Abstract
Cystic fibrosis (CF) is a genetic, life-limiting disease without a cure; treatment is complex and lifelong. Respiratory failure is the most common cause of death; however, gastrointestinal disease, diabetes and liver disease are common comorbidities. Coronavirus disease (COVID-19) rapidly changed healthcare services across the globe, including redeployment of healthcare professionals. This adult CF service was challenged to continue a patient facing service within severe staffing and structural limitations.
Not only were many members of the CF multidisciplinary team (MDT) redeployed at the start of the first wave, but also both the CF and ambulatory care wards were closed. Fortunately, the CF clinical nurse specialists (CF-CNSs) remained in their role. Rapid change and adaptation of the CF service was required to ensure that patients did not feel abandoned and access to treatment remained available. The role of the CF-CNS was therefore pivotal in this change.
The aim of this project was to use quality improvement methodology to plan an emergency service allowing a reintroduction of ambulatory care services. Success was measured by the number of patients clinically reviewed with or without intervention, and the reasons for patients contacting the CF-CNS via email and phone were recorded.
In weeks 1 and 2 of the emergency service, the CF-CNSs triaged patients by phone, then reviewed face-to-face when necessary. This first step allowed the CF-CNSs to start two patients on home intravenous antibiotics. This service continued to be developed over the following 12 weeks, leading to a total of 36 patient attendances. In March 2020, n=1187 patients made contact (mostly COVID-19, unwell and medication related), in April n=904 and May n=870 (blood test results, unwell and medication related).
The motivation of the CF-CNSs was pivotal to the success of this initiative with the CF MDT available to provide some support and advice. It concluded at week 12, which then saw the opening of the formal ambulatory care ward and returning redeployed ward staff.
Keywords: COVID-19, quality improvement, PDSA, nurses
Problem
Coronavirus disease (COVID-19) was reported from China in December 2019 and later identified as a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). It was declared a global pandemic by WHO on 11th March 2020.1 2 The unknown effects of COVID-19 led to the cancellation of routine face-to-face clinics and ambulatory care assessment across certain trusts in the UK.
In April 2020, all people with cystic fibrosis (CF) were advised to shield and labelled as clinically extremely vulnerable by Public Health England.3
This adult CF service is one of the largest in Europe with approximately 600 patients. International and national guidelines for the care of children and adults with CF reflect the complexity and lifelong nature of the disease. Care must be provided by an multidisciplinary team (MDT) skilled in the needs of adults with CF and include physiotherapists, dietitians, psychologists, pharmacists, social workers, doctors and clinical nurse specialists. Access must also be available to specialists such as gastroenterologists, microbiologists and endocrinologists. As well as staffing, the guidelines also recommend specialist inpatient wards with particular attention to cross-infection issues and access to ambulatory care so that, as much as possible, adults with CF can receive treatment while continuing with daily life.4
As with other national services, the redeployment of local specialist CF staff, both medical and allied health professionals meant an abrupt change to the service. The closure of both the CF and ambulatory care wards led to a loss of 28 beds and the ability to review and/or start home intravenous antibiotic (IVAB) therapy as all planned and ad hoc treatment stopped. The unknown effects of COVID-19, the loss of the CF ward, the cancellation of all routine face-to-face clinics and halting of ambulatory care caused panic among our cohort of patients with CF.
Although the specialist CF ward was closed, it became apparent that there was an ongoing need to admit the very sick. Consequently, space was found on another ward that was quickly adapted to become a general respiratory ward. Many of the CF ward nurses were redeployed to this ward, which allowed for some continuity of specialist care. Face-to-face clinics were replaced with virtual ‘face-to-face’ clinics aided by self-monitoring spirometry.
Replacing ambulatory care services was a much more difficult task as not only had staff been redeployed, but also the department had been closed. Prepandemic, this fully staffed unit held 20 day-case beds including single-room facilities allowing segregation for those with CF, minimising cross infection. This was replaced in an outpatient setting allowing for three single side rooms, allowing for continued segregation cross infection and inclusive for COVID-19 infection control measures. Although staff were limited in the outpatient department, patients on arrival were escorted to the side room allocated for the CF clinical nurse specialists (CF-CNSs), and staff were made aware of patient arrivals.
