Abstract
This paper examines the role of institutions—notably the degree of administrative decentralisation across levels of government—in health care decision-making and health spending as well as life expectancy. The empirical analysis builds on a new methodology to analyse health sector performance. In particular, the present analysis examines the impact of centralisation versus decentralisation of responsibilities across levels of government, making use of newly collected data on governance and expenditure assignment, as well as non-linear empirical specifications. An interlocking U-shaped relationship is found with respect to expenditure and life expectancy. Under moderate decentralisation, public spending in health care is lower, while life expectancy is higher, compared with more centralised systems; however, in highly decentralised systems, public spending is higher and life expectancy is lower. This finding of a “fish-shaped” relationship for decentralisation and outcomes also helps to understand recent reforms of OECD health systems, which have often reverted towards more moderate degrees of administrative decentralisation.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10198-021-01390-1.
Keywords: Public economics, Health care, Intergovernmental fiscal relations, Governance
Introduction
This paper reports novel findings of an empirical analysis aimed at exploring the role of institutions—notably the degree of administrative decentralisation across levels of government—in health care decision-making, public spending on health care, and life expectancy. This empirical analysis builds upon de la Maisonneuve et al. [1] and Lorenzoni et al. [2], and extends this earlier work by adding “decentralisation” as a key explanatory variable in a simultaneous equation regression model. Decentralisation may allow for health systems to better target regional needs, while fostering good competition [3, 4]; at the same time, taken too far, it can lead to fragmentation and overly high costs [5]. The administrative decentralisation indicator and indicators for other institutional features of health care systems such as financial incentives to improve quality and depth of basic coverage are used in a country-level analysis of the impact of policy changes on public spending on health care and life expectancy.
With regard to decentralisation, several new findings emerge from this analysis:
The results point to a statistically significant effect of “administrative decentralisation” on health care expenditure and life expectancy.
The sign and size of the coefficients suggest that a moderate degree of decentralisation reduces public spending on health care and increases life expectancy—saving public resources and improving outcomes—as compared to countries with very low decentralisation.
However, “excessive” decentralisation is associated with higher public spending on health care and lower life expectancy—reversing cost-saving and outcome-enhancing effects—as compared to a situation with an intermediate degree of decentralisation.
This paper is divided into three sections. The first section describes data sources used and how scores were assigned to the decentralisation indicator, and the empirical approach. The second section presents regression results for the model, and discusses the impact of a higher degree of decentralisation on health care spending and life expectancy. The third section concludes.
Methods and data
Data on health systems characteristics obtained through OECD surveys carried out in 2008, 2012, 2016 and 2018 were used to derive an indicator of “decentralisation” as well as 16 additional indicators to describe key institutional features that shape health care financing and coverage arrangements, health care delivery systems, governance and resource allocation (Table 1). These 16 policy-oriented indicators were selected on the basis of their relevance to performance analysis and the applicability of a standard measurement approach to the 2008, 2012 and 2016 surveys on health system characteristics carried out by the OECD [6].
Table 1.
List of indicators selected for the analysis by domain
| Health financing and coverage arrangements | Indicator | Short definition and interpretation |
|---|---|---|
| Depth of basic coverage | Coverage of eight health care functions by basic primary health insurance. The higher the score the more depth of coverage reported | |
| Level of financial protection for health care users | Share of health care spending financed by the public sector, social insurance and private insurance in total health spending. The higher the score the lower the share of out-of-pocket expenditure in total health spending | |
| Out-of-pocket payments for curative care | Share of OOP expenditure for inpatient and outpatient curative care in total health spending. The higher the score the higher the share of curative care paid OOP by households | |
| Degree of user choice for basic coverage | Sources of basis health coverage, ability/freedom to choose an insurer and market share covered by top insurers. A high score indicates multiple insurers and a situation where individuals can choose among more than five insurers | |
| “Over the basic” coverage | Role played by private health insurance offering complementary, supplementary or duplicative coverage on a voluntary basis. The higher the score the larger the role of a high competitive insurance market for "over the basic" coverage | |
