Abstract
Background
While social assistance through the U.S. federal CARES Act provided expanded unemployment insurance benefits during the COVID-19 pandemic until the summer of 2020, it is unclear whether social assistance was sufficient in subsequent months to meet everyday spending needs and to curb the adverse health-related sequelae of financial hardship.
Methods
Using multivariable Poisson log-binomial regression and repeated cross-sectional Household Pulse Survey data between September and December 2020 on 91,222 working-aged U.S. adults and 28,842 adult housing renters, this study explored the associations of financial hardship with mental health outcomes and food and housing insecurity after accounting for receipt of social assistance.
Results
Financial hardship rose progressively from September to December 2020, and disproportionately affected Black non-Hispanic and Hispanic Americans and lower-income households. Experiencing considerable financial hardship (vs no hardship) predicted nearly 3-fold higher risks of anxiety and depressive symptoms (e.g., adjusted prevalence ratio, PR of depression = 2.75, 95% CI = 2.54–2.98, P < .001), a 23-fold higher risk of food insufficiency (PR = 22.71, 95% CI = 15.62–33.01, P < .001), and a 27-fold higher risk of a likely eviction (PR = 27.20, 95% CI = 10.63–69.59, P < .001). Across outcomes, these relationships were stronger at each successively higher level of financial hardship (all P values for linear trend <0.001), and more than offset benefits from social assistance.
Conclusions
Even after accounting for social assistance receipt, working-aged adults experiencing financial hardship had markedly greater risks of anxiety and depressive symptoms, food insufficiency, and an anticipated housing eviction. These findings point to the urgent need for direct and sustained cash relief well in excess of current levels of social assistance to mitigate the pandemic's adverse impacts on the well-being of millions of Americans, including vulnerable minority and low-income populations.
Keywords: Financial hardship, Social assistance, Mental health, Food security, Housing security, COVID-19 pandemic
Introduction
By late January 2021, the coronavirus disease 2019 (COVID-19) pandemic led to the filing of over 75 million unemployment insurance (UI) claims in the United States (U.S.) (U.S. Department of Labor, 2021), and was accompanied by heightened levels of food and housing insecurity (Center on Budget and Policy Priorities, 2021). Through the federal Coronavirus Aid, Relief, and Economic Security (CARES) Act enacted in March 2020, expanded UI benefits consisted of a $600 weekly payment on top of state payments, 13 extra weeks of UI benefits, and broader UI eligibility guidelines (Driessen, 2020). The federal bonus expired in late July 2020, and was followed by a six-week $300 weekly benefit in the majority of states through a federal lost wages assistance program (FEMA, 2021). Other provisions along with a federal housing eviction moratorium implemented in September 2020 expired in late December 2020. In early January 2021, both the U.S. Congress and President Trump approved a $900 billion COVID-19 relief package that included a one-time direct payment of $600 to individuals (with a 2019 adjusted gross income of up to $75,000) and a federal UI bonus of $300 weekly for 11 weeks (Bernard & Lieber, 2021).
UI and social assistance can plausibly reduce financial strain and debt, with associated sequelae of relationship strain and social isolation. In theory, these forms of assistance can thereby offer protection against mental health conditions such as anxiety and depression, food insufficiency, and the inability to afford housing (Haw et al., 2015).
An analysis of data from the U.S. Census Bureau's Household Pulse Survey (HPS) administered in June and July 2020 identified UI receipt as associated with better mental health and lower health-related social needs among working-aged adults (Berkowitz & Basu, 2020). However, since the federal UI bonus subsequently lapsed and was followed by a subsidy considerably smaller in both amount and duration, it is unclear whether social assistance was sufficient in the ensuing months to meet everyday spending needs and to curb adverse sequelae of financial hardship among those experiencing employment-related income loss.
The present study was undertaken to estimate levels of and changes in financial hardship among working-aged Americans with job-related income loss during recent months of the pandemic, and to explore the associations of financial hardship with mental health outcomes and food and housing insecurity after accounting for receipt of social assistance. In light of evidence that health disparities exist by race/ethnicity, including demonstrated independent associations of race/ethnicity and past poverty duration with mental health outcomes such as depression and stronger associations of financial distress with depression among Black vs White Americans (Assari, 2019; Mossakowski, 2008; Riolo et al., 2005), this study further documents levels of financial hardship experienced during the pandemic by race/ethnicity and pre-pandemic household income.
