Abstract
Objective
T2 inversion sequence is used in routine radiology practice mainly to heighten contrast resolution within the region to be studied but no evidence exists in current literature to assess it's true efficacy for lumbar disc degeneration. The objective of this study was to analyse T2 inversion and evaluate it's efficacy in assessment of lumbar disc pathology,.
Materials and methods
This retrospective single-centre study included 50 randomly selected patients presenting with back pain and radiculopathy. T2 inversion sequence was obtained in both axial and sagittal planes in addition to routine sequences. All the Magnetic Resonance Imaging (MRI) procedures were performed on 3T. One senior Musculoskeletal (MSK) radiologist, 2 general radiologists and a spinal surgeon blinded to final results reviewed images for the various disc pathologies individually analysing conventional and T2 inversion images. Data was analysed using Fischer's test and Chi2 test with a p value of <0.05 considered as significant.
Results
Fifty randomly selected patients (mean age was 47.3 years(range 35–55 years) with back pain and radicular symptoms were included. The spectrum of disc pathologies included protrusions, annular fissures, discal cysts and calcified discs. Based on the above findings, T2 inversion sequence is not proved to be an alternative imaging sequence to routine MR imaging sequences for the depiction of various disc pathologies.
Conclusion
T2 inversion sequence does not increase the depiction of various lumbar disc pathologies in comparison with conventional sequences when used by experienced MSK radiologists. It may highlight abnormalities better for relatively inexperienced readers such as general radiologists and spinal surgeons.
Keywords: MRI, Lumbar spine, T2 inversion sequence, Disc pathologies
1. Introduction
Back pain is one of the most common causes of morbidity, loss of productivity and emergency work absenteeism. Disc pathologies may be the primary cause of symptoms in the majority of patients.1, 2, 3 For the assessment of disc injuries, a variety of imaging modalities are available, including plain radiographs and Computerized Tomography (CT)-myelography. Over the last few decades, Magnetic Resonance (MR) imaging of the spine has advanced significantly, becoming the preferred tool for detecting lumbar disc herniation.1,4,5 MR imaging's sensitivity and specificity for intervertebral disc disorders are well established.6, 7, 8 T2 sagittal and axial images are in general, primarily used to assess the disc bulges and nerve root impingement. These images are routinely viewed as Grey scale images on Picture Archiving and Communication System (PACS). Although grey scale T2 sequences are good in depicting disc bulges, they are limited in differentiating disc calcification from a disc bulge and intra discal cyst from annular tears.
Some of the recent studies have demonstrated the utility of inverted grey scale images in providing additional inputs in interpreting the images, particularly in assessment of pulmonary nodules in chest radiographs and also in identification of the calcification on mammograms.9, 10, 11, 12, 13 While greyscale inversion images have been studied in radiographs, utility of grey scale inversion MRI images are still unexplored. The aim of this study was to assess the efficacy of T2 inversion sequence in the depiction of various lumbar disc pathologies in comparison with routinely performed lumbar spine sequences.
1.1. MRI imaging techniques
MRI of the lumbar spine generally includes a sagittal T1-weighted spin echo sequence, a sagittal T2-weighted spin echo sequence, and axial T2-weighted images. Additional sequences including axial T1-weighted sequences, short tau inversion recovery (STIR) or modified Dixon (mDixon), and gadolinium-based contrast enhanced T1-weighted sequences may be obtained depending on the institution and the indication for the MRI examination.
Sagittal T1-weighted images are useful in the assessment of bone marrow, which is normally fatty in adults and demonstrates high T1 and T2 signal. Alignment of the vertebral bodies can also be assessed on the sagittal T1-weighted sequence. Due to the high contrast between fat and nerve roots, the T1 sagittal sequences are excellent for assessing the degree of neural foraminal stenosis.
Sagittal T2-weighted images provide excellent contrast between cerebrospinal fluid (CSF) in the thecal sac and the surrounding structures, allowing for assessment of the degree of spinal stenosis at multiple levels on a single image. These sequences are also useful for assessment of the intervertebral discs. Fluid sensitive sequences such as STIR and mDixon are used for detecting areas of bone marrow oedema.
Axial T2-weighted images provide a level-by-level assessment of the relationship between the thecal sac and the surrounding bony and ligamentous structures and are particularly useful for assessing spinal stenosis and narrowing of the lateral or subarticular recesses. These sequences are also used in assessing the facet joints and ligamentum flava.
2. Materials and Methods
This study consisted of 50 randomly selected patients referred with back pain and radicular symptoms. Local ethical committee approval was obtained.The study was performed during the period from December 2019 to January 2021. MR examinations were performed with Siemens 3T. The conventional lumbar MR imaging protocol included T1 and T2W TSE sagittal and T2W TSE axial planes, which were analysed as grey scale images on the GE PACS. (GE Centricity™ Universal Viewer v 6.0).Using the GE PACS image manipulation tool, grey scale T2 axial and sagittal images were inverted to produce T2 inversion images.
