Graphical abstract
Keywords: COVID-19, PM10, COVID-19 mortality, COVID-19 severity
Abstract
Background
Age, sex, race and comorbidities are insufficient to explain why some individuals remain asymptomatic after SARS-CoV-2 infection, while others die. In this sense, the increased risk caused by the long-term exposure to air pollution is being investigated to understand the high heterogeneity of the COVID-19 infection course.
Objectives
We aimed to assess the underlying effect of long-term exposure to NO2 and PM10 on the severity and mortality of COVID-19.
Methods
A retrospective observational study was conducted with 2112 patients suffering COVID-19 infection. We built two sets of multivariate predictive models to assess the relationship between the long-term exposure to NO2 and PM10 and COVID-19 outcome. First, the probability of either death or severe COVID-19 outcome was predicted as a function of all the clinical variables together with the pollutants exposure by means of two regularized logistic regressions. Subsequently, two regularized linear regressions were constructed to predict the percentage of dead or severe patients. Finally, odds ratios and effects estimates were calculated.
Results
We found that the long-term exposure to PM10 is a more important variable than some already stated comorbidities (i.e.: COPD/Asthma, diabetes, obesity) in the prediction of COVID-19 severity and mortality. PM10 showed the highest effects estimates (1.65, 95% CI 1.32–2.06) on COVID-19 severity. For mortality, the highest effect estimates corresponded to age (3.59, 95% CI 2.94–4.40), followed by PM10 (2.37, 95% CI 1.71–3.32). Finally, an increase of 1 µg/m3 in PM10 concentration causes an increase of 3.06% (95% CI 1.11%-4.25%) of patients suffering COVID-19 as a severe disease and an increase of 2.68% (95% CI 0.53%-5.58%) of deaths.
Discussion
These results demonstrate that long-term PM10 burdens above WHO guidelines exacerbate COVID-19 health outcomes. Hence, WHO guidelines, the air quality standard established by the Directive 2008/50/EU, and that of the US-EPA should be updated accordingly to protect human health.
1. Introduction
COVID-19 is caused by the Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV-2). Age, sex, race, as well as a number of comorbidities, including hypertension, cardiovascular diseases, obesity and diabetes have been reported as determinants to overcome COVID-19 (Ejaz et al., 2020, Grasselli et al., 2020, Richardson et al., 2020). However, these factors have been insufficient to explain the high heterogeneity of the infection course. Other known causes are genetic factors of the host are pointed out as individual risk factors (Hu et al., 2021), while the potential role of environmental stressors is currently being explored (Bashir et al., 2020, Tian et al., 2021).
Exposure to air pollution is associated with an increased oxidative stress, which in turn, is the primary cause for respiratory and cardiovascular morbidity and premature mortality (Khafaie et al., 2016, Yang et al., 2017, World Health Organization, 2020, Hahad et al., 2021). In addition, exposure to air pollutants might lead to more severe and lethal forms of respiratory viruses, including SARS-CoV-2 (Domingo and Rovira, 2020, Paital and Agrawal, 2020, Marquès and Domingo, 2021). This topic is being explored by means of ecological studies focused on the impact of the typical environmental pollutants from urban areas (i.e.: PM10, PM2.5, NO2, O3) on the incidence, mortality and/or lethality of COVID-19 (Copat et al., 2020, Frontera et al., 2020, Marquès et al., 2020, Meo et al., 2020, Sciomer et al., 2020, Maleki et al., 2021, Zheng et al., 2021). According to Barnett-Itzhaki and Levi (2021), long-term exposure to air pollutants concentrations exceeding WHO guidelines might exacerbate morbidity and mortality rates from COVID-19.
To date, the severity and mortality of COVID-19 considering the long-term exposure to environmental pollution in addition to the individual clinical variables has not been addressed yet. The present study was aimed at assessing the underlying effect of long-term exposure to NO2 and PM10 on the severity and mortality of COVID-19. Clinical variables of individuals admitted to various hospitals in Catalonia (Spain) due to COVID-19 infection have been examined together with the clinical histories and the estimated long-term exposure to NO2 and PM10.
2. Methods
2.1. Study design
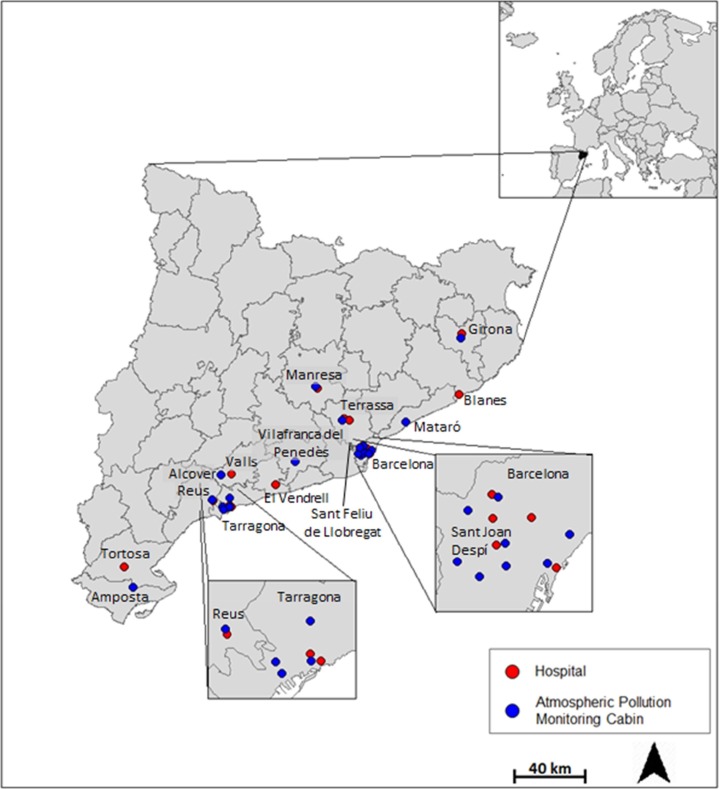
A retrospective observational study was conducted with 2112 patients with COVID-19 infection admitted to Catalan hospitals between April and June 2020. Patients aging at least 18 years and staying at the hospital for a minimum of 24 h were invited to join the cohort (Cohort registration code NCT04407273-STACOV). Hospitals participating in the study were the following: Pius Hospital de Valls, Hospital Verge de la Cinta (Tortosa), Hospital Universitari Sant Joan (Reus), Hospital Universitari de Joan XXIII (Tarragona), Hospital Sant Pau i Santa Tecla (Tarragona), Hospital del Vendrell, Hospital del Mar (Barcelona), Hospital HM Delfos (Barcelona), Hospital Universitari Vall d’Hebron (Barcelona), Hospital Santa Creu Sant Pau (Barcelona), Hospital de Santa Caterina (Girona), Althaia (Manresa), Hospital Comarcal de Blanes, Consorci Sanitari de Terrassa, Hospital Moisès Broggi (Sant Joan Despí) (Fig. 1 ).
Fig. 1.
Location of the hospitals and atmospheric pollution monitoring cabins.
2.2. Clinical data
An ad hoc database with data on anthropometry, personal medical antecedents and clinical outcomes during the stay in the hospitals was built. All data were anonymized and recorded in accordance with legal provisions of the protection of personal data in Spain and European Union Regulations (EU) 2016/6799 on the physical protection of the treatment of personal data. The study was compliant with the Declaration of Helsinki. The Ethics Committee of the Pere Virgili Health Research Institute approved the study (Ref. CEIM: 106/2020). More details on confidentiality are already described elsewhere (Masana et al., 2020).
