Abstract
Levels of loneliness across the world have reached epidemic proportions, and their impact upon population health is increasingly apparent. In response, policies and initiatives have attempted to reduce loneliness by targeting social isolation among residents of local communities. Yet, little is known about the social psychological processes underpinning the relationships between community belonging, loneliness, and well‐being. We report three studies which apply the Social Identity Approach to Health to examine the mechanisms underpinning the relationships between community identity, health, and loneliness. Hypotheses were tested through secondary analyses of the 2014–2015 UK Community Life Survey (N = 4,314) as well as bespoke household surveys in a more (N = 408) and less (N = 143) affluent community at high risk of loneliness. Studies 1 and 2a demonstrated that the relationship between community identification and well‐being was mediated by increased social support and reduced loneliness. In Study 2b, community identification predicted well‐being through reduced loneliness, but not through social support. Our results are the first to evidence these relationships and suggest that community‐level interventions that enhance community identification and peer support can promote a potential Social Cure for loneliness.
Keywords: community, loneliness, social cure, social identity, social support
Background
International surveys of population health have shown that loneliness poses a threat to health as severe as that of smoking and obesity (Holt‐Lunstad, Smith, Baker, Harris, & Stephenson, 2015; Holt‐Lunstad, Smith, & Layton, 2010). This has prompted the creation of public health initiatives to understand and tackle loneliness within the context of local communities. These typically identify poor community cohesion and integration as contributing factors to loneliness and increased social integration as part of the solution.
However, such policies are rarely grounded in an in‐depth understanding of the complex relationships between community belonging, loneliness, and health. Social Psychology’s Social Identity Approach to Health, commonly referred to as the ‘Social Cure’ (Haslam, Jetten, Cruwys, Dingle, & Haslam, 2018), articulates the ways in which group memberships enhance individual well‐being. This approach has yet to be applied to investigations of how loneliness and health are shaped by community identification. Here, we report a programme of research, grounded in the Social Identity Approach to Health, which sets out to demonstrate the role of loneliness reduction as a key process through which community identification contributes to health.
Community impacts on health and well‐being
Pioneers in social psychology pointed to the role of local community in shaping residents’ social lives (e.g., Deutch & Collins, 1951; Festinger, Schachter, & Back, 1950). Since then, the community has come to occupy a secondary role – acting as the backdrop to individual and group life. Meanwhile, the sociological literature has demonstrated that the ‘social capital’ fostered within local communities has important implications for health and well‐being (Ehsan, Klaas, Bastianen, & Spini, 2019; Poortinga, 2006).
Social capital refers to the ties between individuals and the trust, mutual reciprocity, and support that these networks provide (Putnam, 2000). It comprises both behavioural and psychological components (Perkins & Long, 2002). Of the latter, the most widely studied is ‘psychological sense of community’ (or the feeling that one belongs to a larger social system, (Sarason, 1977)). Both social capital and psychological sense of community are broadly positively associated with health and well‐being (Ehsan et al., 2019; Perkins & Long, 2002; Pretty, Bishop, Fisher, & Sonn, 2007; Vinson, 2004). For instance, higher levels of social capital are associated with reduced loneliness in older adults (e.g., Coll‐Planas et al., 2017; Gallardo‐Peralta, de Roda, Angeles Molina‐Martinez, & Schettini del Moral, 2018), while sense of community is predictive of well‐being, satisfaction with life, and reduced loneliness (Farrell, Aubry, & Coulombe, 2004; Prezza, Amici, Roberti, & Tedeschi, 2001).
Conversely, socially disadvantaged neighbourhoods tend to be characterized by high levels of loneliness (Kearns, Whitley, Tannahill, & Ellaway, 2015; Scharf & de Jong Gierveld, 2008) due to barriers to social engagement, including low‐income levels, poor neighbourhood environment, a transient population, and poor services (Kearns et al., 2015). The range of supports from fellow neighbours tend to be narrower than in more affluent communities and tend to offer less protection against loneliness (Ehsan et al., 2019; Scharf & de Jong Gierveld, 2008). Given the links between these social resources, loneliness, and health, researchers have called for the use of specific case studies when examining the impact of neighbourhood SES on health (Ehsan et al., 2019; Scharf & de Jong Gierveld, 2008).
While the above evidence demonstrates that social capital and psychological sense of community are beneficial to health, both have been criticized for being vague concepts (Perkins & Long, 2002) that are not grounded in a theoretical framework that is able to specify the psychological mechanisms through which they confer their health benefits (Haslam et al., 2018). We argue that the Social Identity Approach to Health can address this gap.
The social cure in the community
Self‐defining in terms of a social group has been shown to impact upon individual physical and mental health through two main routes (Haslam et al., 2018; Jetten, Haslam, Haslam, & Branscombe, 2009). First, groups help their members to make sense of the world and interpret potential threats and opportunities (Haslam, O’Brien, Jetten, Vormedal, & Penna, 2005). This ‘primary appraisal’ serves to structure perceptions of both social and physical environments including noise, temperature, and crowdedness as well as social, economic, and political changes (Haslam et al., 2018).
Second, groups provide a range of psychological resources including social support and collective efficacy (Haslam et al., 2018). These serve to impact upon ‘secondary appraisal’ processes whereby group members evaluate their ability to cope with collective challenges. Greater levels of group support ensure that group members feel able to collectively cope with threat, thereby reducing stress and improving health. These effects have been found across a range of groups, including people with long‐term mental health problems (Cruwys et al., 2014), older adults (Gleibs, Haslam, Haslam, & Jones, 2011), adolescents (Miller, Wakefield, & Sani, 2016), and those recovering from addiction (Buckingham, Frings, & Albery, 2013).
Aside from the family and the nation, residential community is one of the most influential social groups for many people. Due to the many social categorizations shared among residents, it affords the development of multiple group memberships (Haslam et al., 2020), while at the same time, the range of social, economic, political, and environmental factors affecting local communities means that these groups often need to be strong social psychological units to allow coordinated coping (Fong, Cruwys, Haslam, & Haslam, 2019; Stevenson et al., 2019). In effect, local community can be a rich source of group support (Heath, Rabinovich, & Barreto, 2017; McNamara, Stevenson, & Muldoon, 2013). Moreover, local community can provide a strong sense of belonging to residents, giving meaning and purpose to their lives over and above the social interactions that occur there. In other words, local community identity has the potential to impact heavily on both primary and secondary appraisal processes.
There is emerging evidence of multiple positive consequences of community identification (Fong et al., 2019; McIntyre, Wickham, Barr, & Bentall, 2018; McNamara et al., 2013). It has been shown to have positive effects on psychological health (Fong et al., 2019; Heath et al., 2017; McNamara et al., 2013), well‐being and intergroup attitudes (Stevenson et al., 2019), satisfaction with life (Wakefield et al., 2017), and depression and paranoia (McIntyre et al., 2018). However, research also suggests that these relationships differ across community settings (McNamara et al., 2013). For instance, while community identification was associated with increased perceptions of social support in a socio‐economically disadvantaged neighbourhood, social support was not a significant mediator of the relationship between identification and well‐being (McNamara et al., 2013). This has also been found in other socially disadvantaged groups, including Black Americans (Outten, Schmitt, Garcia, & Branscombe, 2009), and young adults from socio‐economically disadvantaged backgrounds (Bakouri & Staerklé, 2015). Overall, this work suggests that community identification has a consistent direct effect on well‐being independently of social support (Bakouri & Staerklé, 2015) but that its effects on well‐being through increased social support appear to be dependent on the specific group context.
More recent research into the ways in which community identity has these positive effects has pointed to the role of loneliness reduction as a key factor. A longitudinal study of ‘Social Prescribing’ interventions to connect socially vulnerable community residents to activity groups has shown that their effects on community belonging serve to lower feelings of loneliness and, through this, lower primary health care usage (Kellezi et al., 2019). In other words, increased community belonging is associated with loneliness reduction, though the reasons why this should be the case remain under‐theorized.
Loneliness, threat and community identity
The psychological state of loneliness is associated with a range of neurological, cognitive, and behavioural effects (Cacioppo & Hawkley, 2009). The Hypervigilance to Social Threat hypothesis proposes that loneliness activates the hypothalamic–pituitary–adrenal (HPA) axis (Bangee, Harris, Bridges, Rotenberg, & Qualter, 2014; Qualter et al., 2013). For lonely individuals, this hypervigilance is specifically for identifying and attending to social threats whereby they are predisposed to interpret ambiguous social stimuli as threatening (Bangee & Qualter, 2018).
