Abstract
Irritable bowel syndrome (IBS) is a common functional gastrointestinal disorder that affects specific groups of people. The relationship between breakfast consumption frequency and the risk of IBS is unclear. This study aimed to investigate the association between breakfast consumption frequency and the risk of IBS among Chinese female college students.
In this cross-sectional study (n = 706) conducted in October 2018, the frequency of breakfast consumption was categorized as 0 to 3 times/week, 4 to 6 times/week, or daily. IBS was diagnosed according to the Rome III criteria and was based on the presence of abdominal pain or discomfort for at least 3 months during the previous 6 months, with at least 2 or more of the following conditions: changes in frequency or form of stool and/or decrease in pain after defecation. We adjusted for confounding factors, including age, only child (yes or no), parents’ educational levels (senior high school or below, college, or postgraduate), parents’ marital status (married, widowed, or divorced), smoking status (smoker or nonsmoker), drinking status (drinker or nondrinker), body mass index, and depressive symptoms. A multiple logistic regression analysis was performed to determine the relationship between breakfast frequency and the risk of IBS.
Among 706 participants, 23.7% were the only child in their family, and the proportion of parents divorced or widowed was 18.5%. The proportion of fathers and mothers with high school education or above was 93.3% and 96.3%, respectively. The prevalence of IBS among the participants was 17.3% (122/706). Multivariate logistic regressions analysis showed that breakfast consumption frequency is negatively associated with the risk of IBS after adjusting for confounding factors. The odds ratios (95% confidence intervals) for IBS in the breakfast frequency category of 0 to 3 times/week, 4 to 6 times/week, and daily were 1.00 (reference), 0.96 (0.58, 1.60), and 0.45 (0.26, 0.78), respectively (P = .002).
Our data revealed that regular breakfast consumption is associated with a lower risk of IBS among Chinese college students. Future cohort and/or interventional studies should be conducted to further explore the association between breakfast consumption frequency and IBS.
Keywords: breakfast frequency, Chinese female college student, irritable bowel syndrome
1. Introduction
Irritable bowel syndrome (IBS) is a common functional gastrointestinal disorder characterized by abdominal discomfort associated with a change in stool form or frequency.[1] A global meta-analysis showed that the prevalence of IBS is 11.0%, and the prevalence rate of IBS among adolescents is higher than that of the general population (11.0% vs 7.8%).[2] IBS may increase the risk of several diseases, such as indigestion,[3] Parkinson disease,[4] and epilepsy,[5] and lower the patients’ quality of life.[6] We need to develop effective strategies for lowering the incidence risk of IBS.
Breakfast reflects daily dietary habits, and therefore, it is recognized as the most important meal of the day, contributing to 20% to 30% of the total energy intake.[7] Furthermore, it affects food choices throughout the day. A systematic review meta-analysis showed that regular breakfast eaters consume more calories, fiber, vegetables, and fruits and less fat than those who skip breakfast.[8] Notably, foods rich in dietary fiber, such as vegetables and fruits,[9,10] have been confirmed as protective factors against the risk of IBS[11,12] because dietary fiber stimulates the colonic mucosa, thereby increasing secretion and peristalsis, which subsequently increases fecal mass.[13] Although we inferred from the aforementioned findings that breakfast consumption frequency could be associated with IBS, few empirical studies evaluating this association have been conducted. Consequently, we designed a cross-sectional study to examine whether there are significant relationships between breakfast consumption frequency and the risk of IBS.
2. Methods
2.1. Site
Chongqing, a municipality located in the Southwest of China, is the center of economic, financial, scientific, and technological innovation and trade in the upper reaches of the Yangtze River. Chongqing Nursing Vocational College is the only nursing university in Chongqing and is the largest nursing college in Western China. The students in this school are predominantly female. The major qualifications consist of 6 disciplines, including nursing science, midwifery, rehabilitation, the provision and administration of geriatric services, community-based rehabilitation, and rehabilitation through traditional Chinese medicine. According to an epidemiological survey, university students in Southern China are at high risk of IBS[14]; therefore, it was desirable to carry out this study at Chongqing Nursing Vocational College.
