Abstract
The role of resilience in mediating the negative effects of the COVID-19 pandemic on the mental health of US women is poorly understood. We examined socioeconomic factors associated with low resilience in women, the relationship of low resilience with psychiatric morbidity, and the mediating role of resilience in the relationship between pandemic-related stress and other coincident psychiatric morbidities. Using a quota-based sample from a national panel, we conducted a web-based survey of 3200 US women in April 2020. Weighted, multivariate logistic regression was used to model the odds of pandemic-related stress, and coincident depression and anxiety symptoms among those with and without low resilience. Structural equation modeling was used to evaluate resilience as a mediator of the relationship between pandemic-related stress and other coincident psychiatric morbidities. Risk factors for low resilience included younger age, lower household income, lower education, unemployment, East/Southeast Asian race, unmarried/unpartnered status, and higher number of medical comorbidities. Low resilience was significantly associated with greater odds of depression symptoms (OR = 3.78, 95% CI [3.10–4.60]), anxiety symptoms (OR = 4.17, 95% CI [3.40–5.11]), and pandemic-related stress (OR = 2.86, 95% CI [2.26–3.26]). Resilience acted as a partial mediator in the association between pandemic-related stress and anxiety symptoms (proportion mediated = 0.23) and depression symptoms (proportion mediated = 0.28). In the early days of the COVID-19 pandemic, low resilience mediated the association between pandemic-related stress and psychiatric morbidity. Strategies proven to enhance resilience, such as cognitive behavioral therapy, mindfulness-based stress reduction, and addressing socioeconomic factors, may help mitigate mental health outcomes.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00737-021-01184-7.
Keywords: COVID-19, Mental health, Anxiety disorders, Depression, Women’s health
Introduction
Widespread crises cause incident and cumulative mental health effects (North 2014). Compared to pre-pandemic levels, early studies from the current COVID-19 pandemic indicate significantly elevated rates of stress, anxiety, and depression (Lee et al., 2020; Lindau et al., 2021; Twenge & Joiner 2020; Wang et al., 2020a). Women may be especially vulnerable to pandemic-related psychopathology because of their higher baseline anxiety and depression (Hasin et al., 2018; Kessler et al., 2005). Also, certain socioeconomic factors were likely to increase the vulnerability of women to stress during the COVID-19 pandemic. More women are employed in essential worker roles, they have greater responsibility for child-rearing and family caregiving, and they experience gender-based disparities in wages. In addition, interpersonal violence intensified during the pandemic (Lee et al., 2020; Sediri et al., 2020). Depression and anxiety cause significant individual suffering with potentially deleterious effects on the family (Ahun et al., 2018). Our current, over-burdened mental health system is ill-equipped to address increased psychiatric morbidity (Racine et al., 2020). Consequently, it is critical to identify vulnerable populations and implement ways to buffer against stress in times of global crisis.
Psychological resilience is the ability to resist illness, adapt positively, and return to a pre-morbid level of functioning in the face of ongoing stress (Dooley et al., 2017; Kalisch et al., 2017; Smith et al., 2010). The importance of resilience lies in its action as a buffer against stress and as a mediator between stress and mental health morbidity (Barzilay et al., 2020; Chen et al., 2020). Resilience has been shown to mediate between stress and mental health morbidity in the aftermath of disasters such as hurricanes and earthquakes (Xi et al., 2020). In their survey of resilience in 3042 general adult participants in the USA and Israel during the COVID-19 pandemic, Barzilay and colleagues looked at the anxiety and depression scores of 1350 participants, 74% of which were female (2020). This study showed that a one standard deviation increase in resilience was associated with 65% and 69% less in indices of anxiety and depression, respectively (Barzilay et al., 2020). However, they did not stratify their data by gender or account for the socioeconomic factors often associated with low resilience, and less than half of the participants provided data about mental health, which limited the interpretation of the study (Barzilay et al., 2020). Several studies have demonstrated that, in times of disaster, addressing modifiable socioeconomic factors, such as social isolation and poverty, can enhance resilience (Mayer 2019; Vinkers et al. 2020).
A prior study has shown that women who experienced domestic violence had lower levels of resilience when compared with others (Tsirigotis and Łuczak 2018). The study described here analyzes cross-sectional data from the National Women’s Health COVID-19 Study. In the seminal study, Lindau and colleagues found that women who reported a new or worsening health-related socioeconomic risk (HRSR), such as housing instability or interpersonal violence, during the early phase of the pandemic had two to threefold higher adjusted odds of anxiety, depression, and traumatic stress (2021). Among those without pre-pandemic HRSRs, incident interpersonal violence (a broader construct that may include domestic violence) was associated with higher rates of depression and traumatic stress (Lindau et al., 2021).
To understand if resilience mediates the effect of the pandemic on psychiatric comorbidities, we hypothesized that, in the early days of the COVID-19 pandemic: (1) low resilience in women is associated with socioeconomic factors; (2) low resilience is positively associated with pandemic concern, traumatic stress, depression symptoms, and anxiety symptoms; and (3) resilience mediates the association between pandemic-related stress, depression symptoms, and anxiety symptoms. Our findings help us to ascertain how US women are adapting to the stress of COVID-19 and the role of environmental and structural factors in this adaptation. They also highlight ways in which resilience may be helpful in promoting coping.
Materials and methods
The National Women’s Health COVID-19 Study was conducted online between April 10, and 24, 2020, and has previously been described (Lindau et al., 2021). At the time of the study, there was more uncertainty about safety, how the virus was spread, and the implications of the virus for work and finances. Concurrently, widespread quarantining was instituted and schools closed, forcing families to immediately adopt remote work and learning. At this critical time, potential participants for the National Women’s Health COVID-19 Study aged 18 and older were identified from a research panel maintained by the survey research firm, Opinions 4 Good (Op4G). Op4G maintains a diverse panel of 350,000 English-speaking residents in the USA and has been used in prior academic health studies (Baudry 2019; Forrest et al., 2014; Gruber-Baldini et al., 2017). To facilitate targeted recruitment, Op4G collects prospective data on panelists’ sociodemographic information and health conditions.