2.3. Long-term exposure to environmental pollution
The closest cabin from the Catalan Atmospheric Pollution Monitoring and Forecasting Network was allocated to each hospital participating in the study (Fig. 1). The cities of Tarragona and Barcelona count with several atmospheric pollution monitoring cabins as well as several hospitals included in the study. In those cases, we averaged the measurements of all cabins and allocated them to all the hospitals in each city. The only cabin from Terrassa was allocated to the two hospitals from this city. Time series data of hourly average NO2 and PM10 from the air monitoring cabins were obtained from the open data portal from the Government of Catalonia (Generalitat de Catalunya, 2021). The average long-term exposure to PM10 and NO2 was estimated by calculating the median concentration with data from January 1, 2014 to March 13, 2020. This selected time-period is linked to data availability, the COVID-19 outbreak, and that exposure of a year or more can be considered as a long-term exposure (Hoek et al., 2013). The WHO air quality guideline values for PM10 (20 μg/m3 annual mean) and NO2 (40 μg/m3 annual mean) were considered as thresholds to determine low and high long-term exposures in the multivariate predictive models (World Health Organization, 2020).
2.4. Statistical analysis
Continuous variables were tested for normality using the Shapiro–Wilk test. Data are presented as medians and 25th and 75th percentiles for continuous variables with a non-normal distribution or as the means and standard deviations (SDs) for those variables with a normal distribution. Unless indicated otherwise, categorical variables are reported as percentages. Differences between groups were analysed using the non-parametric Mann–Whitney test or the Student’s parametric t test for continuous variables, and the chi-square test or Fisher’s exact test for categorical variables. All continuous variables were standardized and normalized when necessary.
Two sets of multivariate predictive models were carried out in order to assess the relationship between the pollutants and COVID-19 outcome. Firstly, we built two regularized logistic regressions where the probability of either death or severe COVID-19 outcome was predicted as a function of all the clinical variables together with the exposure to high concentrations of pollutants. These show the harmful effect of PM10 but not the importance of this variable versus the rest of variables under analysis. Therefore, a series of random forest models with the same setup as the regressions were carried out to assess the relative importance of each variable by determining the out-of-bag accuracy before and after variable permutation.
Secondly, two regularized linear regressions were constructed to predict the percentage of dead or severe patients in each of the hospitals involved in the study. Since our “n” was small (16), we maintained only the most relevant clinical variables (age, sex, smoking, cancer and diabetes) and environmental pollutants (PM10).
Finally, we provide odds ratios for the logistic regressions and estimates for the linear regressions, both with 95% confidence intervals and p-values.
All continuous variables were normalized when needed prior to model training. Missing data was imputed by multiple imputation by chained equations with a random forest based method (White et al., 2011).
All statistical analyses were performed using the R software package version 4.0. (R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing. 2020. Vienna, Austria. URL: https:// www.R-project.org/).
3. Results
The demography, anthropometry and clinical characteristics of the studied population, together with the long-term exposure to NO2 and PM10 are summarized in Table 1 . Additional clinical details, such as clinical inflammation and respiratory biomarkers, as well as drug therapies, are described elsewhere (Masana et al., 2020). The cohort participants were mainly men (57.1%). The average age of the infected individuals was 66 years old, being slightly older (72 years) those admitted to Hospital del Vendrell and Althaia (Manresa). Most of the individuals hereby assessed underwent mild COVID-19 (67.1%). Specifically, the highest rates of mild COVID-19 corresponded to Hospital Comarcal de Blanes (76.0%) and Hospital Moisès Broggi (81.0%), Pius Hospital de Valls (81.5%) and Hospital del Vendrell (86.6%). In contrast, the highest rates of mortality were found in Hospital de Santa Caterina (20.5%), Hospital Sant Joan de Reus (21.7%) and Althaia (30.2%). In turn, Reus, Girona and Manresa were above the WHO guideline value for PM10 (20 µg/m3), while Valls, El Vendrell, Mataró and Sant Joan Despí were below this reference concentration. In addition, those individuals affected by COVID-19 in Girona and Manresa had a previous high rate of one or more respiratory and cardiovascular diseases, which in turn, might be related to long-term exposure to PM10 (Henderson et al., 2011, Zhu et al., 2021). Finally, up to 31.4% of patients infected with COVID-19 in Terrassa suffered severe COVID-19, or even died. Furthermore, a high rate of individuals showed high blood pressure, stroke and COPD/asthma. The population living in Terrassa had the highest long-term exposure to PM10, while they were the only group exposed to a NO2 concentration above the reference value (40 µg/m3). Finally, similar rates of mild, severe and death patients were found in Barcelona and Amposta. Surprisingly, Barcelona was above the PM10 WHO threshold and close to the NO2 guideline level, while Amposta is one of the localities with the lowest concentrations of NO2 and PM10. Table 2 summarizes the characteristics of the cohort according to the COVID-19 severity (mild, severe and death). The average age of mild, severe and death patients was 64, 62 and 80 years old, respectively. COVID-19 severity increased as the incidence of history and chronic diseases (high blood pressure, coronary heart disease, stroke, COPD/Asthma, as well as chronic liver, kidney and rheumatologic diseases, and cancer) increased. In contrast, the clinical outcomes (Intensive Care Unit hospitalization, fever, cough, dyspnea, bilateral alteration thorax X ray, Acute respiratory distress syndrome, high-flow mechanical ventilation and tracheal intubation) occurred more frequently in those patients suffering severe COVID-19 than in those who died. Finally, the exposure to NO2 and PM10 did not differ among COVID-19 severity groups. Unfortunately, long-term exposure of each individual depends only on the city of hospitalization, and consequently, only 11 average long-term exposures to NO2 and PM10 for all the 2112 individuals have been estimated.
Table 1.
Demography, anthropometry, clinical characteristics and long-term exposure to NO2 and PM10 of the population included in the study.
