Abstract
An increasing body of research indicates that, whilst young adults are at the lowest risk of becoming severely physically ill as a result of COVID-19, they are at the greatest risk of adverse mental health outcomes. Using data from the Understanding Society COVID-19 survey, the current study examined the mental health of 18-25-year-olds during the pandemic. Current mental health was measured at six time points using the 12-item General Health Questionnaire (GHQ-12), a validated measure for mental distress. The analytic sample included 880 young adults (292 = males; 588 = females). The trajectory of mental health was modeled from April to November 2020, using demographic information and health behaviors (physical activity, alcohol consumption, and smoking cigarettes) as covariates. Growth curve modeling indicated that alcohol consumption, smoking, being female, having a lower income, and having a pre-existing mental health condition were risk factors for worse mental health during the pandemic. For females, their mental health was lowest in April but gradually improved until September, when it began to decline again. Males, in contrast, had a relatively stable trajectory of mental health across the pandemic. These findings can help inform targeted interventions for at risk groups to minimize the adverse impact of the pandemic on young adults’ mental health.
Keywords: Mental health, COVID-19, Trajectories, Gender, Young adults, Smoking, Alcohol consumption
1. Introduction
A growing body of evidence on COVID-19 indicates that young adults are facing the greatest adverse effects on their mental health despite being at the lowest risk of becoming seriously physically unwell (e.g., Alonzi et al., 2020; Evans et al., 2021; O'Connor et al., 2020; Smith et al., 2020). The pandemic has disrupted education and work, alongside declining economic prospects, job opportunities, and reduced social contact (Alonzi et al., 2020; Power et al., 2020; Shanahan et al., 2020; Smith et al., 2020). Due to young adults being at a critical point in their careers, social life, and education (Alonzi et al., 2020; Lee et al., 2020), these disruptions may be particularly damaging to their mental health. However, there is limited longitudinal research focusing on this vulnerable group, with most of the current research focused on the initial months of lockdown. The current study fills this gap through an examination of the trajectory of mental health and its predictors in a longitudinal sample of young adults.
Regarding possible predictors of mental health during COVID-19, studies in the UK and elsewhere have found that females and those from low-income households have the highest prevalence of mental health issues in the initial months (March to May 2020) of the pandemic (e.g., Evans et al., 2021; Pierce et al., 2020; Smith et al., 2020). Additionally, it has been postulated that the mental health of those in higher socio-economic groups may have improved during the pandemic due to increased family time, positive changes to work, and no commuting, all of which may reduce stress and increase wellbeing (Pierce et al., 2020). With respect to ethnicity, Pierce et al. (2020) found no significant differences in adult mental health among ethnic groups in April 2020 but postulated that differences between ethnic groups may become more evident as the pandemic continues. Therefore, longitudinal research is necessary to monitor and identify differences.
Research assessing associations between mental health and health behaviors including smoking cigarettes and consuming alcohol are mixed. A UK cross-sectional study by Smith et al. (2020) in March 2020 revealed that consuming low amounts or no alcohol was associated with worse mental health, as was being a smoker. Similarly, in a sample of UK university students, Evans et al. (2021) found that depressive symptoms increased and wellbeing declined at the start of the pandemic in April/May 2020, whereas alcohol consumption was lower than it was in October 2019.
Furthermore, current research suggests that physical activity is associated with better mental health (Arora and Grey, 2020; López-Bueno et al., 2020; Pieh et al., 2020; Stanton et al., 2020; Zhang et al., 2020). In a UK sample, physical activity was found to be a protective factor for mental health (Jacob et al., 2021). However, there are currently mixed findings in relation to the association between physical activity, mental health, and gender. López-Bueno et al. (2020) found a stronger association between engaging in the amount of physical activity recommended by the WHO (World Health Organization) and a better mood and lower levels of perceived anxiety in females than males. Conversely, Pieh et al. (2020) found that increased duration and intensity of physical activity was associated with a lower prevalence of depression in males but not females in an Australian sample.
Whilst these previous studies are informative, they have only examined the initial stage of the pandemic. However, there may be a spike effect in which findings represent the initial shock and emotional response, which may diminish as young adults adjust (Pierce et al., 2020). Conversely, mental health may deteriorate as the pandemic continues (Pierce et al., 2020; Power et al., 2020). This can only be assessed through longitudinal data, which can track changes in the mental health of young adults throughout the pandemic and the factors that are associated with improving or worsening symptoms.