A nested quota sampling strategy was used to generate a sample demographically representative based on the education and age of women aged 18 and older in the 2018 US population (U.S. Census Bureau 2018). East/Southeast Asian women (Chinese, Filipino, Japanese, Korean, and Vietnamese) were intentionally over-sampled to generate more precise estimates for this racial group, which has been a target for COVID-related harassment and violence (Jeung and Nham 2020).
A personalized, one-time survey link was emailed to potential participants. Informed consent was documented digitally and participants received a small incentive for completing the self-administered, web-based survey. In total, 3200 out of 3634 eligible women contacted completed the survey, yielding an 88% cooperation rate (AAPR 2016). Post hoc power calculations for this study indicated that 3200 women would provide sufficiently precise estimates of low resilience (i.e., the half-width of the 95% confidence interval would be no larger than ± 2%). The protocol was approved by the University of Chicago Institutional Review Board.
Study design and measures
Resilience was measured using the Brief Resilience Scale (BRS), which averages responses from six items (scored 1–5) and is designed to assess the ability to bounce back from stress (Smith et al., 2008). Higher BRS scores represent higher resilience and BRS ≤ 3 is defined as low resilience (Smith et al., 2010; Smith et al., 2008). The BRS was chosen for brevity, excellent psychometric properties, development for use in adults, and the focus on resilience as an ability or skill (Windle et al., 2011). Psychiatric comorbidities were defined as anxiety symptoms, depression symptoms, traumatic stress, and loneliness. Validated measures of anxiety (Generalized Anxiety Disorder-7) and depression (Patient Health Questionnaire-2) were used (Kroenke et al., 2003; Spitzer et al., 2006). We used a two-item form for traumatic stress: (1) feeling very upset by pandemic reminders and (2) disturbing thoughts. These items represent the two symptoms from the Modified Posttraumatic Stress Disorder Checklist that were most commonly endorsed by US adults surveyed after the 9/11 terrorist attacks (Schuster et al., 2001). A response of “quite a bit” or “extremely” to either or both of the two questions from the modified PTSD checklist was considered a positive for the presence of traumatic stress. Participants were asked to self-rate feelings of loneliness, including the frequency (hardly ever, some of the time, often); lonely was defined as responses of some of the time or often. The questions about loneliness were adapted from the English Longitudinal Study of Aging (ELSA) (Shankar et al., 2011). Interpersonal violence was measured by the Centers for Medicare & Medicaid Services Accountable Health Communities (AHC) screening tool (Anon n.d.). Respondents were asked to identify health-related comorbidities; a measure of medical comorbidities was adapted from the Modified Charlson Comorbidity Index (Chaudhry et al., 2005). Sleep was evaluated using 2 novel questions measuring sleep duration and incident change. Participants were also asked to self-rate their mental health (excellent, very good, good, fair, poor) and pandemic concern (very, somewhat, not very, not at all). Item non-response was low; the mean missing response rate was 0.4% (range 0–2.5%).
Statistical analysis
Factors associated with low resilience were examined using univariable and multivariable logistic regression. Multivariable logistic regression models were fitted to determine how low resilience correlates with mental health measures, with adjusted odds ratios (aORs) and 95% confidence intervals (C.I.s) calculated. For further assessment of whether increasing resilience was associated with mental health (i.e., a “dose effect”), quartiles of the BRS were included in the models instead of low resilience (versus not).
To determine the degree to which resilience mediated the relationship between pandemic-related stress and coincident depression and anxiety symptoms, two mediation analyses were performed (Xi et al., 2020; Zhang et al., 2018). To examine the degree to which resilience mediated the relationship between pandemic-specific stress symptoms (loneliness and concern about the pandemic) and depression and anxiety symptoms, further mediation analyses were performed. Structural equation models (SEMs) were fit, and the mediated association was calculated using the product method. Bias-corrected bootstrapped 95% C.I.s for the mediated association were constructed using 1000 bootstrapped samples. Partial mediation would be evident if both the mediated and direct associations (i.e., the association between traumatic stress and anxiety/depression not accounted for by resilience) were statistically significant. The proportion mediated, defined as mediated effect/total effect, was also calculated.
Covariates used in multivariable and mediation analyses included race/ethnicity, age, education, income, marital status, children in the household, comorbidities, and employment status. These covariates were chosen based on the univariable analysis results from this study and on known factors associated with resilience and mental health.
Survey weights were applied so that marginal distributions for age group, race, education, income category, and geographic region matched 2018 population estimates. Statistical significance was defined as p < 0.05. Analyses were performed using Stata 16 (StataCorp LLC, College Station, TX).
Results
Sample characteristics
The mean (S.D.) age was 47.7(17.0) years. Most women were non-Hispanic white (65.3%) and educated, with 62.8% reporting post-high school education. More than 60% were married or partnered. More than a third lived with at least one child in the household (38.9%). More than half of respondents reported annual household income greater than fifty thousand dollars (Table 1).
Table 1.
