Abstract
Although multiple antimicrobial resistance (AMR) determinants can confer the same in vitro antimicrobial susceptibility testing (AST) phenotype, their differing effect on optimal therapeutic choices is uncertain. Using a large population-based collection of clinical strains spanning a 3.5-year period, we applied WGS to detect inhibitor resistant (IR), extended-spectrum β-lactamase (ESBL), and carbapenem resistant (CR) β-lactamase (bla) genes and compared the genotype to the AST phenotype in select isolates.
All blaNDM-1 (9/9) and the majority of blaNDM-1/OXA-48 (3/4) containing isolates were resistant to CAZ/AVI as predicted by WGS. The combination of ATM and CAZ/AVI restored susceptibility by disk diffusion assay. Unexpectedly, clinical Kp isolates bearing blaKPC-8 (V240G) and blaKPC-14 (G242 and T243 deletion) did not test fully resistant to CAZ/AVI. Lastly, despite the complexity of the β-lactamase background, CAZ/AVI retained potency. Presumed phenotypes conferred by AMR determinants need to be tested if therapeutic decisions are being guided by their presence or absence.
Keywords: Klebsiella pneumoniae, beta-lactamase inhibitors, avibactam, ceftolozane, aztreonam
Introduction
Antimicrobial susceptibility testing (AST) is currently still the “gold standard” method in guiding effective antibiotic therapy. In contrast, whole genome sequencing (WGS) provides comprehensive data providing insight on gene content and gene mutations, and offers possible genetic explanations for AST phenotypes (1, 2). However, multiple resistance determinants can confer the same in vitro AST phenotype [e.g. inhibitor resistant (IR), extended-spectrum β-lactamase (ESBL), or carbapenem resistant (CR) phenotype] with varying MIC values in the resistant range. The biological effect of different genotypes on AST phenotype is not well studied; therefore, we undertook an investigation that begins to close this knowledge gap.
Efforts to develop novel statistical methods and machine learning to predict AST results are presently ongoing (3–7). Historically, an antimicrobial resistance phenotype is determined and then in some cases a genotypic explanation is sought. However, rapid molecular diagnostics (RMDs) could potentially change this current approach, as results of RMD platforms are assessed to predict phenotype from genotype (3–5). In addition, other features such as promoter mutations, porin mutations, and changes in efflux pump expression can contribute to phenotype, as do β-lactamase genes (1, 2).
In this study, we tested three hypotheses about resistance mechanisms correlated with certain resistant phenotypes using an existing library of 1,777 published Klebsiella pneumoniae (Kp) genomes (8). They were: 1) blaNDM-1 positive isolates will be ceftazidime/avibactam (CAZ/AVI) and ceftolozane/tazobactam (TOL/TAZO) resistant. The combination of aztreonam (ATM) and CAZ/AVI will restore a susceptible phenotype; 2) blaKPC-8 and blaKPC-14 will confer resistance to CAZ/AVI, piperacillin/tazobactam (PIP/TAZO) and TOL/TAZO; and 3) complex β-lactamase backgrounds in singular isolates [inhibitor resistant TEM (IRT) and ESBL, with or without blaKPC/CTX-M genes, n=24] will be susceptible to CAZ/AVI.
Material and Methods
For this study, we used the WGS data from a previously sequenced collection of 1,777 ESBL-producing Kp isolates cultured from patients in the Houston Methodist Hospital system between September 2011 and May 2015 (8). The data was further analyzed with regard to their β-lactamase content, and 42 isolates were selected for AST. Isolates chosen possessed the following β-lactamase genes: blaNDM-1 (n=9); blaNDM-1 and blaOXA-48 (n=4); blaKPC-8 or blaKPC-14 (n=5); and those with a very complex β-lactamase background [n=24, all possessed a blaTEM-IRT, blaSHV/TEM-ESBL, +/− blaCTX-M, and +/− blaKPC]. These were the only clinical isolates out of the collection of 1,777 that had the genotypes we required to test our hypotheses, and were thus selected for further analysis.
AST for PIP/TAZO, CAZ, ATM, CAZ/AVI, and TOL/TAZO was performed by disk diffusion assay using Clinical and Laboratory Standards Institute (CLSI) methods (9). The addition of ATM to the CAZ/AVI disks was performed as previously described (10). We chose disk diffusion as our AST method because CAZ/AVI and TOL/TAZO are not routinely found in standard panels and they are a CLSI approved way of determining antimicrobial susceptibility to these antimicrobial agents.
