Abstract
Objective
Investigate the challenges experienced by survivors of critical illness and their caregivers across the transitions of care from intensive care to community, and the potential problem-solving strategies used to navigate these challenges.
Design
Qualitative design - data generation via interviews and data analysis via the Framework Analysis method.
Setting
Patients and caregivers from three continents, identified through the Society of Critical Care Medicine’s THRIVE international collaborative sites (follow-up clinics and peer support groups).
Subjects
Patients and caregivers following critical illness.
Interventions
Nil
Measurements and Main Results
From 86 interviews (66 patients, 20 caregivers), we identified the following major themes: 1. Challenges for patients – Interacting with the health system and gaps in care; Managing others’ expectations of illness and recovery; 2. Challenges for caregivers – Health system shortfalls and inadequate communication; and Lack of support for caregivers. 3. Patient and caregiver-driven problem solving across the transitions of care – Personal attributes, resources, and initiative; Receiving support and helping others; and Acceptance.
Conclusions
Survivors and caregivers experienced a range of challenges across the transitions of care. There were distinct and contrasting themes related to the caregiver experience. Survivors and caregivers used comparable problem-solving strategies to navigate the challenges encountered across the transitions of care.
Keywords: transitions of care, critical care, recovery
INTRODUCTION
Critically ill patients and their caregivers navigate and adjust as they move through the health system. Challenges are especially prominent at the transition points, from the immediate health shock of a critical care admission, to discharge to the ward or rehabilitation program, and then on to return to the community. Challenges encountered may include communications gaps, lapses in medical judgement and empathy, adverse events, loss of rehabilitative gains, and fragmentation of care (1–5). Concurrently, support needs often change across the trajectory of recovery (6, 7).
In the intensive care unit (ICU), patients, families, and clinicians are often inadequately informed about the issues of survivorship following ICU discharge (8). After leaving the hospital, communication gaps between secondary and primary care can exacerbate these challenges and impede recovery. Due to the complexity of their healthcare and related psychosocial issues, lack of comprehensive care in this population can lead to early rehospitalisation (9). Additionally, prolonged weakness, difficulty concentrating, sleep problems, anxiety and depression, may further impede recovery when untreated (10). Beyond hospital discharge, the opportunity for ICU patients and their caregivers to receive help can be limited. Few survivors or caregivers will have access to specialised supports such as follow-up clinics or peer support groups (11), and must rely on primary care (12).
Patients and their caregivers may also adapt well to such challenges. In a single-site study of the post-hospital phase, 63% of survivors had normal resilience, and 9% had high resilience, while only 28% had low resilience (13). Based on the work of Maley and colleagues in critical care survivors, the following definition of resilience can be used where it has been defined as: “a modifiable psychological trait, relates to one’s ability to adapt and adjust ” (14). Attributes of resilience and coping in caregivers of the critically ill may also impact the degree of emotional distress experienced (15–17). These data suggest patients and their caregivers may possess inherent psychological attributes and internal resources they can draw on to help them problem-solve and navigate transitions of care.
The aim of this study was to investigate in an international cohort, the challenges experienced by patients and their caregivers across the transitions of care, and to identify potential problem-solving strategies they used to navigate these challenges.
METHODS
This study was reported using the Consolidated Reporting of Qualitative Research (COREQ) checklist (18).
Setting and ethical approval
This study was conducted across 14 hospital sites in the United States (US), United Kingdom (UK), and Australia who participated in the SCCM Thrive Peer Support Collaborative and/or Clinic Collaborative, described elsewhere (19). Ethical approval was obtained from the institutions of the lead principal investigators (CS, JM, KH), in their respective countries.
Study design
Qualitative study design (Framework Analysis (20)) was used to understand the participants’ experiences of the transitions of care. This design was chosen to understand in their own words, the experiences of patients and caregivers across the arc of care (ICU to post-hospital settings).
Participants, sampling, and recruitment
Participants were screened against the following: i) inclusion criteria - English-speaking patients older than 18 years admitted to the ICU; ii) exclusion criteria - ongoing severe neurological and/or cognitive impairment, or continued inpatient status in a hospital or rehabilitation setting at the time of the study. Purposive sampling was used to promote socio-demographic and geographic diversity in the sample by seeking participants from various international hospital sites, educational levels, and employment statuses. We also sought to understand different recovery trajectories across time and recruited patients at different time-points in the post-hospital phase.