Methods
Study population
Repeated cross-sectional individual-level data were pooled from nationally-representative HPS surveys administered from September 2—December 21, 2020 (U.S. Census Bureau, 2021a). The study population consisted of adults age 18–64 years reporting a loss of household employment income since the beginning of the pandemic (March 13, 2020). For the samples analyzed in multivariable models, data were available on up to 91,222 working-aged adults (representative of 43 million individuals) with income disruption in their households and 28,842 adult housing renters. Aggregate data were also drawn from the HPS public-use survey data tables (December 9—December 21). The HPS used the U.S. Census Bureau's Master Address File as the source of sampled housing units (HUs). The sampling frame was a systematic sample of all eligible HUs. The HPS was conducted online by Qualtrics as the data collection platform. Across data collection periods, survey response rates ranged from 5.3% to 10.6% (U.S. Census Bureau, 2021b).
Predictors
Financial hardship was defined as household difficulty (not at all/a little/somewhat/very difficult) to pay for usual household expenses including food, rent/mortgage, and loans within the previous week. UI receipt was taken as self-reported household receipt of UI benefits since the pandemic began. Supplemental Nutritional Assistance Program (SNAP) receipt was defined as household participation in SNAP and using SNAP benefits to meet spending needs within the previous week (U.S. Census Bureau, 2021b).
Outcomes
Outcomes available through the HPS consisted of the frequency of anxiety and depressive symptoms (using the 2-item Generalized Anxiety Disorder-2 (GAD-2) and Patient Health Questionnaire-2 (PHQ-2), respectively, for scores of 3–6 vs 0–2 to screen for anxiety and depressive disorders, the level of food insufficiency (often or sometimes not enough to eat vs enough to eat), and, among housing renters, the likelihood of being evicted within the next 2 months (very/extremely likely vs somewhat/not at all likely) (U.S. Census Bureau, 2021b). Using a cut-off score of ≥3, the GAD-2 demonstrated the optimal degree of sensitivity and specificity (sensitivity = 0.71, specificity = 0.69), and the PHQ-2 exhibited peak sensitivity and adequate specificity (sensitivity = 0.64, specificity = 0.85). Internal consistency reliability was high for both measures (Cronbach's α = 0.81 and 0.83 for the GAD-2 and PHQ-2, respectively) (Staples et al., 2019).
Statistical analysis
Multivariable Poisson log-binomial regression models were fit to estimate adjusted prevalence ratios (PR) from generalized estimating equations that accounted for repeated measures within individuals and person-level survey weights and provided robust standard errors based on sandwich estimators (Zhu et al., 2018). Binomial rather than multinomial models were applied because health-related outcomes such as anxiety and depression are typically reported as dichotomous, particularly for clinical audiences. All models were adjusted for individual age, age squared, gender, race/ethnicity, marital status, education, 2019 household income, other federal stimulus assistance, household size, presence of children in the household, general health status, state, and survey period. The model for current food insufficiency also controlled for pre-pandemic food insufficiency.
For outcomes, data were missing in 16.1% for anxiety, 16.2% for depression, 9.5% for food insufficiency, and 0.4% for likely housing eviction. For predictors, data were missing in 21.2% for income, 15.8% for health status, 2.5% for difficulty paying expenses, and 0.5% for marital status. Multiple imputation analysis (using 25 multiply imputed datasets and the MCMC algorithm without rounding under a missing at random assumption (Allison, 2005)) and complete case analysis were used to handle missing data for predictor and outcome variables, respectively. All analyses were conducted using SAS version 9.4 (SAS Institute Inc., Cary, NC).
