Abstract
Objectives
Transcatheter aortic valve implantation (TAVI) is an important treatment option for patients with severe aortic stenosis. To improve patient selection, shared decision‐making is recommended to elicit patients' treatment expectations and goals. We assessed patients' expectations and goals before TAVI treatment and whether these were met after treatment. Additionally, we evaluated how meeting these goals aligned with quality of life and functional recovery.
Design
A mixed method study.
Setting
An academic medical center.
Participants
Seventy‐four patients undergoing TAVI between 2015 and 2017.
Measurements
Patients' expectations and goals were assessed qualitatively before treatment. Six to twelve months post procedure, quality of life was measured with the EuroQuol‐5D and any change in the number of dependencies in (instrumental) activities of daily living was assessed.
Results
Mean age of patients was 81.5 years, and 37.8% were male. Regaining the ability to engage in a specific hobby or activity was the most important treatment goal (33 patients, 54.1%), followed by reducing symptoms (19 patients 31.1%). 66.2% of patients stated that their treatment goal was met. Quality of life was higher in this group, as compared with patients who had not met their treatment goal. Twenty‐three patients (31.1%) showed functional improvement.
Conclusion
TAVI patients were quite capable of eliciting treatment goals and a majority stated, after treatment, that these had been met patients' experience of treatment benefits regarding these goals had poor alignment with functional outcomes. This raises questions regarding relevant outcome measurements in this population, and could aid in improving shared decision‐making and patient selection for TAVI.
Keywords: activities of daily living, goals, patient‐centered outcomes, quality of life, shared decision‐making, transcatheter aortic valve implantation
Key Points
Most patients undergoing TAVI were able to identify specific treatment goals.
Regaining the ability to engage in a specific hobby or activity was the most important treatment goal of patients undergoing TAVI.
The patient's perspective of treatment benefit aligns poorly with functional outcome after TAVI.
Why Does this Paper Matter?
This paper provides new information about treatment expectations and goals of TAVI patients, and raises important questions regarding how to define and measure the success of treatment in this population.
INTRODUCTION
Degenerative valvular aortic stenosis is a common medical condition with a prevalence that increases with age, and has a poor prognosis if left untreated. 1 , 2 Aside from conventional surgical aortic valve replacement (sAVR), transcatheter aortic valve implantation (TAVI) is an important treatment option, especially for older patients with comorbidities who are considered too high risk for sAVR. TAVI reduces mortality similar to sAVR, even in patients with low or intermediate surgical risk. 3 , 4 , 5
Importantly, not all patients improve from TAVI in terms of quality of life or functional recovery. 6 Therefore, selecting patients who will benefit from this procedure is a topic of debate. To improve patient selection, current guidelines advocate shared decision‐making (SDM) for patients with aortic stenosis. 7 In SDM, the benefits and risks of a procedure are weighted and incorporated with the patients values and treatment goals. 8 Little is known about treatment goals of patient evaluated for TAVI. 9
Therefore, the aim of this study is to assess patient expectations and goals before TAVI, and determine after treatment whether they had been met. Second, we aim to assess how a patients' perspective of treatment benefits regarding these goals corresponds with quality of life and functional performance after TAVI.
METHODS
Setting and participants
An observational prospective cohort study was performed between July 2015 and December 2017 at a university teaching and tertiary hospital in the Netherlands. Patients who underwent elective TAVI, and gave informed consent to participate in a follow‐up visit after 6–12 months, were included. All patients were preoperatively evaluated by a geriatrician and discussed in a multidisciplinary heart team comprising invasive cardiologists, imaging cardiologists, and cardiothoracic surgeons to establish the indication and suitability for TAVI. All patients had received information regarding the procedure and possible complications from the cardiology department. Permission was granted by the local Medical Ethics Committee.
