Abstract
Objective
Theoretical models of mindfulness meditation conceptualize the cultivation of focused attention and regulation of emotional states, with the attitudinal foundations that promote nonjudgment and acceptance, to facilitate cognitive and affective processing resulting in improved brain health. Within the scientific study of mindfulness meditation, outcomes assessing behavioral and neural correlates of attentional control and emotion regulation have been examined for their malleability as a function of engagement in mindfulness practices. This review synthesizes the results of our pilot trials examining the preliminary effects of mindfulness meditation on metrics of cognitive, affective, and brain health in older adults and in individuals with multiple sclerosis.
Conclusions
There is promising support for mindfulness meditation to enhance attentional control, reduce mind-wandering, and reduce emotion dysregulation. However, well-powered efficacy trials, with an objective assessment of mindfulness practice data are needed to further provide causal and comprehensive evidence supporting the efficacy of mindfulness meditation for brain health. Inclusion of independently derived and validated brain-based signatures of cognitive and affective functioning can additionally enable a parsimonious understanding of how mindfulness meditation can causally impact metrics of functional and structural integrity of the human brain.
Keywords: Attention, Elderly/geriatrics/aging, Emotions/emotional processing, Multiple sclerosis
Mindfulness, as implemented in our research program, is defined as “paying attention, in a particular way: on purpose, in the present moment, and non-judgmentally” (Kabat-Zinn, 1990, 1994). This definition by Jon Kabat-Zinn, and the ensuing development of the 8-week mindfulness-based stress reduction program (Kabat-Zinn, 1982, 2003), launched the systematic study of contemplative sciences in the western world in the last quarter of the 20th century. Designed for individuals with chronic pain, mindfulness meditation practices were taught in a group-based format to cultivate present-moment awareness within an attitudinal framework of acceptance, trust, nonjudgment, patience, letting go, beginner’s mind, and nonstriving (Kabat-Zinn, 1982). In the last four decades since the publication of this seminal work, there has been a surge of interest in co-opting the mindfulness-based stress reduction (MBSR) program for a myriad of clinical and nonclinical populations—including those with psychiatric disorders (Goldberg et al., 2018); neurological disorders (Russell-Williams et al., 2018) including mild cognitive impairment (Klainin-Yobas et al., 2019); chronic health conditions (Zhang, Xue, & Huang, 2020); vascular disease, including hypertension, diabetes, and hypercholesterolemia (Abbott et al., 2014; Priya & Kalra, 2018; Toivonen, Zernicke, & Carlson, 2017); and healthcare professionals (McConville, McAleer, & Hahne, 2017; West, Dyrbye, Erwin, & Shanafelt, 2016). Across these populations, target outcomes have been variegated, with MBSR programs showing promise for attentional control (Prakash, Fountain-Zaragoza, Kramer, Samimy, & Wegman, 2020), emotion regulation (Schirda et al., 2020), insomnia (Gong et al., 2016), pain (Hilton et al., 2017), and stress (Baer, Carmody, & Hunsinger, 2012).
In our program of research, we have attempted to bridge the conceptualization of mindfulness as involving sustained, present-moment awareness with theoretical developments in cognitive and affective sciences, to systematically study the impact of mindfulness training on cognitive and affective health. In this review article, we briefly describe the training we offer, the results of our two, pilot randomized controlled trials, our ongoing projects, and future directions for the empirical study of mindfulness meditation.
Mindfulness-Based Training
Mindfulness training involves a combination of didactics, wherein trained facilitator(s) outline the principles of mindfulness, the attitudinal foundations, and the experiential exercises that invoke maintenance of sustained attention in the presence of distracting thoughts, worries, and ruminations. Although mindfulness-based training programs vary along several dimensions, including length of training, inclusion of specific meditative practices, and emphasis on didactics versus experiential exercises, most training programs, specifically adaptations of MBSR programs, involve focused attention and open monitoring practices (Hölzel et al., 2011; Lutz, Dunne, & Davidson, 2007).
Focused attention practices, like body scan and breath awareness, offer an invitation to cultivate awareness by anchoring attention to a specific phenomenon, such as the in-breath and the out-breath during breath awareness practices or sensations in different parts of the body during a body scan. These practices form the foundational elements of mindfulness training programs, wherein novice meditation practitioners asked to attend to these simple phenomena often notice mind-wandering or the spontaneous shifts in attention from the task at hand to internal mentation (Smallwood & Schooler, 2006). Group-based discussions, didactics around mindfulness, and teachings from mindfulness scholars further assist with honing focused attention skills, which gradually metamorphosize from a unidimensional focus on one phenomenon to an awareness of the myriad of potential experiences. These practices, involving the gradual inclusion of various phenomena like thoughts, sensations, and emotions in present-moment awareness, mark a qualitative progression to open monitoring practices. Choiceless awareness, a prototypical open monitoring practice, involves the sweeping invitation to attend to experiences as they show up. In contrast to choosing to attend to the breath or the sensations, choiceless awareness opens up the gestalt of awareness to whatever arises. Both sets of focused attention and open monitoring practices are designed to cultivate intrapersonal awareness, whereby participants engage in meditative practices and inquiry-based processes to foster a better understanding of their present-moment experiences. These experiences include the nature of their thought patterns, perceptions of sensory phenomena, such as chronic pain, the experience of negative and positive affect, and importantly, the interconnectedness of these phenomena.
