Abstract
Background
Laparoscopic cholecystectomy is one of the most performed surgeries worldwide but its learning curve is still unclear.
Methods
A systematic review was conducted according to the 2009 Preferred Reporting Items for Systematic Reviews and Meta‐analyses guidelines. Two independent reviewers searched the literature in a systematic manner through online databases, including Medline, Scopus, Embase, and Google Scholar. Human studies investigating the learning curve of laparoscopic cholecystectomy were included. The Newcastle–Ottawa scale for cohort studies and the GRADE scale were used for the quality assessment of the selected articles.
Results
Nine cohort studies published between 1991 and 2020 were included. All studies showed a great heterogeneity among the considered variables. Seven articles (77.7%) assessed intraoperative variables only, without considering patient's characteristics, operator's experience, and grade of gallbladder inflammation. Only five articles (55%) provided a precise cut‐off value to see proficiency in the learning curve, ranging from 13 to 200 laparoscopic cholecystectomies.
Conclusions
The lack of clear guidelines when evaluating the learning curve in surgery, probably contributed to the divergent data and heterogeneous results among the studies. The development of guidelines for the investigation and reporting of a surgical learning curve would be helpful to obtain more objective and reliable data especially for common operation such as laparoscopic cholecystectomy.
Keywords: education, laparoscopic cholecystectomy, laparoscopy, learning curve, training
(1) Laparoscopic cholecystectomy is one of the most performed surgeries worldwide but its learning curve is still unclear. (2) A systematic review was conducted according to the 2009 Preferred Reporting Items for Systematic Reviews and Meta‐analyses guidelines. (3)The lack of clear guidelines when evaluating learning curve in surgery, probably contributed to the divergent data and heterogeneous results among the studies.
Introduction
An “inexperienced clinician” is defined as a physician at the initial stage of his learning curve with an expectation of improvement as his clinical experience increases. 1 The concept of learning curve was introduced by T.P. Wright in 1936, according to the theory to which the efficiency of a component of a plane went up as the worker's experience and skill increase. 2 Subsequently, the concept of the learning curve was applied in the field of industrial manufacturing and software development. 3 In 1980, the learning curve was introduced in medicine and recognized as a parameter to assess professional responsibility. Recently, the concept of the learning curve evolved from a purely theoretical framework to a parameter upon which evaluating clinical outcomes such as mortality and morbidity. 2 Learning curve can be used in surgery to evaluate the surgeon's skill and performance as the experience increases and can be useful to plan adequate training programs. 1 Nowadays, a well‐designed learning curve process is considered essential for the acquisition of surgical skills, but different factors could influence the learning process and should be taken into account.
Laparoscopic cholecystectomy is one of the most performed surgeries worldwide 4 representing one of the first operations performed by young surgeons during their training. 5 However, there is no definite guideline on how to measure the learning curve of this specific surgical intervention and literature is conflicting on the minimum number of procedures to perform to achieve proficiency and ensure a safe laparoscopic cholecystectomy. 3 The present systematic review aims to analyze the available literature about the learning curve of laparoscopic cholecystectomy. To our knowledge, there is no existing review on the topic performed with a systematic approach.
Materials and methods
A systematic review was performed based on the Cochrane collaboration‐specific protocol 6 and was reported according to the Preferred Reporting Items for Systematic Reviews and Meta‐analyses (PRISMA) statement checklist.
Studies that investigated the learning curve associated with laparoscopic cholecystectomy were searched in the following databases without date restrictions: Medline (through PubMed), Scopus, Embase, Cochrane Register, and Google Scholar.
A specific research equation was used for each database, using the following keywords and Mesh Terms: learning curve, cholecystectomy, laparoscopic cholecystectomy, education, training, residency.
According to the PICOS schema, the following criteria were used to formulate the research question and to search the literature:
Population: Surgeons and residents who performed laparoscopic cholecystectomy.
Intervention: Analysis of the learning curve associated with laparoscopic cholecystectomy in both emergency and elective settings.
Comparisons: No comparison or learning curve for cholecystectomy performed with techniques other than laparoscopy.
Outcome(s): Learning curve was defined as the numbers of surgeries needed to see proficiency based on operative time decrease, number of intraoperative, and postoperative complications, conversion rate reduction, postoperative stay, and mortality rate decrease.