Results
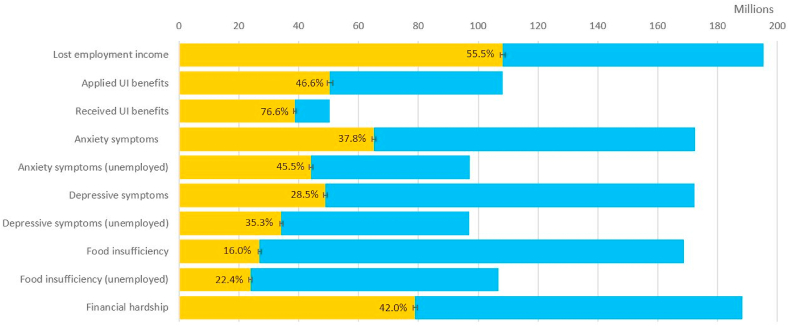
Fig. 1 shows the estimated numbers and survey-weighted percentages of U.S. working-aged adults with employment income loss, receipt/denial of UI benefits, mental health-related symptoms, food insufficiency, and financial hardship in the December 9—December 21 survey period of the HPS (n = 10,139). Over half (55.5%) of working-aged adults (representing more than 108 million adults) experienced job-related income loss in their households since the start of the pandemic. Of those who lost employment income, less than half (46.6%) applied for UI benefits, and of those who applied, 76.6% received UI. More than one-third (37.8%) and one-quarter (28.5%) reported a higher frequency of feeling anxious or depressed (more than half the days/nearly every day vs several days/not at all) over the previous week, respectively. 16.0% (corresponding to 27 million adults) experienced food insufficiency. Over half (51.7%) of renters (representative of 4.8 million adults) indicated a high likelihood of being evicted. 42.0% (corresponding to 79 million adults) reported a higher level of financial hardship (somewhat difficult to very difficult to pay for usual household expenses) over the previous week. All proportions were at least 5 percentage points higher among those with employment income loss (Fig. 1).
Fig. 1.
Estimated Numbers and Percentages of Working-Aged Adults with Household Employment Income Loss, Application for/Receipt of UI Benefits, Mental Health-Related Symptoms, Food Insufficiency, and Financial Hardship During the COVID-19 Pandemic, U.S. Census Bureau Household Pulse Survey, December 2020 a
Abbreviations: COVID-19, coronavirus disease 2019; UI, unemployment insurance.
a Aggregate data were drawn from the U.S. Census Bureau Household Pulse Survey public-use data tables for surveys administered between December 9, 2020 and December 21, 2020 (n = 10,139). All estimates are for adults age 18–64 years except anxiety and depressive symptoms, for which available estimates are for adults age 18–69 years. The combined yellow and blue bars indicate the number of adults (in millions), while the yellow bars alone correspond to estimated proportions reflecting the number of adults as a percentage of the total number of adults in the denominator (e.g., number responding someone in household lost employment income, number who applied for UI benefits, number who responded to the survey item). Anxiety symptoms were measured by a survey item that inquired about the frequency of feeling nervous, anxious, or on edge (more than half the days/nearly every day vs. several days/not at all) over the previous week. Depressive symptoms were measured by a survey item that inquired about the frequency of feeling down, depressed, or hopeless (more than half the days/nearly every day vs. several days/not at all) over the previous week. Financial hardship corresponded to it being somewhat difficult to very difficult (vs not at all difficult or a little difficult) to pay for usual expenses over the previous week. All estimates account for survey weights. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
