Abstract
Objective
Approximately one in four deaths among people living with HIV (PLWH) in the United States can be attributed to cigarette smoking. Using a nationally representative sample of PLWH, this study examines the prevalence, time-trends, and correlates of current cigarette smoking among PLWH compared to people without HIV.
Design
Secondary analysis of population-based cross-sectional biobehavioral survey.
Methods
Data were pooled from the 1999–2016 National Health and Nutrition Examination Survey (NHANES). All adults (20–59 years) who self-reported their smoking status and were tested for HIV (HIV+ = 152; HIV− = 26 305) were included in the analysis. Prevalence with 95% confidence interval (95% CI), trend analysis by year and group (HIV+/HIV−), and multivariable logistic regression analyses were performed with the complex survey design adjustments.
Results
Overall, 47.0% of PLWH were current smokers compared to 25.5% of those without HIV. From 1999 to 2016, the decline in smoking in PLWH was comparable to those without HIV (10.7% vs. 8.0%). PLWH smokers were more likely than PLWH nonsmokers to be substance users (adjusted odds ratio [aOR] = 17.52; 95% CI = 2.04 to 27.8). Compared to smokers without HIV, PLWH smokers were more likely to be older (1.10; 1.06 to 1.14), males (7.96; 2.50 to 25.40), non-Hispanic Black (10.45; 4.13 to 26.45), with depression (Patient Health Questionnaire-9 sum score ≥5) (3.79; 1.22 to 11.79), and less likely to be gay (0.02; 0.00 to 0.07).
Conclusion
Cigarette smoking among PLWH is a major public health problem in the United States. Targeted and tailored smoking cessation interventions that incorporate assessment and treatment of depression and co-occurring substance use are critical for PLWH, especially among those who are disproportionately affected by smoking and HIV (sexual minority).
Implications
This study offers important research implications in four areas:
1. The decline in smoking among PLWH over 18 years has been modest, and half of PLWH are still smokers.
2. More resources and efforts should be allocated to reduce cigarette smoking among PLWH.
3. There is a critical need to develop and test culturally tailored smoking cessation interventions for minority subgroups who are most impacted by HIV infection and smoking (non-Hispanic Blacks and men who have sex with men)
4. Smoking cessation interventions designed for PLWH should incorporate assessment and treatment of depression and substance use.
Introduction
In 2017, it was estimated that 1 003 782 adults in the United States have been diagnosed with HIV infection.1 Owing to major advances in HIV treatment, people living with HIV (PLWH) who use antiretroviral therapy (ART) are expected to live as long as people without HIV.2 However, cigarette smoking causes 24% of deaths among PLWH,3 and substantially increases HIV-related and non-related morbidity, even for individuals on successful ART.4 Compared with PLWH who are nonsmokers, smokers have threefold the risk of cancers,5 double the risk of cardiovascular complications,6 twice the risk of developing tuberculosis, a 6–15 year shorter lifespan,7 and lower self-reported quality of life.8 In contrast, smoking cessation among PLWH reduces non-AIDS malignancy by 34%, the risk of cardiovascular disease by 20%, and overall mortality by 16%.3
Despite the substantial negative health effects of smoking on PLWH, only modest progress has been made in reducing their smoking, and nationally representative prevalence, time-trends, and current smoking correlates have not been adequately investigated. Several studies have reported a high rate of smoking among PLWH ranging between 45% and 70%.9 However, most of these studies have focused on clinic‐ or small community‐based samples,10,11 with only four studies reporting on cigarette smoking among PLWH in large, national samples. Among these, only one used a national representative sample of PLWH; however, that study determined HIV status based on self-report and focused on only PLWH, without comparison with the general population.12 The other three studies included only PLWH who are currently receiving medical care, and as such their results are not generalizable to those with less healthcare access.13–15 In addition, the most recent study was reported in 2014, and changes in smoking among PLWH at the national level after 2014 have not been examined.13 Therefore, a more updated smoking profile investigation of PLWH drawn from a nationally representative sample would contribute to identifying opportunities for interventions.
Monitoring change in cigarette smoking prevalence and profile among PLWH compared to the general population is important to identify progress and opportunities for reducing the burden of tobacco use among this population. Smoking prevalence among US adults has been falling dramatically since the first Surgeon General Report in 1964 and is half the prevalence of 1964 (17.8%); however, smoking rates in medically vulnerable population groups such as PLWH are still high.16 Only two prior studies reported on time-trends in smoking prevalence among PLWH, and both have shown a decline in smoking among PLWH comparable to that in the general population.13 Although they are important contributions to the literature, the first report included only women with HIV, and the second report included only PLWH who are currently receiving medical care in Medical Monitoring Project facilities.13 Hence, their results are not generalizable to all PLWH in the United States.
Despite the high interest in quitting among PLWH smokers (40%–75%), very few quit smoking.17 Although reasons for the low quit rates among PLWH are not well understood, several barriers to quitting smoking have been identified. PLWH smokers experience structural barriers (ie, poverty, stigma, lack of social support) as well as psychiatric comorbidities such as depressive and substance use disorders that hinder their smoking cessation efforts.18 The syndemic of unhealthy alcohol use, cigarette use, and depressive symptoms is common among PLWH.19 Estimates indicate that 60% of PLWH have at least two of these conditions, and 15% have had all three.19
To address the limitations in previous studies, this study used a nationally representative sample of US adults and relied on HIV antibody blood assay test to determine HIV status.20 The current study aims to: (a) compare characteristics of PLWH who are current smokers with people without HIV; (b) compare the time-trend of smoking prevalence and lifetime smoking cessation measured by the quit ratio over a period of 18 years (from 1999 to 2016) between PLWH and those without HIV; and (c) identify correlates of smoking among PLWH, specifically sociodemographic characteristics and risk factors, such as alcohol consumption, depression, and substance use that often co-occur with smoking. Mapping and documenting this information are important to assess the magnitude of the smoking problem among PLWH as well as guide future prevention and cessation efforts to reduce their tobacco use.
