Abstract
Background
The decision to choose cruciate retaining (CR) insert or cruciate substituting (CS) insert during total knee arthroplasty (TKA) remains a controversial issue. We hypothesized that there are different knee kinematics between CR and CS inserts and that a raised anterior lip design would offer a potential minimization of the paradoxical movement and provide joint stability. The objective of this study was to evaluate and compare kinematics of a CR and CS TKA of the same single-radius design.
Methods
We investigated the in vivo knee kinematics of 20 knees with a CR TKA (10 knees in the CR insert and 10 knees in the CS insert). Patients were examined during deep knee flexion using fluoroscopy and femorotibial motion was determined using a 2- to 3-dimensional registration technique, which used computer-assisted design models to reproduce the spatial positions of the femoral and tibial components. We evaluated the knee range of motion (ROM), femoral axial rotation relative to the tibial component, anteroposterior translation, and kinematic pathway of the nearest point of the medial and lateral femoral condyles on the tibial tray.
Results
The average ROM was 121.0 ± 17.3° in CR and 110.8 ± 12.4° in CS. The amount of femoral axial rotation was 7.2 ± 3.9° in CR, and 7.4 ± 2.7° in CS. No significant difference was observed in the amount of anterior translation between CR and CS. The CR and CS inserts had a similar kinematic pattern up to 100° flexion that was central pivot up to 70° flexion and then paradoxical anterior femoral movement until 100° flexion.
Conclusion
The present study demonstrated that there was no significant difference between the inserts in knee kinematics. These kinematic results suggested that the increased anterior lip could not control anterior movement in the CS insert.
Keywords: Total knee arthroplasty, In vivo, Kinematics, Fluoroscopy, 2D/3D registration
1. Introduction
Total knee arthroplasty (TKA) is a successful procedure for pain relief and functional restoration in patients with advanced knee osteoarthritis,1,2 and has excellent long-term results, with several designs having greater than 90% survivorship at 10–20 years postoperatively.3,4
Recent reports show that approximately 19% primary TKA patients were not satisfied with their outcomes5 and patients undergoing TKA expressed lower satisfaction when compared with patients undergoing THA6 in general. The difficulty in performing activities of daily life has significant influence on patient satisfaction and expectations. In particular, “squatting” is a very important activity that significantly correlates with patient expectation after TKA.7 Therefore, manufacturers have attempted to improve the stability and durability of their designs and recreate kinematics that better approximate those seen in the native knee.
Many factors affect the determination of in vivo knee kinematics after TKA, particularly the effect of implant design.8, 9, 10 Previous studies have reported that the implant design substantially affects knee kinematics in deep knee flexion under weight-bearing.11, 12, 13 Thus, the geometry of the tibial polyethylene insert may affect knee kinematics.
On the other hand, there is some controversy over whether it is best to retain the posterior cruciate ligament (PCL) and use a cruciate retaining (CR) prosthesis or to remove it and use a cruciate substituting (CS) prosthesis during TKA.
CR designs offer the potential advantage of preserving the PCL, which in turn may aid knee kinematics, maintain femoral rollback during flexion, and increase the overall stability of the prosthesis.14, 15, 16, 17 Despite the excellent outcomes reported for CR designs, some authors have expressed doubts about the function of the remaining PCL in CR knees, questioned the above advantages and reported conflicting results regarding anteroposterior laxity, relative difficulty of surgery and decreased range of motion.18,19
The Triathlon total knee system (Stryker Orthopaedics, Mahwah, New Jersey, USA) was introduced in 2004. The femoral component has a single-radius from 10° to 110° flexion and the insert has a spherical rotary arc design to facilitate the rotation needed for deep knee flexion. These designs were made in an attempt to recreate natural knee kinematics without losing stability and to maximize range of motion.
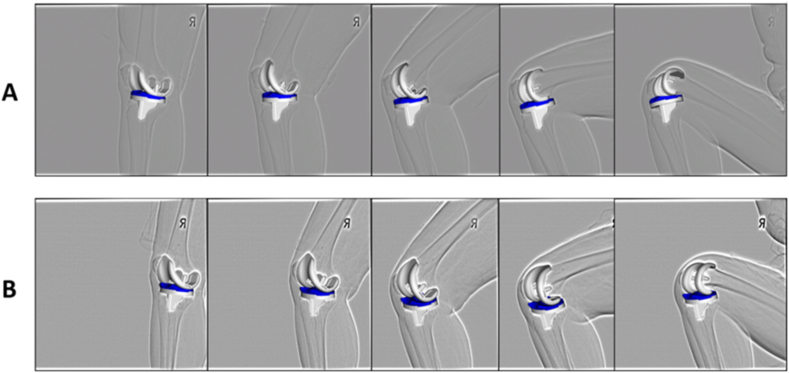
Compared with the standard CR insert, the more constrained CS insert has a raised anterior lip that provides greater anterior constraint and a recess to allow for stability in hyperextension (Fig. 1), and it can be used in cases where the PCL is sacrificed but a Posterior Stabilized (PS) insert is not used.
