Abstract
Background and Purpose
Complete reperfusion (TICI 3) after the first thrombectomy attempt or first pass effect (FPE) is associated with best clinical outcomes in large‐vessel occlusion (LVO) acute ischemic stroke. While endovascular therapy techniques have improved substantially, FPE remains low (24–30%), and new methods to improve reperfusion efficiency are needed.
Methods
In a prospective observational cohort study, 40 consecutive patients underwent cyclical aspiration thrombectomy using CLEARTM Aspiration System (Insera Therapeutics Inc., Dallas, TX). Primary outcome included FPE with complete/near‐complete reperfusion (TICI 2c/3 FPE). Secondary outcomes included early neurological improvement measured by the National Institute of Health Stroke Scale (NIHSS), safety outcomes, and functional outcomes using modified Rankin Scale (mRS). Outcomes were compared against published historical controls.
Results
Among 38 patients who met criteria for LVO, median age was 75 (range 31–96). FPE was high (TICI 3: 26/38 [68%], TICI 2c/3: 29/38 [76%]). Among anterior circulation strokes, core lab‐adjudicated FPE remained high (TICI 3: 17/29 [59%], TICI 2c/3: 20/29 [69%]), with excellent final successful revascularization results (Final TICI 3: 24/29 [83%], Final TICI 2c/3: 27/29 [93%]). FPE in the CLEAR‐1 cohort was significantly higher compared to FPE using existing devices (meta‐analysis) from historical controls (TICI 2c/3: 76% vs. 28%, p = 0.0001). High rates of early neurological improvement were observed (delta NIHSS≥4: 35/38 [92.1%]; delta NIHSS≥10: 27/38 [71%]). Similarly, high rates of good functional outcomes (mRS 0–2: 32/38 [84%]) and low mortality (2/38 [5%]) were observed.
Conclusion
Cyclical aspiration using the CLEARTM Aspiration System is safe, effective, and achieved a high TICI 3 FPE for large‐vessel strokes.
Keywords: blood clots, cyclical aspiration, device, stroke, thrombectomy
INTRODUCTION
Large‐vessel strokes have a poor natural history with a high mortality (41.9%) and low rate of good functional outcomes defined by the modified Rankin Scale (mRS) of 0–2 (mRS 0–2 [20.7%]). 1 Vessel reopening with complete distal territory reperfusion (TICI 3) in the first thrombectomy attempt, also known as the first pass effect (FPE), has become the top‐line metric for a successful thrombectomy in patients with large‐vessel strokes. 2 TICI 3 FPE is associated with the lowest mortality (mRS 6 [16.3%]) and the highest rates of functional independence (mRS 0–2 [61.3%]). 2 When multiple passes are required, rates of good outcome decline (final TICI 3 in multiple passes: mRS 6 [20.5%]; mRS 0–2 [55%]). Similarly, when incomplete reperfusion (TICI 2b) is achieved, outcomes can suffer (TICI 2b or greater on first pass: mRS 6 [31%]; mRS 0–2 [52.4%], and final TICI 2b or greater in multiple passes: mRS 6 [30.2%]; mRS 0–2 [44.3%]). 2
Although substantial technological improvements in endovascular therapy have been achieved since the initial studies in 2015, 3 TICI 3 FPE remains low at 24–30% for retrievable stents (North American solitaire stent retriever acute [NASA] stroke registry, 2 , 4 TREVO Stent‐Retriever acute Stroke registry [TRACK] registry, 5 Analysis of Revascularization in Ischemic Stroke with EmboTrap [ARISE] 2 study 6 ) or continuous uniform aspiration (continuous uniform aspiration arm of Aspiration versus Stent Retriever [ASTER], 7 , 8 Endovascular Treatment of Ischemic Stroke [ETIS] registry 9 ). More recently, it has been suggested that near‐complete reperfusion (TICI 2c) is associated with comparable good outcomes as TICI 3 Stroke Thrombectomy and Aneurysm Registry (STAR) registry. 10 A recent meta‐analysis has shown that FPE inclusive of near‐complete reperfusion (TICI 2c/3) is also low at 28% with existing mechanical thrombectomy devices. 11 There is clearly an unmet need for a novel mechanical thrombectomy device to improve the relatively low rate of TICI 2c/3 FPE seen with current retrievable stents or continuous uniform aspiration systems, 4 , 5 , 6 , 7 , 8 , 9 and thereby help achieve better outcomes in patients with large‐vessel strokes.
Preclinical results with a novel mechanical thrombectomy device that can generate cyclical aspiration, the CLEARTM Aspiration System (Insera Therapeutics Inc., Dallas, TX), have shown an improved safety profile, 12 and demonstrated that complete clot ingestion with cyclical aspiration also increases first pass recanalization and reduces distal embolization. 13 There is a need to understand how these preclinical results translate from the bench to the bedside. The authors aim to describe the clinical safety and efficacy profile for cyclical aspiration, using the CLEARTM Aspiration System, and its impact on TICI 2c and 3 FPE.
METHODS
Study design
A real‐world observational study was performed with retrospective analysis of a prospectively maintained registry at the local institution, the Cyclical, Luminal, Evacuation, Aspiration and Retrieval (CLEAR) registry. The prospective cohort in the CLEAR registry includes a consecutive series of patients who met the broad principles of patient selection criteria in the local institution and underwent cyclical aspiration thrombectomy in the stroke interventional lab at the local institution (University Hospital Center ‘Sestre Milosrdnice’, Zagreb, Croatia). Thrombectomy was performed using cyclical aspiration after Conformité Européenne (CE Mark) approval was obtained for the CLEARTM Aspiration System (Insera Therapeutics Inc.) in the European Union (EU). Approval was also obtained from the local institutional leadership/institutional review board. Informed consent prior to each thrombectomy procedure was obtained as required by the local institutional guidelines.
Population and patient selection
In this analysis (CLEAR‐1 cohort), a consecutive series of patients with large‐vessel strokes who met the broad principles of patient selection criteria in the local institution and underwent thrombectomy using cyclical aspiration were included. There were no patient selection criteria imposed and thrombectomy was performed as per the local institutional protocols. Broad principles for patient selection criteria for stroke thrombectomy at the local institution included: (1) clinical signs and symptoms consistent with the diagnosis of an acute ischemic stroke, (2) refractory to or ineligible for intravenous (IV) tissue plasminogen activator (r‐tPA) or thrombolytics, (3) no limitations according to age, (4) large‐vessel stroke patients with National Institute of Health Stroke Scale (NIHSS) of at least ≥4, (5) endovascular treatment initiated within 24 h from the time last seen well (TLSW) as per local institution protocol.
Broad principles for imaging selection criteria at the local institution included: (5) Alberta Stroke Program Early Computed Tomographic Score (ASPECTS) >5, (6) large‐vessel occlusion (LVO) of the internal carotid artery (ICA) or middle cerebral artery, anterior cerebral artery, posterior cerebral artery (PCA), basilar artery or vertebral artery identified on CT angiography, MR angiography, and/or confirmed on digital subtraction angiography (DSA).
Exclusion criteria at the local institution included: (1) evidence of intracranial hemorrhage on baseline CT/MRI, (2) history of severe allergy (more than rash) to contrast medium, and (3) any other condition that, in the opinion of the physician, precludes an endovascular procedure or poses a significant hazard to the patient if an endovascular procedure was performed.
