Abstract
We investigate the effect of social capital on health outcomes during the Covid-19 pandemic in independent analyses for Austria, Germany, Great Britain, Italy, the Netherlands, Sweden and Switzerland. Exploiting detailed geographical variation within countries, we show that a one-standard-deviation increase in social capital leads to between 14% and 34% fewer Covid-19 cases per capita accumulated from mid-March until end of June 2020, as well as between 6% and 35% fewer excess deaths per capita. Our results highlight the positive health returns of strengthening social capital.
Keywords: Covid-19, Social capital, Collective action, Health costs, Europe
1. Introduction
Human behavior is widely seen as a key margin to contain the Covid-19 pandemic (Van Bavel et al., 2020). Policymakers and health experts around the world appeal to social responsibility, asking people to limit social contacts, follow strict hygiene and distancing recommendations, and get vaccinated.1 In economic terms, politicians urge their citizens to consider the social costs of their individual actions. Leveraging social capital in this way has a central role in official Covid-19 strategies. Yet there is little systematic evidence on the contribution social capital makes to containing Covid-19 and protecting population health. To the best of our knowledge, this study is the first to systematically analyze the dynamic relationship between social capital and health outcomes, as measured by Covid-19 cases and excess mortality.2 On the basis of separate analyses for seven European countries – Austria, Germany, Great Britain, Italy, the Netherlands, Sweden and Switzerland – we show consistently that social capital has a causal and positive effect on pandemic-related health outcomes.3 We contribute to the literature by presenting robust evidence at the fine-grained geographical level of micro-areas within countries: our analysis is at the NUTS-3 or even municipal level for some countries, as explained below. This enables us to control for confounding shocks, say regional policies implemented at the state level, by including the respective fixed effects.
We define the willingness to act collectively and pursue socially valuable activities – like following hygiene and distancing recommendations – as social capital (Putnam, 1993, Putnam, 2000). In this definition, sometimes also referred to as civic capital (Guiso, Sapienza, Zingales, 2011, Lichter et al., 2021), we narrow down the broader concept of social capital to its positive facet of helping a group to overcome free rider problems, which fits best to the Covid-19 crisis. In this, we primarily relate to what is called the “bridging” dimension of social capital (Putnam, 2000, Schmitt, van der Eijk, 2007) that stresses across-group solidarity. We follow a well-established literature and apply various common measures of social capital. The underlying principle for the selection of our measures is that they should be official, recent and comprehensive. First, we use electoral turnout in the 2019 European election. Turnout as a proxy for social capital derives directly from the seminal contributions by Putnam, 1993, Putnam, 2000 and has widely been used (see, e.g. Barrios et al., 2021, Bolsen et al., 2014, Guiso, Sapienza, Zingales, 2004). Turnout has three major advantages in the context of our study. First, it is comparable because it refers to the same election in six of the seven countries under study.4 Second, turnout exhibits sufficient regional variation within countries. Third, turnout is a precise measure even at very disaggregated geographical levels. It is based on the universe of eligible voters and thus less prone to measurement and small sample problems than survey-based measures (Bauernschuster et al., 2014). As a second measure, we use blood and organ donations, which are available at sufficiently fine geographical levels and have little measurement error. Again, this is a standard proxy in the literature (Guiso, Sapienza, Zingales, 2004, Putnam, 2000). Third, we use other common measures like association density (Giuliano, Wacziarg, 2020, Satyanath et al., 2017) or historical literacy rates (Tabellini, 2010) whenever available.
We choose the number of Covid-19 cases as our main outcome variable because it is a comprehensive measure of the extent of the pandemic which is available on a daily basis at fine geographical levels across many countries. To address potential issues of measurement error and endogeneity related to the number of reported cases, such as (non-random) differences in testing, we use excess mortality as an alternative outcome wherever available at fine geographical levels. Excess mortality is defined as the number of all deaths in a given time period relative to the average number for the same period in 2015–2019. In addition, we can test whether there were significant changes in micro-area-level excess deaths related to social capital (but unrelated to the new virus) before the outbreak of the pandemic.
As countries differ in many macroeconomic and Covid-19-specific aspects, it is challenging to identify the systematic effect of economic or cultural factors from cross-country comparisons (Goodman-Bacon and Marcus, 2020). For this reason, we implement a within-country-across-countries research design. We investigate the dynamic relationship between social capital and the spread of Covid-19 in independent analyses for seven European countries, implementing the identical empirical strategy in each country. We regress log cumulative cases or excess mortality on a measure of pre-determined social capital interacted with day fixed effects. This allows us to test whether the evolution of the pandemic has differed systematically depending on the level of social capital.5 The specification boils down to a two-way fixed effects model with micro-area fixed effects and region-specific time fixed effects capturing regional outbreak patterns and policy responses. In a robustness check, we further account for potentially different outbreak patterns over time by including weeks-since-outbreak-by-day fixed effects.
From a theoretical perspective, social capital, the spread of Covid-19 and containment policies interact in various ways. First, high-social-capital areas are known to be more vibrant and connected, both economically and socially (see, e.g., Knack and Keefer, 1997, Tabellini, 2010). Hence, we expect the virus to spread more quickly in those areas in the beginning of the pandemic, when information about the disease and its severity is still incomplete. Second, as soon as the importance of behavioral containment norms becomes more salient, we expect the relationship to change. Complying with containment norms yields a classical collective action problem (Ostrom, 1991). It is costly for the individual, while the single individuals’ contribution to the collective goal is negligible. Social capital is assumed to overcome exactly such problems by increasing the willingness to contribute to the common good (Coleman, 1990, Ostrom, 1999, Putnam, 1993, Putnam, 2000). Hence, we expect that informal rules of containment are more likely to be (voluntarily) adopted in high-social-capital areas, leading to a relative decrease in infections. Third, there are interactions with the strictness of containment policies. During lockdowns, rules are formalized and violations are easier to detect and sanction, making non-compliance more costly. Consequently, we expect containment to depend less on social capital during stricter policy regimes.
We derive the following main findings. First, high-social-capital areas accumulated between 14% and 34% fewer Covid-19 cases between mid-March and late June 2020. Likewise, high-social-capital areas recorded between 6% and 35% fewer excess deaths in Great Britain, the Netherlands, Italy, and Sweden. According to our estimates, a one-standard-deviation increase in social capital could have prevented between 1632 deaths in Sweden and 14,303 deaths in Great Britain over the considered time period. Second, we find qualitatively similar patterns across all independently analyzed countries, which we regard as strong evidence for the robustness of our results. Third, we show a consistent dynamic pattern: the number of Covid-19 cases is initially higher in high-social-capital areas. As information on the virus spreads, high-social-capital areas start to show a slower increase in Covid-19 cases in all seven countries. The role of social capital diminishes when national lockdowns are enforced. Last, our results are robust to (i) using alternative measures of social capital, (ii) adding finer fixed effects, (iii) controlling for obvious potential confounders such as income, population density, age structure, education levels or hospital density, (iv) the influence of unobserved confounders as measured by the test of Oster (2019).
To the best of our knowledge, this is the first and most comprehensive paper to empirically study the direct relationship between social capital and health outcomes during the Covid-19 pandemic. A related paper by Borgonovi et al. (2020) provides evidence that U.S. counties with higher social capital experienced lower case fatality rates and took less time until an area reached 10 (or 15) cases.
There is a related strand of the literature studying the relationship between social capital and individual mobility, as measured by cellphone or Google mobility data. Reducing mobility is one type of socially responsible behavior known to reduce the number of infections. Several studies show that citizens in counties with high social capital reduce mobility more than those in low-social-capital U.S. counties (Bai, Jin, Wan, 2020, Borgonovi, Andrieu, Brodeur, Grigoryeva, Kattan, 2021, Ding, Levine, Lin, Xie, 2020) and/or European regions (Bargain, Aminjonov, 2020, Barrios et al., 2021, Durante et al., 2021).
These findings nicely illustrate an important mechanism driving our results. The studies show that mobility behavior, one frequently-discussed determinant of the spread of the virus, varies with social capital. By studying health outcomes, we are able to directly assess the net effect of all potential behavioral responses, including mobility. Looking at the direct net effect on cases or deaths is key to understanding the role of social capital in slowing down the pandemic. In contrast, it is very challenging to infer this net health effect by studying only one specific behavior, as it is unlikely that the different behavioral channels are perfectly positively correlated. In fact, they might even be substitutes: a socially responsible person who has to make a business trip will be more likely to wear a mask and wash her hands frequently. An alternative approach to quantify the importance of certain behaviors on health outcomes would be the use of structural models. However, one would need to model all relevant mechanisms and their interactions and find relevant data moments to meaningfully calibrate or estimate such a model, which is demanding.
