Abstract
Cardiovascular disease (CVD) and osteoporosis often occur together, suggesting an association between CVD and bone loss. Similarly, the correlation of bone loss, atherosclerosis, and aortic calcification, especially in patients with chronic kidney disease, exemplifies a bone-vessel connection. In this issue of the JCI, Santhanam et al. investigated the role of the angiogenesis factor platelet-derived growth factor–BB (PDGF-BB) in vascular stiffening. Serum levels of bone-derived PDGF-BB differed between young and aged mice, and in mice fed a high-fat diet (HFD) compared with those fed normal chow. Experiments with genetic models led the authors to conclude that bone-derived PDGF-BB mediates the hallmark arterial stiffening of aging and metabolic stress. Notably, excessive preosteoclast-derived PDGF-BB production during aging inhibited osteoblastic bone formation and increased circulating PDGF-BB, which in turn, accelerated vascular stiffness. These findings suggest that modifying circulating PDGF-BB levels may benefit patients with CVD, osteoporosis, and other age-related diseases.
Bone-vessel connection
Cardiovascular disease (CVD) remains the leading cause of morbidity and mortality worldwide, with a steady increase in the number of deaths over the past decade. Osteoporosis is likewise a crippling disease of public health importance, which continues to grow in prevalence in older women and men. The two diseases often present concurrently, especially in an increasingly aging population. Mounting biological and epidemiological data support a direct association of CVD with bone loss. It is clear from large-scale, cross-sectional, and longitudinal studies that reduced bone density and cardiovascular risk correlate (1). There is also a strong correlation among bone loss, atherosclerosis, and aortic calcification, particularly in patients with chronic kidney disease. These findings underpin the evolving concept of a bone-vessel connection (2–5). In this circuitry, molecules secreted by bone cells, namely osteopontin, osteoprotegerin, and sclerostin, will participate in such inter-organ crosstalk.
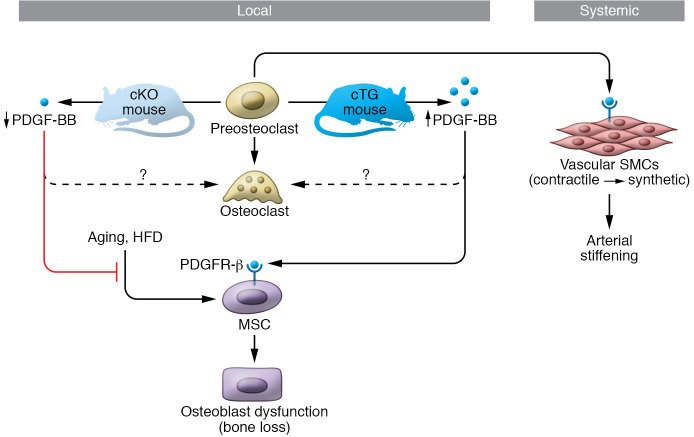
The skeleton has traditionally been viewed as an inert organ responsible for physical support and locomotion, and as a reservoir for calcium that is regulated by ions, autacoids, cytokines, and hormones (6). Thus, it has been suggested that lost bone in osteoporosis is merely a risk factor for CVD (7). Contrarily, there is recent recognition that bone is itself an endocrine organ, and that bone cells—osteoclasts, osteoblasts, and osteocytes—synthesize and secrete molecules that regulate bodily functions, including energy expenditure, fat deposition, appetite control, skeletal muscle adaptation, male fertility, and cognition (8). In particular, the osteoclast not only secretes growth factors and cytokines, collectively termed “clastokines,” but, during resorption, also releases molecules trapped within the bone matrix, such as transforming factor β (9–11). The clastokine of interest in this Commentary is the potent angiogenesis factor, platelet-derived growth factor–BB (PDGF-BB). Elegant prior studies have shown that osteoclast precursor cells, or preosteoclasts, secrete PDGF-BB, which, in turn, induces the formation of a capillary subtype, type H vessels, for new bone formation during bone modeling and remodeling (12). Thus, the cell-selective depletion of Pdgfb in preosteoclasts reduces both angiogenesis and bone synthesis, eventually resulting in bone loss (12). Preosteoclast-derived PDGF-BB is therefore a mediator of angiogenesis and bone formation (Figure 1).