Lonely individuals typically have a ‘social isolation schema’ whereby they construe social events in line with their expectations of rejection and adopt a pessimistic‐avoidant coping strategy to social challenges (Cacioppo & Hawkley, 2005) which serves to perpetuate their isolation. Where social interactions do occur, these biases in attention, perception, and cognitive processing tend to predispose lonely individuals to unsuccessful and negative social encounters (Hawkley, Browne, & Cacioppo, 2005). They experience high levels of social anxiety which undermine their ability to engage in successful social interaction (Knowles, Lucas, Baumeister, & Gardner, 2015) and corrode their social networks over time (Lim, Rodebaugh, Zyphur, & Gleeson, 2016).
This patterning of perception and behaviour is in effect a mirror image of the positive effects of group membership and as such bears much similarity to the phenomenon of group‐based rejection known as the ‘Social Curse’ (Kellezi & Reicher, 2012). Research examining the effects of spoiled or stigmatized identities on group members’ interactions has similarly noted heightened threat‐based perception, avoidance of social encounters, and self‐defeating interactional strategies among excluded group members (e.g., Stevenson, McNamara, & Muldoon, 2014). Conversely, an emerging body of research in the Social Cure tradition has indicated that group identifications can serve to counter these effects and reduce loneliness: Social identity‐based interventions aimed at building group identifications can reduce loneliness and social anxiety (Haslam et al., 2019). Moreover, in the context of diverse communities, Social Cure research has shown that community identification predicts better intergroup relations though lowered intergroup anxiety (Stevenson et al., 2019). This relationship occurs both directly and indirectly through the social support that flows from community identification (Stevenson, Costa, Easterbrook, McNamara, & Kellezi, 2020). In other words, community identification appears to both reduce intergroup threat perception directly (via an effect on primary appraisal) while also indirectly providing the resource to manage these threats more effectively (via an effect on secondary appraisal).
Given the impact of loneliness on social threat perception detailed above, we might then expect community identification to play a role in ameliorating this effect. Specifically, we propose that local community identification can be a particularly rich source of meaning (belonging) and of practical resource (neighbourhood support) which should redress the effects of loneliness on primary and secondary appraisal. In effect, we would expect the psychological resources unlocked by community identification to have distinct and measurable impacts on loneliness. However, as noted above, the pathways through which community identification impacts upon well‐being vary according to group disadvantage and so these processes need to be examined as they occur in different neighbourhood contexts.
The current research
Previous research has shown that community identification is associated with a specific sense of locality‐based belonging which has significant impacts on residents (McNamara et al., 2013), including attenuating the negative impact of low neighbourhood SES on mental health (Fong et al., 2019), and allowing residents to cope better with neighbourhood diversification (Stevenson et al., 2019). It is also associated with an increase in the perception of a particular source of support – that from one’s neighbours (Heath et al., 2017; McNamara et al., 2013). Thus, in the current research, we first expect community identification to predict better well‐being. We also expect this relationship to be partially mediated through increased perceptions of support, specifically support received from neighbours, though this may differ across different community contexts. Finally, we propose a serial mediation model, such that identification with the community predicts increased perceptions of social support, which predicts reduced feelings of loneliness, which in turn predicts well‐being. This is in part to demonstrate the consequentiality of our findings for the well‐being of individuals and in part to allow us to specify that loneliness reduction is a key element of the well‐established association of community identification with well‐being.
We will test these hypotheses in a series of three studies using cross‐sectional community surveys. Study 1 tests these relationships at a national level using the 2014‐2015 UK Government’s Community Life Survey. This allows us to use a range of variables reflecting the broad meaning of the concepts we use (neighbourhood belonging, specific forms of supportive interactions with neighbours) which ensure the validity of our investigation. Studies 2a and 2b report the results of our analysis of custom neighbourhood surveys where we use validated measures of the theoretical constructs of interest which allows us to test the robustness of the previous findings as well as investigating the specific applicability of the Social Cure approach. In these latter studies, we explore the hypothesized relationships in two neighbourhoods both identified as having a high risk of loneliness, but which differ in terms of levels of socio‐economic deprivation. This allows us to address previous calls for these investigations to be conducted in the context of specific neighbourhoods with differing SES levels.
STUDY 1
Study 1 involved a secondary analysis of the 2014–2015 UK Community Life Survey. This is a random probability survey that uses the postal address file held by the Post Office as its sample source. Selected addresses were sent an information letter, after which an interviewer visited the address to attempt to complete the survey. One adult over the age of 16 is randomly selected to take part in each selected household. This survey contains in‐depth information on 5,000 respondents on a range of personal and social factors affecting their lives within their communities. The ‘face to face’ and the ‘web‐postal’ 2014–2015 Community Life Survey UK Cabinet databases were combined in the present study, and only respondents that answered the selected questions were included in the analyses.
Method
Participants
Participants (N = 4,314, 55% female and 45% male, Mage = 51.19 years, SD = 18.27, age range = 16–95 years) were from different regions of England. Just over half (52%) were married or in a civil partnership.
Measures
Measures comprised items that captured community identification, neighbour support, loneliness, and well‐being. Multiple items of the same variable were coded to ensure that higher scale scores indicated higher levels of the construct, and then were standardized before calculating averages (the selected items are included in Appendix S1).
Community Identification was measured using a single item (‘How strongly do you feel you belong to your immediate neighbourhood?’) rated from 1 (very strongly) to 4 (not at all strongly) scale.
Perceptions of social support were captured using three different items focusing on instrumental social support from neighbours (e.g., ‘If you were ill and at home on your own, and needed someone to collect a few shopping essentials, how comfortable would you feel asking a neighbour to do this for you?’). Participants rated their agreement from 1 (very strongly or definitely agree) to 4 (not at all strongly or definitely disagree).
Loneliness was measured using five items (e.g., ‘If I wanted company or to socialise, there are people I can call on’). Participants rated their agreement with the items on different scales that were standardized before averaging. Two items used a scale from 1 (definitely agree or often/always) to 4 (definitely disagree), other two items used a scale from 1 to 3 using different labels, and one item used a scale from 1 (often/always) to 5 (never).
Well‐being was measured with the 4‐item UK Office for National Statistics’ (2018) Personal Well‐being Scale. Participants rated each item (e.g., ‘Overall, how anxious did you feel yesterday?’) on a scale from 0 to 10, and responses were then recoded (to reflect positive well‐being) and averaged.
Results
Table 1 displays descriptive statistics and zero‐order correlations for all the variables. A saturated path model using maximum likelihood estimation with bootstrapped estimates using 5,000 resamples to obtain bias‐corrected confidence intervals around the indirect effect estimates (Preacher & Hayes, 2008) was conducted with Lavaan. The model was defined by the following paths: from community identification to perceived social support, loneliness, and well‐being; from perceived social support, to loneliness, and well‐being; and from loneliness to well‐being. As this was a saturated model (Figure 1), no fit indices are reported. To have a more conservative model, we controlled for the effect of background variables of age, gender, and marital status1. Age was included as continuous variable, while gender was included in the model as a dummy variable (1=male; 2=female) as was marital status which was coded with six dummy variables (married, cohabiting, single, separated, divorced, and widowed) with 1 indicating a response in each marital status category and 0 as the absence of this response. To avoid redundancy between groups, the category ‘others’ (without responses) was used as reference group (Cohen, Cohen, West, & Aiken, 2013).
Table 1.
Descriptive statistics, reliabilities, and correlational analyses for each of the Study 1 variables
| Min | Max | M | SD | Ske | Kur | α | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Community Id | −1.99 | 1.34 | .00 | 1.00 | −.32 | −.68 | − | |||||||||||||
| 2. Social Support | −1.72 | 1.21 | .00 | .85 | −.35 | −.97 | .81 | .50** | ||||||||||||
| 3. Loneliness | −1.17 | 4.47 | .00 | .69 | 1.40 | 2.41 | .71 | −.27** | −.27** | |||||||||||
| 4. Well−being | −3.28 | 1.17 | .00 | .79 | −.82 | .75 | .80 | .27** | .23** | −.49** | ||||||||||
| 5. Gender | 1 | 2 | – | – | – | – | − | .02 | −.01 | −.03* | .03* | |||||||||
| 6. Age | 16 | 95 | 51.19 | 18.27 | 0.00 | −0.92 | − | .19** | .27** | .00 | .09** | −.05** | ||||||||
| 7. Married | 0 | 1 | – | – | – | – | − | .12** | .17** | −.18** | .14** | −.08** | .19** | |||||||
| 8. Cohabiting | 0 | 1 | – | – | – | – | – | −.09** | −.09** | −.03* | −.01 | −.01 | −.20** | −.35** | ||||||
| 9. Single | 0 | 1 | – | – | – | – | – | −.11** | −.18** | .12** | −.12** | −.01 | −.43** | −.51** | −.17** | |||||
| 10. Separated | 0 | 1 | – | – | – | – | – | −.02 | −.04* | .06** | −.03 | .04* | .00 | −.15** | −.05** | −.07** | ||||
| 11. Divorced | 0 | 1 | – | – | – | – | – | −.02 | .01 | .08** | −.06** | .04* | .13** | −.31** | −.10** | −.14** | −.04** | |||
| 12. Widowed | 0 | 1 | – | – | – | – | – | .08** | .07** | .08** | .00 | .12** | .37** | −.30** | −.10** | −.14** | −.04** | −.09** |
N = 4314
Ske = skewness; Kurt = kurtosis; gender was coded as 1 = male and 2 = female; and each category of the civil status was coded as 1 = yes and 0 = no.
p < .01.
