Abstract
Background and Aims
Exertional heatstroke (EHS) is associated with strenuous physical activity in hot environments. The present study aimed to investigate dynamic changes of hepatic function indices in EHS patients and determine risk factors for death.
Methods
This single-center retrospective cohort study considered all patients with EHS admitted to the intensive care unit at the General Hospital of Southern Theater Command of PLA from October 2008 to May 2019. Data on general characteristics, organ function parameters, and the 90-day outcome of enrolled patients were collected. Hepatic indices were collected dynamically, and patients with acute hepatic injury (AHI) were identified by plasma total bilirubin (TBIL) ≥34.2 µmol/L and an international normalized ratio ≥1.5, or with any grade of hepatic encephalopathy.
Results
In patients who survived, TBIL, alanine aminotransferase and aspartate aminotransferase were increased at 24 h, peaked at 2–3 days, and began to decrease at 5 days. In non-survivors, TBIL continuously increased post-admission. The area under the receiver operating characteristic curve for the prediction of mortality based on sequential organ failure assessment (SOFA) scores was 89.8%, and the optimal cutoff value was 7.5. Myocardial injury and infection were identified as independent risk factors for death in EHS patients with AHI.
Conclusions
In EHS patients, hepatic dysfunction usually occurred within 24 h. Patients with AHI had more severe clinical conditions, and significantly increased 90-day mortality rates. SOFA scores over 7.5, complicated with myocardial injury or infection, were found to be risk factors for death in EHS patients with AHI.
Keywords: Exertional heatstroke, Acute hepatic injury, Mortality, TBIL, SOFA
Introduction
Heatstroke is a life-threatening condition involving a significant elevation of core body temperature with central nervous system dysfunction, and includes symptoms such as combativeness, delirium, seizures, or even a comatose state.1,2 It has been reported that at least 3,332 deaths can be attributed to heatstroke between the years of 2006 to 2010 in the USA.3 As global warming worsens, the morbidity of heatstroke has increased, and it has been predicted that heatstroke-related deaths could increase to nearly 2.5 times the current annual baseline by 2050.4 Based on the underlying cause, heatstroke can be classified as either classical heatstroke (CHS) or exertional heatstroke (EHS). In both types, the increased core body temperature is attributed to excessive heat accumulation. CHS involves exposure to heat from the environment with poor heat dissipation, whereas EHS is associated with strenuous physical activity in hot environments and excessive production of metabolic heat that overwhelms physiological heat loss.5 It is still unclear whether the different mechanisms of initiation result in unique pathophysiological disease processes, but organ dysfunction may differ between these two types of heatstroke patients. EHS is usually observed in young, healthy men, most of whom have few underlying diseases. However, the incidence rate of hepatocellular insufficiency in EHS patients is higher compared to that in CHS patients.1,6 For EHS patients with severe acute liver failure, the hepatic injury due to EHS can result in death that occurs approximately 1 week after the onset of heatstroke, unless a liver transplant is performed.7,8
EHS remains a major problem for individuals who regularly meet strenuous physical demands, such as athletes, firefighters, and agricultural workers. The current knowledge regarding EHS patients complicated by acute hepatic injury (AHI) is limited. In the present study, the clinical and prognostic data of heatstroke patients admitted to the intensive care unit (ICU) at a single center in China over a 10-year period were retrospectively collected. The aim was to investigate the dynamic changes of hepatic function indices in EHS patients and determine the risk factors for death in these patients.
Methods
Study design and participants
Patients diagnosed with EHS in the ICU of the General Hospital of Southern Theater Command in China from October 2008 to May 2019 were considered for inclusion. The inclusion criteria9 consisted of 1) ≥ 18 years of age, and 2) met the diagnostic criteria of EHS. These diagnostic criteria included a history of strenuous activity (with or without exposure to hot and humid weather), concurrent hyperthermia (central temperature above 40°C), and neurological dysfunction (such as delirium, cognitive disorders, or disturbed consciousness). The exclusion criteria consisted of 1) existing irreversible underlying diseases affecting mortality, and 2) pregnant or breastfeeding women. The study was approved by the Research Ethics Commission of General Hospital of Southern Theater Command of PLA and the requirement for informed consent was waived by the Ethics Commission.
