Abstract
Objectives
Investigate factors associated with the intention to have the COVID-19 vaccination following initiation of the UK national vaccination programme.
Study design
An online cross-sectional survey completed by 1500 adults (13th–15th January 2021).
Methods
Linear regression analyses were used to investigate associations between intention to be vaccinated for COVID-19 and sociodemographic factors, previous influenza vaccination, attitudes and beliefs about COVID-19 and COVID-19 vaccination and vaccination in general. Participants’ main reasons for likely vaccination (non-)uptake were also solicited.
Results
73.5% of participants (95% CI 71.2%, 75.7%) reported being likely to be vaccinated against COVID-19, 17.3% (95% CI 15.4%, 19.3%) were unsure, and 9.3% (95% CI 7.9%, 10.8%) reported being unlikely to be vaccinated. The full regression model explained 69.8% of the variance in intention. Intention was associated with: having been/intending to be vaccinated for influenza last winter/this winter; stronger beliefs about social acceptability of a COVID-19 vaccine; the perceived need for vaccination; adequacy of information about the vaccine; and weaker beliefs that the vaccine is unsafe. Beliefs that only those at serious risk of illness should be vaccinated and that the vaccines are just a means for manufacturers to make money were negatively associated with vaccination intention.
Conclusions
Most participants reported being likely to get the COVID-19 vaccination. COVID-19 vaccination attitudes and beliefs are a crucial factor underpinning vaccine intention. Continued engagement with the public with a focus on the importance and safety of vaccination is recommended.
Keywords: Hesitancy, Side effects, Beliefs, Attitudes, Barriers, Covid-19 vaccines
Introduction
One year on from the emergence of COVID-19 in China in December 2019, there have been more than 112 million cases of COVID-19 and nearly 2.5 million deaths worldwide.1 While countries have implemented a variety of public health measures to try to prevent the spread of the virus, scientists across the world have worked on developing effective vaccines. On 2nd December 2020, the United Kingdom (UK) became the first country to approve a COVID-19 vaccine that had been through a large-scale trial,2 and on 8th December, the first dose of the Pfizer/BioNTech vaccine was administered.3 This was swiftly followed by UK approval of the Oxford/AstraZeneca vaccine on 30th December 2020 and the Moderna vaccine on 8th January 2021. Given the severity of the pandemic and associated clinical outcomes, it is imperative that COVID-19 vaccination uptake is maximised so that, alongside ongoing protective public health practices, the spread of infection can be reduced.4 To achieve this, we need to understand the factors that affect people's willingness to have a vaccine.
The existing peer-reviewed research exploring the acceptability of a COVID-19 vaccination was all conducted before a vaccine was available,5, 6, 7, 8 when details about the actual vaccine were still a matter of speculation. For example, in a survey of 1500 UK adults that we conducted in July 2020,5 64% of participants reported being very likely to be vaccinated against COVID-19, 27% were unsure, and 9% reported being very unlikely to be vaccinated. Intention to be vaccinated was associated with: more positive general COVID-19 vaccination beliefs and attitudes; weaker beliefs that the vaccination would cause side effects or be unsafe; greater perceived information sufficiency to make an informed decision about COVID-19 vaccination; greater perceived risk of COVID-19 to others; older age; and having been vaccinated for influenza the previous year. Studies conducted before a vaccine was available provided useful data with which to start planning communication strategies about vaccine rollout. With national vaccination programmes currently underway internationally, further research is needed to understand how COVID-19 vaccine acceptance and factors affecting acceptance might have changed now that vaccination has materialised.
Contextual factors such as news stories and media coverage also influence vaccine acceptance.9 The approval of the COVID-19 vaccines and the rollout of the vaccination programme has been accompanied by considerable press reporting of the differences between the vaccines, including the type of technology used (mRNA vs viral vector10), speculation about levels of efficacy observed in clinical trials, and potential variation of effectiveness in a public health context.11 There was coverage related to two doctors in the United Kingdom who had an allergic reaction to the vaccine12 and some controversy over the deviation from prior clinical trial administration of the required 2 doses of each vaccine 3 weeks apart so that they were administered 12 weeks apart,13 as well as the potential to mix vaccine types.14 These issues may also have influenced COVID-19 vaccine acceptance.
The aim of this study was to investigate associations between COVID-19 vaccination intention and sociodemographic, psychological, and contextual factors in a demographically representative sample of the UK adult population at the start of the COVID-19 vaccination programme rollout.
Methods
Design
We conducted an online cross-sectional survey (13th to 15th January 2021) hosted on Qualtrics.
Participants
Participants (n = 1500) were recruited through Prolific's online research panel and were eligible for the study if they were aged eighteen years or over, lived in the United Kingdom, and had not completed our previous survey5 (n > 31,000 eligible participants). Prolific set quotas based on UK census data to ensure respondents were broadly representative of the UK population in terms of age, sex and ethnicity. Of 1508 people who began the survey, 1503 completed it (99.7% completion rate). Three participants were excluded from the sample as they did not meet quality control checks (specifically, they failed to correctly answer two or more of three attention check questions). Participants were paid £2 for a completed survey.
Measures
Full survey materials are available online.15 Most items were the same as those in the UK survey reported above,5 which was conducted in July 2020 and consisted of items that were based on previous literature.16, 17, 18, 19, 20 Some further items were added, and some removed or amended to reflect the availability of specific COVID vaccinations and the timing of the survey.
Personal and clinical characteristics
We asked participants to report their age, gender, ethnicity, religion, highest educational or professional qualifications, current working situation, and total household income. We also asked participants what UK region they lived in, how many people lived in their household, whether they or someone else in their household (if applicable) had a long-standing illness, disability or infirmity and, if so, whether they had received a letter from the NHS recommending that they took extra precautions against coronavirus (‘shielding’) or whether they had a chronic illness that made them clinically vulnerable to serious illness from COVID-19. We also asked whether they or anyone they lived with were classified as obese or were pregnant and if they worked or volunteered in roles considered critical to the COVID-19 response (‘key worker’ roles).
Last, we asked participants whether they had been vaccinated for seasonal influenza last winter and/or had (or intended to be) this winter (yes/no).
