Abstract
Background
Early intraoperative hypotension (eIOH) is a common complication of general anesthesia and is significantly associated with postoperative morbidity and mortality. The incidence of eIOH was high, especially in resource-limited settings. Identifying the factors associated with the occurrence of eIOH might allow avoidance and planning of a timely treatment of it.
Objective
To assess the incidence of early intraoperative hypotension and its associated factors among surgical patients undergoing Surgical procedures under general anesthesia at XX Comprehensive Specialized Hospital, North-central Ethiopia, 2021.
Methods
A total of 424 surgical patients under general anesthesia were included in this prospective observational study. The data were collected by a structured questionnaire. Variables with p-values of less than 0.2 in the bivariable logistic regression were fitted to multivariable logistic regression. Data was presented in odds ratios with a 95% confidence interval. Descriptive statistics were used to summarize data.
Results
The incidence of early intra-operative hypotension (eIOH) was 21.2%. In this study older age (age≥ 60 years) (AOR: 2.063 (95% CI;1.194, 3.563)), ASA physical status (AOR: (II2.259 (95% CI;1.229, 4.153)), III(AOR: 2.810 (95% CI;1.319, 5.986)), a BMI of 25–29.9 kg/m2 (AOR: 2.098 (1.128, 3.901), a BMI of ≥30 kg/m2 (AOR: 3.090 (95% CI;1.324, 7.210)), emergency surgical procedures (AOR: 2.215 (95% CI;1.287, 3.810)), the estimated blood loss greater than 500 ml (AOR: 2.510 (95% CI;1.478, 4.261)) were found to be independent factors of eIOH.
Conclusion
This study revealed that the incidence of eIOH was high (21.2%). Older age, ASA II and III, BMI ≥25, emergency surgical procedures, and a significant amount of blood loss (EBL ≥500 ml) were the main predictors of an increased occurrence of eIOH.
Keywords: Early intraoperative hypotension, General anesthesia, Surgical procedures
Highlights
-
•
Early intraoperative hypotension is associated with postoperative morbidity and mortality.
-
•
Emergency surgical procedures, and a significant amount of blood loss are the main predictors of an increased occurrence of eIOH.
-
•
Thyroidectomy has a relatively short duration and less amount of estimated blood loss when compared to major surgical procedures.
-
•
The occurrence of eIOH after general anesthesia for general surgery is a common problem.
-
•
Arterial hypotension in patients undergoing surgery under general anesthesia usually described by the very general term intraoperative hypotension.
1. Introduction
There were a variety of definitions for eIOH. Hypotension was defined as either mean arterial blood pressure (MAP) decrease of >40% and MAP <70 mm Hg or MAP<60 mm Hg. A decline in arterial blood pressure of 30% from the preoperative reading value is another definition of it. The other definition of eIOH is a decrement in systolic blood pressure SBP less than 90 mmHg.
In this study, early intraoperative hypotension (eIOH) was defined as a decrease in systolic blood pressure SBP< 90 mmHg, which was supported by recent literature that might lead to similar conclusions for having postoperative IOH-related risk of morbidity and mortality in contrast to a decline of arterial blood pressure from a baseline [[1], [2], [3]].Early intraoperative hypotension has been associated with adverse outcomes like kidney failure, myocardial injury, and mortality. Therefore prevention of early IOH may be a key in improving patient outcomes [4].
Arterial hypotension in patients undergoing surgery under general anesthesia usually described by the very general term ‘intraoperative hypotension (IOH) is highly prevalent and associated with unfavorable patient outcomes. An arterial blood pressure decline below the lower limit of the vascular autoregulation curve might lead to ischemia of vital organs (i.e. Heart, Brain, and Kidney) [5]. An association between intraoperative hypotension and adverse outcomes remains debatable and there is no consensus on the lowest acceptable intraoperative blood pressure. Data indicate a higher mortality rate in the elderly when there is a decrease in SBP of 40–45% from the preoperative baseline. However, recent reports indicated that intraoperative hypotension contributes to troponin elevation and is associated with increased 30-day mortality [6].