| Pius Hospital de Valls | Hospital Verge de la Cinta (Tortosa) | Hospital Universitari Sant Joan (Reus) |
Hospital Universitari Joan XXIII Hospital Sant Pau i Santa Tecla (Tarragona) |
Hospital del Vendrell | Hospital Santa Creu Sant Pau Hospital Universitari Vall d’Hebron Hospital del Mar Hospital HM Delfos (Barcelona) |
Hospital de Santa Caterina (Girona) | Althaia (Manresa) |
Hospital Comarcal de Blanes | Consorci Sanitari de Terrassa | Hospital Moises Broggi (Sant Joan Despí) |
|
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | 81 | 62 | 143 | 172 | 112 | 572 | 220 | 248 | 100 | 302 | 100 |
| Sex (female) | 28 (34.6%) | 27 (43.5%) | 57 (39.9%) | 58 (33.7%) | 47 (42.0%) | 282 (49.3%) | 76 (34.5%) | 102 (41.1%) |
42 (42.0%) | 153 (50.7%) | 34 (34.0%) |
| Age | 64.0 [51.0;76.0] | 69.0 [57.0;75.8] | 64.0 [55.0;77.0] | 70.0 [57.0;78.2] | 72.0 [56.8;82.0] | 65.5 [53.0;79.0] | 66.0 [53.0;81.0] | 72.0 [61.0;80.0] | 62.0 [53.8;74.2] | 70.0 [59.0;80.0] | 50.5 [43.0;56.2] |
| Smoker | 4 (14.8%) | 2 (3.39%) | 6 (4.65%) | 7 (4.27%) | 7 (7.37%) | 32 (5.68%) | 16 (7.66%) | 12 (4.84%) | 6 (6.59%) | 8 (2.68%) | 5 (5.00%) |
| Personal history of diseases | |||||||||||
| High Blood Pressure | 34 (42.0%) | 36 (58.1%) | 73 (51.0%) | 93 (54.1%) | 60 (53.6%) | 293 (51.4%) | 107 (48.6%) | 131 (52.8%) | 47 (47.5%) | 158 (52.3%) | 21 (21.0%) |
| Diabetes | 16 (19.8%) | 21 (33.9%) | 37 (25.9%) | 47 (27.3%) | 21 (18.8%) | 127 (22.2%) | 54 (24.5%) | 71 (28.6%) | 30 (30.0%) | 54 (17.9%) | 16 (16.0%) |
| Obesity | 9 (45.0%) | 23 (42.6%) | 16 (26.7%) | 47 (28.8%) | 16 (22.5%) | 179 (32.7%) | 59 (28.5%) | 40 (16.8%) | 30 (41.1%) | 80 (30.9%) | 19 (19.2%) |
| Coronary Heart Disease | 2 (2.50%) | 5 (8.06%) | 6 (4.20%) | 22 (12.8%) | 11 (9.82%) | 67 (11.7%) | 25 (11.4%) | 17 (6.85%) | 13 (13.0%) | 26 (8.61%) | 2 (2.00%) |
| Stroke | 1 (1.23%) | 3 (4.84%) | 10 (6.99%) | 10 (5.81%) | 3 (2.68%) | 44 (7.69%) | 14 (6.36%) | 15 (6.05%) | 8 (8.00%) | 24 (7.95%) | 0 (0.00%) |
| Peripheral Arterial Disease | 2 (2.47%) | 1 (1.61%) | 5 (3.50%) | 12 (6.98%) | 1 (0.89%) | 29 (5.07%) | 17 (7.73%) | 19 (7.66%) | 4 (4.00%) | 9 (2.98%) | |
| Heart Failure | 0 (0.00%) | 2 (3.23%) | 8 (5.59%) | 16 (9.30%) | 10 (8.93%) | 50 (8.74%) | 36 (16.4%) | 21 (8.47%) | 9 (9.00%) | 27 (8.94%) | 0 (0.00%) |
| COPD/Asthma | 8 (9.88%) | 6 (9.68%) | 13 (9.09%) | 28 (16.3%) | 25 (22.3%) | 102 (17.9%) | 50 (22.7%) | 42 (16.9%) | 17 (17.0%) | 61 (20.2%) | 9 (9.00%) |
| Chronic Liver disease | 0 (0.00%) | 0 (0.00%) | 8 (5.59%) | 8 (4.65%) | 0 (0.00%) | 12 (2.10%) | 4 (1.82%) | 10 (4.03%) | 2 (2.00%) | 11 (3.64%) | 3 (3.00%) |
| Chronic Kidney disease | 5 (6.17%) | 2 (3.23%) | 14 (9.79%) | 12 (6.98%) | 14 (12.5%) | 57 (9.98%) | 26 (11.8%) | 40 (16.1%) | 9 (9.00%) | 32 (10.6%) | 0 (0.00%) |
| Rheumatologic disease | 4 (4.94%) | 2 (3.23%) | 6 (4.20%) | 6 (3.51%) | 4 (3.57%) | 34 (5.95%) | 5 (2.27%) | 12 (4.84%) | 1 (1.00%) | 25 (8.28%) | 4 (4.00%) |
| Cancer | 11 (13.6%) | 5 (8.06%) | 16 (11.2%) | 28 (16.3%) | 17 (15.2%) | 48 (8.42%) | 27 (12.3%) | 41 (16.5%) | 7 (7.00%) | 37 (12.3%) | 1 (1.00%) |
| Clinical outcomes | |||||||||||
| Intensive Care Unit Hospitalization | 9 (11.1%) | 18 (29.0%) | 32 (22.4%) | 43 (25.0%) | 1 (0.89%) | 72 (12.6%) | 38 (17.4%) | 55 (22.2%) | 11 (11.0%) | 30 (9.93%) | 13 (13.0%) |
| Fever | 77 (95.1%) | 55 (88.7%) | 126 (88.1%) | 147 (85.5%) | 91 (82.0%) | 446 (78.0%) | 190 (86.4%) | 207 (84.5%) | 87 (87.9%) | 251 (83.1%) | 84 (84.0%) |
| Cough | 49 (60.5%) | 50 (80.6%) | 108 (75.5%) | 117 (68.0%) | 89 (80.2%) | 395 (69.2%) | 127 (62.9%) | 178 (72.7%) | 71 (71.0%) | 196 (64.9%) | 67 (67.0%) |
| Dyspnea | 25 (30.9%) | 39 (62.9%) | 96 (68.1%) | 106 (61.6%) | 80 (71.4%) | 312 (54.6%) | 159 (72.6%) | 138 (56.3%) | 67 (68.4%) | 150 (49.7%) | 66 (66.0%) |
| Bilateral alteration Thorax X ray | 58 (71.6%) | 52 (83.9%) | 105 (73.9%) | 138 (80.2%) | 81 (72.3%) | 362 (63.4%) | 162 (73.6%) | 215 (87.8%) | 77 (77.0%) | 224 (74.9%) | 87 (87.0%) |
| Acute Respiratory Distress Syndrome | 11 (13.6%) | 14 (22.6%) | 61 (43.0%) | 68 (39.5%) | 15 (13.4%) | 122 (21.4%) | 70 (31.8%) | 136 (54.8%) | 19 (19.2%) | 77 (25.6%) | 17 (17.3%) |
| Respiratory Failure | 14 (17.3%) | 10 (38.5%) | 62 (43.4%) | 43 (28.1%) | 37 (33.0%) | 73 (26.1%) | 80 (37.9%) | 92 (41.1%) | 19 (20.2%) | 65 (25.5%) | 11 (22.9%) |
| High-Flow Mechanical Ventilation | 2 (2.47%) | 4 (6.45%) | 12 (8.39%) | 47 (27.3%) | 1 (0.89%) | 68 (11.9%) | 62 (28.2%) | 70 (28.2%) | 29 (29.0%) | 58 (19.3%) | 17 (17.3%) |
| Invasive Mechanical Ventilation. Tracheal Intubation | 7 (8.64%) | 12 (19.4%) | 25 (17.5%) | 35 (20.3%) | 2 (1.79%) | 58 (10.1%) | 36 (16.4%) | 41 (16.5%) | 11 (11.0%) | 24 (7.97%) | 11 (11.2%) |
| Disseminated Intravascular Coagulation | 1 (1.23%) | 1 (1.61%) | 7 (4.93%) | 5 (2.92%) | 0 (0.00%) | 2 (0.35%) | 4 (1.82%) | 9 (3.63%) | 4 (4.04%) | 2 (0.67%) | 1 (1.02%) |
| Acute Renale Failure | 15 (18.5%) | 11 (17.7%) | 29 (20.3%) | 33 (19.2%) | 30 (26.8%) | 65 (11.4%) | 36 (16.4%) | 68 (27.5%) | 11 (11.0%) | 41 (13.6%) | 2 (2.04%) |
| Liver alterations | 2 (2.47%) | 1 (1.61%) | 5 (3.52%) | 9 (5.23%) | 1 (0.89%) | 11 (1.92%) | 6 (2.73%) | 22 (8.91%) | 5 (5.00%) | 5 (1.67%) | 0 (0.00%) |
| Shock | 1 (1.23%) | 5 (8.06%) | 23 (16.1%) | 15 (8.72%) | 2 (1.79%) | 18 (3.16%) | 12 (5.45%) | 30 (12.1%) | 4 (4.00%) | 22 (7.33%) | 0 (0.00%) |
| Severity | |||||||||||
| Mild | 66 (81.5%) | 43 (69.4%) | 90 (62.9%) | 102 (59.3%) | 97 (86.6%) | 390 (68.2%) | 133 (60.5%) | 132 (53.2%) | 76 (76.0%) | 207 (68.5%) | 81 (81.0%) |
| Severe | 8 (9.88%) | 12 (19.4%) | 22 (15.4%) | 39 (22.7%) | 9 (8.04%) | 94 (16.4%) | 42 (19.1%) | 41 (16.5%) | 19 (19.0%) | 40 (13.2%) | 18 (18.0%) |
| Death | 7 (8.64%) | 7 (11.3%) | 31 (21.7%) | 31 (18.0%) | 6 (5.36%) | 88 (15.4%) | 45 (20.5%) | 75 (30.2%) | 5 (5.00%) | 55 (18.2%) | 1 (1.00%) |
| Long-term exposure to environmental pollutants | Alcover | Amposta | Reus | Tarragona | Vilafranca del Penedès | Barcelona | Girona | Manresa | Mataró | Terrassa | Sant Feliu de Llobregat |
| NO2 (µg/m3) | 9.89 | 14.73 | 18.72 | 21.05 | 16.88 | 38.25 | 29.55 | 30.22 | 24.36 | 40.77 | 21.36 |
| PM10 (µg/m3) | 19.55 | 19.12 | 21.98 | 19.08 | 19.25 | 24.18 | 23.98 | 23.09 | 19.29 | 24.38 | 19.90 |
Table 2.