The initial 20 patients (n = 20/40, 50.0%) in this cohort were treated in the pre‐Corona Virus Disease 2019 (COVID‐19) era wherein protocols similar to published consensus criteria for developing and maintaining a stroke interventional lab were followed. 14 The second half of this cohort (n = 20/40, 50.0%) in this cohort were treated during the COVID‐19 era wherein additional preparedness similar to several multisociety consensus recommendations were implemented. 15 , 16 , 17
Demographics, initial stroke severity, and stroke systems of care
Information on baseline demographics, NIHSS, IV r‐tPA use prior to thrombectomy (which was permitted as per local institutional protocol), large‐vessel stroke presentation direct to comprehensive stroke center (CSC) or via transfer to CSC, time from stroke onset (in witnessed strokes) or time from last seen well (in unwitnessed strokes) to skin puncture (groin or radial) in the early time window (defined as <6 h from TLSW, and/or endovascular treatment <8 h from stroke onset or TLSW) or extended time window (defined as outside the early time window and within 24 h from TLSW), and wake up stroke or not were obtained from the prospectively collected registry.
Procedural information
Cyclical aspiration was performed, using the CLEARTM Aspiration System (Insera Therapeutics Inc.) after CE Mark approval in the EU, on a consecutive series of large‐vessel stroke patients who met the patient selection criteria in the local institution during this CLEAR‐1 cohort period (n = 38). Further enrollment in this cohort was limited due to the December 2020 earthquake that affected Zagreb, Croatia, as well as the COVID‐related restrictions. CLEARTM is a digital smart vacuum aspiration system that can generate continuous uniform aspiration as well as cyclical or pulsatile or intermittent suction pattern, with a proprietary suction intensity and frequency, all within the safe suction range of 0 to −98.2 kPa (0 to −29 in Hg). The liquid crystal display screen on the vacuum source digitally displays the precise suction intensity in real‐time for the physicians. The CLEARTM Aspiration System can be activated remotely for thrombectomy via an iPad app (CLEARTM, CLEARTM Pro apps), in the control room or within the neuro‐interventional lab and communicates with the vacuum source using Bluetooth technology.
Standard commercially available aspiration catheters, medium and large‐bore aspiration catheters, balloon guide catheters, and guide catheters, with inner diameters (ID) ranging from 0.032” (0.81 mm) to 0.088” (2.24 mm), and outer diameters (OD) ranging from 3F to 9F (1.0–3.0 mm) that have CE Mark approval in the EU were used for access to the clot and were appropriately chosen by the treating physician based on each target vessel diameter.
In nearly half the patients (n = 17/38, 45%), there was good catheter access to the proximal face of the clot using standard techniques including direct “snaking” without microcatheter and microwire support, or catheterizing with a microwire and microcatheter and then tunneling the aspiration catheter over the microcatheter and microwire for support. Cyclical aspiration was directly performed. This is referred to as the PACE (Proximal Aspiration using Cyclical followed by Corking Embolectomy) technique. 12 , 13
In the rest of the patients (n = 21/38, 55%), there was difficulty in advancing the large‐bore aspiration catheter. This was related to excessive vessel tortuosity especially in the older population, for example, in several octogenarians and nonagenarians. This is not uncommon for current large‐bore aspiration catheters, with reported rates of nearly 25–40% of patients, having difficult catheter access. 18 In these patients, to avoid catheter herniation and improve catheter delivery to the clot, the active portion of a stent retriever is anchored distal to the clot and the retriever wire is used as a support to track and advance the large‐bore aspiration catheter to the proximal face of the clot (“grappling hook” technique). 18 Cyclical aspiration is then performed. This is also referred to as the ReWiSed (Retriever Wire Supported) PACE technique.
Procedural information regarding angiographic outcomes at the end of the procedure, the number of passes required, complete clot ingestion (wherein the clot is completely inside the catheter, tubing, or canister) or partial clot ingestion (wherein the clot is corked, partially inside the catheter and partially exposed outside the catheter), emboli to distal territory or emboli to new territory, any device‐related adverse events or intraprocedural complications, and whether clots were aspirated in a single piece or multiple pieces were obtained.
Imaging analysis
For early ischemic changes, the ASPECTS was measured on noncontrast‐enhanced CT head scans. For large‐vessel stroke clot locations, the specific LVO locations were confirmed on DSA and further grouped for ease of analysis into M1 (includes middle cerebral artery M1 segment), M2 (includes proximal middle cerebral artery M2 segment), M2/M3 (includes middle cerebral artery distal M2 with or without associated M3 segments), ICA (includes ICA T occlusions, tandem occlusions, extracranial, and/or intracranial carotid occlusions), and vertebrobasilar (includes the entire posterior circulation). For control imaging postprocedure, a noncontrast‐enhanced CT head scan (n = 32/38) or MRI brain scan (n = 1/38) was performed at 24 h (−6/+24) (n = 33/38, 87%) post‐thrombectomy as per local institutional protocol. Due to COVID‐19 and bed capacity issues, a few patients were transferred back to the initial referral facility once they were stable after the thrombectomy procedure. In these patients, a control noncontrast‐enhanced CT head was performed within 36 h (n = 5/38, 13%) post‐thrombectomy at the referral facility from where the patient was initially transferred from.
For reperfusion, the modified Thrombolysis in Ischemic Stroke (mTICI) 19 score (range, 0 [no perfusion], 1 [minimal flow past occlusion but no perfusion], 2a [minor partial reperfusion, <50%], 2b [major partial reperfusion, 50–89%], 2c [near complete reperfusion except for slow flow or distal emboli in a few cortical vessels, ≥90%], to 3 [full perfusion with filling of distal branches]), as well as the expanded TICI (eTICI) 20 scores were measured on DSA. The mTICI score is essentially similar to the eTICI score except that mTICI 2b (50–89% partial reperfusion) is further classified as eTICI 2b‐50 (50–66% partial reperfusion) and eTICI 2b‐67 (67–89% partial reperfusion). 19 , 20 The CT and angiographic images were adjudicated locally at treating facility. Baseline and procedural characteristics among the large‐vessel stroke patients with FPE having complete reperfusion (TICI 3) or near‐complete reperfusion (TICI 2c) compared to the non‐FPE cohort are shown in Table 1.
Table 1.
Baseline and procedural characteristics of the CLEAR‐1 first pass effect cohort
| First pass effect (TICI 2c or 3) | ||||
|---|---|---|---|---|
| Characteristic | CLEAR‐1 full cohort | Yes | No | p‐value |
| Baseline characteristics based on demographics and initial National Institute of Health Stroke Scale (NIHSS) | ||||
| Age (years): mean (±Standard Deviation) | 73.6 (±12.5 SD) | 75.3 (±11.1 SD) | 68.1 (±15.6 SD) | 0.13 |
| Women, n (%) | 25/38 (66%) | 18/29 (62%) | 7/9 (78%) | 0.69 |
| Initial NIHSS, median (IQR) | 15.5 (4–33) | 15 (4–33) | 17 (15–20) | 0.19 |
| Procedural characteristics based on large vessel occlusion site | ||||
| Anterior circulation, n (%) | 29/38 (76.3%) | 20/29 (69%) | 9/29 (31%) | 0.08 |
| Posterior circulation, n (%) | 9/38 (23.7%) | 9/9 (100%) | 0/9 (0%) | |
| Procedural characteristics based on aspiration catheter access to occlusion site (cyclical aspiration technique) | ||||
| Good catheter access to the clot (PACE) | 17/38 (45%) | 16/17 (94%) | 1/17 (6%) | 0.03* |
| Difficult catheter access to the clot (retriever wire supported PACE) | 21/38 (55%) | 13/21 (62%) | 8/21 (28%) | |
| Procedural characteristics based on comparison to FPE using existing devices from historical controls | ||||
| CLEAR‐1 (full cohort) | n = 38 | 29/38 (76%) | 9/38 (24%) | 0.0001* |
| Historical controls: meta‐analysis (2021) with existing devices (stent retrievers, continuous uniform aspiration, or combination) 11 | n = 9082 | 2440/9082 (28%, 95% CI: 26–32%) | 6642/9082 (72%, 95% CI: 68–74%) | |
Note: SD indicates standard deviation; IQR indicates interquartile range; n indicates sample size; CI indicates confidence interval; PACE technique indicates proximal aspiration using cyclical followed by corking embolectomy when there is good catheter access to the clot; ReWiSed PACE indicates retriever wire supported PACE when there is difficult catheter access to the proximal face of clot. A stent retriever is anchored distal to the clot and the retriever wire is used to track the aspiration catheter to the proximal face of the clot, cyclical aspiration is then performed; FPE indicates first pass effect; TICI indicates Thrombolysis in Cerebral Ischemia Score.19,20
Statistically significant (p‐value ≤0.05) using the Fisher Exact P test.