Psychological and contextual factors
Participants were asked to what extent they thought ‘coronavirus poses a risk to’ people in the United Kingdom and to themselves personally, on a five-point scale, from ‘no risk at all’ to ‘major risk’. They were asked if they thought they ‘have had, or currently have, coronavirus’. Participants could answer ‘I have definitely had it or definitely have it now’, ‘I have probably had it or probably have it now’, ‘I have probably not had it and probably don't have it now’, and ‘I have definitely not had it and definitely don't have it now’. They were also asked if they personally knew anyone who had had COVID-19 (yes/no).
Further, we asked participants a series of eight questions about their attitudes towards COVID-19. They were asked whether, as far as they knew, they were in one of the groups that had so far been offered the vaccine. Participants were then asked if they had been vaccinated (yes, I've had one/two doses/no), and if they answered yes, they were asked which vaccine they had received (Pfizer-BioNTech/Oxford University-AstraZeneca). All participants were then asked 21 questions about COVID-19 vaccination. Statements measured theoretical constructs, including perceived susceptibility to COVID-19, the severity of COVID-19, benefits of a COVID-19 vaccine, barriers to being vaccinated against COVID-19, ability to be vaccinated (self-efficacy), subjective norms, behavioural control, anticipated regret, knowledge, trust in the Government, and trust in the NHS. These items also investigated concerns about commercial profiteering and participants' beliefs about vaccination allowing life to get back to ‘normal’ and having to follow social distancing and other restrictions for COVID-19 if vaccinated. Participants rated the statements on an eleven-point scale (0–10) from ‘strongly disagree’ to ‘strongly agree’. We adjusted the wording to make the grammatical tense either retrospective for those who had received the vaccine or prospective for those who had not. Participants who had not yet received a vaccine were additionally asked how likely they thought it was that they would get side effects from a coronavirus vaccine. We also asked participants if the coronavirus vaccination had been recommended to them by a health care professional and whether their employer did/would want them to have the COVID-19 vaccination. The order of items was quasi-randomised.
Outcome measure
To measure vaccination intention, we asked participants who had not yet been vaccinated to state how likely they would be to have a COVID-19 vaccination ‘now that a coronavirus vaccination is available’ on an eleven-point scale from ‘extremely unlikely’ (0) to ‘extremely likely’ (10).
We additionally asked participants to report the main reason why they were likely or unlikely to have a coronavirus vaccination in an open-text comment box.
Ethics
Ethical approval for this study was granted by Keele University's Research Ethics Committee (reference: PS-200129).
Sample size
A target sample size of 1500 was chosen to provide a high ratio of cases to estimated parameters in order to avoid overfitting and loss of generalisability in the regression model.21
Analysis
To identify variables associated with an intention to have the COVID-19 vaccination in those who had not yet been vaccinated, we constructed a linear regression model. Ordinal and multinomial predictors were converted to dummy variables. To aid interpretation of the model and to achieve a more parsimonious set of predictor variables, we ran principal component analyses22 on items investigating beliefs and attitudes about a) COVID-19 and b) COVID-19 vaccination. This resulted in a smaller number of new variables (components) that are linear combinations of the original items and represent different latent dimensions that underlie these items. The components were generated separately for the items relating to COVID-19 as an illness and those relating to COVID-19 vaccination, and the components were named in accordance with the items that loaded most heavily upon them.
Variables entered into the regression model were selected a priori based on their theoretical relevance; no variable selection procedures were employed. Five groups of variables were included in the model: personal and clinical characteristics; seasonal influenza vaccination; general beliefs and attitudes relating to vaccination; beliefs and attitudes relating to COVID-19 illness; and beliefs and attitudes relating to COVID-19 vaccination. The percentage of variance in the outcome variable explained by each predictor was calculated as the squared semipartial correlation for a numerical or binary predictor and the change in R 2 attributable to a set of dummy variables.
As well as fitting the full model, we also added the groups of variables as successive blocks in a hierarchical model to determine the incremental increase in the adjusted R 2 value as these groups of variables were added to the model.
Due to the large number of predictors in the model, statistical significance was set at P ≤ .01 to control Type 1 errors, and 99% confidence intervals (CIs) were correspondingly calculated for the regression coefficients. Assumptions of the analysis were checked. Analyses were conducted in SPSS 26.
To analyse open-ended responses for reasons why participants were likely or unlikely to have a coronavirus vaccination, we conducted a content analysis using an emergent coding approach, whereby codes were identified from the data rather than a priori.23 Two authors (MC and HD) jointly coded a small sample of statements to understand the scope of the data. They then each independently coded sufficient responses that they achieved a run of 15 statements without encountering any new codes. At this point, they compared the codes they had generated and discussed any discrepancies. They then independently applied these codes to the rest of the statements, after which they checked that they had applied the same codes across the statements and discussed and resolved any additional codes and any discrepancies. This process was first applied to those participants who were uncertain about whether they would have the vaccine, then to those who were unlikely to have it, and finally to those participants who were likely to have it.
Results
Participants were broadly representative of the UK population (mean age 45.6 years, SD = 15.6, range 18–86; 51% female; 85% white ethnicity; Table 1 , see Supplementary Materials 1 for further breakdown). At the time of completing the survey, only 30 respondents had received one or both doses of a coronavirus vaccine.
Table 1.
Participant characteristics.