Demography, anthropometry, clinical characteristics and long-term exposure to environmental pollutants of the population according to COVID-19 severity
| Mild | Severe | Death | p.overall | |
|---|---|---|---|---|
| N | 1417 | 344 | 351 | <0.001 |
| Age | 64.0 [52.0;77.0] |
62.0 [53.0;71.0] | 80.0 [73.0;87.0] |
<0.001 |
| Sex (female) | 646 (45.6%) | 117 (34.0%) | 143 (40.7%) | <0.001 |
| Smoker | 64 (4.83%) | 23 (7.06%) | 18 (5.39%) | |
| Personal history of diseases | ||||
| High Blood Pressure | 649 (45.9%) | 156 (45.5%) | 248 (70.7%) | <0.001 |
| Diabetes | 296 (20.9%) | 84 (24.4%) | 114 (32.5%) | <0.001 |
| Obesity | 320 (26.9%) | 108 (36.4%) | 90 (29.6%) | 0.005 |
| Coronary Heart Disease | 120 (8.47%) | 29 (8.43%) | 47 (13.4%) | 0.014 |
| Stroke | 78 (5.50%) | 18 (5.23%) | 36 (10.3%) | 0.003 |
| Peripheral Arterial Disease | 51 (3.60%) | 15 (4.36%) | 33 (9.40%) | <0.001 |
| Heart Failure | 98 (6.92%) | 14 (4.07%) | 67 (19.1%) | <0.001 |
| COPD/Asthma | 212 (15.0%) | 59 (17.2%) | 90 (25.6%) | <0.001 |
| Chronic Liver disease | 37 (2.61%) | 7 (2.03%) | 14 (3.99%) | 0.250 |
| Chronic Kidney disease | 118 (8.33%) | 20 (5.81%) | 73 (20.8%) | <0.001 |
| Rheumatologic disease | 64 (4.52%) | 19 (5.52%) | 20 (5.70%) | 0.549 |
| Cancer | 137 (9.68%) | 37 (10.8%) | 64 (18.2%) | <0.001 |
| Clinical outcomes | ||||
| Intensive Care Unit Hospitalization | 11 (0.78%) | 230 (67.1%) | 81 (23.1%) | <0.001 |
| Fever | 1152 (81.5%) | 313 (91.0%) | 296 (84.8%) | <0.001 |
| Cough | 946 (67.3%) | 277 (81.2%) | 224 (65.5%) | <0.001 |
| Dyspnea | 707 (50.1%) | 283 (82.3%) | 248 (71.3%) | <0.001 |
| Bilateral alteration Thorax X ray | 949 (67.3%) | 317 (92.2%) | 295 (84.5%) | <0.001 |
| Acute Respiratory Distress Syndrome | 96 (6.79%) | 257 (74.9%) | 257 (73.6%) | <0.001 |
| Respiratory Failure | 215 (20.9%) | 141 (43.3%) | 150 (54.7%) | <0.001 |
| High-Flow Mechanical Ventilation | 26 (1.84%) | 224 (65.1%) | 120 (34.2%) | <0.001 |
| Invasive Mechanical Ventilation. Tracheal Intubation | 1 (0.07%) | 188 (54.7%) | 73 (20.8%) | <0.001 |
| Disseminated Intravascular Coagulation | 5 (0.35%) | 13 (3.80%) | 18 (5.16%) | <0.001 |
| Acute Renale Failure | 119 (8.42%) | 78 (22.7%) | 144 (41.1%) | <0.001 |
| Liver alterations | 19 (1.35%) | 23 (6.69%) | 25 (7.14%) | <0.001 |
| Shock | 3 (0.21%) | 55 (16.0%) | 74 (21.2%) | <0.001 |
| Long-term exposure to environmental pollutants | ||||
| NO2 (µg/m3) | 30.2 | 30.2 | 30.2 | |
| PM10 (µg/m3) | 24.0 | 24.0 | 24.0 |
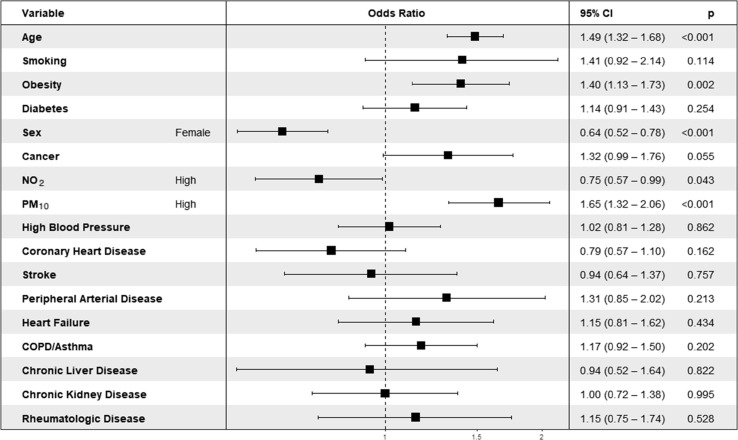
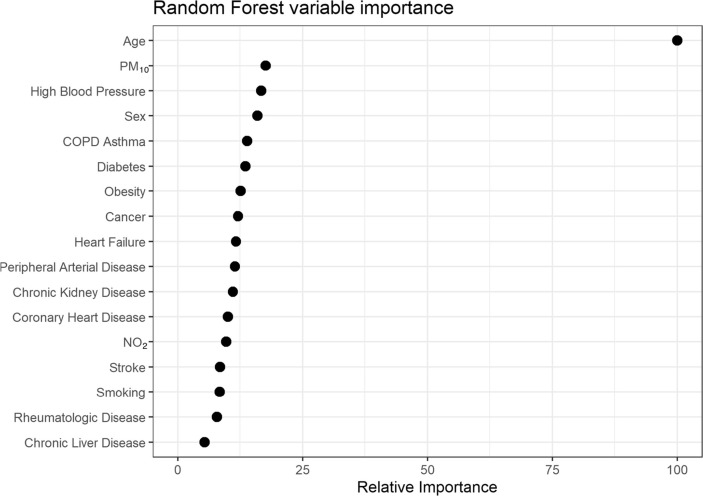
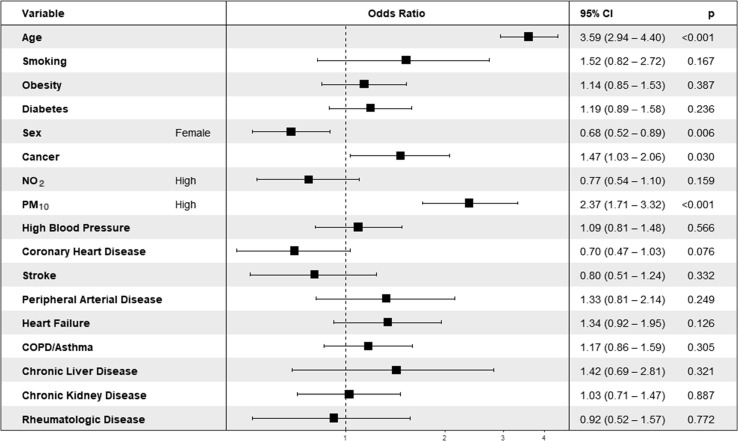
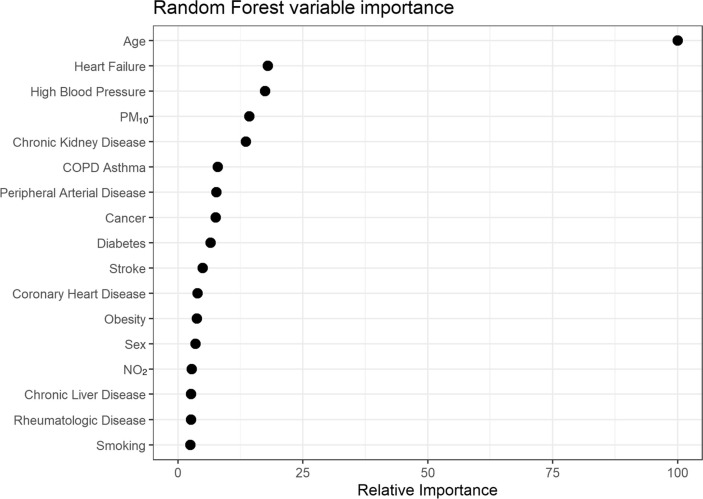
The multivariate analysis indicates that along with the age, sex and obesity, long-term exposure to NO2 and PM10 are significant variables for COVID-19 severity (Fig. 2 ). In turn, the effect estimates for NO2 and PM10 are 0.75 (95% CI 0.57–0.99) and 1.65 (95% CI 1.32–2.06), respectively. Albeit the significance and the effect estimate of NO2 is < 1, the random forest model demonstrates that long exposure to NO2 is a variable with a rather low importance on COVID-19 severity outcomes (Fig. 3 ). For that reason, it was discarded from the subsequent analysis. On the contrary, long-term exposure to PM10 is within the top 4 important variables determining COVID-19 severity. Regarding mortality, age, sex, cancer and PM10 are significant variables (Fig. 4 ). COVID-19 infected males are more prone to die than females, while the effect estimates of cancer and PM10 are 1.47 (95% CI 1.03–2.06) and 2.37 (95% CI 1.71–3.32), respectively. Furthermore, long-term exposure to PM10 is the second most important variable for COVID-19 mortality (Fig. 5 ). Hence, exceeding the WHO guideline value for PM10 (20 µg/m3) is a risk factor for a fatal health outcome after COVID-19 infection. Based on the regularized linear regressions built for this purpose, an increase of 1 µg/m3 in PM10 concentration causes an increase of 3.06% (95% CI 1.11% − 4.25%) of patients suffering COVID-19 as a severe disease, and in addition, an increase of 2.68% (95% CI 0.53% − 5.58%) of deaths.
Fig. 2.
Estimates for severity of COVID-19.
Fig. 3.
Importance of variables on COVID-19 severity.
Fig. 4.
Estimates for mortality of COVID-19.
Fig. 5.
Importance of variables on COVID-19 mortality.
4. Discussion