The second component of the definition proposed by Jon Kabat-Zinn emphasizes the importance of attitudinal foundations in the cultivation of both focused attention and open monitoring practices. Attitudinal foundations provide the lens through which experiential engagement with mindfulness practices is encouraged with mindful inquiry further scaffolding participant reflections in principles of letting go, trust, acceptance, patience, non-judgment, beginner's mind, and non-striving. These foundations thus help solidify the intention of present-moment awareness, providing participants a repertoire of strategies to assist with the range of affective experiences surfacing during engagement with both focused attention and open monitoring practices.
Our mindfulness training programs, involving engagement with meditative practices designed to cultivate sustained attention in the presence of the wandering tendencies of the mind and scaffolded with the various attitudinal foundations, are thus targeted at enhancing attentional control and emotion regulation. This potentially influences both the neural circuitry and the behavioral manifestation of augmented cognitive and affective health.
Mindfulness, Attention, and the Aging Brain
Mindfulness, as defined above, is the practice of purposefully directing attention, in a nonjudgmental way, to observe the unfolding of each moment as it takes place (Kabat-Zinn, 1982, 1994). As such, attention is considered central to the construct of mindfulness, and it has been a key outcome variable in many longitudinal studies investigating the impact of mindfulness meditation. In a recent, systematic review of this literature, we examined the impact of engagement in mindfulness practices on various attentional processes (Prakash et al., 2020). Another goal of the literature review was to critically evaluate the methodological rigor of the existent literature. Given the increasing scientific and public interest in these training techniques, it is imperative that the field of contemplative sciences adopts rigorous study designs that allow us to thoroughly assess the benefits of mindfulness training for attention. Across 57 longitudinal studies that included a mix of nonrandomized and randomized controlled trials (RCTs), we found equivocal evidence for the three components of attention included in the classical taxonomy proposed by Posner and Petersen (1990)—alerting, orienting, and executive control of attention. Additionally, the review clearly highlighted the need for rigorous, randomized controlled trials. In fact, of the five criteria highlighted in the review as essential metrics for RCTs, only 4 of the 57 studies met all five criteria—underscoring the need for sound, rigorous studies that address alternative interpretations to avoid making unsubstantiated claims. It is important to note, however, that these methodological limitations are not confined to the mindfulness training literature but plague much of the current cognitive training literature as well (Boot, Simons, Stothart, & Stutts, 2013). Recently, a large group of experts, conducting research on behavioral interventions to improve cognitive functioning, reviewed the methodological challenges we face as a field. They outlined the standards that we need to adopt to generate evidence-based guidelines for enhancing cognitive functioning (Green et al., 2019). Adoption of these standards will allow for a more thorough and comprehensive assessment of the impact of mindfulness training specifically, and cognitive training more broadly, on domains of cognitive functioning.
Building off of the recommendations we proposed in our systematic review, we designed and conducted a pilot study investigating the effects of 4 weeks of mindfulness training, compared with an active control group, matched for therapist contact time, homework assignments, and format of training (Whitmoyer et al., 2020). Seventy-five older adults were randomized to one of two active groups with measures of sustained attention and mind-wandering serving as the primary outcome variables. Through our previous work, we have shown mind-wandering, the generation of task-unrelated thoughts while performing an externally focused task, to underlie performance on tasks of sustained attention (Fountain-Zaragoza, Puccetti, Whitmoyer, & Prakash, 2018). Additionally, we have shown that dispositional mindfulness has a negative association with mind-wandering on tasks requiring effortful attentional control (Fountain-Zaragoza, Londerée, Whitmoyer, & Prakash, 2016). We hypothesized that one pathway through which mindfulness training may exert its salutary effects on attentional control abilities is by reducing mind-wandering (see Fig. 1). Interestingly, we found mindfulness training to reduce both subjective and objective markers of mind-wandering in the context of a Go/No-Go task with attentional control improvements noted only for those with high baseline working memory capacity. These results, to our knowledge, provide evidence for an important moderating variable, namely baseline working memory, to impact the benefits conferred through this training program. Taken together, mindfulness training, with its emphasis on the cultivation of sustained attention in the presence of internal and external distractions, has been proven to reduce mind-wandering, thereby improving executive control of attention. However, this improvement seems to be contingent on the availability of key cognitive reserves, like working memory, suggesting that mindfulness training could be particularly beneficial as a preventative training program in midlife before age-related declines in working memory occur.
Fig. 1.