For recanalization, the Arterial Occlusive Lesion (AOL) scale was used to measure the degree of recanalization at the target arterial lesion. 19 Baseline and final angiographic images were core‐lab adjudicated based on the degree of luminal opening (none, partial, or complete) with further qualification based on the presence (grades 2 or 3) or absence (grades 0 or 1) of any downstream flow. 19
To compare angiographic outcomes of the CLEAR‐1 cohort with those of recent registries or trials of current retrievable stents or continuous uniform aspiration systems in anterior circulation strokes, 3 , 21 , 22 an angiographic analysis of all the anterior circulation strokes (n = 29/38, 76.3%) in the CLEAR‐1 cohort was performed by an independent core lab. Blinded core lab‐adjudication was done using the mTICI, 19 and the eTICI scores in patients with anterior circulation occlusions, consistent with prior studies. 20
Outcome measures
In this analysis, the primary outcome is the “first pass effect” (FPE) which includes angiographic outcomes of complete (TICI 3), near‐complete (TICI 2c), or partial vessel reopening (TICI 2b, also called modified FPE) in the first operative thrombectomy attempt. 2
The secondary outcomes include (1) angiographic outcomes: (a) proportion of patients with “successful revascularization” (percentages) post procedure by angiographic measurement of complete (final TICI 3), near‐complete (final TICI 2c), or partial reperfusion (final TICI 2b) in one or more operative thrombectomy attempts, (b) vessel recanalization rates (percentages) post procedure by angiographic measurement of the AOL score; (2) clinical outcomes based on “early neurological improvement” on the NIHSS at 24 (−6/+24) h post‐procedure, and/or at day 5–7/discharge (whichever is earlier), defined as an improvement of NIHSS of ≥4 points (mild), 9 or of ≥8 points (moderate), 21 or of ≥10 points (dramatic) from baseline, 22 or improvement to an NIHSS of 0 or 1; 9 , 21 , 22 (3) safety outcomes: (a) incidence of symptomatic intracerebral hemorrhage associated with neurological deterioration of ≥4 points on the NIHSS score from the baseline score or asymptomatic intracerebral hemorrhage, 22 , 23 defined as any intracerebral hemorrhage within 24 (−6/+24) h post procedure, (b) incidence of device‐related serious adverse events through 24 (−6/+24) h post procedure; 22 and (4) functional outcomes based on mRS at day 5–7/discharge (whichever is earlier), at 30 and 90 days with good functional outcome defined as mRS score of 0–2. Early neurological improvement and functional outcomes during the hospitalization were assessed directly by the treating physician and team. Functional outcomes at 30 and 90 days were assessed indirectly through chart review, telephone, or feedback from referring physician. In this analysis, all missing 30‐ or 90‐day mRS values were imputed by last observation carried forward as performed in previous trials. 24
Statistical analysis
The population's mean (standard deviation [SD]), median (interquartile range [IQR]), and dispersion characteristics are described as appropriate. Descriptive statistics were used for demographics, initial stroke severity, procedural information, and outcomes (primary and secondary). Comparison of the baseline and procedural characteristics between the FPE and non‐FPE groups for mean data were evaluated using the unpaired, 2‐tailed t test, median data using the Mann–Whitney U test, and categorical variables using the Fisher's Exact P test for proportions where appropriate (p≤0.05 was considered significant). All analyses were performed using the SPSS Statistics software package (SPSS Inc., Chicago, IL).
RESULTS
A total of 40 patients underwent cyclical aspiration thrombectomy, of whom 38 patients had large‐vessel strokes (13/38 men [34%]; 25/38 women [66%]; mean [SD] age, 73.6 [12.5] years; median [IQR] age, 75 [31–96] years) and were included in this analysis. Two patients had clots successfully removed from the peripheral vasculature (one patient with bilateral submassive pulmonary embolism from venous thrombus; and one patient with limb ischemia from arterial thrombus) and were not included in this analysis.
Demographics and baseline characteristics
Full demographics of the CLEAR‐1 cohort are provided in Table 1. The CLEAR‐1 cohort included a large number of elderly patients. The mean age was 73.6 ± 12.5 years; 66% (25/38) were female; and the median NIHSS was 15.5 (IQR 4–33).
Large‐vessel stroke presentation direct to the CSC or mothership was observed in less than half (16/38, 42%) of the patients in this CLEAR‐1 cohort and the rest (22/38, 58%) were via transfers from the regional stroke network. The time from stroke onset to skin puncture (femoral or radial) was in the early time window for nearly 2/3rd of the patients (25/38, 66%) and in the extended time window for the rest. Site of vascular access was femoral in all the patients (38/38, 100%) in the CLEAR‐1 cohort, although more recently the local institution has also successfully launched their radial access program. IV r‐tPA use prior to thrombectomy was observed in a small proportion of large‐vessel stroke patients (4/38, 10.5%) because the local institution protocol was similar to a direct to mechanical thrombectomy (Direct‐MT) 25 approach when available and appropriate.
LVOs in the anterior circulation accounted for 76.3% (29/38) and the rest 23.7% (9/38) were in the posterior circulation. The location of the large vessel occlusion sites in the anterior circulation treated with cyclical aspiration were M1 in 31.6% (12/38), proximal M2 in 10.5% (4/38), M2/M3 5.3% (2/38), and ICA in 28.9% (11/38). Among the ICA occlusions, the location of LVOs were intracranial ICA in 10.5% (4/38), extracranial ICA in 2.6% (1/38), and tandem ICA occlusions in 15.8% (6/38). The median baseline ASPECTS was 9 (IQR 6–10).
The location of the large vessel occlusion sites in the posterior circulation were vertebral in 2.6% (1/38), basilar in 18.4% (7/38), and PCA in 2.6% (1/38). The median baseline posterior circulation (pc) ASPECTS was 10 (IQR 6–10).
Revascularization: Entire cohort (anterior and posterior circulation strokes)
The number of thrombectomy attempts in the CLEAR‐1 cohort was one pass in 30/38 (79%) patients, and multiple (2–5) passes in 8/38 (21%) patients. The median number of thrombectomy attempts was 1 (IQR 1–5).
Successful recanalization using cyclical aspiration in the first operative attempt was achieved in majority of the patients (AOL score 3 on first pass: 30/38, 78.9%), and successful recanalization after all attempts was achieved in the entire cohort (final AOL score 3: 38/38, 100%).
The rate of successful reperfusion after the first cyclical aspiration attempt, the FPE, was high: complete reperfusion (TICI 3 FPE) in 68.4% (26/38), near‐complete reperfusion (TICI 2c/3 FPE) in 76.3% (29/38), and substantial reperfusion (TICI 2b‐67/3 FPE) in 78.9% (30/38) (Figure 1A). Comparator studies for endovascular stroke therapy using retrievable stents (NASA registry, 2 , 4 TRACK registry, 5 ARISE 2 study 6 ) or using continuous uniform aspiration (continuous uniform aspiration arm of ASTER, 7 , 8 ETIS registry 9 ), wherein the TICI 3 FPE rates have been published, are shown in Figure 1A. Final revascularization results for the entire cohort (in one or multiple attempts) were TICI 3 in 86.8% (33/38), TICI 2c/3 in 94.7% (36/38), TICI 2b‐67/3 in 97.4% (37/38), and TICI 2b/3 in 100% (38/38).