Study designs: Observational studies (cohort and case–control), case series, and interventional studies (randomized and non‐randomized controlled trials).
The literature review was completed by an extensive search using the “related articles” function in PubMed. Results were limited to human studies, with review articles and case report being excluded. The reference lists of the eligible records and of pertinent review articles were double‐checked to identify potential additional articles. Articles were selected and reviewed if written in English only.
Literature search and selection were performed independently and blindly by two reviewers (ER and ES). Records were removed from the selection if both reviewers exclude the articles at the title/abstract screening levels. Disagreements were resolved with a discussion with a third reviewer (GLG).
Data extraction
Both reviewers performed an independent full‐text analysis and data extraction by filling in an electronic database. Extracted data include first author name, year of publication, journal, study design, study period, gallbladder pathology, number of surgeries performed during the study period by surgeons and residents, number of procedure in elective and emergency settings, intraoperative complications, conversion rate, operative time, and expected learning curve.
Study quality assessment and risk of bias
Two reviewers (ER and ES) carried out the study quality assessment and risk of bias evaluation of the selected articles. According to the study design, the Newcastle–Ottawa scale (NOS) 7 and the GRADE system 8 were used.
Results
After merging, the records found on the different databases searched and after removing duplicates, 200 articles were screened for eligibility based on the title and abstract. Fifteen articles were retrieved for a full‐text evaluation. A total of nine articles were finally included in the present systematic review. The flow chart of studies identification and inclusion/exclusion process is shown in Figure 1.
Fig 1.
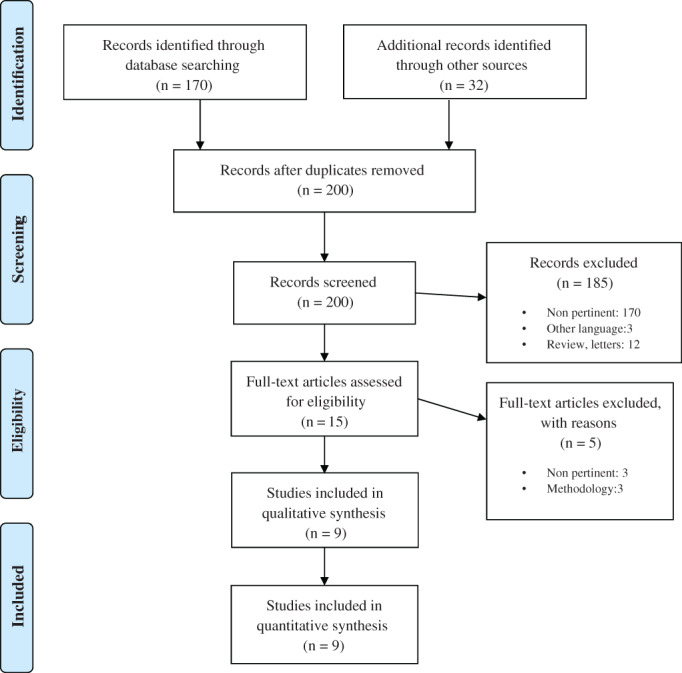
PRISMA flow diagram for study search, selection, inclusion, and exclusion. Example or search terms strategy: (“cholecystectomy”[MeSH terms] OR “cholecystectomy”[all fields] OR “cholecystectomies”[all fields]) AND (“learning curve”[MeSH terms] OR (“learning”[all fields] AND “curve”[all fields]) OR “learning curve”[all fields]) AND (“laparoscopie”[all fields] OR “laparoscopy”[MeSH terms] OR “laparoscopy”[all fields] OR “laparoscopies”[all fields]) AND (“education”[MeSH subheading] OR “education”[all fields] OR “training”[all fields] OR “education”[MeSH terms] OR “train”[all fields] OR “train s”[all fields] OR “trained”[all fields] OR “training s”[all fields] OR “trainings”[all fields] OR “trains”[all fields]).
Study characteristics
The selected studies were published between 1991 and 2020 and they were all cohort or case–control studies. These were carried out in Europe (n = 2), Asia and Pacific (n = 5), and North America (n = 2). The general characteristics of the included studies are displayed in Table 1. The total number of laparoscopic cholecystectomies considered was 12 278. Laparoscopic cholecystectomy was carried out for symptomatic stones or gallbladder polyps in six articles 9 , 10 , 11 , 12 , 13 , 14 whereas the gallbladder pathology was not specified in the remaining three articles 15 , 16 , 17 (Table 1).
