Abstract
Many of the respiratory pathogens show seasonal patterns and association with environmental factors. In this article, we conducted a cross‐sectional analysis of the influence of environmental factors, including climate variability, along with development indicators on the differential global spread and fatality of COVID‐19 during its early phase. Global climate data we used are monthly averaged gridded data sets of temperature, humidity and temperature anomaly. We used Human Development Index (HDI) to account for all nation wise socioeconomic factors that can affect the reporting of cases and deaths and build a stepwise negative binomial regression model. In the absence of a development indicator, all environmental variables excluding the specific humidity have a significant association with the spread and mortality of COVID‐19. Temperature has a weak negative association with COVID‐19 mortality. However, HDI is shown to confound the effect of temperature on the reporting of the disease. Temperature anomaly, which is being regarded as a global warming indicator, is positively associated with the pandemic's spread and mortality. Viewing newer infectious diseases like SARS‐CoV‐2 from the perspective of climate variability has a lot of public health implications, and it necessitates further research.
Keywords: COVID‐19, environmental factors, climate variability, temperature, humidity, temperature anomaly, Human Development Index
Key Points
Climate variability has a significant association with COVID‐19 transmission and mortality
Surface air temperature and Specific humidity does not have any statistically significant association with COVID‐19 transmission, though there is a weak relationship between temperature and the pandemic's mortality
Human development has a significant influence on case detection and reporting of COVID‐19; hence it can confound the effect of environmental variables
1. Introduction
Since the first reporting from Wuhan, Hubei province, China, the coronavirus disease has spread to more than a 150 countries across the globe, with a varying case‐fatality ratio among them (WHO Coronavirus (COVID‐19) Dashboard | WHO Coronavirus (COVID‐19) Dashboard With Vaccination Data, n.d; World Health Organization, 2020). Countries that were known to have a robust health system are now facing several hurdles not only in containing the disease but also in saving their affected population (Machhi et al., 2020). Although the same pathogen has affected all these countries, there exists a significant variation in the pattern and magnitude of spread, the proportion of patients who require critical care, and fatality among the confirmed cases (Mortality Analyses ‐ Johns Hopkins Coronavirus Resource Center (jhu.edu), n.d.; WHO Coronavirus (COVID‐19) Dashboard | WHO Coronavirus (COVID‐19) Dashboard With Vaccination Data, n.d). This difference can be attributed chiefly to the unlikeness among characteristics of either the host or the environment or both, which include general health and well‐being of the population, dissimilarities in demographic, environmental and socio‐political factors.
Environmental factors are well known to influence infectious disease epidemiology. In diseases of respiratory origin, low temperature and dry weather favor the survival of droplets and promote rapid transmission (Davis et al., 2016; Mäkinen et al., 2009; Yang & Marr, 2012). Studies have also found that absolute and relative humidity can modulate influenza virus survival and its transmission (Lowen et al., 2007; Shaman & Kohn, 2009). The perceivable relationship between environmental factors and several infectious diseases has also shifted our attention to the problem of climate variability. Temperature has been rising from a global perspective, with an accelerated soar of 0.18°C/decade in the past 30 years (Menne et al., 2020; World Meteorological Organization, 2020). Global warming can adversely affect all fields of life; hampered food production, increased occurrences of natural calamities, economic setbacks, impact on key and iconic ecosystems, and emerging and reemerging infectious diseases being only a few among them. WHO had warned the governments that climate change is likely to cause ∼2.5 Lakhs additional deaths per year, on account of infectious causes and heat stroke (Climate Change and Health, Environment, Climate Change and Health, 2018). Parameters like monthly surface air temperature anomaly (SATAn), global annual average temperature anomalies, and global temperature trends are widely being used as indicators of climate variability (World Meteorological Organization, 2017). Research papers that discuss the prospects of infectious disease burden to increase with climate variability are many. We found previous studies that identify regions with risk of ENSO, a large‐scale ocean surface temperature anomaly related phenomenon associated with infectious diseases (Fisman et al., 2016; Kovats et al., 1999). Climate anomalies have an effect on the occurrence of outbreaks of diseases like dengue, chikungunya, zika, rift valley fever, cholera, and plague (Kovats et al., 2003; Patz, 1996; Redding et al., 2017). Many articles are there on the influence of climate factors on the transmission of and mortality due to COVID‐19 (Bashir et al., 2020; Qi et al., 2020). Hence it is essential to look for any possible association of COVID‐19 with environmental factors, including climate variability, whatever the result is, and have many public health implications. We used the monthly SATAn as an indicator of climate variability.