Baseline assessment
At baseline, patients were evaluated at the geriatric outpatient clinic with a comprehensive geriatric assessment (CGA) to gather information regarding demographic data, social status, current health status, comorbidities, cognitive, and functional status. We used the Charlson Comorbidity Index to list comorbidities. 10 Cognition was evaluated with the Mini‐Mental State Examination (MMSE). 11 For functional status, two different questionnaires were used. During the first year of the study, the Groningen Activity Restriction Scale (GARS‐4) was used, which comprises 11 items concerning activities of daily living (ADLs) and 7 items concerning instrumental activities of daily living (IADLs). Each item is scored on four levels: independent without difficulty (1), independent with some difficulty (2), independent with much difficulty (3), or dependent (4). These categories can be recoded into a dichotomous outcome: independent (levels 1–3) or dependent (level 4), which is how it was used in this analysis (thus named GARS‐2). 12 During the rest of the study period the 15‐item modified Katz Index of Activities of Daily Living (Katz‐15) was used. This scale consists of 8 ADL and 7 IADL items, scored as dependent or independent. 13 Surgical risk was calculated using the logistic European System for Cardiac Operative Risk Evaluation (EuroSCORE). 14 Expectations and goals with regard to TAVI treatment were elicited during the CGA, by asking the following question: “What do you hope to accomplish by undergoing this treatment?” This question was adapted from an earlier study on treatment goals of TAVI patients. 9
Follow‐up assessment
Between 6 and 12 months after TAVI, a follow‐up visit was scheduled. Patients were asked whether their previously mentioned expectations and goals for TAVI were met (recorded as a “yes” or “no”). Health‐related quality of life after TAVI was measured using the EuroQuol‐5D (EQ‐5D). The EQ‐5D consists of five dimensions (mobility, self‐care, usual activities, pain/discomfort, and anxiety/depression), which are scored on three levels: no, some, or extreme problems. A single index value was generated by aggregating and weighting the five domains, using de Dutch EQ‐5D tariff. 15 The resulting score ranges from less than 0 (0 is a health state equivalent to death, negative values are valued as “worse than death”) to 1 (perfect health). The EQ‐5D visual analogue scale (VAS), ranging from 0 to 100 (higher score indicating better health) was used to measure patients' perceived general health status. Functional status was assessed using the Katz‐15 or GARS‐2, using the same scale that was used at baseline. Functional improvement was defined as a decrease of at least one point on the Katz‐15 or GARS‐2 at follow up compared with baseline. Perioperative complications were recorded according to the Valve Academic Research Consortium‐2 consensus document. 16
Data analysis
SPSS version 23.0 (IBM, Corp., Armonk, NY) was used for data analysis. Baseline characteristics and outcome measurements of patients were summarized with descriptive statistics. For the qualitative analysis of patients expectations, two independent reviewers (SF and SB) categorized expectations into four themes that were formulated in the previous work of Fried and colleagues: (i) maintaining independence; (ii) staying alive; (iii) reducing/ eliminating pain or symptoms; and (iv) ability to do a specific activity. 9 , 17 A fifth category named “other” was used for expectations that did not fit within any of these categories. Discrepancies were resolved through discussion.
Alignment of the patient's experiences of treatment benefits with functional improvement after TAVI was evaluated by classifying patients into four mutually exclusive categories, based on whether goals were met (yes/no) and measured functional improvement (yes/no).
RESULTS
Patient recruitment and baseline characteristics
During the study period 100 consecutive patients were eligible to participate in the study. One patient had an incomplete functional assessment at baseline. At follow‐up, 5 patients declined to participate, 2 patients were not able to participate due to poor condition, 1 was lost to follow‐up, and 10 had died. IN addition, 7 patients had incomplete data on patient perspective after TAVI, resulting in 74 patients that were included in this study.
Baseline characteristics of the 74 included patients are summarized in Table 1. Mean age was 81.5 years (standard deviation 5.8), 87.8% were previously living at home and the median number of IADL dependencies was two (interquartile range [IQR] 1.0–4.3). Median MMSE score was 28 (IQR 27.0–29.0). As indicated by the logistic EuroSCORE, 20.3% of patients had low, 56.7% had intermediate, and 23.0% had high surgical risk. Excluded patients were similar to included patients in terms of baseline characteristics (Table S1).
TABLE 1.
