Abstract
Clinical reasoning in general practice is increasingly challenging because of the rise in the number of patients with multimorbidity. This creates uncertainty because of unpredictable interactions between the symptoms from multiple medical problems and the patient's personality, psychosocial context and life history. Case analysis may then be more appropriately managed by systems thinking than by hypothetic‐deductive reasoning, the predominant paradigm in the current teaching of clinical reasoning. Application of “systems thinking” tools such as causal loop diagrams allows the patient's problems to be viewed holistically and facilitates understanding of the complex interactions. We will show how complexity levels can be graded in clinical reasoning and demonstrate where and how systems thinking can have added value by means of a case history.
Keywords: clinical reasoning, complexity‐informed, general practice, gut feelings, multimorbidity, uncertainty
1. BACKGROUND
Clinical reasoning is the key part of general practitioners' (GPs') work. It becomes increasingly challenging in an era in which more patients present with multimorbidity. In this context, GPs' clinical reasoning often results in the difficult awareness of uncertainty. 1
The idealistic view of clinical reasoning is of the GP, like Sherlock Holmes, carefully and patiently trying to find and arrange puzzle pieces. The GP, in time, reveals enough to formulate a diagnosis, or at least working hypotheses, and a management plan. 2 , 3 , 4 In general, the medical history is the most powerful diagnostic tool, leading to the majority of all regular diagnoses. 5 , 6 The patient presents with a complaint, and a diagnosis may be quickly formed on the basis of pattern recognition. If not, a list of hypotheses is formed compatible with the symptoms. These are then tested using additional information from further questions, clinical signs, clinical decision rules or indeed laboratory tests or imaging. This step‐by‐step, partly rational (i.e., generating hypotheses often automatically, checking them deductively) way of analysing is possible and often very satisfying when the case is not too difficult. 7 , 8 In such cases it offers the potential to reach a high level of diagnostic certainty in an explicit way.
This type of clinical reasoning still relies on a linear causality, from disease drivers to disease consequences. This clinical reasoning may be characterized as “simple”, when it results in identifying just one cause for the clinical problem, or as “complicated”, when more causal factors are identified, which are still linearly and synergistically or additively related to the symptoms.
The reality in general practice is that patients' presentations are often obscure, uncertain, and ill‐fitting with a model of linear causality. 1 , 9 First, GPs have to deal with a wide range of conditions that often co‐exist in individual patients. Annually GPs meet patients with about 400 rather common diseases with about 200 different symptoms. 10 However, there are lots of diseases GPs meet less frequently. 11 Additionally there are almost 8000 rare diseases, and only some of them GPs meet once in their career. 12 This limits the GP's experience with many disorders and their interactions. Even more important, as people age, most disease presentations develop simultaneously, but at different rates. With increasing age, disease phenotypes become more heterogeneous and different from the prototypical descriptions. 13 , 14 Moreover, these atypical disease presentations cause complex interactions, which greatly hinder GPs' ability to recognize the underlying diseases. For example, the interacting symptoms anxiety, cognitive decline, and cachexia in older persons are often related to heart failure or dementia, or both, though cachexia is classically directly related to cancer. 15
Secondly, the interactions between GP and patient also influence diagnostic reasoning. 16 The patients' fears and concerns, prior knowledge and thought processes all interact with their perception of how they feel, act and participate in the decision making with their GP.
The digital age means patients have access to more health information, and this can place higher demands on physicians.
Finally, clinical reasoning is influenced by the GPs' characteristics. These influences include an increasing workload, the often competing social and professional obligations, the fast‐growing volume of guidelines and evidence, and the organizational changes within their health service. The GPs' characteristics are an active part of the problem‐solving process, which will be influenced by their specific knowledge and experiences, ethical reasoning, emotions, and intuitive feelings. 16 , 17
2. UNDERSTANDING THE DIFFERENCE BETWEEN COMPLICATED AND COMPLEX
Overall, the clinical reasoning process can be characterized as simple, complicated, or complex. This depends on the type and number of factors present. (see Table 1).
TABLE 1.
