Abstract
Objective
Post-inflammatory hyperpigmentation (PIH) is a reactive hypermelanosis of various skin types, which occurs as a sequela of cutaneous inflammation or injury. Despite generally a self-limited and temporary condition, PIH is still a frustrating problem that can have significant psychosocial effects on patients, especially those with darker skin types. Laser therapy is one of the effective treatments for PIH, and various wavelength lasers and light devices have been utilized in PIH therapy. Nonetheless, data on the long-term efficacy of the 755-nm alexandrite picosecond laser are limited.
Methods
This study analyzed two cases of PIH treated with a combination of a 755-nm alexandrite picosecond laser and a diffractive lens array or zoom handpiece. Efficacy of the treatment was determined by the images of skin lesions under a fixed light source before and after each treatment, which were independently reviewed by two plastic-surgery specialists blinded to the clinical data. Improvement was classified as complete (>75%), significant (50–75%), mild (25–50%), and inefficient (<25% or no obvious change). Skin imaging analysis was carried out using the VISIA system (Canfield, USA), and dermoscopy was performed at the same time.
Results
After two to three courses of treatment, all cases showed significant or complete improvement, and no recurrence was observed during the three years of follow-up.
Conclusion
A 755-nm alexandrite picosecond laser in combination with a diffractive lens array or zoom handpiece had significant and long-term efficacy for the treatment of PIH caused by trauma. However, attention should be paid to the problem of transient deepening of pigmentation during treatment.
Keywords: 755 nm, picosecond laser, long-term effect, post-inflammatory hyperpigmentation
Introduction
Post-inflammatory hyperpigmentation (PIH) is a reactive hypermelanosis of various skin types occurring as a sequela of cutaneous inflammation or injury. Although PIH is self-limited and temporary, it is still a frustrating problem that can have significant psychosocial effects on patients, especially those with darker skin types. A variety of physical factors, including trauma and oral medication for acne, can lead to PIH. There are several effective treatments for patients with PIH, including topical decolorant, chemical peels, and laser therapy. The use of a 755-nm alexandrite picosecond laser has been found to be an effective method for wrinkle removal and the treatment of various pigment diseases, but reports evaluating its efficacy in PIH caused by trauma are lacking. The present study reported two cases of PIH caused by trauma and treated by a 755-nm alexandrite picosecond laser in combination with a diffractive lens array or zoom handpiece, with a three-year follow-up.
Methods
The first case was a 38-year-old man with Fitzpatrick skin type III. One year prior to the treatment, he suffered from facial abrasion after falling off a bike. He was not treated for trauma debridement, which resulted in pigmentation. Physical examination showed one rectangular brown patch on the right temporal area, measuring about 2×3 cm, and one brown patch above the right eyebrow arch, measuring about 1×1 cm, with smooth surfaces and without scar hyperplasia. The patient was physically fit and had no previous medical history. The patient was arranged to received four rounds of consecutive treatments with a 755-nm alexandrite picosecond laser (PicoSureTM, Cynosure, USA) combined with a FOCUSTM diffractive lens array with intervals of one to two months. The therapeutic parameters were a pulse width of 750 ps, a frequency of 10 Hz, a spot diameter of 8 mm, and an energy density of 0.4 J/cm2, with 500 ± 50 pulses each time. Skin redness was defined as the treatment endpoint.