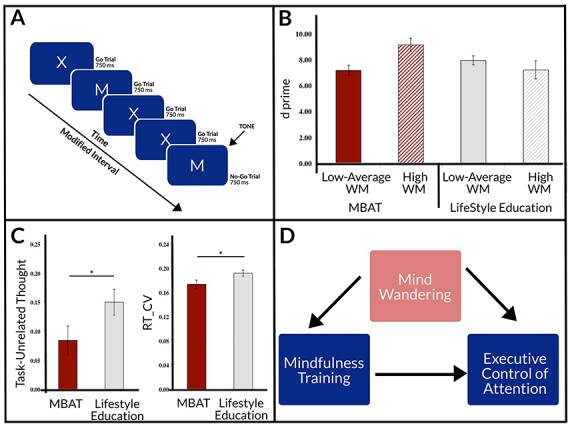
Presents the Go/No-Go task used in the RCT (A), working memory moderating the effects of mindfulness on attention (B), mindfulness training showing reductions in self-report and objective indicators of mind-wandering (C), and the conceptual model linking mindfulness, mind-wandering, and executive control of attention (D).
The results of this study were used as pilot data in our ongoing National Institute on Aging funded, Stage II randomized controlled trial that examines the efficacy of mindfulness meditation for behavioral and neural correlates of attentional control in older adults. We are currently in the fourth year of a 5-year project that involves randomizing 120 older adults to either an 8-week MBSR program or an 8-week lifestyle education training program with booster sessions provided every 3 months and assessment data collected every 6 months. This is an ambitious project that not only conducts several assessment sessions, training sessions, and booster sessions but also includes a web-based and a mobile application, HealthyAgers, that we designed for our participants in both groups to access materials and practices. Figure 2 illustrates the design layout of our mobile application. Panel A shows the individualized home screen where participants can keep track of their weekly engagement with homework practices, and Panel B shows the menu of sitting meditative practices available to the participant. The design of this application was an interdisciplinary effort, involving mindfulness experts, psychologists, computer scientists, graphic designers, and instructional designers, to put together a user-friendly application that will eventually be made accessible to the public. The meta-data being collected through this application, the objective quantification of the frequency and duration of engagement with mindfulness practices, will be critically informative for the dose–response debate in the mindfulness training literature.
Fig. 2.
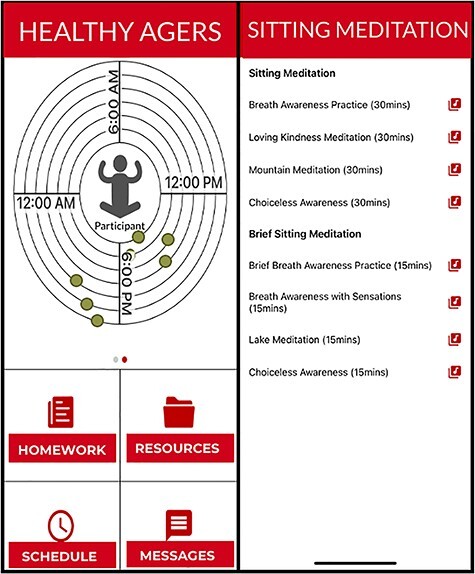
Screenshots of the HealthyAgers mobile application implemented in the Stage II trial.
The primary outcome variable for this Stage-II RCT is the change in behavioral and neural correlates of a task of sustained attention (GradCPT; Esterman, Noonan, Rosenberg, & Degutis, 2013). Since the advent of neuroimaging methodology, there is interest in examining changes in brain features—volumetric measures, activity in key regions, and connectivity across regions—as surrogate endpoints in clinical trials. Mindfulness training, with its known benefits for reducing mind-wandering (Mrazek, Franklin, Phillips, Baird, & Schooler, 2013; Whitmoyer et al., 2020), has been shown to increase connectivity between nodes of the default-mode network and other large-scale canonical networks, like the frontoparietal network (Creswell et al., 2016; Kral et al., 2019); result in an increased volume of the posterior cingulate cortex (Hölzel, Carmody, et al., 2011), a cortical hub of the default-mode network (Buckner et al., 2009); and decrease neural activity in regions of the default-mode network during mediative practice (Garrison, Zeffiro, Scheinost, Constable, & Brewer, 2015). However, in the absence of reliable and valid brain-behavior relationships, decreased activity and increased connectivity have been interpreted as indicators of training-induced plasticity changes with limited understanding of how neural alterations map onto cognitive and behavioral treatment gains. As such, it is increasingly important to identify neuromarkers—brain-based signatures that reliably predict variance in the cognitive domain—and rigorously test them using independent samples (Rosenberg, Finn, Scheinost, Constable, & Chun, 2017; van Essen & Barch, 2015).
