Abstract
Objective: Dermatofibrosarcoma protuberans (DFSP) of the vulva is an uncommon soft tissue tumor with fewer than 60 cases reported previously. Distant metastasis is rare with a high propensity for local invasion. Surgical management is the gold standard with adequate margin excision to prevent future recurrences. We report a case of vulvar DFSP requiring three resections to achieve primary clearance. To the best of our knowledge, this is the first case report from India.
Case report : A 35-years-old female, presented with nodular vulvar mass for the third time arising from the upper part of right labia majora for the last year. She had a history of two similar episodes in the past for which excision was done and histopathology confirmed DFSP. The third wide local resection was performed with 3 cm margins and the margins were sent for intra-operative frozen section analysis, which was confirmed clear by the pathologist. The patient has been free of recurrence for two years.
Conclusion: DFSP is a challenging condition presenting as a non-tender nodular mass characterized by local invasion and recurrence. Early diagnosis and appropriate management using wide local excision with accurate margin assessment can achieve optimal results and prevent future recurrences.
Key Words: Dermatofibrosarcoma, Vulva, Margins of Excision, Local Neoplasm Recurrence
Introduction
Dermatofibrosarcoma protuberans (DFSP) is a rare dermal mesenchymal tumor with an estimated incidence of only 3-5 cases per million persons in the United States of America (1, 2). Clinically, it is a superficial, slow-growing tumor affecting mainly the trunk and extremities. It usually presents in the third and fifth decades of life (3). Vulvar DFSP is strikingly rare with less than 60 cases reported in the literature so far (1). It is characterized by local dermal and subcutaneous infiltration along with the destructive invasion of adjacent tissues (muscle, fascia, and bone) in a lace-like manner (1). It is locally aggressive with 20-49% chances of local recurrence (4). However, it rarely metastasizes with fewer than 5% of patients developing distant spread. Surgery is the first line of management for both primary and recurrent lesions with wide local excision and adequate margin assessment. We present a case of DFSP of the vulva with third-time recurrence that was managed successfully with a radical hemi-vulvectomy with 3 cm healthy margins all around. To the best of our knowledge, this is the first case report from India.
Case report
A 35 years old female, presented with a pedunculated vulvar mass arising from the upper part of right labia majora for the last year. The mass gradually increased in size, causing discomfort in her daily routine tasks. The patient had a history of 2 similar episodes in the past. Initially, the mass appeared for the first time seven years back, about 5*6 cm in size for which wide local excision was done and the histopathology report showed a mesenchymal tumor with intermediate malignant potential-Dermatofibrosarcoma Protuberans. The patient has advised radiotherapy for the same but she did not comply and instead took some homeopathic treatment. Within six months of this excision, the patient had her first local recurrence- growth at the same site measuring 10*8*6 cm. She underwent wide local excision again at some private hospital with histopathology report showing low-grade fibrosarcoma. Then after 5 years, the patient had her third growth (second recurrence) at the same vulvar site. Obstetrics history revealed one full-term delivery by cesarean section, one right-sided tubal ectopic pregnancy for which the patient underwent right salpingectomy 10 years back. There was no history of sexually transmitted diseases or perineal trauma. There was no relevant family or past history. On general examination, her vitals were normal and systemic examination was unremarkable. On local examination- a pedunculated mass of size 6*6 cm was seen arising from the upper part of the right labia majora involving mons pubis. It was firm in consistency and freely mobile with ulceration on the surface (Figure 1). Given her previous history, recurrence of DFSP was kept in mind and the patient was planned for more radical excision. All routine investigations were within normal limits: Hemoglobin-10.5gm%, Total Leucocyte Count-6000/mm3, Platelet Count- 1.2lac/mm3, Blood urea-17mg%, Serum creatinine- 0.4mg%, SGOT (Serum glutamic oxaloacetic transaminase) -77IU/L, SGPT (Serum glutamic pyruvic transaminase)- 97IU/L, Serum Sodium levels-135meq/L, Serum Potassium levels - 4.7 meq/L, HIV (human immunodeficiency virus) and HBsAg (Hepatitis B surface antigen) were non-reactive, but anti HCV (Hepatitis-C Virus) was reactive for which she was undergoing antiviral therapy. After taking informed consent, radical hemi vulvectomy was done with excision of the mass along with 3cm healthy margins all around taking care of the urethral area. On deeper clearance, a small nodule measuring 1*1.5 cm was seen in the deeper tissues, lying separate from the main mass, and was resected separately.