Methods
Data Source
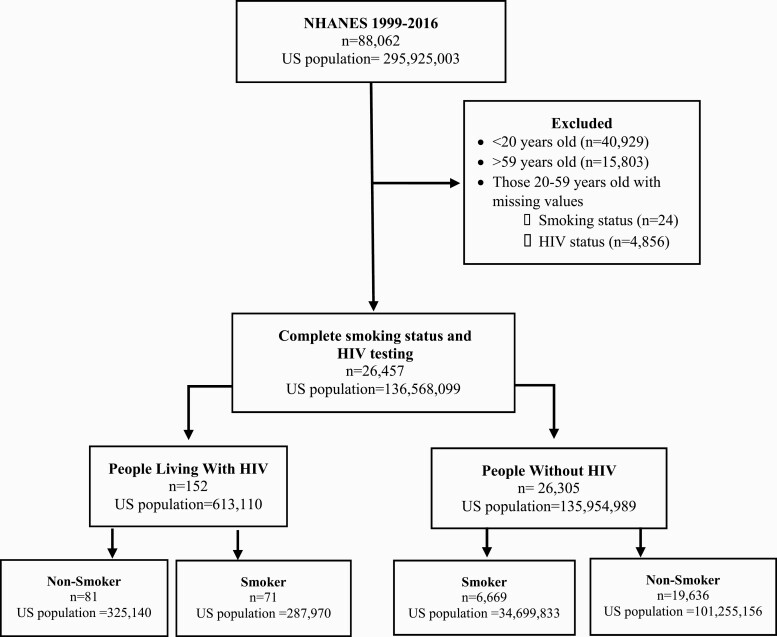
Data were obtained from the 1999–2016 National Health and Nutrition Examination Survey (NHANES). NHANES is a complex multi-stage survey representative of the non-institutionalized US civilian population which over-samples persons 60 and older, African Americans, Asians, and Hispanics. Each participant in the NHANES represents a certain number of individuals based on the survey weights.21 The survey employs household in-person interviews with biologic specimens of blood and urine collected at mobile examination centers. Since 1999, the NHANES has been conducted continuously in two-year cycles. All participants aged 18–59 years completed the HIV antibody blood assay test. All adults 20 years and older self-reported current cigarette smoking (every day/someday). Therefore, all participants who were 20–59 years old, had HIV antibody blood assay test results (positive or negative), and reported their smoking status were included in the analysis (Figure 1).20
Figure 1.
Study diagram, NHANES 1999–2016.
Measures
HIV Diagnosis
HIV status was determined based on the HIV-1 antibody blood assay test results. Based on the test results, participants were grouped into two categories: HIV+ (PLWH) or HIV− (people without HIV infection).20
Smoking
Smoking status was assessed from two self-reported items in the data: “Have you smoked at least 100 cigarettes in your lifetime?” and “Do you smoke cigarettes now?” Smoking status was categorized into three groups: (1) current smokers who reported they smoked at least 100 cigarettes in their lifetime and currently smoke either every day or some days; (2) former smokers who reported they have smoked at least 100 cigarettes in their lifetime, but do not smoke now); and (3) never smokers who reported they have not smoked 100 cigarettes in their lifetime and do not smoke now. Age at smoking initiation was derived from the question: “At what age did you first start to smoke fairly regularly?” Smoking intensity was measured by number of cigarettes smoked per day. Quit attempts were defined as having made a serious quit attempt during the past 12 months and stopped smoking for at least 1 day. The quit ratio was defined as the number of former smokers to the number of ever-smokers (ie, sum of current and former smokers) and was considered as a proxy for smoking cessation.
Socio-demographic Characteristics
Participants reported their age, gender, educational attainment (less than high school or high school, some college or more), health insurance (insured, uninsured), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic), employment status (employed, unemployed), marital status (Married/Living with partner, Divorced/Widowed/Separated, Never married), and sexual orientation (gay, heterosexual, bisexual, Others/Don't Know). A family poverty index ratio (PIR) was used to identify participants as living at or above (PIR ≥ 1) or below the poverty threshold (PIR < 1). PIRs are calculated based on the poverty guidelines that vary family size and geographic location specific to NHANES survey year.
Depression and Mental Health
Depression was assessed using the Patient Health Questionnaire (PHQ-9).22 Based on the total score on nine items, participants were grouped into two categories: having no depression (score 1–4) or having mild/moderate/moderately severe/severe depression (score ≥5–27). Having a mental health problem was based on having self-reported more than 15 days of poor mental health in the past 30 days (NHANES 2001–2012).23
Substance Use
History of substance use behaviors included: (1) risky alcohol consumption (defined as having 4+ (for females) or 5+ (for males) drink/day, every day, at any point in past),24 (2) use of cocaine, heroin, or methamphetamine (NHANES 2005–2016), and (3) use of marijuana or hashish (NHANES 2005–2016).
Statistical Analysis
Data management and statistical analyses were conducted using SAS version 9.4 (SAS Institute Inc., Cary, NC) adjusting for NHANES sample weights and design effects. We stratified the pooled sample into two groups (PLWH, People without HIV) and examined group differences in sociodemographic characteristics, smoking profile, depression, mental health, alcohol and substance use history. We combined our data based on the CDC instructions.21 We weighted records from each survey year according to person-level weights. Then, we adjusted weights per the number of representative years used in the analyses by dividing the original weight by eight, the total number of 2-year survey cycles. Each person was counted as one observation each time in the merged dataset. We calculated weighted prevalence rates and corresponding 95% confidence intervals (95% CI) of current smokers among PLWH compared to people without HIV (Table 1). Chi-square test for independence for categorical variables and independent two-sample Student's t test for continuous variables were then used to detect statistical significance. Prevalence estimates with a relative standard error more than 30% were noted in the tables as they do not meet the NHANES standard of reliability/precision.25 We calculated weighted percentages and used weighted second-degree polynomial linear regression of prevalence on year for the trend analysis of current smoking and quit ratio (Figure 2).26 Two multivariable logistic regression models were fitted (Table 2). The first model included only current smokers, and tested correlates of smoking among PLWH versus people without HIV. In this model, HIV status (positive vs. negative) was the dependent variable. The second model included only PLWH and tested correlates of being a current smoker among PLWH. The dependent variable was smoking status (current smoker vs. former/never smoker). The two models included all sociodemographic characteristics (age, gender, race/ethnicity, marital status, educational attainment, health insurance, employment status, and sexual orientation), substance use (ever heavy alcohol use, ever use any drug including marijuana, cocaine, heroin, methamphetamine, and injection drugs), and depression. Missing data were handled by complete case analysis. Participants with missing values were excluded from the analysis, and sample weights and design effects were adjusted accordingly. We reported results using adjusted odds ratios (aORs) and 95% CIs.