In recent years, evidences are growing that the development of IOH is associated with adverse postoperative outcomes in terms of both morbidity and mortality. In a large observational study in 10,440 adult patients undergoing non-cardiac surgery increased durations of IOH (defined by MAP thresholds between 50 and 80 mmHg) were strongly associated with 30-day mortality. In another large retrospective cohort study in 18,756 patients undergoing non-cardiac surgery these findings again confirmed the case, as an increase in 30-day mortality was found for patients with either SBP <70 mmHg, MAP <49 mmHg, or DBP <30 mmHg for at least 5 min.
Multiple other studies have shown the association between IOH and postoperative morbidity in terms of myocardial and acute kidney injury and possibly for the occurrence of ischemic stroke too. Importantly, these studies also demonstrated that even short instances of IOH (in some studies as short as 1 min) were associated with adverse outcomes. For example in one of these studies performed in 33,330 patients underwent non-cardiac surgery, the odds ratio of postoperative myocardial injury and kidney injury when MAP was lower than 55 mmHg for only 1–5 min. Moreover, even short periods of post-induction hypotension before surgical incision are associated with postoperative acute kidney injury [4].
Intraoperative blood pressures, MAP less than 55 mmHg was associated with the development of acute kidney injury, myocardial injury, and cardiac complications [7].
Arterial hypotension during the early phase of anesthesia can lead to adverse outcomes such as a prolonged postoperative stay or even death. Predicted hypotension during anesthesia induction is complicated by its diverse causes [8].
The occurrence of eIOH after general anesthesia for general surgery is a common problem, especially in resource-limited settings like ours. Knowing the incidence and associated factors causing eIOH helps urgent need of safety and treatment in the service of anesthesia and surgery. This research can also help as formulate baseline information for future researches in Ethiopia. This study will help to determine the incidence and factors associated with eIOH in surgical procedures under general anesthesia in XX Comprehensive Specialized Hospital.
2. Methods and materials
2.1. Study area and period
XX compressive specialized Hospital is a public Hospital established in 1934 and located in South Gonder Zone, Amara region 667 km northwest of Addis Ababa, the capital city of Ethiopia at Debre Tabor town which is 97 km to the southwest of Bahir Dar, the capital city of Amara region. According to the 2007 census, the total population of this town was 155,596. The study was conducted in Debre Tabor Town at XX Referral Hospital 2021 GC. It has one referral hospital, and its altitude of 2706 m or 8878 feet above sea level [9]. The hospital has 6 operation rooms which are divided into specialties i.e. 2 rooms for general surgery, 1 room for obstetrics, 1 room for gynecological procedures, and 2 rooms for orthopedics. So, the study participants were taken from any surgery performed with induction agents as propofol, ketamine, and thiopental with intubating relaxation by suxamethonium, and the study would have been carried out from January 1 to April 25/2021 GC.
2.2. Study design
A prospective Observational study design was used, this study has been registered in a research registry http://www.researchregistry.com with a registry number 6911.
Our work is fully compliant with the STROCSS criteria www.strocssguideline.com, in which a completed STROCSS checklist stating the page numbers(Agha R, Abdall-Razak A, Crossley E, Dowlut N, Iosifidis C and Mathew G, for the STROCSS Group. The STROCSS 2019 Guideline: Strengthening the Reporting of Cohort Studies in Surgery. International Journal of Surgery 2019; 72:156–165).
2.3. Population
2.3.1. Source of population
All elective and emergency surgical patients who would undergo surgery under general anesthesia.
2.3.2. Study population
All elective and emergency surgical patients who would undergo surgery under general anesthesia met the inclusion criteria during the study period.
2.4. Variables
2.4.1. Dependent variable
Early intraoperative Hypotension (Yes/No)
2.4.2. Independent variables
Section 1: demographic variables; Age, sex, ASA physical status, BMI (Kg/m2), patient has any co morbidity, Use of chronic medications
Section 2: Surgery-related variables: Surgeon experience, Planned procedure, Urgency of the procedure, Estimated blood loss, Intraoperative positioning, Duration of surgery,
Section 3: Anesthetic related variables:Anesthetist experience, Premedication, Preoperative fluid intake, Intravenous induction agent, Analgesics used, Muscle relaxant used, ETT size, Number of Intubation attempts, Intraoperative fluid, Intraoperative vasoactive agent.