Connectome-based predictive modeling (CPM) is a whole-brain, data-driven approach that allows for the identification of connectivity patterns within the individual’s entire connectome that are predictive of disease states, symptom severity, or cognitive functioning (Rosenberg et al., 2016; Shen et al., 2017). In what is now considered a set of formative studies in the development of functional MRI-based neuromarkers, Rosenberg et al. derived and tested the generalizability of a whole-brain, functional connectivity-based neuromarker of sustained attention: saCPM (Rosenberg et al., 2017; Rosenberg, Finn, et al., 2016). The saCPM, using leave-one-out cross-validation procedure, predicted over 70% of the variance in sustained attention in a cohort of young adults on whom the model was derived (Rosenberg, Finn, et al., 2016). More importantly, the saCPM neuromarker was then generalized to predict attention-based deficiencies in children with attention-deficit/hyperactivity disorder (Rosenberg, Finn, et al., 2016); to predict cognitive performance on other metrics of attention, like inhibitory control (Rosenberg et al., 2016) and executive control (Rosenberg, Hsu, Scheinost, Todd Constable, & Chun, 2018); and to serve as a surrogate biomarker for treatment efficacy with increased connectivity following methylphenidate treatment for ADHD (Rosenberg, Zhang, et al., 2016). Extending this neuromarker to older adults, our lab, recently evinced support for the saCPM neuromarker to predict attentional control in healthy older adults with the saCPM neuromarker explaining 38.4% of the variance in Stroop task performance across a sample of 16 young adults and 18 older adults (Fountain-Zaragoza, Samimy, Rosenberg, & Prakash, 2019). Given the robustness of this neuromarker of sustained attention in predicting significant variance in attention and its generalizability across the developemental spectrum and in clinical populations, we plan on using this neuromarker as our primary neuroimaging outcome variable in the ongoing RCT. The use of a well-established neuromarker that captures the coactivity of relevant nodes distributed throughout the entire connectome as a surrogate endpoint in a Stage II efficacy trial of mindfulness training will thus help us clearly investigate the effects of this intervention on neural connectivity.
Mindfulness, Emotion Dysregulation, and Multiple Sclerosis
Multiple Sclerosis (MS) is one of the most frequently diagnosed neurological diseases with nearly one million individuals affected in the USA alone (Wallin et al., 2019). The disease typically onsets in individuals in their 20s and 30s (Dendrou, Fugger, & Friese, 2015), and MS is now considered the second leading cause of neurological disability in young adults (Compston & Coles, 2002; Wallin et al., 2019). People with MS (PwMS) experience a constellation of limiting physical symptoms, including difficulties with walking and gait, balance issues, neuropathic pain, spasticity, fatigue, and weakness (Vitkova et al., 2014; Zackowski, Cameron, & Wagner, 2014). Recently, there has been growing recognition of the role that depression and anxiety play in the prognosis and disease course of MS, such that psychiatric disturbances are now considered to be one of the strongest predictors of quality of life (Fruehwald, Loeffler-Stastka, Eher, Saletu, & Baumhackl, 2001; Marrie, Cohen, & Stuve, 2015). Although much of the MS literature has considered depression and anxiety as distinct disorders, the high degree of comorbidity in psychiatric syndromes has catapulted a growing movement to investigate the shared vulnerabilities that give rise to such behavioral disturbances (Insel, Cuthbert, & Garvey, 2010; Kelly, Clarke, Cryan, & Dinan, 2018). Emotion dysregulation, defined as maladaptive patterns of emotional experience and expression which interfere with goal-directed behavior, is a transdiagnostic factor that is increasingly investigated in the affective sciences as a central construct for understanding psychopathology—particularly, mood and anxiety disorders (Aldao, Nolen-Hoeksema, & Schweizer, 2010). In a recent study of 100 PwMS and 98 community controls, we provided evidence for emotion dysregulation, a well-studied transdiagnostic factor underlying mood and anxiety disorders, to be associated with symptoms of anxiety and depression (Prakash, Schirda, Valentine, Crotty, & Nicholas, 2019). PwMS reported significantly higher levels of depressive symptoms, greater emotion dysregulation, and a lower health-related quality of life when compared with community controls. As hypothesized, both depression and anxiety symptoms were associated with greater maladaptive strategy use, and greater emotion dysregulation. Our results suggested that emotion dysregulation, and specifically use of maladaptive strategies, are associated with both depression and anxiety symptoms in MS and are appropriate targets for rehabilitation.