Table 1.
Demographic Characteristics, Psychological Status, Substance Use, and Smoking Profile Among People Living with HIV Who Are Current Smokersa Compared to People Without HIV (NHANES 1999–2016)b
| Characteristics | Overall (N = 26 457) | People with HIV (N = 152) | People without HIV (N = 26 305) | p-valuec | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | % | 95% CI | N | % | 95% CI | N | % | 95% CI | ||
| All | 6740 | 25.6 | 24.6 to 26.6 | 71 | 47.0 | 35.4 to 58.6 | 6669 | 25.5 | 24.5 to 26.5 | <.0001 |
| Age (years) | .003 | |||||||||
| 20–29 | 2009 | 30.9 | 29.4 to 32.3 | 8 | 8.4J | 1.5 to 15.2 | 2001 | 31.1 | 29.6 to 32.5 | |
| 30–39 | 1949 | 29.1 | 27.5 to 30.6 | 18 | 26.5J | 10.5 to 42.5 | 1931 | 29.1 | 27.5 to 30.6 | |
| 40–49 | 1974 | 29.2 | 27.8 to 30.5 | 29 | 41.9 | 25.6 to 58.2 | 1945 | 29.0 | 27.6 to 30.4 | |
| 50–59 | 808 | 10.9 | 9.7 to 12.1 | 16 | 23.3J | 8.7 to 37.8 | 792 | 10.8 | 9.7 to 12.0 | |
| Gender | <.0001 | |||||||||
| Male | 3788 | 54.7 | 53.4 to 56.4 | 52 | 80.7 | 70.8 to 90.7 | 3736 | 54.5 | 53.2 to 55.8 | |
| Female | 2952 | 45.3 | 44.0 to 46.6 | 19 | 19.3 | 9.3 to 29.2 | 2933 | 45.5 | 44.1 to 46.8 | |
| Sexual orientation | <.0001 | |||||||||
| Heterosexual | 5015 | 92.0 | 91.1 to 92.8 | 23 | 35.6 | 18.0 to 53.2 | 4992 | 92.4 | 91.6 to 93.2 | |
| Homosexual | 121 | 2.5 | 1.9 to 3.2 | 19 | 46.2 | 27.4 to 65.1 | 102 | 2.2 | 1.7 to 2.7 | |
| Bisexual | 249 | 4.1 | 3.5 to 4.7 | 8 | 14.6J | 1.8 to 27.4 | 241 | 4.1 | 3.5 to 4.7 | |
| Others/Don't know | 103 | 1.4 | 1.1 to 1.6 | 2 | 3.6 | 0.0 to 8.7 | 101 | 1.3 | 1.1 to 1.6 | |
| Race/Ethnicity | <.0001 | |||||||||
| Non-Hispanic White | 3354 | 73.3 | 70.7 to 75.8 | 14 | 42.9 | 26.3 to 59.5 | 3340 | 73.5 | 71.0 to 76.1 | |
| Non-Hispanic Black | 1540 | 13.5 | 11.9 to 15.0 | 47 | 47.4 | 33.0 to 61.8 | 1493 | 13.2 | 11.6 to 14.7 | |
| Hispanic | 1391 | 13.3 | 11.4 to 15.2 | 10 | 9.7 | 4.0 to 15.4 | 1381 | 13.3 | 11.4 to 15.2 | |
| Education | .125 | |||||||||
| High school or less | 4194 | 57.3 | 55.5, 59.2 | 37 | 44.9 | 28.4 to 61.3 | 4157 | 57.5 | 55.6 to 59.3 | |
| Some college or more | 2543 | 42.7 | 40.8, 44.5 | 34 | 55.1 | 38.7 to 71.6 | 2509 | 42.5 | 40.7 to 44.4 | |
| Marital status | .056 | |||||||||
| Married/Living with partner | 3498 | 54.6 | 52.8 to 56.3 | 27 | 43.3 | 27.2 to 59.5 | 3471 | 54.7 | 52.9 to 56.5 | |
| Divorced/Widowed/Separated | 1248 | 18.0 | 16.7 to 19.3 | 8 | 12.0J | 2.06 to 21.9 | 1240 | 18.1 | 16.8 to 19.3 | |
| Never married | 1934 | 27.4 | 25.7 to 29.1 | 34 | 44.7 | 28.0 to 61.4 | 1900 | 27.3 | 25.6 to 28.9 | |
| Family poverty index ratio (PIR)d | .284 | |||||||||
| <Poverty level (PIR < 1) | 2089 | 25.0 | 23.3 to 26.8 | 30 | 31.9 | 18.2 to 45.7 | 2059 | 25.0 | 23.2 to 26.7 | |
| ≥Poverty level (PIR ≥ 1) | 4158 | 75.0 | 73.2 to 76.7 | 36 | 68.1 | 54.3 to 81.8 | 4122 | 75.0 | 73.3 to 76.8 | |
| Employment | .008 | |||||||||
| Yes | 4401 | 70.3 | 68.7 to 71.9 | 27 | 50.0 | 33.3 to 66.8 | 4374 | 70.5 | 68.9 to 72.1 | |
| No | 2334 | 29.7 | 28.1 to 31.3 | 44 | 50.0 | 33.2 to 66.7 | 2290 | 29.5 | 27.9 to 31.1 | |
| Health care insurance | .058 | |||||||||