Besides all these environmental and climatic variegations, there exist dissimilarities in social factors, economic well‐being, and national development across the globe, which can determine the capacity for case detection, voluntary endorsement of preventive strategies like self‐quarantining and self‐reporting to the health system and the travel and contact patterns of the citizens. Human Development Index (HDI) is a comprehensive measure of development used to compare countries worldwide. It gave weightage on three basic dimensions of human development, viz Life expectancy at birth, mean years of schooling and expected years of schooling, and the gross national income per capita (United Nations Development Programme, 2019). All these factors can have a significant stake in the occurrence and reporting of COVID‐19. The proportion of people in older age segments will be higher in countries with high HDI and hence the impact of COVID‐19 (Human Development Data Center | Human Development Reports (undp.org), n. d.; MRC Centre for Global Infectious Disease Analysis, J‐IDEA; Department of Infectious Disease Epidemiology, Imperial College London., 2020). Similarly, if more and more people are knowledgeable and aware of the pandemic, the reporting will be on a higher side. The knowledge about ways of spreading and strategies to prevent it will help the communities contain the outbreak. The factors contributing to the spread of the pandemic, like international travel, will be more in countries with higher income. Similarly, the ability of a country to purchase test kits can limit the reporting. All the factors explained above should be considered while studying the environmental impact on any disease's spread. We believe, in our current analysis, while studying the environmental impact on the disease's spread and mortality, the HDI of the country can surrogate all the confounders as mentioned heretofore. Our study aims to explore the association of country‐specific environmental factors like surface air temperature (SAT), specific humidity (SH), and the anomaly of air temperature (SATAn) with the reported COVID‐19 cases and deaths during the early phase of the pandemic.
2. Material and Methods
The effect of externalities, like meteorological and development factors in the transmission of SARS‐CoV2, was explored in our cross‐sectional analysis. Our outcome variables are the number of reported cases and deaths due to COVID‐19 in April 2020. We used the WHO's COVID‐19 data and included all countries with a minimum reported caseload of 10 coronavirus disease cases in April. We expressed our outcome variables as the number of COVID‐19 cases per million and the number of COVID‐19 deaths per 10 million to adjust for the population size. April 2020 is unique because the pandemic had reached most of the world by that time. One hundred and thirty‐five nations had reported more than ten COVID‐19 cases to the WHO in March 2020 and 157 in April. The early period of the pandemic is ideal for studying the effect of natural phenomena like environmental factors because their association with the outcome variables will be distorted later by the differential public health policies and actions taken by the governments. An analysis later in the timeline may be largely confounded by interventions at various levels in the system, like better preventive and curative services, including the introduction of newer drugs. Since we quantify the effect of environmental variables on the spread and mortality of COVID‐19, we need to minimize the undue influence of all other factors. Hence we decided to use the data of April in our analysis.
Our environmental explanatory variables are the monthly averaged values of SAT, SH, and SATAn for every country reported in this study. The relative humidity is highly dependent on atmospheric temperature and can vary considerably among indoor and outdoor environments. Absolute humidity is the fraction of water vapor over the air volume; therefore, it relies on the atmospheric temperature as the air volume changes with temperature. To avoid much of the collinearity between humidity and temperature, we used SH in our analysis. The SATAn is the difference between the observed temperature of a region and its long‐term average reference value. A positive anomaly indicates that the measured temperature is warmer than predicted. In contrast, a negative anomaly means the actual temperature is less than expected.
We extracted the explanatory environmental variables using a gridded product data set, simulated from the Noah 3.6.1 model in the Famine Earth Warning Systems Network Land Data Assimilation System, available from the National Aeronautics and Space Administration Goddard Earth Sciences Data and Information Systems‐Giovanni Version 4.34 (GES DISC Dataset: FLDAS Noah Land Surface Model L4 Global Monthly Anomaly 0.1 x 0.1 Degree (MERRA‐2 and CHIRPS). The data range from January 1982 to the present with global spatial coverage (60S, 180W, 90N, 180E) and 0.10° resolution. The LDAS systems (NLDAS and FLDAS) use optimal inputs to produce estimates of water balance and energy balance. We used the global SAT and SH data set, averaged for April, simulated from the FLDAS_Noah Land Surface Model L4, Figure 1. The monthly averaged SATAn for April, simulated from the same Noah 3.6.1 model in the FLDAS system, describes how the month compares to the 35‐year monthly climatology from 1982 to 2016, based on monthly data (Figure 1). We imported the gridded data set into a GIS platform (QGIS Desktop 3.12.0) and then randomly plotted 14 lakhs of points across the model. This procedure ensures representation from every 100 to 110 km2 of land area and can account for the variabilities present inside a country. We averaged all random data points at the country level, which is the unit of our analysis, to arrive at the nation wise mean of all our explanatory variables. The HDI was used in the analysis to adjust confounders reported elsewhere in this article. We used the HDI ranking 2018 and extracted the data from the UNDP's web portal (Human Development Data Center | Human Development Reports (undp.org), n.d.).
Figure 1.