Figure 1.
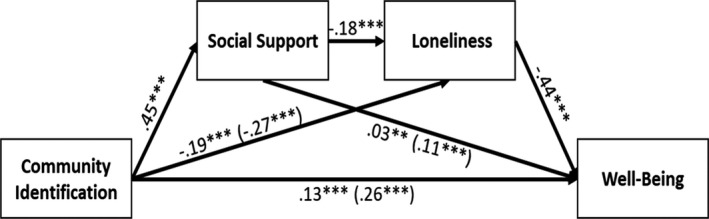
Study 1: Path model of the hypothesized model. Values are standardized. Paths from background variables (age, gender, and marital status) were not reported for purposes of clarity. Direct effects are reported with total effects that are reported in brackets. *p < .05; **p < .01; and ***p < .001.
After identifying significant correlations between these and the study variables, we added paths from each background variable to all the study variables. Results showed that community identification positively predicted perceived social support (b = 0.39, 95% CIs [0.36; 0.41], β = .45, p < .001), negatively predicted loneliness (b = −0.13, 95% CIs [− 0.16; −0.11], β = −.19, p < .001), and positively predicted well‐being (b = 0.10; 95% CIs [0.07; 0.13], β = .13, p < .001). Perceived social support negatively predicted loneliness (b = −0.15, 95% CIs [−0.18; −0.12], β = −.18, p < .001) and positively predicted well‐being (b = 0.03, 95% CIs [0.01; 0.06], β = .03, p = .044). Loneliness negatively predicted well‐being (b = −0.50, 95% CIs [−0.54; −0.46], β = −.44, p < .001).
The total effects from community identification to well‐being (b = 0.21, 95% CIs [0.18; 0.23], β = .26, p < .001), from community identification to loneliness (b = −0.19, 95% CIs [−0.21; ‐ 0.16], β = −.27, p < .001), and from perceived social support to well‐being (b = 0.11, 95% CIs [0.07; 0.14], β = .11, p < .001) were significant. There were also robust indirect effects from community identification to loneliness via perceived social support (b = −0.06, 95% CIs [−0.07; −0.04], β = −.08, p < .001), from community identification to well‐being via perceived social support and loneliness (b = 0.03, 95% CIs [0.02; 0.03], β = .04, p < .001), from community identification to well‐being via loneliness (b = 0.07, 95% CIs [0.056; 0.089], β = .08, p < .001), from perceived social support to well‐being via loneliness (b = 0.07, 95% CIs [0.06; 0.09], β = .08, p < .001), and from community identification to well‐being via perceived social support (b = 0.01, 95% CIs [0.01; 0.02], β = .02, p = .044).
To determine whether SES could moderate the strength of the associations between the study’s variables, a multi‐group analysis was conducted using participants within the top and bottom quartile for economic income as groups. The low‐SES group (lower quartile of personal income) comprised 848 respondents, while the high‐SES group (upper quartile of personal income) comprised 737 respondents. First, an unconstrained model (saturated model) with all paths allowed to vary across the two SES groups was tested and the path coefficients for each link in each subgroup are reported in Table 2. Then, a model with the path from Community Identification to Social Support constrained to be equal across the two groups was used as ‘baseline’ model. Furthermore, a series of constraining models were conducted with only one path (in addition to the path from Community Identification to Social Support) constrained to be equal across the SES groups and each constrained model was compared against the baseline model. Chi‐square difference tests between the baseline and constrained models were used to assess model equivalence across groups. Table 2 reveals that five models with one path constrained to be equal across the two groups were not significant. Compared to a baseline model with only the path from Community Identification to Social Support constrained to be equal across the SES groups and all the other paths allowed to vary across the two groups, the fit indices of the unconstrained models did not significantly differ from the baseline model, indicating structural equivalence across SES groups. The only model that showed significance (p = .047) was the model with the path from community identification to well‐being that was not significant for the high‐SES group but was significant for the low‐SES group.
Table 2.
Study 1:Multi‐group analysis
| Paths | Multi‐group Models | Chi‐square differences | Unconstrained model | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| χ2 | df | p | CFI | RMSEA [CI 90%] | SRMR | Δ χ2 | Δdf | p | Low‐SES group | High‐SES group | |||||
| b | p | β | b | p | β | ||||||||||
| Community Id → Social Support (Baseline Model) | 0.50 | 1 | .482 | 1.00 | .00 [.00, .08] | .006 | – | – | – | .43 | <.001 | .45 | .46 | <.001 | .48 |
| Community Id → Loneliness | 1.61 | 2 | .448 | 1.00 | .00 [.00, .07] | .008 | 1.11 | 1 | .292 | −.13 | <.001 | −.18 | −.09 | .007 | .12 |
| Social Support → Loneliness | 0.74 | 2 | .692 | 1.00 | .00 [.00, .05] | .006 | 0.24 | 1 | .624 | −.15 | <.001 | −.20 | −.13 | <.001 | −.18 |
| Community Id → Well‐being | 4.44 | 2 | .108 | .997 | .00 [.00, .09] | .012 | 3.95 | 1 | .047 | .13 | <.001 | .14 | .05 | .170 | .06 |
| Social Support → Well‐being | 0.51 | 2 | .775 | 1.00 | .00 [.00, .05] | .006 | 0.01 | 1 | .903 | .04 | .259 | .04 | .05 | .159 | .05 |
| Loneliness → Well‐being | 0.55 | 2 | .761 | 1.00 | .00 [.00, .05] | .006 | 0.05 | 1 | .821 | −.51 | <.001 | −.41 | −.53 | <.001 | −.46 |
Multi‐group Models describe the constrained models with the path reported in the first column to be equal across the two groups in addition to the path of the baseline model (in the first row). Coefficients in the unconstrained model (saturated model) describe the paths of low‐SES group and high‐SES group in a model with all the paths allowed to vary across the two SES groups.
Discussion
As hypothesized, participants’ strength of community identification (measured as neighbourhood belonging) was a significant positive predictor of well‐being: supporting previous research (e.g., Fong et al., 2019; Heath et al., 2017; McNamara et al., 2013; Stevenson et al., 2018). Moreover, we observed our predicted serial mediation model, which sheds light on the process through which community identification predicts well‐being: Strength of community identification was a positive predictor of perceived social support from neighbours, which was a negative predictor of loneliness, which itself was a negative predictor of well‐being.
Multi‐group analyses showed that the path from community identification to well‐being was not significant for the high‐SES group but was significant for the low‐SES group. However, overall testing of the invariance of the association between study variables showed that most of the associations between variables are equivalent across SES groups. Therefore, most of the associations between study variables are robust across SES, but the relationship between community identification and well‐being is completely explained by the mediating effects of higher support and reduced loneliness among the more affluent residents. This is in line with previous studies indicating that in economically disadvantaged communities, the effect of community identification on well‐being tends to occur directly rather than indirectly through social support (e.g., McNamara et al., 2013). Study 1 utilized a large random probability sample, illustrating the value of community identification on well‐being across different contexts. However, it does not allow understanding the unique characteristics of each context (e.g., deprivation levels) and is based on retrospectively analysed data not specifically collected to investigate Social Cure processes. Study 2 addresses these limitations. To replicate and extend Study 1 results, we selected geographical areas known to experience high levels of loneliness that differed in terms of neighbourhood deprivation.