Sociodemographic characteristics and factors associated with low resilience
| Overall distribution (%) | % with low resilience based on Brief Resilience Scale | P-value from univariable logistic regression | Adjusted ORa (95% CI) |
|
|---|---|---|---|---|
| Age group (years) | < 0.001 | |||
| 18–44 | 44.6 | 49.9 | Reference | |
| 45–64 | 33.0 | 35.8 | 0.53 (0.43–0.65)*** | |
| 65 + | 22.4 | 25.3 | 0.27 (0.20–0.37)*** | |
| Race/ethnicity | 0.005 | |||
| Non-Hispanic white | 65.3 | 38.1 | Reference | |
| Non-Hispanic black | 10.6 | 37.6 | 0.85 (0.66–1.11) | |
| East/Southeast Asian | 5.2 | 48.5 | 1.81 (1.33–2.47)*** | |
| Hispanic | 13.8 | 45.9 | 1.15 (0.88–1.49) | |
| Other | 5.0 | 39.3 | 0.94 (0.55–1.60) | |
| Marital status | < 0.001 | |||
| Married/partnered | 62.0 | 36.2 | 0.77 (0.64–0.93)** | |
| Other | 38.0 | 45.4 | Reference | |
| Children in household (HH) | < 0.001 | |||
| No children in HH | 61.1 | 35.6 | Reference | |
| 1 or more children in HH | 38.9 | 46.0 | 1.20 (0.98–1.48) | |
| Education (highest grade completed) | < 0.001 | |||
| Never attended or only attended kindergarten | 0.4 | 80.9 | 4.18 (0.58–30.02) | |
| Elementary | 0.7 | 64.2 | 2.68 (1.02–7.00)* | |
| Some high school (HS) | 4.1 | 55.0 | 1.07 (0.69–1.65) | |
| HS graduate | 32.0 | 44.8 | Reference | |
| Some college | 28.2 | 38.2 | 0.81 (0.65–1.01) | |
| College graduate | 34.6 | 33.5 | 0.78 (0.61–0.99)* | |
| Employment | 0.02 | |||
| Employed | 47.1 | 37.1 | Reference | |
| Not employed | 52.9 | 41.9 | 1.37 (1.13–1.67)** | |
| Household income in 2019 | < 0.001 | |||
| < $25 K | 19.6 | 52.9 | Reference | |
| $25–50 K | 21.3 | 41.5 | 0.79 (0.63–0.98)* | |
| $50–100 K | 30.0 | 37.0 | 0.69 (0.55–0.88)** | |
| > $100 K | 29.1 | 32.4 | 0.59 (0.43–0.80)** | |
| # of comorbidities | 0.01 | |||
| 0 | 53.7 | 37.2 | Reference | |
| 1 | 29.4 | 42.5 | 1.47 (1.20–1.80)*** | |
| 2 | 10.4 | 39.2 | 1.42 (1.05–1.93)* | |
| 3 + | 6.6 | 49.0 | 2.13 (1.46–3.10)*** |
aFrom a single multivariable logistic regression model with low resilience as the dependent variable. *: p < 0.05, **: p < 0.01, ***: p < 0.001 for comparison to reference group
OR odds ratio, CI confidence interval
Associations between low resilience and sociodemographic characteristics
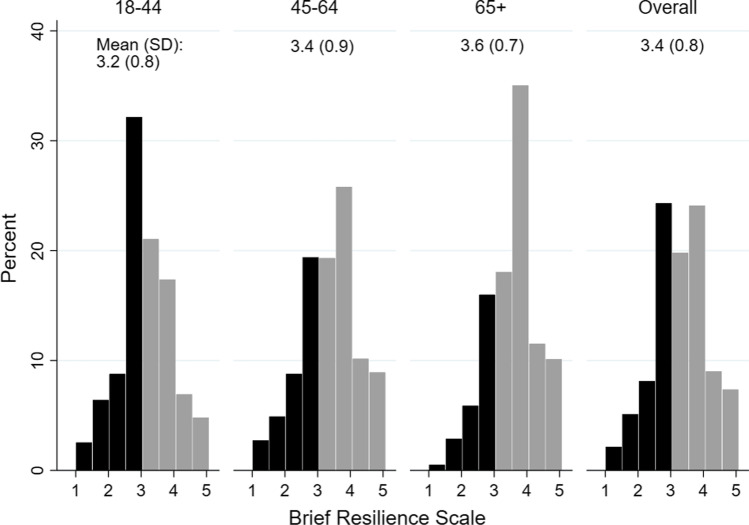
The composite score of the six questions on the brief resilience scale (Supplementary Table 1) showed that the majority (60%) of the population was resilient (Mean (S.D.): 3.4 (0.8)) (Fig. 1). Younger women were, on average, less resilient (18–44 years; Mean (S.D.): 3.2 (0.8)) than older women (45–64: 3.4 (0.9); 65 + : 3.6 (0.7)) (Fig. 1). These differences translated to significant differences (overall p < 0.001) in the proportion of women with low resilience between age groups (49.9% 18–44 years, 35.8% 45–64 years, 25.3% 65 + years; Table 1). Lower income was associated with higher rates of low resilience scores (52.9% < 25 K, 41.5% 25–50 K, 37% 50–100 K, 32.4% > 100 K; overall p < 0.001). Lower education was associated with low resilience (overall p < 0.001). Unmarried and unpartnered women reported low resilience, with 45.4% of single women reporting low resilience compared with 36.2% of partnered women (p < 0.001). Women who identified as East/Southeast Asian demonstrated low resilience compared to non-Hispanic whites, with 48% of East/Southeast Asian women reporting low resilience. Women with greater number of reported health comorbidities were more likely to have low resilience (37.2% 0 comorbidities, 42.5% 1 comorbidity, 39.2% 2 comorbidities, 49.0% ≥ 3 comorbidities, overall p = 0.01). These associations remained significant in adjusted analyses (Table 1).
Fig. 1.
Distribution of the Brief Resilience Scale scores stratified by age group and overall. Black bars indicate low resilience
Associations between low resilience and traumatic stress, depression symptoms, and anxiety symptoms
Women who scored in the lowest quartile for resilience reported higher levels of depression symptoms and traumatic stress when compared with women scoring in the highest quartile. This finding suggests a “dose effect” association between resilience and mental health, with increasing resilience associated with decreasing odds of mental health conditions and vice versa (Table 2).
Table 2.