Table 1.
General studies characteristics
| First author | Year of publication | Journal | Study design | Study period | Gallbladder Pathology | No. of procedures | Procedures performed by senior surgeons | Procedures performed by resident surgeons | Surgeons experience (no. of previous surgeries) | Expected learning curve |
|---|---|---|---|---|---|---|---|---|---|---|
| Jung 13 | 2020 | Indian J Surg | Cohort Study | 2014–2016 |
‐Chronic cholecystitis ‐Gallbladder polyps |
219 | 136 | 83 | > 250 cholecystectomy (senior); >50 procedures (residents) | 20 |
| Jung 9 | 2016 | J Minim Invas Surg | Cohort Study | 2010–2012 |
‐Symptomatic stones ‐Acute cholecystitis |
428 | 277 | 151 | Specified only for residents | – |
| Pariani 11 | 2014 | Surg Res Pract | Cohort Study | 2009–2013 |
‐Symptomatic stones ‐Biliary dyskinesia ‐gallbladder polyps. |
569 | 246 | 323 | Specified only for residents | – |
| Ali 12 | 2012 | JAMC | Cohort Study | 2009–2010 | ‐Symptomatic stones | 94 | 87 | 7 | Not specified | – |
| Salim 15 | 2010 |
Basrah J. |
Cohort Study | 2002–2004 | Not specifies | 100 | 100 | – | Not specified | – |
| Voitk 16 | 2001 | Am J Surg | Cohort study | 1992–1998 | Not specified | 252 | 252 | – | Not specified | 200 |
| Böckler 10 | 1999 | JSLS | Cohort Study | 1992–1996 |
‐Symptomatic stones ‐Acute cholecystitis |
252 | 162 | 89 | Specified only for residents | 50 |
| Moore 17 | 1995 | Am J Surg | Case–Control | 1989–1993 | Not specified | 8.839 | 8.839 | — | Not specified | 50 |
| Davidoff 14 | 1991 | Ann Surg | Cohort Study | 1990–1991 | ‐Chronic cholecystitis | 1518 | 1518 | — | Not specified | 13 |
Surgical experience was defined as the number of procedures/courses performed in laparoscopic settings. Only one of the selected articles 13 specified both surgeons and residents experience; three articles 9 , 10 , 11 specified only the resident experience. The surgical experience of the first operator was not specified in the remaining five articles. 12 , 14 , 15 , 16 , 17
Over the nine selected articles, only five (55.5%) reported the number of the needed procedures to complete the learning curve in laparoscopic cholecystectomy. 10 , 13 , 14 , 16 , 17 The other four articles analyzed the learning process without providing a learning curve cut‐off. Only five articles 9 , 10 , 11 , 12 , 13 compared the learning curve of young surgeons/residents to that one of senior surgeons. However, despite the intention to explore this important area of surgical education, the number of procedures performed by residents was always lower than that performed by senior surgeons, except in one article (Table 1).
Two articles evaluated the learning curve only in relation to bile duct injuries rate and the surgical ability in their management 14 , 17 ; two articles not reported the bile ducts injuries rate 15 , 16 ; only three articles considered the operator experience, preoperative data patients, operative time, conversion rate, postoperative stay, and complications rate 9 , 11 , 13 ; only two articles reported mortality rate 12 , 13 and one article reported readmission rate. 16 Table 2 showed all the variables considered by the selected studies during the learning curve assessment.
Table 2.
Variables considered in the learning curve assessment
| First authors, year | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Operator experience | Pre‐operative data | Bile duct injuries | Operative time | Complications rate | Conversion rate | Postoperative stay | Mortality | Readmission | |
| Jung, 2020 13 | x | x | x | x | x | x | x | x | n/a |
| Jung, 2016 9 | x | x | x | x | x | x | x | n/a | n/a |
| Pariani, 2014 11 | x | x | x | x | x | x | x | n/a | n/a |
| Ali, 2012 12 | x | n/a | x | x | x | x | x | x | n/a |
| Salim, 2010 15 | n/a | n/a | n/a | n/a | x | x | n/a | n/a | n/a |
| Voitk, 2001 16 | n/a | n/a | n/a | x | x | x | n/a | n/a | x |
| Böckler, 1999 10 | x | n/a | x | x | x | x | x | n/a | n/a |
| Moore, 1995 17 | n/a | n/a | x | n/a | n/a | n/a | n/a | n/a | n/a |
| Davidoff, 1991 14 | n/a | n/a | x | n/a | x | x | n/a | n/a | n/a |
n/a, not available data; x, reported data.