2.5. Sampling size determination and sampling technique
2.5.1. Sampling size determination
The sample size was determined by taking the following assumption; since there is no previous study conducted in Ethiopia. We will assume the proportion is 50%, confidence interval of 95% and margin of error of to be tolerated 0.05%.The sample size to be taken for the study was determined using the formula.
Whereas, n = sample size; Z = confidence interval (1.96) for 95% confidence interval; P = estimated prevalence (0.5); d = margin of sampling error to be tolerated (0.05).
n= (1.96)20.5(1–0.5)/0.052–385, by adding 10% non-response rate the total sample size was 424.
2.5.2. Sampling technique
The final study subjects were chosen by a consecutive convenience sampling technique. The study units that happen to be available at the time of data collection were the participants of the study.
2.6. Inclusion and exclusion criteria
2.6.1. Inclusion criteria
All age ≥18years patients who came to OR for elective and emergency surgery under GA during the study period were included.
2.6.2. Exclusion criteria
-
✓
Shocked patient
-
✓
Pregnant mother
-
✓
Cardiac patient
-
✓
ASA IV and more
-
✓
Two or more intubation attempts
2.7. Data collection technique and instrument
Data was collected using structured questionnaires prepared in English. Data was collected by trained anesthetists. the study tool includes demographic data of the study participants (age, sex, ASA physical status, BMI (kg/m2), patient has any comorbidity, use of chronic medications), surgery-related data of the study participants (surgeon experience, planned procedure, urgency of the procedure, estimated blood loss, intraoperative positioning, duration of surgery), and anesthetic related data of the study participant (anesthetist experience, premedication, preoperative fluid intake, intravenous induction agent, analgesics used, muscle relaxant used, ETT size, number of intubation attempts, intraoperative fluid, intraoperative vasoactive agent).This tool was developed after searching various literatures related to this topic [2,10,5,11,12,13].
2.8. Ethical considerations
Ethical approval was obtained from the Ethical Review Committee of XXU. A formal letter was written to XXCSH. Permission was asked from the responsible Authorities of DTCSH. Written consent was obtained from each participant after giving brief explanation about the objective (purpose) and benefit of the study as clearly as possible to the study participants.
2.9. Data quality control and assurance
To ensure the quality of data, a pre-test of the questionnaire was performed on 5% of study populations who fulfill the inclusion criteria at CC specialized and teaching hospital. The completed questionnaire would have been submitted and reviewed daily to avoid loss of data. Close supervision and daily information exchange including by telephone would have been used as a means to correct problems during the data collection period. Data consistency and completeness would have been made throughout the data collection, data entry, and analysis.
2.10. Data processing and analysis
The data were coded and entered and in SPSS version 25 statistics software for analysis. The association between the dependent variable (eIOH) with independent variables was analyzed by bivariable logistic regression and multivariable logistic regression. Variables with p-values of less than 0.2 in the bivariable logistic regression were fitted to multivariable logistic regression. Data was presented in Odds ratios with a 95% confidence interval. Descriptive statistics were be used to summarize data. Tables were used to present the data.
2.11. Operational definitions
Early intraoperative hypotension: Is a systolic blood pressure less than 90 mmHg during the first 30min of surgery [5].
Baseline blood pressure: The measurement of arterial blood pressure taken before the induction of anesthesia.
3. Results
3.1. Demographic and patient-related data of the study participants
Four hundred twenty-four adult elective and emergency surgical patients under general anesthesia took part in this study. Among the participants, 59.9% were male. In this study, 70.75% were ASA I, and the majority (85.85%) did not have co morbidities (Table 1).
Table 1.
