Abstract
The coronavirus disease 2019 (COVID-19) has been shown to have more severe health outcomes in older people specifically in relation to mortality and disability. Vaccination seems to be efficacious and safe for preventing the negative consequences of COVID-19, but vaccine hesitancy seems to be high in older adults. We therefore aimed to investigate the prevalence of unwillingness and the uncertainty to vaccinate against COVID-19 in older people and the factors that can be associated with the unwillingness to vaccinate. For this work, we searched several databases until 18th June 2021 for studies reporting the prevalence of unwillingness and the uncertainty to vaccinate against COVID-19 in people aged >60 years. A meta-analysis of the prevalence, with the correspondent 95% confidence intervals (CIs), was proposed. Factors that can be associated with the unwillingness to vaccinate against COVID-19 were explored through multivariable analyses and reported as odds ratios (ORs). Among 662 papers initially screened, we included 15 studies for a total of 9753 older adults. The prevalence of unwillingness to vaccinate against COVID-19 in older people was 27.03% (95%CI: 15.10–38.95%), whilst the correspondent figure of uncertainty was 19.33% (95%CI: 12.28–26.39). The risk of being unvaccinated was significantly higher in Hispanics (OR=1.197; 95%CI: 1.010–1.418) and in case of low education (OR=1.678; 95%CI: 1.170–2.408) and low income (OR=1.287; 95%CI: 1.127–1.469). In conclusion, the hesitancy for COVID-19 vaccination is a relevant problem in older people, particularly in those with a low income, a low level of education, and in Hispanics living in the United States.
Keywords: COVID-19, older adults, hesitancy, vaccine
1. Introduction
In March 2020, the World Health Organization (WHO) declared the coronavirus disease 2019 (COVID-19) outbreak a global pandemic (Jebril, 2020). During 2020, more than 83 million people were affected by COVID-19, with approximately two million associated deaths (Organization, 2021). It could be hypothesized that COVID-19 is a geriatric syndrome since epidemiological data have clearly indicated that the mortality rates are extremely high in older persons and that the prevalence of COVID-19 is more elevated in older compared to younger persons (Onder et al., 2020). Moreover, in settings dedicated to the older people, such as nursing homes, the highest mortality rate has been observed (Veronese and Barbagallo, 2021).
However, vaccine acceptance in the general population is associated with several factors, such as the perceived risk of an infection and concern regarding its side effects. For example, studies on the uptake of seasonal flu vaccination have shown that the perceived risk of getting influenza and belief in the efficacy of the vaccine are the main drivers towards vaccine acceptance whilst fear of adverse effects is the main deterrent (Troiano and Nardi, 2021). In the United States, as of May 2021, the Centers for Disease Control and Prevention (CDC) reported 84.0% of adults 65 and older have received at least their first COVID-19 vaccine dose and 71.9% have been fully vaccinated, but the rates of fully vaccinated older adults significantly vary across states, from 57.6% in Utah to 87.0% in Vermont (Coustasse et al., 2021). Since the effectiveness of a vaccination program is also dependent on wide vaccine uptake particularly in people that can be more compromised, it is important to understand the prevalence and the various factors that may modify an older person’s willingness to get vaccinated in order to establish effective public health strategies during a pandemic.
Given this background, we aimed to investigate the prevalence of unwillingness and the uncertainty to vaccinate against COVID-19 in older people and the factors that can affect the unwillingness to vaccinate.
2. Methods
This systematic review adhered to the PRISMA statement (Liberati et al., 2009) and followed a pre-planned, but unpublished protocol that can be requested by contacting the corresponding author.