Results
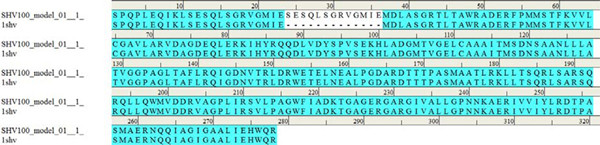
SHV β-lactamase genes, that are often chromosomally encoded in Kp, were present in 1,427/1,777 (80%) of isolates. These included blaSHV-100 (n=724, 41%), blaSHV-ESBLs (n=528, 30%), and blaSHV-non-ESBL/-non-IR/-non-SHV-100 (n=175, 10%). SHV ESBLs were defined as having at least one of the following amino acid substitutions: D104G (n=9), G156D (n=40), G238S/A and/or E240K (n=479) (Ambler class A consensus amino acid numbering) (8, 11–13). SHV-100, which previously was reported only once (14), possessed a 13 amino acid duplication (35SESQLSGRVGMIE36) (Figure 1). In the 20% of isolates that did not contain a blaSHV, variants of blaLEN and blaOKP were present. LEN and OKP are other class A chromosomal βlactamses found in Kp. As reported by Hæggman et al, phylogenetic analysis of blaSHV, blaLEN, and blaOKP revealed parallel evolution of these genes, with the SHV, OKP, and LEN β-lactamase families corresponding to phylogenetic groups KpI, KpII, and KpIII, respectively (15). However, we observed that not every isolate contained one of the 3 associated chromosomal class A enzymes. We suspect that this may be due to limitations of WGS, species misidentification, or the absence of those bla genes.
Figure 1.
Location of the 13 amino acid insertion in SHV-1 that defines SHV-100.
The TEM β-lactamase findings included 255 blaTEM-IRTs, 49 blaTEM-ESBLs, and 492 blaTEM-non-ESBL/-non-IRTs. TEM ESBLs within the collection included TEMs with at least one of the following amino acid substitutions: E104K, R164C, G238S and/or E240K; and IRTs included amino acid substitutions: M69L/V; S130G; or R244G/L/S (Ambler class A consensus amino acid numbering) (16–18). The distribution of substitutions that defined the IRTs were as follows: M69L (n=97), M69V (n=3), S130G (n=30), R244G (n=56), R244L (n=4), and R244S (n=65). A lower percentage of ESBLs was found among blaTEM (6%) vs. blaSHV (37%) genes; contrasting with a much higher and unexpected percentage of IRT genes, 32% out of all blaTEMs, whereas there were no IR blaSHV genes identified within the study (8).
Four KPC variants were identified in this collection, including blaKPC-2 (n=572), blaKPC-3 (n=4), blaKPC-8 (n=4), and blaKPC-14 (n=1). KPC-8 contains a V240G substitution in a KPC-3 background, whereas KPC-14 is in a KPC-2 background with amino acids G242 and T243 deleted. Of note, regional bias may be present with regard to overall β-lactamase composition of the isolates, due to their exclusive collection in the Houston Methodist Hospital system.
Of the 1,777 isolates sequenced, 1,161 carried a CTX-M β-lactamase (65%), primarily blaCTX-M-15 (n=1,112) and blaCTX-M-14 (n=30). In addition to blaKPC, other carbapenemase genes were contained within this collection. Eight had a blaOXA-48 alone, and 13 had a blaNDM-1 [blaNDM-1 alone (n=9), and blaNDM-1 and blaOXA-48 (n=4)] (8).
Many isolates possessed very complex β-lactamase backgrounds (i.e., contained genes for multiple β-lactamases) (8, 12, 13, 16, 18). Examples include, 4 isolates that contained CTX-M-15, TEM-76 (S130G-IRT), and SHV-12 (G238S/E240K-ESBL) or SHV-27 (G156D-ESBL) within a single isolate; and 8 isolates that had in each CTX-M-15, TEM-30 (R244S-IRT), and SHV-5 (G238S-ESBL) or SHV-12 or SHV-27 (one of these also contained KPC-2). In addition, 11 isolates had TEM-79 (R244G-IRT), KPC-2, and SHV-5 or SHV-12 or SHV-27 in each (4 of these also had CTX-M-15); and 1 isolate had CTX-M-15, TEM-33 (M69L-IRT), and SHV-27.