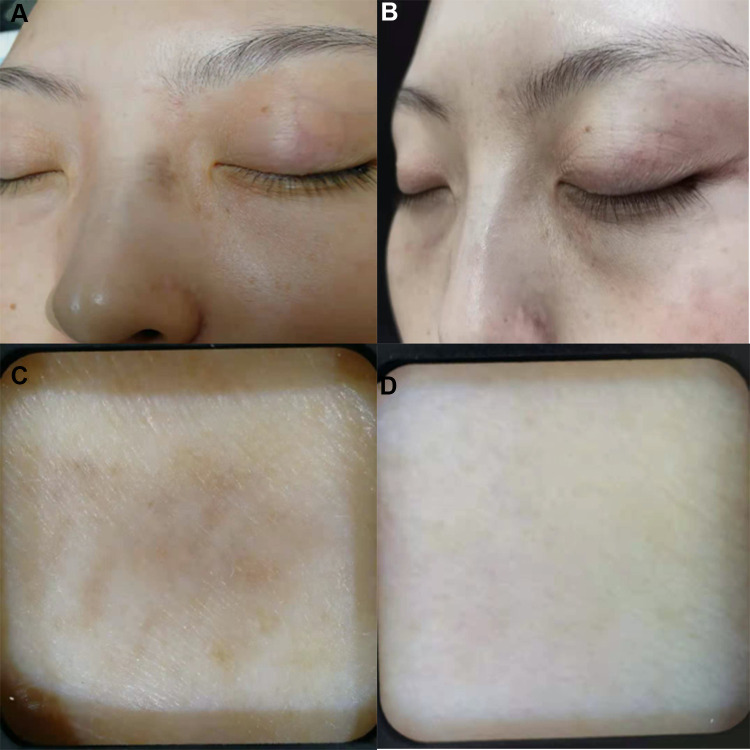
The second case was a 36-year-old woman with Fitzpatrick skin type III admitted to the hospital due to a brown macular rash on the left side of her nasal dorsum for two years. Two years prior to the treatment, the left side of her nasal dorsum was injured, leaving brown pigmentation without treatment. The patient consciously affected the appearance by the lesions and required treatment. Dermoscopy showed uneven brown lesions with unclear boundaries. The patient received treatment with a 755-nm alexandrite picosecond laser and a 2–6 mm zoom (continuously variable) handpiece. The therapeutic parameters included a pulse width of 750 ps, a frequency of 1 Hz, a spot diameter of 3.2 mm, and an energy density of 2.49 J/cm2, with 350 ± 50 pulse each time.
Results
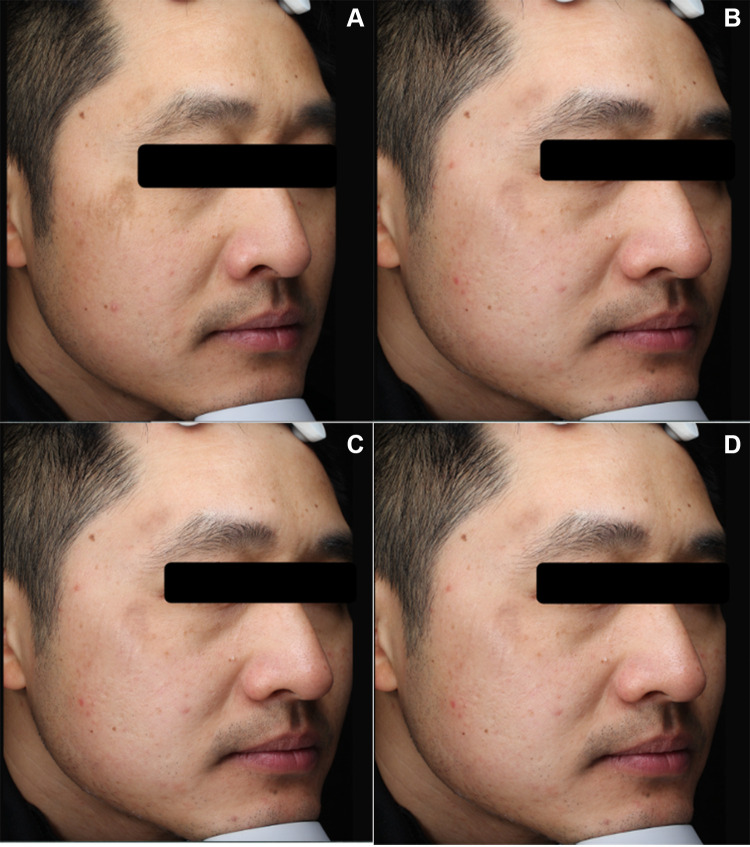
The curative effects of the first case were determined by two plastic-surgery specialists blinded to the treatment; these specialists evaluated the degree of improvement based on images captured before and after treatment. An improvement of 0–25% was defined as inefficient, 25–50% as mild, 50–75% as significant, and 76–100% as complete. Significant improvement was achieved after the second treatment, but the patient showed a deepening of local skin lesions in a follow-up visit prior to the third treatment, and the VISIA examination showed an increase in the counts of brown and ultraviolet patches (Table 1). Therefore, the treatment was suspended for six months before the third treatment was performed again. At the three-year follow-up after three treatments, the lesions were significant improved (50–75%) and the patient was satisfied (Figure 1).