Impact of resilience (“dose effect”) on mental health conditions
| Adjusted odds ratioa (95% CI) |
|||
|---|---|---|---|
| 2nd Q vs. 1st Q | 3rd Q vs. 1st Q | 4th Q vs. 1st Q | |
| Fair/poor self-rated mental health |
0.32 (0.25–0.43) |
0.15 (0.11–0.21) |
0.06 (0.03–0.11) |
| Anxiety |
0.39 (0.30–0.49) |
0.13 (0.10–0.17) |
0.08 (0.05–0.12) |
| Depression |
0.39 (0.31–0.50) |
0.16 (0.13–0.21) |
0.07 (0.05–0.11) |
| Traumatic stress |
0.59 (0.45–0.77) |
0.26 (0.19–0.35) |
0.20 (0.13–0.31) |
| Loneliness |
0.66 (0.49–0.88) |
0.35 (0.27–0.46) |
0.16 (0.12–0.22) |
| Very concerned about pandemic |
0.72 (0.57–0.91) |
0.46 (0.37–0.59) |
0.44 (0.33–0.58) |
| Two or more mental health conditions |
0.37 (0.28–0.50) |
0.17 (0.13–0.22) |
0.08 (0.06–0.12) |
aFrom seven separate logistic regression models adjusted for age (continuous, range 18–90), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, East/Southeast Asian, other), education (continuous, range 1–6), income (< 25 K, 25–50 K, 50–100 K, > 100 K), married/partnered status, number of children in household (none, 1 +), employment status, and number of comorbidities (continuous, range 0–7)
CI confidence interval, Q quartiles of resilience score
Based on multivariable models, women with low resilience had significantly greater odds of self-rated fair or poor mental health (aOR, 95% CI: 4.58 (3.59–5.86)), anxiety (aOR, 95% CI: 4.17 (3.40–5.11)), depression (aOR, 95% CI: 3.78 (3.10–4.60)), traumatic stress (aOR, 95% CI: 2.86 (2.26–3.62)), loneliness (aOR, 95% CI: 2.51 (2.04–3.10)), and being very concerned about the pandemic (aOR, 95% CI: 1.68 (1.40–2.02)) (Table 3). In sensitivity analyses, although women who had worsening of interpersonal violence since the start of the pandemic had higher rates of low resilience compared to other women (60% vs. 37%, p < 0.001), inclusion of this factor into the multivariable models had limited impact on the associations between low resilience and mental health measures. There was a less than 5% change in the odds ratios in all cases (data not shown).
Table 3.
Impact of low resilience on mental health conditions
| Adjusted odds ratioa (95% CI) |
P-value | |
|---|---|---|
| Fair/poor self–rated mental health |
4.58 (3.59–5.86) |
< 0.001 |
| Anxiety |
4.17 (3.40–5.11) |
< 0.001 |
| Depression |
3.78 (3.10–4.60) |
< 0.001 |
| Traumatic stress |
2.86 (2.26–3.62) |
< 0.001 |
| Loneliness |
2.51 (2.04–3.10) |
< 0.001 |
| Very concerned about pandemic |
1.68 (1.40–2.02) |
< 0.001 |
| Two or more mental health conditions |
3.84 (3.14–4.69) |
< 0.001 |
aFrom seven separate logistic regression models with the mental health condition as the dependent variable, adjusted for age (continuous, range 18–90), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, East/Southeast Asian, other), education (continuous, range 1–6), income (< 25 K, 25–50 K, 50–100 K, > 100 K), married/partnered status, number of children in household (none, 1 +), employment status, and number of comorbidities (continuous, range 0–7)
CI confidence interval
The mediating role of resilience in the relationship between pandemic-related stress and coincident depression and anxiety symptoms
The results indicate that resilience partially mediated the association between pandemic-related stress and anxiety and depression symptoms. Specifically, the indirect association (or mediated association) was significant for anxiety (proportion mediated = 0.23), and depression (proportion mediated = 0.28) (Table 4). Resilience also partially mediated the relationship between coincident loneliness and anxiety symptoms, proportion mediated was 0.35, and depression symptoms, proportion mediated was 0.33. In the relationships between pandemic concern and anxiety or depression symptoms, the proportions mediated by resilience were 0.27 and 0.42, respectively.
Table 4.
Mediation analysis
| Depression | Anxiety | |||
|---|---|---|---|---|
| Coef * (SE) | P-value | Coef * (SE) | P-value | |
| Traumatic stress | ||||
| Association of traumatic stress with resilience [a] |
− 0.45 (0.04) |
< 0.001 |
− 0.46 (0.04) |
< 0.001 |
| Association of resilience with depression/anxiety, adjusting for traumatic stress [b] |
− 0.89 (0.04) |
< 0.001 |
− 2.98 (0.12) |
< 0.001 |
| Total association of traumatic stress with depression/anxiety [c] |
1.44 (0.10) |
< 0.001 |
5.91 (0.31) |
< 0.001 |
| Direct association of traumatic stress with depression/anxiety, not accounted for by resilience [c’] |
1.04 (0.10) |
< 0.001 |
4.55 (0.30) |
< 0.001 |
| Indirect (mediated) association of traumatic stress with depression/anxiety, not accounted for by resilience [ab or c–c’]** |
0.40 (0.04) |
< 0.001 |
1.36 (0.14) |
< 0.001 |
| Loneliness | ||||
| Association of loneliness with resilience |
− 0.48 (0.03) |
< 0.001 |
− 0.48 (0.03) |
< 0.001 |
| Association of resilience with depression/anxiety, adjusting for loneliness |
− 0.86 (0.04) |
< 0.001 |
− 3.00 (0.13) |
< 0.001 |
| Total association of loneliness with depression/anxiety |
1.26 (0.07) |
< 0.001 |
4.11 (0.22) |
< 0.001 |
| Direct association of loneliness with depression/anxiety, not accounted for by resilience |
0.85 (0.07) |
< 0.001 |
2.66 (0.22) |
< 0.001 |
| Indirect (mediated) association of loneliness with depression/anxiety, not accounted for by resilience |
0.41 (0.04) |
< 0.001 |
1.45 (0.13) |
< 0.001 |
| Pandemic concern | ||||
| Association of pandemic concern with resilience |
− 0.23 (0.03) |
< 0.001 |
− 0.24 (0.03) |
< 0.001 |
| Association of resilience with depression/anxiety, adjusting for pandemic concern |
− 0.97 (0.04) |
< 0.001 |
− 3.25 (0.12) |
< 0.001 |
| Total association of pandemic concern with depression/anxiety |
0.52 (0.07) |
< 0.001 |
2.78 (0.22) |
< 0.001 |
| Direct association of pandemic concern with depression/anxiety, not accounted for by resilience |
0.30 (0.07) |
< 0.001 |
2.01 (0.20) |
< 0.001 |
| Indirect (mediated) association of pandemic concern with depression/anxiety, not accounted for by resilience |
0.22 (0.03) |
< 0.001 |
0.76 (0.11) |
