Abstract
Introduction
Osteochondroma (solitary) and multiple hereditary exostoses (plural) are defined as a cartilage-capped bony projection arising on the external surface of bone containing a marrow cavity that is continuous with that of the underlying bone. These tumors grow slowly and develop to cause symptoms such as limited range of motion, joint pain, lumps, and deformities. The use of ulnar distraction osteogenesis has gained popularity in treating deformity in forearm osteochondroma. Problems that arise including bone angulation and persistent radial head dislocation.
Case presentation
We describe eight cases of forearm osteochondroma that came to the Prof. Dr. R. Soeharso Orthopedic Hospital, Surakarta, Indonesia. We found two variations in the classification of Masada in these 8 patients, Masada type I and IIB. The main complaint was a bent arm. We decided to do surgery in the form of tumor resection and reconstruction of the deformity by using ulnar gradual lengthening and osteotomies. The results of the procedure were investigated in this study, using clinical and radiological parameters focusing on medium-term functional and structural outcomes.
Discussion and conclusion
Eight patients had overall good results, although performed with a different sequence of operating techniques. Ulnar lengthening with a monorail fixator is still the main choice in its implementation. Gradual ulnar lengthening improves not only the deformity but also the functionality of the associated forearm.
Keywords: Osteochondroma, Multiple hereditary exostoses, Gradual lengthening
Highlights
-
•
Deformity often occurs in children with forearm osteochondroma.
-
•
Ulnar gradual lengthening remains choice of treatment.
-
•
The procedure resulted in good radiological and clinical outcome.
1. Introduction
Osteochondroma is defined as a cartilage-capped bony projection arising on the external surface of bone containing a marrow cavity that is continuous with that of the underlying bone. Osteochondroma often presents solitary but one-eighth of cases of these tumors present as multiple hereditary exostoses (MHE) [1].
Both osteochondroma and MHE occur from an early age. These tumors are growing slowly without clinical symptoms and are usually diagnosed at the age of 10 years which has had enough time to develop to cause symptoms such as limited range of motion, joint pain, lumps, and even deformities [1], [2], [3].
The onset of pain is not a feature of the tumor. However, because the location of the growth of the tumor is near the joint, it will affect the function of the joint, starting from a limited range of motion to causing persistent pain [1]. In the double bone region of the body, if the tumor invades one of the bones it can result in deformity. This can be noticed especially in the forearm consisting of radius-ulna [3].
Masada et al. divided the classification in forearm osteochondroma into three types where type II is divided into two subtypes. They observed the morphology of the tumor deformity and were supported by plain x-ray images. Masada et al. recommended operative measures for each of the types they presented. Type I, excision of osteochondroma, osteotomy of the radius, and immediate ulnar lengthening. Type IIa, excision of osteochondroma, osteotomy of the radius, immediate ulnar lengthening, and excision of the radial head. Type IIb, excision of osteochondroma, osteotomy of the radius, gradual ulnar lengthening. Type III, excision of osteochondroma [4].
We present 8 cases of forearm osteochondroma treated with ulnar distraction osteogenesis by using a monorail fixator. The surgery was performed by 3 senior orthopaedic surgeons. With the update on the consensus surgical case report, the writing of this case series is in accordance with the PROCESS guidelines. [5].
2. Case series
This was a retrospective case series of patients with forearm osteochondroma which underwent reconstruction using ulnar distraction osteogenesis. We collected data including age, gender, procedure, type, and problems/complications (Fig. 1). Type of treatment can be classified to tumor excision, ulnar lengthening, radial shortening osteotomy and ulnar osteotomy reconstruction.
Fig. 1.

Masada et al. classification of the forearm osteochondroma [4].
A total of 8 cases were included in this study. Forearm osteochondroma more commonly occurred in female patients with 5 of 8 (64%) cases. The Masada type IIB is more commonly found with 5 of 8 (64%) cases. No concomitant congenital abnormality was found in our series. There was no history of osteochondroma or MHE in their biological parents. The patients major complain were bent arm and prominent elbow lumps (Fig. 2, Fig. 3).
Fig. 2.
Thirty degrees of angulation in the elbow and prominent elbow lumps.
Fig. 3.