2.1. Analysis of the data set
All images were independently interpreted by two general radiologists, a spinal surgeon and a fellowship trained MSK radiologist with over two years’ of experience. Conventional Lumbar spine sequences were interpreted in the grey scale format. Results of T2 inversion sequences were compared with results obtained by assessing conventional sequences with a single comparison reading.
Statistics: The statistical analysis was performed by Fischer's test and Chi2 test using the SPSS 15.0 written form (SPSS-Inc, Chicago-IL) with a p < 0.05 being considered as statistically significant.
3. Results
Fifty randomly selected patients with back pain and radicular symptoms were included. The mean age of the cohort was 47.3 years (range 35–55 years). The patients presented with varied disc pathologies including bulging discs, annular fissures, discal cysts and calcified discs(Table 1)(Fig. 1, Fig. 2, Fig. 3, Fig. 4).
Table 1.
Categorizing the patients with Disc pathologies.
| Disc pathologies | Number | Percentage |
|---|---|---|
| Bulging discs | 15 | 30 |
| Annular fissures | 10 | 20 |
| Discal cysts | 11 | 22 |
| Calcified discs | 14 | 28 |
| Total | 50 |
Fig. 1.
T2 axial (a) and inversion (b) showing left paracentral disc protrusion (arrow).
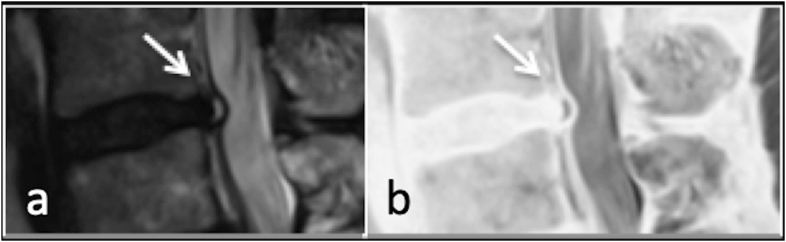
Fig. 2.
T2 sagittal (a) and inversion (b) showing annular fissure (arrow).
Fig. 3.
T2 axial (a) and inversion (b) showing left paracentral disc cyst (arrow).
Fig. 4.
T2 axial (a) and inversion (b) showing right paracentral calcified disc protrusion (arrow).
Results of the independent assessments showed that while the MSK radiologist did not assess both sets of images variably the less experienced radiologist and spinal surgeon had significant variability for all types of disc pathologies (Table 2).
Table 2.
Statistical analysis result interpretation by multidisciplinary readers.
| Disc pathologies | Results of Fischer's test and Chi2 test (p < 0.05 as significant) |
|||
|---|---|---|---|---|
| Evaluation of MRI images by experienced Radiologist | Evaluation of MRI images by General Radiologist | Evaluation of MRI images by Spinal surgeon | Evaluation of MRI images by fellowship trained radiologist | |
| Bulging discs | 0.17 | 0.3 | 0.04 | 0.16 |
| Annular fissures | 0.11 | 0.002 | 0.49 | 0.16 |
| Discal cysts | 0.01 | 0.35 | 0.01 | 0.17 |
| Calcified discs | 0.35 | 0.19 | 0.0002 | 0.35 |
| ‘p’ value | 0.26 | 0.0006 | 0.0001 | 0.26 |
4. Discussion
Advances in the medical imaging technologies have transformed all stages of healthcare provision. Imaging is central to patient care pathways now and plays a vital role in identifying anatomical abnormalities, diagnosis of pathologies, choosing medical vs surgical treatment options and presurgical planning. Images obtained through all the imaging modalities are projected and displayed in various shades of grey scale depending on the attenuation values of an organ on x ray and CT or ability of the organ to return signal on Ultrasound and MRI. Radiologists are trained to interpret these images in the grey scale format. Although the grey scale images are most frequently used method to carry or display the imaging information for analysis and interpretation, recent advances have attempted different ways to represent the imaging data for image interpretation such as colour coded visualization and inversion display of images.14 Image Inversion is a simple tool available in most of the image viewers and PACS, hence obtaining the inversion images is relatively easy.
The utility of Grey scale inversion images in various fields of radiology has been analysed by many researchers. Altunkeser and colleagues found that Grey scale inverted images when used along with standard images facilitated detection of microcalcification in mammography.19 Park and colleagues after analysing the usefulness of Grey scale inversion radiographs, alone or as an additional imaging modality in detecting rib fractures in minor trauma concluded that combined use of inverted images and conventional images improved detection of fracture in junior residents and medical students with no statistically significant improvement in senior residents (20).