Demographic and patient-related data in patients undergoing surgical procedures under general anesthesia at XX Comprehensive Specialized Hospital, 2021 (N = 424).
| Variables | Presence of eIOH |
Total, No. (%) |
||
|---|---|---|---|---|
| Yes, No. (%) | No, No. (%) | |||
| Age (Years) (n = 424) |
19–59 | 48(11.32%) | 261(61.55%) | 309 (72.88%) |
| ≥60 | 42(9.9%) | 73(17.22%) | 115(27.12%) | |
| Sex | Male | 60(14.15%) | 194(45.75%) | 254(59.9%) |
| Female | 30(7%) | 140(33%) | 170(40.1%) | |
| ASA Physical status | ASA I | 46(10.85%) | 254(59.9%) | 300(70.75%) |
| ASA II | 27(6.37%) | 54(12.7%) | 81(19.11%) | |
| ASA III | 17(4%) | 26(6.13%) | 43(10.14%) | |
| BMI (Kg/m2) | 18.5–24.9 | 49(11.56%) | 270(63.7%) | 319(75.23%) |
| 25–29.9 | 28(6.6%) | 47(11%) | 75(17.69%) | |
| ≥30 | 13(3.08%) | 17(4%) | 30(7.08%) | |
| Presence of co morbid disease | NO | 72(17%) | 292(68.87%) | 364(85.85%) |
| Yes | 18(4.24%) | 42(9.9%) | 60(14.15%) | |
| Use of chronic anti-hypertension medications | NO | 75(17.7%) | 299(70.5%) | 374(88.2%) |
| Yes | 15(3.54%) | 35(8.25%) | 50(11.8%) | |
3.2. Surgery-related data of study participants
From 424 surgical patients majority of the surgery constituents abdominal and elective surgical procedure accounts 349(82.32%) and 307(72.4%) respectively and incidence of early intraoperative hypotension during emergency surgery accounts 41(9.67%) (Table 2).
Table 2.
Surgery-related data in patients undergoing surgical procedures under general anesthesia at XX Comprehensive Specialized Hospital, 2021 (N = 424).
| Variables | Presence of eIOH |
Total | ||
|---|---|---|---|---|
| Yes | no | |||
| Type of surgery | Abdominal | 69(16.27%) | 280(66%) | 349(82.32%) |
| Gynecological | 15(3.53%) | 36(8.46%) | 51(12.02%) | |
| Orthopedics | 6(1.4%) | 18(4.24%) | 24(5.66%) | |
| Urgency | Elective | 49(11.56%) | 258(60.85%) | 307(72.4%) |
| Emergency | 41(9.67%) | 76(17.9%) | 117(27.6%) | |
| Positioning | Supine | 72(17%) | 283(66.7%) | 355(83.73%) |
| Lateral | 18(4.24%) | 51(12%) | 69(16.27%) | |
| EBL | <500 ml | 47(11.08%) | 250(59.96%) | 297(70.05%) |
| ≥500 ml | 43(10.14%) | 84(19.81%) | 127(29.95%) | |
| Surgeon experience (years | 0–3 | 12(2.8%) | 63(14.9%) | 75(17.7%) |
| 4–6 | 60(14.1%) | 183(43.2%) | 243(57.3%) | |
| ≥7 | 18(4.3%) | 88(20.7%) | 106(25%) | |
| Duration of surgery (minute | <60min | 38(8.96%) | 152(3.85%) | 190(44.81%) |
| ≥60min | 52(12.27%) | 182(42.92%) | 234(55.19%) | |
3.3. Anesthetic-related data of the study participants
The majority of study participants (41.04%) were induced ketamine. The majority of study participants (89.15%) did not take vasopressors, and most of surgical patients (67.69%) took less than 1000 ml of crystalloids in the intraoperative period (Table 3).
Table 3.