| Patient choice among providers | Whether individuals are free to choose any doctor or hospital to seek care, face incentives to choose a specific doctor or hospital, or have limited choice. A higher score reflects a system with greater choice among providers | |
| Role of primary care in the health system (gate-keeping) | Financial incentives or obligation that individuals face when registering with primary care physicians, and incentives or obligation to access secondary care. A higher score reflects a higher level of constraints for individuals | |
| Health care delivery systems | ||
| Incentives for volume increase in physicians' payment methods | Predominant mode of payment of primary care physicians and specialists. The higher the score the stronger the incentive to generate volumes | |
| Incentives for volume increase in hospitals' payment methods | Predominant mode of payment of hospitals. The higher the score the stronger the incentive to generate volumes | |
| Degree of private provision—physicians | The highest score is assigned when the predominant provision of primary care and out-patient specialist services is private only | |
| Regulation of medical staff in hospitals | Reflects conditions for recruitment and remuneration of medical staff in hospitals. The maximum score is assigned when recruitment is decided at central government level, and pay scales are set or negotiated at central level | |
| Incentives for health care quality | A higher score reflects a system with stronger incentives in place for primary care physicians, specialists and hospitals to increase quality | |
| Governance and resource allocation | ||
| Definition of the health benefit basket | Describes how the benefits covered by basic primary health insurance are defined for medical procedures and pharmaceuticals. A higher score reflects the definition of a benefit basket at central level by a positive list | |
| Use of Health Technology Assessment | Existence and use of health technology structure and capacity to determine benefit coverage, reimbursement level/prices and clinical guidelines. Higher score = greater use of HTA | |
| Regulation of prices/fees for primary care physicians' services paid by third-party payers | The higher the degree of regulation by institutions providing financing of basic primary coverage the higher the score assigned | |
| Regulation of prices/fees for hospitals' services paid by third-party payers | The higher the degree of regulation by institutions providing financing of basic primary coverage the higher the score assigned | |
Source: OECD [6]
With regard to the “degree of decentralisation across levels of government”, countries were asked to indicate the level of government that is responsible for thirteen policy or service areas, covering setting decision-making on funding sources and budgets, allocation of resources, remuneration of physicians, financing and investment in hospitals as well as setting of public health objectives.
For each decision in which the government is involved, a score was attributed on a scale of 0 to 6, with 0 being a fully central government decision, while 6 a fully local government decision; shared decisions are given an intermediate score of 3. Then, an overall score was computed as the average of sub-scores related to each decision, as follows:
The maximum score of six was assigned when all decisions are taken at the local level, and a score of zero was assigned when all decisions are taken at the central level:
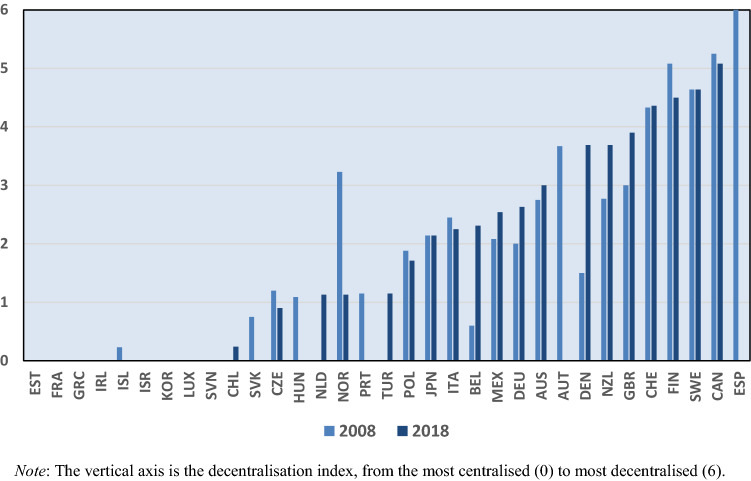
Figure 1 shows the “decentralisation” scores by country in 2008 and 2018. Out of the 22 countries for which responses were available both in 2008 and 2018,1 seven countries reported a lower level of decentralisation in 2018 as compared to 2008, 10 countries a higher level, whereas for five countries, there was no change in the level of decentralisation.
Fig. 1.
Degree of “decentralisation” scores by country, 2008 and 2018
Scores for the other indicators used to characterise the institutional context were assigned applying the methodology described in the online Appendix to the OECD Health System Characteristics survey responses gathered in 2008, 2012 and 2016.2
To explore the relationship between the degree of decentralisation and public spending on health care and life expectancy, a system of simultaneous non-linear equations is used — see de la Maisonneuve et al. [1] and Lorenzoni et al. [2] for a description of the model and its use in previous work. A micro-founded model of utility maximisation by a social planner subject to a budget constraint and a health production function underlies the empirical work (see Appendix A). This model suggests that public spending on health care per capita depends on income and on the share of the elderly (age of 65 + years) in the population. Likewise, life expectancy depends on total health care spending, GDP per capita (net of total health care spending), the stock of people with upper secondary and higher education, the prevalence of daily smoking and alcohol consumption in litres per capita.3 Identification of this system of equations does not raise any specific issues, since: i) usual exclusion restrictions ensuring identification in linear systems do not apply to non-linear systems; ii) the dependent variable in the first equation (i.e. log public expenditure per capita) is different from the explanatory variable in the second equation (i.e. 5-year lag of log total expenditure per capita). We nevertheless take a cautious stance and use in the longevity equation the predicted value of lagged log total expenditure per capita as obtained from a first-stage non-linear regression spanning the 1995–2015 period.