2.1. Data sources and searches
Two investigators (NV and CS) independently conducted a literature search using several databases without language restriction, until 18th June 2021, with the following keywords for Pubmed: “(vaccin* or immunis* or immuniz*) AND (anxiety or attitude* or awareness or behavior or behavior or belief* or criticis* or doubt* or distrust or dropout* or exemption* or fear* or hesitanc* or trust or mistrust or perception* or refus or rejection or rumor* or intent* or controvers* or misconception* or misinformation or opposition or delay or dilemma* or objector* or uptake or barrier* or choice* or mandatory or compulsory or concern* or accepta* or anti-vaccin* or antivaccin*) AND ("covid 19"[MeSH Terms] OR "covid 19"[All Fields] OR "covid19"[All Fields] OR "covid 19"[All Fields] OR "covid 19"[MeSH Terms] OR "covid 19 vaccines"[All Fields] OR "covid 19 vaccines"[MeSH Terms] OR "covid 19 serotherapy"[All Fields] OR "covid 19 serotherapy"[Supplementary Concept] OR "covid 19 nucleic acid testing"[All Fields] OR "covid 19 nucleic acid testing"[MeSH Terms] OR "covid 19 serological testing"[All Fields] OR "covid 19 serological testing"[MeSH Terms] OR "covid 19 testing"[All Fields] OR "covid 19 testing"[MeSH Terms] OR "sars cov 2"[All Fields] OR "sars cov 2"[MeSH Terms] OR "severe acute respiratory syndrome coronavirus 2"[All Fields] OR "ncov"[All Fields] OR "2019 ncov"[All Fields] OR "coronavirus"[MeSH Terms] OR "coronavirus"[All Fields] OR "cov"[All Fields]) AND (older* OR elderly OR older adult OR aged)”. The searches for the single database are reported in Supplementary Table 1. Any inconsistencies were resolved by consensus, with a third author (JD).
2.2. Study selection
Inclusion criteria for this meta-analysis were: (i) made in older adults (age > 60 years); (ii) reporting data on COVID-19 vaccination hesitancy. Studies were excluded if: (i) did not include humans; (ii) were conference abstracts.
2.3. Data extraction
Two independent investigators (NV and CS) extracted key data from the included articles in a standardized Excel spread sheet and a third independent investigator (MB) checked these data for the accuracy. For each article, we extracted data on authors, year of publication, country, the outcomes of interest and the data regarding multivariable analysis, taking unwillingness to get vaccinated or uncertainty as the outcome.
After verifying that the possible eligible article contains at least one part of older people, if specific data regarding COVID-19 vaccine hesitancy in older people were not reported in the original studies or other data were missing, first and/or corresponding authors of the original article were contacted once, given approximately 4 weeks to respond for obtaining unpublished data and additional elaborations.
2.4. Outcomes
The primary outcome of our investigation was to explore the prevalence of vaccine hesitancy against COVID-19 in older people, defined by the World Health Organization Strategic Advisory Group of Experts (WHO SAGE) working group as the “delay of acceptance or refusal of vaccination despite availability of vaccination services” (Domek et al., 2018). Vaccine hesitancy was explored using as estimates the prevalence of unwillingness and the uncertainty to vaccinate.
2.5. Data synthesis and analysis
All analyses were performed using STATA version 14.0 (StataCorp).
The primary analysis reported the prevalence of unwillingness and the uncertainty to vaccinate against COVID-19 in older people (in percentage) with their 95% confidence intervals (CIs), applying a random-effect model (DerSimonian and Laird, 1986). Heterogeneity across studies was assessed by the I2 metric and χ2 statistics, taking an I2 ⩾50% (p < 0.05) as a significant heterogeneity.
Publication bias was assessed by visually inspecting funnel plots and using the Egger bias test (Egger et al., 1997). Then, in case of publication bias, the trim-and-fill method was used, based on the assumption that the effect sizes of all the studies are normally distributed around the center of a funnel plot; in the event of asymmetries, it adjusts for the potential effect of unpublished (trimmed) studies (Duval and Tweedie, 2000).
Moreover, we investigated factors associated with the unwillingness to vaccinate against COVID-19 in older people. To achieve this, analyses were conducted by the research team (in the case of freely accessible data) or the corresponding authors of the included articles were contacted. Since data from multivariable analyses already run in the original studies are the most appropriate for determining factors associated with the outcome of interest (i.e., the unwillingness to vaccinate against COVID-19), we took for every study having these data the most adjusted model and we extracted the ORs for common factors across the studies. In this way, we analyzed several factors potentially associated to the unwillingness to vaccinate, such as presence of any comorbidity, women (vs. men), Hispanic and black ethnicity (vs. whites), low education, low income, rural area, being married and being employed.
For all analyses, a p-value less than 0.05 was considered statistically significant.