Most isolates that contained blaNDM-1, were TOL/TAZO (13/13) and CAZ/AVI (12/13) resistant. However, the combination of ATM and CAZ/AVI restored a susceptible phenotype (Table 1 and Supplemental Table 1). The blaNDM-1 isolates (lone carbapenemase) were primarily sequence type 14 (ST14); however, ST906 and ST307 were also found. The blaNDM-1 and blaOXA-48 isolates belonged to ST37 or to an unknown sequence type (Supplemental Table 1). Those isolates that contained blaKPC-8 and blaKPC-14 were resistant to PIP/TAZO and TOL/TAZO, and of ST258 (n=5, one isolate unknown ST). Unexpectedly, they tested susceptible to CAZ/AVI (Table 2 and Supplemental Table 1).
Table 1.
Prediction: NDM + isolates will be CAZ/AVI and TOL/TAZO resistant. Addition of ATM will restore susceptibility to CAZ/AVI.
| Result | |||||
|---|---|---|---|---|---|
| # of isolates | bla genes | PIP/TAZO | TOL/TAZO | CAZ/AVI | CAZ/AVI/ATM |
| 9 | bla NDM-1 | R * | R | R | S |
| 4 | blaNDM-1 & blaOXA-48 | R | R | R # | S |
(8 isolates R, 1 isolate S),
(3 isolates R, 1 isolate S)
Table 2.
Prediction: blaKPC-8 and blaKPC-14 confers resistance to CAZ/AVI.
| Result | ||||
|---|---|---|---|---|
| # of isolates | bla genes | PIP/TAZO | TOL/TAZO | CAZ/AVI |
| 5 | blaKPC-8 (V240G) or blaKPC-14 (G242 and T243 deletion) | R | R | S ** |
Result not expected, however zone size diminished compared to controls, but did not reach the resistant zone diameter breakpoint.
All 24 complex β-lactamase Kp isolates were susceptible to CAZ/AVI by disk diffusion assay, regardless of the β-lactamase combination (Table 3 and Supplemental Table 1). Most were also susceptible to PIP/TAZO and TOL/TAZO, unless they contained blaKPC or blaSHV-12. The 24 complex β-lactamase background isolates were predominantly ST280 (n=10) if they did not have a blaKPC, and ST258 (n=6) when they possessed a blaKPC (Supplemental Table 1).
Table 3.
Prediction: Complex β-lactamase backgrounds (IRT, ESBL, +/− KPC) test susceptible to CAZ/AVI.
| Result | ||||
|---|---|---|---|---|
| # of isolates | bla genes | PIP/TAZO | TOL/TAZO | CAZ/AVI |
| 3 | blaCTX-M-15, blaTEM-76 (S130G), & blaSHV-27 (G156D) | S | S | S |
| 1 | blaCTX-M-15, blaTEM-76 (S130G), & blaSHV-12 (L35Q/G238S/E240K) | I | R | S |
| 7 | blaCTX-M-15, blaTEM-30 (R244S), & blaSHV-5 (G238S/E240K) or blaSHV-27 | S ^ | S | S |
| 1 | blaCTX-M-15, blaTEM-33 (M69L), & blaSHV-27 | S | S | S |
| 11 | blaTEM-79 (R244G), blaSHV-5 or blaSHV-12, or blaSHV-27, & blaKPC-2 | R | R | S |
| 1 | blaTEM-30 (R244S), blaSHV-12, blaCTX-M-15, & blaKPC-2 | R | R | S |
(6 isolates S, 1 isolate R)
Discussion
In this analysis, we compared the genotype of multiple isolates with their AST phenotype. This approach enabled an investigation of naturally occurring resistance patterns based on gene content and gene mutations. Although it is unlikely in the near future that WGS of clinical isolates will be routine in clinical laboratories, it is becoming increasingly more frequent, and studies such as this are needed to assess the clinical utility of the data generated.
