The translation of discovery into daily clinical practice has proved frustratingly slow and inconsistent across the field of medicine (1). One hypothesis for the slow adoption of new evidence in the intensive care unit (ICU) is that traditional dissemination and implementation strategies have failed to adequately consider the complexity of this environment and the interprofessional teamwork required to deliver high-quality critical care (2). Mechanical ventilation is just one of many common ICU interventions that requires communication and coordination between many interprofessional team members, and the gap between best evidence and delivery of this procedure is well documented (3).
In this issue of ATS Scholar, Rak and colleagues describe a qualitative exploration of interprofessional education and its potential role in ICU implementation efforts (4). In a series of semistructured individual and focus group interviews, the authors solicited opinions regarding interprofessional ICU team dynamics, education delivery preferences, and knowledge, attitudes, and practices surrounding the use of preventive postextubation noninvasive ventilation (NIV). Participants included nurses, respiratory therapists, and physicians from both community and large academic hospitals within a single integrated health system. The authors selected postextubation NIV because this practice requires the input and coordination of multiple interprofessional ICU team members, has been clearly shown to improve outcomes in patients at high risk of respiratory failure, and is recommended by current guidelines but is rarely used despite evidence of its efficacy. The investigators collected and analyzed the data using thematic content analysis.
This was a well-conducted study that adds significant information to the robust but complex body of existing literature relevant to interprofessional education in the ICU (5–9). The authors characterize a number of key themes that emerged as barriers to implementation and practice improvement, including incomplete understanding of interprofessional roles and responsibilities, culture and practice bias, a team-based hierarchy that favored physician decision-making in the absence of NIV protocols, and challenges aligning complex team-based interactions into a shared mental model. It is interesting to note that interprofessional power dynamics extended into implementation practice, with nurses and respiratory therapists describing a “top down” approach to new policies and procedures while physicians spoke to diffusion via peer partnerships. Participants clearly preferred case-based, just-in-time, interprofessional and interactive learning opportunities and acknowledged that the unpredictable nature of ICU practice challenged their ability to dedicate time and attention to formal, classroom-based education.
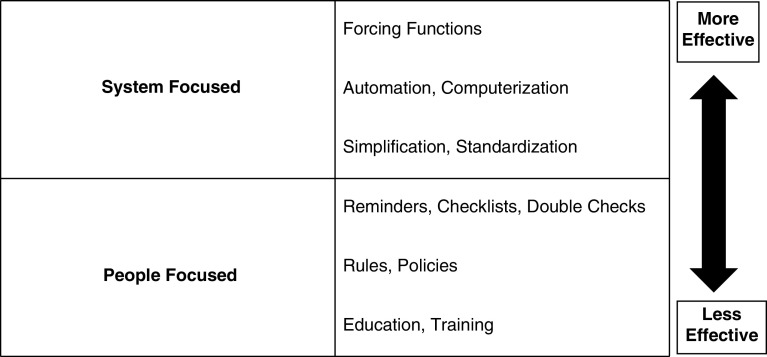
The authors conclude that interprofessional education offers promise to address the important barriers to the use of preventive postextubation NIV. Although we agree with this statement, we would like to highlight and expand on several important considerations that they raise. This study clearly demonstrates the “elephant in the ICU”—our practice environment remains riddled with complex sources of process variation that lead to inconsistent application of best practices and risks the quality of care we deliver. Much to the chagrin of us medical educators, the classic Hierarchy of Intervention Effectiveness—an often-referenced theory in human factors engineering—ranks education and training as the least effective strategy to change this system (Figure 1), and education interventions alone have been predictably poor at changing clinician behavior (10). A discussion of the challenges of organizational culture change is beyond the scope of this editorial, but overcoming practice bias clearly is not easy. Adapting the well-known quote popularized by Ford Motor Co. CEO Mark Fields, “culture eats strategy [and education] for breakfast.” We should not oversell and oversimplify the idea that interprofessional education alone will serve as an effective solution for even the focused problem of postextubation NIV use.
Figure 1.
Hierarchy of intervention effectiveness. Education is the least effective change management strategy in this well-recognized human factors engineering theory and is best used in multifaceted interventions that address both human and system factors.
The way forward to solve these complex problems will require close collaboration between educators and experts in quality improvement, dissemination, and implementation science to develop multifaceted interventions that address both human and system factors (11). Academic medical systems have been primed by the Joint Commission, national quality initiatives, and the Accreditation Council of Graduate Medical Education to forge solutions to the quality gaps that persist in our healthcare systems (12). We also have published implementation frameworks to inform this work and to strengthen the critical care community’s extensive experience developing successful interprofessional processes of care within their practice environment (2, 13).
It is also reasonable to hypothesize that seasoned educators, leveraging elements of adult learning theory, may be able to increase the impact of education within these interventions. The rapid growth of virtual learning platforms during the coronavirus disease (COVID-19) pandemic offers exciting opportunities for flexible, convenient, asynchronous, and collaborative learning regardless of competing clinical demands and schedules. These tools also offer significant promise for bite-sized delivery of curriculum content, reinforcement using spacing and testing effect, and integration with just-in-time simulation for teamwork and procedural skills (14).
