Abstract
This meta-analysis systematically reviewed the evidence on standardized acceptance-/mindfulness-based interventions in DSM-5 anxiety disorders. Randomized controlled trials examining Acceptance and Commitment Therapy (ACT), Mindfulness-Based Cognitive Therapy (MBCT), and Mindfulness-Based Stress Reduction (MBSR) were searched via PubMed, Central, PsycInfo, and Scopus until June 2021. Standardized mean differences (SMD) and 95% confidence intervals (CI) were calculated for primary outcomes (anxiety) and secondary ones (depression and quality of life). Risk of bias was assessed using the Cochrane tool. We found 23 studies, mostly of unclear risk of bias, including 1815 adults with different DSM-5 anxiety disorders. ACT, MBCT and MBSR led to short-term effects on clinician- and patient-rated anxiety in addition to treatment as usual (TAU) versus TAU alone. In comparison to Cognitive Behavioral Therapy (CBT), ACT and MBCT showed comparable effects on both anxiety outcomes, while MBSR showed significantly lower effects. Analyses up to 6 and 12 months did not reveal significant differences compared to TAU or CBT. Effects on depression and quality of life showed similar trends. Statistical heterogeneity was moderate to considerable. Adverse events were reported insufficiently. The evidence suggests short-term anxiolytic effects of acceptance- and mindfulness-based interventions. Specific treatment effects exceeding those of placebo mechanisms remain unclear. Protocol registry: Registered at Prospero on November 3rd, 2017 (CRD42017076810).
Subject terms: Psychology, Health care, Medical research
Introduction
Anxiety disorders differ from normative fear or anxiety by featuring exaggerated symptoms lasting persistently over a prolonged period of time that interfere with daily activities. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) classifies anxiety disorders as Separation Anxiety Disorder, Selective Mutism, Social Anxiety Disorder, Panic Disorder, Agoraphobia, Specific Phobias, and Generalized Anxiety Disorder1. Globally, the one-year prevalence of anxiety disorders ranges from 2.4% to 29.8% with a point prevalence of 7.3%2, while subthreshold anxiety cases are even more common3. For most anxiety diagnoses, women are twice often affected than men4,5. Patients with anxiety disorders report high rates of co-morbidity6 and often suffer from disturbed sleep, headaches, depressed mood, gastrointestinal or cardiovascular problems7,8 leading to increasing costs of health care utilization and work loss9.
As the first-line treatment of anxiety disorders, clinical practice guidelines recommend psychological therapies, particularly Cognitive Behavioral Therapy (CBT) in preference to or in combination with pharmacotherapy10–12. Another treatment option with promising evidence for alleviating anxiety symptoms in non-psychiatric samples13–17 are mindfulness-based interventions such as Mindfulness-based Stress Reduction (MBSR), Mindfulness-Based Cognitive Therapy (MBCT), and Acceptance Commitment Therapy (ACT). MBSR is a standardized group program of 8 weekly sessions lasting an average of 2.5 h combined with an additional silent retreat day. Core components of MBSR include sitting and walking meditation, yoga asanas, and mindful relaxation techniques. Daily home practice is demanded to integrate mindfulness into everyday life18. MBCT combines mindfulness elements with cognitive-behavioral methods like psychoeducation, cognitive restructuring, and the development of pleasant activities – also within an 8-week group setting including a retreat day and daily home practice19. ACT combines acceptance-based and mindfulness strategies with cognitive-behavioral techniques and focuses on accepting experiences while being present, choosing goals according to values, and then taking committed action. ACT is usually an individual-based approach, but also offers group concepts mostly for non-clinical populations20. For patients with manifest anxiety disorders, previous systematic reviews of MBSR, MBCT, and ACT with and without meta-analysis suggest significant greater effects in comparison to usual care and comparable effects to CBT but used outdated methodology or focused on single anxiety disorders, mixed anxiety/obsessive–compulsive and depressive syndromes, or elderly patients/children21–26. To date, there is no comprehensive meta-analysis that assesses and compares the effectiveness and safety of standardized MBSR, MBCT, and ACT in the management of adult patients with DSM-5 anxiety disorders.
Methods
The systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines27 and the Cochrane recommendations28. Before starting the review, the protocol was registered at Prospero (CRD42017076810).
Study selection
Types of studies: Randomized controlled trials (RCTs) or randomized crossover trials were eligible.
Types of patients: Eligible samples included adults diagnosed with an anxiety disorder as defined by DSM-51 including:
Separation Anxiety Disorder (DSM-5: 309.21/ICD-10: F93.0),
Selective Mutism (DSM-5: 321.23/ICD-10: F94.0),
Specific Phobias (DSM-5: 300.29/ICD-10: F40.218, F40.228, F40.23x, F40.248, F40.298),
Social Anxiety Disorder (DSM-5: 300.23/ICD-10: F40.10),
Panic Disorder (DSM-5: 300.01/ICD-10: F41.0),
Agoraphobia (DSM-5: 300.22/ICD-10: F40.00),
Generalized Anxiety Disorder (DSM-5: 300.02/ICD-10: F41.1),
Other Specified (DSM-5: 300.09/ICD-10: F41.8), and
Unspecified Anxiety Disorder (DSM-5: 300.00/ICD-10: F41.9).
Patients who were diagnosed by prior versions of the DSM/ICD were also eligible, if their diagnosis is listed as a DSM-5 anxiety disorder as well. Studies involving patients with anxiety comorbid with other physical/mental disorders were eligible, if the comorbidity was not examined as the primary study outcome. Studies including heterogeneous psychiatric populations such as patients with anxiety disorders as well as those with depression or obsessive–compulsive disorder were excluded, while studies assessing mixed anxiety diagnoses (as defined above) were considered as well.
Types of interventions: Standardized acceptance- or mindfulness-based interventions like MBSR, MBCT, ACT, and variations of these programs (regardless of program length, frequency, or setting) were eligible. Studies allowing individual co-interventions were eligible as long as all participants in all groups received the same co-interventions. Acceptable control interventions were no treatment/wait-list or treatment as usual (TAU) as well as any other active treatments.
Types of outcomes: Improvement in the severity of anxiety symptoms measured by validated clinician- and/or patient-rated scales closest to 2 months after randomization (short-term) were defined as primary outcomes. Secondary outcomes included anxiety symptoms closest to 6 months and 12 months after randomization and safety. The severity of depressive symptoms and health-related quality of life were included as secondary outcomes as well, as anxiety disorders have high rates of comorbidity with depressive symptoms and reduced quality of life. If an outcomes was assessed by more than one instrument, primary endpoints were preferred over secondary ones, disease-specific instruments over generic ones and multi-item over single-item ones. Safety was assessed as the number of adverse events (AE) or study withdrawals due to AEs. AEs were defined as any untoward medical occurrence in a patient, without necessarily having a causal relationship with the study treatment. Cases of any untoward medical occurrence that had resulted in death, was life-threatening, required inpatient hospitalization, or caused persistent or significant disability were rated as serious AEs29.
Data sources
PubMed, Central, PsycInfo, and Scopus were searched from their inception to June 22nd, 2020. An update was executed in PubMed until June 14th, 2021. Table 1 shows the search strategy in PubMed, which was adapted for each database as necessary. No language restrictions were applied. Moreover, we manually searched reference lists of previous reviews. For ongoing and unpublished studies, we searched international trial registries of the WHO and the NIH applying identical search terms. Two reviewers (HH and PB) independently screened titles and abstracts and assessed full-texts for eligibility using EndNote. Any disagreement were rechecked with a third reviewer (HC) until consensus was achieved.
Table 1.
Search strategy in PubMed.
| #1 | MBSR[tiab] OR MBCT[tiab] OR mindful*[ tiab] OR Mindfulness[mesh] OR meditation[tiab] OR Meditation[mesh] OR acceptance-based[tiab] OR (acceptance[tiab] AND commitment[tiab] OR Acceptance and Commitment Therapy [mesh]) |
| #2 | Anxiety[mesh] OR Anxiety Disorders[mesh] OR anxiety[tiab] OR Phobic Disorders[mesh] OR Phobia, Social[mesh] OR phobia[tiab] OR phobic[tiab] OR Panic Disorder[mesh] OR panic[tiab] OR Agoraphobia[mesh] OR agoraphobia[tiab] |
| #3 | Randomized Controlled Trial[mesh] OR Randomized Controlled Trial[pt] OR Controlled Clinical Trial[pt] OR randomized[tiab] OR randomised[tiab] OR RCT[tiab] OR (random*[tiab] AND allocat*[tiab]) OR (random*[tiab] AND assign*[tiab]) OR placebo*[tiab] OR sham[tiab] OR group[tiab] OR trial[tiab] |
| #4 | #1 AND #2 AND #3 |
Data extraction
Two reviewers (PB and MS) independently extracted predefined data on the study setting and characteristics of the included studies. All Discrepancies were rechecked with a third reviewer (HH) until consensus was achieved.