STUDY 2A
Study 2a involved a bespoke community survey comprised of established and validated measures of each variable to provide a more rigorous test of the proposed serial mediation model. It was conducted in ‘Town 1’, a relatively affluent community in Nottinghamshire situated in the district of Broxtowe with an estimated population of 21,305 (Broxtowe Borough Council, 2012). Most of its constituent areas fall within the bottom 25% of deprived areas in England (Census, 2011). 49.4% of the population of Broxtowe is male, and 50.6% is female (Office for National Statistics, 2013). The area has a higher number of people over the age of 45 than the national average, with 18.35% of the population in Broxtowe aged 65 and above (Broxtowe Borough Council, 2014). Within Town 1, 20.09% of households consisted of single pensioners living alone. When consulting the Age UK ‘Risk of Loneliness in England’ map, the areas of Town 1 are considered to have a high to very high risk of loneliness at neighbourhood level for individuals aged 65 and above (Age UK, 2016a). As such, this community provided an ideal social group context within which to test our hypothesized model.
Method
Participants and data collection
Area‐specific postal invites were sent out to all households in Town 1 to participate in an online survey during May to August 2018. Respondents were required to be over 18 years and a resident of that area. Paper copies of the survey were available on request. A total of 452 participants (263 females, 180 males; Mage = 41.01, SD = 15.32, age range = 18–95 years) took part in the online survey which constitutes 2.1% of the total population. Most participants were from a White ethnic background (84.1%, n = 380). Most were engaged in some form of employment (66.1%, n = 299), were university educated (72.6%, n = 328), and lived in privately owned accommodation (60.4%, n = 271). 391 participants completed all the measures of the study and were used in subsequent analyses.
Measures
Measures comprised items that captured community identification, neighbour support, loneliness, and well‐being. Multiple items of the same variable were coded to ensure that higher scale scores indicated higher levels of the construct before calculating averages (the items are included in Appendix S1).
Community identification was measured with a 4‐item scale adapted from Cameron’s (2004) measure (and previously used by McNamara et al., 2013). Participants rated their agreement with each item (e.g., ‘I see myself as a member of my local community’) on a 1 (strongly disagree) to 5 (strongly agree) scale.
Social Support was measured by four items adapted from Haslam et al., (2005). Participants rated their perceptions of social support through agreement with each item (e.g., ‘Do you get the emotional support you need from other people in your local community?’) on a 1 (not at all) to 5 (completely) scale.
Loneliness was measured using the 8‐item UCLA scale of loneliness (ULS 8, Hays & DiMatteo, 1987). This has been found to capture the core experiential element of loneliness and, while it does not allow the consideration of sub‐components of loneliness, is succinct enough for use in surveys with the public. Participants rated their agreement with each item (e.g., ‘I lack companionship’) on a 1 (not at all) to 5 (completely) scale.
Personal well‐being was measured in the same way as in Study 1.
Results
Table 3 displays descriptive statistics and correlations for community identification, perceived social support, loneliness, and well‐being.
Table 3.
Study 2a: Descriptive statistics, reliabilities, and correlational analyses for each of the Study 2 variables
| Min | Max | M | SD | Ske | Kur | α | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Community Id | 1.00 | 5.00 | 3.26 | .83 | −.18 | .10 | .91 | ||||||||||
| 2. Social support | 1.00 | 5.00 | 2.55 | 1.03 | .10 | −.86 | .92 | .56** | |||||||||
| 3. Loneliness | 1.00 | 4.75 | 1.84 | .80 | 1.14 | .91 | .90 | −.33** | −.30** | ||||||||
| 4. Well‐being | 1.00 | 11.50 | 7.61 | 2.11 | −.65 | .16 | .82 | .34** | .27** | −.58** | |||||||
| 5. Gender | 1.00 | 2.00 | – | – | – | – | – | .19** | .16** | −.03 | .07 | ||||||
| 6. Age | 18.00 | 95.00 | 40.57 | 15.16 | .69 | −.45 | − | .16** | −.10* | −.10* | .19** | −.07 | |||||
| 7. Never married | .00 | 1.00 | – | – | – | – | – | −.09 | .03 | .15** | −.20** | −.03 | −.30** | ||||
| 8. Married | .00 | 1.00 | – | – | – | – | – | .19** | .05 | −.21** | .28** | .00 | .34** | −.49** | |||
| 9. Widowed | .00 | 1.00 | – | – | – | – | – | .06 | .04 | −.03 | .01 | −.02 | .13** | −.04 | −.06 | ||
| 10. Long term | .00 | 1.00 | – | – | – | – | – | −.13* | −.02 | .02 | −.12* | −.01 | −.28** | −.34** | −.45** | −.04 | |
| 11. Divorced | .00 | 1.00 | – | – | – | – | – | .01 | −.07 | .04 | .03 | .08 | .26** | −.16** | −.21** | −.02 | −.14** |
N = 391.
Ske = skewness; Kurt = kurtosis; gender was coded as 1 = male and 2 = female; and each category of the civil status was coded as 1 = yes and 0 = no.
p < .01.
Using the same approach as in Study 1, bootstrapping was conducted, and a saturated model achieved controlling for the effect of age, gender, and marital status2. Age was included as continuous variable, while gender and marital status were included in the model as dummy variables as in the previous study.
Results (Figure 2) confirmed that community identification positively predicted perceived social support (b = 0.72, 95% CIs [0.59; 0.83], β = .58, p < .001), negatively predicted loneliness (b = −0.19, 95% CIs [−0.31; −0.08], β = −.20, p = .001), but did not predict well‐being (b = 0.23; 95% CIs [−0.05; 0.53], β = .10, p = .101). Perceived social support negatively predicted loneliness (b = −0.14, 95% CIs [−0.23; −0.05], β = −.18, p = .002), but did not predict well‐being (b = 0.12, 95% CIs [−0.10; 0.31], β = .06, p = .254). Loneliness negatively predicted well‐being (b = −1.25, 95% CIs [−1.49; −1.00], β = −.50, p < .001).
Figure 2.
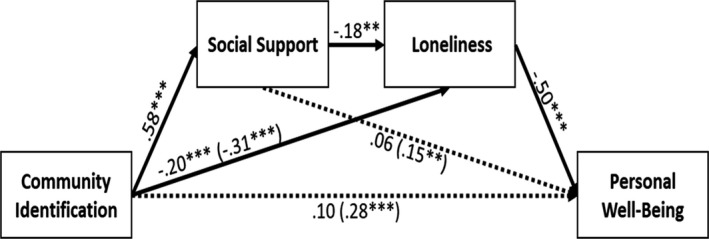
Study 2a: Path model of the model in Study 2a. Values are standardized. Paths from background variables (age, gender, and marital status) were not reported for purposes of clarity. The dotted line represents a non‐significant path. Direct effects are reported with total effects that are reported in brackets. *p < .05; **p < .01; and ***p < .001.
The total effects from community identification to well‐being (b = 0.68, 95% CIs [0.40; 0.96], β = .28, p < .001), from community identification to loneliness (b = −0.30, 95% CIs [−0.40; −0.19], β = −.31, p < .001), and from perceived social support to well‐being (b = 0.30, 95% CIs [0.07; 0.52], β = .15, p = .011) were significant. There were also significant indirect effects from community identification to loneliness via social support (b = −0.10, 95% CIs [−0.17; −0.04], β = −.11, p = .003), from community identification to well‐being via social support and loneliness (b = 0.13, 95% CIs [0.04; 0.23], β = .05, p = .006), from community identification to well‐being via loneliness (b = 0.24, 95% CIs [0.10; 0.40], β = .10, p = .001), and from social support to well‐being via loneliness (b = 0.03, 95% CIs [0.01; 0.04], β = .04, p = .002), while the indirect effect from community identification to well‐being via social support (b = 0.08, 95% CIs [−0.06; 0.23], β = .03, p = .257) was not significant.
Discussion
Study 2a findings partially replicate those from Study 1 in a high‐loneliness neighbourhood using custom‐designed measures. The total effect from community identification to well‐being was found to be significant, and this relationship was serially mediated by perceived social support and loneliness. Once more the pathway from social support to well‐being is weaker than the others (and this time there is no indirect effect of community identification on well‐being via social support), suggesting that in this context the well‐being benefits of social support are deriving largely from its loneliness‐reducing quality. These findings thus shed light on the social processes through which community identification predicts well‐being in a local community.
Promising as these findings are, Study 2a took place in a geographical area which, albeit contending with issues of loneliness, is relatively affluent. Research indicates that socio‐economic deprivation does impact on the level and range of available social support (Thompson et al., 2016) and on residents’ feelings of loneliness (Scharf & de Jong Gierveld, 2008). Study 2b was thus designed with the intention of examining our model in a socio‐economically disadvantaged neighbourhood.