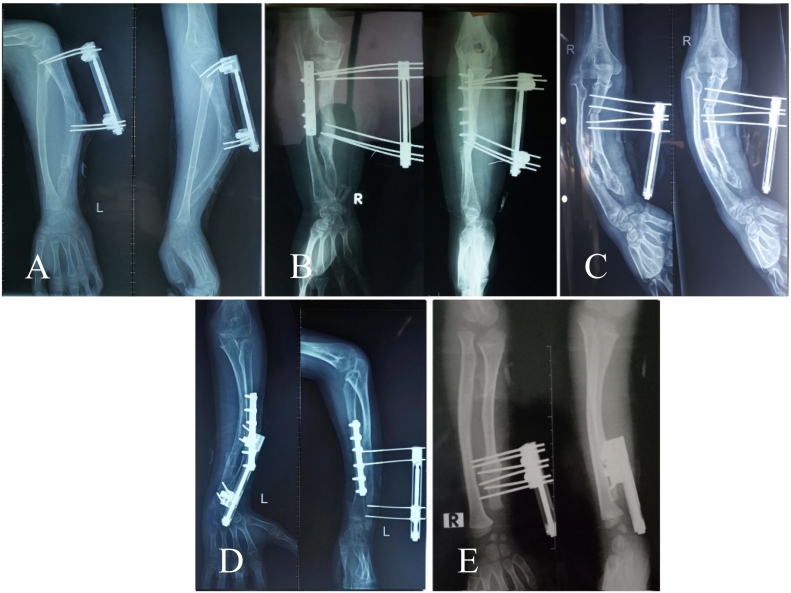
Plain X-rays show Masada classifications of type I (A, E) and type IIb (B, C and D).
The surgery was performed by three surgeons (HCK, MI, ABS). Surgery was performed under anesthesia with a tourniquet in a supine position. Distraction osteogenesis of ulna was performed with the use of 95 mm monorail fixator (® B-fix, Aike, Shanghai Medical Instrument, China). Tumor excision in distal ulna was performed first. The resulting tumor was sent for histopathological analysis. In 2 patients (Masada type II B) we decided to do radial shortening osteotomy and internal fixation using plate and screw in the first stage. The corticotomy/osteotomy for lengthening sites were in the metaphysis of distal ulna in 2 patients and proximal ulna in 6 patients. The latent period for metaphyseal distraction osteogenesis was 6–7 days. Afterward, distraction osteogenesis was performed with a rate 1 mm/day and can be modified by physician discretion. Post-operative follow-up was performed at two weeks, one month, and every 1 month thereafter. Standard rehabilitation protocol was performed on the patients. The patient was allowed for early ROM exercise. Clinical evaluation and radiological evaluation were performed during follow-up.
In the second stage, we performed monorail fixator removal in all patients. Ulnar and radial osteotomy reconstruction using plate and screw were performed in 3 patients. (see Fig. 5). The radiological evaluation indicators of deformities include ulnar shortening (US), radial articular angle (RAA), and carpal slip (CS) [23]. The indexes were recorded preoperatively and at the final follow-up. The Mayo Elbow Performance Score (MEPS) was used to evaluate elbow function. [6]. From the follow-up, all patients had overall good and excellent results (Table 1).
Fig. 5.
After the second stage of surgery, patient A-B-C performed correction of bone angulation, and patient D-E performed removal of fixation.
Table 1.
Distribution of patient data.
| No | Age (y.o)/Sex | Masada type | Treatment |
Complication/problems | Radiological preop | Radiological FFU | MEPS FFU |
Duration of Follow up | |
|---|---|---|---|---|---|---|---|---|---|
| 1st stage | 2nd stage | ||||||||
| 1 | 13/F | II B | Tumor excision + Radial shortening +ulnar gradual lengthening | ROEF | – | US: 1 cm RAA: 380 CS: 50% |
US: 0 cm RAA: 300 CS: 20% |
80 (good) |
24 months |
| 2 | 9/M | IIB | Tumor excision + ulnar gradual lengthening | ROEF + Ulnar reconstruction | Deviation of ulna axis after 1st stage | US: 1.4 cm RAA: 440 CS: 75% |
US: 0.4 cm RAA: 280 CS: 10% |
80 (good) |
13 months |
| 3 | 14/F | IIB | Tumor excision + ulnar gradual lengthening | ROEF + radial shortening + ulnar reconstruction | Radial head dislocation and deviation of ulna axis (+) after 1 st stage | US: 0.4 cm RAA: 550 CS: 75% |
US: 0.2 cm RAA: 410 CS: 35% |
75 (good) |
24 months |
| 4 | 9/F | IIB | Tumor excision + Radial shortening +ulnar gradual lengthening | ROEF | – | US: 0.3 cm RAA: 300 CS: 60% |
US: 0 cm RAA: 280 CS: 5% |
80 (good) |
34 months |
| 5 | 7/M | I | Tumor excision + ulnar gradual lengthening | ROEF | – | US: 1.3 cm RAA: 320 CS: 85% |
US: 0 cm RAA: 280 CS: 25% |
90 (excellent) |
21 months |
| 6 | 11/M | I | Tumor excision + ulnar gradual lengthening | ROEF | – | US: 1 cm RAA: 300 CS: 15% |
US: 0 cm RAA: 260 CS: 10% |
95 (excellent) |
21 months |
| 7 | 9/F | I | Tumor Excision + Ulnar gradual lengthening | ROEF | – | US: 1.1 cm RAA: 320 CS: 50% |
US: 0.6 cm RAA: 250 CS: 25% |
95 (excellent) |
12 months |
| 8 | 5/F | IIB | Tumor excision + +ulnar gradual lengthening | ROEF + radial shortening | Radial head dislocation (+) after 1st stage | US: 0.8 cm RAA: 250 CS: 60% |
US: 0.2 cm RAA: 280 CS: 20% |
90 (excellent) |
12 months |
Abbreviations: ROEF,removal of external fixator; US, ulnar shortening; RAA, radial articular angle; CS, carpal slip; MEPS, mayo elbow performance score; FFU, final follow up.