Characteristics of simple, complicated, and complex modes of clinical reasoning
| Characteristic | Simple | Complicated | Complex |
|---|---|---|---|
| Causality | Single cause, linear | Multiple causes, linear | Multiple causes, cyclic, nonlinear |
| Certainty of diagnosis or treatment | High | Intermediate | Low |
| Importance of patient's history | Low | Low | High |
| Importance of patient's system | Low | Intermediate | High |
| No. of biopsychosocial scales (interactions) involved | Single scale | Single scale | Multiple scales |
| Prototypical examples | Ankle distortion, common cystitis | COPD exacerbation following pulmonary infection a complication of influenza; migraine caused by changes in work stress after moving to another city | Pneumonia and delirium in patient with Parkinson's disease, dysphagia, and COPD, and severe functional impairments, also in attention to eating |
| Complexity needed in clinical reasoning | Often pattern recognition, sometimes hypothetic‐deductive |
Sometimes pattern recognition, often hypothetic‐deductive |
Systems thinking |
Complicated diagnostic situations are characterized by multiple linear causal relationships (if A, then B, and thus next C). We can think about these analytically, limiting remaining uncertainty by acquiring more relevant information from history taking, or examinations.
In complex diagnostic situations the diagnostic process is influenced by more interacting elements and simple and complicated diagnostic models become inadequate. The complexity comes from components interacting with each other and/or forming feedback loops. 18 A more holistic model integrating systems thinking in clinical reasoning is needed. This also helps to understand and accept that the multiple elements act in a less certain way. 19
As we move to more complex patient problems, we increasingly recognize the importance of non‐analytical but integrative parts of clinical reasoning by pattern recognition and clinical intuition, which are both guided by experiential knowledge. Analytical and non‐analytical based reasoning can operate separately but are mostly intertwined in clinical practice. 7 , 17
To illustrate the complexity‐informed approach we will describe how to apply systems thinking to an exemplary diagnostic problem from primary care. We will discuss the benefits that understanding and using this approach can bring to clinical decision making, particularly in patients with multimorbidity. We show how it allows a better assessment of the patients' clinical problem, a better understanding of the patient‐doctor interactions that influences clinical reasoning and inevitably causes uncertainty of the emerging symptoms. Overall, the case will help to define the role of non‐analytical reasoning in primary care practice.
2.1. Case Marie Johnson
Mrs Marie Johnson is 61 and married, with three children. She works part‐time as a cleaner, and visits her GP quite frequently, whom she trusts, despite her health‐related anxiety. She has rheumatic polymyalgia and hypertension, and uses prednisolone, acethaminophen, a diuretic, a beta‐blocker, and has just started an ACE‐inhibitor. She called the practice late Friday afternoon with left shoulder pain and palpitations for 2 days.
Dr Harry May is 34 and a conscientious full‐time GP, with 6 years' experience. He finds it difficult to handle uncertainty and prefers to rationally reach a concrete diagnosis. He is facing personal difficulties due to a recent divorce. On more than one occasion with Mrs J, he has been unable to reach a diagnosis, despite repeated consultations. Consequently, he made a comment in her record ‐ wondering if she also had functional complaints. Additionally, he remembers his somewhat delayed diagnosis of her son's appendicitis.
Mrs Johnson entered Dr May's room and immediately said she was afraid she might be having a heart attack. She described a severe, continuous left‐sided shoulder pain giving her a stitch and making her feel sick. She had palpitations and felt anxious. It had made her think of her father who died suddenly when he was 65 years old. Or could it be a side‐effect of the recently started ACE‐inhibitor, she asked him.
Dr May felt a sense of frustration. He has had a busy, long day and felt tired, conscious of still needing to attend a home visit. He tried to recall diagnoses related to shoulder pain or referred pain. Several obvious diagnoses popped up in his mind such as musculoskeletal diseases but also some “red flag” presentations. He asked relevant questions and examined her thoroughly including an ECG but could rule out coronary artery disease based on a simple prediction rule. 20 He knew she had previously felt overworked which could be again the case. He failed to reassure Mrs. Johnson. She remained worried and repeated her symptoms, and for a moment he wondered how sure he was about his final conclusion. As he started to close the consultation, he became aware of an uneasy feeling. He was still uncertain: did all the symptoms sufficiently fit his conclusion? Did he really exclude all serious conditions as reason for her complaints? He never liked that uncertainty linked gut feeling, but had learned through experience to take it seriously, even when he was fed up.