Two studies considered laparoscopic cholecystectomy performed in elective settings only, 11 , 12 five articles 10 , 13 , 14 , 15 , 16 considered cholecystectomies in both emergency and elective settings. The grade of gallbladder inflammation was not specified in two articles 9 , 17 ;
The intraoperative complications rate was zero in two studies 14 , 16 and not specified in one article. 15 The conversion rate was zero in one study 9 and not specified in one article. 17 The operative time was not specified in three articles 14 , 15 , 17 ; Characteristics of laparoscopic cholecystectomy and main findings of the included studies are reported in Table 3.
Table 3.
Laparoscopic cholecystectomy characteristics and main findings
| First author, year | N elective procedures | N emergency procedures | Intraoperative complications | Conversion rate | Operative time | Main findings |
|---|---|---|---|---|---|---|
| Jung, 2020 13 | 343 | 85 | 9 (2.10%) | 2.33% | 62–51 min | Laparoscopy cholecystectomy is a safe procedure for resident |
| Jung, 2016 9 | n/a | n/a | 7 (3.2%) | 0 | 40.7–63.7 min | No differences between residents and senior |
| Pariani, 2014 11 | 569 | 0 | 8 (1.40%) | 2.98% | 75–87 min | No differences between residents and senior |
| Ali, 2012 12 | 94 | 0 | 11 (11.70%) | 6.38% | 25–60 min | Useful virtual simulated program |
| Salim, 2010 15 | 90 | 10 | n/a | 21% | n/a | Increasing experience decreased conversion rate |
| Moore, 1995 16 | n/a | n/a | 15 (0.16%) | n/a | n/a | Learning curve of 50 cases |
| Böckler, 1999 10 | 198 | 53 | 8 (3.18%) | 5.7% | 111–145 min | Importance of surgical training |
| Voitk, 2001 17 | 425 | 75 | 0 | 3–2% | 35.2 min | Learning curve of 200–300 cases |
| Davidoff, 1991 14 | 7 | 5 | 0 | 25% | n/a | Management of ductal injuries |
n/a, not available.
Laparoscopic cholecystectomy and learning curve
The selected articles described the learning curve as the learning process to reach correct surgical skills in the index procedure, laparoscopic cholecystectomy. All the articles analyzed different variables during the learning curve assessment as reported in Table 2. However, none of the included articles provided specific statistical approaches for learning curve evaluation, like cumulative sum analysis (CUSUM).
Only five studies reported a cut‐off value for the learning curve in laparoscopic cholecystectomy. Two articles estimated a learning curve of 50 surgeries to become proficient: one of them basing the learning curve evaluation only on bile duct injuries decrease, 17 the other one also considering the decreasing of operative time, complications rate, conversion rate, and postoperative stay 10 ; one article assessed this value at 20 surgeries considering all the intraoperative and postoperative complications, and including mortality 13 ; one article assessed this learning curve at 200 surgeries considering operative time, conversion rate, complications rate, and readmissions decrease 16 ; the last article estimated a learning curve of 13 surgeries based on reduction of complications and conversion rate 14 (Table 2).
The remaining four articles described the learning curve process, but they did not identify a specific cutoff of interventions that should be performed to complete the learning curve. 9 , 11 , 12 , 15
Of the five articles considering learning curve in surgical residents, four articles 9 , 10 , 11 , 13 concluded that laparoscopic cholecystectomy was a safe operation when performed by residents under supervision, while one article concluded that the procedure should be learnt on virtual simulated models. 12 (Table 3).
Study quality assessment
Based on the NOS Quality assessment scale, 7 eight studies 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 received five of nine stars and one study 17 received four of nine stars, all resulting being of fair/poor quality. According to the GRADE system, 8 three articles 11 , 13 , 14 were judge as being of low quality and six studies of very low quality. 9 , 10 , 12 , 15 , 16 , 17 Of note, all the included studies were retrospective cohorts thus susceptible, by definition, of major selection bias, and showed high heterogeneity in the learning curve estimation process.