Anesthetic-related data in patients undergoing surgical procedures under general anesthesia at XX Comprehensive Specialized Hospital, 2021 (N = 424).
| Variables | Presence of eIOH |
Total | ||
|---|---|---|---|---|
| Yes | No | |||
| Preoperative fluid intake | <1000 ml | 60(14.15%) | 222(52.36%) | 282(66.51%) |
| 1000 ml-2000 | 18(4.24%) | 89(21%) | 107(25.24%) | |
| 2000–3000 ml | 12(2.83%) | 23(5.42%) | 35(8.25%) | |
| Aspiration prophylaxis | NO | 36(8.5%) | 109(25.7%) | 145(34.2%) |
| Metoclopramide | 54(12.7%) | 225(53%) | 279(65.8%) | |
| Intraoperative analgesics used | Opioids | 51(12%) | 159(37.5%) | 210(49.52%) |
| Diclofenac | 16(3.77%) | 69(16.28%) | 85(20.05%) | |
| Opioids & Diclofenac | 23(5.43%) | 106(25%) | 129(30.43%) | |
| IV induction agent | Ketamine | 36(8.49%) | 138(32.54%) | 174(41.04%) |
| Propofol | 30(7.07%) | 73(17.2%) | 103(24.3%) | |
| Ketofol | 24(5.66%) | 123(29%) | 147(34.66%) | |
| Muscle relaxant used | Suxamethonium | 18(4.24%) | 81(19.1%) | 99(23.35%) |
| Suxamethonium & Vecuronium | 72(16.98%) | 253(59.67%) | 325(76.65%) | |
| ETT size | 6.5 | 18(4.24%) | 74(17.45%) | 92(21.7%) |
| 7.0 | 42(9.9%) | 173(40.8%) | 215(50.7%) | |
| 7.5 | 30(7.07%) | 87(20.5%) | 117(27.6%) | |
| Number of intubation attempts | Single | 72(16.98%) | 282(66.5%) | 354(83.5%) |
| Multiple | 18(4.24%) | 52(12.26%) | 70(16.5%) | |
| Amount intraoperative fluid intake | <1000 ml | 54(12.7%) | 233(54.95%) | 287(67.69%) |
| 1000–2000 ml | 36(8.5%) | 101(23.8%) | 137(32.31%) | |
| Vasoactive agent used | No | 78(18.4%) | 300(70.75%) | 378(89.15%) |
| Yes | 12(2.83%) | 34(8.02%) | 46(10.85%) | |
| Anesthetist experience (years | 0–3 | 12(2.83%) | 52(12.26%) | 64(15.09%) |
| 4–6 | 60(14.2%) | 244(57.5%) | 304(71.7%) | |
| ≥7 | 18(4.24%) | 38(8.97%) | 56(13.21%) | |
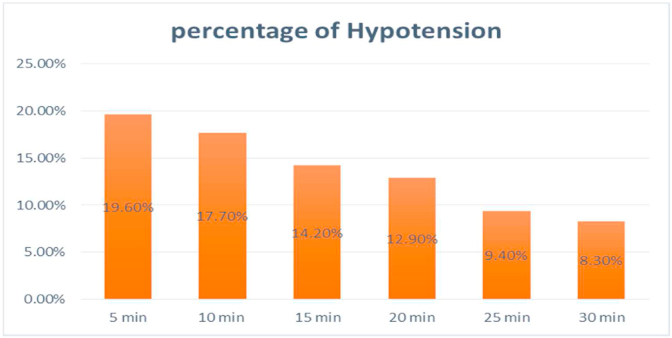
3.4. The incidence of early intraoperative hypotension
In this study, Early intraoperative hypotension was found in 90 (21.2%) of study participants. The majority of (19.6%) of the eIOH occurred within 5 min after the induction of anesthesia (Fig. 1).
Fig. 1.
The incidence of early intraoperative hypotensionin patients undergoing surgical procedures under general anesthesia at XX Comprehensive Specialized Hospital, 2021 (N = 424).