Figure 1.
Clinical picture depicting the nodular growth of the vulva.
The resected margins were subjected to intra-operative frozen section analysis which were clear as confirmed by the pathologist. Both the specimens were sent for histopathological examination afterwards which confirmed the diagnosis of DFSP. On immunohistochemistry, it stained positively for CD34 (Figures 2, 3).
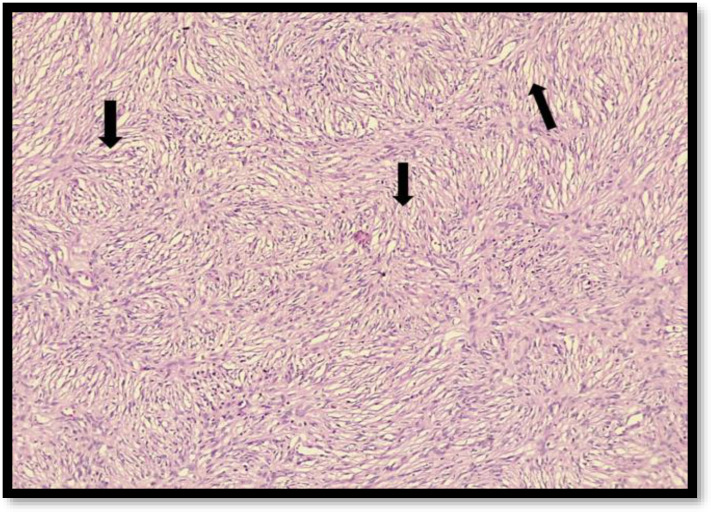
Figure 2.
H&E section (40X) shows a tumor comprised of oval to spindle-shaped cells arranged in a storiform pattern (as depicted by arrows)
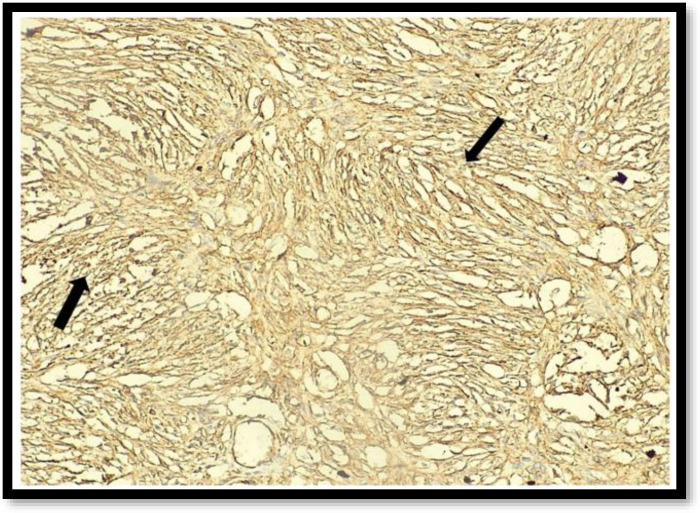
Figure 3.
Immunohistochemistry depicting CD 34 positivity (4+) as depicted by arrows.
The postoperative period was uneventful with proper care of the perineal area keeping it aseptic and dry to avoid any complications. The patient was discharged in a satisfactory condition. The patient had been under regular follow-up for the last two years and is disease-free at the time the report is published.