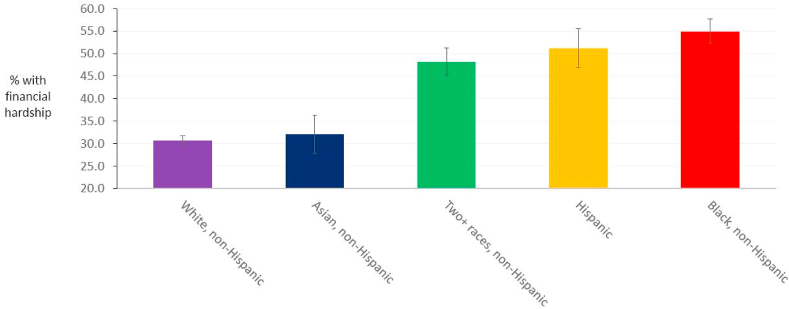
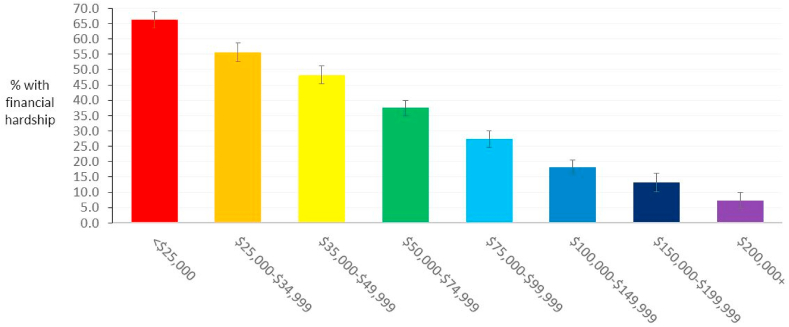
For the same survey period, Fig. 2, Fig. 3 illustrate the variations and patterns in survey-weighted levels of financial hardship by race/ethnicity and pre-pandemic income (2019). In Black non-Hispanic and Hispanic Americans, the estimated prevalences of a higher level of financial hardship were over 50% (54.9% and 51.2%, respectively), compared to 30.6% in White non-Hispanic Americans, respectively (Fig. 2). In those with pre-pandemic income levels of <$25,000, $75,000–99,999, and $200,000+, the estimated prevalences of a higher level of financial hardship varied substantially, from 66.2% to 27.4% and 7.3%, respectively, with evidence of an inverse gradient relationship across all pre-pandemic income levels (Fig. 3). The prevalences of financial hardship were also higher in women than men (39.6% vs 35.3%, respectively) and in households with children than households without children (45.4% vs 32.4%, respectively).
Fig. 2.
Estimated Percentages of Working-Aged Adults Experiencing Household Financial Hardship During the COVID-19 Pandemic. by Race/Ethnicity, U.S. Census Bureau Household Survey, December 2020.a
Abbreviations: COVID-19, coronavirus disease 2019.
a Aggregate data were drawn from the U.S. Census Bureau Household Pulse Survey public-use data tables for surveys administered between December 9, 2020 and December 21, 2020 (n = 10,139). All estimates are for adults age 18–64 years. Financial hardship corresponded to it being somewhat difficult to very difficult (vs not at all difficult or a little difficult) to pay for usual expenses over the previous week. All estimates account for survey weights.
Fig. 3.
Estimated Percentages of Working-Aged Adults Experiencing Household Financial Hardship During the COVID-19 Pandemic. by Pre-Pandemic Household Income Level, U.S. Census Bureau Household Survey, December 2020.a
Abbreviations: COVID-19, coronavirus disease 2019.
a Aggregate data were drawn from the U.S. Census Bureau Household Pulse Survey public-use data tables for surveys administered between December 9, 2020 and December 21, 2020 (n = 10,139). All estimates are for adults age 18–64 years. Financial hardship corresponded to it being somewhat difficult to very difficult (vs not at all difficult or a little difficult) to pay for usual expenses over the previous week. All estimates account for survey weights.
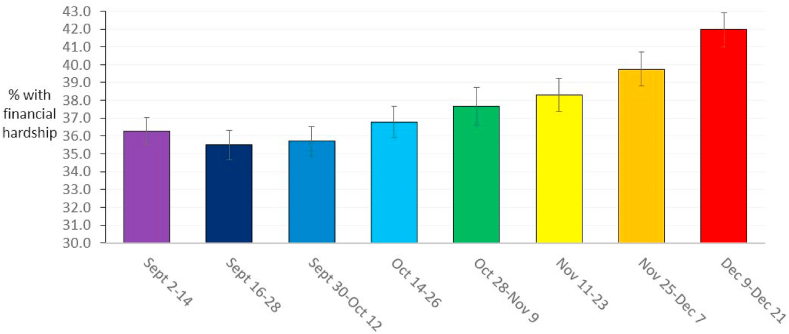
Fig. 4 depicts the estimated survey-weighted national percentages of working-aged adults experiencing household financial hardship (somewhat difficult to very difficult to pay for usual household expenses) by survey period between September 2, 2020 and December 21, 2020. In September 2020, this percentage declined slightly from 36.3% to 35.5%, but then rose progressively during each successive survey period to 42.0% by December 2020. The largest percentage increase (1.4 percentage points) occurred between the two most recent survey periods, suggesting the possibility of an escalating trend (Fig. 4).
Fig. 4.