| Personal and clinical characteristics | Level | n (%) |
|---|---|---|
| Sex | Male | 728 (48.5) |
| Female | 765 (51.0) | |
| Other | 6 (.1) | |
| Prefer not to say | 1 (.1) | |
| Ethnicity | White | 1269 (84.6) |
| Black and minority ethnic | 224 (14.9) | |
| Prefer not to say | 7 (.5) | |
| Religion | No religion | 793 (52.9) |
| Christian | 571 (38.1) | |
| Other religion | 114 (7.5) | |
| Prefer not to say | 22 (1.5) | |
| Highest qualification | Degree equivalent or higherc | 817 (54.5) |
| Other or no qualifications | 677 (45.1) | |
| Prefer not to say | 6 (.4) | |
| Employment status | Full-time | 649 (43.3) |
| Part-time | 269 (17.9) | |
| Not working/other | 572 (38.1) | |
| Don't know | 1 (.1) | |
| Prefer not to say | 9 (.6) | |
| Key worker | Yes | 500 (33.3) |
| No | 1000 (66.7) | |
| Total household incomea | Under £10,000 | 94 (6.3) |
| £10,000–£19,999 | 215 (14.3) | |
| £20,000–£29,999 | 249 (16.6) | |
| £30,000–£39,999b | 236 (15.7) | |
| £40,000–£49,999 | 179 (11.9) | |
| £50,000–£74,999 | 261 (17.4) | |
| £75,000 or over | 161 (10.7) | |
| Don't know | 18 (1.2) | |
| Prefer not to say | 87 (5.8) | |
| Region where respondent livesa | East Midlands | 127 (8.5) |
| East of England | 111 (7.4) | |
| London | 205 (13.7) | |
| North East | 61 (4.1) | |
| North West | 176 (11.7) | |
| Northern Ireland | 27 (1.8) | |
| Scotland | 116 (7.7) | |
| South East | 239 (15.9) | |
| South West | 131 (8.7) | |
| Wales | 56 (3.7) | |
| West Midlands | 122 (8.1) | |
| Yorkshire and the Humber | 127 (8.5) | |
| Prefer not to say | 2 (.1) | |
| Number of people in householda | 1 | 233 (15.5) |
| 2b | 587 (39.1) | |
| 3–4 | 563 (37.5) | |
| 5–6 | 105 (7.0) | |
| 7 or more | 9 (.6) | |
| Prefer not to say | 3 (.2) | |
| Extremely clinically vulnerable – respondent | Yes | 344 (22.9) |
| No | 1156 (77.1) | |
| Extremely clinically vulnerable – other(s) in household | Yes | 254 (16.9) |
| No | 1010 (67.4) | |
| Not applicable/prefer not to say | 236 (15.7) | |
| Influenza vaccination last winterd | Yes | 457 (30.5) |
| No | 1040 (69.3) | |
| Don't know | 1 (.1) | |
| Prefer not to say | 2 (.1) | |
| Influenza vaccine this winterd | Yes | 581 (38.7) |
| No, but intend to | 180 (12.0) | |
| No, and don't intend to | 723 (48.2) | |
| Don't know | 13 (.9) | |
| Prefer not to say | 3 (.2) |
Not included in regression model.
Median category.
Undergraduate (e.g. BA, BSc) or postgraduate (e.g. MA, MSc, PhD) degree or other technical, professional or higher qualification.
Combined into a single variable in the regression model.
Descriptive statistics for items assessing psychological factors are reported in Table 2, Table 3 . These tables show that participants were worried about catching coronavirus and did not believe that it would be a mild illness for them. Approximately three-quarters of participants (76.7%) believed COVID-19 posed a moderate or higher risk to them personally. It was also noteworthy that participants reported considerably more trust in the NHS compared to the Government regarding managing the pandemic.
Table 2.
Descriptive statistics for continuous items measuring beliefs and attitudes about COVID-19 and a COVID-19 vaccination and vaccination intention. Data are mean (standard deviation) on a 0–10 numerical rating scale (0 = strongly disagree, 10 = strongly agree), except where indicated. Also shown is the principal component (as numbered in Table 4) on which the items loaded most, for those items included in the principal components analysis (see Supplementary Materials 2).
| Item | Mean (SD) | Related principal componentb | |
|---|---|---|---|
| Attitudes and beliefs about COVID-19 | I am worried about catching coronavirus | 6.51 (2.82) | 2 |
| I believe that coronavirus would be a mild illness for me | 4.44 (2.73) | 2 | |
| Too much fuss is being made about the risk of coronavirusa | 2.01 (2.63) | 1 | |
| We are all responsible for reducing the spread of coronavirusa | 9.23 (1.59) | 1 | |
| I believe I am immune to coronavirusa | 1.06 (1.91) | 1 | |
| The coronavirus pandemic has had a big impact on my life | 7.51 (2.33) | 4 | |
| I trust the NHS to manage the coronavirus pandemic in the UK | 7.39 (2.21) | 3 | |
| I trust the Government to manage the coronavirus pandemic in the UK | 3.99 (2.98) | 3 | |
| Attitudes and beliefs about a COVID-19 vaccination | How likely do you think it is that you would get side effects from a coronavirus vaccination (0 = very unlikely, 10 = very likely) | 4.01 (2.45) | – |
| A coronavirus vaccination should be mandatory for everyone who is able to have it | 6.27 (3.60) | 6 | |
| Without a coronavirus vaccination, I am likely to catch coronavirus | 6.45 (2.44) | 6 | |
| Two doses of coronavirus vaccination will protect me against coronavirus | 7.52 (2.22) | 1 | |
| If I don't get the coronavirus vaccination and end up getting coronavirus, I will regret not getting the vaccinationa | 7.92 (3.04) | 6 | |
| It would be very easy for me to have a coronavirus vaccinationa | 7.81 (2.51) | 1 | |
| The coronavirus vaccination could give me coronavirus | 1.59 (2.17) | 7 | |
| The way the coronavirus vaccines are being given in the UK goes against the manufacturers’ recommendations | 4.89 (2.99) | – | |
| I might regret getting the coronavirus vaccination if I later experienced side effects from it | 4.42 (3.18) | 7 | |
| The coronavirus vaccination is too new for me to be confident about getting vaccinated | 4.05 (3.28) | 7 | |
| Most people will get a coronavirus vaccination | 7.46 (1.75) | 5 | |
| Other people like me will get a coronavirus vaccinationa | 7.94 (2.20) | 5 | |
| In general, vaccination is a good thinga | 9.02 (1.72) | – | |
| I am afraid of needlesa | 2.77 (3.31) | – | |
| If I were vaccinated, I think I would not need to follow social distancing and other restrictions for coronavirus | 2.60 (2.82) | 9 | |
| I know enough about the coronavirus illness to make an informed decision about whether or not to get vaccinated | 7.73 (2.45) | 8 | |
| I know enough about the coronavirus vaccine to make an informed decision about whether or not to get vaccinated | 6.79 (2.67) | 8 | |
| Only people who are at risk of serious illness from coronavirus need to be vaccinated | 2.39 (3.04) | – | |
| My family would approve of my having a coronavirus vaccinationa | 8.58 (2.16) | 5 | |
| My friends would approve of my having a coronavirus vaccinationa | 8.33 (2.09) | 5 | |
| Widespread coronavirus vaccination is just a way to make money for vaccine manufacturersa | 2.05 (2.62) | – | |
| The coronavirus vaccine will allow us to get back to ‘normal’ | 7.24 (2.32) | 5 | |
| Vaccination intention | Now that a coronavirus vaccination is available, how likely is it you will have one? (0 = very unlikely, 10 = very likely)a | 8.13 (2.96) | – |
Skewed variables; mean values should be interpreted cautiously.