| Yes | 4089 | 65.4 | 63.9 to 70.0 | 53 | 77.0 | 66.1 to 87.9 | 4036 | 65.3 | 63.8 to 66.9 | |
| No | 2619 | 34.6 | 33.0 to 36.1 | 18 | 23.0 | 12.1 to 33.9 | 2601 | 34.7 | 33.1 to 36.2 | |
| Have been heavy alcohol usere | 1715 | 29.0 | 27.5 to 30.5 | 20 | 34.4 | 16.8 to 51.9 | 1695 | 28.9 | 27.4 to 30.4 | .528 |
| Have depressionf | <.0001 | |||||||||
| Score 1–4 Minimal depression | 2710 | 64.9 | 63 to 66.8 | 19 | 38.7 | 19.9 to 57.4 | 2691 | 65.1 | 63.2 to 67 | |
| Score 5–9 Mild depression | 856 | 19.8 | 18.4 to 21.1 | 15 | 51.2 | 30.2 to 72.1 | 841 | 19.5 | 18.2 to 20.8 | |
| Score 10–14 Moderate depression | 429 | 9.6 | 8.5 to 10.8 | 4 | 6.0J | 0 to 12.5 | 425 | 9.7 | 8.5 to 10.8 | |
| Score 15–19 Moderately severe | 181 | 3.9 | 3.1 to 4.6 | 2 | 2.7J | 0 to 6.6 | 179 | 3.7 | 3.1 to 4.6 | |
| Score 20–27 Severe depression | 95 | 1.8 | 1.4 to 2.2 | 1 | 1.5J | 0 to 4.3 | 94 | 1.8 | 1.4 to 2.3 | |
| Have poor mental healthg | 751 | 33.6 | 31.5 to 35.8 | 8 | 26.7J | 3.9 to 49.4 | 743 | 33.7 | 31.5 to 35.9 | .573 |
| Used marijuana or hashishh | 3388 | 83.8 | 82.5 to 85.2 | 33 | 89.1 | 79.5 to 98.8 | 3355 | 83.8 | 82.4 to 85.1 | .352 |
| Used cocaine, heroin, or methamphetaminesh | 1556 | 39.0 | 36.6 to 41.4 | 22 | 54.2 | 35.4 to 73.0 | 1534 | 38.9 | 36.4 to 41.3 | .099 |
| Used injection drugsh | 243 | 6.34 | 5.3 to 7.4 | 2 | 2.8J | 0.0 to 6.9 | 241 | 6.4 | 5.3 to 7.4 | .245 |
| Smoking pattern | .5187 | |||||||||
| Smoke cigarette every day | 5384 | 81.4 | 80.1 to 82.7 | 58 | 84.9 | 75.0 to 94.5 | 5326 | 81.4 | 80.1 to 82.7 | |
| Smoke cigarette some daysh | 1356 | 18.6 | 17.3 to 19.9 | 13 | 15.1J | 5.2 to 25.0 | 1343 | 18.6 | 17.3 to 19.9 | |
| Tried to quit smoking for 1+ day in the past 12 months (yes)I | 814 | 49.9 | 46.6 to 53.2 | 12 | 71.0J | 50.4 to 91.7 | 802 | 49.7 | 46.4 to 53.0 | .0662 |
| Mean [SD] | Mean [SD] | Mean [SD] | ||||||||
| Number of times stopped smoking for 1+ day in the past 12 months | 870 | — | 6.6 [1.62] | 12 | — | 1.8 [0.39] | 802 | — | 5.7 [1.44] | .0082 |
| Age when started smoking regularly | 13452 | — | 18.0 [0.27] | 92 | — | 17.9 [0.70] | 10981 | — | 17.8 [0.27] | .7860 |
| Number of cigarettes smoked per day | 4815 | — | 18.5 [1.00] | 15 | — | 9.9 [3.90] | 3755 | — | 18.2 [1.25] | .0482 |
aSelf-report of smoking cigarettes every day or someday in the last 30 days; bn is unweighted but % and 95% CI are weighted with NHANES survey design weights; cBased on chi-square test or t test; dLiving at or above (PIR ≥ 1) or below the poverty threshold (PIR < 1); e5+ (males) or 4+ (females) drink/day, every day, at any point in past; fBased on the Patients Health Questionnaire (PHQ-9); g Self-reported, ≥15 days of poor mental health past 30 days; hEver use; IDuring the past 12 months, have you stopped smoking for one day or longer because you were trying to quit?; JThe relative standard error (RSE) is 30% or more and may be subject to high sampling error.
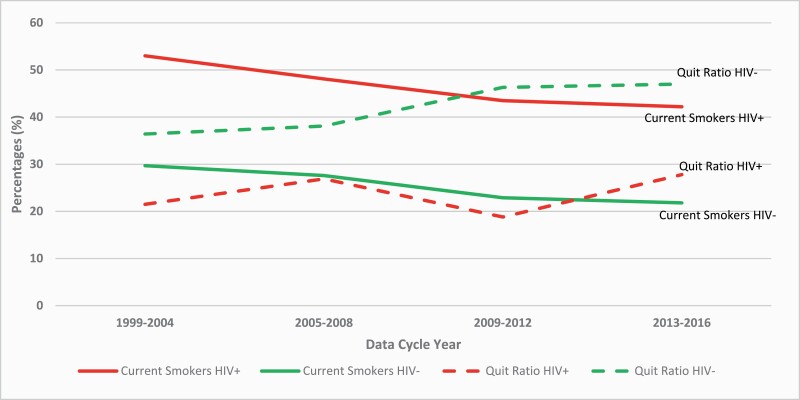
Figure 2.
Trend analysis of change in the percentage of current smoking and quit ratio among people living with HIV compared to people without HIV (NHANES; 8 survey cycles, 1999–2016) (weighted percentages).
Table 2.