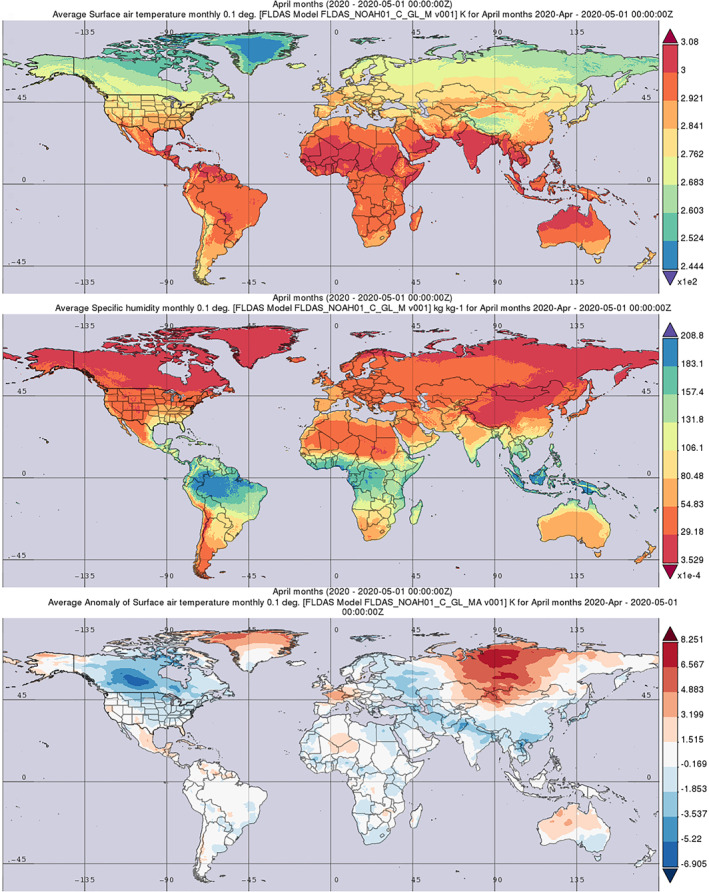
Monthly averaged—surface air temperature, specific humidity, and anomaly of surface air temperature for April. FLDAS Model—Data source: National Aeronautics and Space Administration Goddard Earth Sciences Data and Information Systems‐Giovanni Version 4.34.
2.1. Modeling COVID‐19 Cases and Deaths
Since our outcome variables represent count data, it warranted the use of a generalized linear model (GLM) to model the count data linearly. The purpose of GLM models is to generalize the linear combination of independent variables to the outcome variable by way of using a link function. It is to be noted that the link function in GLMs transform only the conditional mean of the outcome variable such that it is linearly related to the independent variables. The two GLM models that can model a count data using a log link function are Poisson and the negative binomial regression model. The Poisson regression assumes that variance is more or less equal to the mean. Due to the overdispersion of data, a negative binomial regression model with a system estimated dispersion parameter was selected as the final one. We constructed our model in a stepwise approach.
Initially, we tried to model the number of cases and deaths using the environmental variables. To observe the change in the explained variance (McFadden's R 2), we added HDI, the development indicator, into the same model. The best fit model was confirmed by comparing the Akaike information criterion and the Bayesian information criterion. We created a separate model to quantify the effect of a positive anomaly versus a negative anomaly, keeping all other variables the same. We used IBM SPSS statistics (Trial version 26.0) and R (version 3.6.3) to conduct all statistical analyses.
3. Results
Among all countries whose HDI data are available in the public domain, 168 reported their COVID‐19 statistics to WHO. An aggregate of 2,345,549 coronavirus cases and 183,313 deaths were reported in April 2020. One hundred fifty‐seven countries were eligible to be included in our analysis as they have a reported caseload of 10 or more. All the explanatory variables (SAT, SH, and SATAn) show significant (p < 0.001 for all correlations) bivariate correlation with the population‐adjusted number of cases and deaths. SAT and SH negatively correlate with country‐specific population‐adjusted COVID‐19 cases and deaths, whereas the HDI values and SATAn show a positive correlation.
3.1. Model 1. Modeling Cases and Deaths With Environmental Variables
In the initial model, which includes only the environmental variables, the SAT and SATAn were statistically significant predictors of both the population‐adjusted incidence of COVID‐19 cases and deaths (Tables 1 and 2). The NB regression model was significant for COVID‐19 cases (LR χ 2 [3] = 42.62, p < 0.001) with an AIC = 2098.5, BIC, 2118.7, and McFadden's R 2 = 0.192 and for deaths (LR χ 2 [3] = 117.23, p < 0.001) with an AIC = 1703.8, BIC = 1719.1, and McFadden's R 2 = 0.453.
Table 1.
Modeling the Population‐Adjusted Number of Reported Cases—Before and After Inclusion of Human Development Index (HDI)
| Explanatory variables | HDI not included | HDI included | ||||
|---|---|---|---|---|---|---|
| Coefficient (95% CI) | IRR (95% CI) | Statistical significance (p‐value) | Coefficient (95% CI) | IRR (95% CI) | Statistical significance (p‐value) | |
| SAT mean | −0.06 (−0.10, −0.02) | 0.94 (0.90, 0.98) | 0.001 | −0.03 (−0.06, 0.006) | 0.97 (0.94, 1.01) | 0.108 |
| SH mean | −0.01 (−0.08, 0.07) | 0.99 (0.92, 1.07) | 0.849 | 0.04 (−0.03, 0.10) | 1.04 (0.97, 1.11) | 0.271 |
| SATAn mean | 0.53 (0.29, 0.77) | 1.70 (1.34, 2.16) | <0.001 | 0.27 (0.07, 0.48) | 1.31 (1.07, 1.62) | 0.010 |
| HDI | ‐‐‐‐ | ‐‐‐‐ | ‐‐‐‐ | 6.9 (5.3, 8.5) | 998 (202, 4,943) | <0.001 |
Note. The regression coefficient (95% confidence interval) and its statistical significance are shown in this table. SAT, surface air temperature; SATAn, surface air temperature anomaly; SH, specific humidity.
Table 2.