Baseline characteristics of included patients (n = 72)
| Variable | Number, mean or median |
|---|---|
| Age, mean ± SD | 81.5 (5.8) |
| Male, n (%) | 28 (37.8) |
| Living at home, n (%) | 65 (87.8) |
| No or only primary education, n (%) | 29 (39.2) |
| Data missing | 2 |
| Number of IADL dependencies, median (IQR) | 2.0 (1.0–4.3) |
| Subjective memory complaints, n (%) | 24 (32.4) |
| Data missing | 1 |
| Dementia, n (%) | 0 (0) |
| Prior delirium, n (%) | 12 (16.2) |
| MMSE, median (IQR) | 28.0 (27.0–29.0) |
| Charlson Comorbidity Index, median (IQR) | 2.0 (1.0–3.0) |
| Active cancer, n (%) | 7 (9.5) |
| Coronary artery disease, n (%) | 29 (39.2) |
| Chronic obstructive pulmonary disease, n (%) | 24 (32.4) |
| Diabetes mellitus, type II, n (%) | 16 (21.6) |
| Atrial fibrillation, n (%) | 25 (33.8) |
| Number of prescriptions, median (IQR) | 8.0 (5.3–11.0) |
| Logistic EuroSCORE I, median (IQR) | 15.0 (10.0–19.0) |
| Left ventricular ejection fraction in %, median (IQR) | 55.0 (45.0–55.0) |
| eGFR, mean ml/min/1.73 m2 (SD) | 55.9 (15.8) |
Abbreviations: ADL, activities of daily living; IADL, instrumental activities of daily living; IQR, interquartile range; MMSE, Mini‐Mental State Examination; SD, standard deviation.
Patient expectations and goals for TAVI
Six patients were not able to formulate an expectation or goal, or had none. For the remaining 68 patients, the expectation or goal most often reported was regaining the ability to engage in a specific activity or hobby (33 patients, 48.5%), for example gardening, cycling, or engaging in social activities. Reducing or eliminating symptoms was reported by 19 patients (27.9%), followed by maintaining independence, which was reported by 8 patients (11.8%). Only one patient reported staying alive as an expectation for TAVI. We were not able to categorize the answers of seven patients in these four predefined themes. Of those seven, three expected that their overall condition would improve, two expected not to worsen, one stated that TAVI was needed in order to have a hip replacement and one mentioned several expectations without any hierarchy.
Treatment outcomes
Median duration of follow‐up was 7 months (IQR 6.0–9.0 months). At that time point, 49 patients (66.2%) stated that their expectations and goals for TAVI had been met. These patients had a higher surgical risk at baseline, and had experienced vascular (access site and access‐related) complications after TAVI less often than patients whose treatment expectations and goals had not been met. Both EQ‐5D index and VAS were higher in the former group than in the latter (Table 2). Twenty‐three patients (31.1%) showed functional improvement as measured by the Katz‐15 or GARS‐2.
TABLE 2.
Baseline characteristics and (post) procedural outcomes of patients who had and had not met their treatment expectations and goals
| Variable | Expectations/goals met (n = 49) | Expectations/goals not met (n = 25) | p‐Value |
|---|---|---|---|
| Age, mean ± SD | 81.5 (5.4) | 80.6 (6.6) | 0.56 |
| Number of IADL dependencies, median (IQR) | 2.0 (0.0–4.0) | 2.0 (1.0–5.0) | 0.36 |
| Subjective memory complaints, n (%) | 16 (32.7) | 8 (33.0) | 0.95 |
| Data missing | 0 | 1 | |
| MMSE, median (IQR) | 28.0 (27.0–29.0) | 28.0 (25.0–29.0) | 0.75 |
| Charlson Comorbidity Index, median (IQR) | 2.0 (1.0–3.0) | 2.0 (1.0–3.0) | 0.56 |
| Logistic EuroSCORE I, median (IQR) | 16.0 (12.0–20.0) | 12.0 (7.0–17.0) | 0.02 |
| Complications, n (%) | |||
| Stroke | 0 | 0 | n.a. |
| Bleeding | 14 (29.6) | 11 (44.0) | 0.18 |
| Vascular | 5 (10.2) | 8 (32.0) | 0.02 |
| Acute kidney injury | 2 (4.1) | 2 (8.0) | 0.48 |
| Need for pacemaker | 5 (10.2) | 3 (12.0) | 0.81 |
| Length of hospital stay in days, median (IQR) | 7.0 (6.0–8.0) | 8.0 (6.0–9.0) | 0.15 |
| EQ‐5D index, median (IQR) | 0.81 (0.69–0.89) | 0.73 (0.43–0.81) | 0.02 |
| EQ‐5D VAS, median (IQR) | 70.0 (70.0–80.0) | 70.0 (51.3–70.0) | 0.01 |
| Functional improvement, n (%) a | 17 (34.7) | 6 (24.0) | 0.35 |
Abbreviations: ADL, activities of daily living; EQ‐5D, EuroQuol‐5D; IADL, instrumental activities of daily living; IQR, interquartile range; MMSE, Mini‐Mental State Examination; n.a., not applicable; SD, standard deviation; VAS, visual analogue scale..