Our findings demonstrate that socially responsible behavior is particularly important in the absence of containment policies or when soft containment policies like hygiene or stay-at-home recommendations are in place. Our dynamic estimates show that the role of social capital is reduced as soon as strict European-style lockdowns are implemented. This is in line with macro-level evidence that countries with democratically accountable governments introduced less stringent lockdowns, but were more effective in reducing geographic mobility at the same level of policy stringency (Chen et al., 2021). From this perspective, our study is also related to a literature analyzing the effects of different Covid-19 containment policies (see, e.g., Engle et al., 2020, Friedson et al., 2021, Glogowsky, Hansen, Schchtele, 2020, Painter, Qiu, 2021).
More generally, our findings contribute to the literature on the importance of social capital for society. It is well-established that higher social capital has positive economic, social and political effects (see, e.g., Glaeser, Sacerdote, Scheinkman, 1996, Goldin and Katz, 1999, Guiso, Sapienza, Zingales, 2004, Knack and Keefer, 1997, Nannicini, Stella, Tabellini, Troiano, 2013, Tabellini, 2010).
Finally, our paper complements the large literature on social capital and health. In terms of theoretical mechanisms, previous studies have established a positive link between social capital and health at the individual level – either through a reduction in stress (Folland, 2008) or via positive peer effects on health-related preferences (Costa-Font and Mladovsky, 2008). In a recent meta analysis, Xue et al. (2020) summarize the empirical literature studying the effect of social capital on health outcomes and conclude that social capital has only small positive effects. However, the previous literature has mostly focused on non-communicable diseases like cancer, heart disease or diabetes. We suggest a new channel based on collective action for the case of a highly contagious virus. In such a setting, we argue that the spread of the virus is determined by the local level of social capital and show empirically that higher levels of social capital have large mitigating effects on the spread of the disease. Our pandemic-specific estimates are substantially higher than previous empirical results on the effect of social capital in the case of non-contagious diseases. This supports the hypothesis that the positive health benefits from social capital are larger in response to contagious diseases, when behavioral adaptations matter most.
In the light of future similar health crises, our findings have important implications for policymakers. For instance, targeted communication and health education campaigns may be particularly fruitful in areas with lower social capital. Moreover, given findings from the medical literature indicating a positive association between social capital and the willingness to get vaccinated (Chuang, Huang, Tseng, Yen, Yang, 2015, Jung et al., 2013, Rönnerstrand, 2014), this proxy can help to assess the expected effectiveness of vaccination campaigns once vaccines become widely available, such that supply constraints are no longer binding and demand-side factors gain importance.
The remainder of the paper is structured as follows. Section 2 summarizes our data and provides first descriptive evidence. In Section 3, we set-up our econometric model and describe our identification strategy. Section 4 presents our key empirical results together with an extensive sensitivity analysis. Section 5 concludes.
2. Data, institutions and descriptive evidence
In the following, we briefly describe the variables used in the empirical analysis. More information and detailed data sources are documented in Appendix Table A1.
2.1. Variables and sources
We assemble data on health outcomes and social capital from seven European countries – Austria, Germany, Great Britain, Italy, the Netherlands, Sweden and Switzerland – for which the number of total Covid-19 infections is available at a sufficiently high frequency and fine geographical level for the first wave of the pandemic. We select official, recent and comprehensive statistics on both health outcomes and social capital measures.
Outcomes.
Our main outcome variable is the log cumulative number of cases per 100,000 inhabitants. This measure is officially reported for fine geographical units and at a high frequency in all countries under study since the onset of the pandemic. Furthermore, cases are a comprehensive measure of the extent of the spread of the virus: every positive case can lead to further infections, increase the (health) costs for society, block hospital capacities and lead to further health complications.
For all countries, we aim at obtaining the daily number of Covid-19 cases since the early phase of the outbreak at the lowest available geographical level. For the Netherlands, Austria, Switzerland and Sweden, we were able to obtain data at the municipal level. In the other three countries, the geographical level is the NUTS-3 region.6
Hence, our empirical analyses are at the NUTS-3 level or below. Independent of the country-specific name, we call the geographical level at which we run our analyses “micro-area” throughout the paper.7 We summarize the different levels of geography in Appendix Table A3. The respective country samples start when more than 90% of all NUTS-3 areas have registered at least one official case. Such a restriction is necessary from an econometric perspective, as we can only assess the dynamics of the pandemic and their relation to social capital when a large enough share of areas within a region has been hit by the virus.8 We later validate that our estimates are not sensitive to this particular threshold (see Appendix Figure C4). Appendix Figure A1 presents the evolution of cumulative Covid-19 cases per 100,000 inhabitants at the national level across countries.
A potential caveat of using cases as an outcome is that countries have measured and reported cases in different ways, for instance because they had different testing policies. Our within-country design takes care of this issue, as long as testing and measurement do not vary systematically with social capital within countries at the micro-area level. Potential differences in testing at the level of the NUTS-1-region are captured by our fixed effects (see Section 3.2).
Moreover, we use the number of excess deaths as our second health measure. Excess deaths do not suffer from potentially endogenous testing. However, high-frequency information on this measure is only available for Great Britain, the Netherlands, Italy and Sweden at sufficiently low geographical levels.9 We obtained data at the municipal level for Italy, the Netherlands and Sweden, and on the lower tier local authority level for Great Britain (see Appendix Table A3). Excess mortality measures the number of deaths in a period minus the average number of deaths in the same period between 2015 and 2019.10 The evolution of daily excess mortality per 100,000 inhabitants at the national level until June 2020 is visualized in Appendix Figure A2.
Social capital.
We hypothesize that social capital can slow down the spread of the virus, as individuals with higher social capital behave more socially responsible. In the context of this study, our concept of social capital refers mainly to “bridging social capital” (Putnam, 2000, Schmitt, van der Eijk, 2007), termed also “linking” social capital (Szreter and Woolcock, 2004) or civic capital (Guiso et al., 2011) in the more recent literature.11
We proxy social capital by standard measures put forward in the literature which mainly capture the bridging dimension of social capital. In our main specification, we operationalize social capital by voter turnout in the 2019 European Parliament election. Political participation is a frequently-used and well-established measure of social capital, or civicness (Bauernschuster et al., 2014, Guiso, Sapienza, Zingales, 2004, Putnam, 1993, Putnam, 2000). An extensive literature documents that political participation strongly correlates with pro-social preferences and the willingness to contribute to public goods (see, e.g., Bolsen et al., 2014, Dawes, Loewen, Fowler, 2011, Fowler, 2006, Fowler and Kam, 2007, Jankowski, 2007) and it has been shown to be a particularly suitable proxy for social capital. As Guiso et al. (2011) put it, “[s]ince there is no direct economic payoff to voting, this measure captures the extent to which people in a community are willing to pay a personal cost to enhance the common good”. A crucial advantage of turnout as a measure of social capital is that it is valid even at very disaggregated geographical levels, where other common measures, which are often based on surveys, would suffer from low representativeness.
We use turnout in European elections as our main outcome because it enables us to use data from the same election in all but one country.12 A large and long-standing literature in political science postulates that turnout in national and European elections is driven by similar motives (see, e.g., Schmitt and Mannheimer, 1991, Schmitt, van der Eijk, 2007, Steinbrecher, Rattinger, 2012). Moreover, a more recent strand of social capital studies argues that European election turnout is a particularly good proxy to capture civic duty as decisions at the European level are perceived to be more remote and have less of an effect on people’s everyday life. Hence, political responsibility and the enhancement of the common good is a relatively more important factor to explain turnout (see, e.g. Bracco et al., 2015). Consistently, Blais and Galais (2016) document that the feeling of civic duty to vote (civic capital) is a particularly strong predictor of turnout in European elections.
As alternative measures of social capital, we use blood donations and registered organ donors per capita, which are also widely used in the literature (Guiso, Sapienza, Zingales, 2004, Putnam, 1993). Due to data availability, we cannot apply the same measure for all countries. We use blood or organ donations for Great Britain, Italy and the Netherlands. Moreover, we use other common measures of social capital, such as the number of all registered associations per capita in Germany (Buonanno, Montolio, Vanin, 2009, Giuliano, Wacziarg, 2020, Satyanath et al., 2017) and historical literacy rates in Italy (Tabellini, 2010). Overall, our results are not driven by the choice of the social capital measure, as shown in Section 4.2.13
Controls. We test the sensitivity of our results to potential confounders in all countries by controlling for the share of white-collar workers, the share of the population older than 65 years, the share of educated individuals, the number of hospitals per capita, log GDP per capita, and the population density (see Appendix Tables A1 and A2 for details and descriptive statistics). Importantly, our specification allows for the influence of these variables to change over the course of the pandemic.