As such, we designed and recently published the first pilot RCT to examine the impact of mindfulness training on emotion dysregulation and cognitive functioning compared to both active and passive control groups in PwMS (Schirda et al., 2020). Sixty-one participants were randomized to one of three groups: a 4-week mindfulness group, a 4-week adaptive cognitive training group, or a waitlist control group. In this pilot study, we observed an overall retention rate of 82%, with two participants in the mindfulness group, two participants in the adaptive cognitive training group, and four participants in the waitlist group discontinuing participation. Additionally, attendance was 91% for the mindfulness group and 81% for the aCT group. More critically, the pilot study also evinced support for mindfulness training to reduce emotion dysregulation in PwMS with post-hoc comparisons supporting a significant reduction in emotion dysregulation from pre-to-post training for the mindfulness group but neither for the adaptive cognitive training group nor the wait-list control group. In a pre-registered, secondary analyses of this dataset, we also found support for mindfulness training to improve processing speed—a core cognitive deficit in PwMS (Manglani, Samimy, Schirda, Nicholas, & Prakash, 2020). PwMS in the mindfulness training group demonstrated a significant increase in scores on the oral Symbol Digit Modalities Test as compared with participants in the other two groups.
Over the last 5 years, my laboratory has systematically examined the role of emotion dysregulation as a core process in PwMS, provided evidence for feasibility of mindfulness training for PwMS, and demonstrated positive treatment effects of mindfulness meditation for emotion dysregulation and cognitive functioning in MS. My next phase in this programmatic line of research is to conduct a Stage II efficacy trial of mindfulness meditation with PwMS to evince support for the causal effects of mindfulness training for reducing emotion dysregulation and enhancing cognitive functioning in this population.
Conclusions and future directions
Mindfulness meditation training, and its various adaptations, hold great promise for improving cognitive and affective health. However, caution is critical as many trials are still Stage I, pilot investigations. According to the NIH Stage model of behavioral interventions (Onken, Carroll, Shoham, Cuthbert, & Riddle, 2014), intervention development/testing proceeds through a series of cyclical stages with Stages 0 and I being critical for intervention development and refinement and Stages II and beyond as being necessary for robustly determining the causal impact of the intervention on targeted outcome variables. With well-powered efficacy trials currently being implemented, future studies will not only answer the question of whether mindfulness meditation improves metrics of cognitive and affective health, but they will also identify mechanistic and moderating variables that further our conceptual understanding of why and for whom contemplative training can have a meaningful effect. Future research, assessing frequency and duration of engagement in meditative practices via web-based or mobile applications, will also contribute to a clearer understanding of the equivocal relationships that are often observed between self-reported measures of engagement and treatment outcomes (Jensen, Vangkilde, Frokjaer, & Hasselbalch, 2012; Manglani et al., 2020; Rooks, Morrison, Goolsarran, Rogers, & Jha, 2017; Whitmoyer et al., 2020). By better understanding the relationships between different types of meditative practices, the frequency and duration of engagement in these practices, the changes in state levels of mindfulness, and, ultimately, the behavioral and neural correlates of attentional control and emotion dysregulation, we can develop more comprehensive models of contemplative training and offer evidence-based care for variegated outcomes.
Acknowledgments
The content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health or the National Multiple Sclerosis Society. The author would also like to thank her team of graduate students, undergraduate students, post-doctoral scientists, and research volunteers who contributed to the design, implementation, and analyses of the studies reviewed in the manuscript.
Funding
The project described in this publication was supported by awards from the National Institutes of Health (R01AG054427) and the National Multiple Sclerosis Society (PP2183).
References
- Abbott, R. A., Whear, R., Rodgers, L. R., Bethel, A., Thompson Coon, J., Kuyken, W., et al. (2014). Effectiveness of mindfulness-based stress reduction and mindfulness based cognitive therapy in vascular disease: A systematic review and meta-analysis of randomised controlled trials. Journal of Psychosomatic Research, 76(5), 341–351. 10.1016/j.jpsychores.2014.02.012. [DOI] [PubMed] [Google Scholar]