For the osteochondroma Masada type I cases, we performed one stage of surgery consist of tumor excision and ulnar gradual lengthening. In this condition, it is expected that the non-angulated radius bone will guide the lengthening of the ulna, thus avoiding ulnar axis deviation when distraction is performed. We found good radiological and functional results in these 3 cases of Masada I (Fig. 3, Fig. 4).
Fig. 4.
The first stage surgery consist of tumor resection and bone lengthening. X ray after 3 months of follow-up.
On the other hand, we had 5 patients with osteochondroma Masada type IIB. We did tumor excision, ulnar lengthening, and radial reconstruction in the first stage on 2 patients and we did the ulnar and or radial reconstruction in 2nd stage of surgery in 3 patients. From the follow-up, the 5 children had improved radiological measurement and overall good functional results (Fig. 4, Fig. 5, Table 1).
3. Discussion
Osteochondroma and MHE may cause deformity, limited joint function, and even pain due to the influence of surrounding tissues [7]. The deformity in osteochondroma is caused by the shortening of the ulna to the radius. This is caused by the pathology of osteochondroma which is located in the distal metaphyseal of the ulna. The pathogenesis of this deformity is still not clearly understood. However, 4 hypotheses have been known for a long time that explains the pathophysiology of the deformity [8], [9], [10], [11], [20], [21], [22].
As already described, Masada et al. have recommended surgery for each type of osteochondroma based on their classification [4]. However, especially in the type of osteochondroma with radial head dislocation, there is no global agreement on the management of resection and correction of the deformity [12], [13], [14], [15], [16], [17], [18]. In this study, we performed different methods to treat forearm osteochondroma Masada type IIb. Two patients underwent single-stage surgery and 3 patients underwent radial or ulnar osteotomy in the second surgery. We expected the radial head dislocation to be reduced when using ulnar lengthening in the first stage, so if there are any residual deformities, we may correct them in the second stage of surgery.
Zheng C et al. performed a retrospective study of children with MHE. This study involved 37 children aged 4–12 years with an average age of 7 years. Of the available x-rays, all patients have been categorized under the Masada classification. All patients had tumor resection followed by reconstruction of the lengthening ulna. In their statistical analysis, they concluded that the operation resulted in a good outcome. Factors to be considered are deformity and functional forearm such as flexion, extension, supination, and pronation [6].
Li Y et al. also performed a retrospective study of 15 forearms of patients with MHE Masada types I and IIb. This research sample is the same as the case series that is being presented. They concluded that tumor resection accompanied by gradual ulnar lengthening was the right measure to correct forearm deformities that have implications for the return of normal forearm function [19].
Ulnar deviations were found in 2 patients with Masada IIB. They were all corrected in the second stage of surgery. The occurrence of these complications may be related to the position of osteotomy and the direction of the bar. It is recommended to choose the proximal part of ulna for osteotomy avoiding the maximum curvature as much as possible. [6]
For ulnar lengthening in all eight patients, we used a monorail fixator. This is in line with the techniques proposed by Masada et al. and two other studies [4], [6], [19]. The use of the uniplanar system has disadvantages in maintaining the direction of the distraction. This problem can increase the risk of increasing angulation because the ulnar axis is not perfectly straight. However, the use of the Illizarov (circular external lengthening) tool also has limitations when applied to the forearm. The bulky shape of the tool will make it difficult for children to carry out their daily activities. Wires that are attached in a multi-direction are at risk of injuring more soft tissue or even neurovascular bundles [6]. As happened in this case series, due to the uncorrected angulation with the use of uniplanar bone lengthening, it was continued with open reduction and internal fixation reconstruction.
