ABSTRACT
In the United States, the incidence of new cases of syphilis has been rising. The number of cases of primary and secondary syphilis has continued to increase almost every year over the past 2 decades. Secondary syphilis has a variety of clinical manifestations. A frequently overlooked presentation is that of syphilitic hepatitis, which should be part of the differential diagnosis for patients with elevated liver enzymes, a maculopapular rash, and/or risk factors for contracting syphilis. In this study, we report a rare and unusual case of a man with a remote history of syphilis infection who developed acute liver injury.
INTRODUCTION
Syphilis is a chronic, systemic bacterial infection caused by Treponema pallidum. Even in the 21st century, the disease continues to be a public health challenge. The World Health Organization periodically generates a report of estimates of the global prevalence and incidence of the most common curable sexually transmitted infections.1 Based on prevalence data from 2009 to 2016, the estimated pooled global prevalence of syphilis in both men and women, aged 15–49 years, was 0.5% (95% confidence interval: 0.4–0.6) with regional values ranging from 0.1% to 1.6%. Among the 55 nations that participated, the median incidence rate of syphilis was 25.1 cases per 100,000 population. In the United States, in 2018, 35,063 cases of primary and secondary syphilis were reported, with an incidence rate of 10.8 cases per 100,000 population.2 Syphilis is a common disease, but syphilitic hepatitis is not as well known. Among patients with syphilis, the reported incidence ranges from 0.2% to 9.7%.3–5 Furthermore, liver involvement can occur during any stage of the disease. In a 2018 systematic review that included 144 cases of syphilitic hepatitis, 128 (88.9%) had early syphilis (including primary and secondary syphilis), 7 (4.9%) had latent syphilis, and 9 (6.3%) had tertiary syphilis.6 Rarely, patients present with acute liver injury with markedly elevated liver enzymes and coagulopathy. In this study, we report a rare and unusual case of acute liver injury resulting from syphilis infection.
CASE REPORT
A 49-year-old Hispanic man with a history of essential hypertension, genital herpes, and a remote history of syphilis infection 10–12 years ago visited his local emergency department with severe right upper quadrant abdominal pain for 1 week. The pain was dull, aching, 6-7/10 in intensity, persistent, and nonradiating. He also experienced yellowish discoloration of the eyes, dark urine, fatigue, nausea, and poor appetite. He reported no skin lesions or rashes.
The patient took losartan and denied taking any other medications, complementary and alternative therapies, or herbal supplements. He stated that he had completed antibiotic therapy for syphilis many years ago, but he could not provide details regarding his treatment course. He denied any drug allergies. He denied any history of alcohol use, intravenous drug use, smoking, acquiring tattoos or piercings, receiving transfusions of blood or blood products, occupational exposure to toxins, or previous liver diseases. He denied any family history of liver disease. The patient was afebrile and hemodynamically stable. The physical examination was remarkable for icteric sclera and generalized jaundice. There were no rashes. He was fully alert and oriented.
Initial liver chemistries showed aspartate aminotransferase 1,280 U/L, alanine aminotransferase 1,652 U/L, alkaline phosphatase 147 U/L, total bilirubin 19.9 mg/dL, and direct bilirubin 15.5 mg/dL. The international normalized ratio was 1.6. The complete blood count showed white blood cells 6.2 × 103/uL, hemoglobin 15.1 g/dL, and platelet count 100 × 109/L. The serum electrolytes and renal function were normal. No previous laboratory results were available. An abdominal ultrasound revealed no hepatomegaly, no hepatic steatosis, no bile duct dilatation, and mild splenomegaly.
The patient was transferred to a tertiary care liver transplant center. He was started on intravenous N-acetylcysteine for supportive care. An magnetic resonance imaging/magnetic resonance cholangiopancreatography revealed normal liver size, no bile duct dilatation, mild splenomegaly, and no masses. A viral hepatitis panel showed immunity to the hepatitis B virus (HBV) as a result of previous natural HBV infection. The HBV DNA was undetectable. Herpes simplex virus 2 IgG was positive, while tests for herpes simplex virus 1/2 IgM, cytomegalovirus IgM, Epstein-Barr virus IgM, and human immunodeficiency virus were negative. An autoimmune panel was positive for antinuclear antibodies (1:80) but was otherwise negative. A ceruloplasmin level and iron studies were normal. Serologic tests for rapid plasma reagin, followed by fluorescent treponemal antibody-absorption test, were reactive.