- Aldao, A., Nolen-Hoeksema, S., & Schweizer, S. (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review, 30(2), 217–237. 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- Baer, R. A., Carmody, J., & Hunsinger, M. (2012). Weekly change in mindfulness and perceived stress in a mindfulness-based stress reduction program. Journal of Clinical Psychology, 68(7), 755–765. 10.1002/jclp.21865. [DOI] [PubMed] [Google Scholar]
- Boot, W. R., Simons, D. J., Stothart, C., & Stutts, C. (2013). The pervasive problem with placebos in psychology: Why active control groups are not sufficient to rule out placebo effects. Perspectives on Psychological Science, 8(4), 445–454. 10.1177/1745691613491271. [DOI] [PubMed] [Google Scholar]
- Buckner, R. L., Sepulcre, J., Talukdar, T., Krienen, F. M., Liu, H., Hedden, T., et al. (2009). Cortical hubs revealed by intrinsic functional connectivity: Mapping, assessment of stability, and relation to Alzheimer’s disease. Journal of Neuroscience, 29(6), 1860–1873. 10.1523/JNEUROSCI.5062-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compston, A., & Coles, A. (2002). Multiple sclerosis. Lancet (London, England), 359(9313), 1221–1231. 10.1016/S0140-6736(02)08220-X. [DOI] [PubMed] [Google Scholar]
- Creswell, J. D., Taren, A. A., Lindsay, E. K., Greco, C. M., Gianaros, P. J., Fairgrieve, A., et al. (2016). Alterations in resting-state functional connectivity link mindfulness meditation with reduced interleukin-6: A randomized controlled trial. Biological Psychiatry, 80(1), 53–61. 10.1016/j.biopsych.2016.01.008. [DOI] [PubMed] [Google Scholar]
- Dendrou, C. A., Fugger, L., & Friese, M. A. (2015). Immunopathology of multiple sclerosis. Nature Reviews. Immunology, 15(9), 545–558. 10.1038/nri3871. [DOI] [PubMed] [Google Scholar]
- Esterman, M., Noonan, S. K., Rosenberg, M., & Degutis, J. (2013). In the zone or zoning out? Tracking behavioral and neural fluctuations during sustained attention. Cerebral Cortex (New York, N.Y.: 1991), 23(11), 2712–2723. 10.1093/cercor/bhs261. [DOI] [PubMed] [Google Scholar]
- Fountain-Zaragoza, S., Londerée, A., Whitmoyer, P., & Prakash, R. S. (2016). Dispositional mindfulness and the wandering mind: Implications for attentional control in older adults. Consciousness and Cognition, 44, 193–204. 10.1016/j.concog.2016.08.003. [DOI] [PubMed] [Google Scholar]
- Fountain-Zaragoza, S., Puccetti, N. A., Whitmoyer, P., & Prakash, R. S. (2018). Aging and attentional control: Examining the roles of mind-wandering propensity and dispositional mindfulness. Journal of the International Neuropsychological Society, 24(8), 876–888. 10.1017/S1355617718000553. [DOI] [PubMed] [Google Scholar]
- Fountain-Zaragoza, S., Samimy, S., Rosenberg, M. D., & Prakash, R. S. (2019). Connectome-based models predict attentional control in aging adults. NeuroImage, 186, 1–13. 10.1016/j.neuroimage.2018.10.074. [DOI] [PubMed] [Google Scholar]
- Fruehwald, S., Loeffler-Stastka, H., Eher, R., Saletu, B., & Baumhackl, U. (2001). Depression and quality of life in multiple sclerosis. Acta Neurologica Scandinavica, 104(5), 257–261. 10.1034/j.1600-0404.2001.00022.x. [DOI] [PubMed] [Google Scholar]
- Garrison, K. A., Zeffiro, T. A., Scheinost, D., Constable, R. T., & Brewer, J. A. (2015). Meditation leads to reduced default mode network activity beyond an active task. Cognitive, Affective & Behavioral Neuroscience, 15(3), 712–720. 10.3758/s13415-015-0358-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg, S. B., Tucker, R. P., Greene, P. A., Davidson, R. J., Wampold, B. E., Kearney, D. J., et al. (2018). Mindfulness-based interventions for psychiatric disorders: A systematic review and meta-analysis. Clinical Psychology Review, 59, 52–60. 10.1016/j.cpr.2017.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gong, H., Ni, C. X., Liu, Y. Z., Zhang, Y., Su, W. J., Lian, Y. J., et al. (2016). Mindfulness meditation for insomnia: A meta-analysis of randomized controlled trials. Journal of Psychosomatic Research, 89, 1–6. 10.1016/j.jpsychores.2016.07.016. [DOI] [PubMed] [Google Scholar]
- Green, C. S., Bavelier, D., Kramer, A. F., Vinogradov, S., Ansorge, U., Ball, K. K., et al. (2019). Improving methodological standards in behavioral interventions for cognitive enhancement. Journal of Cognitive Enhancement, 3(1), 2–29. 10.1007/s41465-018-0115-y. [DOI] [Google Scholar]
- Hilton, L., Hempel, S., Ewing, B. A., Apaydin, E., Xenakis, L., Newberry, S., et al. (2017). Mindfulness meditation for chronic pain: Systematic review and meta-analysis. Annals of Behavioral Medicine, 51(2), 199–213. 10.1007/s12160-016-9844-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hölzel, B. K., Carmody, J., Vangel, M., Congleton, C., Yerramsetti, S. M., Gard, T., et al. (2011). Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Research, 191(1), 36–43. 10.1016/j.pscychresns.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hölzel, B. K., Lazar, S. W., Gard, T., Schuman-Olivier, Z., Vago, D. R., & Ott, U. (2011). How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science, 6(6), 537–559. 10.1177/1745691611419671. [DOI] [PubMed] [Google Scholar]