For each study, the risk of selection bias, performance bias, detection bias, attrition bias, reporting bias, and other source of bias were independently assessed by two reviewers (PB and MS) using the Cochrane risk of bias tool28. Each domain was assessed as either, ‘low risk of bias’ if all requirements were adequately fulfilled, ‘high risk of bias’ if the requirements were not adequately fulfilled, and as ‘unclear risk of bias’ if insufficient data for a judgment was provided. Divergent assessments were rechecked with a third reviewer (HC) until consensus was achieved.
Data synthesis
Overall analyses
If at least two studies had assessed the same outcome to the same defined time point with the same type of control intervention, pairwise meta-analyses using random-effects models (inverse variance method) with Hedges’ correction for small samples28 were conducted using Review Manager Software (RevMan, Version 5.3, The Nordic Cochrane Centre, Copenhagen). For continuous outcomes, standardized mean differences (SMDs) with 95% confidence intervals (CIs) were calculated indicating the difference in means between groups divided by the pooled standard deviation (SD). In cases where no SDs were published, they were calculated from standard errors, CIs or t-values28, or were requested from trial authors by email. A negative SMD indicated greater effects of the experimental intervention over the respective control condition, except for quality of life. In accordance with Cohen’s categories, SMDs of 0.2–0.5 were interpreted as small effects, SMDs of 0.5–0.8 as medium effects, and SMDs > 0.8 as large effects30. For binary outcomes such as AEs, risk ratio analyses were planned. However, as most studies did not report AEs systematically, AEs were analyzed descriptively.
Assessment of statistical heterogeneity
Statistical heterogeneity between the study effects was analyzed by the Chi2 statistics with a p-value of ≤ 0.10 indicating significant heterogeneity. The magnitude of heterogeneity was categorized by the I2 with I2 > 25%, I2 > 50%, and I2 > 75% representing moderate, substantial, and considerable heterogeneity, respectively28,31.
Subgroup analyses
Subgroup analyses were planned for patients with different anxiety diagnoses and different mindfulness interventions but could only be realized for the latter, as the number of studies for comparisons was too small.
Sensitivity analyses
We conducted sensitivity analyses, where studies with high or unclear risk of bias were compared with those of low risk of bias. If substantial or considerable statistical heterogeneity was present in a meta-analysis, we used sensitivity analyses to explore heterogeneity in effect estimates.
Risk of bias across studies
The assessment of publication bias was planned by visual analysis of funnel plots and Egger's test, if more than 10 studies were included in a meta-analysis32.
Results
Literature search
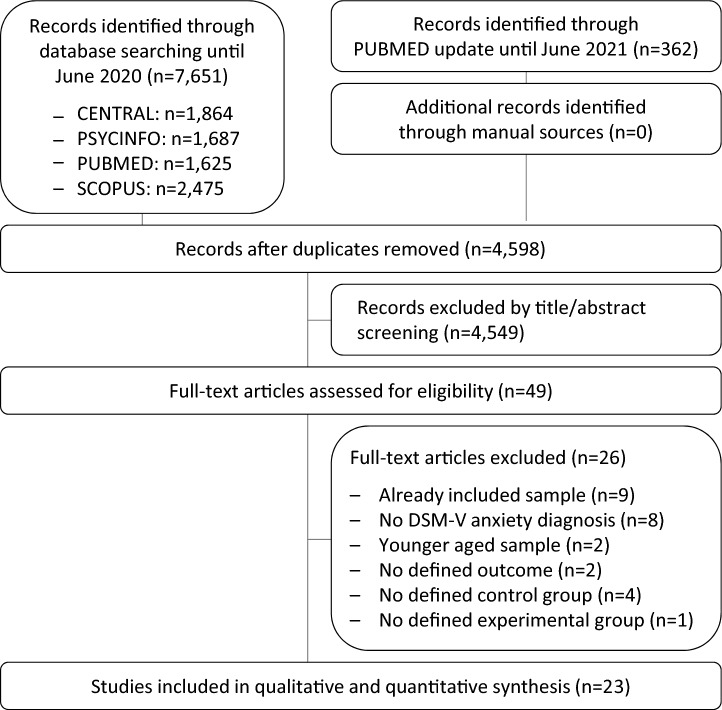
The electronic search revealed 7651 articles, a PubMed update additional 362 ones (Fig. 1). After the exclusion of supplicates and non-eligible abstracts, 49 articles were red in full. We excluded further 9 ones as they reported data of an already included sample33–41, 8 as they included mixed anxiety disorders containing patients with other than the defined DSM-5 anxiety diagnoses42–49, 2 articles because of younger aged samples50,51, 2 as they did not include a predefined outcome52,53, and 4 articles as they did not contain a predefined control group54–57. One additional study did not investigate a standardized ACT, MBCT, or MBSR program58. Thus, 23 RCTs published between 2007 and 2021 including 1815 patients were included in the meta-analysis59–81. Searching of trial registries revealed no additional unpublished or ongoing studies.
Figure 1.
PRISMA flow chart.
Study characteristics
The characteristics of the included RCTs are presented in detail in Table 2. The RCTs were conducted in the US, Sweden, Canada, Germany, Norway, Brazil, Japan, Iran, Romania, and China and investigated patients diagnosed with Generalized Anxiety Disorder, Social Anxiety Disorder, and mixed anxiety diagnoses. Samples randomized ranged from 24 to 182 with a median N of 81 containing a median of 67.1% of women. The participants’ median age was 35.3 years.
Table 2.
Characteristics of the included studies.
| References | Origin | Sample | Mean age ± SD | Females | Sample rando-mized | Intervention | Concur-rent drug intake | Assessment | Outcomes included | Outcomes not included | Safety | Funding | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Treatment | Control | |||||||||||||
| Asmaee Majid 201259 | Iran | GAD | 32.2 ± 2.2 | 0% | N = 33 | 8-week group MBSR + TAU | TAU | N.r | Post |
Patient-rated anxiety (BAI) Depression (BDI-II) |
Patient-rated anxiety (PSWQ) | N.r | No funding received | |
| Boettcher 201460 | Sweden |
PD, GAD, SAD, ADNOS |
38.0 ± 10.3 | 71.4% | N = 91 | 8-week individual online MBSR + TAU | 8-week individual online PE + TAU | 26.3% | Post |
Patient-rated anxiety (BAI)† Depression (BDI-II) Quality of life (QOLI) |
None | N.r | University funding | |
| Craske 201461 | United States | SAD | 28.4 ± 6.8 | 46.0% | N = 100 | 12-week individual ACT + TAU |
WL + TAU 12-week individual CBT + TAU |
32.2% | Post 6mFU 12mFU |
Clinician-rated anxiety (CSR)† Patient-rated social anxiety (composite score of LSAS-SR, SPS, SIAS)† Quality of life (QOLI)† |
None | N.r | Governmental funding | |
| Dahlin 201662 | Sweden | GAD | 39.5 ± 10.7 | 83.5% | N = 103 | 9-week individual online ACT + TAU | WL + TAU | 51.5% | Post |
Patient-rated anxiety (BAI) Depression (MADRS) Quality of life (QOLI) |
Patient-rated anxiety (PSWQ, GAD-7, GAD-Q-IV) Depression (PHQ9) |
N.r | Governmental + university funding | |
| de Almeida Sampaio 202063 | Brazil | GAD | 36.5 ± 12.4 | 73.9% | N = 92 | 14-week group ABBT + TAU | 14-week group PE + TAU | 35.9% | Post 6mFU |
Clinician-rated anxiety (HAM-A)† Patient-rated anxiety (DASS)† Depression (DASS) Quality of Life (WHOQOL) |
Clinician-rated anxiety (CGI) Patient-rated anxiety (PSWQ) |
N.r | N.r | |
| Fathi 201764 | Iran | GAD | 33.0 ± 4.7 | 100% | N = 40 | 12-week group ACT | WL | 0% | Post 5mFU | Patient-rated anxiety (BAI)† | Patient-rated anxiety (MCQ-30) | N.r | No funding received | |
| Gloster 201565 | Germany | PD, AP | 36.9 ± 8.9 | 69.8% | N = 43 | 4-week individual ACT + TAU | WL + TAU | 32.6% | Post |
Clinician-rated anxiety (CGI)† Patient-rated anxiety (BAI)† Depression (BDI-II)‡ |
Patient-rated anxiety (PAS, MI, BSQ, ACQ, ASI, HAM-A, BAFT) |
ACT: 0/33 AEs WL: 0/10 AEs |
Governmental funding | |
| Goldin 201666 | United States | SAD | 32.7 ± 7.8 | 65.6% | N = 108 | 12-week group MBSR |
WL 12-week group CBT |
0% |
Post 6mFU§ 12mFU§ |
Patient-rated anxiety (LSAS-SR)† Depression (RRS) |
Patient-rated anxiety (SAFE) | N.r | Governmental funding | |
| Hayes-Skelton 201367 | United States | GAD | 32.9 ± 12.2 | 65.4% | N = 81 | 16-week individual ACT + TAU | 16-week individual AR + TAU | 18.6% | Post 10mFU |
Clinician-rated anxiety (CSR)† Patient-rated anxiety (STAI-T)† Depression (BDI-II) Quality of life (QOLI) |