STUDY 2B
In Study 2b, we distributed our custom‐developed survey to a second neighbourhood in Nottinghamshire also at high risk of loneliness for those over 65, but more socio‐economically disadvantaged than ‘Town 1’. ‘Town 2’ situated in a district of Mansfield, which has an estimated population of 4,439 (Mansfield District Council, 2008). Most of its constituent areas fall within the top 25% of deprived areas in England (Census, 2011). In Town 2, 48% of the population is male and 52% is female (Mansfield District Council, 2008). The average age of residents is 38, which is younger than the average for the district. 18.2% of the population is aged 65 years and above. 14.6% of households are comprised of pensioners living alone. When consulting the Age UK ‘Risk of Loneliness in England’ map, Town 2 is considered to have a high risk of loneliness at neighbourhood level for individuals aged 65 and above (Age UK, 2016b). These characteristics make it an ideal group context to test the hypothesized relationships.
Method
Participants and data collection
Data collection procedures and inclusion criteria were identical to those in Study 2a. Surveys were distributed to all addresses in the area during May to August 2018. A total of 167 participants (98 females, 66 males, 3 not reported; Mage = 45.36, SD = 15.94, age range = 18–88 years) took part in the online survey, which represents 3.8% of the local population. Most were from a White ethnic background (95%, n = 157), were engaged in some form of employment (66%, n = 109), were educated to college/school level (70%, n = 161), and lived in privately owned accommodation (77%, n = 127). 142 participants completed all the measures of the study and were used in subsequent analyses.
Measures
Measures used were identical to those in Study 2a.
Results
Descriptive statistics and correlations analyses for community identification, perceived social support, loneliness, and well‐being are displayed in Table 4.
Table 4.
Study 2b: Descriptive statistics, reliabilities, and correlational analyses for each of the Study 2b variables
| Min | Max | M | SD | Ske | Kur | α | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Community Id | 1.00 | 5.00 | 2.79 | .96 | −.11 | −.38 | .92 | ||||||||||
| 2. Social support | 1.00 | 5.00 | 2.04 | 1.10 | .83 | −.39 | .94 | .36** | |||||||||
| 3. Loneliness | 1.00 | 5.00 | 1.83 | .94 | 1.33 | 1.32 | .93 | −.34** | −.12 | ||||||||
| 4. Well‐being | .75 | 11.50 | 7.74 | 2.16 | −.15 | −.34 | .79 | .24** | .03 | −.49** | |||||||
| 5. Gender | 1.00 | 2.00 | – | – | – | – | – | .01 | .06 | −.06 | −.04 | ||||||
| 6. Age | 18.00 | 88.00 | 44.43 | 15.89 | .40 | −.83 | − | .02 | −.33** | −.09 | .11 | −.16 | |||||
| 7. Never married | .00 | 1.00 | – | – | – | – | – | −.05 | .16 | .28** | −.17* | −.14 | −.25** | ||||
| 8. Married | .00 | 1.00 | – | – | – | – | – | .17* | .01 | −.28** | .12 | .00 | .21* | −.39** | |||
| 9. Widowed | .00 | 1.00 | – | – | – | – | – | −.03 | −.07 | −.02 | −.06 | .11 | .36** | −.12 | −.27** | ||
| 10. Long term | .00 | 1.00 | – | – | – | – | – | −.09 | −.09 | .00 | .08 | .07 | −.26** | −.20* | −.45** | −.14 | |
| 11. Divorced | .00 | 1.00 | – | – | – | – | – | −.21* | −.11 | .25** | −.12 | .06 | .02 | −.10 | −.23** | −.07 | −.12 |
N = 142.
Ske = skewness; Kurt = kurtosis; gender was coded as 1 = male and 2 = female; and each category of the civil status was coded as 1 = yes and 0 = no.
p < .01.
A saturated model with bootstrapping was conducted, controlling for the background variables of age, gender, and marital status3. Gender and marital status were included in the model as dummy variables as in the previous study. The results (Figure 3) confirmed that community identification positively predicted perceived social support (b = 0.41, 95% CIs [0.20; 0.61], β = .36, p < .001), negatively predicted loneliness (b = −0.24, 95% CIs [−0.40; −0.08], β = −.25, p = .003), but did not predict well‐being (b = 0.24; 95% CIs [−0.15; 0.58], β = .12, p = .200). Perceived social support did not predict loneliness (b = −0.05, 95% CIs [−0.17; 0.07], β = −.06, p = .432) or well‐being (b = −0.04, 95% CIs [−0.41; .030], β = −.02, p = .810). Loneliness negatively predicted well‐being (b = −1.01, 95% CIs [−1.41; −0.62], β = −0.47, p < .001).
Figure 3.
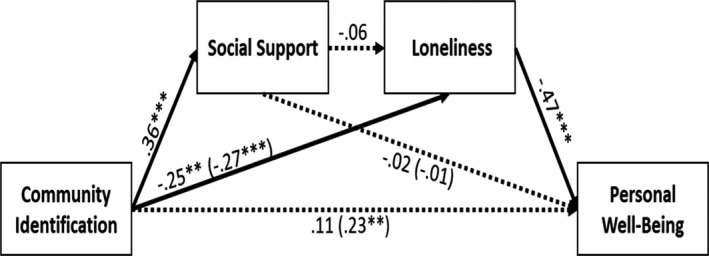
Study 2b: Path model of the model. Values are standardized. Paths from background variables (age, gender, and marital status) were not reported for purposes of clarity. The dotted line represents a non‐significant path. Direct effects are reported with total effects that are reported in brackets. *p < .05; **p < .01; and ***p < .001.
The total effect from community identification to well‐being (b = 0.49, 95% CIs [0.11; 0.82], β = .23, p = .007) and the total effect from community identification to loneliness (b = −0.26, 95% CIs [−0.41; −0.11], β = −.27, p = .001) were significant, while the total effect from social support to well‐being was not significant (b = 0.01, 95% CIs [−0.38; 0.38], β = .01, p = .970). There was also a significant indirect effect from community identification to well‐being via loneliness (b = 0.25, 95% CIs [0.07; 0.47], β = .12, p = .016). No significant indirect effects were found from community identification to loneliness via perceived social support (b = −0.02, 95% CIs [−0.08; 0.03], β = −.02, p = .465), from community identification to well‐being via perceived social support (b = −0.02, 95% CIs [−0.17; 0.13], β = −.01, p = .815), from perceived social support to well‐being via loneliness (b = 0.01, 95% CIs [−0.02; 0.04], β = .01, p = .441), or from community identification to well‐being via perceived social support and loneliness (b = 0.02, 95% CIs [−0.03; 0.08], β = .01, p = .451).
Discussion
Study 2b partially supported our earlier findings as the total effect of community identification on well‐being was significant. However, our serial mediation model was not fully supported: While community identification was a positive predictor of perceived social support, and loneliness was a negative predictor of well‐being, perceived social support did not predict loneliness (or well‐being). Nonetheless, community identification remained a negative predictor of loneliness (and through this, well‐being), which is consistent with our predictions.
While the weakness of the direct relationship between social support and well‐being was evident in the previous studies, the absence of a relationship between social support and loneliness in this community sample is worthy of note. As in Study 1, where the relationship between community identification and well‐being only occurs directly for the low‐SES group, here it would appear that the benefits of community identification in this low‐SES neighbourhood occur directly rather than indirectly via social support. This is again in line with research suggesting that the level and range of social support in low‐SES neighbourhoods provides less protection against loneliness and the effects of deprivation (Poortinga, 2012; Scharf & de Jong Gierveld, 2008; Thompson et al., 2016). However, we acknowledge the relatively small sample size in Study 2b and so differences could be due to the lower statistical power linked to the smaller sample.
GENERAL DISCUSSION
The past two decades have seen growing evidence of the fundamental impact of isolation and loneliness upon health but an absence of coherent theoretical frameworks to explain these effects. Our work brings the Social Identity Approach to Health to bear on the understanding of the potential benefits of community belonging in improving well‐being through both the provision of social support and the reduction of loneliness.
First, our studies contribute to the growing body of evidence pointing to the fundamental role played by community identity in the health and well‐being of residents. Community identification has previously been shown to predict residents’ well‐being and their resilience to social and economic change (Elahi et al., 2018; Fong et al., 2019; Heath et al., 2017; McNamara et al., 2013). Our work builds upon these findings to show that, across two contrasting communities and in a national sample, community identification positively predicts residents’ well‐being.