2.2. Policy responses and timing of effects
The timing of the Covid-19 outbreak and the respective policy responses differs across countries. Moreover, the adopted policy measures vary in strictness. While Italy enforced a strict and long lockdown during the first wave, Sweden did not adopt any kind of lockdown. Eventually, six of the seven countries under study implemented a national lockdown during the first wave, which was stricter than comparable U.S. “stay-at-home” orders. We highlight the most important events in each country in Appendix Table A4.
Any change in behavior or policy will affect the number of Covid-19 cases with a time lag. First, there is the incubation time – the time from the infection until the appearance of first symptoms. Second, there is the confirmation time – the time between the first symptoms and the medical confirmation of the case. Naturally, both periods differ across individuals, countries and over time. For incubation time, we follow the WHO and assume a duration of 5 days (Lauer et al., 2020). There is much less evidence on confirmation time. We assume that the confirmation time is 7 days, using the reported median duration from a study by the official German health agency RKI (an der Heide and Hamouda, 2020). In total, we conclude that any behavioral change will likely affect Covid-19 cases after around 12 days. This conclusion clearly entails a lot of uncertainty. For this reason, we do not use the “incubation plus confirmation” period of 12 days as a rigorous measure in our analyses, but rather as a plausible visual guideline in the graphical representations of our results.
2.3. Descriptive evidence
First, we investigate the descriptive pattern of the spread of Covid-19 and its relationship with social capital across countries. We dichotomize social capital into high-social-capital micro-areas (above-regional-median turnout) and low-social-capital micro-areas (below-regional-median turnout) for each country. We define the ratio of the number of log cases per capita in high- relative to low-social-capital micro-areas within each region and calculate the population-weighted average of this ratio across regions to obtain the national ratio.
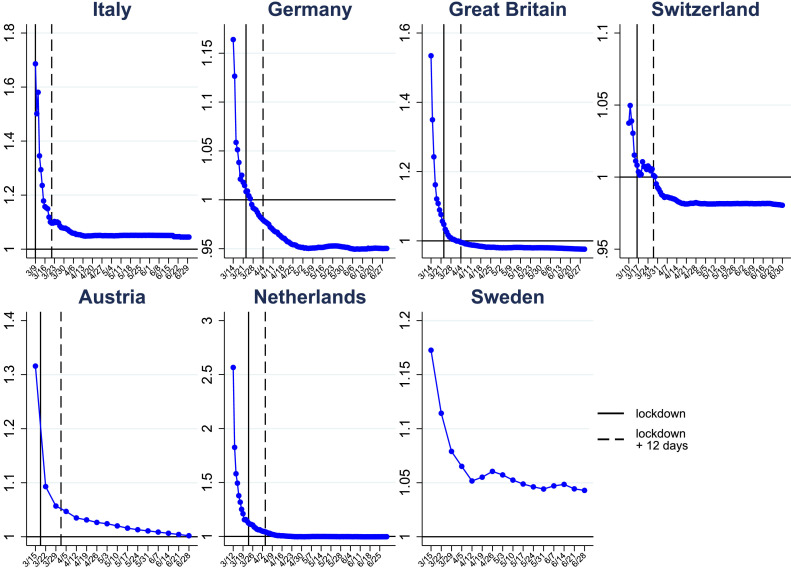
Figure 1 plots the log cumulative Covid-19 cases per capita in high-social-capital relative to low-social-capital micro-areas over time. Across all countries, we see that the virus is initially more prevalent in high-social-capital micro-areas. The initially high level is to be expected. People in areas with a high level of social capital have been shown to have closer social and economic connections (see, e.g., Knack and Keefer, 1997, Tabellini, 2010). This should exacerbate the spread of the virus initially when information on the severity of the virus and appropriate behavior is incomplete.
Fig. 1.
Cumulative Covid-19 cases in high- relative to low-social-capital micro-areas. This figure shows the ratio of log cumulative Covid-19 cases per capita in high- vs. low-social-capital micro-areas. The sample is divided at the median of turnout at the NUTS-1 region level. Micro-areas with a value above the median are defined as high-social-capital micro-areas and those below as low-social-capital micro-areas. The blue lines plot the population-weighted average of the regional log ratios over time. The solid black line marks the date of the national lockdown, the dashed black line the date of the national lockdown plus an incubation period of 12 days. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Starting from this high initial level, we then see a sharp decline in the ratio. Over time, the ratio drops until high-social-capital micro-areas have less than or almost equally many cases per inhabitant as low-social-capital micro-areas. Importantly, the decline starts before national lockdown policies could have been effective. This is a first indication that high- and low-social-capital micro-areas differ systematically in their socially responsible behavior.
3. Empirical model and identification
3.1. Baseline regression model for covid-19 cases
While Figure 1 presents simple correlations over time, we use the following more rigorous empirical model to systematically study the evolution of the relationship between social capital and the spread of the virus in each country. Our main outcome is the log cumulative number of cases per 100,000 inhabitants in micro-area (within NUTS-1 region ) on day , . As stated in Goodman-Bacon and Marcus (2020), the logarithmic model is suitable to capture the exponential growth of the virus and additionally helps to difference out measurement error in the outcome variable, which might be relevant when looking at Covid-19 cases. In order to identify the impact of social capital, we regress log cumulative Covid-19 cases on a pre-determined measure of social capital, , in a two-way fixed effects model. We estimate the following equation, separately for each country:
| (1) |
Our baseline model includes both area fixed effects , which absorb time-invariant heterogeneity, and region-by-date fixed effects , where the region dummy refers to the NUTS-1 region (see Section 3.2 for a more detailed discussion on the important role of these fixed effects).14 We cluster the standard errors at the micro-area level in all specifications.
We proxy for social capital with micro-area-specific turnout in the European Parliament election of 2019, which we normalize by its country-specific standard deviation.15 We interact social capital with date fixed effects to capture the dynamics of the effect of social capital on Covid-19 cases. Accordingly, a one-standard-deviation increase in social capital affects the number of cumulative cases per 100,000 inhabitants measured at date by approximately percent. Hence, the coefficients compare the evolution of micro-areas with a higher to those with a lower turnout over time, and relate the differences in log cases to the level of social capital. Loosely speaking, the empirical model (1) investigates the slope of the country-specific patterns in Figure 1. We normalize the coefficient to zero in all countries, such that all other coefficients measure the effect of social capital relative to this reference day. We set the last day of the sample, , to June 30, when the first wave of the pandemic had ended in all countries.16
3.2. Identification
In the context of our study, treatment status is defined by pre-determined social capital. Our identifying assumption is that no other factors correlated with social capital systematically affect growth rates of Covid-19 cases. While this assumption is untestable, we make various efforts to show that it is likely to hold.
First, our baseline model includes region-by-date fixed effects. These fixed effects flexibly control for any policy response at the regional level, such as periods of state-specific lockdowns, school closures, or test strategies, which were implemented in many countries at the NUTS-1 level. Hence, our estimates compare the evolution of micro-areas within a NUTS-1-region, accounting for any confounding shock at this regional level. The variation in most other European studies on the role of social capital is at the NUTS-1 region level, so it is difficult to disentangle policy from social capital effects.
Another concern is that area-specific outbreak dates vary and that areas may be on different points of their respective infection curves on a given day. Without further adjustments, our model in equation (1) would not be able to identify the causal effect of social capital if (i) area-specific outbreak dates were correlated with social capital and (ii) cases evolved according to a common epidemiological path. We address this challenge as follows. First, we document only a weak correlation of -0.09 between social capital and the start date within regions across countries. Second, despite the weak correlation, we propose a straightforward econometric fix to flexibly account for potentially remaining biases: we augment equation (1) by weeks-since-outbreak fixed effects. These fixed effects synchronize the outbreak dates of the micro-areas by accounting for the average pattern of an outbreak over time. We even go one step further and interact the weeks-since-outbreak fixed effects with date fixed effects (). This allows for changing outbreak patterns over time, for instance due to new information about the virus.17
In order to validate that our reduced-form model is able to cope with the challenges of using Covid-19 cases as a dependent variable, we set up a simple SIR model in Appendix B. First, we show that our estimates would indeed be biased if the outbreak date was correlated with social capital and we did not account for time-since-outbreak effects. However, as Appendix Figure B3 shows, the inclusion of time-since-outbreak fixed effects can correct for that bias. Empirically, it turns out that the inclusion of weeks-since-outbreak-times-day fixed effects hardly affects our estimates. This is due to the weak correlation of social capital and area-specific outbreak dates across micro-areas.