Clinician-rated anxiety (HAM-A) Patient-rated anxiety (PSWQ, DASS) |
ACT: 1/40 serious AE AR: 0/40 AEs |
Governmental funding | |
| Herbert 201868 | United States | SAD | 30.0 ± 11.0 | 51.1% | N = 102 | 12-week individual ACT + TAU | 12-week individual CBT + TAU | 18% | Post |
Clinician-rated anxiety (ADIS)† Patient-rated anxiety (LSAS-SR)† Depression (BDI) Quality of life (QOLI) |
Clinician-rated anxiety (CGI) Patient-rated anxiety (SPAI, BAI) Quality of life (OQ-45) |
N.r | No funding received | |
| Hoge 201369 | United States | GAD | 39.0 ± 13.0 | 51.0% | N = 93 | 8-week group MBSR + TAU | 8-week group PE + TAU | 15.1% | Post |
Clinician-rated anxiety (HAM-A)† Patient-rated anxiety (BAI) |
Clinician-rated anxiety (CGIS) |
MBSR: 1/48 non-serious AE PE: 1/41 non-serious AE |
Governmental + foundation funding | |
| Ivanova 201670 | Sweden | SAD, PD | 35.3 ± 11.0 | 64.5% | N = 152 | 10-week individual online ACT + TAU | WL + TAU | 42.8% | Post |
Patient-rated anxiety (LSAS-SR) Depression (PHQ-9) Quality of Life (QOLI) |
Patient-rated anxiety (PDSS-SR; GAD-7†) | N.r | Governmental funding | |
| Khoramnia 202071 | Iran | SAD | 22.12 ± 1.08 | 70.8% | N = 24 | 12-week individual ACT | WL | 0% | Post 5mFU | Patient-rated anxiety (SPIN)† | Patient-rated anxiety (AAQ-SA) | N.r | University funding | |
| Kocovski 201372 | Canada | SAD | 34.0 ± 11.1 | 55.5% | N = 137 | 12-week group ACT + TAU |
WL + TAU 12-week group CBT + TAU |
37.9% | Post 6mFU |
Clinician-rated anxiety (LSAS-CA) Patient-rated anxiety (SPIN)† Depression (BDI-II) |
Clinician-rated anxiety (CGI) Patient-rated anxiety (AAQ-SA) Depression (RRQ) |
N.r | Governmental + foundation funding | |
| Koszycki 200773 | Canada | SAD | 38.2 ± 13.4 | 45.3% | N = 53 | 8-week group MBSR + TAU | 12-week group CBT + TAU | 28.3% | Post |
Clinician-rated anxiety (LSAS-CA)† Patient-rated anxiety (SPS)† Depression (BDI-II) Quality of life (QOLI) |
Clinician-rated anxiety (CGI) Patient-rated anxiety (SIAS, IPSM) Quality of life (LSRDS) |
MBSR: 0/26 drop-out due to AE CBT: 2/27 drop-out due to AE |
University funding | |
| Koszycki 201675 | Canada | SAD | 39.7 ± 15.5 | 79.0% | N = 39 | 12-week group MBSR + TAU | WL + TAU | 23.1% | Post |
Clinician-rated anxiety (LSAS-CA)† Patient-rated anxiety (SPIN)† Depression (BDI-II) |
Clinician-rated anxiety (CGI) Patient-rated anxiety (SAS-SR) |
MBSR: 1/21 unspecified AE WL: N.r | University funding | |
| Koszycki 202174 | Canada | SAD | 40.86 ± 13.74 | 62.9% | N = 97 | 12-week group MBSR + TAU | 12-week group CBT + TAU | 19.6% | Post 6mFU§ |
Clinician-rated anxiety (LSAS-CA)† Patient-rated anxiety (SPIN) Depression (BDI-II) |
Patient-rated anxiety (SAS-SR) |
MBSR: 2/52 drop-out due to AE CBT: 2/45 drop-out due to AE |
Foundation funding | |
| Ninomiya 202076 | Japan | PD, SAD | 41.4 ± 10.0 | 37.5% | N = 40 | 8-week group MBCT + TAU | WL + TAU | 95% | Post |
Patient-rated anxiety (STAI-T)† Depression (CES-D) Quality of life (SF-12-PCS) |
Patient-rated anxiety (LSAS, MIA, K6) Quality of life (EQ-5D) |
MBSR: 0/20 serious AE WL: 0/20 serious AE |
Govern-mental funding | |
| Piet 201077 | Denmark | SAD | 21.9 ± 2.7 | 68.5% | N = 26 | 8-week group MBCT + TAU | 12-week group CBT + TAU | 11.5% | Post |
Clinician-rated anxiety (LSAS-CA)† Patient-rated anxiety (BAI) Depression (BDI-II) Quality of life (SDS) |
Patient-rated anxiety (SPS, SIAS, FNE-BV) |
MBCT: 1/8 non-serious AE CBT: 1/12 non-serious AE |
N.r | |
| Roemer 200878 | United States | GAD | 33.59 ± 11.74 | 71.0% | N = 31 | 14-week individual ACT + TAU | WL + TAU | 25.8% | Post |
Clinician-rated anxiety (CSR)† Depression (BDI) Quality of life (QOLI) |
Patient-rated anxiety (PSWQ, DASS, AAQ) | N.r | Governmental funding | |
| Stefan 201979 | Romania | GAD | 27.13 ± 7.5 | 84.5% | N = 75 | 16-week individual ABBT |
16-week individual - CBT (BTP) - CBT (REBT) |
0% | Post | Patient-rated anxiety (GAD-Q-IV)† | Patient-rated anxiety (PSWQ)† | N.r | Industrial funding | |
| Vollestad 201180 | Norway | PD, SAD, GAD | 42.5 ± 11.3 | 67.1% | N = 73 | 8-week group MBSR + TAU | WL + TAU | 27.6% | Post |
Patient-rated anxiety (BAI) Depression (BDI-II) Quality of life (SCL-90-R) |
Clinician-rated anxiety (GSI) Patient-rated anxiety (STAI, PSWQ) |
MBSR: 1/39 non-serious AE WL: 0/37 AE |
N.r | |
| Wong 201681 | China | GAD | 50.0 ± 10.0 | 79.1% | N = 182 | 8-week group MBCT + TAU |
WL + TAU 8-week group PE + TAU |
33.5% | Post 5mFU 11mFU |
Patient-rated anxiety (BAI)†‡ Depression (CES-D)‡ Quality of life (SF-12-PCS)‡ |
Patient-rated anxiety (PSWQ) | N.r | Governmental funding | |
AAQ-II = Acceptance and Action in Social Anxiety Questionnaire; ABBT = Acceptance-based Behavioral Therapy; ACQ = Agoraphobic Cognitions Questionnaire; ADIS: Anxiety Disorder interview Schedule; ADNOS = Anxiety Disorder Not Otherwise Specified; AP = Agoraphobia; AR = Applied Relaxation; ASI = Anxiety Sensitivity Index; BAI = Beck Anxiety Inventory; BAFT = Believability in Anxious Feelings and Thoughts Questionnaire; BDI-II = Beck Depression Inventory-II; BSQ = Bodily Sensations Questionnaire; CBT (BTP/REBT) = Cognitive Behavioral Therapy (Borkovec’s treatment package / Rational Emotive Behavior Therapy according to Ellis); CES-D = Centre for Epidemiological Studies-Depression Scale; CGI = Clinical Global Impression Severity Scale; CSR = Clinician Severity Ratings; DASS = Depression Anxiety and Stress Scale; EQ-5D = EuroQol 5-Dimension; FNE-BV = Fear of Negative Evaluation-Brief Version; GAD = Generalized Anxiety Disorder; GAD-Q-IV = Generalized Anxiety Disorder Questionnaire-IV; HAM-A = Hamilton Anxiety Rating Scale; IPSM = Interpersonal Sensitivity Measure; K6 = 6-item Psychological Distress Scale; LSAS-SR/CA = Liebowitz Social Anxiety Scale-Self Report/Clinician Administrated; LSRDS = Liebowitz Self-Rated Disability Scale; MADRS = Montgomery-Åsberg Depression Rating Scale; MBCT = Mindfulness Based Cognitive Therapy; MBSR = Mindfulness Based Stress Reduction; MCQ-30 = Metacognitions Questionnaire; MDD = Major Depressive Disorder; mFU = months after start of study; MIA = Mobility Inventory for Agoraphobia; N = sample size; N.r. = not reported; OQ-45 = 45-item Outcome Questionnaire; PAS = Panic Agoraphobia Scale; PD = Panic Disorder; PDSS-SR = Panic Disorder Severity Scale Self-Rated; PE: Psychoeducation; PHQ-9 = Patient Health Questionnaire; QOLI = Quality of Life Index; RRS = Ruminative Response Scale; RRQ = Rumination-Reflection Questionnaire; SAD = Social Anxiety Disorder; SAFE = Subtle Avoidance Frequency Examination; SAS-SR = Social Adjustment Scale Self-Report; SCL-90-R = Symptom Checklist-90-R; SDS = Shehan Disability Scale; SF-12-PCS = Short-Form Health Survey-Physical Component Score; SIAS = Social Interaction Anxiety Scale; SPIN = Social Phobia Inventory; SPS = Social Phobia Scale; STAI-T = State-Trait Anxiety Inventory-Trait Anxiety Subscale; TAU = treatment as usual; WHOQOL = World Health Organization Quality of Life Questionnaire; WL = wait-list; † = primary outcome(s) of the study; ‡ = data not published but provided by trial authors upon request; § = data not published & not provided by trial authors upon request.