Estimated Percentages of Working-Aged Adults Experiencing Household Financial Hardship During the COVID-19 Pandemic. by Survey Period, U.S. Census Bureau Household Survey, September–December 2020.a
Abbreviations: COVID-19, coronavirus disease 2019.
a Aggregate data were drawn from the U.S. Census Bureau Household Pulse Survey public-use data tables for surveys administered between September 2, 2020 and December 21, 2020 (with sample sizes in each survey period ranging from 8,057 to 14,876). All estimates are for adults age 18–64 years. Financial hardship corresponded to it being somewhat difficult to very difficult (vs not at all difficult or a little difficult) to pay for usual expenses over the previous week. All estimates account for survey weights.
Weighted descriptive statistics of the regression analysis sample (n = 91,222) are reported in Table S1. The mean age in the full sample was 40.3 years. Slightly greater than half of the sample was female (51.9%). Approximately one-fifth (19.6%) had pre-pandemic household income levels less than $25,000, and over one-third (35.4%) reported substantial difficulty with paying usual expenses.
Table 1 displays the main results from the multivariable-adjusted regression models. Experiencing somewhat of a financial hardship (vs no hardship) was linked to 2-fold higher risks of anxiety and depressive symptoms (e.g., PR for anxiety = 1.96, 95% CI = 1.85–2.08, P < .001), a nearly 12-fold higher risk of food insufficiency (PR = 11.60, 95% CI = 7.99–16.85, P < .001), and a close to 7-fold higher risk of a likely eviction (PR = 6.75, 95% CI = 2.59–17.58, P < .001). Experiencing considerable financial hardship (vs no hardship) predicted nearly 3-fold higher risks of anxiety and depressive symptoms (e.g., PR of depression = 2.75, 95% CI = 2.54–2.98, P < .001), a 23-fold higher risk of food insufficiency (PR = 22.71, 95% CI = 15.62–33.01, P < .001), and a 27-fold higher risk of a likely eviction (PR = 27.20, 95% CI = 10.63–69.59, P < .001) (all P for linear trend <0.001). In the same models, UI receipt (vs no receipt) was associated with a 4–5% lower risk of depressive symptoms (95% CI = 0.92–1.00, P = .04), anxiety symptoms (95% CI = 0.92–0.99, P = .005), and food insufficiency (95% CI = 0.91–1.00, P = .08), and a 25% lower risk of an expected eviction (95% CI = 0.68–0.84, P < .001). SNAP receipt was linked to a 2% lower risk of food insufficiency (95% CI = 0.92–1.03, P = .38).
Table 1.
Financial hardship and social assistance as predictors of mental health, food insufficiency, and likely housing eviction among those with job-related income loss during the COVID-19 pandemic, U.S. Census Bureau Household Pulse Survey, September–December 2020 a.
| Outcome |
||||||||
|---|---|---|---|---|---|---|---|---|
| Anxiety symptoms (n = 76,528) | Depressive symptoms (n = 76,474) | Food insufficiency (n = 82,531) | Likely housing eviction c (n = 28,716) | |||||
| Predictor | Prevalence ratio (95% CI)b | P value | Prevalence ratio (95% CI)b | P value | Prevalence ratio (95% CI)b | P value | Prevalence ratio (95% CI)b | P value |
| Difficulty with paying expenses d | ||||||||
| A little difficult | 1.56 (1.46–1.66) | <.001 | 1.52 (1.40–1.66) | <.001 | 4.79 (3.24–7.08) | <.001 | 2.05 (0.75–5.66) | .16 |
| Somewhat difficult | 1.96 (1.85–2.08) | <.001 | 2.01 (1.86–2.18) | <.001 | 11.60 (7.99–16.85) | <.001 | 6.75 (2.59–17.58) | <.001 |
| Very difficult | 2.61 (2.46–2.76) | <.001 | 2.75 (2.54–2.98) | <.001 | 22.71 (15.62–33.01) | <.001 | 27.20 (10.63–69.59) | <.001 |
| P for trend | – | <.001 | – | <.001 | – | <.001 | – | <.001 |
| Receipt of UI benefits e | 0.95 (0.92–0.99) | .005 | 0.96 (0.92–0.997) | .04 | 0.96 (0.91–1.005) | .08 | 0.75 (0.68–0.84) | <.001 |
| Receipt of SNAP benefits e | – | – | – | – | 0.98 (0.92–1.03) | .38 | – | – |
Abbreviations: CI, confidence interval; COVID-19, coronavirus disease 2019; SNAP, Supplemental Nutrition Assistance Program; UI, unemployment insurance.