Modeling the Population‐Adjusted Number of Reported Deaths—Before and After Inclusion of Human Development Index (HDI)
| Explanatory variables | HDI not included | HDI included | ||||
|---|---|---|---|---|---|---|
| Coefficient (95% CI) | IRR (95% CI) | Statistical significance (p‐value) | Coefficient (95% CI) | IRR (95% CI) | Statistical significance (p‐value) | |
| SAT mean | −0.17 (−0.21, −0.12) | 0.85 (0.81, 0.88) | <0.001 | −0.06 (−0.11, −0.02) | 0.94 (0.90, 0.99) | 0.009 |
| SH mean | 0.05 (−0.03, 0.13) | 1.06 (0.98, 1.14) | 0.182 | 0.003 (−0.06, 0.07) | 1.00 (0.94, 1.07) | 0.925 |
| SATAn mean | 0.79 (0.57, 1.02) | 2.21 (1.76, 2.78) | <0.001 | 0.56 (0.34, 0.77) | 1.75 (1.41, 2.16) | <0.001 |
| HDI | ‐‐‐‐ | ‐‐‐‐ | ‐‐‐‐ | 7.90 (5.83, 9.97) | 2,697 (339, 21,424) | <0.001 |
Note. The regression coefficient (95% confidence interval) and its statistical significance are shown in this table. SAT, surface air temperature; SATAn, surface air temperature anomaly; SH, specific humidity.
3.2. Model 2. Environmental Variables and the HDI on COVID‐19 Cases and Deaths
Inclusion of the HDI has improved the goodness of fit (AIC = 2041.2 [cases], 1659.4 [deaths], and BIC = 2059.6 [cases], 1677.7 [deaths]) and the explained variance (McFadden's R 2 = 0.406 for cases and 0.577 for deaths) of both the models for cases and deaths. However, the mean SATAn is the only environmental variable that could retain its statistical significance in both the above said, newly constructed NB regression models. Along with the SATAn, HDI came out as a significant predictor of the caseload and fatality. The mean SAT could retain its association only with the COVID‐19 deaths. As seen earlier, SH was associated neither with the caseload nor with the deaths (Tables 1 and 2). We consider the combined environmental variables—HDI model as the best fit one for our data as they possess better AIC and BIC.
3.3. HDI
The impact of HDI on COVID‐19 transmission and fatality is found substantial. An increment in the index by 0.01 can result in 71 (95% CI: 54–89) more cases per 1,000 cases and 82 (95% CI: 60–105) more deaths per 1,000 deaths over one month. HDI category‐wise (UNDP categorization) distribution of cases and deaths is shown in Figure 2. We did a bivariate analysis of HDI on reported cases and deaths. There is only a single nation with an HDI of less than 0.8 in the top 20 countries with the highest number of cases per million. HDI values show a reasonably good correlation with the number of reported cases and confirmed deaths (Spearman's coefficient = 0.76, p < 0.001)
Figure 2.
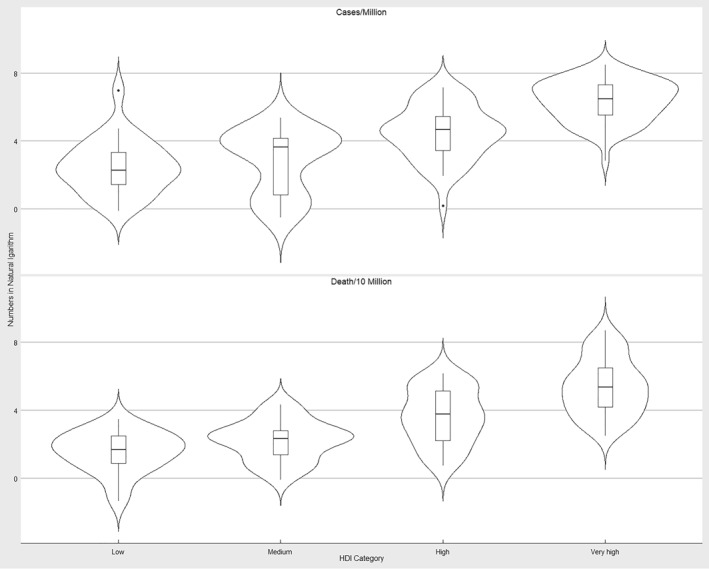
Distribution of cases and deaths among countries categorized based on Human Development Index (HDI). Violin plot showing the distribution of population‐adjusted cases and deaths due to COVID‐19. Countries were categorized according to UNDP classification based on the Human Development Index. The natural logarithm of cases and deaths is used for the plot.
3.4. Surface Air Temperature
The mean SAT fails to elicit a statistically significant association with the number of cases in the presence of other environmental and development variables. In contrast, it elicits a protective effect in the model for COVID‐19 deaths (IRR = 0.94 [95% CI: 0.90–0.99]). The IRR of SAT as per the best fit model for COVID‐19 deaths may be comprehended as 60 (100–10) fewer deaths per 1,000 confirmed deaths for every 1K rise in mean temperature. The inclusion of a development indicator has resulted in the failure of the SAT to retain its statistical significance in the model for COVID‐19 transmission. As most of the countries with a high HDI are located in temperate regions, and proportionately low HDI countries are in the tropical region, the higher incidence of cases in countries with cold climates is the impact of HDI (Figure 3).