Figure 1. A model of preosteoclast-derived PDGF-BB in bone and vascular aging.
Osteoclast precursors (preosteoclasts) in bone marrow secrete PDGF-BB that acts in a concentration-dependent manner on mesenchymal stem cells (MSCs), which ultimately give rise to bone-forming osteoblasts. High bone marrow PDGF-BB levels, as in the Pgdfb-overexpressing mouse (cTG), cause reduced osteoblastic bone formation and bone loss, whereas loss of PDGF-BB in a conditional preosteoclast-selective mutant (cKO) attenuates age- and HFD-induced osteopenia. Preosteoclast-derived PDGF-BB also contributes substantially to circulating PDGF-BB, which increases with age. High serum PDGF-BB acts via PDGFR-β receptors on VSMCs to promote a contractile-to-synthetic phenotypic switch that results in arterial stiffening (13). PDGF-BB may thus be another piece of the puzzle that connects bone with vessel, and osteoporosis with CVD.
Preosteoclasts produce PDGF-BB in the circulation
In this issue of the JCI, Santhanam and colleagues describe a role for PDGF-BB in skeletal and vascular pathologies (13). They found that bone-derived PDGF-BB was higher in aged as compared with young mice, and in mice fed on a high-fat diet (HFD) versus those on normal chow. Based on this finding, the authors examined the concentration dependence of PDGF-BB actions on bone in loss- and gain-of-function studies, respectively, using cell-specific deletion mutants for Pdgfb (cKO), and transgenic mice (cTG) overexpressing PDGF-BB selectively in preosteoclasts. Young cTG mice, in which PDGF-BB was higher in bone marrow, faithfully recapitulated the age-dependent low bone mass phenotype. This result was testament to the deleterious skeletal effect of excessive preosteoclast-derived PDGF-BB during aging. Paradoxically, young, healthy cKO mice also displayed low bone mass at baseline (13), a finding that is consistent with the authors’ earlier report for a necessary function of PDGF-BB in skeletal remodeling (12). Nonetheless, aged cKO mice had increased bone mass with attenuated HFD-induced bone loss (13). In all, the findings suggest that preosteoclast-derived PDGF-BB is a critical mediator of bone loss in aging.
The next experiments set forth to explore the contribution of PDGF-BB secreted from preosteoclasts to total serum PDGF-BB levels, which double with aging in mice. Notably, the selective deletion of Pdgfb in preosteoclasts in aged mice normalized serum PDGF-BB levels to levels observed in young mice, while overexpression of proteoclast PDGF-BB specifically in young mice elevated serum levels to those noted for aged cTG mice. That preosteoclast-derived PDGF-BB appears to be a main source of circulating PDGF-BB led the authors to examine a role for this clastokine in arterial stiffness (13).
A momentous claim
The authors make a momentous claim—that bone-derived PDGF-BB mediates the hallmark arterial stiffening of aging and metabolic stress (13). Arterial aging is characterized by changes in vascular smooth muscle cells (VSMCs), which display a shift from contractile to a dedifferentiated, synthetic phenotype, resulting in intimal and medial thickening, elevated collagen/elastin ratio in the arterial wall, and increased mechanical vessel rigidity and stiffness (14). Vascular stiffness is an independent predictor of cardiovascular morbidity and mortality (15).
Santhanam et al. provide complementary in vitro, in vivo, and ex vivo evidence for a role of bone-derived PDGF-BB in vascular aging. First, conditioned media from Pdgfb-overexpressing preosteoclasts promoted VSMC proliferation and migration. Second, noninvasive measurements of blood pressure and pulse wave velocity, the latter being a surrogate for vascular stiffness, showed that young cTG mice develop increased aorta stiffness. Third, ex vivo tensile and vasoconstriction response testing showed dramatically higher passive stiffness and an increased vasoconstriction response in vessels from young cTG mice. Histologically, cTG mice showed increased collagen fibers in the extracellular matrix and calcification of the aortic wall, both of which are important contributors to the pathogenesis of arterial stiffening. Finally, and importantly, age- and HFD-induced vascular stiffening was markedly attenuated by Pdgfb deletion in preosteoclasts in cKO mice (13). In all, it is clear that the excessive production of PDGF-BB from preosteoclasts during aging induces bone loss by inhibiting osteoblastic bone formation on one hand, and on the other, accelerates the aging of blood vessels by increasing circulating PDGF-BB.