3. Results
3.1. Search results
Supplementary figure 1 shows the PRISMA flow-chart. Overall, among 662 papers initially included, we reviewed the full texts of 29 articles. Of them, 15 were eligible (Abedin et al., 2021, Al-Qerem and Jarab, 2021, Alqudeimat et al., 2021, Bogart et al., 2021, Daly and Robinson, 2020, Gagneux-Brunon et al., 2021, Kourlaba et al., 2021, Latkin et al., 2021, Lazarus et al., 2020, Machida et al., 2021, Malesza and Wittmann, 2021, Oliveira et al., 2021, Petravic et al., 2021, Salmon et al., 2021, Yoda and Katsuyama, 2021), whilst other 14 were excluded mainly because data regarding older people were not reported (n = 12) (full list of references in Supplementary Table 2).
3.2. Study and patient characteristics
Supplementary Table 3 reports the main descriptive findings of the studies included. Overall, the 15 independent studies gave a total sample size of 9753 older people, with five studies carried out in Europe, five in Asia and five in North/South America.
3.3. Prevalence of unwillingness and uncertainty to vaccinate against COVID-19 in older people
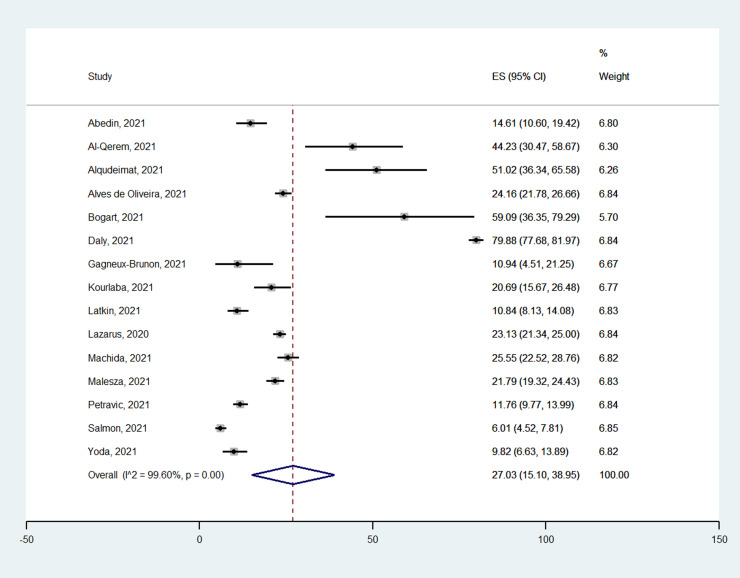
Fig. 1 reports the prevalence of the unwillingness to vaccinate against COVID-19 in older people. Overall, the prevalence was 27.03% (95%CI: 15.10–38.95%) with a range between 6.01% (95%CI: 4.52–7.81) to 79.88% (95%CI: 77.68–81.97), across the 15 studies included. This outcome was characterized by a high heterogeneity (I2 = 99.6%), but not by publication bias (Egger’s test = 1.77 ± 8.59; p = 0.84). The prevalence was similar across the continents (p for the interaction = 0.83).
Fig. 1.
Meta-analysis of the prevalence of the unwillingness to vaccinate against COVID-19 in older people.
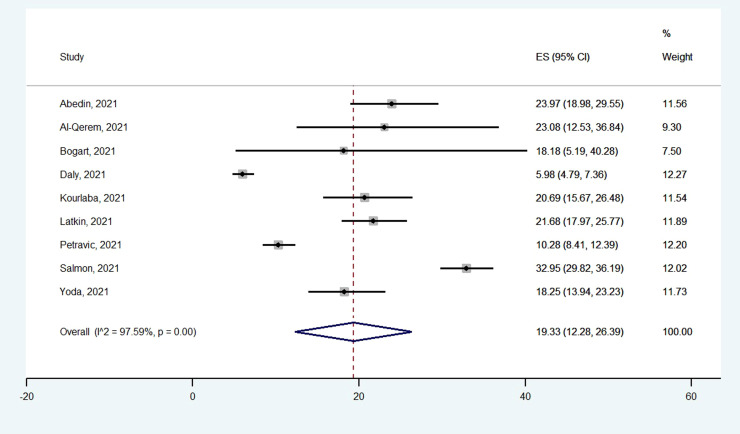
A similar analysis was run for the prevalence of uncertainty to vaccinate against COVID-19. For this outcome, the overall prevalence was 19.33% (95%CI: 12.28–26.39) ( Fig. 2), with data from nine different studies. The prevalence of the uncertainty ranged from 5.98% to 32.95%. This outcome was characterized by a high heterogeneity (I2 = 97.6%) and a marginal statistically significant publication bias (Egger’s test = 6.76 ± 2.84; p = 0.052). After trimming two studies at the left of the mean, the re-calculated prevalence was 16.3% (95%CI: 10.1–22.6%). The prevalence of uncertainty to vaccinate against COVID-19 was significantly higher in American countries (25.57%; 95%CI: 15.86–35.28) compared to Europe (11.62%; 95%CI: 6.07–17.18) (p for interaction = 0.001).