When initiating ambulatory home IVAB therapy, this involved a clinical review to decide treatment, choice of antibiotics, blood tests, an intravenous route (indwelling port, long line, peripheral cannula, a peripherally inserted central catheter (PICC) or cannulation), first dose administration to check for side effects and allergies (including observation for 1 hour post administration) and assessment of patient self-administration techniques, including knowledge of side effects, safety and intravenous line care.
Rapid change in an uncertain time was required. Innovation could help lead this service to success as the pandemic invited freedom to experiment with a service ready for development. Innovation allows for fast learning; this includes failing, reviewing and moving forward.5 This service needed restarting under very different circumstances with minimal resources. Quality Improvement (QI) was therefore fundamental to the CF-CNSs who were at the heart of implementing this change.
Overall, the CF-CNS role includes clinical management, education and advocacy and QI incorporated all these skills stretching their ability to the limit without respite. Nevertheless, we continued to learn the importance of maintaining lines of communication with our patients throughout this journey.
The aim of this project was therefore focused on reintroducing ambulatory care by initiating, implementing and developing an emergency service accessible to adults with CF at the Royal Brompton Hospital. To measure success, the number of patients receiving clinical care via this service was recorded. This included all those attending for review, with or without intervention, such as commencing home IVABs. The number of patient contacts and reasons for contacting the CF-CNSs were also collected.
Background
Cystic fibrosis is an autosomal recessive, genetic disease. The CF gene was identified in 1989, and today over 2000 mutations of the CF gene have been reported describing varying disease severity.6–10 Abnormal mucus production due to the disruption of chloride channels particularly affects the lungs, airways and gastrointestinal tract, leading to chronic bacterial lung infection and gastrointestinal malabsorption and obstruction. Concomitant comorbidities include diabetes, liver disease, osteoporosis and male infertility.6 7 9 Respiratory failure remains the most common cause of death, with a median age of death at 31 years and a median predicted survival of 49.1 years for those born today.11
Cystic fibrosis affects over 10,600 people in the UK; however, global geographical distribution is uncertain.11 Although commonly described in Europe, North America and Australia, poor representation in other areas of the world could be due to lack of patient registries and reporting issues.6–8 11 Cystic fibrosis was previously defined as a disease of childhood mainly due to the lack of diagnostic tests and treatment availability, going back as far as the 1940s and 1950s. Today, CF is described as a life-limiting disease of adulthood. This has been primarily due to understanding diagnostic phenotypes, advances in CF care, specialist MDTs, the introduction of newborn screening leading to earlier treatment, patient registry data and clinical research developments.9 10 12
The first Standards of CF Care were published in 2001.13 This was a significant guideline helping to improve CF care in the UK and Europe; a revision was published in 2011.4 13 This update again emphasised the importance of specialist care provided in a specialist centre with the support of a CF specialist MDT including both paediatric and adult consultants, junior doctors, specialist nurses, physiotherapists, dietitians, psychologists, social workers, pharmacists, admin support and database management. Strict segregation measures were also highlighted due to lung pathogen transmission between patients, as well as the importance of sputum microbiology reporting, pulmonary function monitoring, airway clearance reviews, nutritional support and early intervention of complications. With increasing survival, issues of older patients must be taken into consideration therefore psychological support, effective transition programmes, end of life care management, lung transplantation and regular medical reviews to prevent disease decline must be included.4 13
The global devastation of COVID-19 has led to rapid change in healthcare services and innovation has become a driving force to success. Pre-existing issues may have been identified, suddenly allowing freedom and opportunity to implement change.5 Transformational leadership in healthcare impacts a team positively during a crisis and teamwork is an essential element in achieving success, drawing on each person’s expertise, enabling co-ordination of care particularly in a crisis.14–17 Research on crisis management is rare due to the unexpected environment and demands focusing on the crisis head on; published research therefore tends to be qualitative case studies.14
Measurement
To measure the success of this project, data was collected on the number of patients receiving clinical input with or without intervention (eg, the number of patients receiving home IVAB training). The number of CF-CNS patient contacts were also recorded, including the reason for contact. Both these measures allowed for recognition and need for the CF service as well as helping to support the reopening of the ambulatory care ward.
Speroff et al18 suggests that studies using the plan, do, study, act (PDSA) methodology are appraised for validity and rigour using intervention, measurement, study design and data analysis. This recommendation has therefore been used to guide this QI project.