Decrease of at least one point on the Katz‐15 or GARS‐2 at follow‐up compared with baseline.
Alignment of the patients perspective of treatment benefit with functional improvement after TAVI
There were 17 patients who stated both their treatment expectations and goals had been met and had functional improvement (alignment of treatment benefit), and 19 patients who stated both their treatment expectations and goals had not been met and had no functional improvement (alignment of no treatment benefit) (Figure 1).
FIGURE 1.
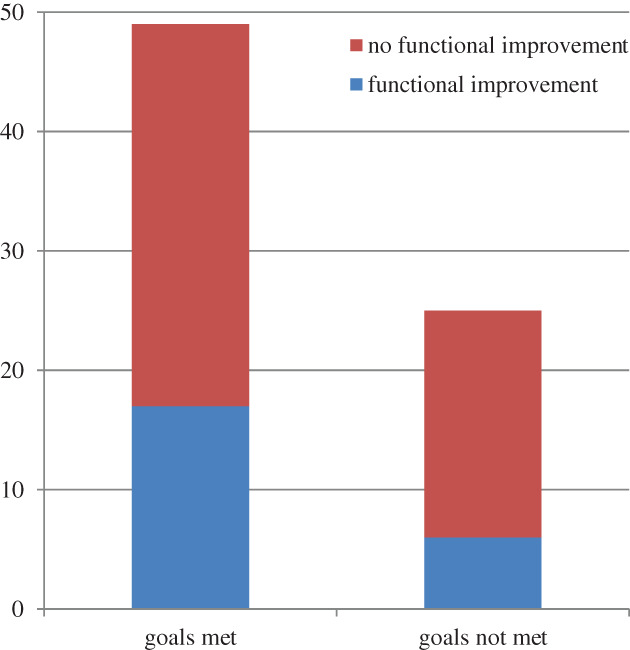
Number of patients in four mutually exclusive categories based on whether goals were met and with or without functional improvement
DISCUSSION
In this study of 72 TAVI patients, we found that regaining the ability to engage in a specific activity or hobby was the most important treatment goal, followed by reducing symptoms. Maintaining independence and staying alive were mentioned less often. Almost two‐thirds of patients stated that their treatment goal had been met, and those patients reported a higher quality of life than patients whose treatment goal had not been met. TAVI treatment resulted in objectively measured functional improvement in less than one‐third of patients. The patients' perspectives of treatment benefits did not align well with functional outcomes.
To the best of our knowledge, there is only one prior study that has addressed expectations and goals in patients undergoing TAVI. Coylewright and colleagues asked 46 older patients about their treatment goals for TAVI and also found that this most often was the ability to do a specific activity or hobby. 9 After 1 month, 87% of patients had reached their treatment goal as was determined retrospectively by reviewing the patient records. This is a higher percentage than we found (66.2%), which might be due to the retrospective character of the study of Coylewright.