Potential participants were identified and invited to participate in the study by the lead clinicians running the program, if attending a post-ICU program at the respective sites, or on social media. If willing to participate, an interview was arranged with the respective study coordinator in each country, who was not involved in the patient’s care, and verbal consent sought at the time of interview.
Data collection and generation
Data were collected using a semi-structured interview guide (Supplementary Appendix 1). These questions were informed by prior literature in the field, discussion amongst the research team, and underwent independent review by a patient consultant and an expert qualitative researcher. Interviews were completed by four researchers (JM, LB, JJ, EH) who were experienced in qualitative methods, and were known to participants through prior involvement in their clinical care. Interviews were conducted via telephone, were audio-recorded and professionally transcribed verbatim and lasted between 20–60 minutes each.
Data analysis and rigor
Framework analysis was used to analyse the data, with ‘content analysis’ as its methodological orientation (20) (see Supplementary Appendix 2). Qualitative analysis software (Dedoose) was used to develop initial coding. After preliminary analyses were conducted on a third of the transcripts by four experienced coders (KH, EH, TH, NL), the team met to group the data manually and elicit major themes until data saturation was reached. Two separate working analytical frameworks for patient and caregiver data were developed (Supplementary Tables 1 and 2) and remaining data were charted to these matrices with supporting quotes; data were interpreted as a group. We also compared and contrasted themes between the patient and caregiver data. To ensure rigor, regular crosschecking of analyses and data was undertaken by the research team (KH, EH, TH, NL). The research team met weekly during data analysis to discuss issues as they arose.
RESULTS
Eighty-six interviews were completed with 66 patients and 20 caregivers. As shown in Table 1, the majority of participants were from the US, had participated in an ICU recovery program, and were more than two years post-ICU discharge. Due to the sampling approach used, of those participants identified and invited to participate, none were excluded. Patients and caregivers described the initial health shock of critical illness, then recovery and adaptation, as they left hospital and returned to their communities (Fig. 1 Patient and Caregiver Transitions of Care). Caregivers followed a parallel journey to the patient, but in a role of intimate observer, and transitioned from spouse (or other familial relationship) to caregiver, and then returned to a former/altered role as the patient recovered (Fig. 1 Patient and Caregiver Transitions of Care).
TABLE 1.
Participant Demographics
| Demographics | Patients (n = 66) | Caregivers (n = 20) |
|---|---|---|
|
| ||
| Age (yr) median (interquartile range) | 52 (40–62.5) | 52 (46–67) |
|
| ||
| Gender, n (%) male | 26 (39.4) | 3 (15) |
|
| ||
| Patient ICU admission diagnosis, n (%) | ||
| Sepsis | 28 (42.4) | NA |
| Respiratory failure | 15 (22.8) | NA |
| Postgastrointestinal surgery | 5 (7.6) | NA |
| Trauma | 2 (3) | NA |
| Other | 16 (24.2) | NA |
|
| ||
| Ventilated, n (%) | ||
| Yes | 57 (86.4) | NA |
| No | 9 (13.6) | NA |
|
| ||
| Length of time since ICU discharge, n (%) | ||
| < 6 mo | 15 (22.8) | NA |
| 7–11 mo | 9 (13.6) | NA |
| 1–2 yr | 12 (18.2) | NA |
| 2–5 yr | 22 (33.3) | NA |
| > 5 yr | 8 (12.1) | NA |
|
| ||
| Relationship to patient, n (%) | ||
| Spouse/significant other | NA | 10 (50) |
| Parent | NA | 5 (25) |
| Sibling | NA | 3 (15) |
| Child | NA | 2 (10) |
|
| ||
| Nationality, n (%) | ||
| United States | 50 (75.7) | 16 (80) |
| United Kingdom | 13 (19.7) | 2 (10) |
| Australia | 3 (4.6) | 2 (10) |
|
| ||
| Participated in an ICU recovery program, n (%) | ||
| Yes | 52 (79) | 11 (55) |
| No | 14 (21) | 9 (45) |
NA = not applicable.
Fig. 1.

Patient and Caregiver Transitions of Care
The major themes identified within the three study domains were:
Challenges encountered by patients across the transitions of care (mapped to Fig. 1 Patient and Caregiver Transitions of Care) - Interacting with the health system and gaps in care; and Managing others’ expectations of illness and recovery.
Challenges encountered by caregivers across the transitions of care (mapped to Fig. 1 Patient and Caregiver Transitions of Care) – Health system shortfalls and inadequate communication; and Lack of support for caregivers.