All models were adjusted for age, age (Center on Budget and Poli), gender, race/ethnicity, marital status, educational attainment, 2019 household income, use of federal stimulus assistance, household size, presence of children in household, overall health status, state of residence, and survey period. The model for current food insufficiency was also adjusted for food insufficiency prior to March 13, 2020. Participants were surveyed in Phases 2 and 3 of the U.S. Census Bureau Household Pulse Survey (Phase 2 waves: September 2–14, September 16–28, September 30—October 12, October 14–26; Phase 3 waves: October 28—November 9, 2020, November 11—November 23, 2020, November 25—December 7, 2020, December 9—December 21, 2020).
Prevalence ratio point estimates, 95% confidence intervals, and P values were derived from Poisson log-binomial regression models fit using generalized estimating equations that incorporated person weights, repeated measures, and robust standard errors. Missing data were handled using 25 multiple imputation data sets.
This analysis was restricted to housing renters.
The reference category was those reporting it was not at all difficult to pay for usual expenses over the previous week.
The reference category was those reporting no household receipt of corresponding UI or SNAP benefits since March 13, 2020.
Discussion
Principal findings
This large U.S. nationally-representative study reveals high levels of financial hardship among working-aged Americans, that progressively worsened from September to December 2020. Higher levels of financial hardship disproportionately affected Black non-Hispanic and Hispanic Americans, and were inversely linked to pre-pandemic income levels. Even after accounting for social assistance receipt and pre-pandemic socioeconomic position, working-aged adults experiencing financial hardship had markedly greater risks of anxiety or depressive symptoms, food insufficiency, and an anticipated housing eviction. Across outcomes, these relationships were stronger at each successively higher level of financial hardship, and more than offset the corresponding generally modest benefits from UI and SNAP. To the author's knowledge, this represents the first study to explore the potential impacts of financial hardship with mental health and food and housing insecurity during the COVID-19 pandemic in the United States.
Comparison with findings from related studies
The associations with mental health outcomes observed in this study are in keeping with previous linkages of sudden income loss to depression and anxiety in labor market surveys conducted in six European countries in March and April 2020 (Witteveen & Velthorst, 2020). There is also evidence from one study to support that during the period that the CARES Act was in effect during the initial phase of the pandemic, among adults whose families lost work or work-related income due to the pandemic, the level of social assistance including the $600 weekly federal bonus for UI recipients was adequate to meet financial needs (Karpman & Acs, 2020). In that study, UI receipt was linked to a 3-percentage point reduction in the share reporting food insecurity, a 3.7 percentage-point reduction in problems paying utility bills, and reductions of 8.6–15.1 percentage points in the share worrying about meeting basic needs (Karpman & Acs, 2020).
Study strengths and limitations
Strengths of this study include its use of large nationally-representative survey data, as well as data from repeated survey waves that enabled the examination of trends in financial hardship over time. Models also controlled for demographic and socioeconomic factors and state fixed effects to reduce confounding. Finally, the modeling of multiple categories for the financial hardship measure permitted a confirmation of the presence of dose-response relationships.
Nonetheless, there are limitations to this study. Because of the study's cross-sectional and observational design, bias due to reverse causation or confounding cannot be entirely ruled out. Moreover, we were unable to account for the actual monetary amounts of UI and SNAP benefits received. While sampling weights accounted for non-response and there is evidence that weighting adjustments mitigated non-response bias due to the low response rates (Peterson et al., 2021), such bias may not have been eliminated and could have led to selection bias either towards or away from the null. Nonetheless, most of the associations for difficulty with paying expenses were strong (PR > 2) for all outcomes examined and are hence unlikely to have been fully attributable to bias. Last, all measures were based on self-report, although the adjustment for general health status in all models should have attenuated the degree of same-source bias. Longer-form measures of anxiety and depression such as the GAD-7 and the PHQ-9 have been previously shown to exhibit higher levels of sensitivity and specificity (Kroenke et al., 2001; Spitzer et al., 2006).