Fig. 1.
Comparison of the insert surface geometry. The insert has spherical rotary arc design. Compared with the CR insert, the CS insert has a raised anterior lip and the same posterior geometry.
However, even if the posterior cruciate ligament is retained in conventional knee implant, paradoxical anterior femoral movement with increasing flexion can sometimes be present with bicondylar femoral rollback occurring after that during deep knee flexion.14, 15, 16 It has not been clearly determined whether the use of a CS insert with the increased anterior lip could provide greater anterior constraint in vivo.
We hypothesized that there are different knee kinematics between CR and CS inserts and that a raised anterior lip design would offer a potential minimization of the paradoxical movement and provide joint stability. The objective of this study was to evaluate and compare in vivo kinematics of the CR and CS inserts in the same single-radius CR TKA design during deep knee flexion.
2. Materials and methods
We analyzed 20 knees of 17 patients who underwent successful TKA resulting in a Knee Society Score higher than 90 points. The review board committee of the author's institution approved this study and informed consent was obtained from all patients. All patients were implanted with Triathlon CR femoral components. The same tibial tray was used in all patients, with 10 knees having the CR insert with retained PCL between November 2008 and March 2011 and 10 knees having the CS insert with PCL sacrifice between May 2011 and May 2012. One senior author performed all the TKA procedures on the subjects using standard operative techniques. The rehabilitation regime was identical in the two groups. Postoperatively all patients were allowed for full weight-bearing, and they underwent rehabilitation the day after the operation. Mean age at the surgery was 70.3 ± 10.5 years (range, 38–80 years). Four patients were male and thirteen were female. Fourteen patients were diagnosed with osteoarthritis and three patients were diagnosed with rheumatoid arthritis. Average duration between the surgery and fluoroscopic surveillance was 17.2 ± 10.1 months (range, 7–41 months). The patient demographics are summarized in Table 1. Both groups were comparable with regard to age, gender, diagnosis, pre-operative range of motion (ROM) and follow-up period. The radiographic component alignment was evaluated following the Knee Society TKA Roentgenographic Evaluation. In the anteroposterior view, the alignment of femoral component was 95.9 ± 1.4° in CR and 96.4 ± 1.8°in CS (α angle) and the tibial angle was 89.5 ± 1.5° in CR and 89.5 ± 1.4° in CS (β angle). In the lateral view, the alignment of femoral component was 2.2 ± 1.9° flexion in CR and 2.8 ± 2.1° flexion in CS (γ angle) and the tibial posterior slope was 1.6 ± 1.7° in CR and 2.0 ± 1.9° in CS (δ angle).
Table 1.
Patient demographics.
| Parameters | CR | CS | P Value |
|---|---|---|---|
| Age (years) | 72 ± 12.4 | 68.6 ± 8.5 | 0.17 |
| BMI (kg/m2) | 25.1 ± 3.4 | 27.2 ± 2.1 | 0.34 |
| Gender (Male:Female) | 3:7 | 2:8 | 0.61 |
| Diagnosis (OA:RA) | 8:2 | 9:1 | 0.54 |
| Pre-operative flexion contracture (°) | 7.5 ± 10.6 | 10.8 ± 11.4 | 0.73 |
| Pre-operative flexion angle (°) | 107.5 ± 16.7 | 105.8 ± 22.3 | 0.74 |
| Follow-up (months) | 21.2 ± 11.2 | 12.3 ± 5.8 | 0.06 |
Under fluoroscopic surveillance in the sagittal plane, each patient was asked to perform sequential deep knee flexion under weight-bearing condition from full extension to maximum flexion. All patients stood with feet in neutral rotation. Patients were allowed to hold onto a handrail for safety. The patients practiced the motion several times before recording. Successful knee motions were recorded as serial digital radiograph images (1024 × 1024 × 12 bits/pixels, 7.5 Hz serial spot images as a DICOM file) on a 17-inch flat panel detector system (C-Vision Safire L; Shimadzu, Kyoto, Japan).
Individual component spatial positioning was estimated using a two-dimensional to three-dimensional (2D/3D) registration technique (Fig. 2).20, 21, 22 This technique was based on a contour-based registration algorithm using single-view fluoroscopic images and 3D computer-aided design models. Estimation accuracy of the relative motion between metal components was ≤0.5° in rotation and ≤0.4 mm in translation.
Fig. 2.