2.2. Sample size calculation
The study sample size was calculated using the following formula:
Where N = sample size
p = prevalence of IBS
t = 1.96
d = 0.1
In a cross-sectional study including Chinese college students, the prevalence of IBS among female college students was expected to be 16.8%.[15] Therefore, it was estimated that the study should include a minimum total sample size of 215 participants.
2.3. Study participants
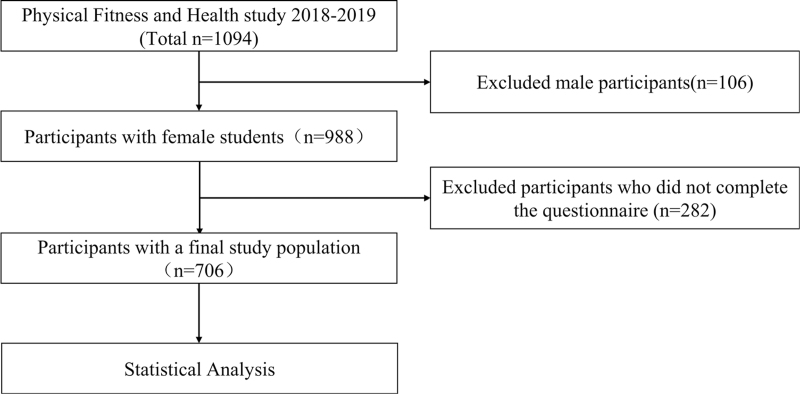
This cross-sectional study originated from the CNVCPFH study, which was a prospective cohort study. The detailed study design has been published elsewhere.[16] A total of 1094 college freshmen were recruited and agreed to participate in this study. Written informed consent forms were obtained from all college freshmen aged ≥16 years or from the primary guardians of participants aged <16 years. We asked each participant to complete a self-designed survey questionnaire that consisted of questions regarding demographic and lifestyle variables. We excluded 106 male college students and 282 participants who did not complete the questionnaire. These exclusions resulted in a final study population of 706 participants (Fig. 1). Ethical approval was obtained from the Institutional Review Board of the College of Physical Education of Southwest University (ethical approval number: SWU20180601).
Figure 1.
Research flowchart.
2.4. Assessment of IBS
IBS was diagnosed according to the Rome III criteria established by the Rome III Committee in 2006.[17] We asked each participant to report the presence of abdominal discomfort or pain according to the Rome III criteria as follows: improvement with defecation; onset associated with a change in frequency of stool; and/or onset associated with a change in form of stool. Participants with 2 of the 3 features mentioned above for abdominal discomfort or pain for at least 3 days per month in the last 3 months were defined as having IBS.[18]
2.5. Assessment of breakfast frequency
Breakfast consumption frequency was assessed with the following question: “How many times per week do you eat breakfast?” Eight response options were provided: never, 1 time/week, 2 times/week, 3 times/week, 4 times/week, 5 times/week, 6 times/week, or daily. We divided all participants into 3 groups according to the distribution of breakfast consumption frequency: 0 to 3 times/week, 4 to 6 times/week, and daily.
2.6. Relevant covariates
Demographic variables were measured using a self-designed questionnaire, including age, only child (yes or no), parents’ educational levels (senior high school or below, college, or postgraduate), and parents’ marital status (married, widowed, or divorced). Lifestyle factors included smoking status (smoker or nonsmoker) and drinking status (drinker or nondrinker). Body mass index was calculated as weight (kg) divided by height squared (m2). Depressive symptoms were assessed according to the Chinese version of the Self-rating Depression Scale.[19] This scale includes 20 items, with each item scored on a scale of 1 to 4. The sum of scores for the 20 items ranges from 20 to 80, with higher scores indicating a more severe depressive status. In the present study, a total score of ≥50 was defined as having depressive symptoms.[20]
2.7. Statistical analysis
Continuous variables are presented as geometric least-square means with 95% confidence intervals, and categorical variables are presented as proportions. P values were assessed using the chi-square tests for categorical variables, and analysis of variance was applied for continuous variables to compare the baseline characteristics of the categorized groups after adjusting for age.