He sat‐up and thought it all over. What had Mrs J. just mentioned? She had repeated her remark about pain in her left hip and calf a week ago, which he related to her arthrosis and polymyalgia. He reconsidered the list of relevant diagnoses, taking into account calf pain, palpitations, left shoulder‐pain, nausea, together with her repeated worries. Now, he tipped to another diagnostic hypothesis, a pulmonary embolism (PE). He examined her leg and carried out a D‐dimer point‐of‐care test, a biomarker for PE. It appeared a bit higher than normal, which added to his uncertainty. He carefully weighed up all arguments, checked the Wells prediction rule and concluded that a PE was still unlikely. 21 He felt reassured and tried to explain his way of reasoning and the conclusion, but Mrs Johnson remained in doubt. Finally, by mutual agreement, he referred her to the emergency department. Diagnostic imaging, however, did not show a PE. Perhaps her complaints were still related to her polymyalgia rheumatica. She was given further analgesia.
He then reflected on this clinical reasoning trip: did he resemble Sherlock Holmes? Perhaps at the PE decision point, but overall, it had not been a rational, straightforward analysis. In fact, his clinical uncertainty made his thinking a bit erratic. He felt satisfied that he had taken his gut feeling seriously, but on the other hand, he kept feeling unsatisfied that no clear cause was found and wondered what Mrs Johnson had made of it. It reminded him of an article about complexity recently published in a medical journal, which might better explain his clinical reasoning trip. 22
2.2. Complexity science and systems thinking
In complexity science, cases with multiple interacting agents are conceptualized as a complex dynamic and adaptive system. 23 , 24 The reasoning in complexity science is therefore called 'systems thinking'. Clinical cases with multimorbidity often resemble such complex systems and may then be best served with systems thinking. To operationalize systems thinking, the dynamic systems are often described and pictured as complex networks with multiple nodes and multiple causal connections (often called “edges”) in between the nodes. These edges reflect positive or negative interactions, sometimes resulting in feedback loops, and are often as at least as important as the nodes (problems) themselves. A small change in a node or edge (medical problem and interaction, resp.) can have a large and sometimes unexpected effect on the whole network (overall health), due to all connections. In contrast, a big change in another node or edge can have almost no effect on the whole system when these are sparsely connected with the rest, or when the system is able to adapt. The network of multiple nodes and their edges together results in a complex clinical presentation, which can be presented in a causal loop diagram. Similarly, the diagnostic reasoning of physicians with all interfering factors may be better understood in such a way.
2.3. Complexity science and clinical reasoning
There are lots of simple, linear relations between symptoms, signs, and diagnoses, for example, dysuria, a positive nitrite test and cystitis, or pain in throat, red and swollen tonsils and laryngitis. Heuristics or rules of thumb are shortcut diagnostic strategies, rely on deliberate but implicit knowledge, and show a linear relation by “if this condition then that response”. 25 , 26 In the case of laryngitis, the problem might become more complicated because of other linear relations between symptoms, signs and diagnoses such as in mononucleosis infectiosa. A forearm fracture of a child is a simple diagnosis managed by protocol, but it quickly becomes a complex diagnostic and management problem if there could be child abuse too. 27 GPs often act in the domain of patient problems in which several of the complexity characteristics are present (Table 1). 27 Indeed understanding these can help explain feelings of uncertainty or why no diagnostic label may be appropriate.
3. APPLYING COMPLEXITY SCIENCE/SYSTEMS THINKING TO THE CASE
3.1. Understanding Mrs J's case
The challenging case of Mrs J was complex in its diffuse presentation of symptoms and did not match a clear disease pattern. She had several issues, such as her current complaints (pain shoulder, palpitations), personality (anxiety about health, concerned about heart attack, talkative), family history (her father's sudden death at the same age), relation with GP (trusts him despite a medical error), medical history (muscle problems, high blood pressure, overworked, unexplained complaints), and medication (side effects of medicine just started?). These issues interacted to affect her presentation. (see Figure 1).
FIGURE 1.