Research procedure
Patient characteristics, organ function parameters, and 90-day outcomes for all enrolled patients were collected. Scores according to the Acute Physiology and Chronic Health Evaluation II (APACHE II), the sequential organ failure assessment (SOFA), and the Glasgow coma scale (GCS) were also collected. The dynamic changes to hepatic indices, including total bilirubin (TBIL), alanine transaminase (ALT), aspartate transaminase (AST), and the international normalized ratio (INR) were evaluated. The time points included admission and 24 h, 2 d, 3 d, 5 d and 7 d after admission. Patients with AHI were identified by plasma levels of TBIL ≥34.2 µmol/L and an INR ≥1.5, or with any grade of hepatic encephalopathy. Myocardial injury was defined by plasma cardiac troponin I >0.2 µg/mL, and kidney injury was defined by serum creatinine >176 µmol/L. Rhabdomyolysis was defined by creatine kinase (CK) >1,000 IU, and patients with procalcitonin (PCT) >2 ng/mL and a white blood cell (WBC) count >10 × 109/L were considered to have an infection. Lymphopenia was defined by a lymphocyte count <0.8 × 109/L. Patients with a GCS score <8 were considered to have a central nervous system (CNS) disorder.1 The primary outcome was 90-day mortality, and the secondary outcome was the ICU length of stay.
Statistical analysis
Categorical data were summarized as numbers and percentages, and inter-group comparisons were performed using either Mann-Whitney U, χ2 or Fisher’s exact tests. Continuous variables were expressed as the median with interquartile range (IQR) and analyzed using a Wilcoxon rank-sum test, since most continuous variables did not show a Gaussian distribution. Kaplan-Meier survival curves and the log-rank test were used for survival analysis. To determine the independent risk factors of 90-day mortality in severe heatstroke patients with AHI, the Cox proportional hazards model was used. Significant indicators were identified using single-factor analysis, and those with a p-value <0.1 were included in the multifactor Cox regression model. The odds ratio (OR) and 95% confidence interval (CI) levels were presented. Statistical analysis was performed using R, version 3.4.0. A two-tailed p-value <0.05 was considered statistically significant.
Results
Dynamic changes of hepatic function indices in patients with EHS: Comparison of survivors and non-survivors
Data from a total of 189 patients were collected. Three cases were excluded due to missing data, and 186 cases were included for analysis. All 186 patients were male, with a median age of 21 years (IQR: 19–27) and without any underlying diseases prior to the onset of heatstroke. At admission, the concentration of TBIL in survivors was normal, but TBIL in non-survivors was slightly increased (Table 1). In patients who survived, TBIL was increased at 24 h, reached a peak between 2–3 days, and began to decrease after day 5. The concentrations of ALT and AST also showed similar changes to TBIL. In non-survivors, the levels of TBIL continuously increased following admission. ALT and AST levels were remarkably increased at 24 h until day 3 (Table 1). Though ALT and AST also decreased 5 days after admission, this did not indicate that the liver injury was alleviated; the decreased ALT and AST may have been due to considerable hepatocyte death. In both survivors and non-survivors, INRs increased immediately after the onset of heatstroke. INRs began to decrease after 24 h in the survival group, but remained high in the non-survival group. These results indicate that if hepatic function indices of an EHS patient are slightly increased between 24 h and 3 days following the onset of heatstroke, and the serum levels of TBIL continuously increase, the patient may have a higher risk of mortality.