Patient and caregiver-driven problem solving across the transition of care (summarised in Fig. 2 Patient and Caregiver Problem-Solving) - Personal attributes, resources, and initiative; Receiving support and helping others; and Acceptance.
Fig. 2.
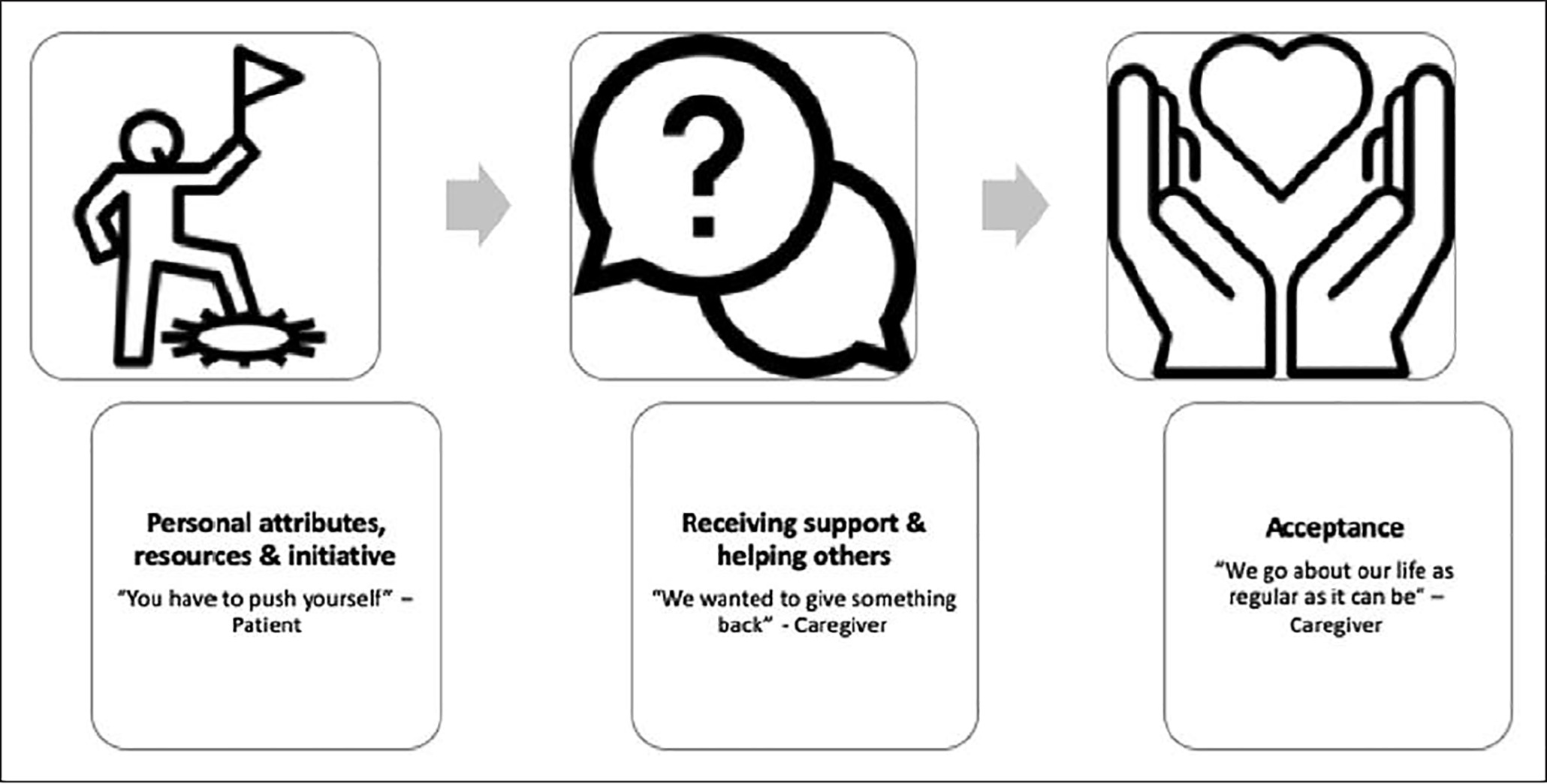
Patient and Caregiver Problem-Solving
1. Challenges encountered by patients across the transitions of care
Patients described challenges when interacting with the health system, and reintegrating with their community. Additional quotes are provided in Supplementary Table 3.
Interacting with the health system and gaps in care.