Multivariable Logistic Regression Analysis (NHANES 1999–2016)
| People living with HIV who are current smokers compared to people without HIV who are current smokers | People living with HIV who are current smokers compared with people living with HIV who are not smokers | |||
|---|---|---|---|---|
| aORa | 95% CIb | aORa | 95% CIb | |
| Age (years) | 1.096 | (1.057 to 1.136) | 1.036 | (0.985 to 1.088) |
| Gender | ||||
| Female | 1.000 | — | 1.000 | — |
| Male | 7.963 | (2.497 to 25.395) | 2.754 | (0.590 to 12.843) |
| Race/Ethnicity | ||||
| Non-Hispanic White | 1.000 | — | 1.000 | — |
| Non-Hispanic Black | 10.449 | (4.129 to 26.445) | 1.107 | (0.243 to 5.034) |
| Hispanic | 2.592 | (0.705 to 9.527) | 1.585 | (0.170 to 14.785) |
| Education | ||||
| High school or less | 1.000 | — | 1.000 | — |
| Some college or more | 2.208 | (0.980 to 4.971) | 1.548 | (0.390 to 6.148) |
| Marital status | ||||
| Never married | 1.000 | — | 1.000 | — |
| Married/living with partner | 1.497 | (0.465 to 4.822) | 1.042 | (0.277 to 3.915) |
| Divorced/Separated/Widowed | 0.638 | (0.134 to 3.034) | 0.925 | (0.123 to 6.980) |
| Sexual orientation | ||||
| Homosexual | 1.000 | — | 1.000 | — |
| Heterosexual/Bisexual/Other | 0.016 | (0.004 to 0.067) | 1.452 | (0.425 to 4.955) |
| Employment | ||||
| No | 1.000 | — | 1.000 | — |
| Yes | 0.760 | (0.300 to 1.923) | 1.283 | (0.454 to 3.627) |
| Heavy alcohol userc | ||||
| No | 1.000 | — | 1.000 | — |
| Yes | 0.804 | (0.219 to 2.952) | 0.830 | (0.170 to 4.044) |
| Having depressiond | ||||
| Not at all | 1.000 | — | 1.000 | — |
| Yes (mild to severe depression) | 3.791 | (1.219 to 11.788) | 3.078 | (0.853 to 11.113) |
| Any drug usere | ||||
| No | 1.000 | — | 1.000 | — |
| Yes | 2.133 | (0.610 to 7.459) | 7.524 | (2.038 to 27.772) |
aOR: adjusted odds ratio by including all the variables above.
b95%CI = 95% Confidence Interval.
c5+ (for males) or 4+ (for females) drink/day, every day, at any point in past.
dBased on having a score of 1–4: no depression, and a score of 5–27: mild to severe depression in Patients Health Questionnaire (PHQ-9).
eEver use of any drug use including marijuana, cocaine, heroin, methamphetamine, and injection drugs.
Results
There was a total of 88 062 participants in NHANES between 1999 and 2016. Among these, 61 605 (70.0%) were excluded from the analysis and 26 457 (30.0%) were included (Figure 1). Excluded participants were younger than 20 years old (not asked about smoking) (n = 40 929), older than 59 years old (not tested for HIV) (n = 15 803) or were missing HIV test results (n = 4856) or smoking status (n = 24). Overall, 26 457 participants (PLWH = 152; people without HIV = 26 305) were included in the analysis. Among PLWH, 71 were smokers and 81 were nonsmokers (former or never smokers). Of those without HIV, 6669 were smokers and 19 636 were nonsmokers.
Characteristics of PLWH Compared to People without HIV
The sociodemographic characteristics of the sample are shown in Table 1. Compared to smokers without HIV, PLWH who are current smokers were significantly older (≥50 years old, 23.3% [95% CIs = 8.7 to 37.8] vs. 10.8% [9.7 to 12.0], male (80.7% [70.8 to 90.7] vs. 54.5% [53.2 to 55.8]), gay (46.2% [27.4 to 65.1] vs. 2.2% [1.7 to 2.7]) and bisexual (14.6% [1.8 to 27.4] vs. 4.1% [3.5 to 4.7]), non-Hispanic Black (47.4% [33.0 to 61.8] vs. 13.2% [11.6 to 14.7]), and unemployed (50.0% [33.3 to 66.7] vs. 29.5% [27.9 to 31.1]). PLWH were also significantly more likely to have depression (61.4% [42.6 to 80.1] vs. 34.9% [33.0 to 36.8]), (p < .05 for all).
Smoking prevalence was significantly higher among PLWH compared to people without HIV (47.0% [35.4 to 58.6] vs. 25.5% [24.5 to 26.5]; p < .0001). Compared to people without HIV, PLWH were less likely to be former smokers (18.3% vs. 14.6%) and never smokers (56.2% vs. 38.4%). Compared to smokers without HIV, the number of successful quit attempts was significantly lower among PLWH (5.7 ± [1.44] vs. 1.8 ± SD [0.39]; p < .0003). However, the number of cigarettes smoked per day was significantly lower in PLWH compared with people without HIV (9.9 ± [3.90] vs. 18.2 ± [1.25]; p = .048).
Time-Trends in Smoking Prevalence and Quit Ratio
Figure 2 depicts the time-trend in smoking prevalence and quit ratio among PLWH compared to people without HIV from 1999 to 2016. Over the 18-year period, the prevalence of current smoking declined by approximately 10% (from 53.0% in 1999 to 42.2% in 2016) among PLWH and by 7.9% (from 29.7 in 1999 to 21.8% in 2016) among people without HIV. However, compared to PLWH, the overall increase in quit ratio was higher in the people without HIV during this period (PLWH: 6.3% increase [from 21.5% in 1999 to 26.9% in 2016]; people without HIV: 10.6% increase [from 36.4% in 1999 to 47.0% in 2016]). The difference between the two groups was not statistically significant for both smoking prevalence and quit ratio.
Correlates of Smoking Among PLWH
In the first multivariable logistic regression model that compared PLWH smokers with smokers among people without HIV, PLWH who are current smokers were more likely to be older (aOR = 1.10; 95% CIs = 1.06 to 1.14), male (7.96; 2.50 to 25.40), non-Hispanic Black (10.45; 4.13 to 26.45), and suffering from depression (3.79; 1.22 to 11.79), while those who were heterosexual or bisexual were less likely to be current smokers (0.02; 0.00 to 0.07) (Table 2). In the second model that compared PLWH smokers with PLWH nonsmokers, those who were substance users were more likely to be current smokers (7.52; 2.04 to 27.8) (Table 2).
Discussion
This study is the first to document the prevalence, time-trends, and correlates of smoking in a nationally representative sample of PLWH compared with people without HIV in the US Consistent with prior reports, our findings confirmed that smoking prevalence in PLWH is double that of the general population.11,27,28 The decline in smoking among PLWH over a period of 18 years has been modest, and almost half of PLWH are still smokers. Disparities in smoking persist among PLWH, with those who are oldest, male, non-Hispanic Black, not employed, and gay more likely to be current smokers.28 These factors are common denominators of smoking, and underlie the deeper roots of unhealthy behavior and barriers to promoting health in groups that face many challenges and have the least resources to address them.29 Our findings are also compatible with prior findings suggesting that PLWH face several challenges such as high rates of substance use and comorbid psychiatric illnesses such as depression that may undermine their smoking cessation efforts.30,31 Given the substantial negative effect of smoking on PLWH's mortality and morbidity,4 greater resources and efforts should be allocated to improve smoking cessation outcomes among PLWH. In addition, smoking cessation interventions designed for PLWH should incorporate assessment and treatment of depression and substance use, especially among those who are disproportionately affected by HIV and smoking including non-Hispanic Blacks and gay.