Table 1. Dynamic changes of the hepatic function indexes in the survivor and non-survivor patients with EHS.
| Overall (n=186) | Survivor (n=164) | Non-survivor (n=22) | p | |
|---|---|---|---|---|
| TBIL in µmol/L | ||||
| Ad | 15.85 [10.10, 29.40] | 14.75 [9.80, 25.47] | 29.90 [14.98, 118.08] | 0.002 |
| 24 h | 27.10 [15.45, 55.65] | 23.70 [15.07, 47.85] | 95.60 [53.53, 176.45] | <0.001 |
| 2 d | 36.65 [17.20, 87.28] | 28.90 [15.70, 55.70] | 176.00 [96.05, 198.20] | <0.001 |
| 3 d | 32.60 [17.60, 97.10] | 24.50 [16.40, 59.75] | 233.45 [166.45, 373.32] | <0.001 |
| 5 d | 23.85 [10.20, 83.05] | 18.90 [9.80, 36.10] | 390.30 [328.10, 422.00] | <0.001 |
| 7 d | 20.90 [12.20, 73.60] | 16.10 [9.70, 28.85] | 400.20 [251.33, 424.70] | <0.001 |
| ALT in U/L | ||||
| Ad | 34.50 [20.00, 222.75] | 32.00 [19.00, 149.50] | 170.50 [61.50, 1,648.25] | <0.001 |
| 24 h | 234.50 [56.25, 956.25] | 174.50 [47.25, 652.00] | 1,530.00 [792.75, 2,649.50] | <0.001 |
| 2 d | 383.00 [134.00, 1,389.50] | 355.00 [134.00, 1,112.50] | 1,660.00 [460.00, 3,474.00] | 0.017 |
| 3 d | 468.00 [164.25, 1,431.00] | 407.50 [144.75, 1,094.75] | 2,573.50 [1,228.50, 4,911.50] | <0.001 |
| 5 d | 373.50 [129.00, 666.00] | 348.00 [110.00, 609.00] | 488.00 [370.50, 870.50] | 0.077 |
| 7 d | 192.00 [106.00, 309.00] | 205.00 [94.50, 312.00] | 148.50 [115.75, 217.50] | 0.726 |
| AST in U/L | ||||
| Ad | 66.50 [34.75, 228.00] | 62.00 [33.50, 163.50] | 356.00 [110.00, 1,645.00] | <0.001 |
| 24 h | 214.00 [60.00, 751.75] | 166.00 [57.00, 559.00] | 2,545.00 [631.00, 5,690.00] | <0.001 |
| 2 d | 278.00 [91.50, 947.50] | 250.00 [89.00, 625.00] | 2,635.00 [421.75, 5,159.00] | <0.001 |
| 3 d | 183.00 [70.50, 568.50] | 162.00 [66.50, 462.00] | 1,629.50 [359.50, 5,276.75] | 0.001 |
| 5 d | 118.50 [59.00, 219.00] | 116.00 [56.00, 190.00] | 220.00 [101.00, 355.00] | 0.058 |
| 7 d | 67.50 [39.25, 101.50] | 58.50 [34.50, 80.75] | 102.50 [75.00, 126.50] | 0.003 |
| INR | ||||
| Ad | 1.29 [1.09, 1.76] | 1.24 [1.09, 1.47] | 3.22 [1.86, 4.82] | <0.001 |
| 24 h | 1.29 [1.09, 1.70] | 1.19 [1.07, 1.54] | 2.76 [2.20, 3.28] | <0.001 |
| 2 d | 1.14 [1.04, 1.65] | 1.10 [1.02, 1.32] | 2.82 [2.04, 3.59] | <0.001 |
| 3 d | 1.05 [0.97, 1.70] | 1.02 [0.96, 1.21] | 3.10 [2.07, 3.53] | <0.001 |
| 5 d | 1.01 [0.93, 1.21] | 0.98 [0.93, 1.11] | 3.02 [2.08, 4.04] | <0.001 |
| 7 d | 1.07 [0.99, 1.33] | 1.03 [0.98, 1.11] | 2.38 [1.53, 2.57] | <0.001 |
d, day.
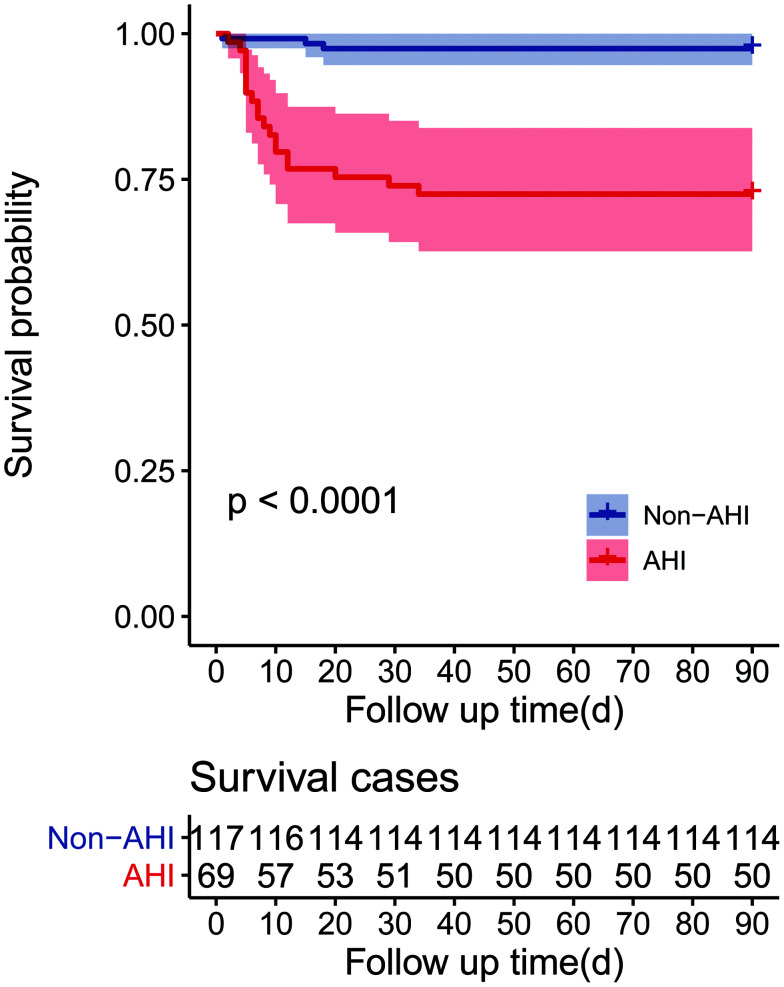
Characteristics and outcomes of EHS patients: Comparison of patients with and without AHI
To further investigate the characteristics of patients with AHI, all patients were divided into either the AHI group or non-AHI group. Among the 186 cases, 69 showed increased TBIL (≥34.2 µmol/L) and INR (≥1.5) and were placed in the AHI group (Table 2). Compared with the non-AHI group, patients in the AHI group showed increased WBC and neutrophil counts, and decreased lymphocyte and platelet counts. In addition, other organ dysfunction indices were also increased in the AHI group, including kidney (urea nitrogen, serum creatinine), muscle (rhabdomyolysis; creatine kinase (CK), CK-Mb), and cardiac (CTNI) injuries. Patients in the AHI group also showed decreased GCS, and increased APACHE II and SOFA scores compared to the non-AHI group. In addition, patients with AHI had increased ICU length of stays and 90-day mortality rates (Table 3). The 90-day mortality of EHS patients with AHI was 27.5% (19/69) but was only 2.6% (3/117) for patients without AHI. The survival times of EHS patients with AHI were also significantly lower compared to those without AHI (Fig. 1).