Patients described that within the hospital, inadequate communication and a lack of empathetic care from clinicians were key issues that caused distress: “I’ve tried not to think about much of the experience because there were so many issues… it was just a nightmare” (Participant 63). The decline in support across the transitions of care was particularly challenging. This stemmed from limited communication and management of expectations for ongoing support – first, when they left ICU for the ward: “we were told we were leaving [ICU] and ‘you’re only a press [of] a button away from assistance’, well that never happened…” (Participant 16). Second, when they left hospital: “There was no support... Because when I left the hospital, nobody called up to say, ‘Hey, how you doing?’” (Participant 10). Third, following hospital discharge, when transitioning to community-based care: “there was such a long, long wait from when I got home till I could get into a rehab session” (Participant 1). Patients also struggled with the lack of understanding about ICU survivorship in the primary care setting: “When I first went to my GP… he had no idea what I’d been through – he just said… you will be right in a couple of weeks, well that wasn’t quite the case…” (Participant 3).
Managing others’ expectations of illness and recovery.
Patients found it difficult to manage how others regarded their illness and post-ICU disability. They felt others could not relate to them that ultimately led to feelings of loneliness and isolation. For some, this lack of understanding occurred within their immediate family: “I’ve gotten to the point where family members are like… ‘This happened, but it’s over, so get over it’ basically” (Participant 59). For others, it occurred within their workplace or social networks: “I do find my life has changed a lot since I’ve been out. I had friends that tried to disown me because they didn’t understand that I was not the same person when I got out of hospital” (Participant 61). This lack of social understanding was tiresome for patients and some actively worked to avoid being in these social situations: “in a way, you get tired of hearing ‘you look good’. So that’s one reason I go to the balcony in the church. Because when it’s over, I can leave, and go right straight outside. I don’t have to congregate with anyone and have to be asked those questions” (Participant 8).
2. Challenges encountered by caregivers across the transitions of care
The following theme of health system shortfalls and inadequate communication was similar to what patients described. However, we found a contrasting theme - lack of support for caregivers. Additional quotes are provided in Supplementary Table 3.
Health system shortfalls and inadequate communication.
Caregivers described shortfalls in care that were notable at times of transition: “like emotional support and information in the hospital, you know, post-ICU when he was recovering on the regular floor… there was nothing in discharge teaching or discharge information…” (Participant 22). Caregivers described a lack of communication and expectation management at some of the key transitions of care: “to let the patient know that once you get out of the hospital, the expectation isn’t that you feel fabulous... To expect depression, to expect anxiety…” (Participant 24). Caregivers highlighted inequities in healthcare – for example, in rural areas that made it difficult for the dyad to access support: “I mean around here you’re not going to find any medical help that’s going to be decent. We’re just so far removed from everything” (Participant 21). Participants also highlighted other inequities in receiving healthcare related to socioeconomic and educational backgrounds: “…people are human beings, and if we lived in a perfect world, everyone would be treated equally, but we don’t.” (Participant 27)
Lack of support for caregivers.
Across the transitions of care, caregivers described a general lack of support for them as individuals to help them as they cared for the patient. For some this was specific to accessing psychological support: “If there’s anything the hospital could do to… maybe open up more counselling, because it’s so hard to get into… the waiting lists are so long” (Participant 2). For others, this was specific to receiving post-hospital help: “…home health is a lot of marketing… you get home and they don’t really help you… they just come in and kind of end up in your home” (Participant 1). This lack of support for caregivers led to feelings of isolation and loneliness following hospital discharge: “Feeling so alone and isolated, that was horrendous for me” (Participant 79).
3. Patient and caregiver-driven problem solving across the transitions of care
Despite these wide-ranging challenges, patients and caregivers employed various problem-solving strategies to help themselves across the transitions of care – from illness to recovery. We identified the following three major themes that were similar across both patient and caregiver data (Fig. 2 Patient and Caregiver Problem-Solving). Further details and supporting quotes are provided in Supplementary Table 4.
Personal attributes, resources and initiative
Patients drew upon their own internal attributes of resilience and will power: “The most successful part of my recovery was just, my determination actually. The fact that I just kept going” (Participant 63). Patients maintained a positive outlook for their recovery, relying on their own internal resources of self-motivation and encouragement to keep propelling themselves forward: “These things don’t come easy. You have to push yourself” (Participant 8). Patients also used straightforward practical solutions to help themselves: “So writing things down, and finding tools that will help me keep up with what’s going on in my life, what day of the week is it, what time is it, those things were very important” (Participant 3). To meet the gaps in care such as mental health support, patients used their initiative to seek out resources to inform and educate themselves, as one explained: “I have different books about anxiety, PTSD” (Participant 59), while others turned to the internet as a primary information source: “I started looking stuff up online because I was so upset with what I was feeling. I was trying to figure out what was going on” (Participant 10).