Thomson JD and collogues assessed the impact of grey scale inversion images in detecting the lung nodules in posteroanterior chest radiographs and found no statistically significant difference in nodule detection. (18). Similarly, inversion images were found not significantly useful in detection of the pneumothorax (21) and in measuring endodontic fills in comparison with conventional images(22) on the other hand Inversion images in some of the newer sequences such as T1 vibe have been found useful to provide additional inputs compared to grey scale images. (23).
When we compared the T2 inversion sequence results with those obtained through routine sequences, the T2 inversion sequence results were not statistically different from those of routine MRI by a fellowship trained radiologist and experienced radiologist. The results were insignificant for each individual variable i.e. each disc pathologies as well as for grouped variables (p > 0.05). On the other hand, results were statistically significant for the general radiologist and the spinal surgeon (Table 2). Based on the above findings, we concluded that, T2 inversion sequence is not proved to be an alternative imaging modality to routine MR imaging sequences for the depiction of various disc pathologies and has no advantages over routine MRI sequence mapping.
To our knowledge, no published studies are available in the literature regarding the utility of T2 inversion in spine assessment. Although there are no similar studies available, we believe our study confirms the results obtained by Park and colleagues and we feel that T2 inversion may be of some use in beginners and less experienced radiologists in identifying various disc related abnormalities, but will not contribute significantly for well-trained or senior radiologists.9, 10, 11, 12, 13, 14, 15, 16, 17
The limitations of our study include a small sample size. Another important factor to consider is that radiologists are trained to interpret the images in the grey scale format. This familiarity with grey scale may act as a bias, which also could explain the results of our study, where in more experienced observers who have more expertise in interpreting grey scale images found T2 inversion images less useful than the less experienced observers.
Conclusion: Although T2 inversion sequences may provide some benefit for beginners, they are not overtly beneficial for well-trained senior radiologists in assessing the disc related pathologies.
Declaration of competing interest
No conflicts of interest.
No financial disclosures.
No funding to declare.
Contributor Information
Kompalli Jwala Satya Siva Raghu Teja, Email: drkjssrt@gmail.com.
Bhamidipaty Kanaka Durgaprasad, Email: bkdveena@gmail.com.
R. Botchu, Email: drbrajesh@yahoo.com.
References
- 1.Maksymowicz H., Sasiadek M., Dusza B., Filarski J. Evaluation of CBASS sequence in degenerative disease of the lumbar spine based on analysis of 78 consecutive cases. Med Sci Mon Int Med J Exp Clin Res. 2004;10:107–111. [PubMed] [Google Scholar]
- 2.Borenstein D.G. Chronic low back pain. Rheum Dis Clin N Am. 1996;22:439–456. doi: 10.1016/s0889-857x(05)70281-7. [DOI] [PubMed] [Google Scholar]
- 3.Valat J.-P., Genevay S., Marty M. Sciatica. Best Pract Res Clin Rheumatol. 2010;24:241–252. doi: 10.1016/j.berh.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 4.Saifuddin A., Braithwaite I., White J., Taylor B., Renton P. The value of lumbar spine Magnetic Resonance Imaging in the demonstration of anular tears. Spine. 1998;23:453–457. doi: 10.1097/00007632-199802150-00009. [DOI] [PubMed] [Google Scholar]
- 5.Ramlı N., Cooper A., Jaspan T. High resolution CISS imaging of the spine. Br J Radiol. 2001;74:862–873. doi: 10.1259/bjr.74.885.740862. [DOI] [PubMed] [Google Scholar]
- 6.Weishaupt D., Zanetti M., Hodler J., Boos N. MR imaging of the lumbar spine: prevalence of intervertebral disc extrusion and sequestration, nerve root compression, end plate abnormalities and osteoarthritis of the facet joints in asymptomatic volunteers. Radiology. 1998;209:661–666. doi: 10.1148/radiology.209.3.9844656. [DOI] [PubMed] [Google Scholar]
- 7.Tirman P.F.J. National orthopedic imaging associates. MRI of the lumbar spine: a sports medicine approach. Advanced MRI. 2002;1:1–4. [Google Scholar]
- 8.Modic M.T., Masaryk T.J., Boumphrey F., Goormastic M., Bell G. Lumbar herniated disc disease and canal stenosis: prospective evaluation of surface coil MR, CT nad myelography. Am Journal Rev. 1986;147:757–765. doi: 10.2214/ajr.147.4.757. [DOI] [PubMed] [Google Scholar]