Finally, the results of this study remind us that implementation initiatives must be done in partnership with the complex systems and teams that they serve. Interprofessional ICU teams are communities of practice and form the building blocks of a social learning system (15). They are bound together by their collective understanding of purpose; their interactions are governed by a mutual understanding of individual roles, relationships, and a common sense of trust. Communities of practice also share common resources, including daily workflows, protocol-based care pathways, and process and outcomes data, to inform intervention reach and effectiveness. Together, these elements create an ICU team’s socially defined competence, and team member interactions within this collective practice constantly generate new learning. Change management and implementation initiatives must foster and support these communities to transform the learning healthcare system, and when possible, power differentials must be minimized to support open and collaborative innovation. We need the help and support of every member of our interprofessional team to move the “elephant” out of the ICU.
Footnotes
Author Contributions: P.J.G.: manuscript preparation. Y.D. and A.S.N.: manuscript review and revision.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1. Lenfant C. Shattuck lecture. Clinical research to clinical practice: lost in translation? N Engl J Med. 2003;349:868–874. doi: 10.1056/NEJMsa035507. [DOI] [PubMed] [Google Scholar]
- 2. Weled BJ, Adzhigirey LA, Hodgman TM, Brilli RJ, Spevetz A, Kline AM, et al. Task Force on Models for Critical Care. Critical care delivery: the importance of process of care and ICU structure to improved outcomes: an update from the American College of Critical Care Medicine Task Force on Models of Critical Care. Crit Care Med. 2015;43:1520–1525. doi: 10.1097/CCM.0000000000000978. [DOI] [PubMed] [Google Scholar]
- 3. Weiss CH, Baker DW, Tulas K, Weiner S, Bechel M, Rademaker A, et al. A critical care clinician survey comparing attitudes and perceived barriers to low tidal volume ventilation with actual practice. Ann Am Thorac Soc. 2017;14:1682–1689. doi: 10.1513/AnnalsATS.201612-973OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rak KJ, Kahn JM, Linstrum K, Caplan EA, et al. Enhancing implementation of complex critical care interventions through interprofessional education.2021;2:370–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Donovan AL, Aldrich JM, Gross AK, Barchas DM, Thornton KC, Schell-Chaple HM, et al. University of California, San Francisco Critical Care Innovations Group. Interprofessional care and teamwork in the ICU. Crit Care Med. 2018;46:980–990. doi: 10.1097/CCM.0000000000003067. [DOI] [PubMed] [Google Scholar]
- 6. Ervin JN, Kahn JM, Cohen TR, Weingart LR. Teamwork in the intensive care unit. Am Psychol. 2018;73:468–477. doi: 10.1037/amp0000247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dietz AS, Pronovost PJ, Mendez-Tellez PA, Wyskiel R, Marsteller JA, Thompson DA, et al. A systematic review of teamwork in the intensive care unit: what do we know about teamwork, team tasks, and improvement strategies? J Crit Care. 2014;29:908–914. doi: 10.1016/j.jcrc.2014.05.025. [DOI] [PubMed] [Google Scholar]
- 8. Reeves S, Goldman J, Gilbert J, Tepper J, Silver I, Suter E, et al. A scoping review to improve conceptual clarity of interprofessional interventions. J Interprof Care. 2011;25:167–174. doi: 10.3109/13561820.2010.529960. [DOI] [PubMed] [Google Scholar]
- 9. van Diggele C, Roberts C, Burgess A, Mellis C. Interprofessional education: tips for design and implementation. BMC Med Educ. 2020;20:455. doi: 10.1186/s12909-020-02286-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cafazzo JA, St-Cyr O. From discovery to design: the evolution of human factors in healthcare. Healthc Q. 2012;15:24–29. doi: 10.12927/hcq.2012.22845. [DOI] [PubMed] [Google Scholar]
- 11. Niven AS, Herasevich S, Pickering BW, Gajic O. The future of critical care lies in quality improvement and education. Ann Am Thorac Soc. 2019;16:649–656. doi: 10.1513/AnnalsATS.201812-847IP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Nasca TJ. Introduction to the CLER National Report of Findings 2016. J Grad Med Educ. 2016;8(2 Suppl 1):7–9. doi: 10.4300/1949-8349.8.2s1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10:21. doi: 10.1186/s13012-015-0209-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Manning KD, Spicer JO, Golub L, Akbashev M, Klein R. The micro revolution: effect of Bite-Sized Teaching (BST) on learner engagement and learning in postgraduate medical education. BMC Med Educ. 2021;21:69. doi: 10.1186/s12909-021-02496-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wenger E. Communities of practice and social learning systems. Organization. 2000;7:225–246. [Google Scholar]