Drawing on the Understanding Society COVID-19 survey, this study used growth curve modeling to assess the trajectory of mental health among young adults from April to November of 2020. We focus on young adults aged 18–25 years-old in accordance with Arnett's theory of emerging adulthood (Arnett, 2000). During this period, individuals enter independence and begin to explore possible life directions in relation to love, work, socialization, and world views (Arnett, 2000; Hochberg & Konner, 2020). Consequently, the disruption caused by the pandemic may impact them disproportionately and have a detrimental impact on their mental health (Gruber et al., 2020). Given this, we expect that their mental health trajectory corresponds to the lockdown restrictions, becoming worse in months with higher restrictions. To assess gender differences, we examined whether the level and rate of change in their mental health trajectory differed between males and females. Given the current research highlighting females had poorer mental health at the start of the pandemic (Evans et al., 2021; Pierce et al., 2020; Smith et al., 2020), we expect females to have worse mental health than males. Demographic information, baseline measures of physical health and mental health, and health behaviors (physical activity, smoking cigarettes, and drinking alcohol) were further included in the model to provide additional information on the predictors of change in the mental health of young adults during the spring to winter months of the pandemic. As alcohol consumption and smoking have been associated with poorer mental health (Evans et al., 2021; Smith et al., 2020), we predict that these factors will be associated with worse mental health. Physical activity has been thought to be a protective factor for mental health, therefore, we predict that physical activity will be associated with better mental health.
2. Method
2.1. Data source
The participants were taken from a variation of the Understanding Society UK Household Longitudinal Study (UKHLS) - a nationally representative, high quality, longitudinal panel survey of UK households - called the Understanding Society COVID-19 survey. Using this data allows the analysis of a large sample that is representative of the population. Ethical approval for the survey was granted by the University of Essex Ethics Committee.
The Understanding Society COVID survey was gathered monthly from April 2020 to June 2020, and every two months from September 2020 onwards. The first four questionnaires were fielded to all the Understanding Society samples who had completed at least one of the last two waves of data. From Wave 5 onwards, only those who participated in at least one of the first four waves of the study were sent the survey.
The present study included data obtained in Waves 1–6 (April, May, June, July, September, and November) from young adults (aged 18–25 in Wave 1). Based on the requirements of growth curve modeling, the final analytic sample included only those young adults who provided responses for the covariates gathered in Wave 1 and responded to the mental health questionnaire at least twice. The final analytic sample included 880 participants: 14% had two waves, 12% had three waves, 13% had four waves, 35% had five waves, and 26% had six waves of data. Of the 880 participants, 69.4% participants were White, 13.0% Asian, 4.3% Mixed, 2.2% Black, and 0.1% Other; 66.8% participants were female.
ANOVA was conducted to assess whether those included in the analytic sample (n = 880) significantly differed from those not included (n = 587). Those who were not included were younger F(1, 1465) = 53.32, p < .001, consumed less alcohol F(1, 1465) = 122.46, p < .001, smoked fewer cigarettes F(1, 1465) = 12.08, p = .001, were more likely to be an ethnic minority F(1, 1465) = 18.38, p < .001 and had higher mental health scores in November (M = 2.31, SD = .61) F(1, 527) = 4.96, p = .03 than those who were included in the analytic sample.
2.3. Measures
Table 1 presents the wave, minimum and maximum, mean, and standard deviation of the measures in this study. This study examined predictors from the first questionnaire (April) only. Current Mental Health was examined for April, May, June, July, September, and November.
Table 1.
Characteristics of the Measures.
| Measure | Wave/file | Min. | Max. | Mean | SD |
|---|---|---|---|---|---|
| Age | 1 | 18.00 | 25.00 | 21.80 | 2.28 |
| Employed | 1 | .00 | 1.00 | .67 | .47 |
| Physical Health Condition | 1 | .00 | 3.00 | .25 | .49 |
| Mental Health Condition | 1 | .00 | 1.00 | .06 | .24 |
| Household Income | 1 | 1.00 | 15.00 | 7.09 | 4.48 |
| Alcohol Consumption | 1 | .00 | 5.00 | 1.66 | 1.48 |
| Cigarette Use | 1 | .00 | 5.00 | .19 | .71 |
| Physical Activity | 1 | .00 | 7.00 | 3.49 | 2.00 |
| GHQ Wave 1 | 1 | 1.00 | 4.00 | 2.21 | .56 |
| GHQ Wave 2 | 2 | 1.00 | 4.00 | 2.20 | .56 |
| GHQ Wave 3 | 3 | 1.00 | 4.00 | 2.15 | .53 |
| GHQ Wave4 | 4 | 1.00 | 4.00 | 2.05 | .49 |
| GHQ Wave 5 | 5 | 1.00 | 4.00 | 2.08 | .52 |
| GHQ Wave 6 | 6 | 1.00 | 4.00 | 2.19 | .53 |
Note. Baseline refers to questions asked in the first questionnaire.