Receiving support and helping others
Participants relied on their existing social networks for support: I had a couple of my friends coming in and helping me. That really meant a lot to me. I think the emotional thing that people were giving me was important” (Participant 32). Others also described establishing new social support networks, where they described altruistically helping others in their recovery, and highlighted the value of peer support groups: “We thought that if we could give something back, you know, if somebody was struggling like we were, that we could tell them – ‘I can see you and you’re exactly like me, and look at me now, you know this is what I found helpful’…”(Participant 2)
Acceptance
Over time participants accepted and adapted to their post-ICU state: “It was just a matter of accepting his limitation” (Participant 5). Caregivers appeared to adjust and accept their role over time: “I think that as the months went on, I felt a lot more comfortable as a caregiver” (Participant 27). Once the patient recovered, for some caregivers they recalibrated their role: “Him being able to really take care of himself… kind of gave me back myself” (Participant 79).
DISCUSSION
For the first time, in a large international qualitative study, we found several varied challenges survivors and their caregivers navigated across the continuum of care. Additionally, we found survivors and their caregivers were highly adaptable and resilient, and utilised various problem-solving strategies to help themselves, and improve the future care of others.
Our findings are particularly novel as we compared and contrasted patient and caregiver data. We found new and distinctly contrasting themes between patients and caregivers that have not been previously reported in the critical care literature. Contemporary and novel themes were related to inequities in healthcare - the challenges of receiving care in rural settings, and the influence of socioeconomic and educational backgrounds that impacted care. We also found similarities between patient and caregiver data related to their interactions with the health system such as gaps in care and communication issues, consistent with prior international literature (9).
Another unique aspect of our findings was the problem-solving naturally adopted by patients and caregivers. To date, the critical care recovery literature has largely focused on describing the problems and post-ICU impairments experienced by patients and their caregivers. There has been less of a focus on the more positive aspects of recovery including attributes such as resilience, coping, and post-traumatic growth, and how these can be fostered by health systems to support and promote optimal recovery (21, 22). These positive attributes are important to investigate as they can mitigate the negative impacts of post-ICU outcomes such as post-traumatic stress syndrome (9), and inform the design of future interventional trials. Further, from a clinical perspective, problem-solving skills and positive attributes could be focused on and deliberately enhanced in ICU recovery programs – for example, peer support groups are a mechanism through which survivors can share the strategies they used to counteract their challenges and adapt to their post-ICU health state (23–25).
This study adds valuable data to the field by highlighting the dynamic problems across the continuum of care that critical care survivors and their caregivers must navigate and problem-solve. Within the critical care survivorship literature, there are few studies designed to encompass this continuum of care. This study highlights the need for establishing a comprehensive care pathway or bundle of care for ICU survivors and their caregivers in a similar way that other bundles of care have been designed and tested for comparable patient cohorts such as cardiac surgery (26), stroke (27), and cancer (28) patients. Such a care pathway could help clinicians better consider how their own implicit biases affect how they communicate, and more intentionally offer additional supports, particularly to vulnerable ICU patient and caregivers across the transitions of care. Specifically, an ICU care pathway could include functional reconciliation and follow up to ensure impairments are identified and rehabilitated in a standard way, following recommendations from a recent international consensus conference (29). It could also encompass written information to help manage patient and caregiver expectations across the transitions of care, help identify those patients/caregivers who may be at risk (30) and who may require additional supports such as early referral to psychology and/or social work services, provide comprehensive communication between secondary and primary care including possible post-ICU impairments to screen for.
A limitation of this study was that the majority of participants attended some type of recovery program, so likely used this as their frame of reference when describing their experiences. This is not the typical experience of critical illness survivors worldwide given the existence of recovery programs internationally are limited, and therefore our results need to be considered in this context. We also relied on patient report to capture demographic data as we did not have access to their medical records due to the study design. A strength of this research was inclusion of international participants, however there is lack of representation from low-and-middle income countries and we only included English-speaking participants which is a further limitation. It will be important for future studies to investigate transitions of care in low-and-middle income countries as well as the experiences of participants from culturally and linguistically diverse backgrounds. Whilst the majority of patients were from United States, which has a distinctly different health system to the United Kingdom and Australia, we found the themes were universal across participants, irrespective of geographical location. Future research should consider how these data contribute to delayed recovery for patients and caregivers following a critical care admission, as well as investigating the experiences of specific and homogenous ICU sub-populations such as those with sepsis or acute respiratory failure.