< 0.001 |
*Unstandardized coefficients, SE standard error; covariates included age (continuous, range 18–90), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, East/Southeast Asian, other), education (continuous, range 1–6), income (continuous, range 1–4), married/partnered status, number of children in household (none, 1 +), employment status, and number of comorbidities (continuous, range 0–7); for these analyses, depression, anxiety, and resilience total scores were used while the dichotomous version of traumatic stress/loneliness/pandemic concern (no/yes) was used
**Since these are linear models, the indirect association calculated by the product method (ab) is identical to the difference method (c–c’)
Discussion
In this snapshot of US women in the early phase of the COVID-19 pandemic, we identified significant associations between low resilience and demographic/socioeconomic variables, including younger age, lower educational level and household income, East/Southeast Asian race, more medical comorbidities, and unmarried or unpartnered status. The relationship between socioeconomic variables and levels of resilience has been documented in global populations. In studies of women during the pandemic, those who experienced pregnancy, post-partum state, miscarriage, and interpersonal violence were more likely to develop mental health concerns and had more severe symptoms of depression, anxiety, and stress (Almeida 2020, Farell 2020, Sediri et al., 2020). However, this is the first large-scale study to characterize the role of resilience in pandemic-coincident mental health morbidity in US women in the early days of the pandemic, identifying potentially modifiable factors.
The high levels of anxiety symptoms, depression symptoms, and traumatic stress symptoms identified in this population of women are consistent with other studies of COVID-19 and during the SARS epidemic (Duan and Zhu 2020; Hawryluck et al., 2004; Ko et al., 2006). Our finding of less psychiatric morbidity in older women is somewhat surprising given the greater risk of physical morbidity, but is also commensurate with other studies (González-Sanguino 2020; Wang et al., 2020b). A number of factors may have contributed to this. (1) Older people report greater spirituality, which has been identified a significant protective factor for depression, anxiety, and PTSD (Gonzalez-Sanguino 2020) (2) The prevalence of interpersonal violence, which is increased in women who are parents or guardian of a child aged less than eighteen, is less in older women (Kimerling et al., 2016). In our study, worsened interpersonal violence was a significant risk factor for low resilience. (3) Since older women are less likely to be living with dependent children, they are less likely to be as worried about infecting their children. (4) To adapt to late-life stressors that are often not “controllable,” older adults more frequently utilize “accommodative coping” which has been shown to uniquely predict remission in late-life depression (Loidl and Leipold 2019).
The importance of resilience enhancing strategies such as accommodative coping in disasters is supported by the significant associations between low resilience and measures of depression symptoms, anxiety symptoms, traumatic stress, and loneliness identified in this study. Resilience has been shown to buffer ongoing stress and reduce the risk of developing psychiatric morbidity in the COVID-19 pandemic (Barzilay et al., 2020; Killgore et al., 2020). We demonstrated a “dose–response” relationship between resilience and mental health measures, highlighting the interrelatedness of resilience, pandemic-related stress, and coincident depression and anxiety symptoms. It is also notable in this population of women that low resilience was significantly associated with fair/poor self-reported overall mental health. The association between negative appraisal of mental health and low resilience concurs with the findings of Veer and colleagues, who demonstrated that positive appraisal style correlated significantly with the ability to recover from stress and also partially mediated the positive association between perceived social support and resilience (2021).
Measuring resilience and the factors that impact it provides a potential opportunity to identify vulnerable populations. Interestingly, our sample showed that women who identified as East/Southeast Asian demonstrated low resilience, despite better self-rated health and higher income. This may reflect bias against East/Southeast Asian communities related to the COVID-19 pandemic (Clark et al., 2020; Dhanani and Franz 2020). New or worsening adverse socioeconomic conditions are associated with increased odds of psychiatric morbidity in our sample (Lindau et al., 2021). While certain socioeconomic factors cannot be changed (e.g., age), others such as poverty and limited social support are modifiable.
At the clinical level, much empirical evidence exists for specific treatments that can bolster resilience (Horn et al., 2016; Tabibnia 2020). Cognitive behavioral therapy (CBT), which addresses the interconnectedness of thoughts, feelings, and behaviors, and active behavioral coping, or the attempts to cope with a stressor by changing how one thinks about it, are examples of effective treatments that act primarily by reducing negative thoughts (Clark and Beck 2010; Ono et al., 2018). Mindfulness Based Stress Reduction (MBSR) involves shifting from self-focused mind wandering to enhanced present-centered awareness (Banks et al., 2015; Thompson et al., 2011). Other interventions that have been shown to promote resilience act by enhancing firing in the dopaminergic pathway, thus activating the reward network: these include psychological (enhancing optimism), physical (improving sleep, exercise, diet), and social (enhancing social support) interventions (Ashdown-Franks et al., 2020; Cruz-Pereira et al., 2020; Eisenberger 2015; Krause et al., 2017; Lai et al., 2020; Lee et al., 2019).