IBS was considered as a dependent variable, and breakfast consumption frequency was considered as an independent variable. Multivariate logistic regression analyses were performed to estimate the relationship between breakfast consumption frequency and the risk of IBS. Model 1 was the crude univariate model; Model 2 was adjusted for age (≤18 or >18 years); and Model 3 was additionally adjusted for demographic variables (only child [yes or no], parents’ educational levels [senior high school or below, college, or postgraduate], parents’ marital status [married, widowed, or divorced], and lifestyle factors such as smoking [smoker or nonsmoker] and drinking status [drinker or nondrinker]), body mass index, and depressive symptoms. The P for trend was calculated by assigning the ordinal numbers 1 to 3 to the 3 categories of frequency of breakfast consumption and adding this as a continuous ordinal variable into the 3 different models. All tests were performed using IBM SPSS Statistics 21.0 software (IBM Corp., Armonk, NY).
3. Results
The participants’ baseline characteristics according to the categories of breakfast consumption frequency are shown in Table 1. Participants with a lower frequency of breakfast consumption reported a higher proportion of depressive symptoms (P < .001) and current smoker status (P = .006). No other significant differences were observed across the categories of breakfast consumption frequency.
Table 1.
Participants’ characteristics according to breakfast consumption frequency at baseline.
| N = 706 | 0 to 3 times/wk (n = 135) | 4 to 6 times/wk (n = 256) | Daily (n = 315) | P value∗ |
| Age, % | .218 | |||
| ≤18 | 74 (54.8) | 121 (47.3) | 145 (46.0) | |
| ≥19 | 61 (45.2) | 135 (52.7) | 170 (54.0) | |
| Only 1 child, % | 32 (23.7) | 65 (25.4) | 78 (24.8) | .935 |
| Father's educational, % | .711 | |||
| Senior high school or below | 126 (93.3) | 237 (92.6) | 297 (94.3) | |
| College or postgraduate | 9 (6.7) | 19 (7.4) | 18 (5.7) | |
| Mother's educational, % | .072 | |||
| Senior high school or below | 130 (96.3) | 251 (98.0) | 297 (94.3) | |
| College or postgraduate | 5 (3.7) | 5 (2.0) | 18 (5.7) | |
| Parents’ marital status, % | .359 | |||
| Married | 110 (81.5) | 214 (83.6) | 269 (85.4) | |
| Widowed | 3 (16.3) | 10 (12.5) | 14 (10.2) | |
| Divorced | 22 (2.2) | 32 (3.9) | 32 (4.4) | |
| Smoking status (Yes) | 13 (9.6) | 15 (5.9) | 8 (2.5) | .006 |
| Drinking status (Yes) | 73 (54.1) | 132 (51.6) | 148 (47.0) | .318 |
| BMI, kg/m2 | 20.2 (16.3, 28.8) | 20.0 (15.6, 34.1) | 20.3 (15.0, 29.7) | .309 |
| Depressive symptoms (SDS ≥ 50) | 26 (19.3) | 31 (12.1) | 18 (5.7) | <.001 |
In this cross-sectional study, the prevalence of IBS was 17.3% (122/706). Multivariate logistic regression analysis revealed that breakfast consumption frequency was inversely associated with the risk of IBS after adjusting for confounding factors (Fig. 2). The odds ratios (95% confidence intervals) for the risk of IBS in each breakfast consumption frequency category were 1.00 (reference) for 0 to 3 times/week, 0.96 (0.58, 1.60) for 4 to 6 times/week, and 0.45 (026, 0.78) for daily (P = .002).
Figure 2.
The relationship between breakfast consumption frequency and the risk of IBS among Chinese college students. IBS = irritable bowel syndrome.
4. Discussion
This study revealed a significant relationship between regular breakfast consumption and a low risk of IBS after adjusting for confounding factors.