Table 2. Comparison of the characteristics between the EHS patients in the non-AHI group and AHI group.
| Overall (n=186) | Non-AHI (n=117) | AHI (n=69) | p | |
|---|---|---|---|---|
| Age | 21.00 [19.00, 27.00] | 20.00 [19.00, 27.00] | 23.00 [19.00, 27.00] | 0.263 |
| WBC, ×109/L | 11.34 [8.72, 14.62] | 10.39 [8.61, 14.25] | 12.13 [9.04, 15.82] | 0.057 |
| Neutrophil, ×109/L | 8.86 [6.54, 12.44] | 8.26 [5.80, 11.41] | 10.14 [7.42, 13.22] | 0.003 |
| Lymphocyte, ×109/L | 1.11 [0.58, 1.89] | 1.35 [0.79, 2.12] | 0.73 [0.40, 1.63] | <0.001 |
| Monocyte, ×109/L | 0.68 [0.38, 0.99] | 0.68 [0.40, 0.97] | 0.66 [0.35, 1.00] | 0.581 |
| PLT, ×109/L | 165.0 [82.00, 219.0] | 185.5 [148.8, 232.25] | 80.00 [35.00, 132.0] | <0.001 |
| BUN in mmol/L | 5.75 [4.50, 7.60] | 5.20 [4.20, 6.50] | 6.80 [5.40, 8.70] | <0.001 |
| SCR in μmol/L | 127.5 [92.00, 162.3] | 107.0 [82.00, 137.0] | 159.0 [128.0, 201.0] | <0.001 |
| CK in U/L | 904.0 [346.75, 2,537.0] | 572.0 [244.0, 1,810.0] | 1,452.0 [853.0, 4,573.0] | <0.001 |
| PT in s | 15.90 [14.10, 20.58] | 14.70 [13.70, 16.10] | 23.40 [18.80, 35.00] | <0.001 |
| APTT in s | 38.95 [33.52, 49.45] | 36.10 [32.60, 40.90] | 50.60 [39.20, 91.20] | <0.001 |
| Fib in g/L | 2.50 [2.00, 2.80] | 2.60 [2.30, 3.10] | 2.00 [1.58, 2.60] | <0.001 |
| D.D in mg/L | 1.86 [0.51, 7.00] | 0.70 [0.36, 2.16] | 9.49 [3.51, 14.55] | <0.001 |
| CK-Mb in ng/mL | 469.40[128.9, 1,000.0] | 239.1 [64.75, 594.5] | 1,000.0 [381.5, 1,000.0] | <0.001 |
| CTNI in ng/mL | 110.00 [21.40, 432.45] | 50.00 [10.00, 143.22] | 410.0 [125.90, 1,407.5] | <0.001 |
| CRP in mg/dL | 3.30 [1.48, 5.98] | 3.18 [0.67, 6.86] | 3.38 [3.14, 5.27] | 0.3 |
| PCT in ng/mL | 1.70 [0.76, 4.14] | 1.43 [0.56, 3.97] | 2.05 [1.08, 4.69] | 0.083 |
| GCS | 12.00 [7.00, 14.00] | 12.00 [9.00, 14.00] | 8.00 [6.00, 13.00] | 0.005 |
| SOFA score | 3.00 [2.00, 6.00] | 3.00 [2.00, 4.00] | 6.00 [4.00, 9.00] | <0.001 |
| APACHE II score | 10.50 [8.00, 15.75] | 9.00 [7.00, 13.00] | 15.00 [10.00, 21.00] | <0.001 |
APACHE, acute physiology and chronic health evaluation; APTT, activated partial thromboplastin time; BUN, blood urea nitrogen; CK, creatine kinase; CK-Mb, creatine kinase-Mb; CTNI, cardiac troponin I; CRP, C-reactive protein; D.D, D-dimer; GCS, glasgow coma scale; PCT, procalcitonin; PLT, platelets; PT, prothrombin time; SOFA, sequential organ failure assessment; SCR, serum creatinine; WBC, white blood cell.