Discussion
The present systematic review shows that currently there is not a consensus on which criteria should be considered and how to measure the learning curve process of laparoscopic cholecystectomy. 3
In our knowledge, this is the first systematic review to analyze the available literature on the learning curve of laparoscopic cholecystectomy. The field of surgical education is an active area of research. 18 The use of surgical simulators and training courses were judged to be important educational tools to improve the surgical learning curve. 3 , 19 Therefore, despite laparoscopic cholecystectomy being one of the most performed surgeries worldwide by young and senior surgeons, 3 its learning curve remains unclear.
The parameters to calculate the learning curve are not standardized. As a result, different authors considered different variables to see the proficiency of surgical skills. Therefore, the definition of the learning curve itself is not very objective, but it is based on arbitrarily chosen parameters.
Only a few articles in the literature suggested a cutoff of surgeries to achieve the learning curve. The lack of guidelines describing the parameters that should be analyzed to determine a learning curve leads to heterogeneous results among them. Indeed, the learning curve of laparoscopic cholecystectomy ranges from 13 to 200 surgeries. None of the included studies showed a specific statistical method for the learning curve evaluation. The CUSUM should represent the preferred analysis to evaluate the surgical competence, 20 , 21 but none of the included articles assessed the learning curve process on this. CUSUM is a graphical method applied for statistical quality control to provide a objective evidence of quality and demonstrate changes in competence over time. 21 The analysis shows the sequential difference of a set of measured values defining a target level. 20 Therefore, CUSUM could be a very useful and objectively tools to shows changes in surgical competences during training.
All the studies evaluated the learning curve process on the reduction of arbitrarily chosen variables 16 , 17 or comparing residents' performance to senior surgeons' ones. 11 , 13 The use of different methods and criteria to estimate the learning curve has resulted in different and not homogeneous cut‐offs that have been proposed by several authors.
According to the progressive reduction in bile duct injuries, one author estimated that 50 laparoscopic cholecystectomies were enough to complete the learning curve. 17 However, the evaluation of the learning curve cannot be based on one single parameter because this could be reductive, and other factors must be considered. 3 Davidoff et al. evaluated also complications and conversion rate decrease, detecting a learning curve of 13 procedures. 14 Other authors 9 , 10 , 11 , 13 evaluated the trend of preoperative, intraoperative, and postoperative factors, such as operative time, complication rate, and conversions rate, often without specify the surgical operator experience. 14 , 15 , 16 However, literature suggested that operator experience (senior vs. residents; PGY level) has an impact on the learning curve process in different type of surgeries and must be considered when calculating a learning curve. 18 , 19 , 22
Not all the studies considered residents in the evaluation of the learning curve (Table 1). However, especially for a surgery often performed in the early stage of surgical training (like the laparoscopic cholecystectomy), consider a young population of surgeons seems to be relevant to achieve a reliable learning curve.
Another important factor is if the surgical procedure has been performed in an emergency or elective setting. In this systematic review, seven articles 10 , 11 , 12 , 13 , 14 , 15 , 16 specify this data. The grade of inflammation and different intraoperative variables could influence the operative time, the conversion rate and the complications rate and must always be considered during the learning curve. 3 , 23
Finally, only three studies 9 , 11 , 13 considered patients preoperative characteristics, like the ASA score, comorbidity, and previous abdominal surgeries. These factors could influence the variables on which the learning curve is evaluated and should be taken into account to avoid bias. 23 , 24 The literature reported a conversion rate ranging from 5% for elective laparoscopic cholecystectomy to 10% in emergency settings. 25 The average time for this operation is usually less than 1 h 26 and the postoperative complications range from 0.5% to 6%. 27 While all the selected studies showed conversion rate in line with the literature, three studies 10 , 11 , 13 reported a high average operative time, even if decreased during the learning curve evaluation.
Patients' average age and comorbidities, grade of gallbladder inflammation and duration of symptoms, could influence the intraoperative variables, 23 and should be considered to avoid bias.
Therefore, different variables should be taken into account when evaluating the learning curve:
patient's factor (age, gender, comorbidities, ASA score, inflammation grade)
surgeon's characteristics (previous experiences, simulation course, laparoscopic training)
intraoperative factors (operative times, complications, anatomical variants)
postoperative factors (in‐hospital stay, morbidity, mortality)
All these variables should be evaluated with ad‐hoc statistical methods to assure objective and reliable learning curves, allowing comparison with other surgical centres.