FIGURE 1.
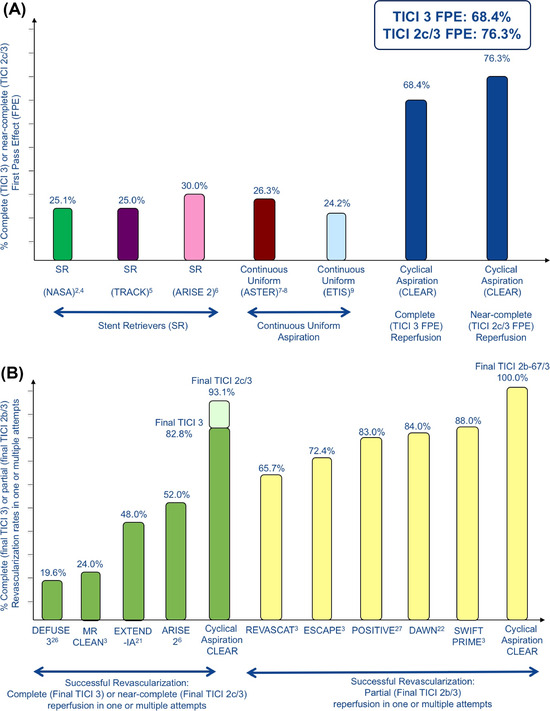
(A) Cyclical aspiration is associated with a high TICI 3 first pass effect (TICI 3 FPE). In the CLEAR‐1 cohort, the first pass effect using cyclical aspiration was high with complete reperfusion (TICI 3 FPE: 26/38 [68.4%]), and near‐complete reperfusion (TICI 2c/3 FPE: 29/38 [76.3%]). CLEAR indicates this Cyclical, Luminal, Evacuation, Aspiration, and Retrieval cohort; NASA indicates North American Solitaire Stent retriever Acute stroke registry; 2 , 4 TRACK indicates TREVO Stent‐Retriever acute Stroke registry; 5 ARISE II indicates Analysis of Revascularization in Ischemic Stroke with EmboTrap study; 6 ASTER indicates the continuous uniform aspiration arm of the Aspiration versus Stent Retriever trial; 7 , 8 ETIS indicates the Sofia aspiration thrombectomy approach within the Endovascular Treatment of Ischemic Stroke registry; 9 TICI indicates the Thrombolysis in Cerebral Ischemia Score; 19 , 20 TICI 3 FPE indicates complete reperfusion in the first operative attempt or first pass effect; 2 TICI 2c/3 FPE indicates near‐complete reperfusion in the first operative attempt or first pass effect. 11 (B) Comparing successful revascularization rates in anterior circulation strokes. Among anterior circulation strokes, core lab‐adjudicated final successful revascularization rates (in one or multiple attempts) were also high with complete reperfusion (final TICI 3: 24/29 [82.8%]), near‐complete reperfusion (final TICI 2c/3: 27/29 [93.1%]), and substantial reperfusion (final TICI 2b‐67/3: 29/29 [100%]). CLEAR indicates this Cyclical, Luminal, Evacuation, Aspiration, and Retrieval cohort; MR‐CLEAN indicates a Multicenter Randomized Clinical Trial of Endovascular Treatment of Acute Ischemic Stroke in the Netherlands; 3 EXTEND‐IA indicates Extending the Time for Thrombolysis in Emergency Neurological Deficits – Intra‐Arterial trial; 21 DEFUSE 3 indicates Endovascular therapy following imaging evaluation for ischemic stroke 3 study; 26 ARISE 2 indicates Analysis of Revascularization in Ischemic Stroke with EmboTrap study; 6 ESCAPE indicates Endovascular Treatment for Small Core and Proximal Occlusion Ischemic Stroke trial; 3 SWIFT‐PRIME indicates Solitaire With the Intention for Thrombectomy as Primary Endovascular Treatment trial; 24 REVASCAT indicates Randomized Trial of Revascularization with Solitaire FR Device versus Best Medical Therapy in the Treatment of Acute Stroke Due to Anterior Circulation Large Vessel Occlusion Presenting within Eight Hours of Symptom Onset trial; 3 DAWN indicates Diffusion‐weighted imaging or CT perfusion Assessment with clinical mismatch in the triage of Wake‐up and late presenting strokes undergoing Neurointervention with Trevo trial; 22 POSITIVE indicates Perfusion Imaging Selection of Ischemic Stroke Patients for Endovascular Therapy trial; 27 and TICI indicates the Thrombolysis in Cerebral Ischemia Score. 19 , 20 Comparator studies for endovascular stroke therapy for anterior circulation strokes wherein final successful revascularization (in one or multiple attempts) with complete reperfusion (final TICI 3: MR‐CLEAN, 3 EXTEND‐IA, 21 DEFUSE 3, 26 ARISE 2 6 ), and partial reperfusion (final TICI 2b/3: ESCAPE, 3 SWIFT‐PRIME, 24 REVASCAT, 3 DAWN,22 POSITIVE 27 ) rates have been published and are shown in B
Core lab‐adjudicated reperfusion: Anterior circulation strokes
The rate of core lab‐adjudicated FPE remained high for anterior circulation strokes: complete reperfusion (TICI 3 FPE) in 58.6% (17/29), near‐complete reperfusion (TICI 2c/3 FPE) in 69.0% (20/29), and substantial reperfusion (TICI 2b‐67/3 FPE) in 72.4% (21/29) (Figure 1B). Final revascularization results (in one or multiple attempts) were TICI 3 in 82.8% (24/29), TICI 2c/3 in 93.1% (27/29), and TICI 2b‐67/3 in 100% (29/29) (Figure 1B). Comparator studies for endovascular stroke therapy for anterior circulation LVOs wherein final revascularization (in one or multiple attempts) with complete reperfusion (TICI 3: Multicenter Randomized Clinical Trial of Endovascular Treatment of Acute Ischemic Stroke in the Netherlands [MR‐CLEAN], 3 Extending the Time for Thrombolysis in Emergency Neurological Deficits – Intra‐Arterial trial [EXTEND‐IA], 21 Endovascular therapy following imaging evaluation for ischemic stroke 3 [DEFUSE 3] 26 ), and partial reperfusion (TICI 2b/3: Endovascular Treatment for Small Core and Proximal Occlusion Ischemic Stroke trial [ESCAPE], 3 Solitaire With the Intention for Thrombectomy as Primary Endovascular Treatment trial [SWIFT‐PRIME], 24 Randomized Trial of Revascularization with Solitaire FR Device versus Best Medical Therapy in the Treatment of Acute Stroke Due to Anterior Circulation Large Vessel Occlusion Presenting within Eight Hours of Symptom Onset trial [REVASCAT], 3 Diffusion‐weighted imaging or CT perfusion Assessment with clinical mismatch in the triage of Wake‐up and late presenting strokes undergoing Neurointervention with Trevo trial [DAWN], 22 Perfusion Imaging Selection of Ischemic Stroke Patients for Endovascular Therapy trial [POSITIVE] 27 ) rates have been published and are shown in Figure 1B. A coded system can help graphically better visualize mTICI or eTICI outcome distributions. 28 Figure 2A shows a similar coded system or tool to better visualize revascularization rates. 28
FIGURE 2.