Although the exact etiology of the association between breakfast consumption frequency and the risk of IBS remains unclear, intake of fiber-rich foods could play a mediating role in this association. Individuals who regularly eat breakfast usually consumed more fiber-rich foods, such as vegetables, fruit, and grains.[21,22] Dietary fibers and their fermented short-chain fatty acids are associated with the prevention of human diseases and are classified as insoluble or soluble according to their solubility in water. Insoluble dietary fiber can stimulate the colonic mucosa and subsequently promote secretion and peristalsis, leading to increased fecal mass.[13] Similarly, soluble dietary fiber is fermented by bacteria in the large intestine and converted into fermentation byproducts, which ultimately increase fecal bulk.[23] Therefore, regular breakfast consumption may improve IBS by increasing dietary fiber intake and thereby increasing fecal mass and bulk. Additionally, vitamin D intake also plays an important role in the association between breakfast consumption frequency and risk of IBS. Previous studies demonstrated that among Chinese college adolescents, regular breakfast eaters consumed more milk and eggs at breakfast than those who skipped breakfast.[9] Dairy and eggs are rich in vitamin D, which has been reported to be involved in preventing IBS. In addition, a previous study indicated that 1, 25 (OH) 2D3 has an important anti-inflammatory role through synthesizing antimicrobial defensive peptides and protecting gut barrier function,[24] subsequently protecting an individual against IBS.
We also considered potential confounding factors. Our previous study demonstrated that regular breakfast consumption is significantly associated with a lower risk of depressive symptoms.[16] Furthermore, patients with IBS have a more severe depressive status than the healthy population.[25] Therefore, depressive symptoms could confound the association between breakfast consumption frequency and risk of IBS. In addition, previous studies indicated that obesity may not only contribute to a higher risk of IBS,[26] but is also identified as the result of skipping breakfast.[27] We also considered the effect of an unhealthy lifestyle (smoking and drinking habits) on IBS. In a previous population-based survey, smoking and drinking habits were found to be important risk factors of IBS.[28] However, after adjusting for these confounding factors, the inverse association between regular breakfast consumption and lower risk of IBS remains significant. Therefore, regular breakfast consumption frequency is independently and significantly associated with a lower risk of IBS.
This study has several limitations. First, the cross-sectional study design limits the establishment of a causal association between breakfast consumption frequency and the risk of IBS. Second, the genetic background could also contribute to the risk of developing IBS. Indeed, a nationwide survey revealed that offsprings of parents with IBS were more likely to develop IBS.[29] Therefore, future studies need to examine whether a family history of IBS confounds the association between breakfast consumption frequency and the risk of IBS. Third, the relatively large number of participants who did not participate in our study may have overestimated the results of this study. Fourth, we did not collect data on the comorbidities (eg, inflammatory bowel disease, carbohydrate malabsorption, functional constipation, and functional dyspepsia) of IBS because it may have confounded the association between breakfast consumption frequency and risk of IBS. Prior studies showed that patients with IBS are more likely to have aforementioned comorbidities compared to healthy individuals.[30] Further studies should explore whether the association between breakfast consumption frequency and the risk of IBS remains significant after adjusting for comorbidities of IBS. Finally, the present study only included Chinese female college students; whether the above-mentioned relationship also exists in Chinese male college students remains unknown.
5. Conclusions
This cross-sectional study confirmed that there was a significant relationship between regular breakfast consumption and a low risk of IBS after adjusting for potential confounders. However, future cohort or interventional studies are needed to further explore the causal association between breakfast frequency and IBS using cohort or interventional studies.
Acknowledgments
We wish to thank the Chongqing Nursing Vocational College students who agreed to participate and provided informed consent to analyze their data. We would also like to thank the staff at this institution for their dedicated work.
Author contributions
Z.R. conceived and designed the research; Z.H., P.C., F.J., and J.Z. collected the data; C.Z. and J.C. analyzed the data and wrote the paper. G.Y. reviewed and edited the paper. All authors read and agreed on the published version of the manuscript.
Conceptualization: Zhongyu Ren.
Data curation: Chaowei Zhang, Jingyu Zhang, Yaru Wang, Rui Lang, Linxiu Su, Miao Yu, Xiaochen Zhao.