CONCLUSION
Patients and caregivers experienced a range of challenges across the transitions of care from ICU to the community. We found patients and caregivers used comparable problem-solving strategies to navigate the challenges encountered across the transitions of care. A care pathway specifically designed to meet the needs of ICU survivors and their caregivers warrants investigation. This may help mitigate challenges and leverage the inherent problem-solving skills of survivors and their caregivers.
Supplementary Material
Take Home Message.
Patients and caregivers experienced a range of challenges across the transitions of care from ICU to the community and used comparable problem-solving strategies. A care pathway specifically designed to meet the needs of ICU survivors and their caregivers warrants investigation.
Acknowledgements:
We would like to acknowledge and thank the wider THRIVE steering group within the Society of Critical Care Medicine. The authors would like to acknowledge and thank the following individuals who collectively contributed to the review of the original grant application: Dr. Daniela Lamas, Ms. Kate Cranwell, Dr. Craig French and Dr. Carol Hodgson.
Conflicts of interest and Sources of Funding: K Haines, J McPeake, C Sevin, L Boehm, and T Quasim received funding from the Society of Critical Care Medicine to undertake this work. L Boehm is funded by National Institutes of Health/National Heart, Lung, and Blood Institute (K12 HL137943) as is T J Iwashyna (K12 HL138039). No conflicts of interest declared by other authors. J McPeake is funded by a THIS.Institute Post-Doctoral Fellowship (PD-2019–02-16).
Role of the funder: This study was funded by the Society of Critical Care Medicine. The scientific questions, analytical framework, data collection, and analyses were undertaken independently of the funder.
Disclaimer: This does not necessarily represent the views of the U.S. government or Department of Veterans Affairs.
Contributor Information
Kimberley J. Haines, Department of Physiotherapy, Western Health, Sunshine Hospital, 176 Furlong Road, St Albans, Melbourne, Victoria 3021, Australia.; Centre for Integrated Critical Care, School of Medicine, The University of Melbourne, Victoria, Australia School of Physiotherapy, The University of Melbourne, Victoria, Australia.
Elizabeth Hibbert, Department of Physiotherapy, Western Health, Melbourne, Victoria, Australia.
Nina Leggett, Department of Physiotherapy, Western Health, Melbourne, Victoria, Australia.
Leanne M. Boehm, School of Nursing, Vanderbilt University, Nashville, Tennessee, US.
Tarli Hall, Department of Physiotherapy, Western Health, Melbourne, Victoria, Australia.
Rita N Bakhru, Wake Forest University School of Medicine, Department of Internal Medicine, Section of Pulmonary, Critical Care, Allergy and Immunology, Winston Salem, North Carolina, US.
Anthony J Bastin, Department of Peri-operative Medicine, St Bartholomew’s Hospital, Barts Health NHS Trust, London, UK.
Brad W Butcher, Department of Critical Care Medicine, University of Pittsburgh Medical Center, Pittsburgh, US.
Tammy L Eaton, University of Pittsburgh Medical Center (UPMC), Department of Critical Care Medicine, Pittsburgh, PA, USA; University of Pittsburgh, School of Nursing, Pittsburgh, PA, USA.
Wendy Harris, University College London Hospitals NHS Foundation Trust, London, UK.
Aluko A Hope, Division of Critical Care Medicine, Albert Einstein College of Medicine of Yeshiva University, New York, US.
James Jackson, Vanderbilt University Medical Center, Tennessee, US.
Annie Johnson, Pulmonary and Critical Care Medicine, Mayo Clinic, Rochester, Minnesota, US.
Janet A. Kloos, University Hospitals Cleveland Medical Center, Cleveland, Ohio.
Karen A Korzick, Geisinger Medical Center, Pulmonary and Critical Care Medicine, Pennsylvania, US.
Pamela Mactavish, Glasgow Royal Infirmary, NHS Greater Glasgow and Clyde, Scotland, UK
Joel Meyer, Guy’s & St Thomas’ NHS Foundation Trust, London, UK.
Ashley Montgomery-Yates, Division of Pulmonary, Critical Care and Sleep Medicine, University of Kentucky, Kentucky, US.