Despite our large set of fixed effects, which account for regional policies and area-specific outbreak patterns, we assess whether omitted variables below the NUTS-1 level might drive our results by adding the most obvious potential confounders to our baseline model. We do this symmetrically in all countries. More precisely, we add (i) education (more skilled people understand more quickly what is at stake); (ii) age structure (older people are more endangered by the virus); (iii) GDP per capita (higher-income groups can afford to reduce their labor supply more); (iv) occupation type (white-collar workers can work from home more easily); (v) population density (facilitates the spread of the disease); and (vi) hospital density (better medical infrastructure helps to fight the virus). We use a pre-outbreak measure of the respective variables and interact each covariate with day fixed effects. This allows the impact of the given variable to depend on the phase of the pandemic, just as the effect of social capital.
Eventually, the model requiring the least restrictive assumptions is given by the following specification
| (2) |
Comparing the point estimates of the baseline model in equation (1) with the extended model in equation (2) gives an indication of whether the identifying assumption is likely to hold. If the point estimates are relatively stable, this indicates that obvious unobserved confounders at higher regional levels (absorbed by the fixed effects) and observed confounders at the micro-area level are not driving our estimates. Last, we assess the likelihood that our estimates might be driven by unobserved confounders at the micro-area level by applying the test suggested by Oster (2019). The results suggest that our estimates are unlikely to be overturned by such unobserved confounders (see Section 4.2 for a more detailed discussion).
There are three important issues that arise when using Covid-19 cases as the main outcome. First, we can only assess the dynamics of the pandemic and their relation to social capital when a large enough share of areas has been hit with the virus. There is a clear trade-off between – on the one hand – starting the sample earlier and capturing the early pandemic dynamics related to social capital and – on the other hand – obtaining precise estimates of these early dynamics that are informed by a meaningful number of micro-areas. In our baseline specification, our sample starts on the day when 90% of all NUTS-3 regions have registered at least one Covid-19 case. In a robustness check we show that our point estimates vary slightly but remain consistently negative with other thresholds (see Appendix Figure C4). As expected, we lose precision when choosing an earlier sample start.
Second, one may be concerned that an initially higher level of cases in high-social-capital micro-areas might mechanically lead to a slower spread of the pandemic in these areas in the subsequent periods (cf. Figure 1). In Appendix B, we show that initial level differences between high- and low-social-capital areas at the sample start, i.e. high-social-capital areas having higher infection rates in the early phase of the pandemic, rather lead to a conservative estimate of the effect of social capital. The SIR model shows that a higher relative level of Covid-19 cases in high-social-capital areas is associated with a weaker effect of social capital on the spread of the virus. The intuition is that a higher number of infected individuals makes every contact riskier.
Third, we study the early dynamics of a pandemic caused by a new virus, so there is no pre-outbreak period. However, one testable implication of our identification assumption is that high- and low-social-capital micro-areas do not already diverge in terms of health outcomes (unrelated to Covid-19) before the outbreak of the pandemic. To assess whether areas with high social capital were on different health trends before, we use excess mortality as an alternative outcome (see Section 3.3). Moreover, we extend our analysis to the second wave. During the summer of 2020, we observe low but positive numbers of Covid-19 cases in all micro-areas across countries and can inspect the dynamics leading up to the second wave.
3.3. Regression model for excess mortality
If higher social capital slows down the spread of Covid-19 cases, we would also expect to see an effect on mortality. As described in Section 2, our preferred measure of mortality is the log cumulative number of excess deaths per 100,000 inhabitants, (Aron and Muellbauer, 2020; Ciminelli and Garcia-Mandic, 2020). Excess mortality is calculated by comparing the number of deaths in micro-area on date in 2020 to the number of deaths in the same micro-area and on the same date in previous years. Using excess deaths as a measure of mortality is preferable to official Covid-19 death counts, as the latter measure is likely to underestimate the true increase in mortality (Ciminelli and Garcia-Mandic, 2020).
Moreover, the number of excess deaths does not depend on testing capacities, which might theoretically vary with social capital. Finally, data on excess deaths are available at very fine geographic levels for the Netherlands, Great Britain, Italy and Sweden, allowing us to control flexibly for potential confounders. More specifically, for Italy, the Netherlands and Sweden we have data at the municipality level and include NUTS-3-by-time fixed effects.18 While excess mortality is a natural additional health outcome to study, it is also interesting for econometric reasons, since it enables us to assess whether there are different health trends between high- and low-social capital areas leading up to the outbreak of the pandemic (cf. Section 3.2).
Using an analogous notation as in equations (1) and (2), the corresponding regression model is given by:
| (3) |
4. Empirical findings
4.1. Main results
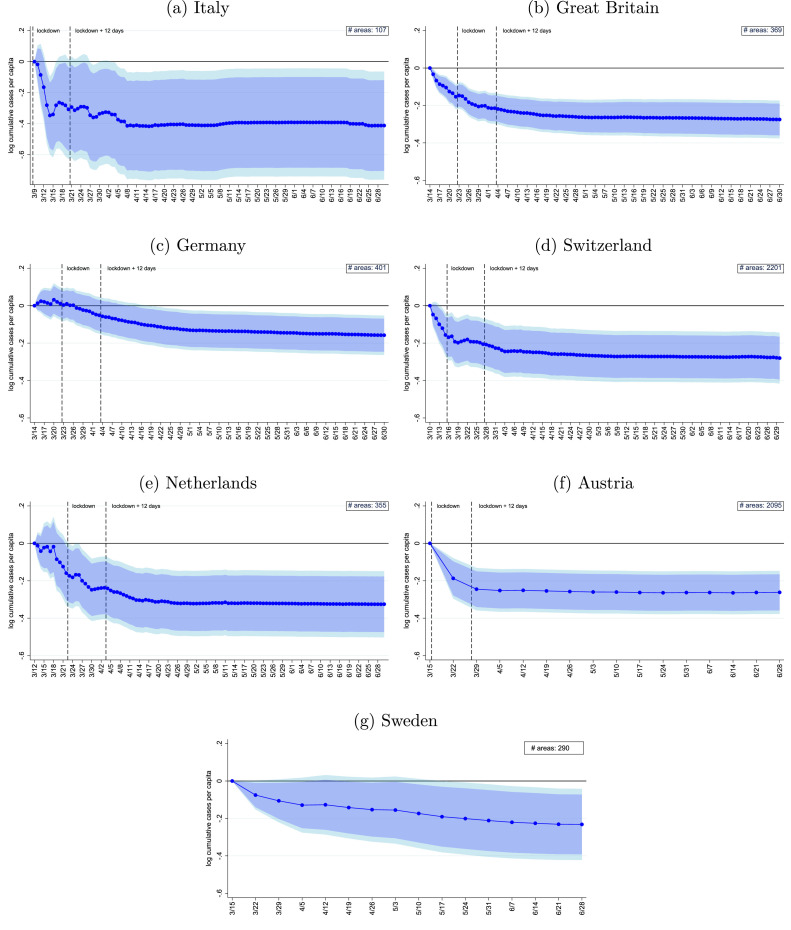
Figure 2 visualizes the coefficients from equation (1). Across all countries, we see a consistent pattern: high-social-capital micro-areas exhibit a slower growth of cumulative cases than low-social-capital micro-areas. A one-standard-deviation increase in social capital reduces the cumulative number of Covid-19 cases in micro-areas over the considered period by 14% () in Germany, 20% () in Austria, 21% () in Sweden, 24% () in Great Britain, 24% () in Switzerland, 28% () in the Netherlands and 34% () in Italy.
Fig. 2.
Effect of social capital on the spread of Covid-19 cases. The figure presents the differential evolution of the relationship between cumulative Covid-19 infections per 100,000 inhabitants and social capital across time. The estimates are based on the model outlined in equation (1) (see Appendix Table C1 for the point estimates). The first dashed line marks the date of the national lockdown, the second dashed line the date of the national lockdown plus 12 days to account for incubation plus confirmation time. Since there was no official lockdown in Sweden, no dashed lines are displayed in panel (g). The dark (light) blue area corresponds to the 90% (95%) confidence interval. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Overall, we interpret the consistent pattern and statistically significant results obtained from independent analyses of seven countries as strong evidence in favor of the hypothesis that social capital plays an important role in slowing down the spread of the virus.