Fig. 2.
Meta-analysis of the prevalence of the uncertainty to vaccinate against COVID-19 in older people.
3.4. Factors associated with the unwillingness to vaccinate against COVID-19 in older people
Table 1 shows factors associated with the unwillingness to vaccinate against COVID-19 derived from the multivariable analyses available in eight studies (Abedin et al., 2021, Alqudeimat et al., 2021, Daly and Robinson, 2020, Latkin et al., 2021, Machida et al., 2021, Oliveira et al., 2021, Petravic et al., 2021, Yoda and Katsuyama, 2021). Overall, in multivariable analyses, Hispanic people in North American studies were more likely not to get vaccinated than the other ethnicities (n = 2 studies; OR = 1.197; 95%CI: 1.010–1.418; p = 0.038; I2 = 0%), as well as those with a lower level of education (compared with higher level of education) (n = 4 studies; OR = 1.678; 95%CI: 1.170–2.408; p = 0.005; I2 = 52.3%) and those with less wealth (compared to higher levels) (n = 2 studies; OR = 1.287; 95%CI: 1.127–1.469; p < 0.0001; I2 = 0%).
Table 1.
Factors associated in the multivariable analyses to the unwillingness to vaccinate against COVID-19 in older people.
| Factor | Number of studies | OR (95%CI) | p-value | I2 |
|---|---|---|---|---|
| Presence of any comorbidity | 5 | 0.899 (0.627–1.288) | 0.561 | 72.2 |
| Female gender | 7 | 1.000 (0.728–1.374) | 0.99 | 79.5 |
| Hispanic | 2 | 1.197 (1.010–1.418) | 0.038 | 0 |
| Black | 2 | 1.192 (0.843–1.686) | 0.319 | 0 |
| Low education | 4 | 1.678 (1.170–2.408) | 0.005 | 52.3 |
| Low income | 2 | 1.287 (1.127–1.469) | <0.0001 | 0 |
| Rural area | 3 | 0.798 (0.502–1.268) | 0.339 | 26.0 |
| Married | 3 | 0.652 (0.401–1.059) | 0.084 | 0 |
| Employed | 2 | 1.192 (0.843–1.686) | 0.319 | 0 |
Abbreviations. OR: odds ratio; CI: confidence intervals. In bold significant values, as p-values <0.05.
4. Discussion
In this systematic review and meta-analysis including 9753 older people from different continents, we found that (i) the prevalence of unwillingness to vaccinate affects 27.03% older adults and (ii) that about 19.33% of older adults are undecided on whether to be vaccinated or not. Moreover, the risk of being unvaccinated was significantly higher in Hispanics and in case of low education and low income.
The present meta-analysis suggests that a consistent part of older people included will not or is undecided whether to get the vaccination against COVID-19, indicating that it is important to encourage and promote vaccination to older people.
We believe that the findings of our meta-analysis in relation to vaccine hesitancy may be justified through several explanations. First, scare mongering on social media has played a role in determining the high hesitancy rate among older people for uptake of the COVID-19 vaccination (Malik et al., 2020). However, it should be noted that the role of social media in determining vaccine hesitancy in older people is probably limited (Puri et al., 2020). Second, as shown in some studies included in this systematic review and meta-analysis, the risk of side effects and the fear of death are among the most important barriers for vaccination in older people. Since 2021, high awareness to side effects was present among older persons, it is therefore possible that this factor could have negatively affected the propensity of older people to get vaccinated.