As predicted from the WGS data and published cases, all blaNDM-1 and most blaNDM-1/OXA-48 containing isolates were resistant to CAZ/AVI. One blaNDM-1/OXA-48 containing isolate was not CAZ/AVI resistant; perhaps the plasmid was lost by the isolate between WGS and disk diffusion assay. The combination of ATM and CAZ/AVI restored susceptibility by disk diffusion assay, as was previously reported (10). In addition, treatment efficacy with the CAZ/AVI/ATM combination has been demonstrated in murine models and in observational studies involving patients (10, 19–21). However, it is important to keep in mind that resistance to any drug combination can likely develop. For example, we recently reported on an NDM-1-, OXA-48-, CTX-M-15- and CMY-16-positive K. pneumoniae isolate that after being serially passaged, had mutational variants selected for based on resistance to ATM/AVI (MIC ≥ 128/4 μg/ml). WGS revealed that resistant mutants lost the blaNDM-1 gene, and acquired an amino acid substitution in CMY-16 (either Y150S or N346H). Both ATM/AVI and CAZ/AVI/ATM resistance (using the CAZ/AVI breakpoint of R ≥ 16/4 μg/ml) was conferred when CMY-16 Y150S or CMY-16 N346H was present in the clinical carbapenemase-producing isolates (22).
Four blaKPC alleles were identified in this collection: blaKPC-2, −3, −8 and −14. We chose isolates that possessed blaKPC-8 and blaKPC-14 for further study, as their substitutions have been associated with CAZ/AVI resistance in clinical isolates (23–26). KPC-8 has a V240G change in a KPC-3 background (27) and was shown to confer CAZ/AVI resistance (MIC = 32/4 μg/ml) to a clinical isolate as compared to clinical isolates possessing KPC-3 with no additional relevant genomic changes (MIC = 2–4/4 μg/ml) (25). In addition, the V240G substitution in a KPC-2 background was reported to confer higher levels of resistance to ceftazidime via increased ceftazidime hydrolysis, and an even greater fold change in the kcat/KM for ceftazidime was observed for V240G in a KPC-3 background (27). However, previous work on blaKPC-8 cloned into DH10B E. coli demonstrated a CAZ/AVI MIC of 4/4 ug/ml. Albeit the MIC being higher than for any of the other KPCs tested, it did not reach the clinically resistant breakpoint of ≥ 16/4 μg/ml (28). Thus, we felt the need to further test the hypothesis that KPC-8 in clinical isolates produce a CAZ/AVI resistant phenotype.
KPC-14 (amino acids G242 and T243 deleted in a KPC-2 background) has also been associated with CAZ/AVI resistance. When blaKPC-14 was cloned and expressed in E. coli, MICs for CAZ/AVI were increased compared to KPC-2 without the G242 and T243 deletions, 24/4 μg/ml vs. 0.38/4 μg/ml, respectively (24). In addition, a T243M substitution in a KPC-3 background was associated with increased MICs to CAZ/AVI (25, 29). Surprisingly, in the present study blaKPC-8 and blaKPC-14 in the clinical Kp isolates did not confer resistance to CAZ/AVI by disk diffusion assay. However, a trend toward lowered susceptibility was observed via smaller zone sizes for blaKPC-8 (mode = 23 mm, R ≤ 21 mm, Supplemental Table 1). KPC variants that carried substitutions at amino acid position D179, a site often associated with CAZ/AVI resistance, were not found within the collection (25, 26, 30–32).
Clavulanic acid resistance is caused by substitutions at amino acids 69, 130, and 244 in the TEM and SHV β-lactamases (12, 16, 18, 33–35). However, PIP/TAZO and CAZ/AVI clinical resistance has not been reported due to substitutions at these sites. Our data is consistent with those observations, even when the IRT was coupled with an extended-spectrum SHV and CTX-M-15 β-lactamases.
Conclusions
In the presence of a very complex β-lactamase background or increased CAZ hydrolysis by KPC-8, CAZ/AVI remains an effective treatment option based on our in vitro data. We also showed that in the absence of blaKPC and blaSHV-12, TOL/TAZO and PIP/TAZO maintain efficacy. Nonetheless, caution has to be taken since there are limits to our approach, i.e., this study represents only a snapshot of a much broader landscape, as it is based on a local set of ESBL-producing isolates. However, taken together, these results add to our understanding of utilizing WGS data to predict clinical phenotypes.