Moreover, our empirical model enables us to analyze the dynamics of the effect of social capital in detail. Figure 2 clearly shows that micro-areas with high social capital exhibit a slower growth in Covid-19 cases in the early phase of the pandemic. Importantly, the responses occur before the national lockdowns could have had any effect: assuming an incubation plus confirmation time of about 12 days (cf. Section 2.2), Figure 2 shows that the bulk of the effect has already materialized before the 12 days following the national lockdown are reached.
It is exactly during this initial phase of the pandemic that we expect the impact of social capital to be strongest, as responsible individual behavior is the only means to flatten the curve. After national lockdowns take effect, the growth differential in Figure 2 between low- and high-social-capital areas stabilizes. This argument is further supported by the Swedish results. As Sweden is the only country that did not implement a national lockdown, social capital should matter over the whole sample period. Correspondingly, the decline in Sweden is more continuous and does not flatten over time. This pattern becomes even clearer when looking at the second wave in Appendix Figure C2.
4.2. Sensitivity
In the following, we test the sensitivity of our main results along various dimensions.
Confounding variables. One concern is that measures of social capital like voter turnout might be correlated with other Covid-19-related characteristics. If this correlation were similar across the seven countries, we could wrongly attribute their effects to social capital. As discussed in Section 3.2, we test the sensitivity of our results by adding (i) different sets of (time-since-outbreak) fixed effects and (ii) obvious confounding variables interacted with day fixed effects (cf. equation (2)).
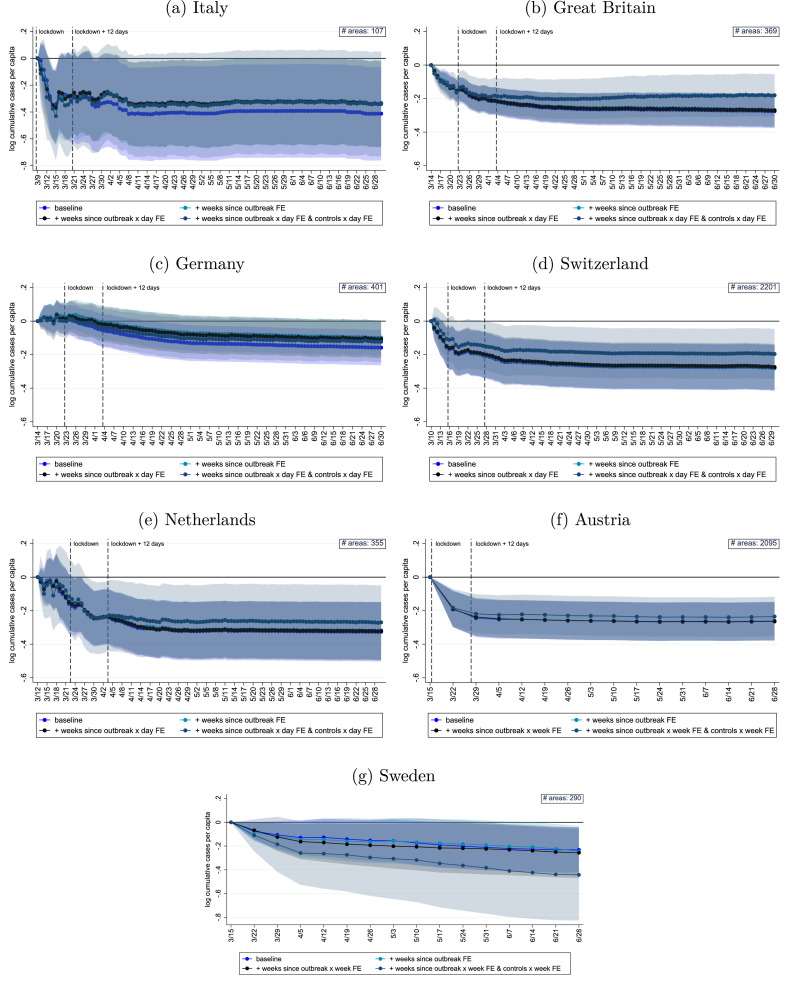
Figure 3 shows the resulting estimates. Magnitudes, dynamics and statistical significance are generally similar across specifications, which is a first indication that further unobserved confounders are unlikely to drive the results.19
Fig. 3.
Effect of social capital on cases with additional fixed effects and controls. This graph shows alternative specifications for the results reported in Figure 2. The dark blue line reports the baseline results in Figure 2 (see Appendix Table C1 for point estimates). The light-blue line includes weeks-since-outbreak fixed effects; the black line includes weeks-since-outbreak x date fixed effects. The grey line additionally includes a set of controls interacted with date fixed affects. The first vertical dashed line marks the date of the national lockdown in each country. The second vertical dashed line corresponds to the date of the national lockdown plus 12 days, which accounts for incubation plus confirmation time. The shaded areas report the 95% confidence intervals. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
To assess the role of unobserved confounders more formally, we also implement the method suggested by Oster (2019), which additionally takes into account movements in the across specifications. We apply the suggested bounding exercise to the last point estimate of our dynamic model (1). Appendix Table C4 shows that all bounded estimates stay negative and close to our baseline estimates when assuming that unobservables are as important as the observables in explaining the effects (). In other words, the table suggests that our findings are robust to omitted variable bias, e.g., due to fear of infection.20
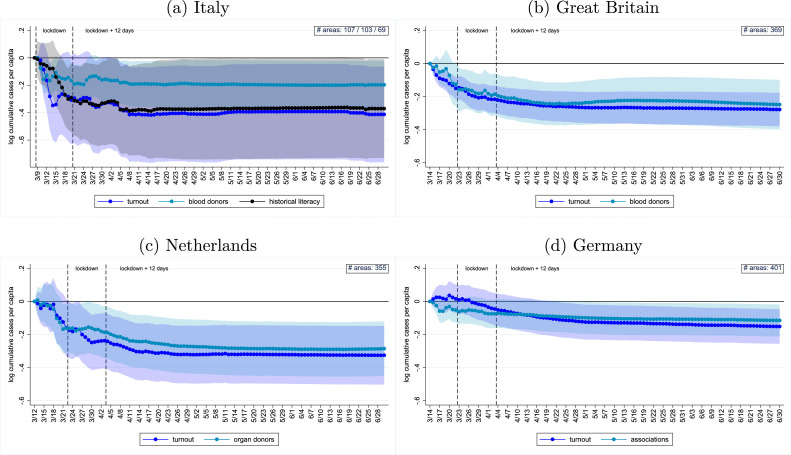
Alternative social capital measures In order to validate that our results are not driven by the choice of our proxy for social capital, we assess the sensitivity of our estimates with respect to alternative social capital measures. Apart from turnout, the literature has validated blood and organ donations as useful proxies of social capital (see, e.g., Guiso, Sapienza, Zingales, 2004, Putnam, 1993). For Italy and Britain, we obtained sufficiently fine-grained data on blood donations. For the Netherlands, we obtained data on the number of registered organ donors willing to donate (see Appendix Table A1 for details). Panels (a) to (c) of Figure 4 show that the results are similar when using these alternative measures.
Fig. 4.
Alternative social capital measures. The figure shows the estimation results of the impact of social capital on the evolution of Covid-19 infections. They are based on the estimation model outlined in equation (1) and the outcome variable is the log cumulative number of Covid-19 infections per 100,000 inhabitants. As measure of social capital, in panel (a) we use turnout, literacy rates in 1821 and blood donations per capita, in panel (b) we use turnout and blood donations per capita, in panel (c) we use turnout and the number of registered organ donors per capita, in panel (d) we use turnout and associations per capita (see Appendix Table C3 for point estimates).
As no comparable data are available for Germany, we use the density of associations, another widely used proxy (Putnam, 2000, Satyanath et al., 2017). Panel (d) shows a very similar effect on Covid-19 cases using this proxy. Last, the literature on social capital frequently studies the case of Italy, because there is large variation in social capital that can be attributed to historical origins that influence social capital to this day (see, e.g., Nannicini, Stella, Tabellini, Troiano, 2013, Putnam, 2000). It is well established that culture, and thus also cultural traits like social capital, are passed on from generation to generation and are thus quite persistent over time (Alesina et al., 2013, Bisin, Verdier, 2000, Tabellini, 2008). Following Tabellini (2010), we use province-level literacy rates from Italy in 1821 as another, historical proxy for social capital, using data from Ciccarelli and Weisdorf (2018).21 This measure again yields a very similar pattern (see Figure 4). Appendix Figure C1 confirms that our results are again robust to the inclusion of additional fixed effects and controls.