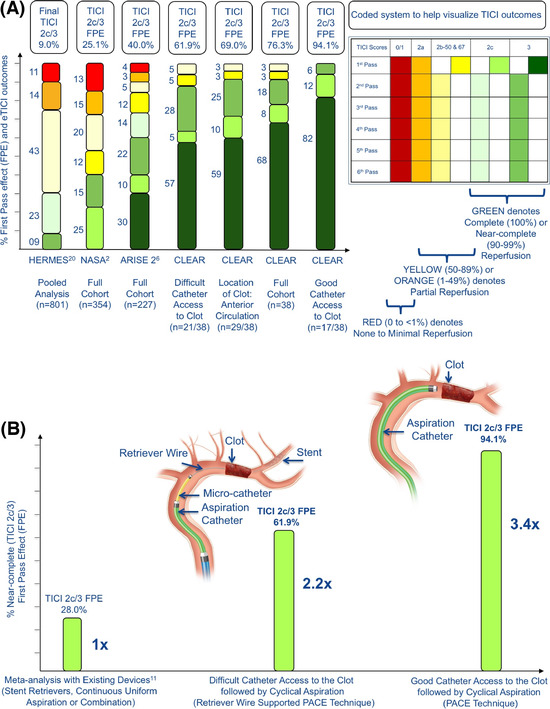
(A) Comparing revascularization rates relative to location and catheter access to clot. A novel coded system or tool to help better visualize reperfusion rates with respect to one or multiple operative attempts or passes is shown, wherein broadly green signifies complete (TICI 3, 100%) or near‐complete (TICI 2c, 90–99%) reperfusion, yellow (TICI 2b‐50 and 2b‐67, 50–89%) and orange (TICI 2a, 1–49%) signify partial reperfusion, and red signifies trickle of flow (TICI 1, <1%) or no (TICI 0, 0%) reperfusion. n indicates sample size. CLEAR indicates this Cyclical, Luminal, Evacuation, Aspiration, and Retrieval cohort. The complete (dark green) or near complete (parrot green) first pass effect (TICI 2c/3 FPE) is high in the CLEAR‐1 cohort and its subgroups based on location and catheter access to clot. HERMES indicates a pooled analysis of seven (7) endovascular stroke trials, Highly Effective Reperfusion Evaluation in Multiple Endovascular Stroke trials; 20 NASA indicates North American Solitaire Stent retriever Acute stroke registry; 2 ARISE II indicates Analysis of Revascularization in Ischemic Stroke with EmboTrap study. 6 (B) Comparing first pass effect with cyclical aspiration relative to the ease or difficulty in catheter access to the proximal face of the clot. A recent meta‐analysis comprising 16,870 patients has shown that with existing thrombectomy devices, the complete or near‐complete first pass effect is low (TICI 2c/3 FPE: 28%). 11 CLEAR indicates this Cyclical, Luminal, Evacuation, Aspiration, and Retrieval cohort; PACE indicates Proximal Aspiration using Cyclical followed by Corking Embolectomy technique; 12 , 13 ReWiSed PACE indicates Retriever Wire Supported PACE technique; 18 , 29 TICI indicates the Thrombolysis in Cerebral Ischemia Score. 19 , 20 In the CLEAR‐1 cohort, among patients with difficult catheter access to the clot, the active component of a stent retriever is anchored distal to the clot and the retriever wire is used to track the large‐bore aspiration catheter to the proximal face of the clot, like a “grappling hook.” 18 Cyclical aspiration is then performed, also known as ReWiSed PACE technique, 29 with a high first pass effect (approximately two‐fold higher). 11 Among patients with ease of catheter access to the clot, cyclical aspiration is directly performed, also known as PACE technique, 12 , 13 with a much higher first pass effect (3.4‐fold higher than the recent meta‐analysis) 11
Reperfusion: Catheter access to proximal face of clot
Figure 2B shows the reperfusion rates in this CLEAR‐1 cohort relative to the ease or difficulty in accessing the proximal face of the clot compared to the recent meta‐analysis of existing devices. In nearly half the patients (n = 21/38, 55%), the stent part of a stent retriever is anchored distal to the clot and the retriever wire is used as a support to track and advance the large‐bore aspiration catheter to the proximal face of the clot, like a “grappling hook.” 18 Cyclical aspiration is then performed, also known as ReWiSed PACE technique, 29 with a high FPE (TICI 2c/3 FPE: 13/21, 61.9%).
In the rest of the patients (n = 17/38, 45%), there was good catheter access to the proximal face of the clot using a microwire and microcatheter or direct catheter access. Cyclical aspiration is directly performed, also known as PACE technique, 12 , 13 with much higher FPE (TICI 2c/3 FPE: 16/17, 94.1%).
Figure 3 shows a sampling of large‐vessel stroke patients treated using cyclical aspiration from the CLEAR‐1 cohort.
FIGURE 3.
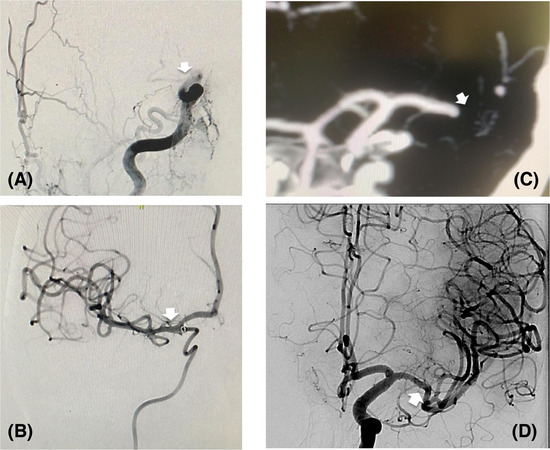
Sampling of large‐vessel stroke patients treated using cyclical aspiration. (A). Baseline digital subtraction angiogram (DSA) in the anterior‐posterior (AP) projection in a 71‐year‐old gentleman in the early time window with a moderate to severe stroke with the National Institutes of Health Stroke Scale (NIHSS) of 15 due to a clot causing a right internal carotid artery (ICA‐T) occlusion (see white arrow in Panel A). TICI indicates the Thrombolysis in Cerebral Ischemia Score. 19 , 20 (B) Right ICA‐T clot ingested using cyclical aspiration (CLEARTM Aspiration System, Insera Therapeutics). Post‐treatment DSA (AP projection) showing TICI 3 first pass effect (TICI 3 FPE) (see white arrow in Panel B). (C) Baseline CT angiogram (AP projection) in a 74‐year‐old lady in the early time window with a severe stroke (NIHSS 20) due to a left middle cerebral artery (M1) clot (see white arrow in Panel C). (D) Left M1 clot ingested using cyclical aspiration (CLEARTM Aspiration System, Insera Therapeutics). Post‐treatment DSA (AP projection) showing TICI 3 FPE (see white arrow in Panel D)
Clinical outcomes
Early neurological improvement was mild (NIHSS ≥4 improvement or an improvement to a score of 0 or 1) in 92.1% (35/38) at 24 h (at discharge [36/38, 94.7%]); moderate (NIHSS ≥8 improvement or improvement to a score of 0 or 1) in 73.7% (28/38) at 24 h (at discharge [35/38, 92.1%]); and dramatic (NIHSS ≥10 improvement or an improvement to a score of 0 or 1) in 71.0% (27/38) at 24 h (at discharge [31/38, 81.6%]). Figure 4A–C shows comparative results from other studies.
FIGURE 4.