Moreover, our work indicates that low socio-economic status (SES), represented by low educational level and low income, is an important risk factor of unwillingness to get the COVID-19 vaccination in older people. Of importance, some studies have reported that before the availability of these vaccines, low SES was an independent risk factor for hospitalization, due to severe forms of COVID-19 (Hawkins et al., 2020). At the same time, these people seem to be afraid of getting vaccination. One possible explanation is reported using the 3C model (confidence, complacency, convenience) that, briefly, indicates that the attitude of people in getting vaccinated is determined not only by the confidence (e.g., the vaccination is safe), but also by complacency (e.g., the role of COVID-19 on quality of life) and convenience (e.g., to have the vaccination against COVID-19 is physically difficult) (Domek et al., 2018). In this regard, people with low SES may have a limited access to correct information about the role of vaccines in preventing the disease. To the contrary, people with higher educational achievement were less likely to be vaccine hesitant because of better education and access to health services. Another possible problem could be the trust issue, i.e. fear of betrayal, abandonment, and manipulation that is particularly present in people with low SES. At the same time, it is also possible that low income may prevent vaccination via other avenues in addition to hesitancy such as via lower accessibility to transportation or that caregivers have less free time for bringing older people to vaccinations’ points (Bertoncello et al., 2020).
Finally, even if limited to only two studies carried out in the U.S,. our meta-analysis indicated that Hispanic people do not want to be vaccinated against COVID-19, compared to Caucasians. In support data reported by the Centers for Disease Control and Prevention (CDC), showed that the prevalence rate of Hispanic people vaccinated is among the lowest (Hughes et al., 2021). A high rate of hesitancy and a low prevalence of vaccination may be explained via several reasons. First, a higher confluence of factors associated with COVID-19 vaccination hesitancy in Hispanics (e.g., lower education with a consequent higher vulnerability to myths and misinformation; lower income often indicating a greater perceived barriers for obtaining COVID-19 vaccines; and higher personal experience of discrimination often associated with a greater medical mistrust) could be present (Khubchandani and Macias, 2021). Moreover, some recent documents have also indicated that minority-dominated socially deprived communities in the U.S. were not receiving adequate resources for COVID-19 vaccines or had lower coverage. In this sense, lower allocation is another issues present in Hispanic people that may decrease mass vaccination with COVID-19 vaccines and increase vaccine hesitancy (Khubchandani and Macias, 2021). At the same time, we believe that COVID-19 vaccination hesitancy in Hispanics should not be considered as impossible to overcome and specific interventions for these people (e.g., material written in Spanish rather than in English) should be prepared, with a particular attention to older people and their necessities. However, these findings can be applied only in an U.S. context, whilst the generalization of these findings in other contexts is practically impossible.
We believe that our findings could be important in order to conduct empirical studies in areas with high vaccine unwillingness for better understanding the specific barriers present and, finally for developing tailored interventions for older persons. First, correct education regarding COVID-19 vaccination is an essential step. This intervention could be implemented using accessible and culturally adequate information, and trusted sources specific for older adults. Second, it seems mandatory to reach caregivers and social and health professionals involved in the care of older people, who are in the position of being advocates of vaccinations. Unfortunately, however, they often are not getting themselves the vaccination against COVID-19 (Goldman et al., 2020). Finally, older people can have more frequently than younger counterparts mobility problems and need of assistance to go to the health centers; therefore, administering vaccines at home or in small group settings (e.g., residential facilities) would make it easier and it could decrease the hesitancy to the vaccination.
The findings of our work should be interpreted within its limitations. First, the data collected ranged across different periods of 2020 and 2021 and this could affect the results since in the early 2020 the hesitancy against COVID-19 vaccination was low, but significantly increased thereafter. In one study assessing the willingness to get vaccinated during 2020 the percentage of older people that did not want the vaccine increased from 14.1% during the first semester to 24.0% in October (Daly and Robinson, 2020). Second, information regarding hesitancy were collected using self-administered questionnaires and this could have limited the applicability of our results to people not able to complete them, such as those affected by severe sensory impairments, serious health conditions, or dementia, further under-representing older people or including only the healthier subjects (Batty et al., 2021). Finally, twelve possible eligible articles were not included: even if we tried to reach these authors for having specific data on older people, they unfortunately did not answer to our invitation. However, how these missing data can affect our results is hard to determine.
In conclusion, our systematic review with meta-analysis has reported that hesitancy for COVID-19 vaccination is a relevant problem in older people, particularly in those with a low level of income, education and are of a Hispanic ethnicity. Since older people are among those most affected by the negative consequences of COVID-19, future tailored strategies are needed for increasing the vaccination coverage.
Acknowledgments
We thank the Corresponding Authors of the works included that helped us in the elaborations of this work, indicating the free-accessible databases, such as: https://www.norc.org/, https://www.adp.fdv.uni-lj.si/eng/).