Twelve RCTs investigated ACT interventions, 3 ones MBCT, and 8 ones MBSR. Individual- and group-based approaches varied as well as online and offline/in-person settings. Control interventions included TAU/wait-list, individualized or group-based CBT, psychoeducation, and relaxation. The median duration of the study treatments was 10 (4 to 16) weeks. Concurrent psychotropic drug use was reported by a median of 26.1% of the participants.
All studies provided data directly after the end of the intervention. Seven RCTs assessed a follow-up closest to 6 months after randomization, 4 RCTs additionally closest to 12 months after randomization. Outcomes included clinician-rated severity of anxiety, patient-rated severity of anxiety, patient-rated severity of depression, and patient-rated health-related quality of life.
Funding was reported by all but 3 RCTs and contained no specific funding (3 RCTs), university grants (4 RCTs), governmental grants (8 RCTs), university and governmental funding (1 RCT), private foundations (3 RCTs), and industrial funding (1 RCT).
Risk of bias of individual studies
Risk of selection bias was assessed as low in 21.7% of the included studies. Additional 30.4% reported adequate random sequence generation but did not provide information or reported in-adequate information about allocation concealment. No study had low risk of performance bias. The risk of detection bias was low in 60.9% of the studies. Here, a low risk of bias judgement was also given in cases, when the outcome was clinician-reported and the clinician was blinded to group allocation but also when the staff who handed out the patient questionnaires was blinded, even if patients cannot be blinded. The same amount of the studies (60.9%) were assessed as low risk of attrition bias as they recorded less than 10% drop-outs per group or/and performed intention-to treat analysis. The risk of reporting bias and possible risks of other sources of bias were low in 21.7% and 78.3% of the studies, respectively (Fig. 2).
Figure 2.
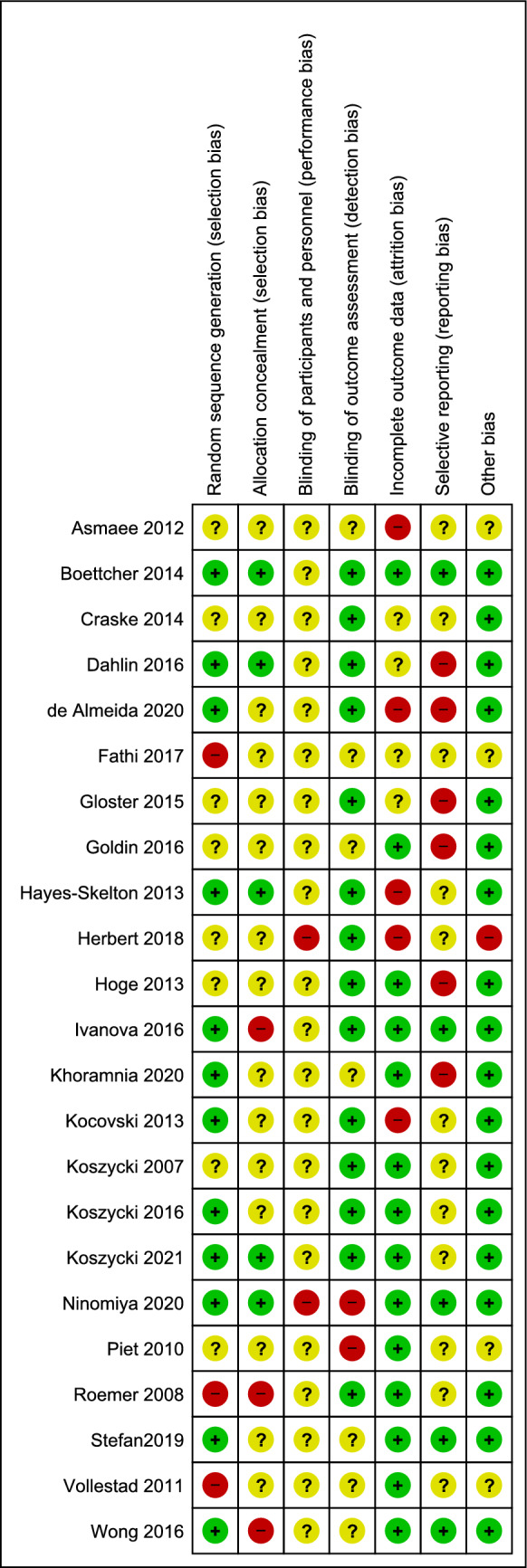
Risk of bias summary.
Pooling of effects
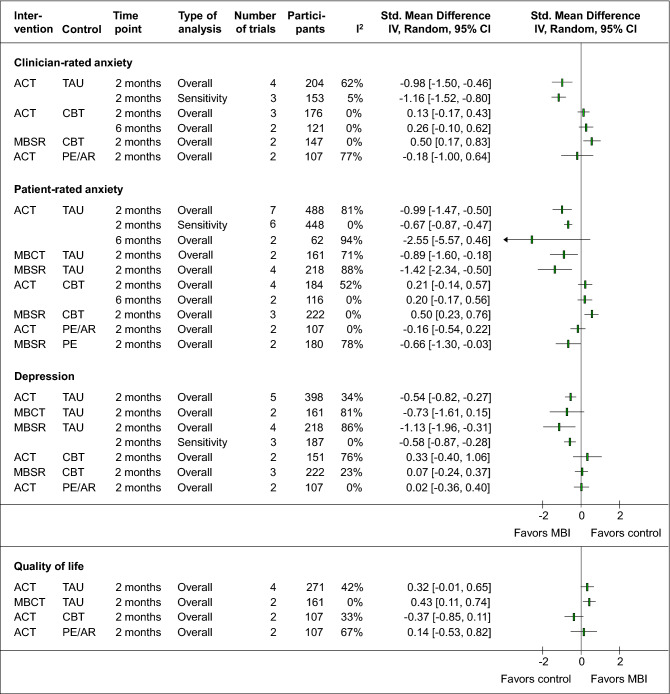
Clinician-rated anxiety
ACT showed a significantly larger short-term effect than TAU on clinician-rated anxiety (4 RCTs, SMD = −0.98, 95%CI = [−1.50, −0.46], I2 = 62%, N = 204). The substantial heterogeneity could be reduced by excluding one RCT65 with mostly high/unclear risk of bias and the only effect which crossed zero (3 RCTs, SMD = −1.16, 95%CI = [−1.52, −0.80], I2 = 5%, N = 152) (Fig. 3). The analyses were robust against risk of detection bias, attrition bias, and other bias. In comparison to CBT, ACT homogeneously showed non-significant short-term (3 RCTs, SMD = 0.13, 95%CI = [−0.17, 0.43], I2 = 0%, N = 176) and medium-term effects up to 6 months (2 RCTs, SMD = 0.26, 95%CI = [−0.10, 0.62], I2 = 0%, N = 121) (Fig. 3). However, for both analyses, only the risk of detection bias and other bias was low. Up to 12 months, again no significant differences were found between ACT and CBT61. In comparison to less complex psychological interventions such as psychoeducation or relaxation, ACT did not show a significant larger effect (2 RCTs, SMD = −0.18, 95%CI = [−1.00, 0.64], I2 = 77%, N = 107) (Fig. 3). Because of the considerable heterogeneity, the pooled effect should be interpreted with restraint, also because one of the RCTs63 reported significant medium-term effects of ACT against psychoeducation. Detailed analyses can be found in the Supplementary Fig. 1.