Gender was a dichotomous variable, coded as ‘0’ for female; ‘1’ for male.
Ethnicity was coded into five groups: White, Asian, Mixed, Black, and Other.
PhysicalHealth Condition was a count of 20 items which asked if the participant had any long-standing physical health conditions including asthma, cancer, diabetes, epilepsy, stroke, congestive heart disease, or another condition.
Mental Health Condition was a dichotomous variable indicating whether the participant had a pre-existing emotional, nervous, or psychiatric problem, coded ‘0’ for no; ‘1’ for yes.
Household Income was a continuous variable of income per year coded as ‘1’ for £0-£5,000; ‘2’ for £5,001-£10,000; ‘3’ for £10,001-£15,000; ‘4’ for £15,001-£20,000; ‘5’ for £20,001-£25,000; ‘6’ for £25,001-£30,000; ‘7’ for £30,001-£35,000; ‘8’ for £35,001-£40,000; ‘9’ for £40,001-£45,000; ‘10’ for £45,001-£50,000; ‘11’ for £50,001-£55,000; ‘12’ for £55,001-£60,000, ‘13’ for £60,001-£65,000; ‘14’ for £65,001-£70,000; ‘15’ for £70,001 and greater.
Alcohol Consumption was assessed with the question: “Thinking about the last 4 weeks, how often did you have a drink containing alcohol?” where ‘0’ = never or not a drinker; ‘1’ = once; ‘2’ = 2–4 times in total; ‘3’ = 2-3 times per week; ‘4’ = 4–6 times per week; ‘5’ = daily.
Cigarette Use was assessed with the question: “Approximately how many cigarettes a day do you usually smoke, including those you roll yourself?” the responses were coded: ‘0’ for none or not a smoker; ‘1’ for 1-5; ‘2’ for 6-10; ‘3’ for 11-15; ‘4’ for 16-20; ‘5’ for more than 20.
Physical Activity was assessed with the question: “During the last 7 days, on how many days did you do vigorous physical activities like heavy lifting, digging, aerobics, or fast bicycling?” They were asked to only include occasions where the activities lasted at least 10 min at a time.
Current Mental Health was measured in each questionnaire using the 12-item General Health Questionnaire (GHQ) (Goldberg, 1988), which is a validated measure for mental distress in the last two weeks and is often used in non-clinical populations (Li and Wang, 2020; Pierce et al., 2020). The 12 questions measured the participant's depressive symptoms, anxiety symptoms, and other wellbeing symptoms using a four-point scale (1 = less than usual; 2 = no more than usual; 3 = rather more than usual; 4 = much more than usual) Li and Wang (2020). The gold standard for interpreting the GHQ-12 is a 2/3 cut off (Aalto et al., 2012). The 12 questions had high internal consistency ( = .90) at each wave; therefore, the participant's average across the questions was used for each month as the measure of current mental health.
2.4. Data analysis
All analyses were completed using SPSS 26. Growth curve modeling (GCM) was used to examine the trajectory of mental health (GHQ) from April to November of 2020, using Waves 1-6 of the Understanding Society COVID-19 survey. GCM is appropriate in this instance as this statistical method does not require equal spacing between time points and accounts for missing data which allows participants to be included even if they have not participated in all six questionnaires. Maximum likelihood estimation was used to account for the missing data. To examine the trajectory over time, a time variable corresponding to month was created. This was coded in accordance with the number of months the questionnaire was completed after April (when Wave 1 took place): April = ‘0’; May = ‘1’; June = ‘2’; July = ‘3’; September = ‘5’; November = ‘7’. A level 1 model was used to assess current mental health across time, assessing both the linear and quadratic functions. Then, level 2 models were built on the level 1 model by incorporating covariates and interactions between gender and linear time and between gender and quadratic time.
3. Results
As shown in Table 2 , the significant intercept indicated that mental health scores were highest at the start of lockdown in April (indicating poorer mental health). There was a significant negative linear slope, showing an improvement in mental health during the first three months of the pandemic. There was also a significant positive quadratic slope, showing a decline in mental health from September onwards.
Table 2.