Table 3. Comparison of the outcome between the EHS patients in Non-AHI group and AHI group.
| Overall (n=186) | Non-AHI (n=117) | AHI (n=69) | p | |
|---|---|---|---|---|
| ICU time in days | 5.00 [3.00, 9.00] | 4.00 [3.00, 7.00] | 8.00 [5.00, 14.00] | <0.001 |
| Outcome, % | <0.001 | |||
| Survive | 164 (88.2) | 114 (97.4) | 50 (72.5) | |
| Death | 22 (11.8) | 3 (2.6) | 19 (27.5) |
Fig. 1. Survival curves of 90-day mortality rate in the AHI group and non-AHI group.
Risk factors for EHS patients with AHI
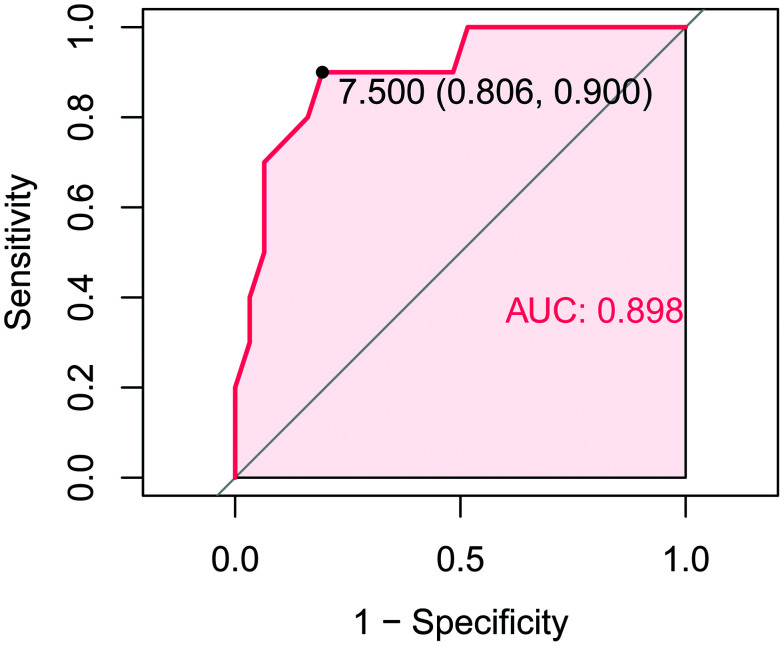
To further determine the risk factors for death in EHS patients with AHI, the organ function indices of the survivors and non-survivors were compared (Table 4). The non-survivors had more severe disease conditions compared to survivors, as evidenced by higher levels of serum creatinine, CK, CTNI, PCT etc. at the time of admission. The non-survivors also had higher SOFA scores. The area under the receiver operating characteristic curve for the prediction of mortality based on the SOFA scores at the time of admission was 89.8%, and the optimal cutoff value was 7.5 (sensitivity of 90.0%, specificity of 80.6%; Fig. 2). Among the patients in the AHI group, 44 cases had myocardial injuries, 32 cases had injury to the kidney, 57 cases were experiencing rhabdomyolysis, 18 cases had a CNS disorder, 45 cases had an infection, and 54 cases showed signs of lymphopenia. Single variable analysis showed that complications due to myocardial injuries, a CNS disorder or infection were risk factors for death in patients with AHI (Table 5). The ORs were 13.10 (95% CI: 1.74, 98.26; p=0.012), 2.86 (95% CI: 1.15, 6.96; p=0.024) and 6.14 (95% CI: 1.42, 26.62; p=0.025), respectively. In the multi-variate analysis, myocardial injury and infection were found to be independent risk factors for death in EHS patients with AHI, with ORs of 12.169 (95% CI: 1.526, 94.806; p=0.023) and 5.637 (95% CI: 1.219, 26.064; p=0.027), respectively.
Table 4. Comparison of the characteristics between the survivors and non-survivors in the AHI group.