Strengths of our study include the large sample of women surveyed during a critical time period, the 6 weeks following the declaration of a pandemic and during a time when quarantining was widespread. However, the findings from this study should be interpreted in light of their limitations. This study is not a probability sample, but use of a national research panel allowed rapid enrollment at a critical time in the pandemic. Furthermore, as a cross-sectional study, it does facilitate the discovery of crucial correlational relationships, but it does not allow causal inference. There is a great need for longitudinal studies on the role of resilience as a marker of psychiatric vulnerability and the identification of optimal interventions, especially during a time of disaster. It is also a limitation of our study that information about the past history of psychiatric morbidity and suicide attempts, of the participants and their families, was not obtained. Another limitation was the use of the PHQ-2 to measure depressive symptoms, given that it does not measure somatic symptoms of depression which are especially relevant in older women. However, the lack of a specific measure of somatic symptoms of depression was partially mitigated by the use of additional questions in the survey measuring sleep and self-reported health. Change in sleep is a neurovegetative symptom of depression and it is interesting that while older age was associated with greater rates of poor/fair self-reported health, fewer of the most senior group of women (≥ 65) reported a change in sleep since the start of the pandemic (31% versus 59% in women aged 18–44). This suggests that the PHQ-2 did not necessarily miss depression symptoms in older women.
In this study, we characterize the well-being of women in the early pandemic. The high rates of depression and anxiety symptoms found are alarming and indicate an urgent need for actions to address suffering, both at the individual level and more broadly, to support women in their key roles in pandemic recovery. Resilience plays a role in mediating the effects of stress on mental health and may offer a useful opportunity for intervention.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to thank Dr. Stacy Lindau, MD, MAPP, and Dr. Jennifer A. Makelarski, PhD, MPH (The University of Chicago, Department of Obstetrics and Gynecology) for their significant contribution to this manuscript including the original data collection and study design as well as edits and feedback on the manuscript. Additionally, we would like to thank Gail Isenberg for editing the manuscript.
Declarations
Conflict of interest
E.L. receives research funding from AbbVie and Arsenal Bio to perform translational ovarian cancer research that is completely unrelated to this study. All other authors report no disclosures.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Ahun MN, Consoli A, Pingault J-B, Falissard B, Battaglia M, Boivin M, Tremblay RE, Côté SM. Maternal depression symptoms and internalising problems in the offspring: the role of maternal and family factors. Eur Child Adolesc Psychiatry. 2018;27(7):921–932. doi: 10.1007/s00787-017-1096-6. [DOI] [PubMed] [Google Scholar]
- Ashdown-Franks G, Firth J, Carney R, Carvalho AF, Hallgren M, Koyanagi Ai, Rosenbaum S, Schuch FB, Smith L, Solmi M, Vancampfort D, Stubbs B. Exercise as medicine for mental and substance use disorders: a meta-review of the benefits for neuropsychiatric and cognitive outcomes. Sports Med. 2020;50(1):151–170. doi: 10.1007/s40279-019-01187-6. [DOI] [PubMed] [Google Scholar]
- Banks K, Newman E, Saleem J. An overview of the research on mindfulness-based interventions for treating symptoms of posttraumatic stress disorder: a systematic review. J Clin Psychol. 2015;71(10):935–963. doi: 10.1002/jclp.22200. [DOI] [PubMed] [Google Scholar]
- Barzilay R, Moore TM, Greenberg DM, DiDomenico GE, Brown LA, White LK, Gur RC, Gur RE. Resilience, COVID-19-related stress, anxiety and depression during the pandemic in a large population enriched for healthcare providers. Transl Psychiatry. 2020;10(1):1–8. doi: 10.1038/s41398-020-00982-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baudry A-S, Vanlemmens L, Anota A, Cortot A, Piessen G, Christophe V. Profiles of caregivers most at risk of having unmet supportive care needs: recommendations for healthcare professionals in oncology. Eur J Oncol Nurs: the Off J Eur Oncol Nurs Soc. 2019;43:101669. doi: 10.1016/j.ejon.2019.09.010. [DOI] [PubMed] [Google Scholar]
- Chaudhry S, Jin L, Meltzer D. Use of a self-report-generated Charlson comorbidity index for predicting mortality. Med Care. 2005;43(6):607–615. doi: 10.1097/01.mlr.0000163658.65008.ec. [DOI] [PubMed] [Google Scholar]
- Chen HA, Trinh J, Yang GP. Anti-Asian sentiment in the United States – COVID-19 and history. Am J Surg. 2020;220(3):556–557. doi: 10.1016/j.amjsurg.2020.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark DA, Beck AT. Cognitive theory and therapy of anxiety and depression: convergence with neurobiological findings. Trends Cogn Sci. 2010;14(9):418–424. doi: 10.1016/j.tics.2010.06.007. [DOI] [PubMed] [Google Scholar]
- Clark, Eva, Karla Fredricks, Laila Woc-Colburn, Maria Elena Bottazzi, and Jill Weatherhead. 2020. “Disproportionate impact of the COVID-19 pandemic on immigrant communities in the United States.” PLoS Neglected Tropical Diseases 14(7). doi: 10.1371/journal.pntd.0008484. [DOI] [PMC free article] [PubMed]
- Cruz-Pereira JS, Rea K, Nolan YM, O’Leary OF, Dinan TG, Cryan JF. Depression’s unholy trinity: dysregulated stress, immunity, and the microbiome. Annu Rev Psychol. 2020;71(1):49–78. doi: 10.1146/annurev-psych-122216-011613. [DOI] [PubMed] [Google Scholar]
- Dhanani LY, Franz B. Unexpected public health consequences of the COVID-19 pandemic: a national survey examining anti-Asian attitudes in the USA. Int J Public Health. 2020;65(6):747–754. doi: 10.1007/s00038-020-01440-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dooley LN, Slavich GM, Moreno PI, Bower JE. Strength through adversity: moderate lifetime stress exposure is associated with psychological resilience in breast cancer survivors. Stress Health. 2017;33(5):549–557. doi: 10.1002/smi.2739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan Li, Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. The Lancet Psychiatry. 2020;7(4):300–302. doi: 10.1016/S2215-0366(20)30073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberger NI. Meta-analytic evidence for the role of the anterior cingulate cortex in social pain. Soc Cogn Affect Neurosci. 2015;10(1):1–2. doi: 10.1093/scan/nsu120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forrest CB, Bevans KB, Pratiwadi R, Moon JeanHee, Teneralli RE, Minton JM, Tucker CA. Development of the PROMIS ® pediatric global health (PGH-7) measure. Quality of Life Research: an International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation. 2014;23(4):1221–1231. doi: 10.1007/s11136-013-0581-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Sanguino C, Ausín B, Castellanos MÁ, Saiz J, López-Gómez A, Ugidos C, Muñoz M. Mental health consequences during the initial stage of the 2020 coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun. 2020;87:172–176. doi: 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber-Baldini AL, Velozo C, Romero S, Shulman LM. Validation of the PROMIS® measures of self-efficacy for managing chronic conditions. Qual Life Res. 2017;26(7):1915–1924. doi: 10.1007/s11136-017-1527-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Sarvet AL, Meyers JL, Saha TD, June Ruan W, Stohl M, Grant BF. Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiat. 2018;75(4):336–346. doi: 10.1001/jamapsychiatry.2017.4602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis. 2004;10(7):1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horn SR, Charney DS, Feder A. Understanding resilience: new approaches for preventing and treating PTSD. Exp Neurol. 2016;284:119–132. doi: 10.1016/j.expneurol.2016.07.002. [DOI] [PubMed] [Google Scholar]
- Jeung, Russell, and Kai Nham. 2020. “Incidents of coronavirus-related discrimination.” Asian Pacific Policy and Planning Council. Retrieved December 4, 2020 (https://a1w.90d.myftpupload.com/wp-content/uploads/2020/10/Stop_AAPI_Hate_Monthly_Report_200423.pdf).
