Abstract
Background
Appendicitis accounts for the most frequent surgical emergencies in childhood. The guidance from the Royal College of Surgeons and poor post operative outcomes in surgical patients during the pandemic, it would be expected that only children who had clinical signs of appendicitis and were unwell, would have undergone surgery. Hence, the negative appendicectomy rate during the pandemic should have decreased.
The aim of this retrospective study was to assess the rate of negative appendicectomy amongst children <16 years of age during the first wave of the pandemic, from the announcement of the lockdown and determine if there was a true difference by comparing the rate with the same time period in 2019.
Material and methods
Data of all children aged<16 years who were operated for appendicitis between 23/3/2020 and 30/06/2020 was collected retrospectively and compared with that of children operated during the same time period in 2019 for the rate of negative appendicectomy.
Data were analysed using the two-tailed t-test for continuous data and χ2 or Fishers exact tests for categorical data with p value of <0.05 considered significant.
Results
Twenty three paediatric patients presenting with acute appendicitis underwent appendicectomy during the COVID-19 pandemic and 35 patients during 2019.
Overall 17.39% patients underwent laparoscopic appendicectomy in 2020 while 54.29% in 2019. The negative appendicectomy rate was zero during the pandemic while it was 17.14% in 2019. There was no difference in the median length of hospital stay during the two time periods. There was no significant difference in complication or re-admission rate.
Conclusion
This study has the lowest reported incidence of negative appendicectomy rate during the pandemic following wider use of pre operative imaging and early senior involvement in decision making. The increased number of complicated appendicitis during the pandemic did not translate to worse clinical outcomes.
Keywords: Paediatric appendicectomy, Negative appendicectomy, Emergency
Highlights
-
•
This study has the lowest reported incidence of negative appendicectomy rate during the pandemic.
-
•
There was wider use of pre operative imaging and early senior involvement in decision making.
-
•
There was a higher proportion of complicated appendicitis during the pandemic. However, this did not result in increased complications or re admission rate.
-
•
It is possible to reduce negative paediatric appendicectomy rate by following the same lines of management.
1. Background
Appendicectomy is one of the most common emergency surgeries performed [1]. Appendicitis accounts for the most frequent surgical emergencies in childhood, with peak incidence between ages of 11 and 12 years, and carries a lifetime risk of 7–9% [2]. International guidelines do support the use of non-operative treatment for selected children with uncomplicated acute appendicitis [3]; however, non-operative treatment is not widespread in the UK. It is used by only a small minority of surgeons or as part of a research study [4]. Laparoscopic appendicectomy has been considered a safe approach in children [5].
Open and laparoscopic appendicectomy have both been recognized to be safe and effective surgical approaches for appendicitis in children, however laparoscopic approach has gained widespread use in the UK [6]. Laparoscopic approach is routinely used for paediatric appendicectomy at our hospital.
Laparoscopy is considered an aerosol generating procedure, and early guidance from the Royal College of Surgeons England at the start of the COVID-19 pandemic, suggested that laparoscopy should only be used in procedures where the risk of an open procedure to the patient outweighed the potential risk to staff in theatre [7].
It was also recommended that non-operative treatment should be used to avoid surgery for all conditions, including appendicitis [8]. Additionally, there were early reports of adverse post operative outcomes in patients with COVID-19 [9,10]. This led to most surgeons adopting non-operative management of acute appendicitis, including that for children; though data emerged through the first months of the pandemic that children are much less likely to become infected with COVID-19 than adults and the impact of COVID-19 on outcomes following surgery in children is less clear [11].
The effect of the pandemic on management of acute appendicitis in adults has been assessed in numerous studies; however that in children is less extensively assessed. The RIFT study group identified that negative appendicectomy rate in children in UK and Ireland was 15.9% [12]. Considering the guidance from the Royal College of Surgeons and poor post operative outcomes in surgical patients during the pandemic, it would be expected that only children who had clinical signs of appendicitis and were unwell, would have undergone surgery. Hence, the negative appendicectomy rate during the pandemic should have decreased.
The aim of this retrospective study was to assess the rate of negative appendicectomy amongst children <16 years of age during the first wave of the pandemic, from the announcement of the lockdown and determine if there was a true difference by comparing the rate with the same time period in 2019.