- Insel, T., Cuthbert, B., & Garvey, M. (2010). Research Domain Criteria (RDoC): Toward a new classification framework for research on mental disorders. American Journal of Psychiatry, 167(7), 748–751. 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- Jensen, C. G., Vangkilde, S., Frokjaer, V., & Hasselbalch, S. G. (2012). Mindfulness training affects attention–or is it attentional effort? Journal of Experimental Psychology. General, 141(1), 106–123. 10.1037/a0024931. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn, J. (1982). An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. General Hospital Psychiatry, 4(1), 33–47. 10.1016/0163-8343(82)90026-3. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn, J. (1990). Full catastrophe living: The program of the stress reduction clinic at the University of Massachusetts Medical Center. New York, N.Y: Delta. [Google Scholar]
- Kabat-Zinn, J. (1994). Wherever you go, there you are: Mindfulness meditation in everyday life. New York: Hyperion. [Google Scholar]
- Kabat-Zinn, J. (2003). Mindfulness-based stress reduction (MBSR). Constructivism in the Human Sciences, 8(2), 73–107. [Google Scholar]
- Kelly, J. R., Clarke, G., Cryan, J. F., & Dinan, T. G. (2018). Dimensional thinking in psychiatry in the era of the Research Domain Criteria (RDoC). Irish Journal of Psychological Medicine, 35(2), 89–94. 10.1017/ipm.2017.7. [DOI] [PubMed] [Google Scholar]
- Klainin-Yobas, P., Kowitlawakul, Y., Lopez, V., Tang, C. T., Hoek, K. E., Gan, G. L., et al. (2019). The effects of mindfulness and health education programs on the emotional state and cognitive function of elderly individuals with mild cognitive impairment: A randomized controlled trial. Journal of Clinical Neuroscience, 68, 211–217. 10.1016/j.jocn.2019.05.031. [DOI] [PubMed] [Google Scholar]
- Kral, T. R. A., Imhoff-Smith, T., Dean, D. C., Grupe, D., Adluru, N., Patsenko, E., et al. (2019). Mindfulness-based stress reduction-related changes in posterior cingulate resting brain connectivity. Social Cognitive and Affective Neuroscience, 14(7), 777–787. 10.1093/scan/nsz050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutz, A., Dunne, J. P., & Davidson, R. J. (2007). Meditation and the neuroscience of consciousness: An introduction. In Zelazo, P. D., Moscovitch, M., & Thompson, E. (Eds.), The Cambridge handbook of consciousness (, pp. 499–551). New York, N.Y: Cambridge University Press. [Google Scholar]
- Manglani, H. R., Samimy, S., Schirda, B., Nicholas, J. A., & Prakash, R. S. (2020). Effects of 4-week mindfulness training versus adaptive cognitive training on processing speed and working memory in multiple sclerosis. Neuropsychology, 34(5), 591–604. [DOI] [PubMed] [Google Scholar]
- Marrie, R. A., Cohen, J., & Stuve, O. (2015). A systematic review of the incidence and prevalence of comorbidity in multiple sclerosis: Overview. Multiple Sclerosis, 21(3), 263–281. 10.1177/1352458514564491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McConville, J., McAleer, R., & Hahne, A. (2017). Mindfulness training for health profession students-the effect of mindfulness training on psychological well-being, learning and clinical performance of health professional students: A systematic review of randomized and non-randomized controlled trials. Explore, 13(1), 26–45. 10.1016/j.explore.2016.10.002. [DOI] [PubMed] [Google Scholar]
- Mrazek, M. D., Franklin, M. S., Phillips, D. T., Baird, B., & Schooler, J. W. (2013). Mindfulness training improves working memory capacity and GRE performance while reducing mind wandering. Psychological Science, 24(5), 776–781. 10.1177/0956797612459659. [DOI] [PubMed] [Google Scholar]
- Onken, L. S., Carroll, K. M., Shoham, V., Cuthbert, B. N., & Riddle, M. (2014). Reenvisioning clinical science. Unifying the discipline to improve the public health. Clinical Psychological Science, 2(1), 22–34. 10.1177/2167702613497932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posner, M. I., & Petersen, S. E. (1990). The attention system of the human brain. Annual Review of Neuroscience, 13(1), 25–42. 10.1146/annurev.ne.13.030190.000325. [DOI] [PubMed] [Google Scholar]
- Prakash, R. S., Fountain-Zaragoza, S., Kramer, A. F., Samimy, S., & Wegman, J. (2020). Mindfulness and attention: Current state-of-affairs and future considerations. Journal of Cognitive Enhancement, 4(3), 340–367. 10.1007/s41465-019-00144-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prakash, R. S., Schirda, B., Valentine, T., Crotty, M., & Nicholas, J. (2019). Emotion dysregulation in multiple sclerosis: Impact on symptoms of anxiety & depression. Multiple Sclerosis & Related Disorders, 36(101399), 1–7. 10.1016/j.msard.2019.101399. [DOI] [PubMed] [Google Scholar]