We investigated the relationship between long-term exposure to the air concentrations of NO2 and PM10 and COVID-19 severity and mortality by means of a retrospective study. Using multivariate predictive models, this retrospective study provided evidence of a link between long-term exposure to PM10 and the severity and mortality of COVID-19. However, the importance of NO2 was low.
Almost 70% of the study participants suffered mild COVID-19. However, the highest rates of mild COVID-19 occurred in localities where the average PM10 concentration was below the PM10 WHO guideline value. In contrast, the highest rates of mortality were found in localities above this PM10 reference limit. Hence, geographical differences in COVID-19 severity after infection can be linked to the already demonstrated long-term exposure to PM10 and related harmful effects on health (Renzi et al., 2019, Zhou et al., 2015). In addition to COVID-19 severity outcomes, those cities above the WHO guideline of PM10 presented higher mortality than those below such reference.
The PM10 effects estimates were 1.67 and 2.38 for severity and mortality of COVID-19. An increase of 1 µg/m3 in long-term exposure to PM10 means an increase of 3.06% of patients suffering severe COVID-19, as well as an increase of 2.68% of the number of deaths.
Our random forest model showed the importance of the long-term exposure to PM10 on the COVID-19 severity and mortality prognosis versus other clinical variables clearly stated as comorbidities, such as COPD/asthma , cancer , diabetes and obesity, among others (Cardamone and Donatiello, 2020, Kong et al., 2021, McGurnaghan et al., 2020, Mohammad et al., 2021, Oh and Song, 2021). Notwithstanding, we also found that age, sex (male) and obesity significantly increased the severity of COVID-19, which is in agreement with other studies (Elezkurtaj et al., 2021). In turn, cancer significantly increased the COVID-19 mortality due to the depressed immune system of cancer patients (Cavalcanti and Soares, 2020, Vahabi et al., 2021). Nonetheless, long-term exposure to PM10 showed the highest effect estimates, being the second most important variable determining the severity of COVID-19. Moreover, even though PM10 was in the fourth position of importance in the ranking of mortality, its value was higher than that of severity. Furthermore, the effect estimate was only slightly lower than that of the age, showing the great importance of the long-term exposure to PM10 on COVID-19 fatality. Finally, the low importance of smoking on COVID-19 severity and mortality might be related to the fact that adverse effects of environmental PM10 exposure in respiratory diseases are more severe in never-smokers (Lee et al., 2020).
To the best of our knowledge, this is the first study where the impact of long-term exposure to air pollutants (NO2 and PM10) on COVID-19 severity and mortality has been assessed by means of a retrospective study counting with clinical variables of 2112 individuals. To date, most of the assessments carried out are epidemiological studies performed with public data on environmental pollutants and COVID-19 morbidity and mortality.
The infection risk is not addressed in the present study. However, PM10 and NO2 have shown strong correlations with the risk of COVID-19 infection (Wu et al., 2021, Zhang et al., 2021, Hutter et al., 2020). In this sense, PM has been pointed out as a potential carrier of SARS-CoV-2 (Setti et al., 2020), but high concentrations of PM are necessary (Linillos-Pradillo et al., 2021). Lembo et al. (2021) analyzed public available databases from 33 European countries, concluding that high levels of pollution in Europe should be considered as a potential risk for severe COVID-19 and SARS-CoV-2 related deaths. That study found remarkable correlations for PM2.5 and nitrogen oxides with the cumulative number of COVID-19 deaths. Although Hutter et al. (2020) also demonstrated a significant association between NO2 and death from COVID-19, our results are in disagreement with the relevant role of nitrogen oxides. On the other hand, an ecological association of city-level COVID-19 case fatality rate with PM10 and PM2.5 exposure was reported by Ran et al., (2020), while Hou et al., (2021) also observed that air pollutants such as PM2.5 may assist with the prediction of COVID-19 death. Yao et al., 2020 determined that for every 10 µg/m3 increase in PM2.5 and PM10 concentrations, the COVID-19 case fatality rate increased by 0.24% and 0.26%, respectively. This increase in the number of deaths is much lower than that found for PM10 in the present study.