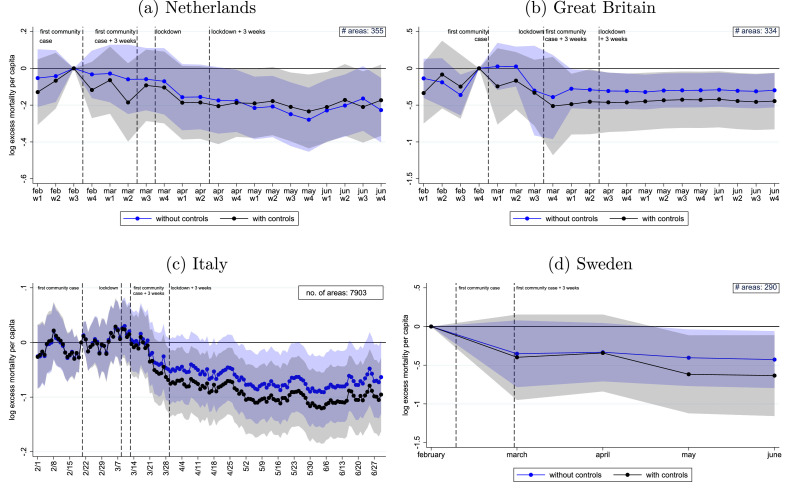
Excess mortality. Additionally, we present the results from using excess mortality as an alternative Covid-related health outcome, estimating equation (3). Figure 5 shows that by the end of June 2020, a one-standard-deviation increase in turnout is significantly associated with fewer accumulated excess deaths per 100,000 inhabitants in Italy, the Netherlands, Sweden and Great Britain. The effect size ranges from 6% in Italy to 35% in Sweden and stays relatively similar when including control variables (see Appendix Table C5). The estimates imply that a one-standard-deviation increase in social capital could have prevented 1632 deaths in Sweden, 1787 deaths in the Netherlands, 2823 deaths in Italy, and 14,303 deaths in Great Britain. Reassuringly, excess mortality before the pandemic evolves in parallel between high- and low-social-capital micro-areas, which lends support to our identifying assumption.22
Fig. 5.
Effect of social capital on excess deaths. The figure presents the differential evolution of the relationship between cumulative excess deaths per 100,000 inhabitants and social capital over time. The estimates are based on the model outlined in equation (3) including NUTS-3 x time FE instead of NUTS-1 x time FE (see Appendix Table C5 for the point estimates). The shaded areas correspond to the 95% confidence interval.
In terms of dynamics, Figure 5 corroborates the evidence shown in Figures 1 and 2: the number of excess deaths in high-social-capital micro-areas starts to drop around the time of (or even before) the national lockdown. This decrease cannot be driven by the lockdown due to the incubation time and the duration of the disease before it leads to fatalities. Instead, we find that excess mortality drops in high-social-capital micro-areas about two to three weeks after the first community case. Moreover, effects stabilize about three weeks after the lockdown. This pattern is in line with evidence that deaths tend to occur around three weeks after the infection (Yang et al., 2020) and points to the specific role of social capital in the absence of strict policy measures.
Extension to the second wave Last, we extend our dataset on Covid-19 cases until the December 31, 2020 to additionally examine the effect of social capital in the second wave, which hit the countries under study in the fall. To this end, we estimate equation 1 on the extended sample. We measure the effect of social capital during the second wave by testing for the difference between the estimate on December 31, 2020 and the estimate on the June 30, 2020. The latter date marks the last day of our baseline sample, when the first wave had receded in all countries (see Appendix Figure A1). During the summer months the case numbers were low but positive in all countries. Hence, we can observe whether cases in high- and low-social-capital micro-areas evolve similarly before the second wave starts. Appendix Figure C2 plots the estimates for all countries, together with an estimate of the additional impact of social capital during the second wave. In six out of the seven countries, we observe an additional social capital effect during the second wave. A one-standard-deviation increase in social capital leads to an additional reduction in cumulative cases per 100,000 inhabitants of 4% () in Switzerland, 7% () in the Netherlands, 7% () in Great Britain, 10% in Germany (), 21% in Sweden () and 28% in Italy (). It is only for Austria that we do not observe a significant additional effect during the second wave. The pattern of the effect is very similar to the first wave. In all cases, the effect materializes before the lockdowns during the second wave could have had any effect, as indicated by the dashed lines. This underscores our interpretation that social capital is particularly important in the absence of strict lockdowns. This interpretation is reinforced by the pattern of the Swedish estimates: in the absence of a lockdown, the effect grows continuously over the whole sample period.
5. Conclusion
In this paper, we provide evidence from seven European countries that social capital has a considerable impact on the spread of Covid-19 cases and the number of excess deaths. Social capital, long known to be related to favorable economic developments, can thus unfold additional potential in times of (health) crises, which call for collective action and socially responsible behavior. The positive effects of social capital are likely to go beyond health outcomes. Experience from the Spanish Flu suggests that a higher level of social capital also has an indirect positive effect on the economy during and after the crisis (Barro, 2020, Barro, Ursúa, Weng, 2020).
Our results have important implications for policymakers. Given the faster spread of the virus in areas with lower social capital, it may help to launch targeted information campaigns and health education programs in these areas. It its important to note that social capital is likely to remain relevant even after vaccines are widely available because the willingness to get vaccinated is a public good just as the willingness to practice social distancing (Chuang, Huang, Tseng, Yen, Yang, 2015, Jung et al., 2013, Rönnerstrand, 2014, Schmelz and Bowles, 2021).
Our results also imply that social capital formation is an important insurance against similar future pandemics. Hence, the insights from our study should encourage policymakers to invest not only in the health system, but also in building social capital to be well prepared. Possible points of departure are social components in transfer programs, or local community programs to increase social exchange, which may carry over to increased cooperation and pro-social behavior (see, e.g., Attanasio, Polania-Reyes, Pellerano, 2015, Fearon et al., 2009, Feigenberg et al., 2013).
CRediT authorship contribution statement
Alina Kristin Bartscher: Conceptualization, Methodology, Data curation, Writing – review & editing. Sebastian Seitz: Conceptualization, Methodology, Data curation, Writing – review & editing. Sebastian Siegloch: Conceptualization, Methodology, Data curation, Writing – review & editing. Michaela Slotwinski: Conceptualization, Methodology, Data curation, Writing – review & editing. Nils Wehrhöfer: Conceptualization, Methodology, Data curation, Writing – review & editing.
Acknowledgements
The views expressed in the paper are solely the responsibility of the authors and should not be interpreted as reflecting the views of Danmarks Nationalbank, Deutsche Bundesbank or the Eurosystem.
Footnotes
We thank the editor, Owen O’Donnell, two anonymous referees, Ulrich Glogowsky, Jarkko Harju, Jan Marcus, Andrew Oswald, Andreas Peichl, Kurt Schmidheiny, Felix Weinhardt, and seminar participants at the University of Mannheim for their helpful comments. We thank the Electronic Epidemiological Reporting System and the Swiss Federal Office of Public Health for providing us with municipal level data on Covid-19 cases for Austria and Switzerland, respectively. Axel Franzen and Katrin Botzen generously shared their data on German associations with us. We are grateful to Elisa Casarin, Christian Hilscher and Dorian Weber, who provided excellent research assistance. We aknowledge funding by the Open Access Publication Fund of the ZEW - Leibniz Centre for European Economic Research. Bartscher acknowledges funding by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation) under Germany’s Excellence Strategy - EXC 2126/1 390838866.
Two prominent examples are: Emmanuel Macron (16.03.2020): “But the best rule is the rule that you, as citizens, impose on yourselves. Once again, I am appealing to your sense of responsibility and solidarity.” Giuseppe Conte (26.04.2020): “The responsible conduct of every one of us will be fundamentally important. (...) If you love Italy, keep your distance.”
There are various studies that analyze the effect of social capital on individual behavior – mostly mobility (see below for a detailed discussion of the literature). However, looking at specific behavioral responses only gives a partial picture of the role of social capital in the pandemic and its net health effects, as different behavioral channels might be substitutes. For instance, individuals who restrict mobility might follow hygiene or social distancing recommendations less strictly.
We selected these countries because high-frequency information on Covid-19 cases was available at a fine geographical level when writing this study in the first wave of the pandemic in early 2020.
For Switzerland, we use participation in the 2019 national elections.
The logarithmic model accounts for the exponential growth of infections and helps to difference out potential measurement error (Goodman-Bacon and Marcus, 2020).