PDGF-BB has been widely implicated in cardiovascular pathogenesis, including atherosclerosis, pulmonary arterial hypertension, diabetes, angiogenesis, and inflammation (16). The importance of the current study therefore is not to link PDGF-BB with cardiovascular pathogenesis or risk, but instead, to illuminate the fact that the increased circulating PDGF-BB in aging is derived from a bone cell, at least in mice (13). This clarity leads to calls to determine the mechanism of action through which aging alters the production of PDGF-BB in bone and bone marrow preosteoclasts.
Conclusions and future directions
The bigger question for bone biologists is whether preosteoclasts begin to produce other modifiers in addition to PDGF-BB with aging. Indeed, no prior studies have investigated whether skeletal preosteoclasts acquire a senescence-associated secretory phenotype (SASP). We also need to know precisely how increased bone-derived PDGF-BB causes bone loss. The authors showed reduced osteoblast numbers and unchanged osteoclast numbers in the cTG mice, providing a basic framework for future studies (13). It presently remains unclear whether PDGF-BB affects osteoblast commitment from mesenchymal stromal cells, their differentiation, and/or the function and lifespan of mature cells.
Influential future experiments would determine whether the aberrant production of PDGF-BB during aging is also associated with other disorders of aging, such as osteoarthritis, obesity, or neurodegeneration. It is plausible that single hormones, such as PDGF and follicle-stimulating hormone (FSH), among others, which become elevated with age, have ubiquitous functions. High serum FSH levels, for example, associate not only with bone loss, but also with obesity, hyperlipidemia, osteoarthritis, and neurodegeneration (17–20). Likewise, the authors have previously shown that PDGF-BB derived from preosteoclasts drives subchondral bone angiogenesis in osteoarthritis (21). Dysregulated PDGFR-β signaling is also involved in multiple pathologies, including compromised brain–blood barrier, ocular neovascularization, and importantly, oncogenesis, just to name a few. And, while targeted therapies to block this tyrosine kinase receptor continue to be developed for certain cancers, it may be prudent in the future to focus on ligand-specific molecules, such as antibodies (17), that would fine-tune circulating PDGF-BB levels toward a therapeutic advantage in chronic diseases that accompany aging.
Acknowledgments
MZ and TY are supported by grants from the National Institute of Aging and the National Institute of Diabetes, Digestive, and Kidney Diseases.
Version 1. 10/15/2021
Electronic publication
Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
Copyright: © 2021, American Society for Clinical Investigation.
Reference information: J Clin Invest. 2021;131(20):e153644. https://doi.org/10.1172/JCI153644.
See the related article at Skeleton-secreted PDGF-BB mediates arterial stiffening.
Contributor Information
Mone Zaidi, Email: mone.zaidi@mssm.edu.
Daria Lizneva, Email: daria.lizneva@mssm.edu.