Figure 3.
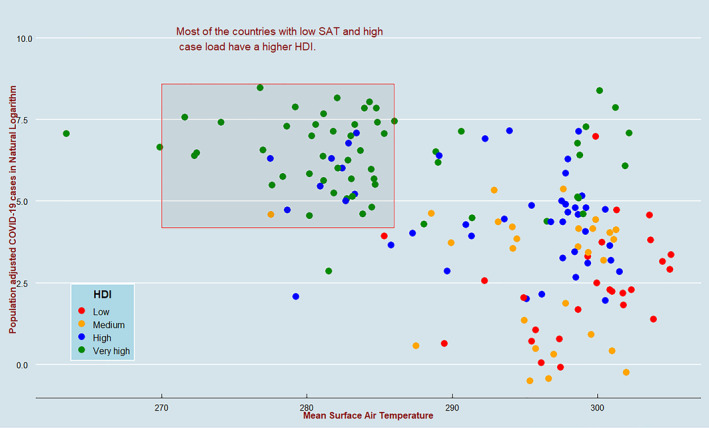
Scatterplot of population‐adjusted COVID‐19 cases and surface air temperature (SAT) mean showing the distribution of Human Development Index (HDI). The scatterplot shows a negative correlation between mean SAT and the natural logarithm of population‐adjusted COVID‐19 cases. Almost all of the countries with high caseloads and low temperatures have high HDI values.
3.5. Temperature Anomaly
The correlation plot of SATAn with population‐adjusted caseload and fatality in COVID‐19 portrays a statistically significant positive association for both outcomes (Figure 4). The IRR of SATAn is 1.31 (95% CI: 1.07–1.62) and 1.75 (95% CI: 1.41–2.16) for reported cases and confirmed deaths, respectively, which translates into 310 (70–620) additional cases for every 1,000 reported cases and 750 (410–1,160) more deaths for every 1,000 confirmed deaths over one month for each 1K positive anomaly. Based on the SATan data, we grouped the countries into two: those with a positive anomaly and a negative anomaly. A positive anomaly is associated with an IRR of 2.71 ([1.63, 4.50], [p < 0.001]) for cases and 5.15 ([2.76, 9.61], [p < 0.001]) for deaths when compared to a negative anomaly. The high HDI temperate countries that were having a significantly lesser ambient temperature compared to the rest of the world do not display any such pattern in the distribution of SATAn. Hence it is to recount that there is no confounding effect HDI in the air temperature anomaly—COVID‐19 caseload/fatality relationship.
Figure 4.
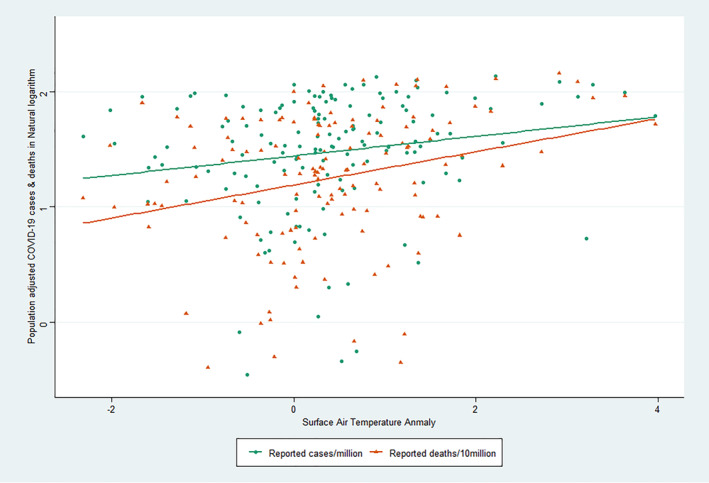
Scatterplot showing the distribution of surface air temperature anomaly and COVID‐19 cases and deaths (in natural logarithm). The scatterplot shows a positive correlation between the population‐adjusted number of COVID‐19 cases and deaths with the temperature anomaly.
4. Discussion
It is evident from this analysis that the overall social and economic development is a powerful determinant of the reported morbidity and mortality due to SARS‐CoV‐2 infection.
However, the environmental variables explained a higher variability in the COVID‐19 mortality (45.3%) compared to the disease spread (19.2%).
4.1. Temperature
Many studies had analyzed and reported the impact of meteorological factors on the transmission and fatality of many respiratory viruses, including COVID‐19 (Shi et al., 2020). A Hong Kong‐based study on SARS‐CoV‐1 proves that a higher risk of the epidemic is linked to a lower temperature (Lin et al., 2006). There is evidence of the diminished survival of the virus on hot surfaces (Riddell et al., 2020). A research article by Chen et al. is about a nonlinear relationship between climate variables and COVID‐19 transmission (Chen et al., 2020). However, there are published papers on the limited role of meteorological factors in COVID‐19 incidence (Chong et al., 2021; To et al., 2021). In the absence of a development indicator, the association between temperature and the disease's spread was significant. Nevertheless, the inclusion of HDI as a development indicator had nullified the statistical significance of temperature in the model. Although there is a negative association between temperature and COVID‐19 mortality, the confidence interval of the incidence rate ratio is closer to the null value. Hence, we think the impact of temperature on the pandemic's mortality, compared to other variables is minimal.