Non-institutional data used in the analysis cover 26 OECD countries over the period 2000 to 2015, as well as comparable life expectancy at birth data extracted from OECD. Stat and expenditure data from the OECD’s System of Health Accounts4 [8] database.
The economic intuition underlying the non-linear specification of the model is straightforward. There are fundamental factors driving the core amount of health care spending which can be magnified by some health policies and institutions, or conversely be reduced by efficient regulations and practices. For that reason, policies and institutions intervene in a multiplicative way in the model and affect all determinants in a similar way.
The econometric model of public spending on health care per capita (HPublic) for country i in year t can be written as:
where GDP is the Gross Domestic Product per capita at constant US Purchasing Power Parities net of total health care expenditure, D is the share of the elderly (age of 65 + years) in the population, is a normalized index of institutional and health system features (m) with zero-mean and unity standard deviation, a coefficient capturing the effect of institutional and health systems variables on public spending on health care, e are unobserved country effects and f unobserved time effects.
The econometric model of life expectancy (LE) for country i in year t can be written as:
where H is the total health care spending expressed in per capita constant USD Purchasing Power Parities, a coefficient capturing the effect of institutional and health systems variables on life expectancy, c are unobserved country effects and is a set of other observed factors, which includes income as measured by GDP per capita at constant USD PPP net of total health care expenditure, the stock of upper secondary and higher education, prevalence of daily smoking and alcohol consumption in litres per capita.
Results
Regression results are reported in Table 2. The core determinants of public spending on health care are examined first. The share of the old-age population is not statistically significant in the regression and has a negative sign. While contrary to previous results (see [2]), this is in line with the hypothesis that increasing expenditure is correlated with time to death, rather than with ageing per se [9]. The results also show that a 1% increase in GDP per capita is associated with a 0.47% increase in health spending. This partial income elasticity is lower than results reported in previous studies and meta-analyses.5
Table 2.
Results for the effects of institutional arrangements on public spending on health care and life expectancy
| Dependent variable | Log public spending on health care per capita | Log life expectancy |
|---|---|---|
| Core determinants | (1) | (2) |
| Log of share of old−age population | −0.137 | |
| (0.17) | ||
| Log of total health care spending per capita | 0.033*** | |
| (0.00) | ||
| Log of GDP per capita | 0.478*** | 0.035*** |
| (0.11) | (0.00) | |
| Log higher education | 0.004 | |
| (0.00) | ||
| Log smoking | − 0.015*** | |
| (0.00) | ||
| Log alcohol consumption | − 0.012*** | |
| (0.00) |
| Health system characteristics | ||
|---|---|---|
| Health financing an coverage arrangements | ||
| Depth of basic coverage | − 0.221*** | 0.106*** |
| (0.04) | (0.02) | |
| Level of financial protection for health care users | − 1.008*** | 0.369*** |
| (0.09) | (0.06) | |
| Out−of−pocket payments for curative care | − 1.051*** | 0.338*** |
| (0.12) | (0.06) | |
| Degree of user choice for basic coverage | 0.196*** | 0.056** |
| (0.04) | (0.03) | |
| "Over the basic" coverage | − 0.487*** | 0.114*** |
| (0.05) | (0.03) | |
| Patient choice among providers | 0.363*** | -0.111*** |
| (0.06) | (0.03) | |
| Role of primary care in the health system (gate−keeping) | 0.508*** | -0.223 |
| (0.07) | (0.04) | |
| Health care delivery systems | ||
| Incentives for volume increase in physicians' payment methods | 0.055 | -0.022 |
| (0.06) | (0.04) | |
| Incentives for volume increase in hospitals' payment methods | 0.376*** | -0.007 |
| (0.05) | (0.03) | |
| Degree of private provision of physicians services | 0.288*** | − 0.014 |
| (0.06) | (0.03) | |
| Regulation of medical staff in hospitals | − 0.143*** | 0.251*** |
| (0.07) | (0.03) | |
| Incentives for health care quality | − 0.04 | 0.059** |
| (0.04) | (0.02) | |
| Governance and resource allocation | ||
| Definition of health benefits basket | − 0.053 | 0.042* |
| (0.04) | (0.02) | |
| Use of Health Technology Assessment | 0.184*** | 0.044* |
| (0.04) | (0.02) | |
| Regulation of prices/fees for primary care physicians' services paid by third−party payers | − 0.310*** | 0.086*** |
| (0.06) | (0.03) | |
| Regulation of prices/fees for hospitals' service paid by third−party payers | 0.211*** | -0.179*** |
| (0.06) | (0.03) | |
| Decentralisation | − 0.970*** | 0.344*** |
| (0.11) | (0.05) | |
| Decentralisation—squared term | 0.193** | − 0.064*** |
| (0.02) | (0.01) | |
| N = 410 | ||
| Country dummies | Yes | Yes |
| Time dummies | Yes | No |
| Adjusted R2 | 0.999 | 0.999 |
Robust standard errors in parentheses. Statistical significance: * 10% level; ** 5% level; *** 1% level. Decentralisation-related coefficients and standard errors are shown in bold. Note the non-linear estimator generates an unusually high R-squared value, without a standard interpretation
Focusing on the core determinants of longevity, a 1% increase in total health care spending per capita is associated with a gain of 0.33 months of life expectancy,6 and a 1% increase in GDP per capita is associated with a gain of 0.35 months of life expectancy. A 1% increase in smoking is associated with a loss of 0.15 months of life expectancy, and a 1% increase in alcohol consumption is associated with a loss of 0.12 months of life expectancy.