Initial baseline timelines were estimated from data sourced from the now closed ambulatory care ward (approximately 5 hours and 15 min per patient with the support of the full CF MDT). This data was used to calculate the minimum number of hours a patient attending a medical review plus home IVAB training took. This helped to allocate time for each face-to-face patient contact in the new service. During this project, the length of time for each patient contact, as well as a description of each intervention, was recorded. By reviewing and learning from each contact, the service was able to rapidly grow to include more patients.
The project team also looked at historic patient contact data (collected for other reasons) to compare with the current pandemic demand. During a 4-month period in 2006, there were 405 patient contacts, and over 2 months in 2016, there were 1201 patient contacts. Working practice for the CF-CNSs is to report and log each patient contact via telephone or email; data were therefore available; 2961 patient contacts were recorded over 3 months from March to April 2020.
Project design
A crisis requires innovation to succeed as well as a dedicated team. This QI project was driven by the need to implement an emergency service for patients in the community while preventing hospital admissions in a stretched NHS during the pandemic. QI methodology is best suited to plan and develop services under difficult circumstances with minimal resources, and the PDSA methodology is used widely in the healthcare setting. This methodology allows for the development, testing and implementation of change with a focus on small actions that acquire knowledge, allowing development of cycles before implementation.19 It was therefore ideal for this project as data were collected following each patient contact, reviewed as a cycle and adapted from the lessons learnt.
Pandemic staff redeployment meant the MDT was substantially cut, leading subsequently to a reduced project team. However, five CF-CNSs with support from a CF consultant, CF pharmacists and administrators were able to continue. In partnership with the CF-CNSs, these healthcare professionals became the project team.5 The CF-CNSs met each day after a cycle, followed by a wider MDT discussion with the project team. In an ideal, prepandemic world without redeployment, the project team discussions would have taken place with the entire CF MDT.
Although space was identified in an unused area of the outpatient department, the CF-CNSs still had to source equipment such as intravenous access equipment (including long line, midline and cannulas), intravenous pumps, personal protective equipment (PPE), anaphylaxis kits (from pharmacy) and locate the nearest emergency crash trolley. Further unexpected challenges included a full day of online training in the administration of oral and intravenous drugs for two recently appointed CF-CNSs. Additionally, before starting, all CF-CNSs had to retrain in various intravenous access techniques as prepandemic, cannulation had been performed by a different team. There was little time to practice, so much of this learning was done on the spot. For patients with known venous access issues, the CF-CNSs arranged advanced discussions with the radiology team who inserted PICC lines radiologically.
Strategy
This project started by process mapping the prepandemic, ambulatory care ward patient journey and role of the CF-CNS. NHS Improvement20 recommend starting with this process to allow a visual picture to form reflecting a truer representation. The CF-CNS team focused on a clinical review including home IVAB training and initiation. This was then used to identify what was needed for the emergency service. As medical staff were not initially available to carry out patient reviews, the CF-CNSs took this on (having been trained previously to take a medical history and examine a patient) alongside their other duties. Medical advice from a CF consultant was available, mostly by phone. Emergency medical support was available from the hospital emergency crash team should it be required. Three PDSA cycles were performed.
PSDA cycle 1
Aim
To receive direct contact from an unwell patient.
CF-CNS triage including clinical review of the patient and treatment decision (advice from consultant).
Train patient and start home IVAB therapy.
Issues
Excessive waiting time around prescribing and dispensing, leading to hours of lost time for both patient and CF-CNS.
Refreshment facilities were closed; the patient did not have anything to eat or drink during this time.
Difficult intravenous access requiring radiology input (ultrasound guided midline/radiological PICC insertion), which increased patient attendance time.
Change strategy
Preadmission alert to an administrator allowed for the patient to be ‘admitted’ to a ward, ensuring timely online prescribing.
This meant that patients could have intravenous antibiotics pre-prepared and delivered to their home prior to attending the hospital; they could bring the first dose in with them.
Patients with known difficult intravenous access to be discussed with radiology prior to attendance.
Patients to be asked to bring refreshments with them.
PDSA cycle 2
Aim
To receive direct contact from two unwell patients.
CF-CNS triage including clinical review of two patients and treatment decisions made (advice from consultant).
Train patients and start home IVAB therapy, in a shorter time than cycle 1, allowing for difficult intravenous access and refreshment.
Issues
The first patient required a chest X-ray; the department is in a different building.
This highlighted whether we were meeting infection control measures, as face masks had not yet been made mandatory by the UK government. Clinical staff were wearing PPE when face-to-face with patients.