- Kalisch R, Baker DG, Basten U, Boks MP, Bonanno GA, Brummelman E, Chmitorz A, Fernàndez G, Fiebach CJ, Galatzer-Levy I, Geuze E, Groppa S, Helmreich I, Hendler T, Hermans EJ, Jovanovic T, Kubiak T, Lieb K, Lutz B, Müller MB, Murray RJ, Nievergelt CM, Reif A, Roelofs K, Rutten BPF, Sander D, Schick A, Tüscher O, Van Diest I, van Harmelen A-L, Veer IM, Vermetten E, Vinkers CH, Wager TD, Walter H, Wessa M, Wibral M, Kleim B. The resilience framework as a strategy to combat stress-related disorders. Nat Hum Behav. 2017;1(11):784–790. doi: 10.1038/s41562-017-0200-8. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore WDS, Taylor EC, Cloonan SA, Dailey NS. Psychological resilience during the COVID-19 lockdown. Psychiatry Res. 2020;291:113216. doi: 10.1016/j.psychres.2020.113216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimerling R, Iverson KM, Dichter ME, Rodriguez AL, Wong A, Pavao J. Prevalence of intimate partner violence among women veterans who utilize Veterans Health Administration primary care. J Gen Intern Med. 2016;31(8):888–894. doi: 10.1007/s11606-016-3701-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko C-H, Cheng-Fang Yen J-Y, Yen, and Ming-Jen Yang. Psychosocial impact among the public of the severe acute respiratory syndrome epidemic in Taiwan. Psychiatry Clin Neurosci. 2006;60(4):397–403. doi: 10.1111/j.1440-1819.2006.01522.x. [DOI] [PubMed] [Google Scholar]
- Krause AJ, Simon EB, Mander BA, Greer SM, Saletin JM, Goldstein-Piekarski AN, Walker MP. The sleep-deprived human brain. Nat Rev Neurosci. 2017;18(7):404–418. doi: 10.1038/nrn.2017.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- Lai J, Ma S, Wang Y, Cai Z, Jianbo Hu, Wei N, Jiang Wu, Hui Du, Chen T, Li R, Tan H, Kang L, Yao L, Huang M, Wang H, Wang G, Liu Z, Shaohua Hu. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee LO, James P, Zevon ES, Kim ES, Trudel-Fitzgerald C, Spiro A, Grodstein F, Kubzansky LD. Optimism is associated with exceptional longevity in 2 epidemiologic cohorts of men and women. Proc Natl Acad Sci. 2019;116(37):18357–18362. doi: 10.1073/pnas.1900712116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SW, Yang JM, Moon SY, Yoo IK, Ha EK, Kim SY, Park UM, Choi S, Lee S-H, Ahn YM, Kim J-M, Koh HY, Yon DK. Association between mental illness and COVID-19 susceptibility and clinical outcomes in South Korea: a nationwide cohort study. The Lancet Psychiatry. 2020;7(12):1025–1031. doi: 10.1016/S2215-0366(20)30421-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindau, S. T., J. M. Makelarski, Kelly Boyd, KE Doyle, Sadia Haider, Shivani Kumar, Nita Karnik Lee, El Pinkerton, Marie Tobin, Milkie Vu, Kristen E. Wroblewski, and Ernst Lengyel. 2021. “Change in health-related social risk factors and mental health during the early phase of the COVID-19 pandemic: a national survey of U.S. women.” doi: 10.1089/jwh.2020.8879. [DOI] [PMC free article] [PubMed]
- Loidl B, Leipold B. Facets of accommodative coping in adulthood. Psychol Aging. 2019;34(5):640–654. doi: 10.1037/pag0000378. [DOI] [PubMed] [Google Scholar]
- Mayer B. A review of the literature on community resilience and disaster recovery. Current Environmental Health Reports. 2019;6(3):167–173. doi: 10.1007/s40572-019-00239-3. [DOI] [PubMed] [Google Scholar]
- North CS. Current research and recent breakthroughs on the mental health effects of disasters. Curr Psychiatry Rep. 2014;16(10):481. doi: 10.1007/s11920-014-0481-9. [DOI] [PubMed] [Google Scholar]
- Ono M, Kochiyama T, Fujino J, Sozu T, Kawada R, Yokoyama N, Sugihara G, Murai T, Takahashi H. Self-efficacy modulates the neural correlates of craving in male smokers and ex-smokers: an FMRI study. Addict Biol. 2018;23(5):1179–1188. doi: 10.1111/adb.12555. [DOI] [PubMed] [Google Scholar]
- Racine N, Birken C, Madigan S. Supporting the mental health of parents and children during and after coronovirus. J Dev Behav Pediatr. 2020;41(7):508–510. doi: 10.1097/DBP.0000000000000847. [DOI] [PubMed] [Google Scholar]
- Schuster MA, Stein BD, Jaycox L, Collins RL, Marshall GN, Elliott MN, Zhou AJ, Kanouse DE, Morrison JL, Berry SH. A national survey of stress reactions after the September 11, 2001, terrorist attacks. N Engl J Med. 2001;345(20):1507–1512. doi: 10.1056/NEJM200111153452024. [DOI] [PubMed] [Google Scholar]