2. Materials and methods
2.1. Study design
This was a retrospective cohort study of all paediatric patients aged <16 years undergoing surgery for acute appendicitis.
2.2. Setting
Our Hospital is a large acute NHS Hospital in England, serving a population of around 750,000 from a wide range of social and ethnic groups across North East London.
2.3. Time period
Data of all children aged<16 years who were operated for appendicitis between 23/3/2020 and 30/06/2020 was collected retrospectively and compared with that of children operated during the same time period in 2019.
2.4. Outcomes
The primary outcome was the rate of negative appendicectomy.
Secondary outcome included the proportion of open and laparoscopic surgeries, use of diagnostic imaging, inflammatory markers at time of presentation, length of hospital stay, complication and 30-day re-admission. Negative appendicectomy rate was the proportion of resected appendixes found to be normal on histopathological examination. Complicated appendicitis was defined as presence of gangrenous or perforated appendix on histology.
2.5. Data collection
Data was collected using Electronic patient records and all data was anonymized.
Patient demographics included age and gender.
The duration of symptoms, laboratory test results, radiological investigations, post operative complications, length of hospital stay and 30-day re-admission rate was recorded.
2.6. Statistical analysis
All data was collected using Microsoft Excel. Continuous data was expressed as median.
Data were analysed using the two-tailed t-test for continuous data and χ2 or Fishers exact tests for categorical data. A level of statistical significance was set at P value of <0.05.
2.7. Ethical consideration
This study was approved by the divisional governance committee and complied with all local and Institutional guidelines on information and research governance.
Hospital research ethics committee exempted this study from ethics approval.
This study has been reported in line with the ‘Strengthening the reporting of cohort studies in surgery’ (STROCSS) criteria [13]. This study is registered with Research Registry with the unique identifying number (UIN) researchregistry7128 [14].
3. Results
Twenty three paediatric patients presenting with acute appendicitis underwent appendicectomy during the COVID-19 pandemic and 35 patients during 2019.
Comparative clinical, laboratory, radiological findings of patients operated during the two time periods are summarised in Table 1.
Table 1.
Comparative clinical, laboratory and radiological findings.
| 2019 | 2020 | P value | |
|---|---|---|---|
| N | 35 | 23 | |
| Male (%) | 21(60%) | 12(52.17%) | 0.59a |
| Female (%) | 14(40%) | 11(47.82%) | |
| Age, years (Range) | 12(5–16) | 12(8–16) | 0.54# |
| Duration of symptoms, days (Range) | 2(1–9) | 2(1–5) | 0.99# |
| WCC on admission | 12.2 | 15.1 | 0.09# |
| CRP on admission | 32 | 67 | 0.52# |
| USS | 24 | 15 | |
| MRI | 1 | 1 | |
| X-Ray | 2 | 0 | |
| No pre operative imaging | 10(28.57%) | 8(34.78%) | |
| Laparoscopic (Lap) | 19(54.29%) | 4(17.39%) | |
| Open | 16(45.71%) | 19(82.6%) | |
| Lap converted to open | 1(2.85%) | 0 | |
| Negative appendicectomy | 6(17.14%) | 0 | 0.008a |
| Complicated appendicitis | 9(25.71%) | 6(26.1%) | 1.0a |
Fischer's exact test #Two tailed t-test.
Overall 17.39% patients underwent laparoscopic appendicectomy in 2020 while 54.29% in 2019. There was no relation between the choice of approach and suspected severity of appendicitis. There was a significant difference in rates of negative appendicectomy during the two time periods (Table 1). The negative appendicectomy rate was zero during the pandemic while it was 17.14% in 2019.
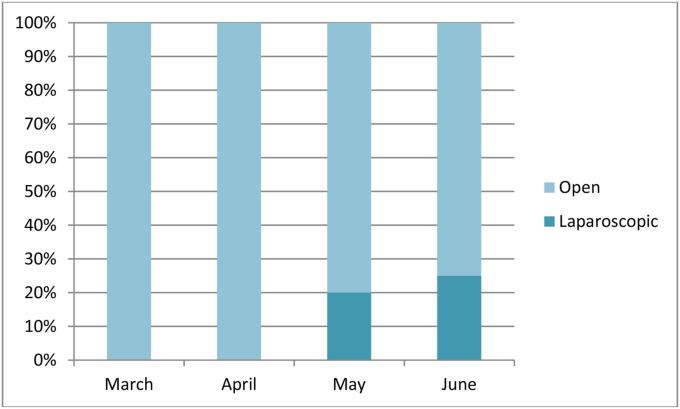
All cases underwent open surgery in March and April 2020, which increased to 20% in May, and 25% in June 2020 (Fig. 1). All patients were operated within one day of admission. Only one patient required conversion to open during 2019.