Standards of care recommend regular sputum culture analysis and spirometry to ensure appropriate and effective treatment choices. Both are aerosol-generating procedures.
Change strategy
Masks and information regarding the importance of not removing them to be offered to patients as they entered the hospital.
Prior to attending the hospital, patients will be sent sputum specimen pots and return envelopes and asked to send the specimen back or bring it with them, preventing aerosol exposure in the hospital setting.
Digital home spirometers were distributed to all patients with CF. Patients will be asked to perform spirometry during the CF-CNS telephone triage and assessment. This allows for further effective care management and stops aerosol exposure.
This cycle was successful; the first patient received a clinical review and was trained in the administration of home IVAB with a smoother service and reduced waiting times, allowing a second patient to attend.
PDSA cycle 3
Aim
To receive direct contact from more than two unwell patients.
CF-CNS triage including clinical review of patients and treatment decisions made (advice from consultant).
Train patients and start home IVAB therapy.
Issues
A risk to communal use of the bathroom facilities in the outpatient department now that more than one patient was attending in 1 day.
Change strategy
The project team decided each bathroom should be terminally cleaned after each use. The cleaning contractors’ contact details were made available in the outpatient department for all staff.
Team discussion after each cycle improved timing, patient and staff safety, efficiency and patient satisfaction. This meant that increasing patient numbers could be managed successfully. Change strategies developed from innovative thinking around postal sputum specimens, preadmission home spirometry, IVAB home delivery prior to commencement and asking the patient to attend with the first dose.
Results
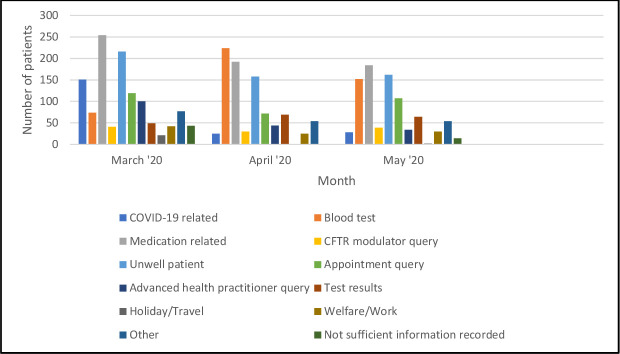
The emergency service continued for 12 weeks in total. Figure 1 illustrates the number of patients reviewed over this period, supporting evidence that QI and PDSA methodology led to the success in this service implementation. Evidence to support this success was gained by learning from each PDSA cycle. This service started with 1 then 2 patients in the first cycles, increasing to 34 patient reviews in weeks 11 and 12.
Figure 1.
Number of patients booked into the emergency service between 31st March 2020 and 19th June 2020. This figure details the increase in patient attendance starting with just 2 patients in the first 2 weeks and 34 patients in the final 11th and 12th week.
The increase in patient attendance was because members of the CF MDT slowly returned to the service from week 4 onwards, including the CF consultants, physiotherapists and dietitians. As well as opening the service to more patients, this allowed for the reintroduction of CF standards of care around safety and increased medical input. Additional benefits included essential blood monitoring, regular heparin flushes for indwelling intravenous access devices to maintain patency, single-dose intravenous or subcutaneous injections, and easier intravenous line replacement or removal, as well as the reintroduction of physiotherapy and nutrition reviews.
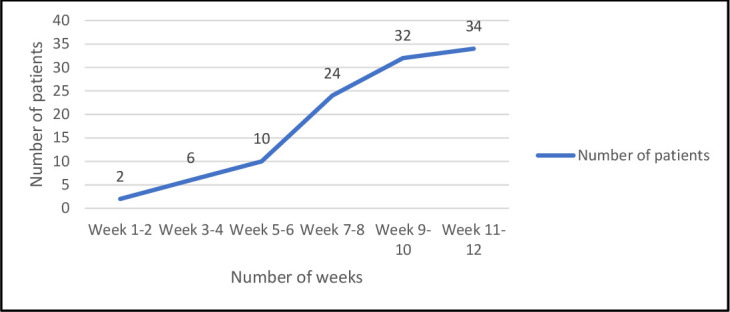
The success of this service implementation was the facility to provide emergency care to treat respiratory exacerbations in a timely way, thus delaying possible long-term deterioration in health status. Figure 2 displays the reason for patient attendance, including commencing home IVABs.