We found that the percentage of patients that stated their treatment goal had been met, and thus had benefited from TAVI from a patients perspective, was higher than the percentage of patients that showed functional improvement as measured on an IADL scale. The subjective statement that treatment expectations and goals had been met might be influenced by feelings of gratitude or relief at having survived this major health event. We found that patients whose treatment expectations and goals were met had a higher surgical risk. These feelings might be stronger in this group, as compared with patients with a lower surgical risk. Additionally, a patients' perception of the values underlying their treatment expectations might change over time, a phenomenon called “response shift.” 18 , 19 This can result in a measured improvement in self‐reported health over time, although it is not measured objectively. Lastly, in our study, one‐third of patients reported subjective memory complaints, which might have resulted in recall bias. 20 Measuring change in IADLs is more objective, and also an important outcome from a patient's perspective, as maintaining independence is highly valued by older patients. 21 However, given that only 13.1% of our patients reported maintaining independence as their treatment goal, functional improvement might be a poor substitute for treatment benefit in our study population. In order to regain the ability to engage in a specific activity or hobby, the most often mentioned treatment goal, functional improvement might not be a necessary condition. Additionally, measuring change on an IADL scale has its own methodological limitations, as it is questionable if a clinically important change in a timeframe of 6 months can be reliably measured with such often used questionnaires as the Katz‐ADL. 22 Given the few limitations in IADLs that were measured at baseline in our population (Table 1), with 23% of patients having no IADL limitations, detecting no improvement over time can also be due to the ceiling effect. Thus, the instruments used to assess function may have been insensitive to functional improvements that patients actually experienced.
A limitation of this study is that excluding 26 patients who either died during follow‐up or had incomplete data, might have introduced selection bias, resulting in overestimating the apparent benefits of TAVI. However, in Table S1 we have shown that excluded patients were similar to included patients in baseline characteristics. A second limitation is that two different instruments were used to measure IADLs. These instruments are very similar, although there are some differences in the number of items (Katz‐15 consists of 15 items and GARS‐2 18) and the content of the items. Lastly, by choosing the wording “what do you hope” in the question on goals for treatment, patients may have been encouraged to respond with best case scenarios instead of what they actually believed to be realistic. A strength of this study is that all patients received a complete CGA with both quantitative and qualitative measurements.
In conclusion, in this study of 74 TAVI patients, we found that their most important treatment goal was to regain the ability to engage in a specific activity or hobby. The patient's perspective of treatment benefit had poor alignment with functional outcomes. Our findings pose questions regarding how to define and measure treatment success in TAVI patients. Subjective measures regarding expectations for treatment might be valuable additions. A simple question regarding these expectations can be the first step to elicit patients' values and preferences for treatment, and can aid in the process of shared decision‐making.
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTIONS
Festen, van Munster and Beishuizen developed the study concept and design. Festen, van der Werf and de Graeff acquired subjects and data. Festen, van Munster and Beishuizen contributed to analysis and interpretation of the data. All authors contributed to drafting the article and revising it critically.
SPONSOR'S ROLE
None.
Supporting information
Table S1. Baseline characteristics of included and excluded patients. SD = Standard Deviation, ADLs = Activities of Daily Living, IADL = Instrumental Activities of Daily Living, IQR = Interquartile Range, MMSE = Mini Mental State Examination
ACKNOWLEDGMENTS
Beishuizen SJE, Festen S, van der Werf HW, de Graeff P, van Munster BC. Was it worth it? Benefits of transcatheter aortic valve implantation from a patient's perspective. J Am Geriatr Soc. 2021;69(9):2605–2611. 10.1111/jgs.17216
REFERENCES