Figure 3.
Forest plot summary of the effects on primary and secondary outcomes. Legend. ACT: Acceptance and Commitment Therapy; AR: Applied relaxation; CBT: Cognitive Behavioral Therapy; CI: Confidence interval; I2: Measure of statistical heterogeneity; IV: Inverse variance; MBCT: Mindfulness-based Cognitive Therapy; MBSR: Mindfulness-based stress reduction; PE: Psychoeducation; TAU: Treatment as usual.
One further RCT investigated MBSR against TAU and showed significantly higher improvements on clinician-rated anxiety up to 2 months post randomization75, while as compared to CBT, MBSR showed significantly lower short-term improvements (2 RCTs, SMD = 0.50, 95%CI = [0.17, 0.83], I2 = 0%, N = 147) (Fig. 1).
Further 2 RCTs of mostly unclear risk of bias, one on MBCT against CBT77 and another on MBSR against psychoeducation69 did not show any significant short-term superiority of the respective interventions.
Patient-rated anxiety
The meta-analyses of ACT in comparison to TAU revealed a significantly larger effect in favor of ACT (7 RCTs, SMD = −0.99, 95%CI = [−1.47, −0.50], I2 = 84%, N = 488) but revealed considerable heterogeneity, which could be decreased by excluding one RCT64 with the greatest effect in favor of ACT and the weakest study quality (6 RCTs, SMD = −0.67, 95%CI = [−0.87, −0.47], I2 = 0%, N = 448) (Fig. 3). The effect was robust against the risk of selection bias, detection bias, attrition bias, reporting bias, and other bias. No significant differences occurred for ACT versus TAU at 6 months (2 RCS, SMD = −2.55, 95%CI = [−5.57, 0.46], I2 = 94%, N = 62), while both individual trials64,71 reported significant differences. However, the two RCTs were both of unclear/high risk of bias and included very small samples, which may explain the considerable heterogeneity. The meta-analysis of ACT versus CBT contained RCTs with mostly unclear/high risk of bias and revealed neither significant short-term (4 RCTs, SMD = 0.21, 95%CI = [−0.14, 0.57], I2 = 52%, N = 284) nor medium-term (2 RCTs, SMD = 0.20, 95%CI = [−0.17, 0.56], I2 = 0%, N = 116) (Fig. 3) or longer-term differences61 between the two therapies. In comparison to less complex psychological interventions, ACT led to no significantly different short-term effect (2 RCTs, SMD = −0.16, 95%CI = [−0.54, 0.22], I2 = 0%, N = 107) (Fig. 3).
The meta-analyses of MBCT revealed a significant larger but heterogeneous short-term effect than TAU (2 RCTs, SMD = −0.89, 95%CI = [−160, −0.18], I2 = 71%, N = 161) (Fig. 3). At 6 months, a single RCT reported persisting longer-term effects as well81. In comparison to CBT, MBCT did not lead to significantly larger short-term effects77. MBCT and psychoeducation at 2, 6, and 12 months did not significantly differ from each other81.
The meta-analysis of MBSR versus TAU showed a significantly larger short-term effect in favor of MBSR (4 RCTs, SMD = −1.42, 95%CI = [−2.34, −0.50], I2 = 88%, N = 218) (Fig. 3). While the heterogeneity could not be reduced by excluding individual RCTs, the effect remained significant when excluding the RCTs with unclear/high risk of detection bias, attrition bias, and other bias. In comparison to CBT, the meta-analysis showed significantly lower improvements for MBSR (3 RCTs, SMD = 0.50, 95%CI = [0.23, 0.76], I2 = 0%, N = 222) (Fig. 1). In comparison to psychoeducation, MBSR showed a significantly larger short-term effect (2 RCTs, SMD = −0.66, 95%CI = [−1.30, −0.03], I2 = 78%, N = 180) (Fig. 3). The meta-analysis contained considerable heterogeneity but could be considered as robust against all risk of bias domains except the risk of performance bias. Detailed analyses on patient-rated anxiety is provided in Supplementary Fig. 2.
Depressive symptoms
For depressive symptoms, the meta-analysis revealed significantly higher short-term effects of ACT than of TAU (5 RCTs, SMD = −0.54, 95%CI = [−0.82, −0.27], I2 = 34%, N = 398), which was found to be robust against risk of selection bias, detection bias, and other bias. In comparison to CBT (2 RCTs, SMD = 0.33, 95%CI = [−0.40, 1.06], I2 = 76%, N = 151) and less complex psychological interventions (2 RCTs, SMD = 0.02, 95%CI = [−0.36, 0.40], I2 = 0%, N = 107), ACT did not reveal larger short-term effects (Fig. 3). Longer-term effects at 12 months did also not significantly differ from psychoeducation67.
For MBCT, the meta-analysis did not show significantly higher effects on depressive symptoms against TAU, neither at short-term (2 RCTs, SMD = −0.73, 95%CI = [−1.61, 0.15], I2 = 81%, N = 161) nor at 6 months81. Short- and longer-term effects did not differ between MBCT and CBT77 or psychoeducation81.
For MBSR, the meta-analysis revealed significantly larger short-term anti-depressive effects against TAU (4 RCTs, SMD = −1.13, 95%CI = [−1.96, −0.31], I2 = 86%, N = 218). The considerable heterogeneity could be reduced by excluding one low-quality RCT with the largest effect that compared MBSR to TAU without using a waiting list59. This resulted in still significantly higher short-term effects of MBSR compared to TAU (3 RCTs, SMD = −0.58, 95%CI = [−0.87, −0.28], I2 = 0%, N = 187) (Fig. 3). The effect was robust against risk of detection bias, attrition bias, and other bias. In comparison to CBT, no superiority of MBSR on depressive symptoms could be detected (3 RCTs, SMD = 0.07, 95%CI = [−0.24, 0.37], I2 = 23%, N = 222) (Fig. 3). One additional RCT showed that MBSR was superior to psychoeducation in reducing short-term depressive symptoms60. Detailed analyses on depression can be found in the Supplementary Fig. 3.
Quality of life
ACT showed no significantly different short-term effect on quality of life compared to TAU (4 RCTs, SMD = 0.32, 95%CI = [−0.01, 0.65], I2 = 42%, N = 271), CBT (2 RCTs, SMD = −0.37, 95%CI = [−0.85, 0.11], I2 = 33%, N = 107) or less complex psychotherapeutic interventions (2 RCTs, SMD = 0.14, 95%CI = [−0.53, 0.82], I2 = 67%, N = 107) (Fig. 3). Longer-term effects of ACT did not significantly differ from those of CBT at 6 and 12 months61, were reported as significantly higher as those of psychoeducation at 6 months63, but not significantly different from those of relaxation at 12 months67.
MBCT was found to be superior to TAU in the short-term (2 RCTs, SMD = 0.43, 95%CI = [0.11, 0.74], I2 = 0%, N = 161) (Fig. 3), but not to CBT77 or to psychoeducation81. More detailed analyses can be found in the Supplementary Fig. 4.
Further RCTs reported significantly higher short-term effects on quality of life in favor of MBSR compared to TAU80 but not compared to CBT73 or psychoeducation60.
Safety
Safety data were reported insufficiently (Tab. 2). Fourteen RCTs did not report any information on AEs or reasons for study withdrawal. Serious AEs were reported by one RCT in the ACT group (bypass surgery), which was highly likely not related to the study intervention67. Minor AEs were equally distributed between experimental and control groups65,69,73–77,80.
Discussion
Summary of evidence
The literature search revealed 23 RCTs investigating the effectiveness of ACT, MBCT, and MBSR in patients with DSM-5 anxiety disorders such as Generalized Anxiety Disorder, Social Anxiety Disorder, and mixed samples including different anxiety diagnoses. The meta-analyses revealed at least short-term effects on clinician- and patient-rated anxiety for ACT, MBCT and MBSR in addition to TAU versus TAU alone. In comparison to CBT, ACT and MBCT showed comparable effects on both anxiety outcomes, while MBSR showed significantly lower effects. Pooled effects up to 6 months post randomization can only be calculated for ACT but did not show any significant differences compared to TAU or CBT. Short-term effects of ACT, MBCT and MBSR on secondary outcomes were superior against TAU but not against CBT or less complex psychotherapeutic interventions such as psychoeducation or applied relaxation. Most effects were robust against most risk of bias domains. However, the risk of selection bias and performance bias remains unclear or high for almost all meta-analyses. Statistical heterogeneity could be reduced in several meta-analyses by excluding low-quality studies with extreme values. A correlation of those extreme values with funding concerns from industrial companies or private foundations could not be determined. Moreover, comparisons to CBT should be interpreted with restraint as the number of included trials was very low and none of the studies tested non-inferiority. Adverse events were reported insufficiently. If safety issues were reported, ACT, MBCT, and MBSR did not lead to more adverse events than usual care and comparable adverse events to CBT.