Fig. 1.
Operative management method, laparoscopic versus open from March to June 2020.
There was no difference in the median length of hospital stay during the two time periods.
However, three patients developed post operative complications in 2019. One had post operative ileus, one intra abdominal collection and one developed pre renal AKI. All were managed conservatively.
The readmission rate was higher during the pandemic as compared to the previous year (Table 2). Both re admissions were due to intra abdominal collection which was managed conservatively with antibiotics.
Table 2.
Comparative post operative outcomes of patients.
| 2019 | 2020 | P value | |
|---|---|---|---|
| Complications | 3(8.57%) | 2(8.70%) | 1.0a |
| Clavien-Dindo classification | |||
| Grade I | 2 | 0 | |
| Grade II | 1 | 2 | |
| Grade III | 0 | 0 | |
| Grade IV | 0 | 0 | |
| Length of stay, days(Range) | 3(2–9) | 3 (1–6) | 0.634# |
| Readmission | 2(5.71%) | 2(8.70%) | 1.0a |
At 30 days there was no reported mortality.
Fischer's exact test #Two tailed t-test.
4. Discussion and conclusion
This study confirms the suspicion that rate of paediatric negative appendicectomy rate has decreased during the corona virus pandemic alongwith a shift towards open appendicectomy.
At our hospital, all paediatric patients are reviewed by consultant surgeon or registrar pre-operatively after admission. During the pandemic, they were involved to review the children at the time of presentation to the hospital in order to decrease the admissions in light of the pandemic, with adequate safety net advice given to parents of the children not admitted.
Over the course of the study period in 2020 the proportion of cases undergoing open surgery decreased, with gradual increase in laparoscopic appendicectomy towards end of May 2020. We believe this pattern is a reflection of initial guidance from professional bodies proposing non-surgical treatments be sought wherever possible and cautioning against the use of laparoscopy [8]. Subsequent evolution of that guidance over time may have encouraged surgeons to resume their normal practice.
Reports of decreased paediatric emergency department presentations due to reluctance of people to leave home and fear of contracting the virus [15], would imply possible delayed presentation of children to hospitals. This can result in an increased likelihood of complicated appendicitis [16]. Contrary to reports regarding delayed presentation [17], in our study there was no difference in the duration of symptoms before presentation to the hospital during the pandemic compared to 2019. This could be attributed to the fact that most children presented with high grade fever and vomiting, with abdominal pain, which might have prompted the parents to seek early medical advice.
In this study, rate of complicated appendicitis was higher as compared to the previous year (26.08% v/s 25.71%), however this could be due to the small sample size resulting in a beta error. This error could be mitigated by larger sample size by including multiple centers.
Both open and laparoscopic appendicectomy are recognized to be safe and effective surgical approaches for appendicitis in children, however laparoscopic approach has gained widespread use in the UK [6].
The low rate of laparoscopic appendicectomy during the pandemic such that only 17% children were operated using laparoscopic approach was likely following the guidance from the various professional bodies that laparoscopy may increase the risk of SARS-CoV- 2 transmission in positive cases [7].
The trend towards a higher proportion of cases being performed by laparoscopic approach over time (Fig. 1) is consistent with updated guidance from professional bodies and a greater understanding about the epidemiology of COVID-19 in children [11].
Recently the high negative appendicectomy rate observed in the UK (15.9% in children) has been highlighted and achieved significant public interest [12].
The zero negative appendicectomy rate during the pandemic in our study is of particular note as it is the lowest reported in UK [12,18,19]. Similar to our study, C Sheath et al. [17], had no negative appendicectomy during COVID in their study. However, in our study the negative appendicectomy rate in 2019 was 17.14% which is higher than the national average. This is concerning as half of the patients underwent surgery without any imaging, while the rest had an inconclusive ultrasound. There was a higher use of pre operative imaging during the pandemic as compared to the previous year (34.78% v/s 28.57%). The increased use of imaging could be one of the contributory factors for the zero negative appendicectomy rates during the pandemic as it helped in pre operative diagnosis. Of note is that, all patients who underwent imaging during the pandemic had positive findings. Additionally, with the global shift in practice towards conservative management during the pandemic [20], it was possible to avoid negative appendicectomy in some children who would have otherwise undergone surgery for a normal appendix.