Over the next several days, the liver chemistries showed no meaningful improvement, the international normalized ratio increased to 2.5, and the patient underwent a liver biopsy, which showed severe acute hepatitis with a mixed inflammatory infiltrate in the portal, periportal, and lobular areas (Figure 1). There were substantial areas of liver cell death along with cholestasis. The specimens were further immunostained for spirochetes and were positive (Figure 2). Because of uncertainty regarding his previous treatment course for syphilis, he was administered benzathine penicillin G. Afterward, his clinical status and liver enzymes gradually improved, and he was discharged home.
Figure 1.
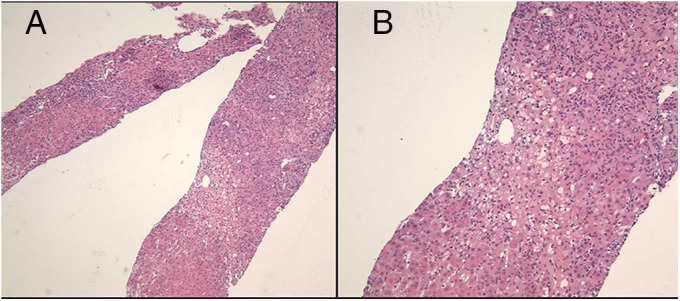
(A) 100× and (B) 200× magnification histopathology of the acute liver injury showing severe acute hepatitis with a portal, periportal, and lobular mixed inflammatory infiltrate comprising lymphocytes, eosinophils, plasma cells, and extensive neutrophils. Zone 3 collapse and confluent necrosis are seen, abundant single-cell apoptosis and degenerative hepatocyte changes. Cholestasis is present. Trichrome and reticulin stains highlight the areas of confluent necrosis, and the trichrome stain also shows increased periportal fibrosis and sinusoidal fibrosis.
Figure 2.
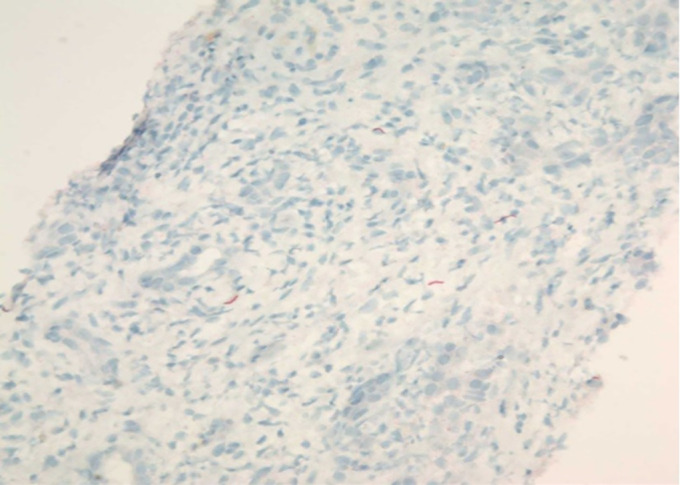
Histopathologic image of the patient's acute liver injury from liver biopsy showing positive immunostaining for spirochetes.
DISCUSSION
Syphilis is in the differential diagnosis of genital ulcers (primary syphilis, chancre) and a diffuse, symmetric maculopapular rash (secondary syphilis), particularly in patients at high risk of contracting syphilis. It is known as a “great imitator” because its symptomatology and physical examination findings in the different stages mimic a variety of other illnesses. In this case, other causes of hepatitis and chronic liver disease were excluded. Notably, given the degree of liver enzyme elevations, in this case, the differential diagnosis included other infectious causes, drug-induced liver injury, autoimmune disorders, and ischemic hepatitis.
To the best of our knowledge, this is among the very few reported cases of syphilitic hepatitis presenting as the sole clinical manifestation of secondary syphilis.7 Furthermore, when manifesting as acute hepatitis, syphilis is generally accompanied by an elevated alkaline phosphatase level, frequently with normal or only mildly elevated aminotransferase levels.7 Rarely, as in this case, patients develop acute liver injury and present with a mixed, rather than a purely cholestatic, picture.