1 = perceived severity of COVID-19; 2 = individual vulnerability to COVID-19; 3 = trust in COVID-19 management; 4 = impact of COVID-19 on one's life; 5 = social norms; 6 = the necessity of vaccination; 7 = safety of the vaccine; 8 = adequacy of information about the vaccine; 9 = freedom from restrictions through the vaccine.
Table 3.
Descriptive statistics for categorical and ordinal items measuring beliefs, attitudes and behaviour relating to COVID-19 and a COVID-19 vaccination.
| Item | Level | n (%) |
|---|---|---|
| To what extent do you think coronavirus poses a risk to people in the UK? | No risk at all | 6 (.4) |
| Minor risk | 69 (4.6) | |
| Moderate risk | 197 (13.1) | |
| Significant risk | 568 (37.9) | |
| Major risk | 659 (43.9) | |
| Don't know | 1 (.1) | |
| To what extent do you think coronavirus poses a risk to you personally? | No risk at all | 37 (2.5) |
| Minor risk | 306 (20.4) | |
| Moderate risk | 539 (35.9) | |
| Significant risk | 424 (28.3) | |
| Major risk | 187 (12.5) | |
| Don't know | 7 (.5) | |
| Do you believe you have had, or currently have, coronavirus? | Definitely not | 460 (30.7) |
| Probably not | 621 (41.4) | |
| Probably | 164 (10.9) | |
| Definitely | 79 (5.3) | |
| Don't know | 175 (11.7) | |
| Prefer not to say | 1 (.1) | |
| Do you personally know anyone (excluding yourself) who has had coronavirus? | Yes | 1153 (76.9) |
| No | 336 (22.4) | |
| Don't know | 10 (.7) | |
| Prefer not to say | 1 (.1) | |
| As far as you know, would your employer want you to have the coronavirus vaccination? | Yes | 572 (60.6) |
| No | 59 (6.3) | |
| Don't know | 313 (33.2) | |
| Not applicable | 556 |
Principal component analyses
Four components emerged from the principal component analysis on beliefs and attitudes about COVID-19, accounting for 75% of the variance in original items, and five components emerged from the principal component analysis investigating items related to a COVID-19 vaccination, accounting for 68% of the variance in the original items (see Supplementary Materials 2).
Vaccination intention
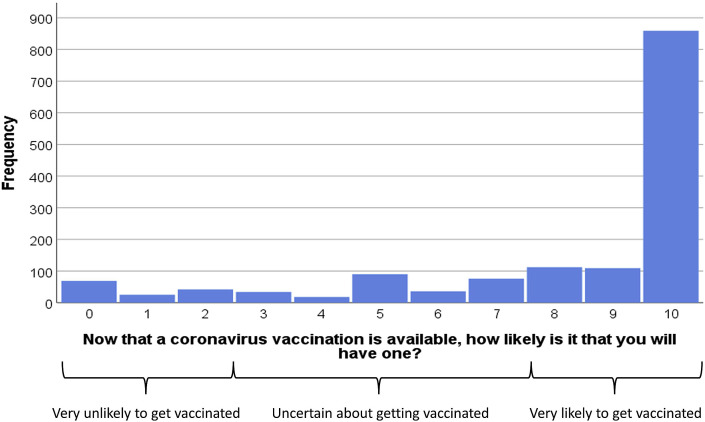
Participants' vaccination intention (in participants who had not already received one or both doses) is presented in Fig. 1 . Vaccination intention exhibited a marked negative skew (mean = 8.13, standard deviation = 2.96, median = 10.00). In order to categorise respondents in terms of their vaccination intention, we applied a priori cut-points to the 0–10 scale (with scores of zero to two as ‘very unlikely’, three to seven as ‘uncertain’ and eight to ten as ‘very likely’, as per our July 2020 survey [5]). On this basis, 9.3% (95% CI 7.9%, 10.8%) reported being very unlikely to be vaccinated (n = 136), 17.3% (95% CI 15.4%, 19.3%) reported being uncertain about their likelihood of vaccination (n = 254), and 73.5% (95% CI 71.2%, 75.7%) reported being very likely to be vaccinated (n = 1080).
Fig. 1.
Perceived likelihood of having a vaccination (0 = ‘extremely unlikely’ to 10 = ‘extremely likely’). The figure also shows cut-points that we used to categorise respondents in terms of their vaccination intention.
The final model explained 69.8% of the variance in intention to vaccinate (Table 4). Increased likelihood of being vaccinated for COVID-19 was significantly associated with having been vaccinated for influenza last or this winter (or intending to do so this winter), and with all of the components derived from the items relating to COVID-19 vaccination, other than ‘freedom from restrictions through the vaccine’. Vaccination intention also showed a significant negative association with beliefs that only people who are at risk of serious illness from coronavirus need to be vaccinated and that widespread coronavirus vaccination is just a way to make money for vaccine manufacturers.
Table 4.
Results of the full linear regression model analysing associations with vaccination intention (adjusted R2 = .698). Parameter estimates relate to the full model containing all predictors. The unstandardised regression coefficients represent the change in likelihood of vaccination for a one-unit increase in the predictor variable (or, for dummy variables, a shift from the reference category to the category concerned). The figures under ‘% variance explained’ represent the percentage of variance in the outcome variable uniquely explained by the item (or set of dummy variables) concerned. The model was based on 1401 cases with complete data.