Tara Quasim, Glasgow Royal Infirmary, NHS Greater Glasgow and Clyde, Scotland, UK; School of Medicine, Dentistry and Nursing, University of Glasgow, Scotland, UK.
Andrew Slack, Guy’s & St Thomas’ NHS Foundation Trust, London, UK.
Dorothy Wade, University College London Hospitals NHS Foundation Trust, London, UK.
Mary Still, Emory University Hospital (Emory Healthcare), Georgia, US.
Giora Netzer, Division of Pulmonary and Critical Care Medicine, University of Maryland School of Medicine, Maryland, US; Department of Epidemiology and Public Health, University of Maryland School of Medicine, Maryland, US.
Ramona O Hopkins, Department of Medicine, Pulmonary and Critical Care Division, Intermountain Medical Center, Murray, Utah, US; Center for Humanizing Critical Care, Intermountain Health Care, Murray, Utah, US; Psychology Department and Neuroscience Center, Brigham Young University, Provo, Utah, US.
Theodore J Iwashyna, Department of Medicine, Division of Pulmonary & Critical Care, University of Michigan, Ann Arbor, Michigan, US; Center for Clinical Management Research, VA Ann Arbor Healthcare System, Ann Arbor, Michigan, US.
Mark E Mikkelsen, Division of Pulmonary, Allergy, and Critical Care Medicine, Hospital of the University of Pennsylvania, Philadelphia, US.
Joanne McPeake, Glasgow Royal Infirmary, NHS Greater Glasgow and Clyde, Scotland, UK; School of Medicine, Dentistry and Nursing, University of Glasgow, Scotland, UK.
Carla M. Sevin, Department of Medicine, Division of Allergy, Pulmonary, and Critical Care Medicine, Vanderbilt University Medical Center, Nashville, Tennessee, US.
References
- 1.Kripalani S, Jackson AT, Schnipper JL, Coleman EA: Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med 2007; 2(5):314–323 [DOI] [PubMed] [Google Scholar]
- 2.Haggstrom M, Backstrom B: Organizing safe transitions from intensive care. Nurs Res Pract 2014; 2014:175314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hosein FS, Bobrovitz N, Berthelot S, Zygun D, et al. : A systematic review of tools for predicting severe adverse events following patient discharge from intensive care units. Crit Care 2013; 17(3):R102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pandullo SM, Spilman SK, Smith JA, Kingery LK, et al. : Time for critically ill patients to regain mobility after early mobilization in the intensive care unit and transition to a general inpatient floor. J Crit Care 2015; 30(6):1238–1242 [DOI] [PubMed] [Google Scholar]
- 5.MacTavish P, Quasim T, Shaw M, Devine H, et al. : Impact of a pharmacist intervention at an intensive care rehabilitation clinic. BMJ Open Qual 2019; 8(3):e000580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Czerwonka AI, Herridge MS, Chan L, Chu LM, et al. : Changing support needs of survivors of complex critical illness and their family caregivers across the care continuum: a qualitative pilot study of Towards RECOVER. J Crit Care 2015; 30(2):242–249 [DOI] [PubMed] [Google Scholar]
- 7.Amar-Dolan LG, Horn MH, O’Connell B, Parsons SK, et al. : “This Is How Hard It Is”. Family Experience of Hospital-to-Home Transition with a Tracheostomy. Ann Am Thorac Soc 2020; 17(7):860–868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Govindan S, Iwashyna TJ, Watson SR, Hyzy RC, et al. : Issues of survivorship are rarely addressed during intensive care unit stays. Baseline results from a statewide quality improvement collaborative. Ann Am Thorac Soc 2014; 11(4):587–591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Donaghy E, Salisbury L, Lone NI, Lee R, et al. : Unplanned early hospital readmission among critical care survivors: a mixed methods study of patients and carers. BMJ Qual Saf 2018; 27(11):915–927 [DOI] [PubMed] [Google Scholar]
- 10.Sevin CM, Bloom SL, Jackson JC, Wang L, et al. : Comprehensive care of ICU survivors: Development and implementation of an ICU recovery center. J Crit Care 2018; 46:141–148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haines KJ, McPeake J, Hibbert E, Boehm LM, et al. : Enablers and Barriers to Implementing ICU Follow-Up Clinics and Peer Support Groups Following Critical Illness: The Thrive Collaboratives. Crit Care Med 2019; 47(9):1194–1200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Admon AJ, Tipirneni R, Prescott HC: A framework for improving post-critical illness recovery through primary care. Lancet Respir Med 2019; 7(7):562–564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maley JH, Brewster I, Mayoral I, Siruckova R, et al. : Resilience in Survivors of Critical Illness in the Context of the Survivors’ Experience and Recovery. Ann Am Thorac Soc 2016; 13(8):1351–1360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Charney DS: Psychobiological mechanisms of resilience and vulnerability: implications for successful adaptation to extreme stress. Am J Psychiatry 2004; 161(2):195–216 [DOI] [PubMed] [Google Scholar]