This study has several limitations. The currently available literature is based on retrospective cohort studies which represents a low quality of evidence. All the included studies showed a high heterogeneity in the interpretation of the learning curve. Thus, caution should be paid in the interpretation of the results since several biases can be mentioned in the individual studies, such as reporting bias, publication bias, and geographical bias. However, we tried to control for search biases by searching the literature on multiple databases, by manual crosscheck of the reference lists, and by performing a critical selection by two independent reviewers.
Conclusions
This systematic review provides an exhaustive summary of the literature on the learning curve process of a highly common surgical procedure, such as laparoscopic cholecystectomy. The critical appraisal of the available literature and the evaluation of the current evidence highlights the actual lack of consensus in the evaluation of the laparoscopic cholecystectomy learning curve and a great heterogeneity in this relevant field of surgical educations.
Organized training programs and multicentric studies should be suggested to clarify which is the learning curve of laparoscopic cholecystectomy and consequently provide important data to improve residency programs.
Author contributions
Elisa Reitano: Conceptualization; data curation; project administration; resources; supervision; validation; visualization; writing‐original draft. Nicola de'Angelis: Conceptualization; formal analysis; investigation; supervision; validation; writing‐review & editing. Elena Schembari: Conceptualization; data curation; methodology; supervision; visualization; writing‐review & editing. Maria Clotilde Carrà: Data curation; methodology; resources; validation; visualization; writing‐original draft. Elisa Francone: Conceptualization; formal analysis; methodology; resources; validation; visualization; writing‐review & editing. Sergio Gentilli: Conceptualization; data curation; methodology; supervision; validation; visualization; writing‐review & editing. Gaetano La Greca: Conceptualization; investigation; methodology; supervision; writing‐review & editing.
Conflict of interest
None declared.
Acknowledgements
PRISMA 2009 checklist statement: The authors have read the PRISMA 2009 Checklist, and the manuscript was prepared and revised according to the PRISMA 2009 Checklist.
E. Reitano MD; N. de'Angelis MD, PhD; E. Schembari MD; M. C. Carrà MD,PhD; E. Francone MD, PhD; S. Gentilli MD; G. La Greca MD.
This article is not based on a previous communication to a society or meeting.
References
- 1. Hopper AN, Jamison MH, Lewis WG. Learning curves in surgical practice. Postgrad Med J. 2007;83:777–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Perticone F, Hollands CEC. Learning curve. Videochirurgia Pediatrica – Principi di tecnica in laparoscopia. 1st ed. Italy: toracoscopia e retroperitoneoscopia pediatrica; 2010. [Google Scholar]
- 3. Ferrarese A, Gentile V, Bindi M, Rivelli M, Cumbo J, Solej M, et al. The learning curve of laparoscopic holecystectomy in general surgery resident training: old age of the patient may be a risk factor? Open Med. 2016;11:489–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Comitalo JB. Laparoscopic cholecystectomy and newer techniques of gallbladder removal. JSLS. 2012;16:406–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Steigerwald SN, Park J, Hardy KM, Gillman L, Vergis AS. The fundamentals of laparoscopic surgery and LapVR evaluation metrics may not correlate with operative performance in a novice cohort. Med Educ. 2015;20:30024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, WV Page MJ. Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Handbook 2019.