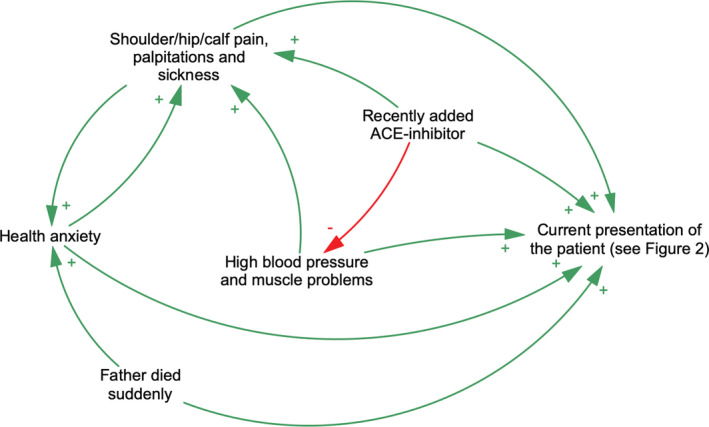
Causal loop diagram of a complexity‐informed approach of a clinical case presentation.Many different factors influence clinical case presentation. They are contributing (+, green) or counteracting (−, red), depending on the context
3.2. Understanding physician‐patient interactions
In the process of clinical reasoning, we can identify many GP and patient‐related process factors. All those factors tend to reinforce or weaken the GP's clinical reasoning and interact between themselves. (see Figure 2) This GP's personality (conscientious, committed to his patients, prefers rational reasoning) interacted with his uncertainty (difficult to deal with, age gap, medical error in the past). His personal circumstances (recently divorced) added to his workload (full‐time working, end of the day, end of the week). The GP's medical knowledge and expertise might still enable him to weigh up and give meaning to all signs and symptoms against the background of his contextual knowledge about the patient (multimorbidity with hypertension, polymyalgia rheumatica, polypharmacy; medical anxiety, frequent attender, trusts her GP, overworked in the past, recent added medication, sudden death of her father at a similar age). However, the presentation of the patient (talkative, concerned, cannot be reassured) made him consider if he was overlooking a serious diagnosis. So, Dr May's clinical reasoning also took into account the input of his patient.
FIGURE 2.
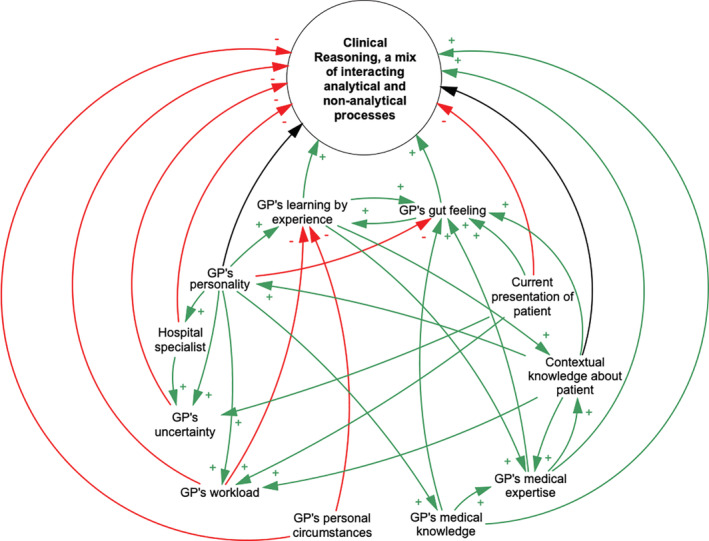
Causal loop diagram of a complexity‐informed approach of clinical reasoning.Many different factors influence clinical reasoning. They are contributing (+, green), counteracting (−, red) or both (black), depending on the context
Finally, his gut feeling (caused by an initial hidden cue: a casual remark about pain in a leg last week) changed the direction of his clinical reasoning process. It acted as an early warning signal for another potential diagnosis and triggered him to consider the diagnosis of PE. He rationally weighed all arguments and concluded that a PE is unlikely. His uncertainty decreased and he decided not to refer his patient. 28 However, his efforts to reassure his patient failed, and he agreed to her referral request. His reflection on the case, that is, learning by experience, created curiosity to find out more about complexity and diagnostic reasoning, and this might influence his diagnostic decision making in the future. 29
3.3. Understanding non‐analytical clinical reasoning processes
All the interacting factors are schematically organized together in a causal loop diagram. (see Figure 2). There are many interacting factors that influence this GP's clinical reasoning, in which he starts using both analytical and non‐analytical processes. Clinical intuition made him tip towards the PE‐hypothesis, before he could implement the new casual remark on pain in the calf in a more complex picture of this case. The unease with the uncertainty in his clinical reasoning process made him rely heavily on the non‐analytical clinical reasoning.