Smoking among PLWH seems to be a global public health problem in need of special attention. The positive association between HIV and cigarette smoking observed in our study aligns with previous reports from other countries across the globe. For example, similar results were reported in Canada and Italy indicating that smoking among PLWH is double that in the general population.32,33 In addition, in a study in 28 low- and middle-income countries, male PLWH were 41% more likely to use tobacco than men without HIV.34 Similarly, in a cross-sectional survey in Zimbabwe among 6111 factory workers, smoking prevalence among PLWH was double that among those without HIV (27% vs. 17%).35 As in prior research, our results indicated that tobacco-related disparities by gender, sexual orientation, and race/ethnicity among PLWH persists and mirrors those who are most affected by HIV infection.13,14,36 Smoking rates were the highest among males, gay, and non-Hispanic Blacks. In the United States, non-Hispanic Blacks represent 45% of all new HIV infections each year,37 and non-Hispanic Black men who have sex with men (MSM) constitute more than 75% of new infections in this race group.38 Prior studies have documented significantly higher rates of cigarette smoking among MSM HIV patients.39 Qualitative research exploring smoking cessation among this group indicated that the most common barriers to quitting smoking are low self-efficacy, emotional stress, substance use, and cultural factors related to sexual orientation (eg, considering bars an important social venue where smoking helps them feel more relaxed and able to “fit in” socially).18 To date, very few interventions have been developed to address the complex social and emotional needs that may impact smoking behavior and response to smoking cessation interventions within this group.40 We found only one pilot study that examined a culturally tailored smoking cessation intervention among 31 HIV non-Hispanic black MSM smokers.18 Results indicated that the intervention was feasible, acceptable, and showed benefits for reducing smoking and depression scores. However, this study was a feasibility trial, and therefore was limited in terms of the size and scope of its findings. Thus, there is a critical need to further develop and test through a large-scale trial culturally acceptable and effective smoking cessation interventions for those minority subgroups most disproportionately impacted by HIV infection and at risk for smoking-related health disparities.41
Our time-trends results are consistent with two prior reports suggesting that the decline in smoking prevalence among PLWH was comparable to that in the general population.13,42 This could be due to increasing attention to the alarming high smoking rates among PLWH and the substantial negative impact of smoking on HIV progression and treatment. Improving smoking cessation among PLWH has recently become a high priority area for the National Institutes of Health (NIH), and more resources and funds have been devoted to achieving this goal nationally and internationally. However, our results have shown that the increase in the quit ratio in the general population was higher than that in PLWH. A possible explanation could be that the decline in smoking among PLWH is not related to improvement in smoking cessation but rather to fewer individuals initiating smoking due to recent wide implementation of tobacco control measures targeting this group (eg, publicizing anti-smoking campaigns, banning tobacco advertising and promotion, increasing taxes on tobacco products, promoting smoke-free environments, banning smoking in public places).43,44
Our findings indicated that PLWH who smoke are more likely to be depressed than smokers in the general population.14,45 Depression represents a significant barrier to successful smoking cessation.46–48 To date, only two pilot clinical trials have addressed this problem among PLWH smokers.49,50 Although these two studies are promising and have provided some evidence of benefit, they were methodologically limited by having small sample sizes, low numbers of female participants, high attrition rate, and lack of active control group. Given the potential of such interventions in helping PLWH to quit smoking, more trials with a larger and more diverse sample are warranted. Another important area to improve cessation among PLWH is the need to address the intersection between substance use and smoking. The observed association between current smoking and substance use among PLWH in the present study is compatible with prior findings, and is an important consideration in designing or adapting smoking cessation interventions for PLWH.10,36 Yet, engaging substance users in smoking cessation treatment is a significant challenge. Currently, there are no official medical recommendations for the treatment of tobacco addiction in illicit polysubstance users. We are not aware of any previous study that has tried to address this problem among PLWH. Smoking cessation interventions specifically designed for PLWH may benefit from flexibility to address the concurrent use of tobacco and substance use. For example, identifying dual substance and tobacco users within HIV primary care and evaluating combined interventions that address the two problems might improve smoking cessation efforts among PLWH.
There are several study limitations that should be addressed. The cross-sectional design of the NHANES prevented us from making any causal inferences of the observed associations. Smoking status was based on self-report rather than on biochemical data, which could result in under-reporting due to social desirability. An additional limitation was that despite pooling data across several survey years, sample sizes for some subgroups were small thus limiting the power to detect statistically significant differences and resulting in wider CIs for aORs. Despite these limitations, this report presents unique, nationally representative findings about a serious public health problem in the United States.
Conclusion
PLWH are a group at high risk for tobacco-related health problems and should be a prime focus for smoking cessation efforts. Despite the substantial negative health effect of smoking among PLWH, only modest progress has been made in reducing their smoking. Almost half of this population are current smokers, and tobacco-related health disparity persists. PLWH who are current cigarette smokers are members of several marginalized groups including ethnic minorities, the unemployed, and gay.28 PLWH have a complex psychosocial profile with socioeconomic challenges, psychiatric conditions (ie, depression), and illicit drug use (ie, marijuana, alcohol) that hinder their smoking cessation efforts.18,28 Targeted and tailored smoking cessation interventions that address their unique profile and needs are urgently needed. In particular, improving the screening and treatment of PLWH smokers who are substance users or have depression is critical to improve their smoking cessation outcomes.
Supplementary Material
A Contributorship Form detailing each author’s specific involvement with this content, as well as any supplementary data, are available online at https://academic.oup.com/ntr.
Acknowledgments
For the current study, TA conceptualized and designed the study and drafted the initial manuscript. TSK supervised and performed the initial analyses. All authors contributed to interpretation of the results and critically revised the manuscript for significant intellectual content. All authors approved the final draft of the manuscript as submitted and agreed to be responsible for all aspects of the study.