| Predictor variable | Level | Standardised coefficient | Unstandardised coefficient | 99% confidence interval | P value | % variance explained |
|---|---|---|---|---|---|---|
| Block 1 – personal and clinical characteristics | ||||||
| Age | Years | .046 | .008 | –.001, .018 | .023 | .11 |
| Sex (reference: female) | Male | –.024 | –.135 | –.364, .094 | .129 | .05 |
| Ethnicity (reference: black and minority ethnic) | White | –.002 | –.016 | –.378, .346 | .907 | <.01 |
| Religion (reference: none) | .935 | <.01 | ||||
| Christian | .000 | .003 | –.249, .255 | |||
| Other | .006 | .068 | –.414, .549 | |||
| Qualifications (reference: other) | Degree equivalent or higher | .028 | .162 | –.070, .393 | .066 | .07 |
| Employment status (reference: not working/other) | .336 | .05 | ||||
| Part-time | .014 | .105 | –.236, .446 | |||
| Full-time | –.014 | –.080 | –.356, .197 | |||
| Key worker (reference: not key worker) | Key worker | –.003 | –.018 | –.280, .245 | .863 | <.01 |
| Extremely clinically vulnerable – self (reference: no) | Yes | –.023 | –.155 | –.444, .134 | .166 | .04 |
| Extremely clinically vulnerable – household member (reference: no) |
Yes |
–.022 |
–.173 |
–.474, .129 |
.140 |
.05 |
| Block 2 – previous influenza vaccination | ||||||
| Did you/will you have a vaccination for influenza last/this winter? (reference: no) |
Yes |
.047 |
.270 |
.012, .528 |
.007a |
.14 |
| Block 3 – general vaccination beliefs and attitudes | ||||||
| Vaccination is generally good (0–10) | 0–10 scale | .011 | .018 | –.079, .116 | .627 | .01 |
| I am afraid of needles (0–10) |
0–10 scale |
.016 |
.014 |
–.021, .049 |
.295 |
.02 |
| Block 4 – beliefs and attitudes about COVID-19 | ||||||
| Perceived risk of COVID-19 to people in the UK (reference: major) | .822 | .02 | ||||
| None/minor | –.012 | –.166 | –.897, .565 | |||
| Moderate | .007 | .063 | –.380, .507 | |||
| Significant | .002 | .015 | –.261, .290 | |||
| Perceived risk of COVID-19 to oneself (reference: major) | .021 | .21 | ||||
| None/minor | .059 | .407 | –.190, 1.005 | |||
| Moderate | .082 | .493 | .036, .951 | |||
| Significant | .067 | .429 | .034, .824 | |||
| Do you have/have you had COVID-19? (reference: probably/definitely) | .288 | .08 | ||||
| Probably not | .028 | .163 | –.180, .586 | |||
| Definitely not | –.002 | –.010 | –.375, .355 | |||
| Don't know | .018 | .164 | –.283, .610 | |||
| Do you know anybody who has had COVID-19? (reference: no) | Yes | .005 | .032 | –.246, .310 | .764 | .02 |
| Component 1: perceived severity of COVID-19 | –.028 | –.083 | –.257, .091 | .219 | .03 | |
| Component 2: individual vulnerability to COVID-19 | –.045 | –.130 | –.308, .048 | .060 | .08 | |
| Component 3: trust in COVID-19 management | –.005 | –.015 | –.144, .114 | .766 | <.01 | |
| Component 4: impact of COVID-19 on one's life |
–.011 |
–.031 |
–.156, .093 |
.513 |
.01 |
|
| Block 5 – beliefs and attitudes about COVID-19 vaccination | ||||||
| Component 5: social norms | .378 | 1.106 | .954, 1.259 | <.001a | 7.55 | |
| Component 6: the necessity of vaccination | .460 | 1.329 | 1.172, 1.487 | <.001a | 10.20 | |
| Component 7: safety of the vaccine | .370 | 1.068 | .923, 1.212 | <.001a | 7.83 | |
| Component 8: adequacy of information about the vaccine | .148 | .431 | .308, .554 | <.001a | 1.76 | |
| Component 9: freedom from restrictions through the vaccine | .015 | .043 | –.077, .164 | .353 | .02 | |
| The way the coronavirus vaccines are being given in the UK goes against the manufacturers’ recommendations | .005 | .005 | –.035, .045 | .751 | <.01 | |
| Only people who are at risk of serious illness from coronavirus need to be vaccinated | 0–10 scale | –.064 | –.061 | –.106, −.016 | .001a | .26 |
| Widespread coronavirus vaccination is just a way to make money for vaccine manufacturers | 0–10 scale | –.060 | –.067 | –.128, −.006 | .004a | .18 |
p ≤ .01.
The principal component that related to the necessity of vaccination explained more variance in vaccination intention than any other predictor in the statistical model, followed by the principal components concerning social acceptance and safety of the vaccine. Other significant predictors only explained small percentages of variance.
When the groups of variables were entered hierarchically as blocks, we could infer the percentage of additional variance explained by each block from the change in incremental adjusted R 2. Personal and clinical characteristics (block 1) alone explained very little (8.8%) of the variance in intention to be vaccinated. When previous influenza vaccination (block 2) was added, it explained an additional 6.4% of the variance. Adding general vaccination beliefs and attitudes (block 3) resulted in the largest increase in percentage (25.1%) of explained variance (although in the full model, the predictors in this group were no longer significant). When beliefs and attitudes about COVID-19 (block 4) were added to the model, they explained 6.5% more of the variance in vaccination intention. Adding positive beliefs and attitudes about a COVID-19 vaccination (block 5) explained a further 23.0% of the variance. Each block explained a statistically significant percentage of the variance (P < .001 in each case).
Content analysis
Of the 1470 participants who had not yet received a vaccine and were asked to give a reason for the score provided on the likelihood of having the vaccination question, 1461 participants (99.4%) provided a response. Answers ranged from one word to 455 words (mean = 20.3, SD = 20.6). The content analysis generated 102 unique codes. The codes were then further organised into themes, and these, along with a frequency count of comments per theme, are presented in Table 5 . A breakdown of codes and themes is provided in Supplementary Materials 3.
Table 5.
Thematic categorisation of codes generated by content analysis of reasons for likelihood of having, or not having, the COVID-19 vaccination, including a breakdown by likelihood of having the vaccination (likely, uncertain, likely). Themes are presented in descending order of overall frequency.
| Theme name | Illustrative code | Number of comments per theme (likely, uncertain, unlikely) |
|---|---|---|
| Self-protection (including health reasons) | Perceived high personal risk of disease severity | 675 (651, 22, 2)a |
| To protect others | Protecting the wider community | 667 (609, 54, 4)a |
| To end the pandemic and its negative impacts | To end lockdown | 345 (331, 14, 0)a |
| Confidence in vaccine and authority | The vaccine is effective | 317 (276, 39, 2)a |
| Safety concerns about the COVID-19 vaccine | Concerns re quick development of the vaccine | 226 (28, 110, 88)b |
| Concerns re details of vaccine (other than safety) | Concerns re dose time scale | 173 (22, 89, 62)b |
| Low risk/no personal need for vaccine | Only high-risk groups need the vaccine | 144 (25, 75, 44)b |
| Concern about health effects of COVID-19 | Concerns re long term side effects of virus | 77 (71, 6, 0)a |
| Other (miscellaneous) | Currently no access due to visa status | 67 (46, 13, 8)a |
| Precontemplation/not made decision | Not offered yet | 64 (12, 44, 8)b |
| Unspecified concerns about COVID-19 vaccine | Anxiety re the vaccine | 62 (0, 24, 38)b |
| To travel/move around more freely | Wanting to visit family | 55 (42, 13, 0)a |
| Specific health concerns about the COVID-19 vaccine | Fertility concerns | 39 (5, 19, 15)b |
| Avoid/delay having the vaccine by waiting | Wanting others to test it first | 36 (5, 25, 6)b |
| Lack of trust in authority | Lack of trust in media transparency | 33 (7, 7, 19)b |
| General vaccine concerns | Fear of needles | 30 (4, 8, 18)b |
Comments were made more frequently by those who were likely to vaccinate.