Table 1.
Case 1. Data of Brown Patches and Ultraviolet Patches from VISIA
| Time | Counts of Brown Patches | Score of Brown Patches | Counts of Ultraviolet Patches | Score of Ultraviolet Patches |
|---|---|---|---|---|
| Before treatment | 183 | 58.276 | 330 | 18.523 |
| After the second treatment | 202 | 48.654 | 353 | 18.882 |
| Before the third treatment | 192 | 54.429 | 349 | 20.856 |
| After the third treatment | 169 | 50.794 | 362 | 17.662 |
Figure 1.
Pictures of the first case. (A) Before treatment, (B) after the second treatment, (C) the color of the original lesions deepened before the third treatment, and (D) 3-year follow-up after the third treatment.
As for the second case, the scab fell off after seven days of treatment, but some skin lesions remained. After six months, the second picosecond laser treatment was performed with the same parameters as before. Blinded evaluations by two plastic-surgery specialists agreed that the lesions were clear, with 100% improvement and complete disappearance of pigmentation under dermoscopy compared with the lesions before treatment (Figure 2). After three years of follow-up, the efficacy remained stable.
Figure 2.
Pictures of the second case. (A) Before treatment, (B) after the second treatment, (C) dermatoscopy showed uneven brown lesions with unclear boundaries, and (D) the original skin lesion became normal after three years treatment.
Discussion
As a common yet troubling sequelae of inflammatory skin disease, PIH is the pathological process that the skin uses to defend against various injuries. The causes of PIH include both internal and external factors, such as physical factors, chemical factors, and biological factors. PIH is more likely to occur in people with Fitzpatrick skin type III or IV, with a wide range of involvement and high incidence. Although it is self-limited to a certain extent, it has a negative impact on quality of life.1 Current treatments mainly include topical medications, oral tranexamic acid, chemical peels, laser therapy, and other methods.2,3 Previous reports have described improvement in PIH after treatment with intense pulsed light, a 1064-nm Q-switched laser, a 694-nm ruby laser, and a non-ablative 1927-nm fractional laser.4,5 However, as laser therapy itself may aggravate PIH, caution is required in its clinical application.6
Picosecond laser treatment differs from nanosecond laser treatment in that it has an extremely short pulse width and high peak power density. In addition to producing photothermal effects, it can also produce strong photomechanical effects. Compared with nanosecond lasers, the ultra-short pulse duration and small thermal energy generated during PIH treatment of picosecond laser can effectively reduce the photothermal effect and avoid thermal damage to the surrounding tissue; thus, its safety and effectiveness are higher.