Of note is that the patients who underwent surgery even without imaging had appendicitis on histology, could reflect the high clinical suspicion in view of symptoms and signs highly suggestive of appendicitis.
Although more patients had complicated appendicitis, this did not translate into increase in the length of hospital stay or post operative complication, thus reflecting the maintenance of good standard of care of children.
This study reflects that pre operative imaging and early senior involvement in decision making regarding surgery can help decrease rate of negative appendicectomy. Although final decision making would depend on clinical judgment, following these can be feasible even after the pandemic restrictions are lifted, and may thereby have a role in avoiding unnecessary operations, reducing the negative appendicectomy rate and improving patient safety.
Further multicentre studies may help show if these findings are reproducible.
However, this is certainly an area of interest as reduced paediatric negative appendicectomy during the pandemic is an unforeseen benefit for improvement in patient care.
The strength of this study is that the appendicectomy rates were based on histological diagnosis and not on intra operative findings. Thereby, reflecting a true negative appendicectomy rate.
The retrospective data collection with a small sample size which increases the probability of bias is a limitation to the study. Since the cohort was from a single institute, the generalizability to other settings may be limited.
In this study we present the evidence of change practice during the pandemic. There was shift of practice towards open appendicectomy. This study has the lowest reported incidence of negative appendicectomy rate during the pandemic following wider use of pre operative imaging and early senior involvement in decision making. The increased number of complicated appendicitis during the pandemic did not translate to worse clinical outcomes. Parents did not delay presenting to medical attention and early senior assessment prevented delay in surgical management of the patients and helped avoid unnecessary operations. With the progression of pandemic, following same lines of management will help to avoid negative appendicectomy. Further multicentre studies will help assess if these findings are reproducible.
Funding sources
None.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Ethical approval
This study was exempted from ethics approval.
Author contribution
Maitreyi Patel: Study concept or design, Data analysis, Writing paper.
Joel Joy Thomas: Data collection, writing paper.
Haschmatullah Sarwary: Study concept and design, Data interpretation, editing.
Registration of research studies
1. Name of the registry: Research Registry.
2. Unique Identifying number or registration ID: researchregistry7128.
3. Hyperlink to your specific registration (must be publicly accessible and will be checked): https://www.researchregistry.com/browse.
Guarantor
Mr Haschmatullah Sarwary.
Consent
Informed consent was waived.
Declaration of competing interest
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2021.102901.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Newhall K G.P., Albright B., Tosteson A., Ozanne E., Trus T. Cost effectiveness of prophylactic appendectomy: a markov model. Surg. Endosc. 2017;31:3596–3604. doi: 10.1007/s00464-016-5391-y. [DOI] [PubMed] [Google Scholar]
- 2.Grosfeld J., O’Neill J., Coran A., Fonkalsrud E. Pediatric Surgery. sixth ed. Vol. 2. Mosby Elsevier; 2006. Appendicitis.https://www.elsevier.com/books/pediatric-surgery/grosfeld/978-0-323-02842-4 [Google Scholar]
- 3.G A., Di Saverio Salomone, Podda Mauro, De Simone Belinda, Ceresoli Marco, Augustin Goran. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J. Emerg. Surg. 2020;15:27. doi: 10.1186/s13017-020-00306-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nigel J Hall E.W., Eaton Simon, Sherratt Frances C., Reading Isabel. CONservative TReatment of Appendicitis in Children: a randomised controlled feasibility Trial (CONTRACT) Arch. Dis. Child. 2021;106 doi: 10.1136/archdischild-2020-320746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harsh Grewal W.D.V., Sweat Jeffrey. Laparoscopic appendectomy in children can be done as a fast-track or same-day surgery. J. Soc. Laparoendosc. Surg. 2004;8:151–154. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3015535/ [PMC free article] [PubMed] [Google Scholar]
- 6.Bethell G, Adams S, Johnson T, et al. Laparoscopy Uptake for Paediatric Appendicectomy – a Comparison of Adult General Surgeons vs Paediatric Surgeons in England from 1997 to 2015. Nottingham, UK: British Association of Paediatric Surgeons Annual Internat, (n.d.). [DOI] [PMC free article] [PubMed]
- 7.B De Simone 1 F.C., Chouillard E., Di Saverio S., Pagani L., Sartelli M., Biffl W.L., Coccolini F., Pieri A., Khan M., Borzellino G., Campanile F.C., Ansaloni L. Emergency surgery during the COVID-19 pandemic: what you need to know for practice. Ann. R. Coll. Surg. Engl. 2020;102:323–332. doi: 10.1308/rcsann.2020.0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Joint Guidance for Surgeons: Guidance for Surgeons Working during the COVID-19 Pandemic from the Surgical Royal Colleges of the United Kingdom and Ireland. Royal College of Surgeons of England. Available: https://www.rcseng.ac.uk/coronavirus/joint-g, (n.d.).