The analysis performed in this paper shows that an increase in the depth of basic coverage is associated with a decrease in health spending and an increase with longevity. This is consistent with the view that coverage expansion significantly increases patients’ access to care and the use of preventive care [11, 12]. Likewise, better financial protection for health care users and lower out-of-pocket payments for curative care have similar effects.
Another policy examined in this study concerns supplementary, complementary or duplicate coverage for health spending by health insurers (“secondary coverage” or “over the basic” coverage). Such insurance covers a range of services that “depend on the scope of the basic benefit package, on effective access to covered care and on government regulation on possible roles for private health insurance” [13]. In this analysis, a larger role played by a highly competitive secondary insurance market is associated with lower public spending on health care, which may be explained by a less comprehensive coverage of the benefit package.
There is mixed evidence in the literature on the impact of patient choice of providers on expenditure. On the one hand, patient choice of providers may—in principle—encourage providers to seek efficiency gains and maintain quality of care [14, 15]. However, if prices are not fixed or there is no cap on total payments to providers [16], individual choice of provider can also lead to higher spending and have mixed effects on quality of care. Our results point in the direction of higher spending associated with larger choice of providers.
Gate-keeping arrangements are expected to help control costs by requiring primary care physicians to pre-authorise service use by patients, screening out unnecessary services [17]. There has been wide variation in the stringency of gate-keeping regulations and incentives across countries, and the evidence on the system-wide impacts on health spending and outcome of gate-keeping implementation is still limited [18–23]. The results of the analysis carried out in this paper show that more stringent gate-keeping arrangements can rather increase public spending on health.
Empirical studies have generally supported the theoretical predictions in that traditional fee-for-service (FFS) payment is associated with “over-treatment” or “inappropriate treatment” [24–26] as physicians’ remuneration depends on the level and mix of services provided and not appropriateness of care. An extensive literature review [27] showed that salary payments are associated with fewer services per patient and longer consultations in comparison to both FFS and capitation. Stronger incentives for volume increase embedded in physicians’ remuneration are conducive to higher spending, which is consistent with the findings of this analysis.
Economic theory has suggested that, all else being equal, payment schemes based on provider or patient characteristics generally give hospitals stronger incentives to contain spending compared to payments based on service characteristics [25]. A systematic review and meta-analysis [28] found high variability of the impact of activity-based payment on the volume of hospital care. It also pointed to a possible increase in readmissions and discharges to post-acute care, and thus to increase in health spending, which is consistent with the results of this study.
Another policy analysed in this paper targets privately organised provision of physicians’ services. In line with the literature, our study shows that a higher degree of private provision of physicians’ services is associated with larger health spending, often linked to the use of new and expensive technologies [29].
Incentives for quality have been widely used across OECD countries as a way to realign payment incentives to providers to enhance quality and increase efficiency [30–34]. In primary care, bonuses are paid most frequently for the achievement of targets relating to preventive care and the management of chronic diseases, less often for the uptake of IT initiatives, patient satisfaction or prescription of generic medicines. In hospitals, payment bonuses relate most commonly to patient experience, clinical outcomes and the use of appropriate processes. According to the analysis in this paper and in line with the literature, these incentives increase health spending but are not associated with a positive impact on longevity.
Health technology assessment (HTA) can complement the use of evidence-based clinical guidelines by providing evidence related to new medical technologies during assessment, appraisal and decision-making processes [35, 36]. However, the use of HTA can also lead to expenditure increases mainly related to the additional use of effective services, as well as cost increases related to the up-front investment to create, expand and operate health technology assessment agencies. Thus, it seems plausible that higher scores in use of HTA—which reveal the existence of institutional structures and capacity for technology assessment and encourage the additional use of effective services—are associated with higher health spending as suggested by the positive coefficient on this variable in our study.