Figure 2.
Reasons for attending the emergency service between 31st March 2020 and 19th June 2020. The first 4 weeks represent the intravenous antibiotic training and administration to patients alongside medical reviews carried out by the CF-CNS. From week 4 onwards displays the increase in patient attendance and services offered due to the returning of the redeployed CF MDT. CF, cystic fibrosis; CF-CNS, CF clinical nurse specialist; MDT, multidisciplinary team.
In addition to the practical hurdles, there were strategic issues to deal with. Although the service was developed in the outpatient department, because it was essentially shut to patients, it was not fit for purpose. However, the CF-CNS team sourced equipment from various places, and the single rooms supported infection prevention and control. Hospitals work on internal computer systems; rapid changes to wards and staffing meant that technology had not caught up. Administrative support therefore allowed patients to be ‘admitted’ to closed wards, permitting medication to be prescribed using the online systems.
Our initial baseline timelines were an assessment of prepandemic ambulatory activity following process mapping. We had estimated that in the previous service, a medical review and commencement of home IVAB took 5 hours 15 min. While our first PDSA cycle had taken a lot longer (6 hours 5 min), we managed to reduce this to 3 hours 25 min, allowing an increase in patient footfall per day.
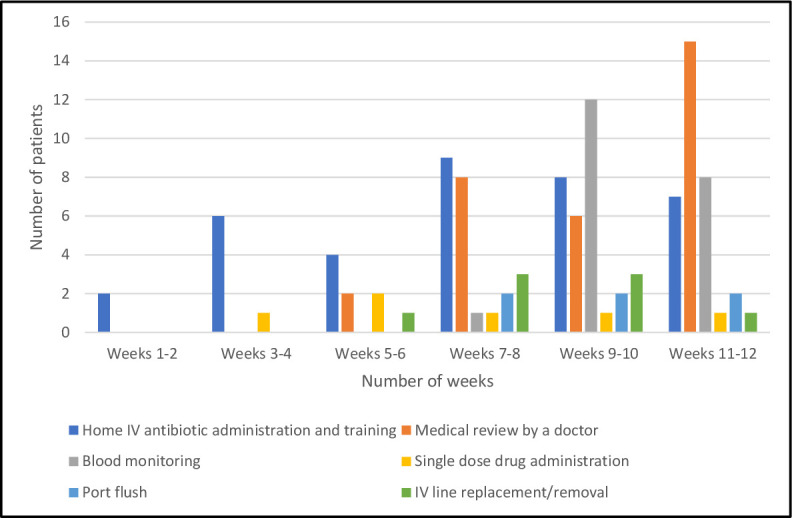
Secondary baseline data analysis also included the reason patients made contact to the CF-CNS team during this time, by phone or email (figure 3). Contact started high with 1187 patient contacts in March. This reduced over the same 3-month period with 904 patient contacts in April and 870 patient contacts in May. The most common reason for contact in the first month were medication queries, COVID-19-related queries and those unwell. During the second and third months, the most common queries related to bloods tests, medication and those unwell.
Figure 3.
Reasons for patient contact between March and May 2020. The UK lockdown started in March 2020, and the highest reasons for patient contact during this month were medication queries, COVID-19-related queries and patients unwell needing advice. Interestingly, COVID-19-related queries reduced thereafter; however, there still remained a large number of patients unwell requiring support and input. CFTR, cystic fibrosis transmembrane conductance regulator.
The emergency service completed roll-out at week 12, as the ambulatory ward was relocated and opened. During the PDSA cycles, several unexpected consequences became apparent. These included patients developing allergic reactions to the IVABs despite previous exposure and dealt with rapidly and safely by the CF-CNSs. Being able to manage aerosol generating procedures in light of the concerns around coronavirus infection, and developing the rapid response service itself in what felt like isolated circumstances. The final unexpected consequence of this project was the enthusiasm, patience and support of the patients. Although recognition of the responsiveness, inventiveness and hard work of the project team is described here, there is no doubt that it was done in partnership with the patients with CF.