3.5. The variables associated with the eIOH
In this study older age 2 times (age≥ 60 years) (AOR: 2.063 (95% CI;1.194, 3.563)) more likely to develop eIOH, ASA II patients had 2.2 times (AOR: 2.259 (95% CI;1.229, 4.153)) more likely to develop eIOH as compared to ASA I patients, ASA III patients were 2.8 times (AOR: 2.810 (95% CI;1.319, 5.986)) more likely to develop eIOH when compared to ASA I patients, a BMI of 25–29.9 kg/m2 was 2 times (AOR: 2.098 (1.128, 3.901) more likely to develop eIOH when compared with patients having normal BMI, a BMI of ≥30 kg/m2 was 3 times (AOR: 3.090 (95% CI;1.324, 7.210)) more likely to develop eIOH when compared with patients having normal BMI, emergency surgical procedures were 2.2 times (AOR: 2.215 (95% CI;1.287, 3.810)) more likely to develop eIOH when compared with elective surgical procedures, the estimated blood loss greater than 500 ml was 2.5 times (AOR: 2.510 (95% CI;1.478, 4.261)) more likely to develop eIOH when compared with patients having an estimated blood loss less than 500 ml (Table 4).
Table 4.
Variables associated with the early intraoperative hypotensionin patients undergoing surgical procedures under general anesthesia at XX Comprehensive Specialized Hospital, 2021 (N = 424).
| Variables | Presence of eIOH |
COR (95% CI) | AOR (95% CI) | P-value | ||
|---|---|---|---|---|---|---|
| Yes | No | |||||
| Age (Years) | 19–59 | 48 | 261 | 1 | 1 | |
| ≥60 | 42 | 73 | 3.128 (1.919,5.100) | 2.063 (1.194, 3.563) | 0.009 | |
| ASA Physical status | ASA I | 46 | 254 | 1 | 1 | |
| ASA II | 27 | 54 | 2.761 (1.579,4.827) | 2.259 (1.229, 4.153) | 0.009 | |
| ASA III | 17 | 26 | 3.610 (1.816,7.178) | 2.810 (1.319, 5.986) | 0.007 | |
| BMI (Kg/m2) | 18.5–24.9 | 49 | 270 | 1 | 1 | |
| 25–29.9 | 28 | 47 | 3.283 (1.879,5.736) | 2.098 (1.128, 3.901) | 0.019 | |
| ≥30 | 13 | 17 | 4.214 (1.925,9.226) | 3.090 (1.324, 7.210) | 0.009 | |
| Urgency | Elective | 49 | 258 | 1 | 1 | |
| Emergency | 41 | 76 | 2.840 (1.745,4.624) | 2.215 (1.287, 3.810) | 0.004 | |
| EBL (ml) | <500 | 47 | 250 | 1 | 1 | |
| ≥500 | 43 | 84 | 2.723 (1.682,4.408) | 2.510 (1.478, 4.261) | 0.001 | |
4. Discussion
Early intraoperative hypotension is associated with postoperative morbidity and mortality(8,9,19,21–23). In this study, we found that the incidence of early intraoperative hypotension within 30 min after general anesthesia in major surgery was 21.2%. In line with our finding, a study conducted by Su et al. [5] found that the incidence of eIOH was 24.7%. Incongruent to our result, Kalezic et al. [11] reported that the incidence of IOH was lower (6.5%) as compared to our finding. This might be due to differences in the type of surgery (thyroid surgery). Thyroidectomy has a relatively short duration and less amount of estimated blood loss when compared to major surgical procedures (e.g. abdominal) in which the operation can last a longer duration (several hours) and might have a significant blood loss. Jor et al., and Cheung et al. observed that there was a higher incidence of IOH (55.4% [14], 36.5% [10]) as compared to our findings. This difference might be due to most of the patients were induced with propofol.
In this study, early intraoperative hypotension (eIOH) was defined as a decrease in systolic blood pressure SBP<90 mmHg. Some recent studies support this approach, revealed that definitions of eIOH using SBP less than 90 mmHg might lead to similar conclusions for having postoperative IOH-related risk of morbidity and mortality when compared with a lower arterial blood pressure from baseline (SBP >30% decline from preoperative arterial BP) [2,3].
In this study older age (age≥ 60 years), ASA physical status (II, III), BMI (>25 kg/m2), emergency surgical procedures, estimated blood loss greater than 500 ml were found to be independent factors of an increased occurrence of eIOH.