4.2. Humidity
Many research papers reported the association of relative humidity and absolute humidity with COVID‐19 spread and mortality (Mecenas et al., 2020; Wu et al., 2020). Since we used SH, which is the mass of water vapor over the mass of air, to avoid its dependency on atmospheric temperature, the effect of water vapor content of air on disease characteristics uninfluenced by atmospheric temperature is modeled in our analysis. We could not establish a significant association of SH with COVID‐19 transmission or mortality.
4.3. Temperature Anomaly
Climate variability and its relation to infectious diseases have become an essential point of debate for ecologists, climate scientists, and epidemiologists worldwide. A recently published article by Sasikumar and coworkers was able to establish an association between extreme climate variability and the spread of COVID‐19 pandemic in epicenters of India at the initial stage of transmission (Sasikumar et al., 2020). It is important to mention that these epicenters coincide with the CO2 emission hotspots (Sasikumar et al., 2020). Our article is the first of its kind that has studied the association between temperature anomaly and COVID‐19. Climate extremes were believed as essential contributors to evolution and are shown to cause genetic disquietudes in lower animals. Exposure to artificial heatwaves simulating global warming could result in differed gene expressions (Bergmann et al., 2010). Rodrı'guez‐Trelles and coworkers demonstrated that the extent of the genetic anomaly was analogous with the temperature anomalies (Rodríguez‐Trelles et al., 2013). Roberts and coworkers studied the effect of temperature on species susceptibility to RNA virus and found out that temperature may cause host shifts for viruses and increases the susceptibility of more susceptible species (Roberts et al., 2018). Curtailing the likelihood of survival of an infectious agent caused by a reduction in biodiversity, changing phenology, including the geographic expansion of living organisms triggered by the changing climates, and ever‐increasing human‐wildlife interactions may act as potentiating contributors for such a host‐species jump. Many of the emerging infectious diseases including Ebola, viral influenza, Nipah, and the SARS‐Cov are considered to originate from an animal host. Novel approaches in this regard, like modeling the likelihood of host‐human spill over of Lassa virus infections attributes a large extent of such events to the climate variability (Redding et al., 2016). We could make out from our study, a positive association for SATAn with the number of confirmed cases and deaths due to COVID‐19 contrasted to a protective effect by temperature on coronavirus mortality. We were not able to make out any specific pattern of distribution of temperature in its anomaly. Hence we think, it is not unwise to assume that climate variability has diverse causal pathways on the differential spread of and mortality due to COVID‐19. The human costs and economic costs of emerging infectious events, being on the rise point toward better reasoning of the present scenario.
4.4. HDI
Latitude specific spread of coronavirus disease pandemic across the temperate countries during its initial phase seems to have followed the pattern of other respiratory infections. However, it is an observable fact that temperate countries where the mean temperature is less when compared to tropical countries are mostly developed nations. As discussed earlier, HDI is a composite measure of counting development in a couple of areas. The association between development parameters and coronavirus disease transmission is not astounding. Nations with better per capita income have robust surveillance systems. Only a capable surveillance system can distinguish a significant proportion of the undetected cases, primarily mildly symptomatic and asymptomatic, which get reflected in the number of reported cases. Identifying all those persons who had contacted a confirmed patient, strict observance of them under the health system for any COVID‐19 related symptoms, and time‐bound testing for the virus's presence depends heavily on the robustness of the surveillance system and the economic well‐being of the state. The disease reporting is also determined by the population awareness of the disease, modes of transmission, and its symptoms, where literacy has a principal role. Those countries with a higher life expectancy at birth are expected to harbor a higher proportion of older adults, thus causing the reporting of cases and deaths on the upper side. Here it is essential to say that development parameters, if not adequately adjusted in modeling the transmission and mortality of COVID‐19, can confound the influence of climate factors.
5. Conclusion
Human development, differential across the globe, is a determinant of detecting and reporting cases and deaths due to COVID‐19. This fact should be considered while quantifying the impact of climate factors on any infectious disease with a cross‐border spread.
A good understanding of how the climate anomalies are associated with other contributing factors resulting in the emergence of newer infectious diseases and their propagation is necessary to use them for improved and sustainable health outcomes, which warrants the need for further research in this arena.
5.1. Limitations
Our analysis, based on country‐wise data, could have missed some of the microclimate variegations and regional spread of the disease.
Conflict of Interest
The authors declare no conflicts of interest relevant to this study.
Supporting information
Supporting Information S1
Acknowledgments
The authors are extremely grateful to the following individuals and organizations for their support in making this research possible. Dr Indu PS, Professor and Head, Department of Community Medicine, Government Medical College Thiruvananthapuram. Dr Siba S, Dr Harikrishnan, and Dr Betsy Varghese, Junior Residents, Department of Community Medicine, Government Medical College Thiruvananthapuram. All the staff, Kerala State Disaster Management Authority. National Aeronautics and Space Administration Goddard Earth Sciences Data and Information Systems‐Giovanni Version 4.34 for providing the environmental variables' data and graphical illustrations.