Formal analysis: Jingyu Zhang, Yaru Wang, Rui Lang, Linxiu Su, Miao Yu, Xiaochen Zhao.
Investigation: Zhongyu Ren.
Methodology: Zhongyu Ren.
Resources: Jingyu Zhang.
Writing – original draft: Chaowei Zhang.
Writing – review & editing: Guang Yang, Zhongyu Ren.
Footnotes
Abbreviation: IBS = irritable bowel syndrome.
How to cite this article: Zhang C, Zhang J, Wang Y, Lang R, Su L, Yu M, Zhao X, Yang G, Ren Z. Association between breakfast consumption frequency and the risk of irritable bowel syndrome among Chinese female college students: a cross-sectional study. Medicine. 2021;100:41(e27541).
This study was supported in part by the Fundamental Research Funds for the Central Universities (SWU1909734, SWU1909105), 2020 Chongqing Municipal Education Commission Humanities and Social Sciences Research Project (General Project; 20SKGH364), and 111 project (B21036). The funders participated in the study's design, data collection, statistical analysis, interpretation of data, manuscript writing, language editing, and publication charge.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
BMI = body mass index; SDS = Self-Rating Depression Scale.
†Continuous variables were expressed as mean (95%CI) and categorical variables were expressed as n (%).
P value were assessed using chi-square-test for categorical variables and analysis of variance for continuous variables.
References
- [1].Longstreth GF, Thompson WG, Chey WD, et al. Functional bowel disorders. Gastroenterology 2006;130:1480–91. [DOI] [PubMed] [Google Scholar]
- [2].Lovell R, Ford AC. Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Gastorenterol Hepatol 2012;10: 712.e4-721.e4. [DOI] [PubMed] [Google Scholar]
- [3].Dinicolantonio JJ, Lucan SC. Is fructose malabsorption a cause of irritable bowel syndrome? Med Hypotheses 2015;85:295–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Lai SW, Liao KF, Lin CL, et al. Irritable bowel syndrome correlates with increased risk of Parkinson's disease in Taiwan. Eur J Epidemiol 2014;29:57–62. [DOI] [PubMed] [Google Scholar]
- [5].Chen CH, Lin CL, Kao CH. Irritable bowel syndrome increases the risk of epilepsy. Medicine 2015;94:e1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Weaver KR, Melkus GD, Fletcher J, et al. Perceived stress, its physiological correlates, and quality of life in patients with irritable bowel syndrome. Biol Res Nurs 2018;20:312–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Matthys C, De Henauw S, Bellernans M, De Maeyer M, De Backer G. Breakfast habits affect overall nutrient profiles in adolescents. Public Health Nutr 2007;10:413–21. [DOI] [PubMed] [Google Scholar]
- [8].Giménez-Legarre Natalia, Flores-Barrantes Paloma, Miguel-Berges María Luisa, et al. Breakfast characteristics and their association with energy, macronutrients, and food intake in children and adolescents: a systematic review and meta-analysis. Nutrients 2020;12:2460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].López-González L, Becerra-Tomás N, Babio N, et al. Variety in fruits and vegetables, diet quality and lifestyle in an older adult Mediterranean population. Clin Nutr 2021;40:1510–8. [DOI] [PubMed] [Google Scholar]
- [10].Wiley Blackwell, Saura-Calixto F, Pérez-Jiménez J, Goñi I. Dietary Fiber and Associated Antioxidants in Fruit and Vegetables. 2017. [Google Scholar]
- [11].Nagarajan N, Morden A, Bischof D, et al. The role of fiber supplementation in the treatment of irritable bowel syndrome: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol 2015;27:1002–10. [DOI] [PubMed] [Google Scholar]
- [12].Oskouie FH, Vahedi H, Shahrbaf MA, et al. Dietary fiber and risk of irritable bowel syndrome: a case-control study. Gastroenterol Hepatol Bed Bench 2018;11:20–4. [PMC free article] [PubMed] [Google Scholar]