- Sediri S, Zgueb Y, Ouanes S, Ouali U, Bourgou S, Jomli R, Nacef F. Women’s mental health: acute impact of COVID-19 pandemic on domestic violence. Archives of Women’s Mental Health. 2020 doi: 10.1007/s00737-020-01082-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shankar A, McMunn A, Banks J, Steptoe A. Loneliness, social isolation, and behavioral and biological health indicators in older adults. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association. 2011;30(4):377–385. doi: 10.1037/a0022826. [DOI] [PubMed] [Google Scholar]
- Smith BW, Tooley EM, Christopher PJ, Kay VS. Resilience as the ability to bounce back from stress: a neglected personal resource? J Posit Psychol. 2010;5(3):166–176. doi: 10.1080/17439760.2010.482186. [DOI] [Google Scholar]
- Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. 2008;15(3):194–200. doi: 10.1080/10705500802222972. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Tabibnia G. An affective neuroscience model of boosting resilience in adults. Neurosci Biobehav Rev. 2020;115:321–350. doi: 10.1016/j.neubiorev.2020.05.005. [DOI] [PubMed] [Google Scholar]
- The American Association for Public Opinion Research. 2016. Standard definitions: final dispositions of case codes and outcome rates for surveys. 9th ed. AAPOR.
- Thompson RW, Arnkoff DB, Glass CR. Conceptualizing mindfulness and acceptance as components of psychological resilience to trauma. Trauma Violence Abuse. 2011;12(4):220–235. doi: 10.1177/1524838011416375. [DOI] [PubMed] [Google Scholar]
- Tsirigotis K, Łuczak J. Resilience in women who experience domestic violence. Psychiatry Q. 2018;89(1):201–211. doi: 10.1007/s11126-017-9529-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twenge JM, Joiner TE. U.S. Census Bureau-assessed prevalence of anxiety and depressive symptoms in 2019 and during the 2020 COVID-19 pandemic. Depress Anxiety. 2020;37(10):954–956. doi: 10.1002/da.23077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. 2018. “2018 American community survey 1-year estimates.” Retrieved May 15, 2020 (https://www2.census.gov/programs-surveys/acs/summary_file/2018/data/?#).
- Veer IM, Riepenhausen A, Zerban M, Wackerhagen C, Puhlmann LMC, Engen H, Köber G, Bögemann SA, Weermeijer J, Uściłko A, Mor N, Marciniak MA, Askelund AD, Al-Kamel A, Ayash S, Barsuola G, Bartkute-Norkuniene V, Battaglia S, Bobko Y, Bölte S, Cardone P, Chvojková E, Damnjanović K, De Calheiros J, Velozo L, de Thurah YI, Deza-Araujo AD, Farkas K, Feller C, Gazea M, Gilan D, Gnjidić V, Hajduk M, Hiekkaranta AP, Hofgaard LS, Ilen L, Kasanova Z, Khanpour M, Lau BHP, Lenferink DB, Lindhardt TB, Magas DÁ, Mituniewicz J, Moreno-López L, Muzychka S, Ntafouli M, O’Leary A, Paparella I, Põldver N, Rintala A, Robak N, Rosická AM, Røysamb E, Sadeghi S, Schneider M, Siugzdaite R, Stantić M, Teixeira A, Todorovic A, Wan WWN, van Dick R, Lieb K, Kleim B, Hermans EJ, Kobylińska D, Hendler T, Binder H, Myin-Germeys I, van Leeuwen JMC, Tüscher O, Yuen KSL, Walter H, Kalisch R. Psycho-social factors associated with mental resilience in the corona lockdown. Transl Psychiatry. 2021;11(1):1–11. doi: 10.1038/s41398-020-01150-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinkers CH, van Amelsvoort T, Bisson JI, Branchi I, Cryan JF, Domschke K, Howes OD, Manchia M, Pinto L, de Quervain D, Schmidt MV, van der Wee NJA. Stress resilience during the coronavirus pandemic. European Neuropsychopharmacology: the Journal of the European College of Neuropsychopharmacology. 2020;35:12–16. doi: 10.1016/j.euroneuro.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C, Pan R, Wan X, Tan Y, Linkang Xu, Ho CS, Roger CH. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C, Pan R, Wan X, Tan Y, Linkang Xu, McIntyre RS, Choo FN, Tran B, Ho R, Sharma VK, Ho C. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windle G, Bennett KM, Noyes J. A methodological review of resilience measurement scales. Health Qual Life Outcomes. 2011;9:8. doi: 10.1186/1477-7525-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xi Y, Hui Yu, Yao Y, Peng Ke, Wang Y, Chen R. Post-traumatic stress disorder and the role of resilience, social support, anxiety and depression after the Jiuzhaigou earthquake: a structural equation model. Asian J Psychiatr. 2020;49:101958. doi: 10.1016/j.ajp.2020.101958. [DOI] [PubMed] [Google Scholar]
- Zhang M, Zhang J, Zhang F, Zhang Li, Feng D. Prevalence of psychological distress and the effects of resilience and perceived social support among Chinese college students: does gender make a difference? Psychiatry Res. 2018;267:409–413. doi: 10.1016/j.psychres.2018.06.038. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.