Thazhathedath Hariharan, H. , Surendran, A. T. , Haridasan, R. K. , Venkitaraman, S. , Robert, D. , Narayanan, S. P. , et al. (2021). Global COVID‐19 transmission and mortality—Influence of human development, climate, and climate variability on early phase of the pandemic. GeoHealth, 5, e2020GH000378. 10.1029/2020GH000378
Data Availability Statement
All data used for the analysis are available in the following data repository (https://doi.org/10.7910/DVN/ZDUYGB).
References
- Bashir, M. F. , Ma, B. , Bilal, Komal, B. , Bashir, M. A. , Tan, D. , & Bashir, M. (2020). Correlation between climate indicators and COVID‐19 pandemic in New York, USA. Science of the Total Environment, 728, 138835. 10.1016/j.scitotenv.2020.138835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergmann, N. , Winters, G. , Rauch, G. , Eizaguirre, C. , Gu, J. , Nelle, P. , et al. (2010). Population‐specificity of heat stress gene induction in northern and southern eelgrass Zostera marina populations under simulated global warming. Molecular Ecology, 19(14), 2870–2883. 10.1111/j.1365-294X.2010.04731.x [DOI] [PubMed] [Google Scholar]
- Chen, B. , Liang, H. , Yuan, X. , Hu, Y. , Xu, M. , Zhao, Y. , et al. (2020). Roles of meteorological conditions in COVID‐19 transmission on a worldwide scale (preprint). medRXiv (accepted for publication in BMJ Open). 10.1101/2020.03.16.20037168 [DOI] [Google Scholar]
- Chong, K. C. , Ran, J. , Lau, S. Y. F. , Goggins, W. B. , Zhao, S. , Wang, P. , et al. (2021). Limited role for meteorological factors on the variability in COVID‐19 incidence: A retrospective study of 102 Chinese cities. PLoS Neglected Tropical Diseases, 15(2), e0009056. 10.1371/journal.pntd.0009056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Climate Change and Health, Environment, Climate Change and Health . (2018). COP24 Special report: Health & Climate Change. Retrieved from World Health Organization. https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health [Google Scholar]
- Davis, R. E. , Dougherty, E. , McArthur, C. , Huang, Q. S. , & Baker, M. G. (2016). Cold, dry air is associated with influenza and pneumonia mortality in Auckland, New Zealand. Influenza and Other Respiratory Viruses, 10(4), 310–313. 10.1111/irv.12369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisman, D. N. , Tuite, A. R. , & Brown, K. A. (2016). Impact of El Niño Southern Oscillation on infectious disease hospitalization risk in the United States. Proceedings of the National Academy of Sciences, 113(51), 14589–14594. 10.1073/pnas.1604980113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Human development data (1990‐2018). (n.d.). Retrieved from http://hdr.undp.org/en/data
- Kovats, R. S. , Bouma, M. J. , Haines, A. , & WHO Task Force on Climate and Health . (1999). El Niño Southern Oscillation (ENSO) and health. World Health Organization. Retrieved from https://www.who.int/globalchange/publications/en/elnino.pdf [Google Scholar]
- Kovats, R. S. , Bouma, M. J. , Hajat, S. , Worrall, E. , & Haines, A. (2003). El Niño and health. The Lancet, 362(9394), 1481–1489. 10.1016/S0140-6736(03)14695-8 [DOI] [PubMed] [Google Scholar]
- Lin, K. , Fong, D. Y.‐T. , Zhu, B. , & Karlberg, J. (2006). Environmental factors on the SARS epidemic: Air temperature, passage of time and multiplicative effect of hospital infection. Epidemiology and Infection, 134(2), 223–230. 10.1017/S0950268805005054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowen, A. C. , Mubareka, S. , Steel, J. , & Palese, P. (2007). Influenza virus transmission is dependent on relative humidity and temperature. PLoS Pathogens, 3(10), 1470–1476. 10.1371/journal.ppat.0030151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Machhi, J. , Herskovitz, J. , Senan, A. M. , Dutta, D. , Nath, B. , Oleynikov, M. D. , et al. (2020). The natural history, pathobiology, and clinical manifestations of SARS‐CoV‐2 infections. Journal of Neuroimmune Pharmacology, 15(3), 359–386. 10.1007/s11481-020-09944-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mäkinen, T. M. , Juvonen, R. , Jokelainen, J. , Harju, T. H. , Peitso, A. , Bloigu, A. , et al. (2009). Cold temperature and low humidity are associated with increased occurrence of respiratory tract infections. Respiratory Medicine, 103(3), 456–462. 10.1016/j.rmed.2008.09.011 [DOI] [PubMed] [Google Scholar]
- Mecenas, P. , Bastosda, R. T. R. M. , Vallinoto, A. C. R. , & Normando, D. (2020). Effects of temperature and humidity on the spread of COVID‐19: A systematic review. PLoS One, 15(9), e0238339. 10.1371/journal.pone.0238339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menne, M. J. , Williams, C. N. , Gleason, B. E. , Rennie, J. J. , & Lawrimore, J. H. (2018). The global historical climatology network monthly temperature dataset, version 4. Journal of Climate, 31(24), 9835–9854. 10.1175/jcli-d-18-0094.1 [DOI] [Google Scholar]
- Mortality analyses. (n.d.). Retrieved from https://coronavirus.jhu.edu/data/mortality