| Overall (n=69) | Survivor (n=50) | Non-survivor (n=19) | p | |
|---|---|---|---|---|
| Age | 23.00 [19.00, 27.00] | 23.00 [20.00, 27.00] | 21.00 [18.00, 23.50] | 0.103 |
| WBC, ×109/L | 12.13 [9.04, 15.82] | 12.22 [9.37, 15.71] | 10.56 [8.46, 15.48] | 0.648 |
| Neutrophil, ×109/L | 10.14 [7.42, 13.22] | 10.61 [7.95, 13.71] | 8.86 [6.38, 13.18] | 0.323 |
| Lymphocyte, ×109/L | 0.73 [0.40, 1.63] | 0.73 [0.51, 1.55] | 0.67 [0.33, 2.81] | 0.909 |
| Monocyte, ×109/L | 0.66 [0.35, 1.00] | 0.64 [0.36, 1.00] | 0.73 [0.26, 0.90] | 0.92 |
| PLT, ×109/L | 80.00 [35.00, 132.00] | 85.50 [42.25, 167.00] | 72.00 [29.00, 89.00] | 0.097 |
| BUN in mmol/L | 6.80 [5.40, 8.70] | 6.55 [5.40, 8.10] | 8.10 [6.30, 9.25] | 0.209 |
| SCR, μmol/L | 159.00 [128.00, 201.00] | 146.00 [125.50, 171.50] | 228.00 [189.00, 280.00] | <0.001 |
| CK in U/L | 1,452.0 [853.00, 4,573.0] | 1,278.0 [803.00, 3,769.0] | 3,220.0 [1,014.0, 7,931.5] | 0.076 |
| PT in s | 23.40 [18.80, 35.00] | 21.25 [16.33, 26.90] | 37.50 [25.70, 45.00] | <0.001 |
| APTT in s | 50.60 [39.20, 91.20] | 44.90 [37.68, 68.18] | 91.20 [77.35, 122.85] | <0.001 |
| Fib in g/L | 2.00 [1.58, 2.60] | 2.20 [1.70, 2.60] | 1.30 [0.90, 1.90] | 0.001 |
| D.D in mg/L | 9.49 [3.51, 14.55] | 5.32 [1.61, 13.06] | 10.27 [10.00, 20.00] | 0.001 |
| CK-Mb in ng/mL | 1,000.0 [381.48, 1,000.0] | 789.00 [264.90, 1,000.0] | 1,000.0 [967.55, 1,000.0] | 0.088 |
| CTNI in ng/mL | 410.00 [125.90, 1,407.50] | 230.00 [100.00, 699.90] | 1,530.0 [952.80, 2,930.0] | <0.001 |
| CRP in mg/dL | 3.38 [3.14, 5.27] | 3.37 [2.13, 5.37] | 3.38 [3.30, 3.58] | 0.668 |
| PCT in ng/mL | 2.05 [1.08, 4.69] | 2.02 [0.97, 4.08] | 2.95 [1.46, 5.81] | 0.263 |
| GCS | 8.00 [6.00, 13.00] | 10.00 [6.00, 14.00] | 5.50 [3.00, 7.00] | 0.003 |
| SOFA score | 6.00 [4.00, 9.00] | 5.00 [3.00, 7.00] | 11.50 [9.25, 13.75] | <0.001 |
| APACHE II score | 15.00 [10.00, 21.00] | 14.00 [8.00, 16.50] | 22.50 [18.50, 23.75] | 0.001 |
Fig. 2. Receiver operating characteristic curve analysis of SOFA to predict the 90-day mortality of patients with AHI.
Table 5. Risk factors for the EHS patients with AHI.
| Variable | Univariate |
Multivariate |
||
|---|---|---|---|---|
| OR (95 % CI) | p | OR (95 % CI) | p | |
| Myocardial injury | 13.10 (1.744, 98.26) | 0.012 | 12.169 (1.562, 94.806) | 0.023 |
| Kidney injury | 1.156 (0, Inf) | 0.997 | ||
| Rhabdomyolysis | 2.077 (0.476, 9.992) | 0.328 | ||
| CNS disorder | 2.862 (1.147, 6.96) | 0.024 | 1.106 (0.425, 2.879) | 0.837 |
| Infection | 6.143 (1.418, 26.62) | 0.153 | 5.637 (1.219, 26.064) | 0.027 |
| Lymphopenia | 28.78 (0, Inf) | 0.998 | ||
Inf, infinity.
Discussion
The present retrospective cohort study revealed that hepatic dysfunction usually occurred within 24 h after admission in EHS patients. The patients with AHI had more severe clinical conditions, significantly increased 90-day mortality rates, and shorter survival times. Complications with myocardial injuries or infection were found to be independent risk factors for death in EHS patients with AHI.