Discussion
DFSP is a well-differentiated fibro-cutaneous neoplasm of low to intermediate grade malignancy commonly involving the head & neck and upper and lower extremities. Involvement of the vulva is uncommon but when present constitutes 1.5-5% of all vulvar malignancies (5). The tumor was first described in 1890 by Taylor (3). Darier and Ferrand recognized it as a clinicopathological entity in 1929 (6). Although the exact aetiology is unknown but some available data suggests an association with previous trauma, scars, burns tattoos, vaccination scars, and radiodermatitis (1,7). In 2010, Edelweiss et al published the largest case series of 13 patients with histologically confirmed DFSP. Out of 13 patients, 12 presented with a vulvar mass with right labia majora being the most frequent site of origin (in 8 patients) and one with a pigmented skin lesion. All patients were managed surgically with excision biopsy, wide local excision, or radical vulvectomy. Out of these, 7 patients had local recurrences with one patient developing distant metastasis to the lungs. All the local recurrences were offered a repeat surgery. On follow-up over 2 to 444 months, 9 patients were disease-free, 2 alive with disease, one patient had died due to metastasis and another died due to some other pathology (8). The tumor can involve labia majora, labia minora, clitoris, para-clitoral area or mons pubis. Most of the case reports describe left labia majora as the most frequent site of origin with or without the involvement of clitoris or mons pubis (4). However, our patient presented with a vulvar mass on the right labia majora with the involvement of mons pubis similar to Edelweiss et al.. Clinically, the patient may be asymptomatic or may present with pain, ulceration, bleeding, or nodular vulvar mass which is freely mobile on deeper tissues. Our patient had a nodular mass along with ulceration with a gradual increase in size. Grossly, the tumor seems to be a well-circumscribed nodular growth due to condensation of connective tissue at the margins of the nodules which is a false impression as it has microscopic finger-like projections (cartwheel appearance) that infiltrate the surrounding tissues responsible for frequent recurrence (9). Owing to the unusual location and indolent course, vulvar DFSP remains undetected in the early stages posing a diagnostic challenge. The differential diagnosis includes leiomyosarcoma which is also composed of spindle cells but differs immunohistochemically by staining positive for smooth muscle makers like actin, desmin, and vimentin. A rare variant of malignant melanoma may also mimic DFSP, which however can be differentiated by intraepidermal melanocytic proliferation and are positive for S-100. Another rare tumor of the vulva which can be confused with DFSP is a solitary fibrous tumor and can be differentiated by the random arrangement of spindle cells (pattern-less pattern) in comparison to the typical storiform pattern of DFSP. Similarly, benign neural tumors can be mistaken for DFSP, but S-100 negative/CD34 positive status on immunohistochemistry can correctly identify DFSP (8). The definitive diagnosis for DFSP is by histopathology and immunohistochemistry, and most DFSP’s stain positively for CD34 including our case (10).
≥11). In our patient, radical hemi vulvectomy was done with 3 cms of adjacent margins which were confirmed to be disease-free on frozen section analysis during surgery. Also, a deep nodular growth of size 1*1.5 cms was removed separately. Further chances of local recurrence can be minimized by Mohs’ micrographic surgery which employs microscopic examination of lateral and deep margins using frozen tissue sections (12). Several studies report a recurrence rate as low as 1.5% using this technique (12). However, it is time-consuming and expensive requiring a specialized team of surgeons. Another method is CCPDMA (Complete Circumferential Peripheral and Deep Margin Assessment) which involves excision of the tumor with a margin <3 cms followed by histological evaluation by the pathologist and additional immunohistochemistry in doubtful cases. The reported recurrence is less than 10% (13). Currently, there are no randomized controlled trials or prospective studies available to determine the superiority of one surgical technique over the other. Due to the rareness of lymphatic spread and no signs of metastasis in our patient, lymphadenectomy was not required. The overall survival rate is 91-100% (14). As per the previous studies, most of the recurrences are reported within 3 years of primary surgery, so follow-up every 3-6 months for the initial three years is advocated. However, our patient had a second recurrence after 6.5 years of initial growth. So, long-term follow-up every 6 months seems to be reasonable. Adjuvant therapy in the form of RT (Radiotherapy) or chemotherapy is debatable and their routine use in the management of DFSP needs further studies. However, in some studies, RT has been shown to reduce recurrence when used along with surgical management (3). According to NCCN (National Comprehensive Cancer Network), 2014 guidelines, post-operative RT or chemotherapy with Imatinib mesylate can be considered in positive margins where any more resection is not possible (12). Our case-report has certain key-highlights that differentiate it from the previous ones. Firstly, this is the first case reported from India. Secondly, the cases that have been published so far, reported recurrence within 3 years of the primary growth of the vulva. However, we report a recurrence as late as six years from the date of primary growth which is unusual and should be highlighted. Lastly wide local excision with accurate margin assessment can achieve optimal results and prevent future recurrences as seen in our patient who has been under follow up for the last two years and has been disease free so far. So, we propose a long term follow up of such patients for timely detection and management.
Conclusion
To conclude, DFSP of the vulva is an exceptionally challenging condition causing severe cosmetic and functional mutilation to the patient. Diagnosis is often difficult due to its unusual location and needs to be distinguished from other tumors by histopathology and immunohistochemistry. Management is complicated requiring complete surgical excision with negative margins to achieve good results. Intra-operative frozen section analysis is beneficial in assessing the resection margins to reduce the chances of future recurrences. Owing to a higher propensity to reoccur, long-term follow-up is advocated in such patients.