Supplementary Material
Acknowledgments
Funding
Research reported in this publication was supported by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health (NIH) to R.A.B. under Award Numbers R01AI100560, R01AI063517, and R01AI072219. This study was also supported in part by funds and/or facilities provided by the Cleveland Department of Veterans Affairs, Award Number 1I01BX001974 to R.A.B. from the Biomedical Laboratory Research & Development Service of the VA Office of Research and Development, and the Geriatric Research Education and Clinical Center VISN 10. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Department of Veterans Affairs.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Shelburne SA, Kim J, Munita JM, Sahasrabhojane P, Shields RK, Press EG, Li X, Arias CA, Cantarel B, Jiang Y, Kim MS, Aitken SL, Greenberg DE. 2017. Whole-Genome Sequencing Accurately Identifies Resistance to Extended-Spectrum beta-Lactams for Major Gram-Negative Bacterial Pathogens. Clin Infect Dis 65:738–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tamma PD, Fan Y, Bergman Y, Pertea G, Kazmi AQ, Lewis S, Carroll KC, Schatz MC, Timp W, Simner PJ. 2019. Applying Rapid Whole-Genome Sequencing To Predict Phenotypic Antimicrobial Susceptibility Testing Results among Carbapenem-Resistant Klebsiella pneumoniae Clinical Isolates. Antimicrob Agents Chemother 63:e01923–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Evans SR, Hujer AM, Jiang H, Hill CB, Hujer KM, Mediavilla JR, Manca C, Tran TT, Domitrovic TN, Higgins PG, Seifert H, Kreiswirth BN, Patel R, Jacobs MR, Chen L, Sampath R, Hall T, Marzan C, Fowler VG Jr., Chambers HF, Bonomo RA 2017. Informing Antibiotic Treatment Decisions: Evaluating Rapid Molecular Diagnostics To Identify Susceptibility and Resistance to Carbapenems against Acinetobacter spp. in PRIMERS III. J Clin Microbiol 55:134–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Evans SR, Hujer AM, Jiang H, Hujer KM, Hall T, Marzan C, Jacobs MR, Sampath R, Ecker DJ, Manca C, Chavda K, Zhang P, Fernandez H, Chen L, Mediavilla JR, Hill CB, Perez F, Caliendo AM, Fowler VG Jr., Chambers HF, Kreiswirth BN, Bonomo RA. 2016. Rapid Molecular Diagnostics, Antibiotic Treatment Decisions, and Developing Approaches to Inform Empiric Therapy: PRIMERS I and II. Clin Infect Dis 62:181–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Evans SR, Tran TTT, Hujer AM, Hill CB, Hujer KM, Mediavilla JR, Manca C, Domitrovic TN, Perez F, Farmer M, Pitzer KM, Wilson BM, Kreiswirth BN, Patel R, Jacobs MR, Chen L, Fowler VG Jr., Chambers HF, Bonomo RA. 2018. Rapid Molecular Diagnostics to Inform Empiric Use of Ceftazidime/Avibactam and Ceftolozane/Tazobactam against Pseudomonas aeruginosa: PRIMERS IV. Clin Infect Dis 68:1823–1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim J, Greenberg DE, Pifer R, Jiang S, Xiao G, Shelburne SA, Koh A, Xie Y, Zhan X. 2020. VAMPr: VAriant Mapping and Prediction of antibiotic resistance via explainable features and machine learning. PLoS Comput Biol 16:e1007511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nguyen M, Brettin T, Long SW, Musser JM, Olsen RJ, Olson R, Shukla M, Stevens RL, Xia F, Yoo H, Davis JJ. 2018. Developing an in silico minimum inhibitory concentration panel test for Klebsiella pneumoniae. Sci Rep 8:421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Long SW, Olsen RJ, Eagar TN, Beres SB, Zhao P, Davis JJ, Brettin T, Xia F, Musser JM. 2017. Population Genomic Analysis of 1,777 Extended-Spectrum Beta-Lactamase-Producing Klebsiella pneumoniae Isolates, Houston, Texas: Unexpected Abundance of Clonal Group 307. MBio 8:e00489–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clinical and Laboratory Standards Institute. 2019. M100-S29. Performance Standards for Antimicrobial Susceptibility Testing, 28th Edition Clinical and Laboratory Standards Institute, Wayne, PA. [Google Scholar]