In contrast to prior systematic reviews, which found promising effects of mindfulness on anxiety symptoms in the general population13,14,23 and somatically ill samples15,17, the evidence for patients with manifest DSM-5 anxiety disorders should be interpreted with restraint. Reasons include the low number of studies investigating longer-term effects against eligible control conditions such as CBT, the overall unclear study quality, and the often missed systematic assessment and reporting of adverse events.
Limitations
This meta-analysis has further limitations. We often were not able to pool data of RCTs because of non-comparable controls, or could perform sensitivity analyses of comparisons including only 2 RCTs. In addition, we were not able to calculate subgroup analyses of different anxiety disorders. Thus, the present meta-analysis does not allow to draw conclusions for a specific diagnosis. Since risk of publication bias could not be assessed, the effects might also be overestimated due to unpublished studies, even if the search of trial registries did not result in registered but unpublished studies82.
Implications for further research
Further higher-quality trials on mindfulness-based interventions are needed to verify the effects in patients with manifest anxiety disorders. Authors should ensure rigorous methodology and reporting according to CONSORT83 and choose adequate control conditions. Recent meta-analyses on pharmacological and psychological intervention for anxiety disorders conclude that wait-list control groups may produce nocebo effects in trials of psychotherapy84. TAU, in addition, was also found to be a very heterogeneous control condition and anything but usual or standard care85,86. Psychological placebo effects were estimated on average 0.83 in patients with anxiety disorders87. Thus, adequate control groups for trials on manifest disorders rather than subclinical symptoms should be designed considering nocebo as well as placebo effects. Non-inferiority trials against standard psychotherapies such as CBT are missing completely. To enhance study quality and reduce the risk of performance bias, even if patients and therapists cannot be blinded, controlling for patients’ treatment expectations and their perceptions of quality of the alliance towards the treating therapist would be feasible. Blinding of outcome assessors, especially for clinician-rated outcomes as well as more adequate statistics (including intention-to-treat analyses) should be standard. Future studies are requested to strictly report AEs and reasons of drop-out.
Conclusions
The evidence suggests clinically relevant short-term anxiolytic effects of acceptance-based and with less extent of mindfulness-based interventions when added to usual care that, however, might be a result of nocebo- and/or placebo effects. The relevance of longer-term effects as well as the comparability to standard CBT remain preliminary until further high-quality studies will be published.
Supplementary Information
Author contributions
H.H. was responsible for the conception and design of the meta-analysis, the collection and analysis of the study data and for drafting the manuscript. P.B. and M.S. participated in the collection and analysis of the study data and critically revised the manuscript. G.D. critically revised the manuscript. H.C. participated in the conception and design of the meta-analysis, the analysis of the study data, and critically revised the manuscript. All authors approved the final manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL. Holger Cramer was supported by the Erich Rothenfußer Stiftung. Apart from this, the review received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Data availability
The data and material analyzed during the current study are available from the corresponding author on request.
Code availability
The RevMan code used for the current study is available from the corresponding author on request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-99882-w.
References
- 1.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5) American Psychiatric Publishing; 2013. [Google Scholar]
- 2.Baxter AJ, Scott KM, Vos T, Whiteford HA. Global prevalence of anxiety disorders: A systematic review and meta-regression. Psychol. Med. 2013;43:897–910. doi: 10.1017/s003329171200147x. [DOI] [PubMed] [Google Scholar]
- 3.Haller H, Cramer H, Lauche R, Gass F, Dobos GJ. The prevalence and burden of subthreshold generalized anxiety disorder: A systematic review. BMC Psychiatry. 2014;14:128. doi: 10.1186/1471-244X-14-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grenier S, et al. Association of age and gender with anxiety disorders in older adults: A systematic review and meta-analysis. Int. J. Geriatr. Psychiatry. 2019;34:397–407. doi: 10.1002/gps.5035. [DOI] [PubMed] [Google Scholar]
- 5.Gustavson K, et al. Prevalence and stability of mental disorders among young adults: Findings from a longitudinal study. BMC Psychiatry. 2018;18:65. doi: 10.1186/s12888-018-1647-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kessler RC, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 7.Nabi H, et al. Psychological and somatic symptoms of anxiety and risk of coronary heart disease: The health and social support prospective cohort study. Biol. Psychiat. 2010;67:378–385. doi: 10.1016/j.biopsych.2009.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pelletier L, O'Donnell S, McRae L, Grenier J. The burden of generalized anxiety disorder in Canada. Health Promotion and Chronic Disease Prevention in Canada : Research, Policy and Practice. 2017;37:54–62. doi: 10.24095/hpcdp.37.2.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wittchen HU, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur. Neuropsychopharmacol. 2011;21:655–679. doi: 10.1016/j.euroneuro.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 10.Bandelow, B. et al. Deutsche S3-Leitlinie Behandlung von Angststörungen. (2014). https://www.awmf.org/uploads/tx_szleitlinien/051-028l_S3_Angstst%C3%B6rungen_2014-05_2.pdf.
- 11.Katzman MA, et al. Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive-compulsive disorders. BMC Psychiatry. 2014;14(Suppl 1):S1. doi: 10.1186/1471-244x-14-s1-s1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Institute for Health and Care Excellence (NICE). Generalised anxiety disorder and panic disorder in adults: management. (2019). https://www.nice.org.uk/guidance/cg113/resources/generalised-anxiety-disorder-and-panic-disorder-in-adults-management-pdf-35109387756997. [PubMed]
- 13.Gotink RA, et al. Standardised mindfulness-based interventions in healthcare: An overview of systematic reviews and meta-analyses of RCTs. PLoS ONE. 2015;10:e0124344. doi: 10.1371/journal.pone.0124344. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 14.Guillaumie L, Boiral O, Champagne J. A mixed-methods systematic review of the effects of mindfulness on nurses. J. Adv. Nurs. 2017;73:1017–1034. doi: 10.1111/jan.13176. [DOI] [PubMed] [Google Scholar]
- 15.Haller H, et al. Mindfulness-based interventions for women with breast cancer: An updated systematic review and meta-analysis. Acta Oncologica (Stockholm, Sweden) 2017;56:1665–1676. doi: 10.1080/0284186x.2017.1342862. [DOI] [PubMed] [Google Scholar]
- 16.Kishita N, Takei Y, Stewart I. A meta-analysis of third wave mindfulness-based cognitive behavioral therapies for older people. Int. J. Geriatr. Psychiatry. 2017;32:1352–1361. doi: 10.1002/gps.4621. [DOI] [PubMed] [Google Scholar]
- 17.Schell LK, Monsef I, Wockel A, Skoetz N. Mindfulness-based stress reduction for women diagnosed with breast cancer. Cochrane Database Syst. Rev. 2019;3:Cd011518. doi: 10.1002/14651858.CD011518.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. Gen. Hosp. Psychiatry. 1982;4:33–47. doi: 10.1016/0163-8343(82)90026-3. [DOI] [PubMed] [Google Scholar]
- 19.Teasdale JD, et al. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J. Consult. Clin. Psychol. 2000;68:615–623. doi: 10.1037/0022-006X.68.4.615. [DOI] [PubMed] [Google Scholar]
- 20.Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: Model, processes and outcomes. Behav. Res. Ther. 2006;44:1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 21.Norton AR, Abbott MJ, Norberg MM, Hunt C. A systematic review of mindfulness and acceptance-based treatments for social anxiety disorder. J. Clin. Psychol. 2015;71:283–301. doi: 10.1002/jclp.22144. [DOI] [PubMed] [Google Scholar]
- 22.Costa M, Oliveira G, Tatton-Ramos T, Manfro G, Salum G. Anxiety and stress-related disorders and mindfulness-based interventions: A systematic review and multilevel meta-analysis and meta-regression of multiple outcomes. Mindfulness. 2018;10:996–1005. doi: 10.1007/s12671-018-1058-1. [DOI] [Google Scholar]
- 23.Li SYH, Bressington D. The effects of mindfulness-based stress reduction on depression, anxiety, and stress in older adults: A systematic review and meta-analysis. Int. J. Ment. Health Nurs. 2019;28:635–656. doi: 10.1111/inm.12568. [DOI] [PubMed] [Google Scholar]
- 24.Ruiz-Íñiguez R, Santed Germán MÁ, Burgos-Julián FA, Díaz-Silveira C, Carralero Montero A. Effectiveness of mindfulness-based interventions on anxiety for children and adolescents: A systematic review and meta-analysis. Early Interv. Psychiatry. 2020;14:263–274. doi: 10.1111/eip.12849. [DOI] [PubMed] [Google Scholar]
- 25.Coto-Lesmes R, Fernández-Rodríguez C, González-Fernández S. Acceptance and Commitment Therapy in group format for anxiety and depression. A systematic review. J. Affect. Disorders. 2020;263:107–120. doi: 10.1016/j.jad.2019.11.154. [DOI] [PubMed] [Google Scholar]
- 26.Ghahari S, Mohammadi-Hasel K, Malakouti SK, Roshanpajouh M. Mindfulness-based cognitive therapy for generalised anxiety disorder: A systematic review and meta-analysis. East Asian Arch. Psychiatry. 2020;30:52–56. doi: 10.12809/eaap1885. [DOI] [PubMed] [Google Scholar]
- 27.Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G. & Group, P Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int. J. Surg. 2010;8:336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 28.Higgins, J. P. & Thomas, J. Cochrane handbook for systematic reviews of interventions Version 6.2. (2021). https://training.cochrane.org/handbook/current.