- 15.Komachi MHK K: Association between resilience, acute stress symptoms and characteristics of family members of patients at early admission to the intensive care unit. Mental Health & Prevention 2018; 9:34–41 [Google Scholar]
- 16.Meyers EE, Shaffer KM, Gates M, Lin A, et al. : Baseline Resilience and Posttraumatic Symptoms in Dyads of Neurocritical Patients and Their Informal Caregivers: A Prospective Dyadic Analysis. Psychosomatics 2020; 61(2):135–144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shaffer KM, Riklin E, Jacobs JM, Rosand J, et al. : Psychosocial resiliency is associated with lower emotional distress among dyads of patients and their informal caregivers in the neuroscience intensive care unit. J Crit Care 2016; 36:154–159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tong A, Sainsbury P, Craig J: Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. International journal for quality in health care : journal of the International Society for Quality in Health Care / ISQua 2007; 19(6):349–357 [DOI] [PubMed] [Google Scholar]
- 19.Haines KJ, Sevin CM, Hibbert E, Boehm LM, et al. : Key mechanisms by which post-ICU activities can improve in-ICU care: results of the international THRIVE collaboratives. Intensive Care Med 2019; 45(7):939–947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gale NK, Heath G, Cameron E, Rashid S, et al. : Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013; 13:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maley JH, Mikkelsen ME: Sepsis survivorship: how can we promote a culture of resilience? Crit Care Med 2015; 43(2):479–481 [DOI] [PubMed] [Google Scholar]
- 22.Kross EK, Hough CL: Broken Wings and Resilience after Critical Illness. Ann Am Thorac Soc 2016; 13(8):1219–1220 [DOI] [PubMed] [Google Scholar]
- 23.Haines KJ, Beesley SJ, Hopkins RO, McPeake J, et al. : Peer Support in Critical Care: A Systematic Review. Crit Care Med 2018; 46(9):1522–1531 [DOI] [PubMed] [Google Scholar]
- 24.Mikkelsen ME, Jackson JC, Hopkins RO, Thompson C, et al. : Peer Support as a Novel Strategy to Mitigate Post-Intensive Care Syndrome. AACN Adv Crit Care 2016; 27(2):221–229 [DOI] [PubMed] [Google Scholar]
- 25.McPeake J, Hirshberg EL, Christie LM, Drumright K, et al. : Models of Peer Support to Remediate Post-Intensive Care Syndrome: A Report Developed by the Society of Critical Care Medicine Thrive International Peer Support Collaborative. Crit Care Med 2019; 47(1):e21–e27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grant MC, Isada T, Ruzankin P, Whitman G, et al. : Results from an enhanced recovery program for cardiac surgery. J Thorac Cardiovasc Surg 2020; 159(4):1393–1402 e1397 [DOI] [PubMed] [Google Scholar]
- 27.Turner M, Barber M, Dodds H, Murphy D, et al. : Implementing a simple care bundle is associated with improved outcomes in a national cohort of patients with ischemic stroke. Stroke 2015; 46(4):1065–1070 [DOI] [PubMed] [Google Scholar]
- 28.Carey I, Shouls S, Bristowe K, Morris M, et al. : Improving care for patients whose recovery is uncertain. The AMBER care bundle: design and implementation. BMJ Support Palliat Care 2015; 5(1):12–18 [DOI] [PubMed] [Google Scholar]
- 29.Mikkelsen ME, Still M, Anderson BJ, Bienvenu OJ, et al. : Society of Critical Care Medicine’s International Consensus Conference on Prediction and Identification of Long-Term Impairments After Critical Illness. Crit Care Med 2020; 48(11):1670–1679 [DOI] [PubMed] [Google Scholar]
- 30.Haines KJ, Hibbert E, McPeake J, Anderson BJ, et al. : Prediction Models for Physical, Cognitive, and Mental Health Impairments After Critical Illness: A Systematic Review and Critical Appraisal. Crit Care Med 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