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.arr.2021.101489.
Appendix A. Supplementary material
Supplementary material.
.
References
- Abedin M., Islam M.A., Rahman F.N., Reza H.M., Hossain M.Z., Hossain M.A., Arefin A., Hossain A. Willingness to vaccinate against COVID-19 among Bangladeshi adults: understanding the strategies to optimize vaccination coverage. PLoS One. 2021;16 doi: 10.1371/journal.pone.0250495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Qerem W.A., Jarab A.S. COVID-19 vaccination acceptance and its associated factors among a Middle Eastern Population. Front Public Health. 2021;9 doi: 10.3389/fpubh.2021.632914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alqudeimat Y., Alenezi D., AlHajri B., Alfouzan H., Almokhaizeem Z., Altamimi S., Almansouri W., Alzalzalah S., Ziyab A.H. Acceptance of a COVID-19 vaccine and its related determinants among the general adult population in Kuwait. Med Princ. Pract. 2021;30:262–271. doi: 10.1159/000514636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batty G.D., Deary I.J., Fawns-Ritchie C., Gale C.R., Altschul D. Pre-pandemic cognitive function and COVID-19 vaccine hesitancy: cohort study. Brain Behav. Immun. 2021 doi: 10.1016/j.bbi.2021.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertoncello C., Ferro A., Fonzo M., Zanovello S., Napoletano G., Russo F., Baldo V., Cocchio S. Socioeconomic determinants in vaccine hesitancy and vaccine refusal in Italy. Vaccines. 2020;8:276. doi: 10.3390/vaccines8020276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogart L.M., Ojikutu B.O., Tyagi K., Klein D.J., Mutchler M.G., Dong L., Lawrence S.J., Thomas D.R., Kellman S. COVID-19 related medical mistrust, health impacts, and potential vaccine hesitancy among Black Americans living with HIV. J. Acquir. Immune Defic. Syndr. 2021;86:200. doi: 10.1097/QAI.0000000000002570. (1999) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coustasse A., Kimble C., Maxik K. COVID-19 and vaccine hesitancy: a challenge the United States must overcome. J. Ambul. Care Manag. 2021;44:71–75. doi: 10.1097/JAC.0000000000000360. [DOI] [PubMed] [Google Scholar]
- Daly, M., Robinson, E., 2020. Willingness to vaccinate against COVID-19 in the US: Longitudinal evidence from a nationally representative sample of adults from April-October 2020. medRxiv: the preprint server for health sciences.
- DerSimonian R., Laird N. Meta-analysis in clinical trials. Control. Clin. Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- Domek G.J., O’Leary S.T., Bull S., Bronsert M., Contreras-Roldan I.L., Ventura G.A.B., Kempe A., Asturias E.J. Measuring vaccine hesitancy: field testing the WHO SAGE Working Group on Vaccine Hesitancy survey tool in Guatemala. Vaccine. 2018;36:5273–5281. doi: 10.1016/j.vaccine.2018.07.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duval S., Tweedie R. Trim and fill: a simple funnel‐plot–based method of testing and adjusting for publication bias in meta‐analysis. Biometrics. 2000;56:455–463. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- Egger M., Smith G.D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. Bmj. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gagneux-Brunon A., Detoc M., Bruel S., Tardy B., Rozaire O., Frappe P., Botelho-Nevers E. Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: a cross-sectional survey. J. Hosp. Infect. 2021;108:168–173. doi: 10.1016/j.jhin.2020.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman R.D., Marneni S.R., Seiler M., Brown J.C., Klein E.J., Cotanda C.P., Gelernter R., Yan T.D., Hoeffe J., Davis A.L. Caregivers’ willingness to accept expedited vaccine research during the COVID-19 pandemic: a cross-sectional survey. Clin. Ther. 2020;42:2124–2133. doi: 10.1016/j.clinthera.2020.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins R.B., Charles E., Mehaffey J. Socio-economic status and COVID-19–related cases and fatalities. Public Health. 2020;189:129–134. doi: 10.1016/j.puhe.2020.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes M.M., Wang A., Grossman M.K., Pun E., Whiteman A., Deng L., Hallisey E., Sharpe J.D., Ussery E.N., Stokley S. County-level COVID-19 vaccination coverage and social vulnerability—United States, December 14, 2020–March 1, 2021. Morb. Mortal. Wkly. Rep. 2021;70:431. doi: 10.15585/mmwr.mm7012e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jebril, N., 2020. World Health Organization declared a pandemic public health menace: a systematic review of the coronavirus disease 2019 “COVID-19”, up to 26th March 2020. Available at SSRN 3566298.