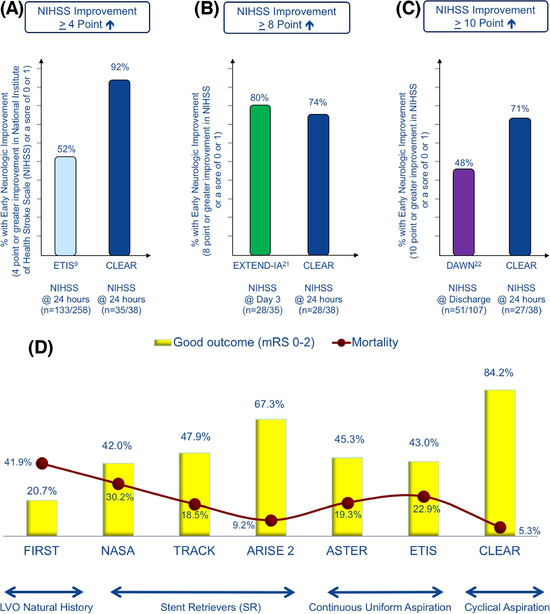
(A–C) Cyclical aspiration is associated with early neurological improvement during hospitalization. (A–C). Early neurological improvement using the National Institutes of Health Stroke Scale (NIHSS) at 24 h post‐thrombectomy procedure (mild improvement of NIHSS≥4 points: 92.1%; moderate improvement of NIHSS≥8 points: 73.7%; dramatic improvement of NIHSS≥10 points: 71.0%) was observed. n indicates sample size. CLEAR indicates this Cyclical, Luminal, Evacuation, Aspiration, and Retrieval cohort; ETIS indicates Sofia aspiration thrombectomy approach within the Endovascular Treatment of Ischemic Stroke registry; 9 EXTEND‐IA indicates Extending the Time for Thrombolysis in Emergency Neurological Deficits – Intra‐Arterial trial; 21 DAWN indicates Diffusion‐weighted imaging or CT perfusion Assessment with clinical mismatch in the triage of Wake‐up and late presenting strokes undergoing Neurointervention with Trevo trial. 22 (D) Cyclical aspiration is associated with improved functional outcomes (mRS 0–2) and lower mortality (mRS 6). mRS indicates score on the modified Rankin Scale. CLEAR indicates this Cyclical, Luminal, Evacuation, Aspiration, and Retrieval cohort; FIRST indicates Functional Improvement and Recovery after Stroke study; 1 LVO indicates large vessel occlusion; *data graphically shown are mRS at 90 days; NASA indicates North American Solitaire Stent retriever Acute stroke registry; 2 , 4 TRACK indicates TREVO Stent‐Retriever acute Stroke registry; 5 ARISE II indicates Analysis of Revascularization in Ischemic Stroke with EmboTrap study; 6 ASTER indicates the continuous uniform aspiration arm of the Aspiration versus Stent Retriever trial; 7 , 8 ETIS indicates the Sofia aspiration thrombectomy approach within the Endovascular Treatment of Ischemic Stroke registry 9
Functional outcomes were available in all patients at time of discharge and at 30 days. The rate of good outcomes (mRS 0–2) was 81.6% (31/38) at discharge. Outcomes were available in 35/38 patients at 90 days. Follow‐up was not possible for three patients treated due to the 2020 earthquake that affected Zagreb, Croatia, as well as COVID‐19 restrictions. In this analysis, the missing mRS values were imputed by last observation carried forward as performed in previous trials, 24 and based on that two out of the three patients had a last observation of mRS 0–2 (32/38, [84.2%]) (Figures 4D and 5).
FIGURE 5.
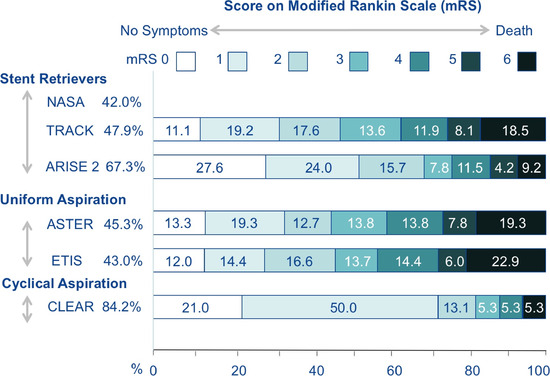
High rate of good functional outcomes (mRS 0–2) with cyclical aspiration. mRS indicates modified Rankin Scale; CLEAR (mRS 0–2: 84.2%) indicates this Cyclical, Luminal, Evacuation, Aspiration, and Retrieval cohort; NASA (mRS 0–2: 42%) indicates North American Solitaire Stent retriever Acute stroke registry; 2 , 4 TRACK (mRS 0–2: 47.9%) indicates TREVO Stent‐Retriever acute Stroke registry; 5 ARISE II (mRS 0–2: 67.3%) indicates Analysis of Revascularization in Ischemic Stroke with EmboTrap study; 6 ASTER (mRS 0–2: 45.3%) indicates the continuous uniform aspiration arm of the Aspiration versus Stent Retriever trial; 7 , 8 ETIS (mRS 0–2: 43%) indicates the Sofia aspiration thrombectomy approach within the Endovascular Treatment of Ischemic Stroke registry; 9 *mRS distribution graphically shown is mRS at 90 days
Safety outcomes
There were no symptomatic intracerebral hemorrhages observed. There were also no device‐related serious adverse events in the CLEAR‐1 cohort. There were six patients with asymptomatic intracerebral hemorrhages (6/38, 15.8%).
There was no mortality at the time of discharge. Cyclical aspiration was associated with a low all‐cause mortality at 30 and 90 days (both 5.3% [2/38]).
DISCUSSION
The primary finding of the CLEAR‐1 cohort is the extremely high FPE rate associated with cyclical aspiration (TICI 3 FPE: 68.4% and TICI 2c/3 FPE: 76.3%). This further resulted in a high rate of dramatic early neurological improvement, excellent safety outcomes, low mortality, and an approximately 80% rate of 90‐day functional independence (mRS 0–2).
Complete reperfusion after the first pass (TICI 3 FPE) is the top‐line metric for stroke thrombectomy as it has been shown to be associated with the lowest mortality (mRS 6: 16.3%) and the best functional outcomes (mRS 0–2: 61.3%), compared to other angiographic metrics. 2 However, published rates of TICI 3 FPE are low (24–30%) for retrievable stents (NASA registry [25.1%], 2 TRACK registry [25%], 4 ARISE 2 study [30%] 5 ) or continuous uniform aspiration (continuous uniform aspiration arm of ASTER [26.3%], 7 , 8 ETIS registry [24.2%] 9 ). More recently, it has been suggested that near‐complete reperfusion (TICI 2c) is associated with comparable good outcomes as TICI 3 (STAR registry 10 ). A recent meta‐analysis has shown that FPE inclusive of near‐complete reperfusion (TICI 2c/3) is also low at 28% with existing mechanical thrombectomy devices. 11 The present CLEAR‐1 findings suggest that TICI 3 FPE and TICI 2c/3 FPE can be dramatically improved using cyclical aspiration.
The site‐adjudicated results of the entire cohort (combined anterior and posterior circulation strokes) were mirrored by the core lab review of the anterior circulation subgroup, core lab‐adjudicated FPE for anterior circulation thrombectomy remained high for both complete reperfusion (TICI 3 FPE: 58.6%) and near‐complete reperfusion (TICI 2c/3 FPE: 69%). The rate of final successful revascularization (in one or multiple attempts) was high for complete reperfusion (final TICI 3: 82.8%), or near‐complete reperfusion (final TICI 2c/3: 93.1%), compared to landmark trials (final TICI 3: DEFUSE 3 [19.6%], 26 MR‐CLEAN [24.0%], 3 EXTEND‐IA [48.0%], 21 ARISE 2 [52.0] 6 ) (Figure 1B). With regard to final substantial reperfusion in CLEAR‐1 (final TICI 2b‐67/3: 100%), the results also compared favorably to other landmark trials of endovascular stroke therapy for anterior circulation LVOs (final TICI 2b/3: REVASCAT [65.7%], 3 ESCAPE [72.4%], 3 POSITIVE [83.0%], 27 DAWN [84.0%],22 SWIFT‐PRIME [88.0%] 24 ) (Figure 1B).