Funding
Funding for this study was provided by the Miami Center for AIDS Research (CFAR) at the University of Miami (P30AI07396 – CFAR developmental award to Dr. Asfar). Supplemental funding was provided by the Sylvester Comprehensive Cancer Center at University of Miami Miller School of Medicine. Research reported in this publication was also supported by the National Cancer Institute of the National Institutes of Health under Award Number P30CA240139. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Declaration of Interests
The authors declare they have no conflicts of interest.
References
- 1. Centers for Disease Control and Prevention. HIV Surveillance Report, 2018 (Preliminary); vol. 30. [Published November 2019]. http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html
- 2. Fumiyo N, Lodwick RK, Smith CJ.et al. Projected life expectancy of people with HIV according to timing of diagnosis. AIDS. 2012;26(3):335–343. [DOI] [PubMed] [Google Scholar]
- 3. Lifson AR, Neuhaus J, Arribas JR, van den Berg-Wolf M, Labriola AM, Read TR; INSIGHT SMART Study Group . Smoking-related health risks among persons with HIV in the Strategies for Management of Antiretroviral Therapy clinical trial. Am J Public Health. 2010;100(10):1896–1903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Helleberg M, May MT, Ingle SM, et al. Smoking and life expectancy among HIV-infected individuals on antiretroviral therapy in Europe and North America. AIDS. 2015;29(2):221–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Clifford GM, Polesel J, Rickenbach M, et al. ; Swiss HIV Cohort . Cancer risk in the Swiss HIV Cohort Study: associations with immunodeficiency, smoking, and highly active antiretroviral therapy. J Natl Cancer Inst. 2005;97(6):425–432. [DOI] [PubMed] [Google Scholar]
- 6. Calvo‐Sánchez M, Perello R, Perez I.et al. Differences between HIV‐infected and uninfected adults in the contributions of smoking, diabetes and hypertension to acute coronary syndrome: two parallel case–control studies. HIV Med. 2013;14(1):40–48. [DOI] [PubMed] [Google Scholar]
- 7. Helleberg M, Afzal S, Kronborg G, et al. Mortality attributable to smoking among HIV-1-infected individuals: a nationwide, population-based cohort study. Clin Infect Dis. 2013;56(5):727–734. [DOI] [PubMed] [Google Scholar]
- 8. Crothers K, Griffith TA, McGinnis KA, et al. The impact of cigarette smoking on mortality, quality of life, and comorbid illness among HIV-positive veterans. J Gen Intern Med. 2005;20(12):1142–1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ledgerwood DM, Yskes R. Smoking cessation for people living with HIV/AIDS: a literature review and synthesis. Nicotine Tob Res. 2016;18(12):2177–2184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Burkhalter JE, Springer CM, Chhabra R, Ostroff JS, Rapkin BD. Tobacco use and readiness to quit smoking in low-income HIV-infected persons. Nicotine Tob Res. 2005;7(4):511–522. [DOI] [PubMed] [Google Scholar]
- 11. Tesoriero JM, Gieryic SM, Carrascal A, Lavigne HE. Smoking among HIV positive New Yorkers: prevalence, frequency, and opportunities for cessation. AIDS Behav. 2010;14(4):824–835. [DOI] [PubMed] [Google Scholar]
- 12. Pacek LR, Harrell PT, Martins SS. Cigarette smoking and drug use among a nationally representative sample of HIV-positive individuals. Am J Addict. 2014;23(6):582–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Frazier EL, Sutton MY, Brooks, JT, et al. Trends in cigarette smoking among adults with HIV compared with the general adult population, United States-2009–2014. Prev Med. 2018;111:231–234. [DOI] [PubMed] [Google Scholar]
- 14. Mdodo R, Frazier EL, Dube SR, et al. Cigarette smoking prevalence among adults with HIV compared with the general adult population in the United States: cross-sectional surveys. Ann Intern Med. 2015;162(5):335–344. [DOI] [PubMed] [Google Scholar]
- 15. Collins RL, Kanouse DE, Gifford AL, et al. Changes in health-promoting behavior following diagnosis with HIV: prevalence and correlates in a national probability sample. Health Psychol. 2001;20(5):351–360. [PubMed] [Google Scholar]
- 16.National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta, (GA): Centers for Disease Control and Prevention (US); 2014. doi: 10.1002/cncr.28695. Epub 2014 Mar 28. [DOI] [PubMed] [Google Scholar]
- 17. Shuter J, Bernstein SL, Moadel AB. Cigarette smoking behaviors and beliefs in persons living with HIV/AIDS. Am J Health Behav. 2012;36(1):75–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Matthews AK, Conrad M, Kuhnset L, et al. A qualitative examination of barriers and motivators to smoking cessation among HIV positive African American MSM smokers. J Health Dispar Res Pract. 2014;7(2):4.25419491 [Google Scholar]
- 19. Chichetto NE, Kundu S, Freiberg MS, et al. ; Veterans Aging Cohort Study . Association of syndemic unhealthy alcohol use, cigarette use, and depression with all-cause mortality among adults living with and without hiv infection: veterans aging cohort study. Open Forum Infect Dis. 2019;6(6):ofz188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. CDC. NHANES: HIV Antibody/HIV-1/HIV-2 Differentiation Assay. 2014. [cited 2020 March, 28]. https://wwwn.cdc.gov/nchs/data/nhanes/2015–2016/labmethods/HIV_I_MET_MS.pdf.