Our study has some limitations. Firstly, we assumed the long-term exposure to NO2 and PM10 for each individual taking into account the hospital of admission and the closest atmospheric pollution monitoring cabin. Hence, it was considered that each individual was admitted to the corresponding reference hospital. Consequently, the long-term exposure to PM10 was that of the allocated atmospheric pollution monitoring cabin. This assumption is usually valid, but some patients could have been transferred between hospitals according to the severity of the individual and the capacity of the intensive care unit. In addition, we also assumed that participants lived in the locality of the hospital where they were admitted, and therefore, they underwent the allocated long-term exposure. On the other hand, even though our cohort counts with more than 2000 individuals, as the long-term exposure depends only on the location of the hospital, many individuals would be subjected to the same exposure. Thus, it was impossible to estimate the long-term exposure to PM10 according to the severity group. Furthermore, the air contaminants here assessed were limited to those regularly monitored by the Catalan Atmospheric Pollution Monitoring and Forecasting Network. Finally, even though this study is focused on the role of environmental pollutants (NO2 and PM10) on COVID-19 severity and mortality, some investigations have found that COVID-19 incidence is associated with GDP per capita (Paez et al., 2020, Bontempi et al., 2021, López-Mendoza et al., 2021). We tested the importance of the GDP per capita in our forest model and it was found to be less important than PM10, corroborating the importance of the later on the severity and mortality of COVID-19. In addition, the effect estimates for GDP is 0.
In conclusion, the current findings highlight the urgent need to protect the population against long-term exposure to PM10, and all toxic air pollutants in general. Our results demonstrate that the current guideline concentration of PM10 fixed by the WHO in 20 µg/m3, the air quality standard established by the Directive 2008/50/EU in 40 µg/m3, and that of the US-EPA in 50 µg/m3, are not safe. It is well established that the long-term exposure to these PM10 concentrations is likely to enhance the development of cardiovascular and respiratory diseases (Rovira et al., 2019, Polichetti et al., 2009, Beelen et al., 2014, Elbarbary et al., 2021, Bodor et al., 2021, Tahery et al., 2021). In addition, subjects infected with respiratory viruses such as SARS-CoV-2 and exposed to PM10 above the present legal thresholds are more prone to develop a severe COVID-19 - or even to die - after SARS-CoV-2 infection. In the current study, individuals living in the metropolitan area of Barcelona, as well as in Manresa, Girona and Reus, are at risk of suffering a more lethal form of COVID-19 due to long-term exposure to PM10.
This is a crucial issue of public health, the WHO and worldwide air quality regulators are called to update the guideline values and air quality standards of PM10. Regulations must be revised without delay to protect the health of the population. Therefore, it is necessary to urgently reduce long-term exposure to PM10 in those locations above the reference limits in order to: i) decrease the incidence of cardiovascular and respiratory diseases; ii) reduce the severity and mortality due to respiratory viruses infection, including SARS-CoV-2; iii) reduce the healthcare costs derived from a sick population.
Finally, present findings mark a turning point to start considering the place of residence - and the related exposure to PM10 - for a proper prognosis of respiratory viral infections.
CRediT authorship contribution statement
Montse Marquès: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Visualization, Writing – original draft. Eudald Correig: Conceptualization, Formal analysis, Investigation, Methodology, Resources, Software, Writing – original draft. Daiana Ibarretxe: Data curation. Eva Anoro: Data curation. Juan Antonio Arroyo: Data curation. Carlos Jericó: Data curation. Rosa M. Borrallo: Data curation. Marcel·la Miret: Data curation. Silvia Näf: Data curation. Anna Pardo: Data curation. Verónica Perea: Data curation. Rosa Pérez-Bernalte: Data curation. Rafael Ramírez-Montesinos: Data curation. Meritxell Royuela: Data curation. Cristina Soler: Data curation. Maria Urquizu-Padilla: Data curation. Alberto Zamora: Data curation. Juan Pedro-Botet: Data curation. Lluís Masana: Investigation, Supervision, Validation, Writing – review & editing. José L. Domingo: Investigation, Supervision, Validation, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
Members of the STACOV-XULA research group who contributed to data acquisition.
Hospital del Mar (Barcelona): Elisenda Climent, Roberto Güerri, Jade Soldado. Hospital Sant Pau i Santa Tecla (Tarragona): Carmen Arto-Fernández. Hospital Universitari Sant Joan (Reus): Núria Plana, Cèlia Rodríguez-Borjabad, Natalia Andreychuk. Hospital del Vendrell: A. Lacal-Martínez, P. Barragan-Galló, G. Vives Masdeu. Hospital Verge de la Cinta (Tortosa): P. Gil-Lluís. Corporació de Salut del Maresme i la Selva: Oriol Alonso-Gisbert, Ana Inés Méndez-Martínez, Hada Iglesias-López. Hospital Santa Creu Sant Pau (Barcelona): Laia Matas. Consorci Sanitari Terrassa: Carolina Guerrero, Marta Mauri, Àngels Pedragosa. Hospital Santa Caterina (Girona): Albert Gómez, Sara García. ALTHAIA, Xarxa Assistencial Universitària de Manresa: Omar El Boutrouki, Andrea Vázquez-Escobales, Maria Cristina Antón-Alonso, Sergio Rivero-Santana. Hospital Moises Broggi (Sant Joan Despi): Maria del Señor Cortes-Fernandez. Hospital Universitari Bellvitge (Hospitalet Llobregat): Marta Fanlo. Hospital Esperit Sant (Santa Coloma): Alicia Taboada. Hospital Universitari Vall d’Hebron (Barcelvona): Núria Rial-Lorenzo, Lourdes Ruiz-Ortega. Hospital Arnau de Vilanova (Lleida): Liliana Gutierrez.