This study has several limitations. This retrospective series has data collection limitations and differences in the follow-up period. This study also didn't compare with another procedure which may have different success or complication rates. However, we believe this study still could give some additional information to previous literature. This study supports the use of ulnar lengthening method for treating forearm osteochondroma. The possible problems related to ulnar lengthening using monoplanar fixator also have been reported in this study.
4. Conclusion
Ulnar lengthening with a monoplanar fixator is still the main choice for treating forearm osteochondroma Masada type I and IIB. Radial shortening osteotomy and ulnar osteotomy may be used for correcting the residual deformity. Despite being performed with a different sequence of operating techniques, all patients had overall good clinical and radiological results. We suggest that further studies be conducted to compare the surgical techniques in forearm osteochondroma.
Patient perspective
All patients stated that their experience of undergoing surgery was the right decision. They said that after surgery, the shape and function of their forearms were improved.
Informed consent
All patients gave informed consent to the researcher. A form stating their consent is attached.
Sources of funding
In this case series, we use our resources without any financial assistance from other parties.
Provenance and peer review: Not commissioned, externally peer-reviewed.
Funding
In this case series, we use our resources without any financial assistance from other parties.
Ethical approval
This case series got ethical approval from our institution.
Consent
We have obtained informed consent from all patients represented by their parents because the patient is still a child. The form is attached in the file.
Guarantor
Hendra Cahya Kumara,
Mujaddid Idulhaq,
Anung Budi Satriadi,
Saddalqous
CRediT authorship contribution statement
Hendra Cahya Kumara/Author 1: Acts as a doctor and surgeon who performs actions on patients. Determine the theme of the case series, study concept, and design as well as make corrections to the writing.
Mujaddid Idulhaq/Author 2: Acts as doctors and surgeons who perform actions on patients. Make corrections to the writing of the case series.
Anung Budi Satriadi/Author 3: Acts as a doctor and surgeon who performs actions on patients.
Saddalqous/Author 4: Acts as the data collector, data analysis and interpretation as well as writing the paper.
Declaration of competing interest
All authors state that there are no financial and personal relationships with other people or organizations that could inappropriately influence (bias) for this case series.
References
- 1.Kitsoulis P., Galani V., Stefanaki K., Paraskevas G., Karatzias G., Agnantis N.J. Osteochondromas: review of the clinical,radiological and pathologicalfeatures. In Vivo. 2008;22:633–646. [PubMed] [Google Scholar]
- 2.Ryckx A., Somers J.F.A., Allaert L. Hereditary multipleexostosis. Acta Orthop. Belg. 2013;79:597–607. [PubMed] [Google Scholar]
- 3.Arienzo A.D., Andreani L., Saccheti F., Colangeli S., Capanna R. Multiple hereditary exostoses: currentinsights. Orthop. Res. Rev. 2019;11:199–211. doi: 10.2147/ORR.S183979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Masada K., Tsuyuguchi Y., Kawai H., Kawabata H., Noguchi K., Ono K. Operations for forearm deformity caused by multiple osteochondromas. J. Bone Joint Surg. 1989;71(B):24–29. doi: 10.1302/0301-620X.71B1.2914999. [DOI] [PubMed] [Google Scholar]
- 5.Agha R.A., Sohrabi C., Mathew G., Franchi T., Kerwan A., O’Neill N for the PROCESS Group The PROCESS 2020 guideline: updating consensus Preferred Reporting Of CasE Series in Surgery (PROCESS) guidelines. Int. J. Surg. 2020;84:231–235. doi: 10.1016/j.ijsu.2020.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Zheng C., Han H., Cao Y. Gradual lengthening of the ulna for the treatment of forearmdeformities in children with hereditarymultipleexostosis:aretrospectivestudy. Res. Square. 2020:1–16. [Google Scholar]