3.4. Assessing GP's clinical reasoning
The interaction we describe between Dr May and his patient Mrs Johnson demonstrates the complexity GPs frequently face, especially in the context of multimorbidity. Dr May's initial response to this was to minimize it and think in a linear way attributing Mrs J's symptoms to a myocardial infarction and after excluding this possibility ascribing them to her anxiety. We have discussed the factors that might have influenced this.
Later, Dr May's clinical reasoning moves to a more complexity informed approach. This includes accepting the predominance of interacting symptoms, uncertainty on the diagnosis and a certain degree of unpredictability of the outcome, all with a low likelihood of serious harm due to a lack of any (hemodynamic) sign of a serious disease. As often, uncertainty likely had a positive effect in this GP's diagnostic reasoning by initiating a reassessment of the medical problem. In general, it can trigger questions, such as “what's going on here”, which may result in the simulation of possible scenario's. 7 , 17 , 30 Ignoring a gut feeling is the denial of uncertainty rather than utilizing it as a realistic trigger for a diagnostic reassessment. 31 At the end of the complex consultation Dr May recognized his gut feeling and appropriately acted on this. The use of a clinic prediction rule (in this case the Wells score) was by his gut feeling as a step to rationalize and focus his diagnostic reasoning on a specific set of Mrs J's symptoms. Prediction rules are valuable checks because a simple prediction rule prioritizes focus on a sub‐part of the complex disease chain and may result in effective treatment options.
Had Dr May been more aware of systems thinking in the consultation, he could have applied this approach to the analytic aspect of his clinical decision making. A complexity‐informed approach from the start would have allowed for an explicit sharing of uncertainty, investigation of Mrs J's problems but would have also helped her and Dr May form a plan to go forward and manage her symptoms and health anxiety. Using Mrs J's case example this could take the following form: recognizing the previous difficult interactions between Mrs J and Dr May. Framing Mrs J's overall problem by acknowledging the multiple complex issues and concerns around her symptoms, such as the context of her father's heart condition, and sharing the clinician's impression that they may relate to her PMR and anxiety; then considering together, the investigation of some of the rarer but more serious issues, like PE; finally setting up a plan by suggesting they work together to map out Mrs J's broader issues, which could help her to manage her complaints and worries.
4. DISCUSSION
We can conclude that clinical reasoning in general practice is often a complex process, which may be related to multiple biopsychosocial patient related factors, physician related factors and health care organization related factors or all three. GPs are mostly trained well in linear diagnostic reasoning, aiming at differential diagnoses to elucidate the primary cause. However, they do not have a diagnostic system to elucidate clinical problems with multiple interacting causes.
The case illustrates that the patient's problem presentation and the GPs' clinical reasoning can be better seen as a complex diagnostic process, in which reality does not move in a straight line from A to B but follows a complex network path. It shows the need for sufficient awareness of the factors that can cause changes in diagnostic reasoning, and of the early warning gut feelings of uncertainty. Acknowledging uncertainty and gut feelings could improve clinical reasoning by thinking of other scenario's that might emerge. 7 , 17 Better insight in the complexity and the mechanisms of this diagnostic process may help in revaluing the early warning signals and determinants of clinical uncertainty. Metacognition, that is, stepping back from the immediate problem to examine and reflect on the thinking process, is considered an important effective cognitive debiasing strategy. 32 In fact, a complexity‐informed approach is a good application of a debiasing strategy, avoiding diagnostic errors.
This complexity‐informed approach of clinical reasoning may also improve medical education. 33 , 34 We advocate that medical students should learn to recognize simple, complicated, and complex cases and how to apply appropriate clinical reasoning in each. The differential diagnosis should be reserved for simple or complicated cases, while causal loop networks can help in understanding multimorbidity.
Furthermore, they have to be taught how to integrate evidence and intuition‐based assessments, different signs and symptoms with gut feelings as early warning signals. 35 , 36 Storytelling such as the case Marie Johnson focussed on the process of generating patient specific knowledge about nonlinear relations and creating time for reflection and feedback may be a first step to support students to cope with the case complexity. 34 This could be extended in a step by step teaching a complexity‐informed approach by other case histories up to clinical reasoning in supervised practice. Additionally, in such complex cases, selecting the most appropriate evidence such as a guideline or prediction rule can only take place after better understanding the patient's problem. 34 In this investigative process of getting more insight, clinical experience, intuition and thinking out loud the possible interactions and time courses play a vital role. Sometimes, a medical problem like Marie Johnson's case cannot be completely solved yet nevertheless “moved forward” by explicitly recognizing the diagnostic complexity multimorbidity creates. 34
In patients, particularly those with multimorbidity, using complexity science and systems thinking can aid understanding of the patient's presentation and the doctor's diagnostic reasoning. Embracing these tools when uncertainty emerges, may help the GP to come, see and conquer the complexity of his cases.