We use weekly data for Austria and Sweden, since that allows us to exploit fine-grained variation at the municipality level. In an earlier version of the paper, we used daily district-level data for Austria and daily county-level data for Sweden. The Swedish data are censored for municipalities with less than 15 cumulative cases. We impute the missing data, assuming a log-linear functional form. The results using the new data are qualitatively similar to our previous results at a higher geographical level, but much more precisely estimated.
In our baseline analysis, micro-area refers to municipalities in the Netherlands, Switzerland, Sweden and Austria, counties in Germany, lower tier local authorities in Great Britain and provinces in Italy.
The threshold value is set at the NUTS-3 level because we want to treat countries symmetrically when defining the sample start. Our micro-areas refer to different types of jurisdictions (e.g. counties in Germany but municipalities in Switzerland), so imposing a common threshold value for micro-areas would lead to a different coverage across countries. NUTS-3 regions are instead harmonized across countries and enable us to adopt a symmetric approach.
Germany, Switzerland and Austria only publish mortality data at the state level. Furthermore, according to Economist (2020), they suffered a substantially lower number of excess deaths per 100,000 inhabitants (Switzerland 8, Germany 9 and Austria 11) than the other countries in our sample in the first wave (Netherlands 58, Sweden 62, Italy 87 and Britain 99). The combination of coarse geographical variation and a low number of deaths makes a systematic analysis impossible.
The Netherlands only publish data at the municipality level for 2019 and 2020.
The literature distinguishes two broad types of social capital: bonding and bridging social capital (Putnam, 2000, Schmitt, van der Eijk, 2007). While the former captures within-group solidarity, the later highlights across-group solidarity. According to, e.g., Putnam (2000) and Satyanath et al., 2017, bonding social capital can have adverse effects and can turn out to be exclusive, while bridging social capital should always have beneficial effects.
For Switzerland, we use data on turnout in the 2019 national elections.
The fine geographical level used in our analysis is important for identification. At the same time, it does not permit us to use common survey-based measures of social capital, such as social trust in the World Values Survey, as these measures are not available at the NUTS-3 or municipal level.
In Switzerland, the whole country is a NUTS-1 region. We therefore perform a robustness check with more granular NUTS-3 fixed effects. The results in Appendix Graph C3 are very similar to the baseline in Figure 2.
As discussed in Section 2, we use alternative measures in Section 4.2 to show that our results are not driven by the choice of the social capital proxy.
In a robustness check, we extend our sample until December 31, and thus include the second wave (see Appendix Figure C2).
Casting the model in event time, where the event is the first case in a specific area, is interesting but not ideal for the research question of this study, as we seek to estimate the impact of social capital on the spread of the virus for given information set about the severity of the virus and given policies in place.
For Great Britain, we use NUTS-1-by-time fixed effects, as the data are reported at the NUTS-3 level. Note that the data do not include Scotland, which only publishes death statistics on a monthly basis.
For better readability of the precision across specifications, Appendix Table C1 reports the last dynamic estimate for each country with standard errors for each specification.
Based on self-collected survey data from the U.S., Barrios et al., 2021 show that fear cannot explain the association between changes in mobility and social capital. Durante et al., 2021 reach the same conclusion, using the distance to regional hotspots as a proxy for fear.
As we operate at least at the NUTS-3 level, we could not use the data in Tabellini (2010), which cover NUTS-1 or NUTS-2 regions across Europe. We transformed our data to the province borders of 1911 (see Appendix Table A1 for details).
Appendix Figure C5 shows a consistent pattern holds for Sweden when using data in 10-day blocks, which are only available from 2018 to 2020.
Supplementary material associated with this article can be found, in the online version, at 10.1016/j.jhealeco.2021.102531
Appendix A. Supplementary materials
Supplementary Raw Research Data. This is open data under the CC BY license http://creativecommons.org/licenses/by/4.0/
References
- Alesina A., Giuliano P., Nunn N. On the origins of gender roles: Women and the plough. Q J Econ. 2013;128(2):469–530. [Google Scholar]
- an der Heide M., Hamouda O. Schätzung der aktuellen entwicklung der Sars-Cov-2-Epidemie in Deutschland. Epidemiologisches Bulletin. 2020;17:10–16. [Google Scholar]
- Aron J., Muellbauer J. INET Oxford Working Paper. 2020. Measuring Excess Mortality: The Case of England during the Covid-19 Pandemic. [Google Scholar]
- Attanasio O., Polania-Reyes S., Pellerano L. Building social capital: conditional cash transfers and cooperation. Journal of Economic Behavior and Organization. 2015;118:22–39. [Google Scholar]
- Bai J.J., Jin W., Wan C. SSRN Working Paper 3609001. 2020. The Impact of Social Capital on Individual Responses to Covid-19 Pandemic: Evidence from Social Distancing. [Google Scholar]
- Bargain O., Aminjonov U. Trust and compliance to public health policies in times of covid-19. J Public Econ. 2020;192:1–13. doi: 10.1016/j.jpubeco.2020.104316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrios J.M., Benmelech E., Hochberg Y.V., Sapienza P., Zingales L. Civic Capital and Social Distancing during the Covid-19 Pandemic. J Public Econ. 2021;193:1–11. doi: 10.1016/j.jpubeco.2020.104310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barro R.J. NBER Working Paper. 2020. Non-Pharmaceutical Interventions and Mortality in U.S. Cities during the Great Influenza Pandemic, 1918–1919. 27049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barro R.J., Ursúa J.F., Weng J. NBER Working Paper. 2020. The Coronavirus and the Great Influenza Pandemic: Lessons from the “Spanish Flu” for the Conoravirus’s Potential Effects on Mortality and Economic Activity. 26866. [Google Scholar]
- Bauernschuster S., Falck O., Woessmann L. Surfing alone? The internet and social capital: Evidence from an unforeseeable technological mistake. J Public Econ. 2014;117:73–89. [Google Scholar]
- Bisin A., Verdier A. Beyond the melting pot: cultural transmission, marriage, and the evolution of ethnic and religious traits. Q J Econ. 2000;115(3):955–988. [Google Scholar]
- Blais A., Galais C. Measuring the civic duty to vote: A proposal. Elect Stud. 2016;41:60–69. [Google Scholar]
- Borgonovi F., Andrieu E., Elodie Bowling together by bowling alone: social capital and covid-19. Social Science & Medicine. 2020;265:113–501. doi: 10.1016/j.socscimed.2020.113501. [DOI] [PubMed] [Google Scholar]
- Bolsen T., Ferraro P.J., Miranda J.J. Are voters more likely to contribute to other public goods? Evidence from a large-scale randomized policy experiment. Am J Pol Sci. 2014;58(1):17–30. [Google Scholar]
- Borgonovi F., Andrieu E., Subramanian S. Community level social capital and Covid-19 infections and fatality in the united states. Covid Economics. 2020;32:110–126. [Google Scholar]
- Bracco E., De Paola M., Green C. Long lasting differences in civic capital: Evidence from a unique immigration event in Italy. Journal of Economic Behavior & Organization. 2015;120:160–173. [Google Scholar]
- Brodeur A., Grigoryeva I., Kattan L. Stay-at-Home orders, social distancing and trust. J Popul Econ. 2021;34:1321–1354. doi: 10.1007/s00148-021-00848-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buonanno P., Montolio D., Vanin P. Does social capital reduce crime? The Journal of Law and Economics. 2009;52(1):145–170. [Google Scholar]
- Chen C., Frey, Carl B., Presidente G. Culture and Contagion: Individualism and Compliance with Covid-19 Policy. Journal of Economic Behavior & Organization. 2021;190:191–200. doi: 10.1016/j.jebo.2021.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuang Y.-C., Huang Y.-L., Tseng K.-C., Yen C.-H., Yang L.-h. Social capital and health-protective behavior intentions in an influenza pandemic. PLoS ONE. 2015;10(4):1–14. doi: 10.1371/journal.pone.0122970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciccarelli C., Weisdorf J. Pioneering into the past: Regional literacy developments in Italy before Italy. Eur Rev Econ Hist. 2018;23(3):329–364. [Google Scholar]
- Ciminelli G., Garcia-Mandic S. Covid-19 in Italy: An analysis of death registry data. J Public Health (Bangkok) 2020;42(4):723–730. doi: 10.1093/pubmed/fdaa165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman J.S. Cambridge, MA: Harvard University Press; 1990. Foundations of social theory. [Google Scholar]
- Costa-Font J., Mladovsky P. Social capital and the social formation of health-related preferences and behaviours. Health Economics, Policy and Law. 2008;3:413–427. doi: 10.1017/S1744133108004635. [DOI] [PubMed] [Google Scholar]
- Dawes C.T., Loewen P.J., Fowler J.H. Social preferences and political participation. J Polit. 2011;73(3):845–856. [Google Scholar]
- Ding W., Levine R., Lin C., Xie W. NBER Working Paper. 2020. Social Distancing and Social Capital: Why US Counties Respond Differently to Covid-19. 27393. [Google Scholar]
- Economist, 2020. Tracking covid-19 excess deaths across countries. Last access: 01.11.2020.