Implications of the study
Overall, the findings from the present study suggest the importance of financial hardship as a fundamental cause (Link & Phelan, 1995) and social determinant of mental health and social needs during the COVID-19 pandemic, and point to the urgent need for direct and sustained cash relief well in excess of current levels of social assistance, as well as the imperative of extending housing renter eviction protections. The current study further offers a critical baseline assessment for evaluating impacts of the U.S. federal government's public policy responses in subsequent months, and potentially years, of the pandemic. Notably, this study also heeds recent calls for a more “consequential” epidemiology, whereby epidemiologic research can serve to more directly inform contemporary social policies to improve population health, including in response to emerging public health threats and crises such as pandemics (Kim, 2019).
Based on the above cited evidence, economic hardship and food insecurity declined among UI recipients after enacting the CARES Act, and according to the present study, a substantial and growing share of working-aged adults experienced household financial hardship since federal UI supplements lapsed by September 2020. In order to alleviate financial hardship and its adverse sequelae, a logical recommendation that follows is that any future federal UI bonus match or even exceed the UI bonus level of $600 weekly as well as a one-time direct payment of $1200 previously provided through the CARES Act (Driessen, 2020).
The COVID-19 relief bill approved by the U.S. Congress and President Trump in early January 2021 limited the federal UI supplement to $300 weekly and a one-time stimulus check of $600 (Bernard & Lieber). In mid-January 2021, then President-elect Biden unveiled a $1.9 trillion economic relief plan for his administration that proposed a one-time direct payment of $1400 (on top of the $600 check) and a UI supplement of $400 weekly through the end of September 2021 (Smialek, 2021). In March 2021, a federal UI supplement of $300 weekly was approved as part of the American Rescue Plan Act through early September 2021 (Smith, 2021). However, as of June 2021, 26 states have since elected to halt these benefits (in 22 states in June 2021 and 4 states in July 2021), citing that the benefits serve as a disincentive to a return to work, despite unemployment claims beginning to rise again (Gonzalez and Davis, 2021). Moreover, the federal moratorium on housing evictions that was renewed after December 2020 is set to expire again at the end of July 2021 (National Low Income Housing Coalition, 2021). The relative $300 or $600 weekly shortfall in the UI supplement compared to the benefits included in the CARES Act would most likely signify that households experiencing income loss during the pandemic will not have their financial needs sufficiently met. Given the strong associations demonstrated between financial hardship and physical and mental health outcomes in the present study, such shortfalls would likely carry substantial negative public health consequences. Over the remainder the pandemic, it is imperative that the U.S. federal government ensure that expanded and needs-based social policy relief measures are provided, and routinely evaluate the adequacy of such measures in order to mitigate the pandemic's short- and long-term adverse impacts on the physical, mental, and social well-being of tens of millions of Americans, including vulnerable minority and low-income populations.
Author contribution
Daniel Kim: Conceptualization, Methodology, Data curation, Formal analysis, Writing – Original draft preparation, Reviewing & editing.
Ethical statement
This study was approved by the Institutional Review Board at Northeastern University.