- 21. CDC. NHANES Analytic and Reporting Guidelines 2005. https://www.cdc.gov/nchs/data/nhanes/nhanes_03_04/nhanes_analytic_guidelines_dec_2005.pdf
- 22. Löwe B, Kroenkeb K, Herzoget W, et al. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9). J Affect Disord. 2004;81(1):61–66. [DOI] [PubMed] [Google Scholar]
- 23. Center for Disease Control and Prevention. Measuring Healthy Days: Population Assessment of Health-related Quality of Life. Atlanta: CDC; 2000:4–6. https://www.cdc.gov/hrqol/pdfs/mhd.pdf [Google Scholar]
- 24. Wechsler H, Nelson TF, Binge drinking and the American college students: what's five drinks? Psychol Addict Behav. 2001;15(4):287. [DOI] [PubMed] [Google Scholar]
- 25. Control, C.f.D., et al. Measuring Healthy Days: Population Assessment of Health-related Quality of Life. Atlanta: CDC; 2000:4–6. [Google Scholar]
- 26. Fan J, Heckman NE, Wand MP. Local polynomial kernel regression for generalized linear models and quasi-likelihood functions. J Am Stat Assoc. 1995;90(429):141–150. [Google Scholar]
- 27. CDC. Cigarette smoking among adults—United States, 2005–2015. MMWR Surveill Summ. 2016;65(44):1205–1211. [DOI] [PubMed] [Google Scholar]
- 28. Pool ERM, Dogar O, Lindsay RP, et al. Interventions for tobacco use cessation in people living with HIV and AIDS. Cochrane Database Syst Rev. 2016(6):CD011120.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Laaksonen M, Rahkonen O, Karvonen S, Lahelma E. Socioeconomic status and smoking: analysing inequalities with multiple indicators. Eur J Public Health. 2005;15(3):262–269. [DOI] [PubMed] [Google Scholar]
- 30. Zyambo CM, Burkholder GA, Cropsey KL, et al. Mental health disorders and alcohol use are associated with increased likelihood of smoking relapse among people living with HIV attending routine clinical care. BMC Public Health. 2019;19(1):1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Goodwin RD, Wall MM, Gareyet L, et al. Depression among current, former, and never smokers from 2005 to 2013: the hidden role of disparities in depression in the ongoing tobacco epidemic. Drug Alcohol Depend. 2017;173:191–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bekele T, Rueda S, Gardner S, et al. Trends and correlates of cigarette smoking and its impacts on health-related quality of life among people living with HIV: findings from the Ontario HIV Treatment Network Cohort Study, 2008–2014. AIDS Patient Care STDs. 2017;31(2):49–59. [DOI] [PubMed] [Google Scholar]
- 33. De Socio GV, Pasqualini M, Ricci E, et al. Smoking habits in HIV-infected people compared with the general population in Italy: a cross-sectional study. BMC Public Health. 2020;20:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Mdege ND, Shah S, Ayo-Yusuf OA, Hakim J, Siddiqi K. Tobacco use among people living with HIV: analysis of data from Demographic and Health Surveys from 28 low-income and middle-income countries. Lancet Glob Health. 2017;5(6):e578–e592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Munyati SS, Redzo N, Dauya E, et al. Human immunodeficiency virus, smoking and self-rated health in Harare, Zimbabwe. Int J Tuberc Lung Dis. 2006;10(11):1279–1285. [PubMed] [Google Scholar]
- 36. Gritz ER, Vidrine DJ, Lazev AB, Amick BC 3rd, Arduino RC. Smoking behavior in a low-income multiethnic HIV/AIDS population. Nicotine Tob Res. 2004;6(1):71–77. [DOI] [PubMed] [Google Scholar]
- 37. Lansky A, Brooks JT, DiNenno E, Heffelfinger J, Hall HI, Mermin J. Epidemiology of HIV in the United States. J Acquir Immune Defic Syndr. 2010;55(suppl 2):S64–S68. [DOI] [PubMed] [Google Scholar]
- 38. McQuillan GM, Kruszon-Moran D, Granade T, et al. Seroprevalence of HIV in the US household population aged 18–49 years: the National Health and Nutrition Examination Surveys, 1999–2006. J Acquir Immune Defic Syndr. 2010;53(1):117–123. [DOI] [PubMed] [Google Scholar]
- 39. Johnson SE, Holder-Hayes E, Tessman GT, et al. Tobacco product use among sexual minority adults: findings from the 2012− 2013 national adult tobacco survey. Am J Prev Med. 2016;50(4):e91–e100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Nahvi S, Cooperman NA. The need for smoking cessation among HIV-positive smokers. AIDS Educ Prev. 2009;21(3 Suppl):14–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Shariati H, Armstrong HL, Cui Z, et al. Changes in smoking status among a longitudinal cohort of gay, bisexual, and other men who have sex with men in Vancouver, Canada. Drug Alcohol Depend. 2017;179:370–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hessol NA, Weber KM, D'Souza G, et al. Smoking cessation and recidivism in the women's interagency human immunodeficiency virus study. Am J Prev Med. 2014;47(1):53–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. WHO. WHO REPORT on the global TOBA CCO epidemic, 2008. The MPOWER package; 2008. https://www.who.int/tobacco/mpower/2008/en/ [Google Scholar]
- 44. Centers for Disease Control Prevention. State smoke-free laws for worksites, restaurants, and bars--United States, 2000–2010. MMWR Morb Mortal Wkly Rep. 2011;60(15): 472. [PubMed] [Google Scholar]
- 45. Jamal A, Agaku IT, O'Connor E, et al. Current cigarette smoking among adults—United States, 2005–2013. MMWR Morb Mortal Wkly Rep. 2014;63(47):1108. [PMC free article] [PubMed] [Google Scholar]
- 46. Koszycki D, Benger M, Shlik J, Bradwejn J. Randomized trial of a meditation-based stress reduction program and cognitive behavior therapy in generalized social anxiety disorder. Behav Res Ther. 2007;45(10):2518–2526. [DOI] [PubMed] [Google Scholar]
- 47. De Francesco D, Underwood J, Post FA, et al. ; POPPY Study Group . Defining cognitive impairment in people-living-with-HIV: the POPPY study. BMC Infect Dis. 2016;16(1):617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Nanni MG, Caruso R, Mitchell AJ, Meggiolaro E, Grassi L. Depression in HIV infected patients: a review. Curr Psychiatry Rep. 2015;17(1):530. [DOI] [PubMed] [Google Scholar]
- 49. Balfour L, Wiebe SA, Cameron WD, et al. An HIV-tailored quit-smoking counselling pilot intervention targeting depressive symptoms plus Nicotine Replacement Therapy. AIDS Care. 2017;29(1):24–31. [DOI] [PubMed] [Google Scholar]
- 50. O'Cleirigh C, Zvolensky MJ, Smits JAJ, et al. Integrated treatment for smoking cessation, anxiety, and depressed mood in people living with HIV: a randomized controlled trial. J Acquir Immune Defic Syndr. 2018;79(2):261–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.