Lessons and limitations
This project was driven primarily out of patient need in unforeseen circumstances. There are limitations of this project, including the lack of further detailed data collection such as ongoing markers of disease decline, lung function measurement, weight and the use of oral antibiotics acquired in the community during this period. We were unable to be specific with the timeline, as well as the predicted number of patients potentially using this service due to the nature and unpredictability of the pandemic. Similarly, patient experience data was not collected as this was a rapid response service development under difficult circumstances. We were also challenged to meet patient needs while adapting the CF standards of care. The strengths of this project, however, were putting patients at the centre of planning, providing access to medical interventions to prevent disease decline and the collaboration of the project team led by the CF-CNSs. Developing an emergency service during a pandemic is not without risk, including medical support via telephone and lack of support staff. Risks were identified, discussed and agreed by the CF centre director and consultants once all mitigation had been attempted.
The psychological impact particularly for patients shielding is unimaginable and, combined with a loss of service, can only be described as truly terrifying.21 High patient contact reflected early anxiety and panic with concerns about medication access, COVID-19 queries and sickness in the first month. Continued communication with patients was also met via monthly emails updating patients and families to the changes in service.
Discussion
It is unlikely that the rapid development of a service such as this will be necessary in the future. We have, however, learnt a great deal, both from our mistakes and successes. Many of the interventions are now in place so that should we need to change direction quickly, we have the skills and some small amount of infrastructure to do this.
To assess the rigour and validity of this project, commonly used recommendations were used.18 A clear implementation plan to develop an emergency service was agreed. This service provided urgent clinical care with or without intervention for adults with CF. The project started with process mapping, which led and guided the PDSA cycles.
Risks and benefits were identified and debated throughout. The overarching risk was the loss of CF services, potentially placing patients at a greater threat of deterioration at home. Therefore, the risk was taken to develop emergency services, including asking adults with CF who were shielding, to attend a hospital environment for intervention and treatment. The project team collected data on the number of patients reviewed over a 12-week period increasing patient footfall throughout. Further data collection included patient contact and reasons for contact. Review of this data at team meetings helped decision making for the next cycles.
Quality Improvement falls under several methodologies, yet not all are suitable for this project. For example, Six Sigma methodology explores variability looking at increasing efficiency and minimising defects, more commonly used in digital technologies.22 Lean methodology focuses on a continuous process aiming to reduce waste with cost savings and customer experience at its core.23 It is also common to use more than one QI methodology at a time. However, the rationale for using PDSA methodology in this instance was because the service was being developed during a crisis, with limited resources. It is acknowledged that aspects of the Lean methodology were occasionally employed, particularly in reducing waiting times. Data analysis allowed measurements of success with the number of patients seen, the number of interventions and patient contacts with reasons. Speroff et al18 asks the question: did this change lead to improvement? For this rapidly developed service, the answer is yes.
Conclusion
The COVID-19 pandemic and patient need drove this rapid change of service. Colleagues from within the CF-MDT and staff from other areas supported this new development, but the day-to-day enthusiasm and push came from the CF-CNSs. To complement this service, the CF-CNS team had also initiated the introduction of virtual teaching and support for patients at home. This included removal of intravenous access lines and needles and flushing in-dwelling ports. This adaption to the new service ensures safety and ongoing care to an ‘extremely clinical vulnerable’ cohort. Undoubtably, CF standards of care were challenged and continue to be challenged in an uncertain time. Quality Improvement methodology supported this development, allowing a return to routine services for patients in unforeseen circumstances.
Acknowledgments
A special thanks to the CF nurse specialist team and the entire CF multidisciplinary team. Without teamwork, this project would not have been possible.
Footnotes
Contributors: RD and SM participated in the conception and design of the project. RD was the primary author of the manuscript, collection and analysis of the data and responsible for the overall content. SM supervised the project, revised the draft manuscript critical for important intellectual content. RD and SM approved the final version.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, conduct, reporting or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
All data relevant to the study are included in the article.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Guan W-jie, Ni Z-yi, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med Overseas Ed 2020;382:1708–20. 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization (WHO) . WHO Director-General’s opening remarks at the media briefing on COVID-19, 2020. Available: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 [Accessed 30 Apr 2020].
- 3.Public Health England (PHE) . Guidance on shielding and protecting people who are clinically extremely vulnerable from COVID-19. Available: https://www.gov.uk/government/publications/guidance-on-shielding-and-protecting-extremely-vulnerable-persons-from-covid-19/guidance-on-shielding-and-protecting-extremely-vulnerable-persons-from-covid-19 [Accessed 30 Apr 2020].