Owing to the high proportion of elderly patients (age ≥80 years [34.2%] in the CLEAR‐1 cohort), there was a substantial number of cases with difficult catheter access to the clot requiring adjunctive stent retriever‐assisted delivery of the aspiration catheter. In these patients, a stent retriever was anchored distal to the clot and the retriever wire was used to track the aspiration catheter to the proximal face of the clot. 18 , 29 Cyclical aspiration was then performed resulting in an approximately two‐fold higher rate of TICI 2c/3 FPE compared to a recent meta‐analysis of stent retrievers and continuous uniform aspiration (61.9% vs. 28%). In patients with good catheter access to the clot, cyclical aspiration resulted in an approximately 3.5‐fold higher rate of TICI 2c/3 FPE (94.1% vs. 28%) than the recent meta‐analysis. 11
The reduced rate of first pass success in patients with difficult catheter access to the clot may be related to the retriever wire and/or the microcatheter, which remain in place during cyclical aspiration. This wire and/or the microcatheter can decrease the luminal inner diameter of the large‐bore aspiration catheter and limit the aspiration force. In addition, the active component of the stent retriever might cause vessel wall injury 12 , 30 , 31 or clot fragmentation, 13 , 32 , 33 requiring multiple passes (multiple passes in the difficult catheter access group: 7/21 [33.3%] compared to the good catheter access group: 1/17 [5.9%]). This observation suggests that improvements in aspiration catheter trackability may augment the efficiency of aspiration thrombectomy.
The potential mechanisms underlying the improved clot ingestion and TICI 3 FPE associated with cyclical aspiration include a triad of fluid dynamics principles that may affect the visco‐elastic behavior of the clot: (1) Improving Dimensional Fit. An oscillating pattern of aspiration (i.e., cyclical aspiration) may allow for dynamic stretching of the clot (within the elastic limits) that can decrease the OD of the clot to become dimensionally a closer fit to the ID of the aspiration catheter. This may help to promote complete clot ingestion by improving the dimensional fit and reducing clot fragmentation by staying within the elastic limits; 13 , 34 , 35 (2) Reducing Frictional Forces. Dynamic or kinetic friction is less than static friction. 36 Once the clot becomes lodged in the catheter tip (corked) under static or continuous uniform aspiration, the static friction may be too difficult to overcome with aspiration. However, the oscillations associated with cyclical aspiration may help to dynamically stretch the clot and allow complete ingestion under conditions of kinetic friction rather than partial corking of the clot at the catheter tip; 13 (3) Improving Lubrication via Micro‐fluid flow. Another potential explanation is that when the clot enters the catheter tip, there are micro‐fluid channels of retrograde blood flow into the catheter (between the clot OD and catheter ID) that may help further ingest the clot into the catheter during a cyclical or pulsating pattern of aspiration acting as a sort of lubrication. This may be one of the reasons for the increased clot ingestion length observed with cyclical aspiration compared to static or continuous uniform aspiration. 13
With the mounting preclinical evidence in favor of cyclical aspiration, 12 , 13 , 30 , 31 , 35 , 37 the strengths of the CLEAR‐1 cohort include it being the first clinical experience of cyclical aspiration for large‐vessel strokes using the CLEARTM Aspiration System. The most demanding metric for stroke thrombectomy namely FPE (TICI 3 FPE and TICI 2c/3 FPE) was used as the primary outcome measure. 2 The results in the anterior circulation subgroup were confirmed by core lab‐adjudication. Importantly, cyclical aspiration was performed using standard commercially available aspiration catheters that have CE mark approval in the EU, allowing for direct comparison with previous studies of continuous uniform aspiration. Further analysis of the CLEAR‐1 cohort will provide invaluable information on what is the most cyclical friendly aspiration catheter (based on design and size) to pair with the CLEARTM Aspiration System for optimal clot ingestion either among the existing pool of approved catheters or the need for the development of newer customized catheters. One of the limitations of this analysis is that the primary and secondary outcomes from the CLEAR‐1 cohort were compared against published historical controls. Further analysis of the CLEAR‐1 cohort (treatment group) using propensity score matching with an LVO cohort of best medical therapy (control group) will be invaluable in the future.
The clinical implications of the findings in the CLEAR‐1 cohort are highly relevant to the unmet need in improving access to stroke thrombectomy worldwide. The ability to activate and have direct control of cyclical vacuum aspiration remotely via an iPad app during stroke thrombectomy 37 could pave the way for robotic or remote stroke thrombectomy in the future.
Cyclical aspiration using the CLEARTM Aspiration System is safe and effective, and achieves an exceedingly high rate of TICI 3 FPE for large‐vessel strokes compared to stent retrievers and aspiration using continuous uniform aspiration.
ACKNOWLEDGMENTS AND DISCLOSURE
Dr. Vallabh Janardhan reports grants from National Science Foundation, other from Insera Therapeutics, Inc., other from Society of Vascular & Interventional Neurology (SVIN), outside the submitted work. In addition, Dr. Janardhan has patents with the United States Patent and Trademark Office (USPTO), over 12+ patents pending, and 70+ USPTO and worldwide patents issued or allowed. Dr. Vikram Janardhan reports grants from National Science Foundation, other from Insera Therapeutics, Inc., outside the submitted work. In addition, Dr. Janardhan has over 12+ patents pending, and 70+ USPTO and worldwide patents issued or allowed. Dr. Vladimir Kalousek reports other from Balt, other from Microvention‐Terumo, outside the submitted work. Dr. Albert J Yoo reports grants from Medtronic, Cerenovus, Penumbra, Stryker, other from Penumbra, Cerenovus, and Insera Therapeutics, outside the submitted work. Dr. Sheth reports grants from the National Institutes of Health, American Academy of Neurology and Society for Vascular and Interventional Neurology, other from Penumbra, and Cerenovus, outside the submitted work. Josip Mamic has nothing to disclose pertinent to this work. The preclinical testing was funded in part by the National Science Foundation (NSF Award: 1819491, Principal Investigator: Vallabh Janardhan, MD).
Kalousek V, Yoo AJ, Sheth SA, Janardhan V, Mamic J, Janardhan V. Cyclical aspiration using a novel mechanical thrombectomy device is associated with a high TICI 3 first pass effect in large‐vessel strokes. J Neuroimaging. 2021;31:912–924. 10.1111/jon.12889
REFERENCES
- 1. Janardhan V, Venizelos A, Gianatasio RM, et al. Abstract W MP8: the natural history of acute stroke from large vessel proximal occlusion: a comparison with the IMS III patients. Stroke 2014;45:AWMP8. [Google Scholar]
- 2. Zaidat OO, Castonguay AC, Linfante I, et al. First pass effect: a new measure for stroke thrombectomy devices. Stroke 2018;49:660‐6. [DOI] [PubMed] [Google Scholar]
- 3. Ding D. Endovascular mechanical thrombectomy for acute ischemic stroke: a new standard of care. J Stroke 2015;17:123‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zaidat OO, Castonguay AC, Gupta R, et al. North American Solitaire Stent Retriever Acute (NASA) Stroke Registry: post‐marketing revascularization and clinical outcome results. J Neurointerv Surg 2018;10:i45‐9. [DOI] [PubMed] [Google Scholar]
- 5. Zaidat OO, Castonguay AC, Nogueira RG, et al. TREVO stent‐retriever mechanical thrombectomy for acute ischemic stroke secondary to large vessel occlusion registry. J Neurointerv Surg 2018;10:516‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zaidat OO, Bozorgchami H, Ribo M, et al. Primary results of the multicenter ARISE II study (analysis of revascularization in ischemic stroke with embotrap). Stroke 2018;49:1107‐15. [DOI] [PubMed] [Google Scholar]
- 7. Ducroux C, Piotin M, Gory B, et al. First pass effect with contact aspiration and stent retrievers in the aspiration versus stent retriever (ASTER) trial. J Neurointerv Surg 2020;12:386‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lapergue B, Blanc R, Gory B, et al. Effect of endovascular contact aspiration vs stent retriever on revascularization in patients with acute ischemic stroke and large vessel occlusion. The ASTER randomized clinical trial. JAMA 2017;318:443‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Marnat G, Barreau X, Detraz L, et al. First‐line sofia aspiration thrombectomy approach within the endovascular treatment of ischemic stroke (ETIS) multicentric registry: efficacy, safety, and predictive factors of success. AJNR Am J Neuroradiol 2019;40:1006‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chen C‐J, Chalhoub R, Ding D, et al. Is a picture‐perfect thrombectomy necessary in acute ischemic stroke? J Neurointerv Surg 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Abbasi M, Liu Y, Fitzgerald S, et al. Systematic review and meta‐analysis of current rates of first pass effect by thrombectomy technique and associations with clinical outcomes. J Neurointerv Surg 2021;13:212‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kadirvel R, Dai D, Brinjikji W, Kallmes DF. Cyclical aspiration has an improved safety profile compared to continuous uniform aspiration: in‐vivo randomized study. Paper presented at: 12th Annual Meeting of the Society of Vascular & Interventional Neurology; 2019; Atlanta, Georgia.