Acknowledgments
Authors have no conflict of interests.
Notes:
Citation: Goyal LD, Garg P, Kaur M, Sharma D. Recurrent Dermatofibrosarcoma Protuberans of the Vulva: A Rare Occurrence and Review of Literature. J Fam Reprod Health 2021; 15(2): 136-40.
References
- 1.Jeremic J, Stefanovic A, Jeremic K, Jovic M, Pilic I, Cvetkovic A, et al. Giant dermatofibrosarcoma protuberans vulvae: Rare clinical presentation and literature review. J Buon. 2019;24:1289–95. [PubMed] [Google Scholar]
- 2.Neff R, Collins R, Backes F. Dermatofibrosarcoma protuberans: A rare and devastating tumor of the vulva. Gynecol Oncol Rep. 2019;28:9–11. doi: 10.1016/j.gore.2019.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Verma H, Sehgal K, Panchal KB, Chakraborty S, Biswas B, Mukherjee G, et al. Presentation and management of dermatofibrosarcoma protuberans: a single center protocol. Indian J Surg Oncol. 2020;11:35–40. doi: 10.1007/s13193-019-01007-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moodley M, Moodley J. Dermatofibrosarcoma protuberans of the vulva: a case report and review of the literature. Gynecol Oncol. 2000;78:74–5. doi: 10.1006/gyno.2000.5821. [DOI] [PubMed] [Google Scholar]
- 5.Oge T, Benedicic C, Tamussino K, Regauer S. Dermatofibrosarcoma protuberans of the vulva: a case report. BMJ Case Rep. 2009;2009:bcr07.2008.0377. doi: 10.1136/bcr.07.2008.0377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leake JF, Buscema J, Cho KR, Currie JL. Dermatofibrosarcoma protuberans of the vulva. Gynecol Oncol. 1991;41:245–9. doi: 10.1016/0090-8258(91)90317-x. [DOI] [PubMed] [Google Scholar]
- 7.Baker PA, O’Dowd GJ, Khan IU. Dermatofibrosarcoma protuberans arising in a decorative tattoo. Sarcoma. 2005;9:37–41. doi: 10.1080/13577140500094289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Edelweiss M, Malpica A. Dermatofibrosarcoma protuberans of the vulva: A clinicopathologic and immunohistochemical study of 13 cases. Am J Surg Pathol. 2010;34:393–400. doi: 10.1097/PAS.0b013e3181cf7fc1. [DOI] [PubMed] [Google Scholar]
- 9.Taylor HB, Helwig EB. Dermatofibrosarcoma protuberans. A study of 115 cases. Cancer. 1962;15:717–25. doi: 10.1002/1097-0142(196207/08)15:4<717::aid-cncr2820150405>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 10.Sardesai VR, Patil RM, Agarwal TD. Dermatofibrosarcoma protuberans at an uncommon site. Indian J Dermatol. 2014;59:635. doi: 10.4103/0019-5154.143602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roses DF, Valensi Q, LaTrenta G, Harris MN. Surgical treatment of dermatofibrosarcoma protuberans. Surg Gynecol Obstet. 1986;162:449–52. [PubMed] [Google Scholar]
- 12.Loghdey MS, Varma S, Rajpara SM, Al-Rawi H, Perks G, Perkins W. Mohs micrographic surgery for Dermatofibrosarcoma protuberans (DFSP): A single-centre series of 76 patients treated by frozen-section Mohs micrographic surgery with a review of the literature. J Plast Reconstr Aesthet Surg. 2014;67:1315–21. doi: 10.1016/j.bjps.2014.05.021. [DOI] [PubMed] [Google Scholar]
- 13.Bertolli E, Bretchbuhl ER, Camarço WR, Campagnari M, Molina AS, Baiocchi G, et al. Dermatofibrosarcoma protuberans of the vulva: Margins assessment and reconstructive options - A report of two cases. World J Surg Oncol. 2014;12:1–6. doi: 10.1186/1477-7819-12-399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Karlen JR, Johnson K, Kashkari S. Dermatofibrosarcoma protuberans of the vulva. A case report. The Journal of reproductive medicine. 1996;41:267–9. [PubMed] [Google Scholar]