Comments were made more frequently by those who were uncertain or unlikely to vaccinate.
The two most frequently cited reasons to support the score participants gave on the likelihood question related to protecting themselves or others. These were primarily the reasons given by participants who indicated they were likely to have the vaccine. In comparison, the most frequently provided reasons provided by participants who were uncertain or unlikely to have the vaccine were related to safety concerns about the COVID-19 vaccine.
Discussion
The UK government has set a target of offering the first dose of a COVID-19 vaccine to all adults in the United Kingdom by the end of July 2021.24 In this study conducted in January 2021, three-quarters of participants reported being very likely to have the vaccination. This is higher than the 64% who reported being very likely to have the vaccination in our study conducted in July 20205 and is consistent with increases in vaccination intention reported elsewhere. For example, in a recent (March 2021) YouGov poll in the UK, 86% of respondents had either already been vaccinated or reported that they would get the vaccine.25 Despite the relatively high intention reported in our study and recent polling, we cannot be complacent about uptake. News stories are emerging almost every week about different variants of the virus, as well as issues around differential uptake of individual vaccines across the world,26 and it is important to understand the factors associated with intention in order to maximise uptake and offset any adverse media reporting, social media misinformation, and the like.
Our results indicate that greater intention to have the COVID-19 vaccination was associated with having been vaccinated for influenza last or this winter or intending to be this winter. This is consistent with our previous findings,5 as well as with findings from the US27 and Europe.28 However, several of the COVID-19 vaccination beliefs and attitudes explained a more substantial proportion of the variance in vaccination intention. Intention was associated with greater perceived social norms around COVID-19 vaccination and the greater perceived necessity of vaccination. These items map onto theoretical constructs that have previously been shown to influence the adoption of health behaviours: subjective norms and perceived susceptibility.5 Previous studies exploring vaccine intentions have also found high levels of positive social norms favouring the vaccine29 and that intention is associated with increased levels of concern related to the risks of the disease.28 , 30 We also found that lower intention was associated with reduced belief in the safety of the vaccine, and this has been found consistently across studies exploring COVID-19 vaccine intentions7 , 8 and vaccine hesitancy.8 This was also reflected in the content analysis of participants’ open-ended responses, in which issues related to vaccine safety were the most frequently identified reason for lower vaccination intention in the participants we classified as uncertain or very unlikely to have the vaccine. This is also consistent with the free-text responses given in an English study exploring vaccine acceptability conducted April to May 2020.7 Since there was less than a year between the genetic code of COVID-19 being made public and the first COVID-19 vaccine being approved, this belief is perhaps unsurprising. However, it does make it essential that there is sufficient engagement with the public's concerns and that good-quality and credible information continues to be made available about the vaccine. This recommendation is reinforced by the association in our data of perceived adequacy of information about the vaccine to facilitate an informed decision with vaccination intention. Since free-text responses related to safety were the most frequent category of response from uncertain responders, it is likely that any reporting of safety concerns in the media may well shift the balance in favour of not being vaccinated, as has been observed previously.31 The WHO guideline for emergency risk communication makes the strong recommendation that ‘Communication by authorities to the public should include explicit information about uncertainties associated with risks, events and interventions, and indicate what is known and not known at a given time.’32 However, it is imperative that halting the rollout of the vaccination programme because of unproven risks, as seen in some European countries in March 2021,26 should be avoided, as this is likely to damage uptake once vaccination is restarted.
Vaccination intention in our study was also associated with a weaker belief that only people who are at risk of serious illness from coronavirus need to be vaccinated, and free-text responses associated with protecting others were frequently given to explain intention to have the vaccine. Statements about protecting others were only second in the content analysis to those relating to self-protection, such as a perceived high personal risk of disease severity, and this is consistent with previous research on COVID-19 vaccine intentions.7 Since those individuals who are less likely to vaccinate believe that only those at risk need to be vaccinated, and those who are more likely to vaccinate favour protecting others, as well as themselves, it may be that messaging needs to be tailored to accommodate the possibility that emphasising the community benefits of vaccination may not motivate hesitant individuals.
Several previous studies have found that various sociodemographic factors are associated with COVID-19 vaccine intention, such as age,5 , 30 gender28 , 33 and ethnicity.7 , 33 We did not find this in our study, and it is not entirely clear why that might be. The lack of impact of ethnicity on intention is perhaps the most striking absence, given both previous research and evidence from actual uptake in the United Kingdom, which shows that a significantly smaller proportion of ethnic minorities compared to white health care workers have had the COVID-19 vaccine.34 We recruited a demographically representative sample based on age, gender and ethnicity. However, the relatively low number of participants from ethnic minority backgrounds necessitated collapsing our data across these categories, which may explain why ethnicity was not associated with intention in our study. The lack of an association with age is also unexpected, especially since by 19th September 2021, 73.9% of 18–24-year-olds had had at least one dose of the vaccine compared to 98.3% of 75–79-year-olds.35 The age difference in actual uptake may in part be due to the way the vaccine was rolled out to the population, with the vaccine being distributed first to older age groups (25–29-year-olds first invited 6 months after distribution to residents in care homes and those aged 80 years and over).36 The percentage of participants in our sample who indicated they were very likely to have the vaccine (73.5%) was lower than the percentage of the UK population who actually did (89.0% had had one dose and 82.9% had two doses by 19th September 202135). This may reflect the fact that our study was conducted when the vaccine was first rolled out and was not yet available to most of our participants. As the rollout gathered pace, subjective norms and perceived susceptibility, both of which are shown to be important determinants of vaccine willingness in our study, may well have increased for older adults, with high uptake fuelling subjective norms and the disparity in reported health outcomes for vaccinated versus unvaccinated adults fuelling perceived susceptibility. Furthermore, the UK government and NHS have been proactive in providing mass vaccination centres, invitations, reminders, and messaging. A recent study found that younger adults in the UK demonstrated more vaccine hesitancy and resistance than older adults,37 which may have prevented the same inflation in uptake relative to the reported likelihood that we have seen in older adults. Studies using appropriate sampling techniques are required to capture and quantify uptake and associated attitudinal differences across different population cohorts. As the vaccination is made available to all those who want it, future research could also usefully focus on those who are uncertain or unlikely to be vaccinated.