The time course of liver damage was found to differ from the damage-associated markers of other organs, since liver damage was often not detected at the onset of heatstroke.10 These results revealed that TBIL levels were increased at 24 h, peaked at 2–3 days, and began to decrease after day 5 in the survivors, while the non-survivors showed continuously increased levels of TBIL after admission. An animal heatstroke model has indicated that heat stress leads to extensive hepatocyte ballooning degeneration and necrosis.11 Data from patient autopsies have revealed that EHS-associated liver damage is characterized by centrilobular degeneration and necrosis with parenchymal damage.1,12 Previous studies have also found that the inhibition of inflammatory mediators, such as high-mobility group box 1 (HMGB1), could alleviate liver injury in a rat model of heatstroke, as evidenced by decreased levels of ALT and AST.11,13 The modulation of coagulation by thrombomodulin was also shown to improve liver function.14 Therefore, the hepatocyte damage in heatstroke patients is thought to be caused by a multifactorial damaging effect, including hyperthermia in combination with hypoxia, inflammatory stimuli, ischemia, and disseminated intravascular coagulation.15,16
Liver dysfunction is not usually detected at the onset of heatstroke, unlike damages to other organs that can be detected much earlier, such as injury to the myocardia or coagulation dysfunction. Currently, the liver is regarded as one of the first organs that becomes injured during heatstroke. Heat stress and the subsequent inflammatory response and coagulation dysfunction could lead to the damage of hepatocytes as well as liver sinusoidal endothelial cells and intrahepatic biliary epithelial cells, characterized by an increase in aminopherase and bilirubin. However, since liver compensatory mechanisms can maintain liver function, the dysfunction indices do not always directly correlate with damage to the liver. In addition, the secondary factors of heat stress, such as the systemic inflammatory response or liver ischemia, could further aggravate liver damage. These factors might also contribute to the delayed detection of liver damage. In the current study, non-survivor EHS patients had concentrations of TBIL over 2-fold higher at 24 h after admission, and these levels continuously increased, suggesting that a dramatic and continuous increase of TBIL may indicate a poor prognosis. Notably, since the liver plays a significant role in the synthesis of coagulation factors, INR was also regarded as a major index for liver function. However, during the pathological process of heatstroke, coagulation dysfunction occurs at an early stage due to the activation of endothelial cells. Therefore, INR was increased at the onset of heatstroke, which differed from other liver function indices.
During the pathophysiological process of heatstroke, the primary cell damage was due to heat-induced necrotic and apoptotic cell death. In later stages, thermoregulatory failure combined with an inflammatory reaction results in multiorgan failure that can cause death. Autopsy studies show that end-organ failure following heatstroke is accompanied by widespread microthrombosis, hemorrhage, and inflammatory injury.5,17,18 In the current study, EHS patients with AHI showed a higher all-cause mortality compared to those without AHI. Hepatocyte damage could result in a weakened detoxification process and decreased protein synthesis, which further increases the risk of infection and coagulation dysfunction. In addition, another explanation could be that EHS patients with AHI were in a more severe condition. Compared to patients in the non-AHI group, the organ dysfunction indices were increased in the AHI group, including those that indicate kidney injury, rhabdomyolysis, and cardiac injury.
To further clarify the risk factors for EHS patients with AHI, since most EHS patients in the AHI group were also experiencing dysfunction of other organs, a Cox hazard analysis was used to investigate the risk factors for death. A single variable analysis showed that complications with myocardial injuries, CNS disorders or infection were risk factors for death. In the multi-variate analysis, myocardial injuries and infection were found to be independent risk factors for death in EHS patients with AHI. In healthy individuals, bacteria are rarely cultured from the systemic circulation, and the liver plays an important role in eliminating micro-organisms from the blood.19 As a result, AHI may contribute to increased circulating endotoxin levels in heatstroke patients due to decreased bacterial clearance function. In EHS patients with AHI and myocardial injury or infection, the circulatory stability was affected. Unstable circulation may aggravate injuries of other organs due to hypoperfusion, leading to an increased risk of death, especially in the acute phase.
Conclusions
In EHS patients, hepatic dysfunction usually occurred 24 h after onset. EHS patients with AHI had more severe clinical conditions, significantly increased 90-day mortality rates, and shorter survival times. Complications of myocardial injuries and infection were found to be independent risk factors for death in EHS patients with AHI.