Second, our work highlights the central role that loneliness has in this relationship. In line with the bulk of research showing the fundamental importance of social relations for health (Holt‐Lunstad et al., ,,,2010, 2015), each of our three survey analyses evidences a significant and substantial negative relationship between loneliness and well‐being. Furthermore, our work situates these relationships within their community context showing that the positive relationship between community identification and well‐being occurs, in part, through reductions in loneliness. While recent research has shown the impact of community belonging in reducing loneliness and reducing health care usage (Kellezi et al., 2019), the current work is the first to provide direct evidence that community identification positively predicts residents’ well‐being via reductions in loneliness.
Next, our work provides evidence of how this process might operate. Our results suggest two pathways, with community identification directly and indirectly predicting lower loneliness. The first pathway is direct, whereby seeing oneself to be part of the local community is associated with lower levels of loneliness. In line with research attesting to the ability of social identification to lend meaning and purpose to peoples' lives (Haslam, Reicher, & Levine, 2012; Haslam et al., 2016), simply feeling as if one belongs within one’s locale predicts reductions in loneliness, independently of the level of support received from neighbours. This was evident in the Community Life Survey which employed a simple single item assessing residents’ feelings of belonging, as well as the community surveys where a more sophisticated assessment of social identification was used. From this, we assert that a sense of community belonging predicts lower levels of loneliness among residents.
A more complex pathway occurs through the receipt of social support from one’s neighbours. The Social Cure approach predicts that sharing a common identity with fellow group members does indeed unlock shared resources such that members are more likely to trust and support one another (Haslam et al., 2012; Jetten, Haslam, & Haslam, 2012). Indeed, this is what we found in the Community Life Survey with neighbourhood support predicting lower levels of loneliness and the negative relationship between community identification and loneliness being mediated, in part, by neighbourhood support. Similar processes were evident in Town 1, with the relationship between support and well‐being being fully explained through its loneliness‐reducing effect.
However, in Town 2, there was little evidence of the relationship between support and loneliness in this community context. While this departs somewhat from the results of Study 1 (which indicated that this relationship held across high‐ and low‐SES groups), it does accord with previous work suggesting that more deprived communities may have a narrower range of social support and that this may be less effective in protecting against loneliness (Bakouri & Staerklé, 2015; McNamara et al., 2013; Outten et al., 2009). However, the persistence of the direct relationship between community identification and well‐being through loneliness reduction does indicate that, even in this context, Social Cure processes persist. Overall then, our third assertion is that community identification can predict reduced loneliness and increased well‐being through unlocking neighbourly support, though this is potentially contingent upon the local community context.
Our findings do not allow us to unpack the reason for this difference between communities. We may speculate that the deprivation experienced in Town 2 means that the loneliness‐related needs of its residents exceed the support available from their neighbours. Alternatively, we might suggest that the type of social support available in Town 2 differs qualitatively from that of Town 1 and hence be less effective in reducing loneliness (Kearns et al., 2015; Scharf & de Jong Gierveld, 2008) or again that the deprivation of residents in Town 2 means that they are not able to reciprocate neighbourly support and hence are unable to avail of this support while retaining good relations with their fellow residents. Our present study does not allow us to adjudicate between these possible interpretations, and we suggest that future in‐depth qualitative work may well shed light on which has most explanatory value.
Moreover, there are further several limitations to the current research which qualify the strength of our assertions. First, the studies are all cross‐sectional in nature and so it is not possible to establish the causal order of the study variables. It is also plausible that people with higher levels of well‐being form connections easier, or that those who do not feel lonely are better capable of noticing support and developing a sense of belonging, which could indicate other possible directions in the observed relationships. Longitudinal research would provide more definitive evidence, as would the evaluation of loneliness reduction interventions which are designed to improve health by enhancing community identification.
Second, while the surveys combine breadth of scope (the England‐wide Community Life survey) with depth (the custom‐designed neighbourhood surveys), the work can only provide tentative explanations for the variations in findings. It is possible that the differences in measures employed between national and local surveys may have given rise to the differences in effects. Moreover, it is possible that Town 2 possesses a distinctive community history or set of local norms which impede effective sharing of social support. Additionally, our research assumes a relatively homogenous local community in each analysis and does not explore the challenges of community diversity and division which can shape community intragroup dynamics (Stevenson et al., 2019).
To resolve these issues, a custom‐designed multi‐level survey would be required to systematically study the effects of variations in neighbourhood size, affluence, and composition on the results found here. Further research could also explore what specific forms of social, emotional, and instrumental resource are available within communities and use specific measures of collective loneliness (Cacioppo, Grippo, London, Goossens, & Cacioppo, 2015) or neighbourhood‐related loneliness to track their effects (e.g., Chipuer, 2001). Furthermore, although the sample size of Study 2a and Study 2b was sufficient for the analysis following the general rules‐of‐thumb for sample size in SEM (Bentler & Chou, 1987), they represent self‐selecting samples. For this reason, participants who chose to respond may be different from the rest, and these populations may be subject to more bias than the larger multi‐regional population surveyed in Study 14. Future studies should try to confirm these findings and capture the specific nature of the community’s history and local norms as well as context‐specific challenges such as lack of basic local infrastructure and shared recreation facilities.
However, even adopting a more circumspect interpretation of the current findings, we point to two major implications of the work. Firstly, while loneliness interventions are often delivered at the neighbourhood level, they rarely focus on local community identification as a key outcome. Our work indicates that feelings of belonging to one’s neighbourhood constitute a potentially significant social psychological resource for residents. From this, we suggest that elements of interventions which can enhance community membership and which can overcome barriers to inclusion should help to enhance residents’ well‐being. Given the social impacts of COVID‐19, we see this as particularly important when considering how to preserve the mental health of community residents whose social interactions are restricted by the pandemic (Templeton et al., 2020).
Second, the results have some bearing for the understanding of the relationship between community deprivation and health. Geographical variations in community health are often difficult to understand (e.g., Catney, 2015) and are often attributed to unequal distribution of health care resources and services. Our results suggest that, while this may be the case, the ability of neighbours to support one another, especially in times of need, may also have benefits for community health. Local communities which lack basic local infrastructure to facilitate social interaction, shared recreation, and collaborative efforts are likely to negatively impact upon residents’ well‐being. In contrast, resourcing and facilitating community identification and peer support are pathways to providing a Social Cure for loneliness in community settings.
Conflict of interest
All authors declare no conflict of interest.
Supporting information
Appendix S1. Items included in Studies 1, 2a and 2b.
Acknowledgements
The research reported in this paper was partly funded by a grant from Nottinghamshire County Council.
Footnotes
The significant paths were not different between the tested model and the model without controlling for the demographic parameters.
In a model without controlling for the demographics parameters, the paths from community identification to well‐being were significant (b = 0.33, 95% CIs [0.06; 0.62], β = .13, p = .021), while after controlling for the demographics parameters, it was not significant.
The significant paths were not different between the tested model and the model without controlling for the demographic parameters.
A simple comparison of some demographics between participants of Study 1 against the participants of Study 2a and Study 2b revealed some differences in age, t(4827) = 11.62, p < .001, and gender e χ2(1) = 3.99, p = .046 such that there was a slightly higher percentage of females in Study 2a and Study 2b suggesting a possible risk for this bias.
Data availability statement
The data that support the findings of the first study in this paper are publicly available from the UK GOV 2018a, 2018b data archive: https://www.gov.uk/government/collections/community‐life‐survey#2014‐to‐2015‐survey. The data that support the findings of the second and third studies are available from the corresponding author upon reasonable request.