The notion of “pricing” sits at the heart of payments for specialist and hospital services across most OECD countries [37]. There is a long and established literature arguing that health care is far from being a classic market for goods and services as it is characterised by patients that have imperfect information. This gives providers (and insurers) a disproportionate influence on the demand for health care goods and services [38], likely driven by providers and insurers’ interests [39]. This combination of information asymmetry and diverging motivations has often justified a greater degree of price regulation in health as governments seek to ensure socially optimal levels of service delivery and increase efficiency [40]. In line with this literature, a stronger regulation of prices/fees for primary care physician services is associated with lower public expenditure on health.
Finally, in a highly underexplored area, the effect of decentralisation on public spending on health care and life expectancy is found to be statistically significant. The sign of linear coefficients shows that a higher degree of decentralisation tends to reduce public spending on health care, and also increases life expectancy. This is broadly in line with the limited literature on this topic [41–43] that also reflects the fact that “the ability of decentralisation to achieve its objectives is complex and ambiguous” [44]. Yet, the significantly negative quadratic term suggests that when decentralisation is “excessive”, cost-savings reverse and outcomes worsen—which is an innovative and novel new finding. This result on both the cost and quality channels is illustrated in Fig. 2. This finding is consistent with the idea that competition-enhancing effects of decentralisation may be helpful in improving efficiency and incentives up to a point, but that excessive decentralisation may lead to over-specialisation and fragmentation of health care services, a finding that has been observed in the health care budgeting and the broader administrative reform literature [45, 46].
Fig. 2.
Marginal effect of decentralisation on public spending on health care and life expectancy
Concluding remarks
Overall, the empirical analysis presented here with regard to the institutional variables provides credible results in line with previous work [1, 2]. Policies aimed at increasing the depth of basic coverage and the level of financial protection for health care users may help achieving higher value for money by raising life expectancy and reducing public spending on health care at the same time, while policies associated to increasing capacity and use of health technology assessments and fostering a higher degree of user choice of basic insurance improve life expectancy and raise public spending on health care at the same time. Stricter health price regulation tends to be associated with lower spending public spending on health care, while the evidence on gate-keeping arrangements is mixed.
The paper finds an intriguing new result that decentralisation exhibits a non-linear “fish-shaped” relationship with costs and outcomes: in moderately decentralised health systems, public spending in health care is lower, while life expectancy is higher, as compared with predominately centralised or more decentralised systems. In fact, the worst cost and quality outcomes are observed in the systems that are “excessively” decentralised. These findings also help to understand recent reforms of OECD country health systems, which have often reverted to more moderate degrees of decentralistion.
These results are particularly significant in light of the wide range of experiences of different countries’ health systems in coping with the recent COVID-19 pandemic outbreak [47]. While our model’s setup makes considerable efforts to address identification, it is possible that some health system features may be partially endogenous, and poor outcomes may feed back into changes in health policy. Likely this would strengthen our interpretation, by making the empirical relationships harder to observe. Yet further work is desirable in this area, notably analysis at the provider level, where we have begun to observe lower hospital costs in countries with a moderate degree of decentralisation, after controlling for hospital management and type of medical condition treated.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors are grateful to Francesca Colombo, Peter Gal, Peter Hoeller, Chris James and delegates of the OECD Network on Fiscal Relations for their useful comments. The paper builds upon collaborative work conducted with the OECD Joint Network of Senior Budget and Health Officials. The opinions expressed and arguments employed herein are solely those of the authors and do not necessarily reflect the official views of the OECD or of its member countries.
Appendix A
To better understand the relationship between health spending, outcomes, institutional arrangements and health system efficiency, we develop a stylised model of utility maximisation by a social planner subject to a budget constraint and a health production function.
Let us consider a representative agent who maximises utility derived from individual consumption expressed in real terms and health status denoted as . For the sake of simplicity, we abstract from the heterogeneity associated with age and consider a unique life period. Utility is given by the following CES function:
| 1 |
As a particular case, a Cobb–Douglas utility function is obtained for . In the above function, health status is an unobserved, latent, health compound that includes both mortality risks (and life expectancy) and morbidity status. The representative agent maximises utility under the budget constraint:
| 2 |
where is real health spending per capita, relative health prices (i.e. health prices divided by a consumption/income deflator), and y real individual income proxied by real GDP per capita. There is no physical capital, no savings and no international trade in the economy.
An individual’s health state is determined by a health production function that uses individual health spending with decreasing returns to scale and is augmented by an exogenous technological variable that captures the quality of health technologies as well as a number of risk factors:
| 3 |
A social planner will maximise aggregate utility over consumption and health spending subject to the resource constraint and the production function of health. Denoting as the share of real health spending in real income, the optimal allocation solves:
| 4 |
The optimal allocation of health spending and consumption satisfies the following first-order condition:
| 5 |
The equation above links the optimal health spending share to the technological variable, relative health prices and real income. The optimal share appears on both sides of the equation. However, Eq. (5) can be further simplified. Health relative prices are on average close to one and the average health spending share is around 8% of the GDP in a sample of high-income OECD countries. The expression is the income elasticity of health spending H, which is likely to be smaller but close to one. This yields the following approximation: . Then, the optimal health spending share in real income can in turn be conveniently approximated as:
| 6 |
And the optimal health spending per capita then is:
| 7 |
Health policies and institutions enter the formulation above as factors that influence the degree of return of health expenditures. In practice, policies and institutional factors determine the magnitude of the parameter in the health production function, with high-return policies raising parameter and therefore the health level for a given amount of health spending.