CONFLICT OF INTERESTS
The authors declare that they have no competing interests.
AUTHORS' CONTRIBUTIONS
Erik Stolper and Marcel Olde Rikkert closely collaborated in the writing process. Paul Van Royen, Edmund Jack and Jeroen Uleman critically followed the writing process with suggestions, comments and proposals for improvements. Jeroen Uleman designed the Figures 1 and 2 and changed them after suggestions made by the other authors. All authors read and approved the final manuscript.
ETHICS STATEMENT
Ethics and Consent to Participate: in the Netherlands, the national guidelines do not require ethical approval by an ethics committee, or a consent to participate, if no patients participate in the study.
Stolper E, Van Royen P, Jack E, Uleman J, Olde Rikkert M. Embracing complexity with systems thinking in general practitioners' clinical reasoning helps handling uncertainty. J Eval Clin Pract. 2021;27:1175–1181. 10.1111/jep.13549
DATA AVAILABILITY STATEMENT
Data sharing not applicable ‐ no new data generated
REFERENCES
- 1. Alam R, Cheraghi‐Sohi S, Panagioti M, Esmail A, Campbell S, Panagopoulou E. Managing diagnostic uncertainty in primary care: a systematic critical review. BMC Fam Pract. 2017;18(1):79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wilbush J. The Sherlock Holmes paradigm–detectives and diagnosis: discussion paper. J RSocMed. 1992;85(6):342‐345. [PMC free article] [PubMed] [Google Scholar]
- 3. Andre D, Fernand G. Sherlock Holmes ‐ an expert's view of expertise. Br J Psychol. 2008;99(1):109‐125. [DOI] [PubMed] [Google Scholar]
- 4. Oderwald AK, Sebus JH. The physician and Sherlock Holmes. J R Soc Med. 1991;84(3):151‐152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Peterson MC, Holbrook JH, Von Hales D, Smith NL, Staker LV. Contributions of the history, physical examination, and laboratory investigation in making medical diagnoses. West J Med. 1992;156(2):163‐165. [PMC free article] [PubMed] [Google Scholar]
- 6. Roshan M, Rao AP. A study on relative contributions of the history, physical examination and investigations in making medical diagnosis. J Assoc Physicians India. 2000;48(8):771‐775. [PubMed] [Google Scholar]
- 7. Norman G, Barraclough K, Dolovich L, Price D. Iterative diagnosis. BMJ. 2009;339:b3490. [DOI] [PubMed] [Google Scholar]
- 8. Norman G, Young M, Brooks L. Non‐analytical models of clinical reasoning: the role of experience. Med Educ. 2007;41(12):1140‐1145. [DOI] [PubMed] [Google Scholar]
- 9. Dinant GJ. Diagnosis and decision. Undifferentiated illness and uncertainty in diagnosis and management. Jones R, Britten N, Gulpepper L, Et al. Oxford Textbook of Primary Medical Care. Oxford: Oxford University Press; 2004. [Google Scholar]
- 10. Okkes IM, Oskam SK, Lamberts H. From Complaint to Diagnosis [Van klacht naar diagnose]. Bussum: Uitg.Coutinho; 1998. [Google Scholar]
- 11. Buntinx F, Mant D, Van den Bruel A, Donner‐Banzhof N, Dinant GJ. Dealing with low‐incidence serious diseases in general practice. Br J Gen Pract. 2011;61(582):43‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rath A, Nguengang Wakap S. Orphanet Report Series, Rare diseases collection. Prevalence and Incidence of Rare Diseases: Bibliographic data. Paris: Orphanet; 2016. [Google Scholar]
- 13. Hani MA, Keller H, Vandenesch J, Sonnichsen AC, Griffiths F, Donner‐Banzhoff N. Different from what the textbooks say: how GPs diagnose coronary heart disease. Fam Pract. 2007;24(6):622‐627. [DOI] [PubMed] [Google Scholar]
- 14. Biesemans L, Cleef LE, Willemsen RTA, et al. Managing chest pain patients in general practice: an interview‐based study. BMC Fam Pract. 2018;19(1):80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Renzi C, Kaushal A, Emery J, et al. Comorbid chronic diseases and cancer diagnosis: disease‐specific effects and underlying mechanisms. Nat Rev Clin Oncol. 2019;16:746‐761. [DOI] [PubMed] [Google Scholar]