Growth Curve Model Predicting Mental Health Trajectory.
| Measure | Coef. | SE |
|---|---|---|
| For Intercept | ||
| Intercept | 2.33*** | .03 |
| Mental Health Condition | .35*** | .06 |
| Gender | -.23*** | .04 |
| Household Income | -.01*** | .00 |
| Alcohol Consumption | .02* | .01 |
| Cigarette Use | .05* | .02 |
| For Linear Slope | ||
| Intercept | -.09*** | .01 |
| Gender × Linear Time | .07*** | .02 |
| For Quadratic Slope | ||
| Intercept | .01*** | .00 |
| Gender × Quadratic Time | -.01** | .00 |
| Residual Variance | Variance | |
| For Intercept | .14*** | |
| For linear slope | .00** |
***p < .001; **p < .01; *p < .05.
At the intercept (April), having a pre-existing mental health condition, living in a lower-income household, and being female were associated with poorer mental health. Smoking cigarettes and drinking alcohol were both associated with worse mental health in April. These factors were not significant at the linear and/or quadratic slopes. The participant's self-reported age, ethnicity, physical health condition, and physical activity were not significant at intercept and/or slopes and thus were removed from the final model for the sake of parsimony.
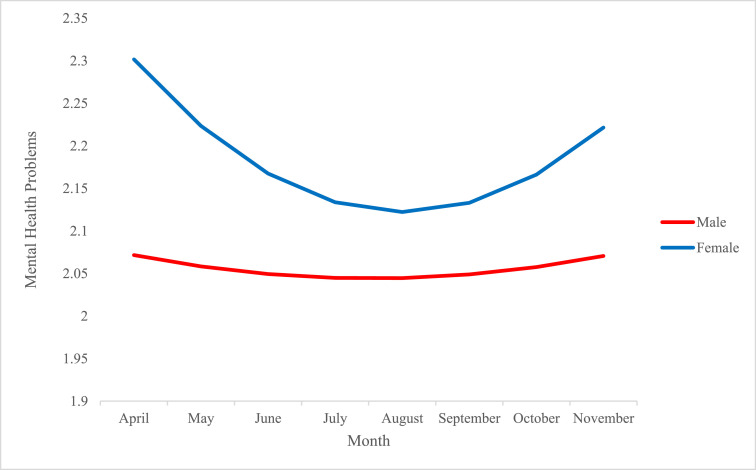
To understand the differences in the trajectory of mental health between males and females, two interactions were included: gender by linear time, and gender by quadratic time. The gender by linear time interaction and gender by quadratic time interaction were both significant (see Table 2). As shown in Figure 1 , males had a relatively stable trajectory of mental health over the pandemic and their GHQ scores were significantly lower than females. Females experienced a peak (highest GHQ score) in April which began to decline, indicating that their mental health improved, until September when their scores began to increase again, indicating worsening mental health.
Fig. 1.
Growth curves showing the mental health of male and female young adults from April to September 2020.
4. Discussion
The current study aimed to investigate the trajectory of mental health for young adults (aged 18–25) during the COVID-19 pandemic from April to November 2020. GCM was used to assess the trajectory of mental health over the time in question, using health behaviors and demographic information as predictors. The results indicate that, as predicted in the first hypothesis, mental health scores were highest in April but decreased over time, showing an improvement in mental health. However, the scores began to increase around September. The trajectory of mental health also differed between males and females, with females having significantly worse mental health and showing more variation across the pandemic than males. Cigarette use and alcohol consumption were associated with higher scores in April.
The trajectory of mental health is in line with lockdown restrictions in the UK, gradually easing over the Spring and Summer months. However, from September onwards, restrictions began to tighten. The ‘rule of six’ was put into place on the 14th of September followed by a three-tiered system on the 14th of October, which further restricted the lives of individuals in the UK. On the 5th of November 2020, the second lockdown was introduced. The events could be used to explain the trajectory of females’ mental health. When restrictions were easing, the mental health of females improved and, when they began tightening again, their mental health worsened. Our results also seem to suggest that the mental health of the males in this sample was not as affected by lockdown restrictions, as there was limited change in males’ mental health during this time.
The findings provide evidence that young adults in UK who regularly drank alcohol at the start of the pandemic were more at risk of having poorer mental health, in contrast with other UK studies (Evans et al., 2021; Smith, 2020). Our findings seem to contradict the Smith et al. (2020) study of UK adults in March 2020, which examined cross-sectional associations and did not control for baseline mental health. Our study, however, supports their findings in relation to the positive association between cigarette use and poorer mental health (Smith et al., 2020). Together, our findings suggest that substance abuse, involving alcohol or cigarettes, was related to worse mental health for young adults at the start of the pandemic but did not appear to influence the rate of change in mental health from the spring to winter months of 2020.