It is interesting to note that the impact of institutions on health spending per capita depends on the value of the elasticity of substitution in the utility function (1). If (or , consumption and health status have low substitutability. Any increase in parameter would lower health expenditures per capita, which is the desired outcome from a public policy perspective.
The specification of our econometric model follows naturally from Eqs. (3) and (7). Taking logs on both sides of the equation yields the following expression:
| 8 |
While this equation is not directly estimable, it suggests a log-linear reduced form where health spending is explained by health policies and institutions (P), through the elasticity of the health production function , the preferences towards health , health care prices and quality, and real income.
We further assume that the share of health spending in the utility term is affected by demographic factors proxied by the ratio of people aged 65 + to working-age population (or the dependency ratio) D,7 as follows:
| 9 |
In the present analysis, we also assume that relative prices of health are equal to 1 (further data work may alleviate this assumption).
The returns to policies in the health production and health spending functions are assumed to be an index of policies, and the exogenous technological variable an index of other economic and risk factors plus country and time effects:
| 10 |
The production function of life expectancy then becomes:
| 11 |
After noting that health return and country time effects jointly form new country effects , that income y also enters in the technological factors X, and considering the average coefficient in front of economic and risk factors Q, the implied equation for health spending (8) becomes:
| 12 |
As it can be seen by inspecting Eqs. (11–12), the economic intuition underlying the non-linear specification is straightforward. On the one hand, there are fundamental factors driving the core amount of health spending: income, demographic factors, the price and the quality of health services (neglected as a first step). On the other hand, the core amount of health spending can be magnified by inefficient health policies and institutions, or on the contrary be reduced by efficient regulations and practices. For that reason, policies and institutions intervene in a multiplicative way in the model and affect all fundamental factors in a similar way. Equations (11–12) are estimated via non-linear least-squares.
Funding
Not applicable.
Availability of data and material
Available upon request.
Code availability
Available upon request.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Four countries – Estonia, Israel, Slovenia and Chile – did not fill in the questionnaire, as they were not members of the OECD in 2008. Seven countries – France, Korea, Slovakia, Hungary, Portugal, Austria and Spain – did not respond to the questionnaire in 2018. For those 11 countries, an assumption of no change in the decentralisation score over time is made in the regression analysis.
This model follows James et al. [7]. Environmental factors, the unemployment rate and healthy diet were excluded from the model, as the association between life expectancy and those variables was not significant in their analysis.
The System of Health Accounts database provides a systematic account of overall financial flows through national health systems, including information on where the money comes from, who manages it, and how it is used. The 2016 release of the SHA used in this study includes national expenditure estimates through 2015.
For example, Acemoglu et al. [10] derive a central estimate for the income elasticity of health spending of around 0.72.
This is computed as follows: 80 (average LE) * 0.033 (regression coefficient for the covariate) / 100 * 12 (months per year).
Note that it is not possible to identify the effect of time-constant policies passing through as other time-constant factors may be channelled through .
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Sean Dougherty, Email: Sean.Dougherty@oecd.org.
Luca Lorenzoni, Email: Luca.Lorenzoni@oecd.org.
Alberto Marino, Email: alb.marino@outlook.com.
Fabrice Murtin, Email: Fabrice.Murtin@oecd.org.