- 9.Leia S.C., Fang Jiangb, Sua W., Chend C., Chene J., Meif W., Zhana L.-Y., Jiaa Y., Zhangg L., Liug D., Xiaa Z.-Y., Xia Zhengyuan. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. 2020:100331. doi: 10.1016/j.eclinm.2020.100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.COVIDSurg Collaborative Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396:27–38. doi: 10.1016/S0140-6736(20)31182-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alasdair Munro D.R. Don’t Forget the Bubbles; 2020. Children and Transmission of SARS-CoV-2. [DOI] [Google Scholar]
- 12.RIFT Study Group on behalf of the West Midlands Research Collaborative Appendicitis risk prediction models in children presenting with right iliac fossa pain (RIFT study): a prospective, multicentre validation study. Lancet Child Adolesc. Heal. 2020;4:271–280. doi: 10.1016/S2352-4642(20)30006-7. Epub 2020. [DOI] [PubMed] [Google Scholar]
- 13.C I., Agha R M.G., Abdall-Razak A., Crossley E., Dowlut N. For the STROCSS group. The STROCSS 2019 guideline: strengthening the reporting of cohort studies in surgery. Int. J. Surg. 2019;72:156–165. doi: 10.1016/j.ijsu.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 14.https://www.researchregistry.com/browse-the-registry#home/registrationdetails/6136664d15ec60001e2e7889/ (n.d.)
- 15.Rachel Isba J.B., Edge Rhiannon, Jenner Rachel, Broughton Emily, Francis Natalie. Where have all the children gone? Decreases in paediatric emergency department attendances at the start of the COVID-19 pandemic of 2020. Arch. Dis. Child. 2020;105:704. doi: 10.1136/archdischild-2020-319385. 2020 Jul;10. 5(7)704 Epub 2020 May 6. [DOI] [PubMed] [Google Scholar]
- 16.Williams M.B.N. Perforation rate relates to delayed presentation in childhood acute appendicitis. J. R. Coll. Surg. Edinb. 1998;43:101–102. [PubMed] [Google Scholar]
- 17.Chloe Sheath D.C., Mohamed Abdelrahman, MacCormick Andrew. Paediatric appendicitis during the COVID-19 pandemic. J. Paediatr. Child Health. 2021;57:986–989. doi: 10.1111/jpc.15359. Epub 2021 Feb 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stefano Giuliani S.S., Cecil Elizabeth V., Apelt Nadja, Sharland Michael. Pediatric emergency appendectomy and 30-day postoperative outcomes in district general hospitals and specialist pediatric surgical centers in England, April 2001 to March 2012: retrospective cohort study. Ann. Surg. 2016;263:184–190. doi: 10.1097/SLA.0000000000001099. [DOI] [PubMed] [Google Scholar]
- 19.et al N.J.H., Tiboni S., Bhangu A. Outcome of appendicectomy in children performed in paediatric surgery units compared with general surgery units. Br. J. Surg. 2014;101:707–714. doi: 10.1002/bjs.9455. [DOI] [PubMed] [Google Scholar]
- 20.Ielpo B., Podda M., Pellino G., Pata F., Caruso R., Gravante G., Di Saverio S. Global attitudes in the management of acute appendicitis during COVID-19 pandemic: ACIE Apply Study. Br. J. Surg. 2020;8 doi: 10.1002/bjs.11999. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.