In this study ASA physical status (II, III) was found to be an independent factor of an increased occurrence of eIOH. In line with this study, Su et al. [5] revealed that ASA physical status affects the occurrence of eIOH. In contrast to our result, a study conducted by Stojanovic et al. [11] ASA physical status did not affect the occurrence of eIOH, this might be due to they included relatively younger patients.
In this study older age (age ≥60 years) was an independent risk factor for eIOH. Similarly, a study conducted by Su et al. [5] found that older age was associated with an increased occurrence of eIOH. Another recent study conducted by Reich et al. [15] and Cheung et al. [14] also revealed that there was an association between eIOH and ages of >65 and > 50 years respectively.
In our study emergency surgical procedures were associated with the occurrence of eIOH. In line with this study, Su et al. revealed that emergency surgical procedures were the predictors of eIOH(6). This finding might reflect the fact that patients undergoing emergency surgical procedures compared with elective surgical procedures are more likely to develop cardiovascular dysfunction.
In this study BMI >25 kg/m2 was found to be independent factors of an increased occurrence of eIOH. In contrast to our result Kalezic et al. [11] revealed that BMI did not affect the occurrence of eIOH, the possible explanation for this difference could be thyroidectomy requires a relatively short duration of time and less amount of estimated blood loss in contrast with our study that most of the surgical procedures were abdominal surgeries, which can last for a prolonged period and having a significant blood loss.
The definition of hypotension is the main problem of this study. The variability of definitions of eIOH, significantly impacts comparisons and interpretations of the results of studies concerning the occurrence of eIOH(2). The other limitation could be this study does not take into consideration the duration of hypotension, and managing eIOH according to the available medical equipment and drugs (e.g. adrenaline is a frequently administered drug for hypotension) could be the limitations of this study.
5. Conclusion
The incidence of eIOH was high (21.2%). Older age, ASA II and III, BMI ≥25, emergency surgical procedures, and a significant amount of blood loss (EBL ≥500 ml) were the main predictors of an increased occurrence of eIOH. Identifying those factors might allow the avoidance and planning of a timely treatment of hypotensive episodes during general anesthesia.
Ethical approval
Ethical clearance was obtained from Debre tabor University research review committee.
Sources of funding
No funding is required.
Author contribution
All authors equally contributed to the study concept or design, data searching, data analysis or interpretation, writing the paper.
Guarantor
Mr. Netsanet Temesgen.
Consent
Not applicable for that.
Funding
None.
Declaration of competing interest
The authors declared that there is no conflict of interest.
Acknowledgements
Debre Tabor University for providing internet Access for our work.
All Staff members of Department of Anesthesia from the University for their meticulous help.
Acronyms and abbreviations
- AOR
Adjusted odds ratio
- ASA
American Societies Anesthesiologist
- CI
Confidence interval
- COR
Crud odds ratio
- XXCSH
XX Comprehensive Specialized Hospitals
- eIOH
early Intraoperative Hypotension
- EBL:
Estimated blood loss
- GA
General Anesthesia
- MAP
Mean Arterial Blood Pressure
- OR
Operation Room
- SBP
Systolic Blood Pressure
- SPSS
Statistical Package for Social Sciences
Provenance and peer review
Not commissioned, externally peer-reviewed.