- 4.Cystic Fibrosis Trust . Standards for the clinical care of children and adults with cystic fibrosis in the UK. Available: https://www.cysticfibrosis.org.uk/~/media/documents/the-work-we-do/care/consensus-docs-with-new-address/cystic-fibrosis-trust-standards-of-care.ashx?la=en [Accessed 2 May 2020].
- 5.Clark L. Innovation in a time of crisis. Available: https://www.harvardbusiness.org/innovation-in-a-time-of-crisis/ [Accessed 20 Apr 2020].
- 6.Hodson ME, Geddes DM, Bush A. Cystic fibrosis. 3 edn. London: Hodder Arnold, 2007. [Google Scholar]
- 7.Elborn JS. Cystic fibrosis. Lancet 2016;388:2519–31. 10.1016/S0140-6736(16)00576-6 [DOI] [PubMed] [Google Scholar]
- 8.Seyed BM, Farnia P, Hassanzad M. Geographical distribution of cystic fibrosis; the past 70 years of data analyzis. BBRJ 2017;1. 10.4103/bbrj.bbrj_81_17 [DOI] [Google Scholar]
- 9.Castellani C, Duff AJA, Bell SC, et al. ECFS best practice guidelines: the 2018 revision. J Cyst Fibros 2018;17:153–78. 10.1016/j.jcf.2018.02.006 [DOI] [PubMed] [Google Scholar]
- 10.Clinical and functional translation of, CFTR. resources / CFTR2. Available: https://cftr2.org [Accessed 10 Feb 2020].
- 11.Cystic Fibrosis Trust . UK cystic fibrosis registry annual data report, 2019. Available: https://www.cysticfibrosis.org.uk/the-work-we-do/uk-cf-registry/reporting-and-resources [Accessed 25 Aug 2020].
- 12.Stern M, Bertrand DP, Bignamini E, et al. European cystic fibrosis Society standards of care: quality management in cystic fibrosis. J Cyst Fibros 2014;13 Suppl 1:S43–59. 10.1016/j.jcf.2014.03.011 [DOI] [PubMed] [Google Scholar]
- 13.Cystic Fibrosis Trust Clinical Standards and Accreditation Group . Standards for the clinical care of children and adults with cystic fibrosis in the UK. London: Cystic Fibrosis Trust, 2001. [Google Scholar]
- 14.Pearson CM, Clair JA. Reframing crisis management. Acad Manage Rev 1998;23:59–76. 10.5465/amr.1998.192960 [DOI] [Google Scholar]
- 15.Sommer SA, Howell JM, Hadley CN. Keeping positive and building strength: the role of affect and team leadership in developing resilience during an organizational crisis. Group Organ Manag 2016;41:172–202. 10.1177/1059601115578027 [DOI] [Google Scholar]
- 16.Klein KJ, Ziegert JC, Knight AP, et al. Dynamic delegation: shared, hierarchical, and Deindividualized leadership in extreme action teams. Adm Sci Q 2006;51:590–621. 10.2189/asqu.51.4.590 [DOI] [Google Scholar]
- 17.Yun S, Faraj S, Sims HP. Contingent leadership and effectiveness of trauma resuscitation teams. J Appl Psychol 2005;90:1288–96. 10.1037/0021-9010.90.6.1288 [DOI] [PubMed] [Google Scholar]
- 18.Speroff T, James BC, Nelson EC, et al. Guidelines for appraisal and publication of PDSA quality improvement. Qual Manag Health Care 2004;13:33–9. 10.1097/00019514-200401000-00003 [DOI] [PubMed] [Google Scholar]
- 19.NHS Improvement . Quality, service improvement and redesign tools: plan, do, study, act (PDSA) cycles and the model for improvement. Available: https://improvement.nhs.uk/documents/2142/plan-do-study-act.pdf [Accessed 9 May 2020].
- 20.NHS Improvement . Process mapping - a conventional model. Available: https://improvement.nhs.uk/resources/process-mapping-conventional-model/ [Accessed 24 May 2020].
- 21.Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 2020;395:912–20. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Niñerola A, Sánchez-Rebull M-V, Hernández-Lara A-B. Quality improvement in healthcare: six sigma systematic review. Health Policy 2020;124:438–45. 10.1016/j.healthpol.2020.01.002 [DOI] [PubMed] [Google Scholar]
- 23.Lean enterprise Institute. What is lean? Available: https://www.lean.org/WhatsLean/ [Accessed 28 Jun 2020].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data relevant to the study are included in the article.