References
- 1.de la Maisonneuve C, Moreno-Serra R, Murtin F, Oliveira MJ. The role of policy and institutions on health spending. Health Econ. 2017;26:834–843. doi: 10.1002/hec.3410. [DOI] [PubMed] [Google Scholar]
- 2.Lorenzoni L, Murtin F, Springare L, Auraaen A, Daniel F. Which policies increase value for money in health care? OECD health working papers 104. Paris: OECD Publishing; 2018. [Google Scholar]
- 3.Oates WE. An essay on fiscal federalism. J. Econ. Lit. 1999;37:1120–1149. doi: 10.1257/jel.37.3.1120. [DOI] [Google Scholar]
- 4.Weingast BR. Second generation fiscal federalism: the implications of fiscal incentives. J. Urban Econ. 2009;65(3):279–293. doi: 10.1016/j.jue.2008.12.005. [DOI] [Google Scholar]
- 5.Rodden J. Reviving leviathan: fiscal federalism and the growth of government. Ind. Organ. 2003;57(4):695–729. doi: 10.1017/S0020818303574021. [DOI] [Google Scholar]
- 6.Paris V, Devaux M, Wei L. Health systems institutional characteristics: a survey of 29 OECD countries. OECD health working papers 50. Paris: OECD Publishing; 2010. [Google Scholar]
- 7.James C, Devaux M, Sassi F. Health and inclusive growth. OECD health working papers 103. Paris: OECD Publishing; 2017. [Google Scholar]
- 8.OECD, Eurostat, WHO . A system of health accounts. Paris: OECD Publishing; 2011. [Google Scholar]
- 9.Lis, M.: Age or time-to-death – What drives health care expenditure? Panel data evidence from the OECD countries. Badań Strukturalnych (IBS) working paper 04/2016, Warsaw (2016)
- 10.Acemoglu D, Finkelstein A, Notowidigdo M. Income and health spending: evidence from oil price shocks. Rev. Econ. Stat. 2013;95(4):1079–1095. doi: 10.1162/REST_a_00306. [DOI] [Google Scholar]
- 11.Moreno-Serra R, Smith PC. Broader health coverage is good for a nation’s health: evidence from country-level panel data. J. R. Stat. Soc. 2015;178(Part 1):101–124. doi: 10.1111/rssa.12048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sommers BD, Gawande AA, Baicker K. Health insurance coverage and health—what the recent evidence tells us. N. Engl. J. Med. 2017;377(6):586–593. doi: 10.1056/NEJMsb1706645. [DOI] [PubMed] [Google Scholar]
- 13.Paris V, Hewlett E, Auraaen A, Alexa J, Simon L. Health care coverage in OECD countries in 2012. OECD health working papers, no. 88. Paris: OECD Publishing; 2016. [Google Scholar]
- 14.Volpp K, William S, Waldfogel J, Silber J, Schwartz J, Pauly M. Market reform in New Jersey and the effect on mortality from acute myocardial infarction. Health Serv. Res. 2013;38:515–533. doi: 10.1111/1475-6773.00131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gaynor M, Moreno-Serra R, Propper C. Death by market power: reform, competition, and patient outcomes in the National Health Service. Am. Econ. J. Econ. Pol. 2013;5:134–166. doi: 10.1257/pol.5.4.134. [DOI] [Google Scholar]
- 16.de Lagasnerie G, Paris V, Mueller M, Kumar A. Tapering payments in hospitals—experiences in OECD countries. OECD health working papers, no. 78. Paris: OECD Publishing; 2015. [Google Scholar]
- 17.Docteur E, Oxley H. Health-care systems: lessons from the reform experience. OECD health working papers, no. 9. Paris: OECD Publishing; 2003. [Google Scholar]
- 18.Or Z. Exploring the effects of health care on mortality across OECD countries. OECD labour and social policy occasional papers no. 46. Paris: OECD Publishing; 2001. [Google Scholar]
- 19.Or Z, Wang J, Jamison D. International differences in the impact of doctors on health: a multilevel analysis of OECD countries. J. Health Econ. 2005;24:531–560. doi: 10.1016/j.jhealeco.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 20.Forrest C. Primary care gatekeeping and referrals: effective filter or failed experiment? BMJ. 2003;326(7391):692–695. doi: 10.1136/bmj.326.7391.692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bhat NV. Institutional arrangements and efficiency of health care delivery systems. Eur. J. Health Econ. 2005;3:215–222. doi: 10.1007/s10198-005-0294-1. [DOI] [PubMed] [Google Scholar]
- 22.Moreno-Serra R. The impact of cost-containment policies on health expenditure: evidence from recent OECD experiences. OECD J. Budg. 2014;12:1–29. [Google Scholar]
- 23.Greenfield G, Foley K, Majeed A. Rethinking primary care’s gatekeeper role. BMJ. 2016;354:i4803. doi: 10.1136/bmj.i4803. [DOI] [PubMed] [Google Scholar]
- 24.Gerdtham U-G, Jönsson B. International comparisons of health expenditure: theory, data and econometric analysis. In: Culyer A, Newhouse J, editors. Handbook of Health Economics. Amsterdam: Elsevier; 2000. [Google Scholar]
- 25.Ellis R, Miller M. Provider payment methods and incentives. In: Kris H, editor. International encyclopaedia of public health. Oxford: Oxford Academic Press; 2008. [Google Scholar]