References
- Age UK (2016). Loneliness maps. Retrieved from http://data.ageuk.org.uk/loneliness‐maps/england‐2016/broxtowe/ [Google Scholar]
- Age UK (2016). Loneliness maps. Retrieved from http://data.ageuk.org.uk/loneliness‐maps/england‐2016/mansfield/ [Google Scholar]
- Bakouri, M. , & Staerklé, C. (2015). Coping with structural disadvantage: Overcoming negative effects of perceived barriers through bonding identities. British Journal of Social Psychology, 54, 648–670. 10.1111/bjso.12102 [DOI] [PubMed] [Google Scholar]
- Bangee, M. , Harris, R. A. , Bridges, N. , Rotenberg, K. J. , & Qualter, P. (2014). Loneliness and attention to social threat in young adults: Findings from an eye tracker study. Personality and Individual Differences, 63, 16–23. 10.1016/j.paid.2014.01.039 [DOI] [Google Scholar]
- Bangee, M. , & Qualter, P. (2018). Examining the visual processing patterns of lonely adults. Scandinavian Journal of Psychology, 59(4), 351–359. 10.1111/sjop.12436 [DOI] [PubMed] [Google Scholar]
- Bentler, P. M. , & Chou, C. (1987). Practical issues in structural modelling. Sociological Methods & Research, 16, 78–117. 10.1177/0049124187016001004 [DOI] [Google Scholar]
- Broxtowe Borough Council (2012). Profile of Broxtowe. Retrieved from https://www.broxtowe.gov.uk/media/1409/2_population_and_demographics.pdf [Google Scholar]
- Buckingham, S. A. , Frings, D. , & Albery, I. P. (2013). Group membership and social identity in addiction recovery. Psychology of Addictive Behaviors, 27, 1132–1140. 10.1037/a0032480 [DOI] [PubMed] [Google Scholar]
- Cacioppo, J. T. , & Hawkley, L. C. (2005). People thinking about people: The vicious cycle of being a social outcast in one’s own mind. In Williams K. D., Forgas J. P. & von Hippel W. (Eds.), The social outcast: Ostracism, social exclusion, rejection, and bullying (pp. 91–108). New York, NY: Psychology Press. [Google Scholar]
- Cacioppo, J. T. , & Hawkley, L. C. (2009). Perceived social isolation and cognition. Trends in Cognitive Sciences, 13, 447–454. 10.1016/j.tics.2009.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo, S. , Grippo, A. J. , London, S. , Goossens, L. , & Cacioppo, J. T. (2015). Loneliness: Clinical import and interventions. Perspectives on Psychological Science, 10, 238–249. 10.1177/1745691615570616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catney, C. (2015). Religious concentration and health outcomes in Northern Ireland. In Lloyd C. D., Shuttleworth I. G. & Wong D. W. (Eds.), Social‐spatial segregation: Concepts, processes and outcomes (pp. 335–362). Bristol, UK: Policy Press. [Google Scholar]
- Chipuer, H. (2001). Dyadic attachments and community connectedness: Links with youth's loneliness experiences. Journal of Community Psychology, 29, 429–446. 10.1002/jcop.1027 [DOI] [Google Scholar]
- Cohen, J. , Cohen, P. , West, S. G. , & Aiken, L. S. (2013). Applied multiple regression/correlation analysis for the behavioral sciences. New York, NY: Routledge. [Google Scholar]
- Coll‐Planas, L. , del Valle Gomez, G. , Bonilla, P. , Masat, T. , Puig, T. , & Monteserin, R. (2017). Promoting social capital to alleviate loneliness and improve health among older people in Spain. Health & Social Care in the Community, 25, 145–157. 10.1111/hsc.12284 [DOI] [PubMed] [Google Scholar]
- Cruwys, T. , Haslam, S. A. , Dingle, G. A. , Jetten, J. , Hornsey, M. J. , Chong, E. D. , & Oei, T. P. (2014). Feeling connected again: Interventions that increase social identification reduce depression symptoms in community and clinical settings. Journal of Affective Disorders, 159, 139–146. 10.1016/j.jad.2014.02.019 [DOI] [PubMed] [Google Scholar]
- Deutch, M. , & Collins, M. E. (1951). Interracial housing. New York, NY: Russell & Russell. [Google Scholar]
- Ehsan, A. , Klaas, H. S. , Bastianen, A. , & Spini, D. (2019). Social capital and health: A systematic review of systematic reviews. SSM‐population Health, 8, 100425. 10.1016/j.ssmph.2019.100425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elahi, A. , McIntyre, J. C. , Hampson, C. , Bodycote, H. J. , Sitko, K. , White, R. G. , & Bentall, R. P. (2018). Home is where you hang your hat: Host town identity, but not hometown identity, protects against mental health symptoms associated with financial stress. Journal of Social and Clinical Psychology, 37, 159–181. 10.1521/jscp.2018.37.3.159 [DOI] [Google Scholar]
- Farrell, S. J. , Aubry, T. , & Coulombe, D. (2004). Neighbourhoods and neighbours: Do they contribute to personal well‐being? Journal of Community Psychology, 32, 9–25. 10.1002/jcop.10082 [DOI] [Google Scholar]
- Festinger, L. , Schachter, S. , & Back, K. (1950). Social pressures in informal groups; a study of human factors in housing. Stanford, CA: Stanford University Press. [Google Scholar]
- Fong, P. , Cruwys, T. , Haslam, C. , & Haslam, S. A. (2019). Neighbourhood identification and mental health: How social identification moderates the relationship between socioeconomic disadvantage and health. Journal of Environmental Psychology, 61, 101–114. 10.1016/j.jenvp.2018.12.006 [DOI] [Google Scholar]
- Gallardo‐Peralta, L. P. , de Roda, A. B. L. , Angeles Molina‐Martinez, M. , & Schettini del Moral, R. (2018). Family and community support among older Chilean adults: the importance of heterogeneous social support sources for quality of life. Journal of Gerontological Social Work, 61, 584–604. 10.1080/01634372.2018.1489928 [DOI] [PubMed] [Google Scholar]
- Gleibs, I. H. , Haslam, C. , Haslam, S. A. , & Jones, J. M. (2011). Water clubs in residential care: Is it the water or the club that enhances health and well‐being? Psychology & Health, 26, 1361–1377. 10.1080/08870446.2010.529140 [DOI] [PubMed] [Google Scholar]
- GOV.UK (2018a). Government’s work on tackling loneliness. Retrieved from https://www.gov.uk/government/collections/governments‐work‐on‐tackling‐loneliness [Google Scholar]
- GOV.UK (2018b). £20 million investment to help tackle loneliness. Retrieved from https://www.gov.uk/government/news/20‐million‐investment‐to‐help‐tackle‐loneliness [Google Scholar]
- Haslam, C. , Cruwys, T. , Chang, M. X. , Bentley, S. V. , Haslam, S. A. , Dingle, G. A. , & Jetten, J. (2019). Groups 4 health reduces loneliness and social anxiety in adults with psychological distress: Findings from a randomised controlled trial. Journal of Consulting & Clinical Psychology, 87, 787–801. 10.1037/ccp0000427 [DOI] [PubMed] [Google Scholar]
- Haslam, C. , Cruwys, T. , Chang, M. X. , Eckley, B. , Buckingham, H. , & Channon, E. (2020). Community group membership protects the well‐being of adults experiencing socio‐economic disadvantage. Journal of Community & Applied Social Psychology, 30, 381–387. 10.1002/casp.2453 [DOI] [Google Scholar]
- Haslam, C. , Jetten, J. , Cruwys, T. , Dingle, G. A. , & Haslam, S. A. (2018). The new psychology of health: Unlocking the social cure. New York, NY: Routledge. [Google Scholar]
- Haslam, S. A. , O’Brien, A. , Jetten, J. , Vormedal, K. , & Penna, S. (2005). Taking the strain: Social identity, social support and the experience of stress. British Journal of Social Psychology, 44, 355–370. 10.1348/014466605X37468 [DOI] [PubMed] [Google Scholar]
- Haslam, S. A. , Reicher, S. D. , & Levine, M. (2012). When other people are heaven, when other people are hell: How social identity determines the nature and impact of social support. In Jetten J., Haslam C. & Haslam S. A. (Eds.), The social cure: Identity, health and well‐being (pp. 157–174). New York, NY: Psychology Press. [Google Scholar]
- Hawkley, L. C. , Browne, M. W. , & Cacioppo, J. T. (2005). How can I connect with thee? Let me count the ways. Psychological Science, 16, 798–804. 10.1111/j.14679280.2005.01617.x [DOI] [PubMed] [Google Scholar]
- Hays, R. D. , & DiMatteo, M. R. (1987). A short‐form measure of loneliness. Journal of Personality Assessment, 51, 69–81. 10.1207/s15327752jpa5101_6 [DOI] [PubMed] [Google Scholar]
- Heath, S. C. , Rabinovich, A. , & Barreto, M. (2017). Putting identity into the community: Exploring the social dynamics of urban regeneration. European Journal of Social Psychology, 47, 855–866. 10.1002/ejsp.2296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt‐Lunstad, J. , Smith, T. B. , Baker, M. , Harris, T. , & Stephenson, D. (2015). Loneliness and social isolation as risk factors for mortality: A meta‐analytic review. Perspectives on Psychological Science, 10, 227–237. 10.1177/17456916145683 [DOI] [PubMed] [Google Scholar]