Handling Editor: Adrian Covaci
References
- Barnett-Itzhaki Z., Levi A. Effects of chronic exposure to ambient air pollutants on COVID-19 morbidity and mortality - A lesson from OECD countries. Environ Res. 2021;195:110723. doi: 10.1016/j.envres.2021.110723. PMID 33484722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beelen R, Stafoggia M, Raaschou-Nielsen O, Andersen ZJ, Xun WW, Katsouyanni K. 2014. Long-term Exposure to Air Pollution and Cardiovascular Mortality, Epidemiology 25(3):368-78, PMID: 24589872, 10.1097/EDE.0000000000000076. [DOI] [PubMed]
- Cardamone C., Donatiello I. Management of COVID-19 in comorbidities. Italian J. Med. 2020;14(4):223–227. doi: 10.4081/itjm.2020.1406. [DOI] [Google Scholar]
- Copat C., Cristaldi A., Fiore M., Grasso A., Zuccarello P., Signorelli S.S., et al. The role of air pollution (PM and NO2) in COVID-19 spread and lethality: a systematic review. Environ Res. 2020;191:110129. doi: 10.1016/j.envres.2020.110129. PMID: 32853663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bashir M.F., Ma B., Bilal K.B., Bashir M.A., Tan D., et al. Correlation between climate indicators and COVID-19 pandemic in New York USA. Sci. Total Environ.728. 2020:138835. doi: 10.1016/j.scitotenv.2020.138835. PMID 32334162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodor K., Micheu M.M., Keresztesi Á., Birsan M.V., Nita I.A., Bodor Z., et al. Effects of PM10 and weather on respiratory and cardiovascular diseases in the Ciuc Basin (Romanian Carpathians) Atmosphere. 2021;12:289. doi: 10.3390/atmos12020289. [DOI] [Google Scholar]
- Bontempi E, Coccia M, Vergalli S, Zanoletti A. 2021. Can commercial trade represent the main indicator of the COVID-19 diffusion due to human-to-human interactions? A comparative analysis between Italy, France, and Spain. Environ Res 201:111529, PMID: 34147467, 10.1016/j.envres.2021.111529. [DOI] [PMC free article] [PubMed]
- Cavalcanti I.D.L., Soares J.C.S. Impact of COVID-19 on cancer patients: A review. Asia-Pac J. Clin. Oncol. 2020;1(7) doi: 10.1111/ajco.13445. PMID 32970923. [DOI] [PubMed] [Google Scholar]
- Domingo JL, Rovira J. Effects of air pollutants on the transmission and severity of respiratory viral infections. Environ Res 187:109650, PMID: 32416357, 10.1016/j.envres.2020.109650. [DOI] [PMC free article] [PubMed]
- Ejaz H, Alsrhani A, Zafar A, Javed H, Junaid K, Abdalla AE, et al. 2020. COVID-19 and comorbidities: Deleterious impact on infected patients. J Infect Public Health. 13(12):1833-1839. PMID: 32788073, 10.1016/j.jiph.2020.07.014. [DOI] [PMC free article] [PubMed]
- Elbarbary E, Oganesyan A, Honda T, Morgan G, Guo Y, Guo Y, et al. 2021. Systemic inflammation (C-Reactive Protein) in older Chinese adults is associated with long-term exposure to ambient air pollution. Int J Environ Res Public Health, 18(6):3258, PMID: 33809857, 10.3390/ijerph18063258. [DOI] [PMC free article] [PubMed]
- Elezkurtaj S, Greuel S, Ihlow J. Michaelis EG, Bischoff P, Kunze CA, et al. 2021. Causes of death and comorbidities in hospitalized patients with COVID-19. Sci Rep 11(1):4263, PMID: 33608563, 10.1038/s41598-021-82862-5. [DOI] [PMC free article] [PubMed]
- Frontera A, Cianfanelli L, Vlachos K, Landoni G, Cremona G. 2020. SARS-CoV-2 spread in Northern Italy: what about the pollution role?. J Infect 81(2):255-259, PMID: 32447007, 10.1016/j.jinf.2020.05.031. [DOI] [PMC free article] [PubMed]
- Generalitat de Catalunya. Departament de Territori i Sostenibilitat. “Dades Meteorològiques de La XEMA.” 13 Mar. 2021, . https://analisi.transparenciacatalunya.cat/Medi-Ambient/Qualitat-de-l-aire-als-punts-de-mesurament-autom-t/tasf-thgu.
- Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. 2020. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA 323(16):1574-1581. PMID: 32250385; 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed]
- Hahad O, Frenis K, Kuntic M, Daiber A, Münzel T. 2021. Accelerated Aging and Age-Related Diseases (CVD and Neurological) Due to Air Pollution and Traffic Noise Exposure. Int J Mol Sci 22(5):2419. PMID: 33670865, 10.3390/ijms22052419. [DOI] [PMC free article] [PubMed]
- Henderson SB, Brauer M, Macnab YC, Kennedy SM. 2011. Three measures of forest fire smoke exposure and their associations with respiratory and cardiovascular health outcomes in a population-based cohort. Environ Health Perspect 119(9):1266-71, PMID: 21659039, 10.1289/ehp.1002288. [DOI] [PMC free article] [PubMed]
- Hoek G, Krishnan RM, Beelen R, Peters A, Ostro B, Brunekreef B et al. 2013. Long-term air pollution exposure and cardio- respiratory mortality: a review. Environ Health 12(1):43, PMID: 23714370, 10.1186/1476-069X-12-43. [DOI] [PMC free article] [PubMed]
- Hou CK, Qin YF, Wang G, Liu QL, Yang XY, Wang H. 2021. Impact of a long-term air pollution exposure on the case fatality rate of COVID-19 patients-A multicity study. J Med Virol 93(5):2938-2946. PMID: 33470428, 10.1002/jmv.26807. [DOI] [PMC free article] [PubMed]
- Hu J, Li C, Wang S, Li T, Zhang H. 2021. Genetic variants are identified to increase risk of COVID-19 related mortality from UK Biobank data. medRxiv [Preprint]. 2020 Nov 9:2020.11.05.20226761. PMID: 33536081, 10.1186/s40246-021-00306-7. [DOI] [PMC free article] [PubMed]
- Hutter HP, Poteser M, Moshammer H, Lemmerer K, Mayer M, Weitensfelder L, et al. 2020. Air pollution is associated with COVID-19 incidence and mortality in Vienna, Austria. Int. J. Environ. Res. Public Health 17(24):9275, PMID: 33322456, 10.3390/ijerph17249275. [DOI] [PMC free article] [PubMed]
- Khafaie M., Yajnik C., Salvi S., Ojha A. Critical review of air pollution health effects with special concern on respiratory health. J. Air Pollut. Health. 2016;1(2):123–136. [Google Scholar]
- Kong X., Qi Y., Huang J., Zhao Y., Zhan Y., Qin X., et al. Epidemiological and clinical characteristics of cancer patients with COVID-19: A systematic review and meta-analysis of global data. Cancer Lett. 2021;508:30–46. doi: 10.1016/j.canlet.2021.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Y.M., Lee J.H., Kim H.C., Ha E. Effects of PM10 on mortality in pure COPD and asthma-COPD overlap: difference in exposure duration, gender, and smoking status. Sci. Rep. 2020;10:2402. doi: 10.1038/s41598-020-59246-2. PMID: 32051443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lembo R, Landoni G, Cianfanelli L, Frontera A. 2021. Air pollutants and SARS-CoV-2 in 33 European countries. Acta Biomed 92(1):e2021166, PMID: 33682802, 10.23750/abm.v92i1.11155. [DOI] [PMC free article] [PubMed]
- Linillos-Pradillo B, Rancan L, Ramiro ED, Vara E, Artíñano B, Arias J. 2021. Determination of SARS-CoV-2 RNA in different particulate matter size fractions of outdoor air samples in Madrid during the lockdown. Environ Res 195:110863, PMID: 33609549, 10.1016/j.envres.2021.110863. [DOI] [PMC free article] [PubMed]
- López-Mendoza H, Montañés A, Moliner-Lahoz FJ. 2021. Disparities in the Evolution of the COVID-19 Pandemic between Spanish Provinces. Int J Environ Res Public Health 18:5085. PMID: 34064938, 10.3390/ijerph18105085. [DOI] [PMC free article] [PubMed]
- Maleki M, Anvari E, Hopke PK, Noorimotlagh Z, Mirzaee SA. 2021. An updated systematic review on the association between atmospheric particulate matter pollution and prevalence of SARS-CoV-2. Environ Res 195:110898, PMID: 33610583, 10.1016/j.envres.2021.110898. [DOI] [PMC free article] [PubMed]