- 10.Marshall S, Hujer AM, Rojas LJ, Papp-Wallace KM, Humphries RM, Spellberg B, Hujer KM, Marshall EK, Rudin SD, Perez F, Wilson BM, Wasserman RB, Chikowski L, Paterson DL, Vila AJ, van Duin D, Kreiswirth BN, Chambers HF, Fowler VG Jr., Jacobs MR, Pulse ME, Weiss WJ, Bonomo RA. 2017. Can Ceftazidime-Avibactam and Aztreonam Overcome beta-Lactam Resistance Conferred by Metallo-beta-Lactamases in Enterobacteriaceae? Antimicrob Agents Chemother 61:e02243–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.SHVTable.aspx https://externalwebapps.lahey.org/studies/ [Google Scholar]
- 12.Hujer AM, Hujer KM, Bonomo RA. 2001. Mutagenesis of amino acid residues in the SHV-1 beta-lactamase: the premier role of Gly238Ser in penicillin and cephalosporin resistance. Biochim Biophys Acta 1547:37–50. [DOI] [PubMed] [Google Scholar]
- 13.Hujer AM, Hujer KM, Helfand MS, Anderson VE, Bonomo RA. 2002. Amino acid substitutions at Ambler position Gly238 in the SHV-1 beta-lactamase: exploring sequence requirements for resistance to penicillins and cephalosporins. Antimicrob Agents Chemother 46:3971–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ramdani-Bouguessa N, Manageiro V, Jones-Dias D, Ferreira E, Tazir M, Canica M. 2011. Role of SHV beta-lactamase variants in resistance of clinical Klebsiella pneumoniae strains to beta-lactams in an Algerian hospital. J Med Microbiol 60:983–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haeggman S, Lofdahl S, Paauw A, Verhoef J, Brisse S. 2004. Diversity and evolution of the class A chromosomal beta-lactamase gene in Klebsiella pneumoniae. Antimicrob Agents Chemother 48:2400–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Canton R, Morosini MI, de la Maza OM, de la Pedrosa EG. 2008. IRT and CMT beta-lactamases and inhibitor resistance. Clin Microbiol Infect 14 Suppl 1:53–62. [DOI] [PubMed] [Google Scholar]
- 17.TEMTable.aspx https://externalwebapps.lahey.org/studies/ [Google Scholar]
- 18.Palzkill T. 2018. Structural and Mechanistic Basis for Extended-Spectrum Drug-Resistance Mutations in Altering the Specificity of TEM, CTX-M, and KPC beta-lactamases. Front Mol Biosci 5:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mojica MF, Ouellette CP, Leber A, Becknell MB, Ardura MI, Perez F, Shimamura M, Bonomo RA, Aitken SL, Shelburne SA. 2016. Successful Treatment of Bloodstream Infection Due to Metallo-beta-Lactamase-Producing Stenotrophomonas maltophilia in a Renal Transplant Patient. Antimicrob Agents Chemother 60:5130–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Monogue ML, Abbo LM, Rosa R, Camargo JF, Martinez O, Bonomo RA, Nicolau DP. 2017. In Vitro Discordance with In Vivo Activity: Humanized Exposures of Ceftazidime-Avibactam, Aztreonam, and Tigecycline Alone and in Combination against New Delhi Metallo-beta-Lactamase-Producing Klebsiella pneumoniae in a Murine Lung Infection Model. Antimicrob Agents Chemother 61:e00486–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yasmin M, Fouts DE, Jacobs MR, Haydar H, Marshall SH, White R, D’Souza R, Lodise TP, Rhoads DD, Hujer AM, Rojas LJ, Hoyen C, Perez F, Edwards A, Bonomo RA. 2019. Monitoring Ceftazidime-Avibactam (CAZ-AVI) and Aztreonam (ATM) Concentrations in the Treatment of a Bloodstream Infection Caused by a Multidrug-Resistant Enterobacter sp. Carrying both KPC-4 and NDM-1 Carbapenemases. Clin Infect Dis doi: 10.1093/cid/ciz1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Niu S, Wei J, Zou C, Chavda KD, Lv J, Zhang H, Du H, Tang YW, Pitout JDD, Bonomo RA, Kreiswirth BN, Chen L. 2020. In vitro selection of aztreonam/avibactam resistance in dual-carbapenemase-producing Klebsiella pneumoniae. J Antimicrob Chemother 75:559–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Galani I, Antoniadou A, Karaiskos I, Kontopoulou K, Giamarellou H, Souli M. 2019. Genomic characterization of a KPC-23-producing Klebsiella pneumoniae ST258 clinical isolate resistant to ceftazidime-avibactam. Clin Microbiol Infect 25:763.e5–763.e8. [DOI] [PubMed] [Google Scholar]