Declaration of competing interest
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2021.100862.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Allison P.D. Imputation of categorical variables with PROC MI. SUGI 30 Proceedings. 2005 Apr 10;113(30):1–4. [Google Scholar]
- Assari S. Race, depression, and financial distress in a nationally-representative sample of American adults. Brain Sciences. 2019 Feb;9(2):29. doi: 10.3390/brainsci9020029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkowitz S.A., Basu S. Unemployment insurance, health-related social needs, health care access, and mental health during the COVID-19 Pandemic. JAMA Internal Medicine. 2020 doi: 10.1001/jamainternmed.2020.7048. Published online November 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernard T.S., Lieber R. The Stimulus Deal: What’s in It for You. https://www.nytimes.com/article/stimulus-deal-update.html Accessed at:
- Center on Budget and Policy Priorities Tracking the COVID-19 recession's effect's on food, housing, and employment hardships. https://www.cbpp.org/research/poverty-and-inequality/tracking-the-covid-19-recessions-effects-on-food-housing-and Accessed at:
- Driessen G. Congressional Research Service; Washington: 2020 Apr 1. The Coronavirus relief fund (CARES Act, Title V): Background and state and local allocations. [Google Scholar]
- FEMA Supplemental Payments for Lost Wages. https://www.fema.gov/disasters/coronavirus/governments/supplemental-payments-lost-wages Accessed at:
- Gonzalez O., Davis L.M. June 21, 2021. 12 states have ended unemployment benefits and $300 weekly bonus. What to know.https://www.cnet.com/personal-finance/12-states-have-ended-unemployment-benefits-and-300-weekly-bonus-what-to-know/ Accessed at: [Google Scholar]
- Haw C., Hawton K., Gunnell D., Platt S. Economic recession and suicidal behaviour: Possible mechanisms and ameliorating factors. International Journal of Social Psychiatry. 2015 Feb;61(1):73–81. doi: 10.1177/0020764014536545. [DOI] [PubMed] [Google Scholar]
- Karpman M., Acs G. Urban Institute; Washington, DC: 2020. Unemployment insurance and economic impact payments associated with reduced hardship following CARES Act. [Google Scholar]
- Kim D. Bridging the epidemiology-policy divide: A consequential and evidence-based framework to optimize population health. Preventive Medicine. 2019 Dec 1;129:105781. doi: 10.1016/j.ypmed.2019.105781. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ‐9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001 Sep;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link B.G., Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior. 1995 Jan 1:80–94. [PubMed] [Google Scholar]
- Mossakowski K.N. Dissecting the influence of race, ethnicity, and socioeconomic status on mental health in young adulthood. Research on Aging. 2008 Nov;30(6):649–671. [Google Scholar]
- National Low Income Housing Coalition . 2021. National Eviction Moratorium.https://nlihc.org/coronavirus-and-housing-homelessness/national-eviction-moratorium Accessed at: [Google Scholar]
- Peterson S., Toribio N., Farber J., Hornick D. U.S. Census Bureau; 2021. Non-response bias report for the 2020 household Pulse survey, version 1.0.https://www2.census.gov/programs-surveys/demo/technical-documentation/hhp/2020_HPS_NR_Bias_Report-final.pdf Accessed at: [Google Scholar]
- Riolo S.A., Nguyen T.A., Greden J.F., King C.A. Prevalence of depression by race/ethnicity: Findings from the national health and nutrition examination survey III. American Journal of Public Health. 2005 Jun;95(6):998–1000. doi: 10.2105/AJPH.2004.047225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smialek J. A look at what's in biden's $1.9 trillion stimulus plan. https://www.nytimes.com/2021/01/14/business/economy/biden-stimulus-plan.html Accessed at:
- Smith K.A. President biden signs stimulus package into law – here's how it’ll affect you. https://www.forbes.com/advisor/personal-finance/biden-signs-third-stimulus-package/ Forbes. March 11, 2021. Accessed at.
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine. 2006 May 22;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Staples L.G., Dear B.F., Gandy M., Fogliati V., Fogliati R., Karin E., Nielssen O., Titov N. Psychometric properties and clinical utility of brief measures of depression, anxiety, and general distress: The PHQ-2, GAD-2, and K-6. General Hospital Psychiatry. 2019 Jan 1;56:13–18. doi: 10.1016/j.genhosppsych.2018.11.003. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau . 2021. Household Pulse Survey: Measuring social and economic impacts during the coronavirus pandemic.https://www.census.gov/programs-surveys/household-pulse-survey.html Accessed at: [Google Scholar]
- U.S. Census Bureau . 2021. Household Pulse Survey technical documentation.https://www.census.gov/programs-surveys/household-pulse-survey/technical-documentation.html Accessed at: [Google Scholar]
- U.S. Department of Labor. Unemployment Insurance Weekly claims report. https://www.dol.gov/newsroom/releases/eta/eta20210128 Accessed at:
- Witteveen D., Velthorst E. Economic hardship and mental health complaints during COVID-19. Proceedings of the National Academy of Sciences. 2020 Nov 3;117(44):27277–27284. doi: 10.1073/pnas.2009609117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu C., Blizzard L., Stankovich J., Wills K., Hosmer D.W. Be wary of using Poisson regression to estimate risk and relative risk. Biostatistics and Biometrics Open Access Journal. 2018;4(5):1–3. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.