- [13].El-Salhy M, Ystad SO, Mazzawi T, et al. Dietary fiber in irritable bowel syndrome (review). Int J Mol Med 2017;40:607–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Dai N, Cong Y, Yuan HJD, et al. Prevalence of irritable bowel syndrome among undergraduates in Southeast China. Dig Liver Dis 2008;40:418–24. [DOI] [PubMed] [Google Scholar]
- [15].Lei S, Hao K, Xiaohua H. Prevalence of irritable bowel syndrome and its relationship with psychological stress status in Chinese university students. J Gastroenterol Hepatol 2010;24:1885–90. [DOI] [PubMed] [Google Scholar]
- [16].Ren Z, Cao J, Cheng P, et al. Association between breakfast consumption and depressive symptoms among Chinese college students: a cross-sectional and prospective cohort study. Int J Environ Res Public Health 2020;17:1571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Sheth AA. ROME III: the functional gastrointestinal disorders. J Clin Gastroenterol 2007;41:867. [Google Scholar]
- [18].D Rossman DA. Rome III: the new criteria. Chin J Dig Dis 2010;7:181–5. [DOI] [PubMed] [Google Scholar]
- [19].Peng H, Zhang Y, Ji Y, et al. Analysis of reliability and validity of Chinese cersion of SDS scale in women of rural area. Shanghai Med Pharm J 2013;14:20–3. [Google Scholar]
- [20].Xu L, Ren J, Cheng M, et al. Depressive symptoms and risk factors in Chinese persons with type 2 diabetes. Arch Med Res 2004;35:301–7. [DOI] [PubMed] [Google Scholar]
- [21].Lesani A, Mohammadpoorasl A, Javadi M, et al. Eating breakfast, fruit and vegetable intake and their relation with happiness in college students. Eat Weight Disord 2016;21:645–51. [DOI] [PubMed] [Google Scholar]
- [22].Sugiyama S, Okuda M, Sasaki S, et al. Breakfast habits among adolescents and their association with daily energy and fish, vegetable, and fruit intake: a community-based cross-sectional study. Environ Health Prev Med 2012;17:408–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Stephen AM, Cummings JHJN. Mechanism of action of dietary fibre in the human colon. Nature 1980;284:283–4. [DOI] [PubMed] [Google Scholar]
- [24].Barbáchano A, Fernández-Barral A, Ferrer-Mayorga G, et al. The endocrine vitamin D system in the gut. Mol Cell Endocrinol 2016;79–87. doi: 10.1016/j.mce.2016.11.028. [DOI] [PubMed] [Google Scholar]
- [25].Fond G, Loundou A, Hamdani N, et al. Anxiety and depression comorbidities in irritable bowel syndrome (IBS): a systematic review and meta-analysis. Eur Arch Psychiatry Clini Neurosci 2014;264:651–60. [DOI] [PubMed] [Google Scholar]
- [26].Nuaman BN. The association between central obesity and the risk of irritable bowel syndrome: a case-control study. Am J Med Sci Med 2017;5:23–6. [Google Scholar]
- [27].Horikawa C, Kodama S, Yachi Y, et al. Skipping breakfast and prevalence of overweight and obesity in Asian and Pacific regions: a meta-analysis. Prev Med 2011;53:260–7. [DOI] [PubMed] [Google Scholar]
- [28].Farzaneh N, Ghobaklou M, Moghimi-Dehkordi B, et al. Effects of demographic factors, body mass index, alcohol drinking and smoking habits on irritable bowel syndrome: a case control study. Ann Med Health Sci Res 2013;3:391–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Yeh Ta-Chuan, Bai Ya-Mei, Tsai Shih-Jen, et al. Risks of major mental disorders and irritable bowel syndrome among the offspring of parents with irritable bowel syndrome: a nationwide study. Int J Environ Res Public Health 2021;18:4679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Riedl A, Schmidtmann M, Stengel A, et al. Somatic comorbidities of irritable bowel syndrome: a systematic analysis. J Psychosom Res 2008;64:573–82. [DOI] [PubMed] [Google Scholar]