- 1. Eveborn GW, Schirmer H, Heggelund G, Lunde P, Rasmussen K. The evolving epidemiology of valvular aortic stenosis. The Tromso study. Heart. 2013;99(6):396‐400. [DOI] [PubMed] [Google Scholar]
- 2. Leon MB, Smith CR, Mack M, et al. Transcatheter aortic‐valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med. 2010;363(17):1597‐1607. [DOI] [PubMed] [Google Scholar]
- 3. Smith CR, Leon MB, Mack MJ, et al. Transcatheter versus surgical aortic‐valve replacement in high‐risk patients. N Engl J Med. 2011;364(23):2187‐2198. [DOI] [PubMed] [Google Scholar]
- 4. Leon MB, Smith CR, Mack MJ, et al. Transcatheter or surgical aortic‐valve replacement in intermediate‐risk patients. N Engl J Med. 2016;374(17):1609‐1620. [DOI] [PubMed] [Google Scholar]
- 5. Mack MJ, Leon MB, Thourani VH, et al. Transcatheter aortic‐valve replacement with a balloon‐expandable valve in low‐risk patients. N Engl J Med. 2019;380(18):1695‐1705. [DOI] [PubMed] [Google Scholar]
- 6. Arnold SV, Reynolds MR, Lei Y, et al. Predictors of poor outcomes after transcatheter aortic valve replacement: results from the PARTNER (Placement of Aortic Transcatheter Valve) trial. Circulation. 2014;129(25):2682‐2690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the Management of Patients with Valvular Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017;135(25):e1159‐e1195. [DOI] [PubMed] [Google Scholar]
- 8. Elwyn G, Frosch D, Thomson R, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27(10):1361‐1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Coylewright M, Palmer R, O'Neill ES, Robb JF, Fried TR. Patient‐defined goals for the treatment of severe aortic stenosis: a qualitative analysis. Health Expect. 2016;19(5):1036‐1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373‐383. [DOI] [PubMed] [Google Scholar]
- 11. Folstein MF, Folstein SE, McHugh PR. “Mini‐mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189‐198. [DOI] [PubMed] [Google Scholar]
- 12. Kempen GI, Suurmeijer TP. The development of a hierarchical polychotomous ADL‐IADL scale for noninstitutionalized elders. Gerontologist. 1990;30(4):497‐502. [DOI] [PubMed] [Google Scholar]
- 13. Weinberger M, Samsa GP, Schmader K, Greenberg SM, Carr DB, Wildman DS. Comparing proxy and patients' perceptions of patients' functional status: results from an outpatient geriatric clinic. J Am Geriatr Soc. 1992;40(6):585‐588. [DOI] [PubMed] [Google Scholar]
- 14. Roques F, Michel P, Goldstone AR, Nashef SA. The logistic EuroSCORE. Eur Heart J. 2003;24(9):881‐882. [DOI] [PubMed] [Google Scholar]
- 15. Lamers LM, Stalmeier PFM, McDonnell J, Krabbe PFM, van Busschbach JJ. Measuring the quality of life in economic evaluations: the Dutch EQ‐5D tariff. Ned Tijdschr Geneeskd. 2005;149(28):1574‐1578. [PubMed] [Google Scholar]
- 16. Kappetein AP, Head SJ, Généreux P, et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium‐2 consensus document (VARC‐2). Eur J Cardiothorac Surg. 2012;42(5):S45‐S60. [DOI] [PubMed] [Google Scholar]
- 17. Fried TR, Tinetti M, Agostini J, Iannone L, Towle V. Health outcome prioritization to elicit preferences of older persons with multiple health conditions. Patient Educ Couns. 2011;83(2):278‐282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sprangers MA, Schwartz CE. Integrating response shift into health‐related quality of life research: a theoretical model. Soc Sci Med. 1999;48(11):1507‐1515. [DOI] [PubMed] [Google Scholar]
- 19. Schwartz CE, Rapkin BD. Reconsidering the psychometrics of quality of life assessment in light of response shift and appraisal. Health Qual Life Outcomes. 2004;2:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. McPhail S, Haines T. Response shift, recall bias and their effect on measuring change in health‐related quality of life amongst older hospital patients. Health Qual Life Outcomes. 2010;8:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Stegmann ME, Festen S, Brandenbarg D, et al. Using the Outcome Prioritization Tool (OPT) to assess the preferences of older patients in clinical decision‐making: a review. Maturitas. 2019;128:49‐52. [DOI] [PubMed] [Google Scholar]
- 22. Suijker JJ, van Rijn M, Ter Riet G, Moll van Charante EP, de Rooij SE, Buurman BM. Minimal important change and minimal detectable change in activities of daily living in community‐living older people. J Nutr Health Aging. 2017;21(2):165‐172. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Baseline characteristics of included and excluded patients. SD = Standard Deviation, ADLs = Activities of Daily Living, IADL = Instrumental Activities of Daily Living, IQR = Interquartile Range, MMSE = Mini Mental State Examination