- 29.European Medicines Agency. ICH Harmonized Tripartite Guideline E6: Note for Guidance on Good Clinical Practice (PMP/ICH/135/95). (European Medicines Agency, 2002).
- 30.Ellis PD. The essential guide to effect sizes. Statistical power, meta-analysis, and the interpretation of research results. Cambridge University Press; 2012. [Google Scholar]
- 31.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Butler RM, et al. Emotional clarity and attention to emotions in cognitive behavioral group therapy and mindfulness-based stress reduction for social anxiety disorder. J. Anxiety Disord. 2018;55:31–38. doi: 10.1016/j.janxdis.2018.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jazaieri, H., Goldin, P. R. & Gross, J. J. The role of working alliance in cbt and mbsr for social anxiety disorder. Mindfulness, No Pagination Specified. 10.1007/s12671-017-0877-9 (2018).
- 35.Millstein DJ, Orsillo SM, Hayes-Skelton SA, Roemer L. Interpersonal problems, mindfulness, and therapy outcome in an acceptance-based behavior therapy for generalized anxiety disorder. Cogn. Behav. Ther. 2015;44:491–501. doi: 10.1080/16506073.2015.1060255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thurston MD, Goldin P, Heimberg R, Gross JJ. Self-views in social anxiety disorder: The impact of CBT versus MBSR. J. Anxiety Disord. 2017;47:83–90. doi: 10.1016/j.janxdis.2017.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wong SY, et al. Mindfulness-based cognitive therapy for generalised anxiety disorder and health service utilisation among Chinese patients in primary care: a randomised, controlled trial. Hong Kong medical journal = Xianggang yi xue za zhi. 2016;22(Suppl 6):35–36. [PubMed] [Google Scholar]
- 38.Brown LA, et al. Self-referential processing during observation of a speech performance task in social anxiety disorder from pre- to post-treatment: Evidence of disrupted neural activation. Psychiatry Res. Neuroimaging. 2019;284:13–20. doi: 10.1016/j.pscychresns.2018.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Horenstein A, et al. Sleep quality and treatment of social anxiety disorder. Anxiety Stress Coping. 2019;32:387–398. doi: 10.1080/10615806.2019.1617854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Morrison AS, et al. Changes in empathy mediate the effects of cognitive-behavioral group therapy but not mindfulness-based stress reduction for social anxiety disorder. Behav. Ther. 2019;50:1098–1111. doi: 10.1016/j.beth.2019.05.005. [DOI] [PubMed] [Google Scholar]
- 41.Sewart AR, et al. Examining positive and negative affect as outcomes and moderators of cognitive-behavioral therapy and acceptance and commitment therapy for social anxiety disorder. Behav. Ther. 2019;50:1112–1124. doi: 10.1016/j.beth.2019.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Arch JJ, et al. Randomized clinical trial of adapted mindfulness-based stress reduction versus group cognitive behavioral therapy for heterogeneous anxiety disorders. Behav. Res. Ther. 2013;51:185–196. doi: 10.1016/j.brat.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 43.Arch JJ, et al. Randomized clinical trial of cognitive behavioral therapy (CBT) versus acceptance and commitment therapy (ACT) for mixed anxiety disorders. J. Consult. Clin. Psychol. 2012;80:750–765. doi: 10.1037/a0028310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lang AJ, et al. Randomized controlled trial of acceptance and commitment therapy for distress and impairment in OEF/OIF/OND veterans. Psychol. Trauma Theory Res. Pract. Policy. 2017;9:74–84. doi: 10.1037/tra0000127. [DOI] [PubMed] [Google Scholar]
- 45.Ritzert TR, et al. Evaluating the effectiveness of ACT for anxiety disorders in a self-help context: outcomes from a randomized wait-list controlled trial. Behav. Ther. 2016;47:444–459. doi: 10.1016/j.beth.2016.03.001. [DOI] [PubMed] [Google Scholar]
- 46.Finnes A, Ghaderi A, Dahl J, Nager A, Enebrink P. Randomized controlled trial of acceptance and commitment therapy and a workplace intervention for sickness absence due to mental disorders. J. Occup. Health Psychol. 2019;24:198–212. doi: 10.1037/ocp0000097. [DOI] [PubMed] [Google Scholar]
- 47.Haddad R, et al. Does patient expectancy account for the cognitive and clinical benefits of mindfulness training in older adults? Int. J. Geriatr. Psychiatry. 2020;35:626–632. doi: 10.1002/gps.5279. [DOI] [PubMed] [Google Scholar]
- 48.Kladnitski N, et al. Transdiagnostic internet-delivered CBT and mindfulness-based treatment for depression and anxiety: A randomised controlled trial. Internet Interv. 2020;20:100310. doi: 10.1016/j.invent.2020.100310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ruiz FJ, et al. Efficacy of a two-session repetitive negative thinking-focused acceptance and commitment therapy (ACT) protocol for depression and generalized anxiety disorder: A randomized waitlist control trial. Psychotherapy (Chic.) 2020 doi: 10.1037/pst0000273. [DOI] [PubMed] [Google Scholar]
- 50.Alimehdi M, Ehteshamzadeh P, Naderi F, Eftekharsaadi Z, Pasha R. The effectiveness of mindfulness-based stress reduction on intolerance of uncertainty and anxiety sensitivity among individuals with generalized anxiety disorder. Asian Soc. Sci. 2016;12:179–187. doi: 10.5539/ass.v12n4p179. [DOI] [Google Scholar]
- 51.Azadeh SM, Kazemi-Zahrani H, Besharat MA. Effectiveness of acceptance and commitment therapy on interpersonal problems and psychological flexibility in female high school students with social anxiety disorder. Global J. Health Sci. 2015;8:131–138. doi: 10.5539/gjhs.v8n3p131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hoge EA, et al. The effect of mindfulness meditation training on biological acute stress responses in generalized anxiety disorder. Psychiatry Res. 2018;262:328–332. doi: 10.1016/j.psychres.2017.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.MacCoon DG, et al. The validation of an active control intervention for Mindfulness Based Stress Reduction (MBSR) Behav. Res. Ther. 2012;50:3–12. doi: 10.1016/j.brat.2011.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gershkovich M, Herbert JD, Forman EM, Schumacher LM, Fischer LE. Internet-delivered acceptance-based cognitive-behavioral intervention for social anxiety disorder with and without therapist support: A randomized trial. Behav. Modif. 2017;41:583–608. doi: 10.1177/0145445517694457. [DOI] [PubMed] [Google Scholar]
- 55.Goldin PR, Ziv M, Jazaieri H, Gross JJ. Randomized controlled trial of mindfulness-based stress reduction versus aerobic exercise: Effects on the self-referential brain network in social anxiety disorder. Front. Hum. Neurosci. 2012;6:295. doi: 10.3389/fnhum.2012.00295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Navarro-Haro MV, et al. Evaluation of a mindfulness-based intervention with and without virtual reality dialectical behavior therapy® mindfulness skills training for the treatment of generalized anxiety disorder in primary care: A pilot study. Front. Psychol. 2019;10:55. doi: 10.3389/fpsyg.2019.00055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Villatte JL, et al. Acceptance and Commitment Therapy modules: Differential impact on treatment processes and outcomes. Behav. Res. Ther. 2016;77:52–61. doi: 10.1016/j.brat.2015.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Costa MA, et al. A three-arm randomized clinical trial comparing the efficacy of a mindfulness-based intervention with an active comparison group and fluoxetine treatment for adults with generalized anxiety disorder. Psychother. Psychosom. 2020 doi: 10.1159/000511880. [DOI] [PubMed] [Google Scholar]
- 59.Asmaee Majid S, Seghatoleslam T, Homan H, Akhvast A, Habil H. Effect of mindfulness based stress management on reduction of generalized anxiety disorder. Iran. J. Public Health. 2012;41:24–28. [PMC free article] [PubMed] [Google Scholar]
