32.Yin Y. HPV vaccination in China needs to be more cost-effective. Lancet. 2017;390(10104):1735-1736. doi: 10.1016/S0140-6736(17)32606-5 [DOI] [PubMed] [Google Scholar]
- 33.Wong LP, Han L, Li H, Zhao J, Zhao Q, Zimet GD. Current issues facing the introduction of human papillomavirus vaccine in China and future prospects. Hum Vaccines Immunother. 2019;15(7-8):1533-1540. doi: 10.1080/21645515.2019.1611157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Oz M, Cetinkaya N, Apaydin A, et al. Awareness and knowledge levels of Turkish College students about human papilloma virus infection and vaccine acceptance. J Canc Educ. 2018;33(2):260-268. doi: 10.1007/s13187-016-1116-0 [DOI] [PubMed] [Google Scholar]
- 35.LaJoie AS, Kerr JC, Clover RD, Harper DM. Influencers and preference predictors of HPV vaccine uptake among US male and female young adult college students. Papillomavirus Res. 2018;5:114-121. doi: 10.1016/j.pvr.2018.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bojar H, Silveira F, Rebelo M, Elżbieta C, Krzysztof C. Health behaviours in Scaffold use risk assessment model–SURAM. Ann Agric Environ Med. 2019;26(1):138-142. doi: 10.26444/aaem/100534 [DOI] [PubMed] [Google Scholar]
- 37.Wang J, Tang D, Wang K, et al. HPV genotype prevalence and distribution during 2009-2018 in Xinjiang, China: baseline surveys prior to mass HPV vaccination. BMC Wom Health. 2019;19(1):90. doi: 10.1186/s12905-019-0785-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li L, Ding YY, Ding YY, et al. Normative beliefs and sexual risk in China. AIDS Behav. 2011;15(6):1251-1258. doi: 10.1007/s10461-010-9835-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang X, Zhou X, Leesa L, Mantwill S. The effect of vaccine literacy on parental trust and intention to vaccinate after a major vaccine scandal. J Health Commun. 2018;23(5):413-421. doi: 10.1080/10810730.2018.1455771 [DOI] [PubMed] [Google Scholar]
- 40.Li L, Li J. Factors affecting young Chinese women’s intentions to uptake human papillomavirus vaccination: an extension of the theory of planned behavior model. Hum Vaccines Immunother. 2020;16:3123-3130. doi: 10.1080/21645515.2020.1779518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cheung T, Lau JTF, Wang JZ, Mo PKH, Ho YS. Acceptability of HPV vaccines and associations with perceptions related to HPV and HPV vaccines among male baccalaureate students in Hong Kong. PloS One. 2018;13(6):e0198615. doi: 10.1371/journal.pone.0198615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jinks AM, Lawson V, Daniels R. A survey of the health needs of hospital staff: implications for health care managers. J Nurs Manag. 2003;11(5):343-350. doi: 10.1046/j.1365-2834.2003.00387.x [DOI] [PubMed] [Google Scholar]
- 43.Thanasas I, Lavranos G, Gkogkou P, Paraskevis D. Understanding of young adolescents about HPV infection: how health education can improve vaccination rate. J Canc Educ. 2020;35(5):850-859. doi: 10.1007/s13187-019-01681-5 [DOI] [PubMed] [Google Scholar]
- 44.Wang Q, Zhang W, Cai H, Cao Y. Understanding the perceptions of Chinese women of the commercially available domestic and imported HPV vaccine: a semantic network analysis. Vaccine. 2020;38(52):8334-8342. doi: 10.1016/j.vaccine.2020.11.016 [DOI] [PubMed] [Google Scholar]
- 45.Zou Z, Fairley CK, Ong JJ, et al. Domestic HPV vaccine price and economic returns for cervical cancer prevention in China: a cost-effectiveness analysis. Lancet Glob Health. 2020;8(10):e1335-e1344. doi: 10.1016/S2214-109X(20)30277-1 [DOI] [PubMed] [Google Scholar]
- 46.Ogundele OA, Omotoso AA, Fagbemi AT. COVID-19 outbreak: a potential threat to routine vaccination programme activities in Nigeria. Hum Vaccines Immunother. 2020;17:661-663. doi: 10.1080/21645515.2020.1815490 [DOI] [PMC free article] [PubMed] [Google Scholar]