- Holt‐Lunstad, J. , Smith, T. B. , & Layton, J. B. (2010). Social relationships and mortality risk: A meta‐analytic review. PLoS Medicine, 7, e1000316. 10.1371/journal.pmed.1000316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jetten, J. , Haslam, C. , & Haslam, S. A. (2012). The social cure: Identity, health and well‐being. New York, NY: Psychology Press. [Google Scholar]
- Jetten, J. , Haslam, C. , Haslam, S. A. , & Branscombe, N. R. (2009). The Social cure. Scientific American. Mind, 20(5), 26–33. 10.1038/scientificamericanmind0909-26 [DOI] [Google Scholar]
- Kearns, A. , Whitley, E. , Tannahill, C. , & Ellaway, A. (2015). Loneliness, social relations and health and well‐being in deprived communities. Psychology, Health & Medicine, 20, 332–344. 10.1080/13548506.2014.940354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kellezi, B. , & Reicher, S. (2012). Social cure or social curse? The psychological impact of extreme events during the Kosovo conflict. In Jetten I. J., Haslam C. & Haslam S. A. (Eds.), The social cure: Identity, health and well‐being (pp. 217–234).New York, NY: Psychology Press. [Google Scholar]
- Kellezi, B. , Wakefield, J. R. H. , Stevenson, C. , McNamara, N. , Mair, E. , Bowe, M. , … Halder, M. M. (2019). The social cure of social prescribing: a mixed‐methods study on the benefits of social connectedness on quality and effectiveness of care provision. British Medical Journal Open, 9(11), e033137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knowles, M. L. , Lucas, G. M. , Baumeister, R. F. , & Gardner, W. L. (2015). Choking under social pressure: Social monitoring among the lonely. Personality and Social Psychology Bulletin, 41, 805–821. 10.1177/0146167215580775 [DOI] [PubMed] [Google Scholar]
- Lim, M. H. , Rodebaugh, T. L. , Zyphur, M. J. , & Gleeson, J. F. (2016). Loneliness over time: The crucial role of social anxiety. Journal of Abnormal Psychology, 125, 620–630. 10.1037/abn0000162 [DOI] [PubMed] [Google Scholar]
- Mansfield District Council (2008). Neighbourhood profiles. Retrieved from http://www.mansfield.gov.uk/media/pdf/2/0/Mansfield_District_Neighbourhood_Profile.pdf [Google Scholar]
- McIntyre, J. C. , Wickham, S. , Barr, B. , & Bentall, R. P. (2018). Social identity and psychosis: Associations and psychological mechanisms. Schizophrenia Bulletin, 44, 681–690. 10.1093/schbul/sbx110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNamara, N. , Stevenson, C. , & Muldoon, O. T. (2013). Community identity as resource and context: A mixed method investigation of coping and collective action in a disadvantaged community. European Journal of Social Psychology, 43, 393–403. 10.1002/ejsp.1953 [DOI] [Google Scholar]
- Miller, K. , Wakefield, J. R. H. , & Sani, F. (2016). Greater number of group identifications is associated with healthier behaviour in adolescents. British Journal of Developmental Psychology, 34, 291–305. 10.1111/bjdp.12141 [DOI] [PubMed] [Google Scholar]
- Office for National Statistics (2018). Personal well‐being user guidance. Retrieved from https://www.ons.gov.uk/peoplepopulationandcommunity/wellbeing/methodologies/personalwellbeingsurveyuserguide [Google Scholar]
- Outten, H. R. , Schmitt, M. T. , Garcia, D. M. , & Branscombe, N. R. (2009). Coping options: Missing links between minority group identification and well‐being. Applied Psychology, 58, 146–170. 10.1111/j.1464-0597.2008.00386.x [DOI] [Google Scholar]
- Perkins, D. D. , & Long, D. A. (2002). Neighbourhood sense of community and social capital: A multi‐level analysis. In Fisher A. T., Sonn C. C. & Bishop B. J. (Eds.), Psychological sense of community: Research, applications, and implications (pp. 291–318). New York, NY: Springer. [Google Scholar]
- Poortinga, W. (2006). Social relations or social capital? Individual and community health effects of bonding social capital. Social Science & Medicine, 63, 255–270. 10.1016/j.socscimed.2005.11.039 [DOI] [PubMed] [Google Scholar]
- Poortinga, W. (2012). Community resilience and health: The role of bonding, bridging, and linking aspects of social capital. Health & Place, 18, 286–295. 10.1016/j.healthplace.2011.09.017 [DOI] [PubMed] [Google Scholar]
- Preacher, K. J. , & Hayes, A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879–891. 10.3758/BRM.40.3.879 [DOI] [PubMed] [Google Scholar]
- Pretty, G. , Bishop, B. , Fisher, A. , & Sonn, C. (2007). Psychological sense of community and its relevance to well‐being and everyday life in Australia. The Australian Community Psychologist, 19, 6–25. [Google Scholar]
- Prezza, M. , Amici, M. , Roberti, T. , & Tedeschi, G. (2001). Sense of community referred to the whole town: Its relations with neighbouring, loneliness, life satisfaction, and area of residence. Journal of Community Psychology, 29, 29–52.10.1002/1520‐6629(200101)29:1<29:AID‐JCOP3>3.0.CO;2‐C [Google Scholar]
- Putnam, R. D. (2000). Bowling alone: The collapse and revival of American community. New York, NY: Simon and Schuster. [Google Scholar]
- Qualter, P. , Rotenberg, K. , Barrett, L. , Henzi, P. , Barlow, A. , Stylianou, M. , & Harris, R. A. (2013). Investigating hypervigilance for social threat of lonely children. Journal of Abnormal Child Psychology, 41, 325–338. 10.1007/s10802-012-9676-x [DOI] [PubMed] [Google Scholar]
- Sarason, S. B. (1977). The psychological sense of community: Prospects for a community psychology. London, UK: Jossey‐Bass. [Google Scholar]
- Scharf, T. , & de Jong Gierveld, J. (2008). Loneliness in urban neighbourhoods: an Anglo‐Dutch comparison. European Journal of Ageing, 5, 103–115. 10.1007/s10433-008-0080-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevenson, C. , Costa, S. , Easterbrook, M. J. , McNamara, N. , & Kellezi, B. (2020). Social cure processes help lower intergroup anxiety among neighbourhood residents. Political Psychology, 41, 1093–1111. 10.1111/pops.12667 [DOI] [Google Scholar]
- Stevenson, C. , Easterbrook, M. , Harkin, L. , McNamara, N. , Kellezi, B. , & Shuttleworth, I. (2019). Neighbourhood identity helps residents cope with residential diversification: Contact in increasingly mixed neighbourhoods of Northern Ireland. Political Psychology, 40, 277–295. 10.1111/pops.12510 [DOI] [Google Scholar]
- Stevenson, C. , McNamara, N. , & Muldoon, O. (2014). Stigmatised identities and service usage in disadvantaged communities: Residents’, community workers’ and service providers’ perspectives. Journal of Community & Applied Social Psychology, 24, 453–466. 10.1002/casp.2184 [DOI] [Google Scholar]
- Templeton, A. , Guven, S. T. , Hoerst, C. , Vestergren, S. , Davidson, L. , Ballentyne, S. , … Choudhury, S. (2020). Inequalities and identity processes in crises: Recommendations for facilitating safe response to the COVID‐19 pandemic. The British Journal of Social Psychology, 59, 674–685. 10.1111/bjso.12400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson, T. , Rodebaugh, T. L. , Pérez, M. , Struthers, J. , Sefko, J. A. , Lian, M. , … Jeffe, D. B. (2016). Influence of neighborhood‐level factors on social support in early‐stage breast cancer patients and controls. Social Science & Medicine, 156, 55–63. 10.1016/j.socscimed.2016.03.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinson, T. (2004). Community adversity and resilience: The distribution of social disadvantage in Victoria and New South Wales and the mediating role of social cohesion. Richmond, Vic.: The Ignatius Centre for Social Policy & Research. [Google Scholar]
- Wakefield, J. R. H. , Sani, F. , Madhok, V. , Norbury, M. , Dugard, P. , Gabbanelli, C. , … Poggesi, F. (2017). The relationship between group identification and satisfaction with life in a cross‐cultural community sample. Journal of Happiness Studies, 18, 785–807. 10.1007/s10902-016-9735-z [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Items included in Studies 1, 2a and 2b.
Data Availability Statement
The data that support the findings of the first study in this paper are publicly available from the UK GOV 2018a, 2018b data archive: https://www.gov.uk/government/collections/community‐life‐survey#2014‐to‐2015‐survey. The data that support the findings of the second and third studies are available from the corresponding author upon reasonable request.