- MRC Centre for Global Infectious Disease Analysis, J‐IDEA; Department of Infectious Disease Epidemiology, Imperial College London . (2020). Impact of non‐pharmaceutical interventions (NPIs) to reduce COVID‐19 mortality and healthcare demand, 16 March 2020. Retrieved from https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/891862/S0057_SAGE16_Imperial_Impact_of_NPIs_to_reduce_Mortality_and_Healthcare_Demand.pdf [Google Scholar]
- Patz, J. A. (1996). Global climate change and emerging infectious diseases. JAMA: The Journal of the American Medical Association, 275(3), 217. 10.1001/jama.1996.03530270057032 [DOI] [PubMed] [Google Scholar]
- Qi, H. , Xiao, S. , Shi, R. , Ward, M. P. , Chen, Y. , Tu, W. , et al. (2020). COVID‐19 transmission in Mainland China is associated with temperature and humidity: A time‐series analysis. Science of the Total Environment, 728, 138778. 10.1016/j.scitotenv.2020.138778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redding, D. W. , Moses, L. M. , Cunningham, A. A. , Wood, J. , & Jones, K. E. (2016). Environmental‐mechanistic modelling of the impact of global change on human zoonotic disease emergence: A case study of Lassa fever. Methods in Ecology and Evolution, 7(6), 646–655. 10.1111/2041-210X.12549 [DOI] [Google Scholar]
- Redding, D. W. , Tiedt, S. , Lo Iacono, G. , Bett, B. , & Jones, K. E. (2017). Spatial, seasonal and climatic predictive models of Rift Valley fever disease across Africa. Philosophical Transactions of the Royal Society B: Biological Sciences, 372(1725), 20160165. 10.1098/rstb.2016.0165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riddell, S. , Goldie, S. , Hill, A. , Eagles, D. , & Drew, T. W. (2020). The effect of temperature on persistence of SARS‐CoV‐2 on common surfaces. Virology Journal, 17(1), 145. 10.1186/s12985-020-01418-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts, K. E. , Hadfield, J. D. , Sharma, M. D. , & Longdon, B. (2018). Changes in temperature alter the potential outcomes of virus host shifts. PLoS Pathogens, 14(10), e1007185. 10.1371/journal.ppat.1007185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez‐Trelles, F. , Tarrío, R. , & Santos, M. (2013). Genome‐wide evolutionary response to a heat wave in Drosophila. Biology Letters, 9(4), 20130228. 10.1098/rsbl.2013.0228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sasikumar, K. , Nath, D. , Nath, R. , & Chen, W. (2020). Impact of extreme hot climate on COVID‐19 outbreak in India. GeoHealth, 4(12), e2020GH000305. 10.1029/2020GH000305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaman, J. , & Kohn, M. (2009). Absolute humidity modulates influenza survival, transmission, and seasonality. Proceedings of the National Academy of Sciences, 106(9), 3243–3248. 10.1073/pnas.0806852106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi, P. , Dong, Y. , Yan, H. , Zhao, C. , Li, X. , Liu, W. , et al. (2020). Impact of temperature on the dynamics of the COVID‐19 outbreak in China. Science of the Total Environment, 728, 138890. 10.1016/j.scitotenv.2020.138890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- To, T. , Zhang, K. , Maguire, B. , Terebessy, E. , Fong, I. , Parikh, S. , & Zhu, J. (2021). Correlation of ambient temperature and COVID‐19 incidence in Canada. Science of the Total Environment, 750, 141484. 10.1016/j.scitotenv.2020.141484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations Development Programme . (2019). UNDP. 2019. Human Development Report 2019. Beyond income, beyond averages, beyond today: Inequalities in human development in the 21st century. New York: United Nations Development Programme. http://hdr.undp.org/en/content/human-development-report-2019 [Google Scholar]
- WHO coronavirus disease (COVID‐19) dashboard . (n.d.) . Retrieved from https://covid19.who.int
- World Health Organization . (2020). Report of the WHO‐China joint mission on coronavirus disease 2019 (COVID‐19). World Health Organization. Retrieved from https://www.who.int/publications/i/item/report-of-the-who-china-joint-mission-on-coronavirus-disease-2019-(covid-19) [Google Scholar]
- World Meteorological Organization . (2017). WMO guidelines on generating a defined set of national climate monitoring products. https://library.wmo.int/doc_num.php?explnum_id=4213 [Google Scholar]
- World Meteorological Organization . (2020). WMO statement on the state of the global climate in 2019. World Meteorological Organization. https://library.wmo.int/doc_num.php?explnum_id=10211 [Google Scholar]
- Wu, Y. , Jing, W. , Liu, J. , Ma, Q. , Yuan, J. , Wang, Y. , et al. (2020). Effects of temperature and humidity on the daily new cases and new deaths of COVID‐19 in 166 countries. Science of the Total Environment, 729, 139051. 10.1016/j.scitotenv.2020.139051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang, W. , & Marr, L. C. (2012). Mechanisms by which ambient humidity may affect viruses in aerosols. Applied and Environmental Microbiology, 78(19), 6781–6788. 10.1128/AEM.01658-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information S1
Data Availability Statement
All data used for the analysis are available in the following data repository (https://doi.org/10.7910/DVN/ZDUYGB).