- 9.Chong A.L., Chandra R.V., Chuah K.C. Proton density MRI increases detection of cervical spinal cord multiple sclerosis lesions compared with T2-weighted fast spin-echo. AJNR Am J Neuroradiol. 2016;37:180–184. doi: 10.3174/ajnr.A4476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thorpe J.W., MacManus D.G., Kendall B.E. Short tau inversion recovery fast spin-echo (fast STIR) imaging of the spinal cord in FIG, 4. Follow-up of a 32-year-old woman with relapsing-remitting MS presenting with acute paresthesia of the upper arm. Sagittal postcontrast T1WI (A) shows an enhancing cervical spinal cord lesion (black arrowhead) corresponding to an active inflammatory lesion. 3D-PSIR reformatted in the sagittal plane shows the same enhancing lesion on the magnitude image (B). 374 Fechner Feb 2019. Magn Reson Imaging. 1994;12:983–989. doi: 10.1016/0730-725x(94)91228-o. www.ajnr.orgmultiplesclerosis [DOI] [PubMed] [Google Scholar]
- 11.Nayak N.B., Salah R., Huang J.C. A comparison of sagittal short T1inversion recovery and T2-weighted FSE sequences for detection of multiple sclerosis spinal cord lesions. Acta Neurol Scand. 2014;129:198–203. doi: 10.1111/ane.12168. [DOI] [PubMed] [Google Scholar]
- 12.Poonawalla A.H., Hou P., Nelson F.A. Cervical spinal cord lesions in multiple sclerosis: T1-weighted inversion-recovery MR imaging with phase-sensitive reconstruction. Radiology. 2008;246:258–264. doi: 10.1148/radiol.2463061900. [DOI] [PubMed] [Google Scholar]
- 13.White M.L., Zhang Y., Healey K. Cervical spinal cord multiple sclerosis: evaluation with2Dmulti-echo recombined gradient echo MR imaging. J Spinal Cord Med. 2011;34:93–98. doi: 10.1179/107902610X12911165975025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sundarakumar D.K., Smith C.M., Hwang W.D. Evaluation of focal cervical spinal cord lesions in multiple sclerosis: comparison of white matter-suppressed T1 inversion recovery sequence versus conventional STIR and proton density-weighted turbo spin-echo sequences. AJNR Am J Neuroradiol. 2016;37:1561–1566. doi: 10.3174/ajnr.A4761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Riederer I., Karampinos D.C., Settles M. Double inversion recovery sequence of the cervical spinal cord in multiple sclerosis and related inflammatory diseases. AJNR Am J Neuroradiol. 2015;36:219–225. doi: 10.3174/ajnr.A4093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nair G., Absinta M., Reich D.S. Optimized T1-MPRAGE sequence for better visualization of spinal cord multiple sclerosis lesions at 3T. AJNR Am J Neuroradiol. 2013;34:2215–2222. doi: 10.3174/ajnr.A3637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hou P., Hasan K.M., Sitton C.W. Phase-sensitive T1 inversion recovery imaging: a time-efficient interleaved technique for improved tissue contrast in neuroimaging. AJNR Am J Neuroradiol. 2005;26:1432–1438. [PMC free article] [PubMed] [Google Scholar]
- 18.Thompson J.D., Thomas N.B., Manning D.J., Hogg P. The impact of greyscale inversion for nodule detection in an anthropomorphic chest phantom: a free-response observer study. Br J Radiol. 2016;89(1064):20160249. doi: 10.1259/bjr.20160249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Altunkeser Ayşegül, Körez M Kazım. Usefulness of grayscale inverted images in addition to standard images in digital mammography. BMC Med Imag. 18 Apr. 2017;17(1 26) doi: 10.1186/s12880-017-0196-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Park J.B., Cho Y.S., Choi H.J. Diagnostic accuracy of the inverted grayscale rib series for detection of rib fracture in minor chest trauma. Am J Emerg Med. 2015 Apr;33(4):548–552. doi: 10.1016/j.ajem.2015.01.015. Epub 2015 Jan 20. PMID: 25690384. [DOI] [PubMed] [Google Scholar]
- 21.Musalar E., Ekinci S., Ünek O. Conventional vs invert-grayscale X-ray for diagnosis of pneumothorax in the emergency setting. Am J Emerg Med. 2017;35:1217–1221. doi: 10.1016/j.ajem.2017.03.031. [DOI] [PubMed] [Google Scholar]
- 22.Oliveira Matheus Lima. Gray scale inversion in digital image for measurement of tooth length. Braz. Dent. J. [online]. 2012;23 doi: 10.1590/S0103-64402012000600013. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0103-64402012000600013&lng=en&nrm=iso>. ISSN 0103-6440 n.6 [cited 2021-04-26], pp.703–706. Available from: [DOI] [PubMed] [Google Scholar]
- 23.Koh Eamon. Vibe MRI: an alternative to CT in the imaging of sports-related osseous pathology? Br J Radiol. 2018;91:1088. doi: 10.1259/bjr.20170815. 20170815. [DOI] [PMC free article] [PubMed] [Google Scholar]