- Marquès M, Rovira J, Nadal M, Domingo JL. 2020. Effects of air pollution on the potential transmission and mortality of COVID-19: A preliminary case-study in Tarragona Province (Catalonia, Spain). Environ Res 2020, 192:110315, PMID: 33058813, 10.1016/j.envres.2020.11031. [DOI] [PMC free article] [PubMed]
- Marquès M., Domingo J.L. Positive association between outdoor air pollution and the incidence and severity of COVID-19. A review of the recent scientific evidences. Environ. Res. 2021;203:111930. doi: 10.1016/j.envres.2021.111930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masana L., Correig E., Rodríguez-Borjabad C., Anoro E., Arroyo J.A., Jericó C., et al. Effect of statin therapy on SARS-CoV-2 infection-related. Eur. Heart J. Cardiovasc. Pharmacother. 2020 doi: 10.1093/ehjcvp/pvaa128. pvaa128, PMID 33135047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGurnaghan SJ, Weir A, Bishop J, Kennedy S, Blackbourn LAK, McAllister DA et al. Risks of and risk factors for COVID-19 disease in people with diabetes: a cohort study of the total population of Scotland. Lancet Diabetes Endocrinol 9(2)82:93, PMID: 33357491, 10.1016/S2213-8587(20)30405-8. [DOI] [PMC free article] [PubMed]
- Meo S.A., Abukhalaf A.A., Sami W., Hoang T.D. Effect of environmental pollution PM2.5, carbon monoxide, and ozone on the incidence and mortality due to SARS-CoV-2 infection in London, United Kingdom. J. King Saud Univ. – Sci. 2020;33(3):101373. doi: 10.1016/j.jksus.2021.101373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohammad S, Aziz R, Al Mahri S, Malik SS, Haji E, Khan AH et al. 2021. Obesity and COVID-19: what makes obese host so vulnerable?. Immun Ageing 18(1):1, PMID: 33390183, 10.1186/s12979-020-00212-x. [DOI] [PMC free article] [PubMed]
- Oh TK, Song IA. 2021. Impact of coronavirus disease-2019 on chronic respiratory disease in South Korea: an NHIS COVID-19 database cohort study. BMC Pulm Med 21(1):12, PMID: 33407347, 10.1186/s12890-020-01387-1. [DOI] [PMC free article] [PubMed]
- Paez A, Lopez FA, Menezes T, Cavalcanti R, Pitta MGDR. 2020. A Spatio-Temporal Analysis of the Environmental Correlates of COVID-19 Incidence in Spain. Geogr Anal. 8:10.1111/gean.12241, PMID: 32836331, doi: 10.1111/gean.12241. [DOI] [PMC free article] [PubMed]
- Paital B., Agrawal P.K. Air pollution by NO2 and PM2.5 explains COVID-19 infection severity by overexpression of angiotensin-converting enzyme 2 in respiratory cells: a review. Environ. Chem. Lett. 2020;18:1–18. doi: 10.1007/s10311-020-01091-w. PMID: 32982622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polichetti G, Cocco S, Spinali A, Trimarco V, Nunziata A. 2009. Effects of particulate matter (PM10, PM2.5 and PM1) on the cardiovascular system, Toxicology 261(1-2)1-8, PMID: 19379789, 10.1016/j.tox.2009.04.035. [DOI] [PubMed]
- Ran J., Zhao S., Han L., Qiu Y., Cao P., Yang Z., et al. Effects of particulate matter exposure on the transmissibility and case fatality rate of COVID-19: A Nationwide Ecological Study in China. J. Travel Med. 2020;27(6) doi: 10.1093/jtm/taaa133. taaa133 PMID: 32779721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renzi M., Forastiere F., Schwartz J., Davoli M., Michelozzi P., Stafoggia M. Long-term PM10 exposure and cause-specific mortality in the Latium Region (Italy): A difference-in-differences approach. Environ Health Perspect. 2019;127(6):67004. doi: 10.1289/EHP3759. PMID: 31166133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW et al. 2020. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA 323(20):2052-2059, PMID: 32320003, 10.1001/jama.2020.6775. Erratum in: JAMA 2020 323(20):2098. [DOI] [PMC free article] [PubMed]
- Rovira J., Domingo J.L., Schuhmacher M. Air quality, health impacts and burden of disease due to air pollution (PM10, PM2.5, NO2 and O3): Application of AirQ+ model to the Camp de Tarragona County (Catalonia, Spain) Sci. Total Environ. 2019;703:135538. doi: 10.1016/j.scitotenv.2019.135538. PMID 31759725. [DOI] [PubMed] [Google Scholar]
- Sciomer S, Moscucci F, Magrì D, Badagliacca R, Piccirillo G, Agostoni P. 2020. SARS-CoV-2 spread in Northern Italy: what about the pollution role? Environ. Monit. Assess. 192(6)325, PMID: 32363409, 10.1007/s10661-020-08317-y. [DOI] [PMC free article] [PubMed]
- Setti L, Passarini F, De Gennaro G, Barbieri P, Perrone MG, Borelli M, et al. 2020. SARS-CoV-2RNA found on particulate matter of Bergamo in Northern Italy: First evidence. Environ Res. 188:109754, PMID: 32526492, 10.1016/j.envres.2020.109754. [DOI] [PMC free article] [PubMed]
- Tahery N, Geravandi S, Goudarzi G, Shahriyari HA, Jalali S, Mohammadi MJ. 2021. Estimation of PM10 pollutant and its effect on total mortality (TM), hospitalizations due to cardiovascular diseases (HACD), and respiratory disease (HARD) outcome. Environ Sci Pollut Res, PMID: 33411285, 10.1007/s11356-020-12052-9. [DOI] [PubMed]
- Tian T, Zhang J, Hu L, Jiang Y, Duan C, Li Z, et al. 2021. Risk factors associated with mortality of COVID-19 in 3125 counties of the United States. Infect Dis Poverty. 10(1):3, PMID: 33397470, 0.1186/s40249-020-00786-0. [DOI] [PMC free article] [PubMed]
- Vahabi N, Salehi M, Duarte JD, Mollalo A, Michailidis G. 2021. County-level longitudinal clustering of COVID-19 mortality to incidence ratio in the United States. Sci Rep 11(1):3088, PMID: 33542313, 10.1038/s41598-021-82384-0. [DOI] [PMC free article] [PubMed]
- White IR, Royston P, Wood AM. 2011. Multiple imputation using chained equations: Issues and guidance for practice. Stat Med 2011 30(4):377-99, PMID: 21225900, 10.1002/sim.4067. [DOI] [PubMed]
- Wu Y., Zhan Q., Zhao Q. Long-term Air Pollution Exposure Impact on CVID-19 Morbidity in China. Aerosol Air Qual. Res. 2021;21(1) doi: 10.4209/aaqr.2020.07.0413. [DOI] [Google Scholar]
- World Health Organization (2020) Ambient (outdoor) air pollution [Fact sheet]. Retrieved from https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health.
- Yang D., Yang X., Deng F., Guo X. Ambient Air Pollution and Biomarkers of Health Effect. Adv. Exp. Med. Biol. 2017;1017:59–102. doi: 10.1007/978-981-10-5657-4_4. PMID 29177959. [DOI] [PubMed] [Google Scholar]
- Yao Y., Pan J., Wang W., Liu Z., Kan H., Qiu Y., et al. Association of particulate matter pollution and case fatality rate of COVID-19 in 49 Chinese cities. Sci Total Environ. 2020;741:140396. PMID: 32592974 doi: 10.1016/j.scitotenv.2020.140396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Yang H, Li S, Li WD, Wang J, Wang Y. 2021. Association analysis framework of genetic and exposure risks for COVID-19 in middle-aged and elderly adults. Mech Ageing Dev 194:111433, PMID: 33444631, 10.1016/j.mad.2021.111433. [DOI] [PMC free article] [PubMed]
- Zheng P, Chen Z, Liu Y, Song H, Wu CH, Li B et al. 2021. Association between coronavirus disease 2019 (COVID-19) and long-term exposure to air pollution: Evidence from the first epidemic wave in China. Environ Pollut 276:116682, PMID: 33631687, 10.1016/j.envpol.2021.116682. [DOI] [PMC free article] [PubMed]
- Zhou M, He G, Liu Y, Yin P, Li Y, Kan H et al. 2015. The associations between ambient air pollution and adult respiratory mortality in 32 major Chinese cities, 2006-2010. Environ Res 137:278-286, PMID: 25601729, 10.1016/j.envres.2014.12.016. [DOI] [PubMed]
- Zhu W, Cai J, Hu Y, Zhang H, Han X, Zheng H et al. 2021. Long-term exposure to fine particulate matter relates with incident myocardial infarction (MI) risks and post-MI mortality: A meta-analysis. Chemosphere 267:128903, PMID: 33213879, 10.1016/j.chemosphere.2020.128903. [DOI] [PubMed]