- 7.Bottner F., Rodl R., Kordish I., Winklemann W., Gosheger G., Lindner N. Surgical treatment of symptomatic osteochondroma. J. Bone Joint Surg. 2003;85(B):1161–1165. doi: 10.1302/0301-620x.85b8.14059. [DOI] [PubMed] [Google Scholar]
- 8.Rodgers W.B., Hall J.E. One-bone forearm as a salvage procedure for recalcitrant forearm deformity in hereditary multiple exostoses. J.Pediatr. Orthop. 1993;13(5):587–591. [PubMed] [Google Scholar]
- 9.Schmale G.A., Conrad E.U., Raskind W.H. The natural history of hereditary multiple exostoses. J. Bone Joint Surg. Am. 1994;76(7):986–992. doi: 10.2106/00004623-199407000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Stanton R.P., Hansen M.O. Function of the upper extremities in hereditary multiple exostoses. J. Bone Joint Surg. Am. 1996;78(4):568–573. doi: 10.2106/00004623-199604000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Massobrio M., Pellicanò G., Albanese P., Antonietti G. Forearm post-traumatic deformities: classification and treatment. Injury. 2014;45(2):424–427. doi: 10.1016/j.injury.2013.09.020. [DOI] [PubMed] [Google Scholar]
- 12.Fogel G.R., McElfresh E.C., Peterson H.A., Wicklund P.T. Management of deformities of the forearm in multiple hereditary osteochondromas. J. Bone Joint Surg. Am. 1984;66(5):670–680. [PubMed] [Google Scholar]
- 13.Arms D.M., Strecker W.B., Manske P.R., Schoenecker P.L. Management of forearm deformity in multiple hereditary osteochondromatosis. J.Pediatr. Orthop. 1997;17(4):450–454. [PubMed] [Google Scholar]
- 14.Akita S., Murase T., Yonenobu K., Shimada K., Masada K., Yoshikawa H. Longterm results of surgery for forearm deformities in patients with multiple cartilaginous exostoses. J. Bone Joint Surg. Am. 2007;89(9):1993–1999. doi: 10.2106/JBJS.F.01336. [DOI] [PubMed] [Google Scholar]
- 15.Ezaki M., Scott M.D., Oishi N. Technique of forearm osteotomy for pediatric problems. J. Hand Surg. Am. 2012;37(11):2400–2403. doi: 10.1016/j.jhsa.2012.08.033. [DOI] [PubMed] [Google Scholar]
- 16.Mader K., Koolen M., Flipsen M., van der Zwan A., Pennig D., Ham J. Complex forearm deformities: operative strategy in posttraumatic pathology. Obere Extrem. 2015;10(4):229–239. doi: 10.1007/s11678-015-0341-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jeuken R.M., Hendrickx R.P.M., Schotanus M.G.M., Jansen E.J. Near-anatomical correction using a CT-guided technique of a forearm malunion in a 15-year-old girl: a case report including surgical technique. Orthop. Traumatol. Surg. Res. 2017;103(5):545. doi: 10.1016/j.otsr.2017.03.017. [DOI] [PubMed] [Google Scholar]
- 18.Utomo P., Idulhaq M., Brilianto B.I. Multiple hereditaryexostosis of distalulna with dislocation of radialhead:acasereport. Indones J. Med. 2020;5(01):63–69. [Google Scholar]
- 19.Li Y., Wang Z., Chen M., Cai H. Gradual ulnar lengthening in masada type I/IIb deformity in patients with hereditary multiple osteochondromas: a retrospective study with a mean follow-up of 4.2 years. J.Orthop.Surg.Res. 2020;15:594–602. doi: 10.1186/s13018-020-02137-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.O’Hagan T., Reddy D., Hussain W.M., Mangla J., Atanda A., Jr., Bielski R. A complex injury of the distal ulnar physeal: a case report and brief review of the literature. Am. J. Orthop. (Belle Mead N.J.) 2012;41(1):E1–E3. [PubMed] [Google Scholar]
- 21.Chimenti P., Hammert W. Posttraumatic distal ulnar physeal arrest: a case report and review of the literature. Hand (NY) 2013;8(1):115–119. doi: 10.1007/s11552-012-9464-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cheng P.G., Chang W.N., Lin H.S., Wu S.K., Wang M.N. Traumatic separation of the distal ulnar physis in children: a new classification for displaced volar flexion injuries. J.Orthop.Trauma. 2014;28(8):476–480. doi: 10.1097/BOT.0000000000000060. [DOI] [PubMed] [Google Scholar]
- 23.Ham J., Flipsen M., Koolen M., Zwan A.V.D., Mader K. Multiple osteochondromas (MO) in the forearm: a 12-year single-centerexperience. Strat. Traum Limb. Recon. 2016;11:169–175. doi: 10.1007/s11751-016-0267-1. [DOI] [PMC free article] [PubMed] [Google Scholar]