- 60.Boettcher J, et al. Internet-based mindfulness treatment for anxiety disorders: a randomized controlled trial. Behav. Ther. 2014;45:241–253. doi: 10.1016/j.beth.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 61.Craske MG, et al. Randomized controlled trial of cognitive behavioral therapy and acceptance and commitment therapy for social phobia: outcomes and moderators. J. Consult. Clin. Psychol. 2014;82:1034–1048. doi: 10.1037/a0037212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dahlin M, et al. Internet-delivered acceptance-based behaviour therapy for generalized anxiety disorder: A randomized controlled trial. Behav. Res. Ther. 2016;77:86–95. doi: 10.1016/j.brat.2015.12.007. [DOI] [PubMed] [Google Scholar]
- 63.de Almeida Sampaio TP, et al. Efficacy of an acceptance-based group behavioral therapy for generalized anxiety disorder. Depress. Anxiety. 2020 doi: 10.1002/da.23021. [DOI] [PubMed] [Google Scholar]
- 64.Fathi R, Khodarahimi S, Rasti A. The efficacy of acceptance and commitment therapy on metacognitions and anxiety in women outpatients with generalized anxiety disorder in Iran. Can. J. Counsell. Psychother. 2017;51:207–216. [Google Scholar]
- 65.Gloster AT, et al. Treating treatment-resistant patients with panic disorder and agoraphobia using psychotherapy: A randomized controlled switching trial. Psychother. Psychosom. 2015;84:100–109. doi: 10.1159/000370162. [DOI] [PubMed] [Google Scholar]
- 66.Goldin PR, et al. Group CBT versus MBSR for social anxiety disorder: A randomized controlled trial. J. Consult. Clin. Psychol. 2016;84:427–437. doi: 10.1037/ccp0000092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hayes-Skelton SA, Roemer L, Orsillo SM. A randomized clinical trial comparing an acceptance-based behavior therapy to applied relaxation for generalized anxiety disorder. J. Consult. Clin. Psychol. 2013;81:761–773. doi: 10.1037/a0032871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Herbert JD, et al. Randomized controlled trial of acceptance and commitment therapy versus traditional cognitive behavior therapy for social anxiety disorder: Symptomatic and behavioral outcomes. J. Contextual Behav. Sci. 2018;9:88–96. doi: 10.1016/j.jcbs.2018.07.008. [DOI] [Google Scholar]
- 69.Hoge EA, et al. Randomized controlled trial of mindfulness meditation for generalized anxiety disorder: effects on anxiety and stress reactivity. J. Clin. Psychiatry. 2013;74:786–792. doi: 10.4088/JCP.12m08083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ivanova E, et al. Guided and unguided Acceptance and Commitment Therapy for social anxiety disorder and/or panic disorder provided via the Internet and a smartphone application: A randomized controlled trial. J. Anxiety Disord. 2016;44:27–35. doi: 10.1016/j.janxdis.2016.09.012. [DOI] [PubMed] [Google Scholar]
- 71.Khoramnia S, et al. The effectiveness of acceptance and commitment therapy for social anxiety disorder: A randomized clinical trial. Trends Psychiatry Psychother. 2020;42:30–38. doi: 10.1590/2237-6089-2019-0003. [DOI] [PubMed] [Google Scholar]
- 72.Kocovski NL, Fleming JE, Hawley LL, Huta V, Antony MM. Mindfulness and acceptance-based group therapy versus traditional cognitive behavioral group therapy for social anxiety disorder: a randomized controlled trial. Behav. Res. Ther. 2013;51:889–898. doi: 10.1016/j.brat.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 73.Koszycki D, Benger M, Shlik J, Bradwejn J. Randomized trial of a meditation-based stress reduction program and cognitive behavior therapy in generalized social anxiety disorder. Behav. Res. Ther. 2007;45:2518–2526. doi: 10.1016/j.brat.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 74.Koszycki D, Guérin E, DiMillo J, Bradwejn J. Randomized trial of cognitive behaviour group therapy and a mindfulness-based intervention for social anxiety disorder: Preliminary findings. Clin. Psychol. Psychother. 2021;28:200–218. doi: 10.1002/cpp.2502. [DOI] [PubMed] [Google Scholar]
- 75.Koszycki D, et al. Preliminary Investigation of a Mindfulness-Based Intervention for Social Anxiety Disorder That Integrates Compassion Meditation and Mindful Exposure. J. Alternat. Complement. Med. (New York, NY) 2016;22:363–374. doi: 10.1089/acm.2015.0108. [DOI] [PubMed] [Google Scholar]
- 76.Ninomiya A, et al. Effectiveness of mindfulness-based cognitive therapy in patients with anxiety disorders in secondary-care settings: A randomized controlled trial. Psychiatry Clin Neurosci. 2020;74:132–139. doi: 10.1111/pcn.12960. [DOI] [PubMed] [Google Scholar]
- 77.Piet J, Hougaard E, Hecksher MS, Rosenberg NK. A randomized pilot study of mindfulness-based cognitive therapy and group cognitive-behavioral therapy for young adults with social phobia. Scand. J. Psychol. 2010;51:403–410. doi: 10.1111/j.1467-9450.2009.00801.x. [DOI] [PubMed] [Google Scholar]
- 78.Roemer L, Orsillo SM, Salters-Pedneault K. Efficacy of an acceptance-based behavior therapy for generalized anxiety disorder: evaluation in a randomized controlled trial. J. Consult. Clin. Psychol. 2008;76:1083–1089. doi: 10.1037/a0012720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Stefan S, Cristea IA, Szentagotai Tatar A, David D. Cognitive-behavioral therapy (CBT) for generalized anxiety disorder: Contrasting various CBT approaches in a randomized clinical trial. J. Clin. Psychol. 2019;75:1188–1202. doi: 10.1002/jclp.22779. [DOI] [PubMed] [Google Scholar]
- 80.Vollestad J, Sivertsen B, Nielsen GH. Mindfulness-based stress reduction for patients with anxiety disorders: Evaluation in a randomized controlled trial. Behav. Res. Ther. 2011;49:281–288. doi: 10.1016/j.brat.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 81.randomised controlled trial Wong, S. Y. et al. Mindfulness-based cognitive therapy v. group psychoeducation for people with generalised anxiety disorder. Br. J. Psychiatry. 2016;209:68–75. doi: 10.1192/bjp.bp.115.166124. [DOI] [PubMed] [Google Scholar]
- 82.Hunot V, et al. 'Third wave' cognitive and behavioural therapies versus other psychological therapies for depression. Cochrane Database Syst. Rev. 2013;20:CD008704. doi: 10.1002/14651858.CD008704.pub2. [DOI] [PubMed] [Google Scholar]
- 83.Schulz, K. F., Altman, D. G., Moher, D. & Group, C CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. PLoS Med. 2010;7:e1000251. doi: 10.1371/journal.pmed.1000251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Furukawa TA, et al. Waiting list may be a nocebo condition in psychotherapy trials: a contribution from network meta-analysis. Acta Psychiatr. Scand. 2014;130:181–192. doi: 10.1111/acps.12275. [DOI] [PubMed] [Google Scholar]
- 85.Cuijpers P, Quero S, Papola D, Cristea IA, Karyotaki E. Care-as-usual control groups across different settings in randomized trials on psychotherapy for adult depression: a meta-analysis. Psychol. Med. 2021;51:634–644. doi: 10.1017/s0033291719003581. [DOI] [PubMed] [Google Scholar]
- 86.Watts SE, Turnell A, Kladnitski N, Newby JM, Andrews G. Treatment-as-usual (TAU) is anything but usual: A meta-analysis of CBT versus TAU for anxiety and depression. J. Affect. Disord. 2015;175:152–167. doi: 10.1016/j.jad.2014.12.025. [DOI] [PubMed] [Google Scholar]
- 87.Bandelow B, et al. Efficacy of treatments for anxiety disorders: A meta-analysis. Int. Clin. Psychopharmacol. 2015;30:183–192. doi: 10.1097/yic.0000000000000078. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data and material analyzed during the current study are available from the corresponding author on request.
The RevMan code used for the current study is available from the corresponding author on request.