Our regression model explained 70% of the variance in vaccination intention, similar to the figure of 76% in our previous study5; the remaining unexplained variance will represent predictors that we did not measure and random measurement error. Given that social science research in general,38 and public opinion surveys in particular,39 do not characteristically yield high R 2 values owing to the likely multiple and complex determinants of individuals' beliefs and attitudes, we believe that our model demonstrates good explanatory power.
Finally, the intention to have the COVID-19 vaccine was associated with a weaker belief that widespread coronavirus vaccination is just a way to make money for vaccine manufacturers. This is consistent with research from Hong Kong,40 in which higher levels of trust in the vaccine manufacturer were associated with increased willingness to have the COVID-19 vaccine.
Limitations of this study include that we measured self-reported intention rather than actual uptake. Intention is usually higher than uptake; however, vaccine intention predicts vaccine uptake and so acts as a useful proxy in the early stages of vaccination rollout. The survey is cross-sectional, so we are unable to infer causality between attitudinal factors and intention. Although our sample was broadly representative across the dimensions of age, sex, and ethnicity, representativeness was not specifically sought in the quota sampling for other dimensions such as location in the United Kingdom or socio-economic status.
To our knowledge, this is the first peer-reviewed study investigating the intention to receive a COVID-19 vaccination in a demographically representative sample of the UK population since the COVID-19 vaccination rollout began in December 2020. Three-quarters of our sample reported being very likely to have the COVID-19 vaccination. However, since vaccine uptake may well be lower than vaccine intention, it is important to understand the factors associated with intention and to ensure that communication and engagement strategies related to the vaccination are informed by those factors. Going forward, it is not yet known for how long COVID-19 vaccines confer immunity or how effective they will continue to be against emerging strains as the virus mutates and, consequently, whether booster vaccines may be required.24 In order to ensure the success of the current vaccination rollout and any subsequent vaccination waves, our findings underline the importance of ongoing clear communication informed by theoretical constructs related to COVID-19 vaccination beliefs and attitudes, and the need for such communication to emphasise social acceptance of the vaccination, the importance of vaccination to stop the spread of COVID-19, even in the absence of underlying risk factors, and the safety of the vaccination.
Author statements
Ethical approval
Ethical approval for this study was granted by Keele University's Research Ethics Committee (reference: PS-200129).
Funding
The authors disclose receipt of the following financial support for the research, authorship, and/or publication of this article: a Keele University Faculty of Natural Sciences Research Development award to SS, JS and NS, and a Kings COVID Appeal Fund award granted jointly to LS, GJR, RA, NS, SS and JS. LS, RA and GJR are supported by the National Institute for Health Research Health Protection Research Unit (NIHR HPRU) in Emergency Preparedness and Response, a partnership between Public Health England, King's College London and the University of East Anglia. NS′ research is supported by the National Institute for Health Research (NIHR) Applied Research Collaboration (ARC) South London at King's College Hospital NHS Foundation Trust. NS is a member of King's Improvement Science, which offers co-funding to the NIHR ARC South London and is funded by King's Health Partners (Guy's and St Thomas' NHS Foundation Trust, King's College Hospital NHS Foundation Trust, King's College London and South London and Maudsley NHS Foundation Trust), and the Guy's and St Thomas’ Charity. The views expressed are those of the authors and not necessarily those of the NIHR, the charities, Public Health England or the Department of Health and Social Care.
Competing interests
NS is the director of the London Safety and Training Solutions Ltd, which offers training in patient safety, implementation solutions and human factors to healthcare organizations and the pharmaceutical industry. The other authors have no conflicts of interest to declare.
Transparency declaration
The authors affirm that the manuscript is an honest, accurate, and transparent account of the study being reported and no important aspects of the study have been omitted; and that any discrepancies from the study as originally planned have been explained.
Data sharing statement
Data are available online15.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.puhe.2021.10.008.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases
- 2.Ledford H., Cyranoski D., Van Noorden R. The UK has approved a COVID vaccine – here's what scientists now want to know. Nature. 2020;588:205–206. doi: 10.1038/d41586-020-03441-8. [DOI] [PubMed] [Google Scholar]
- 3.https://www.bbc.co.uk/news/uk-55227325
- 4.Axelsen P.H., Poland G.A. Vaccines, masks, distancing and credibility: an urgent warning for pandemic management. Vaccine. 2021;39:1173–1174. doi: 10.1016/j.vaccine.2021.01.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sherman SM, Smith L, Sim J, Amlôt R, Cutts M, Dasch H, et al. COVID -19 vaccination intention in the UK: results from the COVID-19 vaccination acceptability study, a nationally representative cross-sectional survey. Hum Vaccin Immunother. 2021;17:1612–1621. doi: 10.1080/21645515.2020.1846397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Freeman D., Loe B.S., Chadwick A., Vaccari C., Waite F., Rosebrock L., et al. COVID-19 vaccine hesitancy in the UK: the Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol Med. 2020 doi: 10.1017/S0033291720005188. online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bell S., Clarke R., Mounier-Jack S., Walker J.L., Paterson P. Parents' and guardians' views on the acceptability of a future COVID-19 vaccine: a multi-methods study in England. Vaccine. 2020;38:7789–7798. doi: 10.1016/j.vaccine.2020.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines. 2021;9:160. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Larson H.J., Jarrett C., Eckersberger E., Smith D.M., Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine. 2014;32:2150–2159. doi: 10.1016/j.vaccine.2014.01.081. [DOI] [PubMed] [Google Scholar]