References
- 1.Hyder JA, et al. Bone mineral density and atherosclerosis: the multi-ethnic study of atherosclerosis, abdominal aortic calcium study. Atherosclerosis. 2010;209(1):283–289. doi: 10.1016/j.atherosclerosis.2009.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jankowski J, et al. Cardiovascular disease in chronic kidney disease: pathophysiological insights and therapeutic options. Circulation. 2021;143(11):1157–1172. doi: 10.1161/CIRCULATIONAHA.120.050686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tanko LB, et al. Low bone mineral density in the hip as a marker of advanced atherosclerosis in elderly women. Calcif Tissue Int. 2003;73(1):15–20. doi: 10.1007/s00223-002-2070-x. [DOI] [PubMed] [Google Scholar]
- 4.Tap L, et al. Unraveling the links underlying arterial stiffness, bone demineralization, and muscle loss. Hypertension. 2020;76(3):629–639. doi: 10.1161/HYPERTENSIONAHA.120.15184. [DOI] [PubMed] [Google Scholar]
- 5.Shao JS, et al. Molecular mechanisms of vascular calcification: lessons learned from the aorta. Arterioscler Thromb Vasc Biol. 2006;26(7):1423–1430. doi: 10.1161/01.ATV.0000220441.42041.20. [DOI] [PubMed] [Google Scholar]
- 6.Zaidi M. Skeletal remodeling in health and disease. Nat Med. 2007;13(7):791–801. doi: 10.1038/nm1593. [DOI] [PubMed] [Google Scholar]
- 7.Hu X, et al. Relationship between senile osteoporosis and cardiovascular and cerebrovascular diseases. Exp Ther Med. 2019;17(6):4417–4420. doi: 10.3892/etm.2019.7518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zaidi M, et al. Regulation of skeletal homeostasis. Endocr Rev. 2018;39(5):701–718. doi: 10.1210/er.2018-00050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Crane JL, et al. Role of TGF-β signaling in coupling bone remodeling. Methods Mol Biol. 2016;1344:287–300. doi: 10.1007/978-1-4939-2966-5_18. [DOI] [PubMed] [Google Scholar]
- 10.Drissi H, Sanjay A. The multifaceted osteoclast; far and beyond bone resorption. J Cell Biochem. 2016;117(8):1753–1756. doi: 10.1002/jcb.25560. [DOI] [PubMed] [Google Scholar]
- 11.Zaidi M, Iqbal J. Translational medicine: double protection for weakened bones. Nature. 2012;485(7396):47–48. doi: 10.1038/485047a. [DOI] [PubMed] [Google Scholar]
- 12.Xie H, et al. PDGF-BB secreted by preosteoclasts induces angiogenesis during coupling with osteogenesis. Nat Med. 2014;20(11):1270–1278. doi: 10.1038/nm.3668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Santhanam L, et al. Skeleton-secreted PDGF-BB mediates arterial stiffening. J Clin Invest. 2021;131(20):e147116. doi: 10.1172/JCI147116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.North BJ, Sinclair DA. The intersection between aging and cardiovascular disease. Circ Res. 2012;110(8):1097–1108. doi: 10.1161/CIRCRESAHA.111.246876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tesauro M, et al. Arterial ageing: from endothelial dysfunction to vascular calcification. J Intern Med. 2017;281(5):471–482. doi: 10.1111/joim.12605. [DOI] [PubMed] [Google Scholar]
- 16.Hu W, Huang Y. Targeting the platelet-derived growth factor signalling in cardiovascular disease. Clin Exp Pharmacol Physiol. 2015;42(12):1221–1224. doi: 10.1111/1440-1681.12478. [DOI] [PubMed] [Google Scholar]
- 17.Gera S, et al. First-in-class humanized FSH blocking antibody targets bone and fat. Proc Natl Acad Sci U S A. 2020;117(46):28971–28979. doi: 10.1073/pnas.2014588117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu P, et al. Blocking FSH induces thermogenic adipose tissue and reduces body fat. Nature. 2017;546(7656):107–112. doi: 10.1038/nature22342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guo Y, et al. Blocking FSH inhibits hepatic cholesterol biosynthesis and reduces serum cholesterol. Cell Res. 2019;29(2):151–166. doi: 10.1038/s41422-018-0123-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu Y, et al. High follicle-stimulating hormone levels accelerate cartilage damage of knee osteoarthritis in postmenopausal women through the PI3K/AKT/NF-κB pathway. FEBS Open Bio. 2020;10(10):2235–2245. doi: 10.1002/2211-5463.12975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Su W, et al. Angiogenesis stimulated by elevated PDGF-BB in subchondral bone contributes to osteoarthritis development. JCI Insight. 2020;5(8):135446. doi: 10.1172/jci.insight.135446. [DOI] [PMC free article] [PubMed] [Google Scholar]