References
- 1.Ranck M.F., Adtke F.M.R., Rahs C.P., Eeling M.S., Apkalla N.P. Documented intraoperative hypotension according to the three most common definitions does not match the application of antihypotensive medication. J. Int. Med. Res. 2011;39:846–856. doi: 10.1177/147323001103900318. [DOI] [PubMed] [Google Scholar]
- 2.Bijker J.B., Van Klei W.A., Kappen T.H., Van Wolfswinkel L., Moons K.G.M., Kalkman C.J. Incidence of intraoperative hypotension as a function of the chosen definition. Anesthesiology. 2007;107(2):213–220. doi: 10.1097/01.anes.0000270724.40897.8e. [DOI] [PubMed] [Google Scholar]
- 3.Salmasi V., Maheshwari K., Dongsheng Y., Mascha E.J., Singh A., Sessler D.I. Thresholds , and acute kidney and myocardial injury after noncardiac surgery. Anesthesiology. 2017;126(1):47–65. doi: 10.1097/ALN.0000000000001432. [DOI] [PubMed] [Google Scholar]
- 4.Vos J.J., Scheeren T.W.L. Intraoperative hypotension and its prediction. Indian J. Anaesth. 2019;63:877–885. doi: 10.4103/ija.IJA_624_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Su S., Brechnitz S., Wagner J.Y., Reese P.C., Pinnschmidt H.O., Reuter D.A. Post-induction hypotension and early intraoperative hypotension associated with general anaesthesia. Br J ofAnaesthesia. 2017;119(1):57–64. doi: 10.1093/bja/aex127. [DOI] [PubMed] [Google Scholar]
- 6.Granath F., Sahle A., Bell M., Hallqvist L., Ma J. Intraoperative hypotension is associated with myocardial damage in noncardiac surgery. Eur. J. Anaesthesiol. 2016;33:450–456. doi: 10.1097/EJA.0000000000000429. [DOI] [PubMed] [Google Scholar]
- 7.Walsh M., Kurz A., Turan A., Rodseth R.N., Cywinski J., Thabane L. Relationship between intraoperative mean arterial pressure and clinical outcomes after noncardiac surgery toward. Anesthesiology. 2013;119(3):507–515. doi: 10.1097/ALN.0b013e3182a10e26. [DOI] [PubMed] [Google Scholar]
- 8.Reum A., Id K., Lee J., Jung W., Lee M., Young S. Development of a prediction model for hypotension after induction of anesthesia using machine learning. PLoS One [Internet. 2020;15(4) doi: 10.1371/journal.pone.0231172. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Langer T., Santini A., Zadek F., Chiodi M., Pugni P., Cordolcini V. Intraoperative hypotension is not associated with postoperative cognitive dysfunction in elderly patients undergoing general anesthesia for surgery : results of a randomized controlled pilot trial. J Clin Anesth [Internet. 2019;52:111–118. doi: 10.1016/j.jclinane.2018.09.021. Available from: [DOI] [PubMed] [Google Scholar]
- 10.Jor O., Maca J., Koutna J., Gemrotova M., Vymazal T., Litschmannova M. Hypotension after induction of general anesthesia : occurrence , risk factors , and therapy . A prospective multicentre observational study. J Anesth [Internet] 2018;32(5):673–680. doi: 10.1007/s00540-018-2532-6. Available from: [DOI] [PubMed] [Google Scholar]
- 11.Stojanovic M., Paunovic I., Sabljak V. Risk factors for intraoperative hypotension during thyroid surgery. Med Sci Monit. 2013;19:236–241. doi: 10.12659/MSM.883869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khan N.A., Campbell N.R., Frost S.D., Gilbert K., Michota F.A., Usmani A. Risk of intraoperative hypotension with loop diuretics: a randomized controlled trial. Am J Med [Internet] 2010;123(11) doi: 10.1016/j.amjmed.2010.07.019. 1059.e1-1059.e8. Available from: [DOI] [PubMed] [Google Scholar]
- 13.Brabant S.M., Eyraud D. Refractory hypotension after induction of anesthesia in a patient chronically treated with angiotensin receptor antagonists. Anesth. Analg. 1999;89:887–888. doi: 10.1097/00000539-199910000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Cheung C.C., Martyn A., Campbell N., Frost S. Predictors of intraoperative hypotension and bradycardia. Am J Med [Internet] 2015;128(5):532–538. doi: 10.1016/j.amjmed.2014.11.030. Available from: [DOI] [PubMed] [Google Scholar]
- 15.Reich D.L., Hossain S., Krol M., Bernstein A., Bodian C.A. Predictors of hypotension after induction of general anesthesia. Anesth. Analg. 2005;101:622–628. doi: 10.1213/01.ANE.0000175214.38450.91. [DOI] [PubMed] [Google Scholar]