Currently, there are three picosecond laser devices, with 532-nm, 755-nm, and 1064-nm wavelengths, that have been widely used in the fields of pigmentation disease,7 acne scars,8 wrinkle removal,9 and other areas, all of which have achieved good results. The 755-nm alexandrite picosecond laser also has FocusTM diffractive lens array technology, which can re-concentrate the energy emitted by the laser to form a non-peelable lattice beam, forming an energy transport mode with a low-energy background area surrounding the high-energy area and resulting in a laser-induced optical breakdown effect on the skin.10 This effect can indirectly stimulate the regeneration of dermal collagen and achieve skin rejuvenation through the effects of pressure, cytokines, and signaling pathways.11
Many case studies have reported the favorable outcome of drug-induced PIH treatment using a 755-nm alexandrite picosecond laser. Sasaki et al12 found that a 755-nm alexandrite picosecond laser can effectively treat pigmentation caused by minocycline, and the efficacy can be maintained for one year. Rivers et al13 reported the case of a 64-year-old white man with PIH that was induced by oral minocycline for acne. After three treatments with a 755-nm alexandrite picosecond laser and a 2.5-year follow-up, pigmentation completely disappeared, which was verified by dermoscopy. Barrett et al14 reported the case of an 81-year-old white woman with PIH caused by oral minocycline for rosacea. Five treatments with a 1064-nm nanosecond laser and 532-nm Q-switched laser produced poor results, but four subsequent treatments with a 755-nm alexandrite picosecond laser produced complete disappearance of the pigmentation. Kok et al15 reported a case in which a 755-nm alexandrite picosecond laser was used to effectively treat PIH caused by imatinib mesylate.
Both the cases in the present study acquired PIH caused by trauma, which differs from PIH induced by oral drugs. After treatment with a 755-nm alexandrite picosecond laser combined with a diffractive lens array or zoom handpiece, the first case achieved significant improvement, and the skin lesions of the second case disappeared completely, which were both verified by VISIA and dermoscopy examination. The clinical effect was maintained after a three-year follow-up. However, it is worth noting that, during the treatment process, the first case experienced transient deepening of the skin lesions after the second treatment, which gradually improved after suspension of treatment for six months. The reason for pigmentation may be associated with the men’s lack of strict sunscreen and the disorder of basal pigment cell activity caused by picosecond laser treatment. It is suggested that picosecond laser treatment should be discontinued in the case of the transient aggravation of PIH and be repeated when the value of brown patches is stable on VISIA examination; the treatment interval should also be extended appropriately. However, the treatment is too frequent to irritate melanocytes and aggravate the skin lesions.
Regarding the frequency of treatment, Lee et al16 reported the case of a 20-year-old woman with PIH in the middle part of the lip, which was treated with a 755-nm alexandrite picosecond laser with a spot diameter of 2 mm and an energy density of 7.25 J/cm2 seven times before significant improvement was achieved. In the present study, the second case was treated with low energy and only required two treatments before a good effect was achieved, and no recurrence was observed after three years of follow-up. Considering it may be related to the fact that high energy leads to better photothermal decomposition of melanin particles, prospective studies are needed to further prove it.
Conclusion
The present study found that a 755-nm alexandrite picosecond laser combined with a diffractive lens array or zoom handpiece is an effective and safe treatment option for PIH in the Asian population and the efficacy can last for a long time. However, further investigation is still required.
Ethics Approval and Consent to Participate