Consistent with existing research, the current study found that having a pre-existing mental health condition was associated with adverse mental health at the start of the pandemic (Power et al., 2020; O'Connor et al., 2020; Pierce et al., 2020). Similarly, this study found further support for an association with income (O'Connor et al., 2020; Daly et al., 2020; Evans et al., 2021; Pieh et al., 2020; Pierce et al., 2020; Smith et al., 2020) as having a lower household income was associated with worse mental health in April. These findings further emphasize the importance of targeting interventions toward those with lower income and with pre-existing mental health conditions.
Like several other studies (Pierce et al., 2020), this research did not find differences in mental health between ethnicities. This could be due to there not being significant differences, or because the sample was mainly White participants. Additionally, it has been postulated that ethnic differences may become more evident over time (Pierce et al., 2020). Therefore, further longitudinal research with more diverse samples is necessary.
5. Limitations
There were several important limitations in this study. Firstly, this research is limited as, due to the nature of the data, the findings are correlational. Therefore, we cannot conclusively state that any specific factors cause negative effects on mental health. A further limitation is the content of the questionnaire. For example, as health behaviors were not measured at each wave, we were unable to assess fluctuations over time or how such changes may impact mental health. For example, it is possible that a reduction in physical activity across the pandemic relates to worse mental health. Furthermore, as information such as occupation was not collected, we could not analyze the impact of other potentially important factors. Another limitation is this study did not compare drinking habits during the pandemic with pre-pandemic levels, so we cannot infer that alcohol is being used as a coping mechanism or that alcohol consumption has changed as a result of the pandemic.
A major limitation of this study is that the GHQ-12 is the only measure of mental health. Whilst the GHQ-12 is a recommended questionnaire with very good psychometric value (Gnambs & Staufenbiel 2018), it is used primarily for screening. Therefore, there is a need for future studies to use more advanced tools to measure different dimensions of mental health.
Moreover, whilst the Understanding Society COVID-19 survey collects data from a representative sample, our sample was heavily female-dominated and included a majority of White participants. Additionally, as is often the case with longitudinal studies, not all participants responded to each questionnaire. Those not included in the final sample differed according to ethnicity, alcohol consumption, and cigarette use in April and mental health in November. Therefore, it is possible that, had they been included, some results may have differed. This highlights the need for further research using larger, more diverse samples.
5.1. Conclusions and Implications
Despite the limitations, this study provides useful insight into the mental health of young adults during the pandemic. The findings highlight that females, those with a pre-existing mental health condition, and those with a low household income are particularly vulnerable to adverse mental health during the pandemic. This research further suggests that drinking alcohol and smoking cigarettes are associated with an increased risk of poorer mental health during COVID-19. This suggests that targeted interventions for young adults which focus specifically on females, those with a lower income, and with pre-existing mental health conditions are needed to mitigate these effects and provide support for those most at risk. These findings can further be used to inform policies and interventions aimed at reducing alcohol consumption and cigarette use in young people, especially for more vulnerable groups.
Overall, this research highlights the devastating effects the pandemic is having on the mental health of young adults, particularly females, and provides insight into their trajectory of mental health between April and November of 2020. There is a need to implement targeted interventions for young adults which focus on the identified risk factors to support mental health, particularly when the toughest restrictions are in place. Understanding how the mental health of young adults is being affected by the COVID-19 pandemic and the potential risk factors is essential to mitigate its adverse effects.
CRediT authorship contribution statement
Isabel Stroud: Conceptualization, Formal analysis, Writing – original draft. Leslie Morrison Gutman: Methodology, Writing – review & editing, Supervision.
Declarations of Competing Interest
None.