- 24.Oueslati S, Iorga BI, Tlili L, Exilie C, Zavala A, Dortet L, Jousset AB, Bernabeu S, Bonnin RA, Naas T. 2019. Unravelling ceftazidime/avibactam resistance of KPC-28, a KPC-2 variant lacking carbapenemase activity. J Antimicrob Chemother 74:2239–2246. [DOI] [PubMed] [Google Scholar]
- 25.Shields RK, Chen L, Cheng S, Chavda KD, Press EG, Snyder A, Pandey R, Doi Y, Kreiswirth BN, Nguyen MH, Clancy CJ. 2017. Emergence of Ceftazidime-Avibactam Resistance Due to Plasmid-Borne blaKPC-3 Mutations during Treatment of Carbapenem-Resistant Klebsiella pneumoniae Infections. Antimicrob Agents Chemother 61:2097–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shields RK, Nguyen MH, Press EG, Chen L, Kreiswirth BN, Clancy CJ. 2017. Emergence of Ceftazidime-Avibactam Resistance and Restoration of Carbapenem Susceptibility in Klebsiella pneumoniae Carbapenemase-Producing K pneumoniae: A Case Report and Review of Literature. Open Forum Infect Dis 4:ofx101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mehta SC, Rice K, Palzkill T. 2015. Natural Variants of the KPC-2 Carbapenemase have Evolved Increased Catalytic Efficiency for Ceftazidime Hydrolysis at the Cost of Enzyme Stability. PLoS Pathog 11:e1004949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Papp-Wallace KM, Bajaksouzian S, Abdelhamed AM, Foster AN, Winkler ML, Gatta JA, Nichols WW, Testa R, Bonomo RA, Jacobs MR. 2015. Activities of ceftazidime, ceftaroline, and aztreonam alone and combined with avibactam against isogenic Escherichia coli strains expressing selected single beta-lactamases. Diagn Microbiol Infect Dis 82:65–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Haidar G, Clancy CJ, Shields RK, Hao B, Cheng S, Nguyen MH. 2017. Mutations in blaKPC-3 That Confer Ceftazidime-Avibactam Resistance Encode Novel KPC-3 Variants That Function as Extended-Spectrum beta-Lactamases. Antimicrob Agents Chemother 61:e02534–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barnes MD, Winkler ML, Taracila MA, Page MG, Desarbre E, Kreiswirth BN, Shields RK, Nguyen MH, Clancy C, Spellberg B, Papp-Wallace KM, Bonomo RA. 2017. Klebsiella pneumoniae Carbapenemase-2 (KPC-2), Substitutions at Ambler Position Asp179, and Resistance to Ceftazidime-Avibactam: Unique Antibiotic-Resistant Phenotypes Emerge from beta-Lactamase Protein Engineering. mBio 8: e00528–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gaibani P, Campoli C, Lewis RE, Volpe SL, Scaltriti E, Giannella M, Pongolini S, Berlingeri A, Cristini F, Bartoletti M, Tedeschi S, Ambretti S. 2018. In vivo evolution of resistant subpopulations of KPC-producing Klebsiella pneumoniae during ceftazidime/avibactam treatment. J Antimicrob Chemother 73:1525–1529. [DOI] [PubMed] [Google Scholar]
- 32.Gottig S, Frank D, Mungo E, Nolte A, Hogardt M, Besier S, Wichelhaus TA. 2019. Emergence of ceftazidime/avibactam resistance in KPC-3-producing Klebsiella pneumoniae in vivo. J Antimicrob Chemother 74:3211–3216. [DOI] [PubMed] [Google Scholar]
- 33.Helfand MS, Bethel CR, Hujer AM, Hujer KM, Anderson VE, Bonomo RA. 2003. Understanding resistance to beta-lactams and beta-lactamase inhibitors in the SHV beta-lactamase: lessons from the mutagenesis of SER-130. J Biol Chem 278:52724–9. [DOI] [PubMed] [Google Scholar]
- 34.Helfand MS, Hujer AM, Sonnichsen FD, Bonomo RA. 2002. Unexpected advanced generation cephalosporinase activity of the M69F variant of SHV beta-lactamase. J Biol Chem 277:47719–23. [DOI] [PubMed] [Google Scholar]
- 35.Sulton D, Pagan-Rodriguez D, Zhou X, Liu Y, Hujer AM, Bethel CR, Helfand MS, Thomson JM, Anderson VE, Buynak JD, Ng LM, Bonomo RA. 2005. Clavulanic acid inactivation of SHV-1 and the inhibitor-resistant S130G SHV-1 beta-lactamase. Insights into the mechanism of inhibition. J Biol Chem 280:35528–36. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.