- 16. Donner‐Banzhoff N. Solving the diagnostic challenge: a patient‐centered approach. Ann Fam Med. 2018;16(4):353‐358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Stolper CF, Van de Wiel MWJ, Van Royen P, Van Bokhoven MA, Van der Weijden T, Dinant GJ. Gut feelings as a third track in general practitioners' diagnostic reasoning. J Gen Intern Med. 2011;26(2):197‐203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rickles D, Hawe P, Shiell A. A simple guide to chaos and complexity. J EpidemiolCommunity Health. 2007;61(11):933‐937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wilson T, Holt T, Greenhalgh T. Complexity science: complexity and clinical care. BMJ. 2001;323(7314):685‐688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bosner S, Haasenritter J, Becker A, et al. Ruling out coronary artery disease in primary care: development and validation of a simple prediction rule. CMAJ. 2010;182(12):1295‐1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hendriksen JM, Lucassen WA, Erkens PM, et al. Ruling out pulmonary embolism in primary care: comparison of the diagnostic performance of "gestalt" and the Wells rule. Ann Fam Med. 2016;14(3):227‐234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Greenhalgh T, Papoutsi C. Studying complexity in health services research: desperately seeking an overdue paradigm shift. BMC Med. 2018;16(1):95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Naaldenberg J, Aarts N. The compatibility of reductionistic and complexity approaches in a sociomedical innovation perspective. BMJ Glob Health. 2020;5(12):e003858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jack E, Maskrey N, Byng R. SHERPA: a new model for clinical decision making in patients with multimorbidity. Lancet. 2018;392(10156):1397‐1399. [DOI] [PubMed] [Google Scholar]
- 25. Gigerenzer G, Todd PM. Simple Heuristics that Makes us Smart. New York: Oxford University Press; 1999. [Google Scholar]
- 26. Andre M, Borgquist L, Foldevi M, Molstad S. Asking for 'rules of thumb': a way to discover tacit knowledge in general practice. FamPract. 2002;19(6):617‐622. [DOI] [PubMed] [Google Scholar]
- 27. Gray B. The Cynefin framework: applying an understanding of complexity to medicine. J Prim Health Care. 2017;9(4):258‐261. [DOI] [PubMed] [Google Scholar]
- 28. Pauker SG, Kassirer JP. The threshold approach to clinical decision making. NEnglJMed. 1980;302(20):1109‐1117. [DOI] [PubMed] [Google Scholar]
- 29. Van de Wiel MWJ, Van den Bossche P, Janssen S, Jossberger H. Exploring deliberate practice in medicine: how do physicians learn in the workplace? Adv Health Sci Educ Theory Pract. 2011;16(1):81‐95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Stolper CF, Van Royen P, Van Bokhoven MA, et al. Consensus on gut feelings in general practice. BMC Fam Pract. 2009;10:66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kay J, King M. Radical Uncertainty. Decision‐making beyond the numbers: Bridge Street Press; 2020. [Google Scholar]
- 32. Croskerry P. The importance of cognitive errors in diagnosis and strategies to minimize them. AcadMed. 2003;78(8):775‐780. [DOI] [PubMed] [Google Scholar]
- 33. Cristancho S, Field E, Lingard L. What is the state of complexity science in medical education research? Med Educ. 2019;53(1):95‐104. [DOI] [PubMed] [Google Scholar]
- 34. Fraser SW, Greenhalgh T. Coping with complexity: educating for capability. BMJ. 2001;323(7316):799‐803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Van Puymbroeck H, Remmen R, Denekens J, Scherpbier A, Bisoffi Z, Van den Ende J. Teaching problem solving and decision making in undergraduate medical education: an instructional strategy. MedTeach. 2003;25(5):547‐550. [DOI] [PubMed] [Google Scholar]
- 36. Van den Ende J, Bisoffi Z, Van Puymbroek H, et al. Bridging the gap between clinical practice and diagnostic clinical epidemiology: pilot experiences with a didactic model based on a logarithmic scale. J EvalClinPract. 2007;13(3):374‐380. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable ‐ no new data generated