References
- Aalto A., Elovainio M., Kivimäki M., Uutela A., Pirkola S. The Beck depression inventory and general health questionnaire as measures of depression in the general population: a validation study using the composite international diagnostic interview as the gold standard. Psychiatry Res. 2012;197(1-2):163–171. doi: 10.1016/j.psychres.2011.09.008. [DOI] [PubMed] [Google Scholar]
- Alonzi S., La Torre A., Silverstein M. The psychological impact of preexisting mental and physical health conditions during the COVID-19 pandemic. Psychol. Trauma. 2020;12(S1):S236–S238. doi: 10.1037/tra0000840. [DOI] [PubMed] [Google Scholar]
- Arnett J. Emerging adulthood: a theory of development from the late teens through the twenties. Am. Psychol. 2000;55(5):469–480. doi: 10.1037/0003-066x.55.5.469. [DOI] [PubMed] [Google Scholar]
- Arora T., Grey I. Health behaviour changes during COVID-19 and the potential consequences: a mini-review. J. Health Psychol. 2020;25(9):1155–1163. doi: 10.1177/1359105320937053. [DOI] [PubMed] [Google Scholar]
- Daly M., Sutin A., Robinson E. Longitudinal changes in mental health and the COVID-19 pandemic: evidence from the UK Household Longitudinal Study. Psychol. Med. 2020:1–10. doi: 10.1017/s0033291720004432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans S., Alkan E., Bhangoo J., Tenenbaum H., Ng-Knight T. Effects of the COVID-19 lockdown on mental health, wellbeing, sleep, and alcohol use in a UK student sample. Psychiatry Res. 2021;298 doi: 10.1016/j.psychres.2021.113819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gnambs T., Staufenbiel T. The structure of the general health questionnaire (GHQ-12): two meta-analytic factor analyses. Health Psychol. Rev. 2018;12(2):179–194. doi: 10.1080/17437199.2018.1426484. [DOI] [PubMed] [Google Scholar]
- Goldberg D.P. NFER-Nelson; Windsor: 1988. User's guide to the General Health Questionnaire. [Google Scholar]
- Gruber J., Prinstein M., Clark L., Rottenberg J., Abramowitz J., Albano A., et al. Mental health and clinical psychological science in the time of COVID-19: Challenges, opportunities, and a call to action. Am. Psychol. 2020 doi: 10.1037/amp0000707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hochberg Z., Konner M. Emerging adulthood, a pre-adult life-history stage. Front. Endocrinol. 2020;10 doi: 10.3389/fendo.2019.00918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob L., Smith L., Armstrong N., Yakkundi A., Barnett Y., Butler L., et al. Alcohol use and mental health during COVID-19 lockdown: a cross-sectional study in a sample of UK adults. Drug Alcohol Depend. 2021;219 doi: 10.1016/j.drugalcdep.2020.108488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee C., Cadigan J., Rhew I. Increases in loneliness among young adults during the COVID-19 pandemic and association with increases in mental health problems. J. Adolesc. Health. 2020;67(5):714–717. doi: 10.1016/j.jadohealth.2020.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L., Wang S. Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López-Bueno R., Calatayud J., Ezzatvar Y., Casajús J., Smith L., Andersen L., López-Sánchez G. Association between current physical activity and current perceived anxiety and mood in the initial phase of COVID-19 confinement. Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.00729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connor R., Wetherall K., Cleare S., McClelland H., Melson A., Niedzwiedz C., et al. Mental health and well-being during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br. J. Psychiatry. 2020:1–8. doi: 10.1192/bjp.2020.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieh C., Budimir S., Probst T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J. Psychosom. Res. 2020;136 doi: 10.1016/j.jpsychores.2020.110186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M., Hope H., Ford T., Hatch S., Hotopf M., John A., et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. The Lancet Psychiatry. 2020;7(10):883–892. doi: 10.1016/s2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Power E., Hughes S., Cotter D., Cannon M. Youth mental health in the time of COVID-19. Irish J. Psychol. Med. 2020;37(4):301–305. doi: 10.1017/ipm.2020.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanahan L., Steinhoff A., Bechtiger L., Murray A., Nivette A., Hepp U., et al. Emotional distress in young adults during the COVID-19 pandemic: evidence of risk and resilience from a longitudinal cohort study. Psychol. Med. 2020:1–10. doi: 10.1017/s003329172000241x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith L., Jacob L., Yakkundi A., McDermott D., Armstrong N., Barnett Y., et al. Correlates of symptoms of anxiety and depression and mental wellbeing associated with COVID-19: a cross-sectional study of UK-based respondents. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanton R., To Q., Khalesi S., Williams S., Alley S., Thwaite T., et al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int. J. Environ. Res. Public Health. 2020;17(11):4065. doi: 10.3390/ijerph17114065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Zhang H., Ma X., Di Q. Mental health problems during the COVID-19 pandemics and the mitigation effects of exercise: a longitudinal study of college students in China. Int. J. Environ. Res. Public Health. 2020;17(10):3722. doi: 10.3390/ijerph17103722. [DOI] [PMC free article] [PubMed] [Google Scholar]