- 10.https://www.bbc.co.uk/news/health-55586410
- 11.https://www.ft.com/content/ac5e5ef8-bccb-482b-9f8d-0dab5cac6f9a
- 12.https://www.telegraph.co.uk/global-health/science-and-disease/coronavirus-news-vaccine-pfizer-nhs-oxford-covid-uk-cases/
- 13.https://www.theguardian.com/world/2021/jan/05/no-data-to-support-uk-delay-of-vaccines-second-dose-says-who
- 14.https://www.theguardian.com/society/2021/jan/03/analysis-is-it-wise-for-england-to-mix-and-match-covid-vaccines
- 15.https://osf.io/dy5jv/
- 16.Rubin G.J., Bakhshi S., Amlôt R., Fear N., Potts H.W.W., Michie S. The design of a survey questionnaire to measure perceptions and behaviour during an influenza pandemic: the Flu TElephone Survey Template (FluTEST) Health Serv Deliv Res. 2014;2:41. doi: 10.3310/hsdr02410. [DOI] [PubMed] [Google Scholar]
- 17.Lee Mortensen G., Adam M., Idtaleb L. Parental attitudes towards male human papillomavirus vaccination: a pan-European cross-sectional survey. BMC Public Health. 2015;15:624. doi: 10.1186/s12889-015-1863-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Myers L.B., Goodwin R. Determinants of adults' intention to vaccinate against pandemic swine flu. BMC Public Health. 2011;11:15. doi: 10.1186/1471-2458-11-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wheelock A., Miraldo M., Thomson A., Vincent C., Sevdalis N. Evaluating the importance of policy amenable factors in explaining influenza vaccination: a cross-sectional multinational study. BMJ Open. 2017;7 doi: 10.1136/bmjopen-2016-014668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smith L.E., Mottershaw A.L., Egan M., Waller J., Marteau T.M., Rubin G.J. The impact of believing you have had COVID-19 on self-reported behaviour: cross-sectional survey. PLoS One. 2020;15 doi: 10.1371/journal.pone.0240399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Riley R.D., Snell K.I.E., Ensor J., Burke D.L., Harrell F.E., Moons K.G.M., et al. Minimum sample size for developing a multivariable prediction model: part I – Continuous outcomes. Stat Med. 2019;38:1262–1275. doi: 10.1002/sim.7993. [DOI] [PubMed] [Google Scholar]
- 22.Bartholomew D.J., Steele F., Moustaki I., Galbraith J.I. Chapman & Hall/CRC; Boca Raton, FL: 2002. The analysis and interpretation of multivariate data for social scientists. [Google Scholar]
- 23.Stemler S. An overview of content analysis. Practical Assess Res Eval. 2000;7:17. doi: 10.7275/z6fm-2e34. [DOI] [Google Scholar]
- 24.Majeed A. 2021. Can the UK meet its target of offering all adults a COVID-19 vaccine by 31 July?https://blogs.bmj.com/bmj/2021/02/22/can-the-uk-meet-the-governments-target-of-offering-all-adults-a-covid-19-vaccine-by-31-july/ [Google Scholar]
- 25.YouGov (12th March 2021) https://yougov.co.uk/topics/health/survey-results/daily/2021/03/12/66e85/3
- 26.https://www.theguardian.com/society/2021/mar/15/which-european-states-have-paused-astrazeneca-jabs-due-to-clotting-concerns
- 27.Ruiz J.B., Bell R.A. Predictors of intention to vaccinate against COVID-19: results of a nationwide survey. Vaccine. 2021;39:1080–1086. doi: 10.1016/j.vaccine.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Patelarou E., Galanis P., Mechili E.A., Argyriadi A., Argyriadis A., Asimakopoulou E., et al. Factors influencing nursing students' intention to accept COVID-19 vaccination: a pooled analysis of seven countries. Nurse Educ Today. 2021;104:105010. doi: 10.1016/j.nedt.2021.105010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Seale H., Heywood A.E., Leask J., Sheel M., Durrheim D.N., Bolsewicz K., et al. Examining Australian public perceptions and behaviors towards a future COVID-19 vaccine. BMC Infect Dis. 2021;21:120. doi: 10.1186/s12879-021-05833-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lackner C.L., Wang C.H. Demographic, psychological, and experiential correlates of SARS-CoV-2 vaccination intentions in a sample of Canadian families. Vaccine X. 2021;8:100091. doi: 10.1016/j.jvacx.2021.10009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Suppli C.H., Hansen N.D., Rasmussen M., Valentiner-Branth P., Krause T.G., Mølbak K. Decline in HPV-vaccination uptake in Denmark – the association between HPV-related media coverage and HPV-vaccination. BMC Public Health. 2018;18:1360. doi: 10.1186/s12889-018-6268-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.World Health Organization . World Health Organization; Geneva: 2017. Communicating risk in public health emergencies: a WHO guideline for emergency risk communication (ERC) policy and practice. [PubMed] [Google Scholar]
- 33.Robertson E., Reeve K.S., Niedzwiedz C.L., Moore J., Blake M., Green M., et al. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav Immun. 2021;94:41–50. doi: 10.1016/j.bbi.2021.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Martin C.A., Marshall C., Patel P., Goss C., Jenkins D.R., Ellwood C., et al. Association of demographic and occupational factors with SARS-CoV-2 vaccine uptake in a multi-ethnic UK healthcare workforce: a rapid real-world analysis. medRxiv. 2021 doi: 10.1101/2021.02.11.21251548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.NHS . 2021. COVID-19 vaccinations.https://www.england.nhs.uk/statistics/statistical-work-areas/covid-19-vaccinations/ [Google Scholar]
- 36.NHS . 2021. News: 25 to 29-year olds to be invited to receive life-saving Covid vaccine.https://www.england.nhs.uk/midlands/2021/06/07/25-to-29-year-olds-to-be-invited-to-receive-life-saving-covid-vaccine/ [Google Scholar]
- 37.Murphy J., Vallières F., Bentall R.P., Shevlin M., McBride O., Hartman T.K., et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. 2021;12:1–15. doi: 10.1038/s41467-020-20226-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Taraday M., Wieczorek-Taraday A. In: Frey B.B., editor. vol. 3. 2021. R-squared; pp. 1631–1633. (The SAGE encyclopedia of educational research, measurement, and evaluation). [Google Scholar]
- 39.Lewis-Beck M.S. In: Lewis-Beck M.S., Bryman A., Liao T.F., editors. vol. 3. 2004. R-Squared; pp. 983–984. (The SAGE encyclopedia of social science research methods). [Google Scholar]
- 40.Wong M.C., Wong E.L., Huang J., Cheung A.W., Law K., Chong M.K., et al. Acceptance of the COVID-19 vaccine based on the health belief model: a population-based survey in Hong Kong. Vaccine. 2021;39:1148–1156. doi: 10.1016/j.vaccine.2020.12.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.