- Priya, G., & Kalra, S. (2018). Mind-body interactions and mindfulness meditation in diabetes. European Endocrinology, 14(1), 35–41. 10.17925/EE.2018.14.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rooks, J. D., Morrison, A. B., Goolsarran, M., Rogers, S. L., & Jha, A. P. (2017). “We are talking about practice”: The influence of mindfulness vs. relaxation training on athletes’ attention and well-being over high-demand intervals. Journal of Cognitive Enhancement, 1(2), 141–153. 10.1007/s41465-017-0016-5. [DOI] [Google Scholar]
- Rosenberg, M. D., Finn, E. S., Scheinost, D., Constable, R. T., & Chun, M. M. (2017). Characterizing attention with predictive network models. Trends in Cognitive Sciences, 21(4), 290–302. 10.1016/j.tics.2017.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg, M. D., Finn, E. S., Scheinost, D., Papademetris, X., Shen, X., Constable, R. T., et al. (2016). A neuromarker of sustained attention from whole-brain functional connectivity. Nature Neuroscience, 19(1), 165–171. 10.1038/nn.4179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg, M. D., Hsu, W.-T., Scheinost, D., Todd Constable, R., & Chun, M. M. (2018). Connectome-based models predict separable components of attention in novel individuals. Journal of Cognitive Neuroscience, 30(2), 160–173. 10.1162/jocn_a_01197. [DOI] [PubMed] [Google Scholar]
- Rosenberg, M. D., Zhang, S., Hsu, W. T., Scheinost, D., Finn, E. S., Shen, X., et al. (2016). Methylphenidate modulates functional network connectivity to enhance attention. Journal of Neuroscience, 36(37), 9547–9557. 10.1523/jneurosci.1746-16.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell-Williams, J., Jaroudi, W., Perich, T., Hoscheidt, S., El Haj, M., & Moustafa, A. A. (2018). Mindfulness and meditation: Treating cognitive impairment and reducing stress in dementia. Reviews in the Neurosciences, 29(7), 791–804. 10.1515/revneuro-2017-0066. [DOI] [PubMed] [Google Scholar]
- Schirda, B., Duraney, E., Lee, K., Manglani, H., Andridge, R., Plate, A., et al. (2020). Mindfulness training for emotion dysregulation in multiple sclerosis: A pilot randomized controlled trial. Rehabilitation Psychology, 65(3), 206–218. 10.1037/rep0000324. [DOI] [PubMed] [Google Scholar]
- Shen, X., Finn, E. S., Scheinost, D., Rosenberg, M. D., Chun, M. M., Papademetris, X., et al. (2017). Using connectome-based predictive modeling to predict individual behavior from brain connectivity. Nature Protocols, 12(3), 506–518. 10.1038/nprot.2016.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smallwood, J., & Schooler, J. W. (2006). The restless mind. Psychological Bulletin, 132(6), 946. 10.1037/0033-2909.132.6.946. [DOI] [PubMed] [Google Scholar]
- Toivonen, K. I., Zernicke, K., & Carlson, L. E. (2017). Web-based mindfulness interventions for people with physical health conditions: Systematic review. Journal of Medical Internet Research, 19(8), e303. 10.2196/jmir.7487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Essen, D. C., & Barch, D. M. (2015). The human connectome in health and psychopathology. World Psychiatry, 14(2), 154–157. 10.1002/wps.20228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitkova, M., Rosenberger, J., Krokavcova, M., Szilasiova, J., Gdovinova, Z., Groothoff, J. W., et al. (2014). Health-related quality of life in multiple sclerosis patients with bladder, bowel and sexual dysfunction. Disability and Rehabilitation, 36(12), 987–992. 10.3109/09638288.2013.825332. [DOI] [PubMed] [Google Scholar]
- Wallin, M. T., Culpepper, W. J., Campbell, J. D., Nelson, L. M., Langer-Gould, A., Marrie, R. A., et al. (2019). The prevalence of MS in the United States: A population-based estimate using health claims data. Neurology, 92(10), e1029–e1040. 10.1212/wnl.0000000000007035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West, C. P., Dyrbye, L. N., Erwin, P. J., & Shanafelt, T. D. (2016). Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. Lancet, 388(10057), 2272–2281. 10.1016/s0140-6736(16)31279-x. [DOI] [PubMed] [Google Scholar]
- Whitmoyer, P., Fountain-Zaragoza, S., Andridge, R., Bredemeier, K., Londerée, A., Kaye, L., et al. (2020). Mindfulness training and attentional control in older adults: Results of a single-blind, placebo-controlled randomized controlled trial. Mindfulness, 11, 203–218. 10.1007/s12671-019-01218-3. [DOI] [Google Scholar]
- Zackowski, K. M., Cameron, M., & Wagner, J. M. (2014). 2nd international symposium on gait and balance in multiple sclerosis: Interventions for gait and balance in MS. Disability and Rehabilitation, 36(13), 1128–1132. 10.3109/09638288.2013.833306. [DOI] [PubMed] [Google Scholar]
- Zhang, Y., Xue, J., & Huang, Y. (2020). A meta-analysis: Internet mindfulness-based interventions for stress management in the general population. Medicine, 99(28), e20493. 10.1097/md.0000000000020493. [DOI] [PMC free article] [PubMed] [Google Scholar]