- 13. Arslanian RA, Marosfoi M, Caroff J, et al. Complete clot ingestion with cyclical ADAPT increases first‐pass recanalization and reduces distal embolization. J Neurointerv Surg 2019;11:931‐6. [DOI] [PubMed] [Google Scholar]
- 14. Shams T, Zaidat O, Yavagal D, Xavier A, Jovin T, Janardhan V. Society of Vascular and Interventional Neurology (SVIN) Stroke Interventional Laboratory Consensus (SILC) criteria: a 7M management approach to developing a stroke interventional laboratory in the era of stroke thrombectomy for large vessel occlusions. Interv Neurol 2016;5:1‐28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Nguyen TN, Abdalkader M, Jovin TG, et al. Mechanical thrombectomy in the era of the COVID‐19 pandemic: emergency preparedness for neuroscience teams – a guidance statement from the Society of Vascular and Interventional Neurology. Stroke 2020;51:1896‐901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fraser JF, Arthur AS, Chen M, et al. Society of Neurointerventional Surgery recommendations for the care of emergent neurointerventional patients in the setting of COVID‐19. J Neurointerv Surg 2020;12:539‐41. [DOI] [PubMed] [Google Scholar]
- 17. Aggour M, White P, Kulcsar Z, Fiehler J, Brouwer P. European Society of Minimally Invasive Neurological Therapy (ESMINT) recommendations for optimal interventional neurovascular management in the COVID‐19 era. J Neurointervent Surg 2020;12:542‐4. [DOI] [PubMed] [Google Scholar]
- 18. Boisseau W, Escalard S, Fahed R, et al. Direct aspiration stroke thrombectomy: a comprehensive review. J Neurointerv Surg 2020;12:1099‐106. [DOI] [PubMed] [Google Scholar]
- 19. Zaidat OO, Yoo AJ, Khatri P, et al. Recommendations on angiographic revascularization grading standards for acute ischemic stroke. A consensus statement. Stroke 2013;44:2650‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Liebeskind DS, Bracard S, Guillemin F, et al. eTICI reperfusion: defining success in endovascular stroke therapy. J Neurointerv Surg 2019;11:433‐8. [DOI] [PubMed] [Google Scholar]
- 21. Campbell BCV, Mitchell TJ, Kleinig HM, et al. Endovascular therapy for ischemic stroke with perfusion‐imaging selection. N Engl J Med 2015;372:1009‐18. [DOI] [PubMed] [Google Scholar]
- 22. Nogueira RA, Jadhav AP, Haussen DC, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med 2018;378:11‐21. [DOI] [PubMed] [Google Scholar]
- 23. Rao NM, Levine SR, Gornbein JA, Saver JL. Defining clinically relevant cerebral hemorrhage after thrombolytic therapy for stroke. Stroke 2014;45:2728‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Saver JL, Goyal M, Bonafe A, et al. Stent‐retriever thrombectomy after intravenous t‐PA vs. t‐PA alone in stroke. N Engl J Med 2015;372:2285‐95. [DOI] [PubMed] [Google Scholar]
- 25. Yang P, Zhang Y, Zhang L, et al. Endovascular thrombectomy with or without intravenous alteplase in acute stroke. N Engl J Med 2020;382:1981‐93. [DOI] [PubMed] [Google Scholar]
- 26. Marks MP, Heit JJ, Lansberg MG, et al. Endovascular treatment in the DEFUSE 3 study. Stroke 2018;49:2000‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mocco J, Siddiqui AH, Fiorella D, et al. POSITIVE: perfusion imaging selection of ischemic stroke patients for endovascular therapy. J Neurointerv Surg 2021;0:1‐8. [DOI] [PubMed] [Google Scholar]
- 28. Fiehler J. First pass rate, best option! Paper presented at: European Society of Minimally Invasive Neurological Therapy (ESMINT) webinar; 2019; Hamburg, Germany. [Google Scholar]
- 29. Behme D, Knauth M, Psychogios M‐N. Retriever wire supported carotid artery revascularization (ReWiSed CARe) in acute ischemic stroke with underlying tandem occlusion used by an internal carotid artery dissection: technical note. Interv Neuroradiol 2017;23:289‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Katz JM, Hakoun AM, Dehdashti AR, Chebl AB, Janardhan V, Janardhan V. Understanding the radial force of stroke thrombectomy devices to minimize vessel wall injury: mechanical bench testing of the radial force generated by a novel braided thrombectomy device compared to laser‐cut stent retrievers in simulated MCA vessel diameters. Interv Neurol 2019;8:206‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Janardhan V, Janardhan V, Kalousek V. COVID‐19 as a blood clotting disorder masquerading as a respiratory illness: a cerebrovascular perspective and therapeutic implications for stroke thrombectomy. J Neuroimaging 2020;30:555‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Chueh JY, Kuhn AL, Puri AS, Wilson SD, Wakhloo AK, Gounis MJ. Reduction in distal emboli with proximal flow control during mechanical thrombectomy: a quantitative in vitro study. Stroke 2013;44:1396‐401. [DOI] [PubMed] [Google Scholar]
- 33. Arslanian R, Caroff J, Marosfoi M, et al. P‐035 is bigger really better for clot ingestion during a direct aspiration first pass technique? J Neurointerv Surg 2018;10:A43‐4. [Google Scholar]
- 34. Kim OV, Litvinov RI, Welsel JW, Alber MS. Structural basis for the nonlinear mechanics of fibrin networks under compression. Biomaterials 2014;35:6739‐49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Marosfoi M, Strittmatter L, Arslanian R, et al. Abstract E‐112: how do clots respond to direct aspiration during interventional treatment of acute ischemic stroke. J Neurointerv Surg 2019;11:A109‐10. [Google Scholar]
- 36. Cotagliola G, Bosia F, Pugno NM. Static and dynamic friction of hierarchical surfaces. Phys Rev E 2016;94:063003. [DOI] [PubMed] [Google Scholar]
- 37. Jagadeesan BD, Janardhan V, Janardhan V. Abstract E‐106: feasibility of automation of staged balloon guide catheter (BGC) aspiration during stroke thrombectomy using a customizable iPad app and a bluetooth‐enabled smart pump: an in‐vitro study. J Neurointerv Surg 2018;10:A100‐1. [Google Scholar]