- Durante R., Guiso L., Gulino G. Asocial capital: Civic culture and social distancing during Covid-19. J Public Econ. 2021;194:104–342. doi: 10.1016/j.jpubeco.2020.104342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engle S., Stromme J., Zhou A. Staying at home: Mobility effects of Covid-19. Covid Economics. 2020;4 [Google Scholar]
- Fearon J.D., Humphreys M., Weinstein J.M. Can development aid contribute to social cohesion after civil war? Evidence from a field experiment in post-conflict Liberia. American Economic Review. 2009;99(2):287–291. [Google Scholar]
- Feigenberg B., Field E.M., Pande R. The economic returns to social interaction: Experimental evidence from microfinance. Review of Economic Studies. 2013;80(4):1459–1483. [Google Scholar]
- Folland S. An economic model of social capital and health. Health Economics, Policy and Law. 2008;3:333–348. doi: 10.1017/S1744133108004532. [DOI] [PubMed] [Google Scholar]
- Fowler J.H. Altruism and turnout. J Polit. 2006;68(3):674–683. [Google Scholar]
- Fowler J.H., Kam C.D. Beyond the self: Social identity, altruism, and political participation. J Polit. 2007;69(3):813–827. [Google Scholar]
- Friedson A.I., McNichols D., Sabia J.J., Dave D. Shelter-in-place orders and public health: Evidence from California during the Covid-19 pandemic. Journal of Policy Analysis and Management. 2021;40(1):258–283. [Google Scholar]
- Giuliano P., Wacziarg R. NBER Working Paper. 2020. Who Voted for Trump? Populism and Social Capital. 27651. [Google Scholar]
- Glaeser E.L., Sacerdote B., Scheinkman J.A. Crime and social interactions. Q J Econ. 1996;111(2):507–548. [Google Scholar]
- Glogowsky U., Hansen E., Schchtele S. CESifo Working Paper. 2020. How Effective Are Social Distancing Policies? Evidence on the Fight Against Covid-19 from Germany. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin C., Katz L.F. Human capital and social capital: The rise of secondary schooling in America, 1910–1940. Journal of Interdisciplinary History. 1999;29(4):683–723. [Google Scholar]
- Goodman-Bacon A., Marcus J. Using difference-in-differences to identify causal effects of Covid-19 policies. Surv Res Methods. 2020;14(2):153–158. [Google Scholar]
- Guiso L., Sapienza P., Zingales L. The role of social capital in financial development. American Economic Review. 2004;94(3):526–556. [Google Scholar]
- Guiso L., Sapienza P., Zingales L. Handbook of Social Economics. Vol. 1. Elsevier; 2011. Civic Capital as the Missing Link; pp. 417–480. [Google Scholar]
- Jankowski R. Altruism and the decision to vote: Explaining and testing high voter turnout. Rationality and Society. 2007;19(1):5–34. [Google Scholar]
- Jung M., Lin L., Viswanath K. Associations between health communication behaviors, neighborhood social capital, vaccine knowledge, and parents H1N1 vaccination of their children. Vaccine. 2013;31(42):4860–4866. doi: 10.1016/j.vaccine.2013.07.068. [DOI] [PubMed] [Google Scholar]
- Knack S., Keefer P. Does social capital have an economic payoff? Across-Country investigation. Quarterly Journal of Economics. 1997;112(4):1251–1288. [Google Scholar]
- Lauer S.A., Grantz K.H., Bi Q., Jones F.K., Zheng Q., Meredith H.R., Azman A.S., Reich N.G., Lessler J. The incubation period of coronavirus disease 2019 (Covid-19) from publicly reported confirmed cases: Estimation and application. Ann. Intern. Med. 2020;172(9):577–582. doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichter A., Löffler M., Siegloch S. The long-Term costs of government surveillance: Insights from stasi spying in East Germany. J Eur Econ Assoc. 2021;19(2):741–789. [Google Scholar]
- Nannicini T., Stella A., Tabellini G., Troiano U. Social capital and political accountability. American Economic Journal: Economic Policy. 2013;5(2):222–250. [Google Scholar]
- Oster E. Unobservable selection and coefficient stability: Theory and evidence. Journal of Business & Economic Statistics. 2019;37(2):187–204. [Google Scholar]
- Ostrom E. New York: Cambridge University Press; 1991. Managing the commons: The evolution of institutions for collective action. [Google Scholar]
- Ostrom E. Washington, DC: World Bank; 1999. Social Capital: A Fad or a Fundamental Concept; pp. 172–214. [Google Scholar]
- Painter M.O., Qiu T. Political beliefs affect compliance with government mandates. Journal of Economic Behavior & Organization. 2021;185:688–701. doi: 10.1016/j.jebo.2021.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putnam R.D. Princeton University Press, Princeton, NJ.; 1993. Making democracy work: Civic traditions in modern Italy. [Google Scholar]
- Putnam R.D. Simon and Schuster; 2000. Bowling alone: The collapse and revival of American community. [Google Scholar]
- Rönnerstrand B. Social capital and immunization against the 2009 A(H1N1) pandemic in the American States. Public Health. 2014;128(8):709–715. doi: 10.1016/j.puhe.2014.05.015. [DOI] [PubMed] [Google Scholar]
- Satyanath S., Voigtlnder N., Voth H.-J. Bowling for fascism: Social capital and the rise of the Nazi Party. Journal of Political Economy. 2017;125(2):478–526. [Google Scholar]
- Schmelz K., Bowles S. Overcoming Covid-19 vaccination resistance when alternative policies affect the dynamics of conformism, social norms, and crowding out. Proceedings of the National Academy of Sciences. 2021;118(25) doi: 10.1073/pnas.2104912118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmitt H., Mannheimer R. About voting and non-voting in the European Elections of June 1989. Eur J Polit Res. 1991;19(1):31–54. [Google Scholar]
- Schmitt H., van der Eijk C. European Elections & Domestic Politics. Lessons from the Past and Scenarios for the Future. 2007. Non-voting in European Parliament Elections and Support for European Integration; pp. 145–167. [Google Scholar]
- Steinbrecher M., Rattinger H. In The Europeanization of National Polities?: Citizenship and Support in a Post-Enlargement Union. Oxford Univ. Press; 2012. Explaining Turnout in European Parliament Elections. [Google Scholar]
- Szreter S., Woolcock M. Health by association? Social capital, social theory, and the political economy of public health. Int J Epidemiol. 2004;33(4):650–667. doi: 10.1093/ije/dyh013. [DOI] [PubMed] [Google Scholar]
- Tabellini G. The scope of cooperation: Norms and incentives. Quarterly Journal of Economics. 2008;123(3):905–950. [Google Scholar]
- Tabellini G. Culture and institutions: Economic development in the regions of Europe. J Eur Econ Assoc. 2010;8(4):677–716. [Google Scholar]
- Van Bavel J.J., Baicker K., Boggio P.S., Capraro V., Cichocka A., Cikara M., Crockett M.J., Crum A.J., Douglas K.M., Druckman J.N., et al. Using social and behavioural science to support Covid-19 pandemic response. Nat. Hum. Behav. 2020:1–12. doi: 10.1038/s41562-020-0884-z. [DOI] [PubMed] [Google Scholar]
- Xue X., Reed W.R., Menclova A. Social capital and health: A meta-analysis. J Health Econ. 2020;72:102317. doi: 10.1016/j.jhealeco.2020.102317. [DOI] [PubMed] [Google Scholar]
- Yang X., Yu Y., Xu J., Shu H., Xia J., Liu H., Wu Y., Zhang L., Yu Z., Fang M., Yu T., Wang Y., Pan S., Zou X., Yuan S., Shang Y. Clinical course and outcomes of critically ill patients with Sars-Cov-2 Pneumonia in wuhan, china: A single-centered, retrospective, observational study. The Lancet Respiratory Medicine. 2020;8(5):475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Raw Research Data. This is open data under the CC BY license http://creativecommons.org/licenses/by/4.0/