- 26.Devlin RA, Sarma S. Do physician remuneration schemes matter? The case of Canadian family physicians. J. Health Econ. 2008;27(5):1168–1181. doi: 10.1016/j.jhealeco.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 27.Gosden T, Forland F, Kristiansen IS, Sutton M, Leese B, Giuffrida A, Sergison M, Pedersen L. Capitation, salary, fee-for-service and mixed systems of payment: effects on the behaviour of primary care physicians. Cochrane Database Syst. Rev. 2000;3:CD002215. doi: 10.1002/14651858.CD002215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Palmer KS, et al. Activity-based funding of hospitals and its impact on mortality, readmission, discharge destination, severity of illness, and volume of care: a systematic review and meta-analysis. PLoS One. 2014;9(10):e109975. doi: 10.1371/journal.pone.0109975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chandra A, Skinner JS. Technology growth and expenditure growth in health care. National Bureau of Economic Research Working Paper No. 16953, 2011. [PubMed]
- 30.OECD . Better ways to pay for health care. OECD Health Policy Studies. Paris: OECD Publishing; 2016. [Google Scholar]
- 31.Epstein AM. Pay for performance at the tipping point. N. Engl. J Med. 2007;356(5):515–517. doi: 10.1056/NEJMe078002. [DOI] [PubMed] [Google Scholar]
- 32.OECD: Achieving better value for money in health care. OECD Health Policy Studies, OECD Publishing, Paris (2009). 10.1787/9789264074231-en
- 33.Charlesworth, A., Davies, A., Dixon, J.: Reforming payment for health care in Europe to achieve better value. Nuffield Trust Research Report (2012). http://www.nuffieldtrust.org.uk/sites/files/nuffield/publication/120823_reforming-payment-for-health-care-in-europev2.pdf. Accessed 15 Dec 2020
- 34.Milstein R, Schreyoegg J. Pay for performance in the inpatient sector: a review of 34 P4P programs in 14 OECD countries. Health Policy. 2016;120(10):1125–1140. doi: 10.1016/j.healthpol.2016.08.009. [DOI] [PubMed] [Google Scholar]
- 35.OECD . Value for money in health spending. OECD health policy studies. Paris: OECD Publishing; 2010. [Google Scholar]
- 36.Auraaen A, Fujisawa R, de Lagasnerie G, Paris V. How OECD health systems define the range of good and services to be financed collectively. OECD health working papers, no. 90. Paris: OECD Publishing; 2016. [Google Scholar]
- 37.Kumar A, de Lagasnerie G, Maiorano F, Forti A. Pricing and competition in specialist medical services—an overview for South Africa. OECD health working papers, no. 70. Paris: OECD Publishing; 2014. [Google Scholar]
- 38.Blomqvist A. The doctor as double agent: Information, asymmetry, health insurance, and medical care. J. Health Econ. 1991;10(4):411–432. doi: 10.1016/0167-6296(91)90023-G. [DOI] [PubMed] [Google Scholar]
- 39.Barber SL, Kumar A, Roubal T, Colombo F, Lorenzoni L. Harnessing the private health sector by using prices as a policy instrument: lessons learned from South Africa. Health Policy. 2018;122(5):558–564. doi: 10.1016/j.healthpol.2018.03.018. [DOI] [PubMed] [Google Scholar]
- 40.Ellis RP, McGuire TG. Supply-side and demand-side cost sharing in health care. J Econ. Perspect. 1993;7(4):135–151. doi: 10.1257/jep.7.4.135. [DOI] [PubMed] [Google Scholar]
- 41.Arendts H. More with less? Fiscal decentralisation, public health spending and health sector performance. Swiss Polit. Sci. Rev. 2017;23(2):144–174. doi: 10.1111/spsr.12242. [DOI] [Google Scholar]
- 42.Channa A, Faguet JP. Decentralisation of health and education in developing countries: a quality-adjusted review of the empirical literature. World Bank Res. Obs. 2016;31(2):199–241. doi: 10.1093/wbro/lkw001. [DOI] [Google Scholar]
- 43.Jimenez D, Smith PC. Decentralisation of health care and its impact on health outcomes. 2005. Discussion Papers in Economics, Department of Economics and Related Studies. York: University of York; 2005. [Google Scholar]
- 44.Saltman RB, Vrangbaek K, Lehto J, Winblad U. Consolidating national authority in Nordic health systems. Eurohealth. 2012;18(3):21–24. [Google Scholar]
- 45.James C, Beazley I, Penn I, Philips L, Dougherty S. Decentralisation in the health sector and responsibilities across levels of government: Impact on spending decisions and the budget. OECD J. Budg. 2019 doi: 10.1787/045f5902-en. [DOI] [Google Scholar]
- 46.Jong D, Tsvetkova A, Lembcke AC, Ahrend R. A comprehensive approach to understanding urban productivity effects of local governments: local autonomy, government quality and fragmentation. OECD regional development papers, no. 11. Paris: OECD Publishing; 2021. [Google Scholar]
- 47.OECD: COVID-19 and fiscal relations across levels of government. Tackling Coronavirus (COVID-19) (2020). https://oe.cd/il/COVID-FF. Accessed 16 Mar 2021
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Available upon request.
Available upon request.