- 7. Stang A. Critical evaluation of the Newcastle‐Ottawa scale for the assessment of the quality of nonrandomized studies in meta‐analyses. Eur J Epidemiol. 2010;25:603–5. [DOI] [PubMed] [Google Scholar]
- 8. Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction ‐ GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383–94. [DOI] [PubMed] [Google Scholar]
- 9. Jung YK, Kwon YJ, Choi D, Lee KG. What is the safe training to educate the laparoscopic cholecystectomy for surgical residents in early learning curve? J Minim Invasive Surg. 2016;19:70–4. [Google Scholar]
- 10. Böckler D, Geoghegan J, Klein M, et al. Implications of laparoscopic cholecystectomy for surgical residency training. JSLS J Soc Laparoendosc Surg. 1999;3:19–22. [PMC free article] [PubMed] [Google Scholar]
- 11. Pariani D, Fontana S, Zetti G, Cortese F. Laparoscopic cholecystectomy performed by residents: a retrospective study on 569 patients. Surg Res Pract. 2014;2014:912143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ali SA, Soomro AG, Mohammad AT, Jarwar M, Siddique AJ. Experience of laparoscopic cholecystectomy during a steep learning curve at a university hospital. J Ayub Med Coll Abbottabad. 2012;24:27–9. [PubMed] [Google Scholar]
- 13. Jung YK, Choi D, Lee KG. Learning laparoscopic cholecystectomy: a surgical resident's insight on safety and training during the initial 151 cases. Indian J Surg. 2020;83:224–9. [Google Scholar]
- 14. Davidoff AM, Pappas TN, Murray EA, et al. Mechanisms of major biliary injury during laparoscopic cholecystectomy. Ann Surg. 1992;215:196–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Salim JH, Al‐Khayat HS. The learning curve of FIRST one HUNDRED laparoscopic cholecystectomy. Basrah J Surg. 2010;16:16–20. [Google Scholar]
- 16. Voitk AJ, Tsao SGS, Ignatius S. The tail of the learning curve for laparoscopic cholecystectomy. Am J Surg. 2001;182:250–3. [DOI] [PubMed] [Google Scholar]
- 17. Moore MJ, Bennett CL. The learning curve for laparoscopic cholecystectomy. Am J Surg. 1995;170:55–9. [DOI] [PubMed] [Google Scholar]
- 18. De'Angelis N, Lizzi V, Azoulay D, Brunetti F. Robotic versus laparoscopic right colectomy for colon cancer: analysis of the initial simultaneous learning curve of a surgical fellow. J Laparoendosc Adv Surg Tech. 2016;26:882–92. [DOI] [PubMed] [Google Scholar]
- 19. Nagakawa Y, Nakamura Y, Honda G, Gotoh Y, Ohtsuka T, Ban D, et al. Learning curve and surgical factors influencing the surgical outcomes during the initial experience with laparoscopic pancreaticoduodenectomy. J Hepatobiliary Pancreat Sci. 2018;25:498–507. [DOI] [PubMed] [Google Scholar]
- 20. DeSouza AL, Prasad LM, Park JJ, Marecik SJ, Blumetti J, Abcarian H. Robotic assistance in right hemicolectomy: is there a role? Dis Colon Rectum. 2010;53:1000–6. [DOI] [PubMed] [Google Scholar]
- 21. Gezer S, Avcl A, Türktan M. Cusum analysis for learning curve of videothoracoscopic lobectomy. Open Med. 2016;11:574–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Pereira N, Lee YH, Suh Y, Choi DH, Suh HS, Jeon JY, et al. Cumulative experience in Lymphovenous anastomosis for lymphedema treatment: the learning curve effect on the overall outcome. J Reconstr Microsurg. 2018;34:735–41. [DOI] [PubMed] [Google Scholar]
- 23. Coccolini F, Catena F, Pisano M, Gheza F, Fagiuoli S, di Saverio S, et al. Open versus laparoscopic cholecystectomy in acute cholecystitis. Systematic review and meta‐analysis. Int J Surg. 2015;18:196–204. [DOI] [PubMed] [Google Scholar]
- 24. Giger UF, Michel JM, Opitz I, Inderbitzin DT, Kocher T, Krähenbühl L. Risk factors for perioperative complications in patients undergoing laparoscopic cholecystectomy: analysis of 22,953 consecutive cases from the Swiss Association of Laparoscopic and Thoracoscopic Surgery Database. J Am Coll Surg. 2006;203:723–8. [DOI] [PubMed] [Google Scholar]
- 25. Livingston EH, Rege RV. A nationwide study of conversion from laparoscopic to open cholecystectomy. Am J Surg. 2004;188:205–11. [DOI] [PubMed] [Google Scholar]
- 26. Subhas G, Gupta A, Bhullar J, Dubay L, Ferguson L, Goriel Y, et al. Prolonged (longer than 3 hours) laparoscopic cholecystectomy: reasons and results. Am Surg. 2011;77:981–4. [PubMed] [Google Scholar]
- 27. Radunovic M, Lazovic R, Popovic N, Magdelinic M, Bulajic M, Radunovic L, et al. Complications of laparoscopic cholecystectomy: our experience from a retrospective analysis. Maced J Med Sci. 2016;4:641–6. [DOI] [PMC free article] [PubMed] [Google Scholar]