- Khubchandani J., Macias Y. COVID-19 vaccination hesitancy in Hispanics and African-Americans: a review and recommendations for practice. Brain Behav. Immun. Health. 2021 doi: 10.1016/j.bbih.2021.100277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kourlaba G., Kourkouni E., Maistreli S., Tsopela C.G., Molocha N.M., Triantafyllou C., Koniordou M., Kopsidas I., Chorianopoulou E., Maroudi-Manta S., Filippou D., Zaoutis T.E. Willingness of Greek general population to get a COVID-19 vaccine. Glob. Health Res. Policy. 2021;6:3. doi: 10.1186/s41256-021-00188-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin C.A., Dayton L., Yi G., Colon B., Kong X. Mask usage, social distancing, racial, and gender correlates of COVID-19 vaccine intentions among adults in the US. PLoS One. 2021;16 doi: 10.1371/journal.pone.0246970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus J.V., Wyka K., Rauh L., Rabin K., Ratzan S., Gostin L.O., Larson H.J., El-Mohandes A. Hesitant or not? The association of age, gender, and education with potential acceptance of a COVID-19 vaccine: a country-level analysis. J. Health Commun. 2020;25:799–807. doi: 10.1080/10810730.2020.1868630. [DOI] [PubMed] [Google Scholar]
- Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J. Clin. Epidemiol. 2009;62:e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- Machida M., Nakamura I., Kojima T., Saito R., Nakaya T., Hanibuchi T., Takamiya T., Odagiri Y., Fukushima N., Kikuchi H., Amagasa S., Watanabe H., Inoue S. Acceptance of a COVID-19 Vaccine in Japan during the COVID-19 Pandemic. Vaccines. 2021;9 doi: 10.3390/vaccines9030210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malesza M., Wittmann E. Acceptance and intake of COVID-19 vaccines among older Germans. J. Clin. Med. 2021;10 doi: 10.3390/jcm10071388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malik A.A., McFadden S.M., Elharake J., Omer S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26 doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliveira B.L.C.Ad, Campos M.A.G., Queiroz R.Cd.S., Souza B.Fd, Santos A.Md, Silva A.A.Md. Prevalence and factors associated with covid-19 vaccine hesitancy in Maranhão, Brazil. Rev. Saúde Pública. 2021;55:12. doi: 10.11606/s1518-8787.2021055003417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onder G., Rezza G., Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. Jama. 2020 doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- Organization, W.H., 2021. COVID-19 weekly epidemiological update, 9 March 2021.
- Petravic L., Arh R., Gabrovec T., Jazbec L., Rupcic N., Staresinic N., Zorman L., Pretnar A., Srakar A., Zwitter M., Slavec A. Factors affecting attitudes towards COVID-19 vaccination: an online survey in Slovenia. Vaccines. 2021;9 doi: 10.3390/vaccines9030247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puri N., Coomes E.A., Haghbayan H., Gunaratne K. Social media and vaccine hesitancy: new updates for the era of COVID-19 and globalized infectious diseases. Hum. Vaccin. Immunother. 2020;16:2586–2593. doi: 10.1080/21645515.2020.1780846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salmon D.A., Dudley M.Z., Brewer J., Kan L., Gerber J.E., Budigan H., Proveaux T.M., Bernier R., Rimal R., Schwartz B. COVID-19 vaccination attitudes, values and intentions among United States adults prior to emergency use authorization. Vaccine. 2021;39:2698–2711. doi: 10.1016/j.vaccine.2021.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troiano G., Nardi A. Vaccine hesitancy in the era of COVID-19. Public Health. 2021 doi: 10.1016/j.puhe.2021.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veronese N., Barbagallo M. Specific approaches to patients affected by dementia and covid-19 in nursing homes: the role of the geriatrician. Ageing Res. Rev. 2021 doi: 10.1016/j.arr.2021.101373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoda T., Katsuyama H. Willingness to receive COVID-19 vaccination in Japan. Vaccines. 2021;9 doi: 10.3390/vaccines9010048. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material.