Liver biopsy typically shows focal hepatocyte necrosis, noncaseating granulomas, and portal tracts with mixed inflammatory infiltrate.8 Importantly, immunohistochemical staining only detects spirochetes in up to 50% of patients and, therefore, has poor sensitivity for diagnosing syphilitic hepatitis.5,9,10 The presence of spirochetes is uncommon, but it is confirmatory. Penicillin is the treatment of choice for all stages of syphilis.
Rarely, syphilitic hepatitis can lead to fulminant liver failure, as demonstrated in the case of a patient who ultimately needed liver transplantation.11 Given the morbidity and mortality related to a missed diagnosis, keen suspicion, timely recognition, and therapy are essential. This uncommon presentation highlights the importance of high clinical suspicion in identifying syphilis as a cause of unexplained acute liver injury. This case should alert physicians to consider syphilis in the differential diagnosis—even in patients who lack the common clinical manifestations of the disease.
DISCLOSURES
Author contributions: J. Shah wrote the manuscript and is the guarantor of the article. V. Lingiah, M. Niazi, R. Olivo-Salcedo, N. Pyrsopoulos, and A. Shahidullah revised the manuscript for intellectual content. M. Galan provided the images.
Financial disclosure: None to report.
Previous presentation: This case was presented at the American College of Gastroenterology Annual Scientific Meeting, October 23–28, 2020; Virtual.
Informed consent was obtained for this case report.
Contributor Information
Vivek Lingiah, Email: lingiava@njms.rutgers.edu.
Mumtaz Niazi, Email: man202@njms.rutgers.edu.
Raquel Olivo-Salcedo, Email: rmo58@njms.rutgers.edu.
Nikolaos Pyrsopoulos, Email: pyrsopni@njms.rutgers.edu.
Mark Galan, Email: galanma@njms.rutgers.edu.
Abul Shahidullah, Email: shahidullah52@gmail.com.
REFERENCES
- 1.Rowley J, Vander Hoorn S, Korenromp E, et al. Chlamydia, gonorrhoea, trichomoniasis and syphilis: Global prevalence and incidence estimates. Bull World Health Organ. 2019;97(8):548–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC). Sexually Transmitted Disease Surveillance 2018. U.S. Department of Health and Human Services: Atlanta, GA, 2019. https://www.cdc.gov/std/stats18/default.htm. Accessed June 14, 2020. [Google Scholar]
- 3.Hahn RD. Syphilis of the liver. Am J Syph Gonorrhea Vener Dis. 1943;27:529–62. [Google Scholar]
- 4.Lee RV, Thornton GF, Conn HO. Liver disease associated with secondary syphilis. N Engl J Med. 1971;284(25):1423–5. [DOI] [PubMed] [Google Scholar]
- 5.Fehér J, Somogyi T, Timmer M, Józsa L. Early syphilitic hepatitis. Lancet. 1975;2(7941):896–9. [DOI] [PubMed] [Google Scholar]
- 6.Huang J, Lin S, Wan B, Zhu Y. A systematic literature review of syphilitic hepatitis in adults. J Clin Transl Hepatol. 2018;6(3):306–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hussain N, Igbinedion SO, Diaz R, Alexander JS, Boktor M, Knowles K. Liver cholestasis secondary to syphilis in an immunocompetent patient. Case Rep Hepatol. 2018;2018:8645068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.German MN, Matkowskyj KA, Hoffman RJ, Agarwal PD. A case of syphilitic hepatitis in an HIV-infected patient. Hum Pathol. 2018;79:184–7. [DOI] [PubMed] [Google Scholar]
- 9.Young MF, Sanowski RA, Manne RA. Syphilitic hepatitis. J Clin Gastroenterol. 1992;15(2):174–6. [PubMed] [Google Scholar]
- 10.Pratt DS. Liver chemistry and function tests. In: Feldman M, Friedman LS, Brandt LJ. (eds). Sleisenger and Fordtran's Gastrointestinal and Liver Disease. Elsevier: Philadelphia, PA, 2016, pp 1243–52. [Google Scholar]
- 11.Lo JO, Harrison RA, Hunter AJ. Syphilitic hepatitis resulting in fulminant hepatic failure requiring liver transplantation. J Infect. 2007;54(3):e115-7. [DOI] [PubMed] [Google Scholar]