Abbreviations
- AHI
acute hepatic injury
- ALT
alanine transaminase
- APACHE
acute physiology and chronic health evaluation
- APTT
Activated Partial Thromboplastin Time
- AST
aspartate transaminase
- BUN
Blood Urea Nitrogen
- CHS
classical heatstroke
- CK
creatine kinase
- CK-Mb
creatine kinase-Mb
- CNS
central nervous system
- CTNI
cardiac troponin I
- CRP
C-reactive protein
- D.D
D-dimer
- EHS
exertional heatstroke
- GCS
glasgow coma scale
- ICU
intensive care unit
- INR
international normalized ratio
- IQR
interquartile range
- OR
odds ratio
- PCT
procalcitonin
- PLT
platelets
- PT
prothrombin time
- SOFA
sequential organ failure assessment
- SCR
serum creatinine
- TBIL
total bilirubin
- WBC
white blood cell
Data sharing statement
The data sets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- 1.Leon LR, Bouchama A. Heat stroke. Compr Physiol. 2015;5(2):611–647. doi: 10.1002/cphy.c140017. [DOI] [PubMed] [Google Scholar]
- 2.Bouchama A, Knochel JP. Heat stroke. N Engl J Med. 2002;346(25):1978–1988. doi: 10.1056/NEJMra011089. [DOI] [PubMed] [Google Scholar]
- 3.Gaudio FG, Grissom CK. Cooling methods in heat stroke. J Emerg Med. 2016;50(4):607–616. doi: 10.1016/j.jemermed.2015.09.014. [DOI] [PubMed] [Google Scholar]
- 4.Argaud L, Ferry T, Le QH, Marfisi A, Ciorba D, Achache P, et al. Short- and long-term outcomes of heatstroke following the 2003 heat wave in Lyon, France. Arch Intern Med. 2007;167(20):2177–2183. doi: 10.1001/archinte.167.20.ioi70147. [DOI] [PubMed] [Google Scholar]
- 5.Epstein Y, Yanovich R. Heatstroke. N Engl J Med. 2019;380(25):2449–2459. doi: 10.1056/NEJMra1810762. [DOI] [PubMed] [Google Scholar]
- 6.Abriat A, Brosset C, Brégigeon M, Sagui E. Report of 182 cases of exertional heatstroke in the French Armed Forces. Mil Med. 2014;179(3):309–314. doi: 10.7205/MILMED-D-13-00315. [DOI] [PubMed] [Google Scholar]
- 7.Bi X, Deising A, Frenette C. Acute liver failure from exertional heatstroke can result in excellent long-term survival with liver transplantation. Hepatology. 2020;71(3):1122–1123. doi: 10.1002/hep.30938. [DOI] [PubMed] [Google Scholar]
- 8.Hassanein T, Razack A, Gavaler JS, Van Thiel DH. Heatstroke: its clinical and pathological presentation, with particular attention to the liver. Am J Gastroenterol. 1992;87(10):1382–1389. [PubMed] [Google Scholar]
- 9.Hifumi T, Kondo Y, Shimizu K, Miyake Y. Heat stroke. J Intensive Care. 2018;6:30. doi: 10.1186/s40560-018-0298-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Deutsch M, Koskinas J, Emmanuel T, Kountouras D, Hadziyannis S. Heat stroke and multi-organ failure with liver involvement in an asylum-seeking refugee. J Emerg Med. 2006;31(3):255–257. doi: 10.1016/j.jemermed.2005.12.022. [DOI] [PubMed] [Google Scholar]
- 11.Geng Y, Ma Q, Liu YN, Peng N, Yuan FF, Li XG, et al. Heatstroke induces liver injury via IL-1β and HMGB1-induced pyroptosis. J Hepatol. 2015;63(3):622–633. doi: 10.1016/j.jhep.2015.04.010. [DOI] [PubMed] [Google Scholar]
- 12.Malamud N, Haymaker W, Custer RP. Heat stroke; a clinico-pathologic study of 125 fatal cases. Mil Surg. 1946;99(5):397–449. [PubMed] [Google Scholar]
- 13.Tong H, Tang Y, Chen Y, Yuan F, Liu Z, Peng N, et al. HMGB1 activity inhibition alleviating liver injury in heatstroke. J Trauma Acute Care Surg. 2013;74(3):801–807. doi: 10.1097/TA.0b013e31827e9a65. [DOI] [PubMed] [Google Scholar]
- 14.Kawasaki T, Okamoto K, Kawasaki C, Sata T. Thrombomodulin improved liver injury, coagulopathy, and mortality in an experimental heatstroke model in mice. Anesth Analg. 2014;118(5):956–963. doi: 10.1213/ANE.0000000000000170. [DOI] [PubMed] [Google Scholar]
- 15.Kew M, Bersohn I, Seftel H, Kent G. Liver damage in heatstroke. Am J Med. 1970;49(2):192–202. doi: 10.1016/s0002-9343(70)80075-4. [DOI] [PubMed] [Google Scholar]
- 16.Kew MC, Minick OT, Bahu RM, Stein RJ, Kent G. Ultrastructural changes in the liver in heatstroke. Am J Pathol. 1978;90(3):609–618. [PMC free article] [PubMed] [Google Scholar]
- 17.Bouchama A, Roberts G, Al Mohanna F, El-Sayed R, Lach B, Chollet-Martin S, et al. Inflammatory, hemostatic, and clinical changes in a baboon experimental model for heatstroke. J Appl Physiol (1985) 2005;98(2):697–705. doi: 10.1152/japplphysiol.00461.2004. [DOI] [PubMed] [Google Scholar]
- 18.Roberts GT, Ghebeh H, Chishti MA, Al-Mohanna F, El-Sayed R, Al-Mohanna F, et al. Microvascular injury, thrombosis, inflammation, and apoptosis in the pathogenesis of heatstroke: a study in baboon model. Arterioscler Thromb Vasc Biol. 2008;28(6):1130–1136. doi: 10.1161/ATVBAHA.107.158709. [DOI] [PubMed] [Google Scholar]
- 19.Nolan JP. Endotoxin, reticuloendothelial function, and liver injury. Hepatology. 1981;1(5):458–465. doi: 10.1002/hep.1840010516. [DOI] [PubMed] [Google Scholar]