This study was conducted with approval from the Ethics Committee of Beijing Hospital National Center of Gerontology Institute of Geriatric Medicine, Chinese Academy of Medical Sciences. This study was conducted in accordance with the declaration of Helsinki. Written informed consent was obtained to have the case details and any accompanying images published.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Maymone MBC, Neamah HH, Wirya SA. The impact of skin hyperpigmentation and hyperchromia on quality of life: a cross-sectional study. J Am Acad Dermatol. 2017;77(4):775–778. doi: 10.1016/j.jaad.2017.05.009 [DOI] [PubMed] [Google Scholar]
- 2.Lindgren AL, Austin AH, Welsh KM. The use of tranexamic acid to prevent and treat post-inflammatory hyperpigmentation. J Drugs Dermatol. 2021;20(3):344–345. doi: 10.36849/JDD.5622 [DOI] [PubMed] [Google Scholar]
- 3.Shenoy A, Madan R. Post-inflammatory hyperpigmentation: a review of treatment strategies. J Drugs Dermatol. 2020;19(8):763–768. doi: 10.36849/JDD.2020.4887 [DOI] [PubMed] [Google Scholar]
- 4.Bae YS, Rettig S, Weiss E, Bernstein L, Geronemus R. Treatment of post‐inflammatory hyperpigmentation in patients with darker skin types using a low energy 1927 nm non‐ablative fractional laser: a retrospective photographic review analysis. Lasers Surg Med. 2020;52(1):7–12. doi: 10.1002/lsm.23173 [DOI] [PubMed] [Google Scholar]
- 5.Park JH, Kim JI, Kim WS. Treatment of persistent facial postinflammatory hyperpigmentation with novel pulse-in-pulse mode intense pulsed light. Dermatol Surg. 2016;42(2):218–224. doi: 10.1097/DSS.0000000000000627 [DOI] [PubMed] [Google Scholar]
- 6.Agbai O, Hamzavi I, Jagdeo J. Laser treatments for postinflammatory hyperpigmentation: a systematic review. JAMA Dermatol. 2017;153(2):199–206. doi: 10.1001/jamadermatol.2016.4399 [DOI] [PubMed] [Google Scholar]
- 7.Hu S, Yang CS, Chang SL, et al. Efficacy and safety of the picosecond 755-nm alexandrite laser for treatment of dermal pigmentation in Asians-a retrospective study. Lasers Med Sci. 2020;35(6):1377–1383. doi: 10.1007/s10103-020-02959-7 [DOI] [PubMed] [Google Scholar]
- 8.Huang CH, Chern E, Peng JH, et al. Noninvasive atrophic acne scar treatment in Asians with a 755-nm picosecond laser using a diffractive optic lens-a retrospective photographic review. Dermatol Surg. 2019;45(2):195–202. doi: 10.1097/DSS.0000000000001669 [DOI] [PubMed] [Google Scholar]
- 9.Wat H, Shek SYN, Yeung CK, et al. Efficacy and safety of picosecond 755-nm alexandrite laser with diffractive lens array for non-ablative rejuvenation in Chinese skin. Lasers Surg Med. 2019;51(1):8–13. doi: 10.1002/lsm.23014 [DOI] [PubMed] [Google Scholar]
- 10.Tanghetti EA. The histology of skin treated with a picosecond alexandrite laser and a fractional lens array. Lasers Surg Med. 2016;48(7):646–652. doi: 10.1002/lsm.22540 [DOI] [PubMed] [Google Scholar]
- 11.McDaniel D. Gene expression analysis in cultured human skin fibroblasts following exposure to a picosecond pulsed alexandrite laser and specially designed focus optic. Lasers Surg Med. 2015;47(S26):22. [Google Scholar]
- 12.Sasaki K, Ohshiro T, Ohshiro T, et al. Type 2 Minocycline-induced hyperpigmentation successfully treated with the novel 755 nm picosecond alexandrite laser-A case report. Laser Ther. 2017;26(2):137–144. doi: 10.5978/islsm.17-CR-03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rivers JK, Zarbafian M, Vestvik B, et al. Minocycline-induced hyperpigmentation: rapid resolution after 755nm alexandrite picosecond laser treatment. J Cosmet Laser Ther. 2020;22(2):96–99. doi: 10.1080/14764172.2020.1740275 [DOI] [PubMed] [Google Scholar]
- 14.Barrett T, Zwaan SD. Picosecond alexandrite laser is superior to Q-switched Nd: YAGlaser in treatment of minocycline-induced hyperpigmentation: a case study and review of the literature. J Cosmet Laser Ther. 2018;20(7–8):387–390. doi: 10.1080/14764172.2017.1418514 [DOI] [PubMed] [Google Scholar]
- 15.Kok WL, Chua SH. Picosecond 755-nm alexandrite lasers are an effective treatment for imatinib-induced hyperpigmentation. Dermatol Surg. 2019;45(4):616–618. doi: 10.1097/DSS.0000000000001868 [DOI] [PubMed] [Google Scholar]
- 16.Lee YJ, Shin HJ, Noh TK, et al. Treatment of melasma and post-inflammatory hyperpigmentation by a picosecond 755-nm alexandrite laser in Asian patients. Ann Dermatol. 2017;29(6):779–781. doi: 10.5021/ad.2017.29.6.779 [DOI] [PMC free article] [PubMed] [Google Scholar]