A two-dimensional to three-dimensional (2D/3D) registration. 2D/3D registration technique uses computer-assisted design models to reproduce the spatial position of femoral and tibial components from single-view fluoroscopic images (A:CR insert, B:CS insert).
We evaluated the ROM of knee joint, femoral axial rotation relative to the tibial component, and anteroposterior (AP) translation of the nearest point of the medial and lateral femoral condyles on the tibial tray.
The origin was defined as the center of gravity for the component in the femoral coordinate system, and as the center of the tibial tray surface in the tibial coordinate system. Knee rotations were described using the joint rotational convention of Grood and Suntay.23
Flexion of the femoral component relative to the tibial component was denoted as positive and extension was denoted as negative. External rotation of the femoral component relative to the tibial component was denoted as positive. In addition, AP translation of the nearest points between the femoral component and the tibial component was measured to evaluate the kinematic pathways. The nearest point was determined as the center of quasi-contact by calculating the closest distance between the surfaces of computer-aided design models for each of the medial and lateral sides. AP positions of the nearest points anterior to the centers of the coordinate system in the tibial component were denoted as positive, and the posterior positions as negative.
All data were expressed as mean ± standard deviation (SD). Non-parametric Mann–Whitney tests were used for comparisons of femorotibial nearest points and comparisons between CR and CS. Values of p < 0.05 were considered statistically significant.
3. Results
3.1. Range of motion (ROM)
The mean maximum knee extension angle was −1.6 ± 11.0° (−15.4 to 12.7) in CR and −0.6 ± 5.6° (−7.5 to 9.8) in CS. The mean maximum knee flexion angle was 119.4 ± 11.0° (102.6–130.7) in CR and 110.2 ± 8.6° (97.9–122.9) in CS. The mean ROM was 121.0 ± 17.3° (92.3–139.0) in CR and 110.8 ± 12.4° (88.2–126.0) in CS. No significant difference was observed between CR and CS with regard to the ROM (p = 0.14).
3.2. Femoral axial rotation
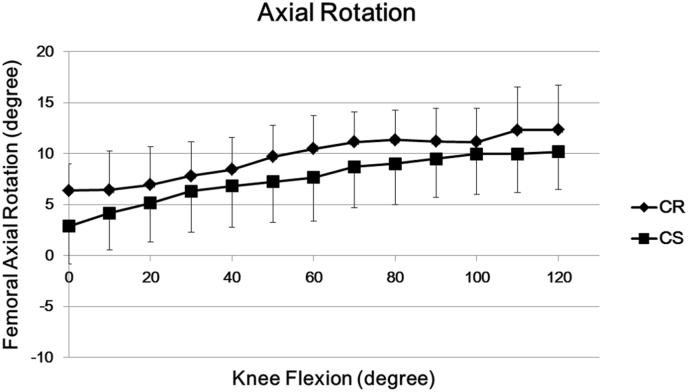
Regarding axial rotation of the femoral component relative to the tibial component, the mean degree of femoral axial rotation was 5.4 ± 3.2° (1.3–9.4) in CR and 2.8 ± 3.7° (−1.1 to 9.0) in CS at maximum extension. Mean axial rotation of the femoral component exhibited gradual external rotation from maximum extension to maximum flexion, and external rotation increased up to maximum flexion (Fig. 3). The mean degree of axial rotation was 12.6 ± 4.2° (6.1–17.0) in CR and 10.2 ± 3.7° (3.6–16.2) in CS at maximum flexion. All knees exhibited external rotation.
Fig. 3.
Axial Rotation. Regarding axial rotation, the external rotation of the femoral component relative to the tibial component increased up to maximum flexion.
The mean range of axial rotation from maximum extension to maximum flexion was 7.2 ± 3.9° (3.7–15.4) in CR and 7.4 ± 2.7° (2.8–11.5) in CS. No significant difference was observed in the amount of femoral external rotation (p = 0.60). Five of 10 knees in CR and 7 of 10 knees in CS had external rotation more than 5°. Furthermore, 2 of 10 knees in CR and 2 of 10 knees in CS had external rotation more than 10°.
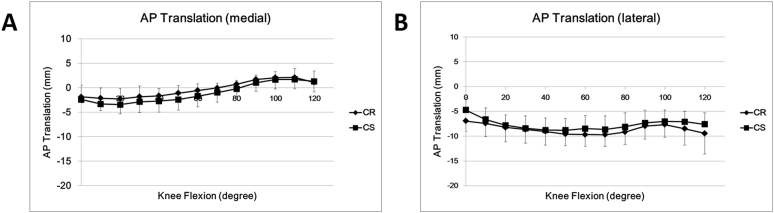
3.3. Anteroposterior (AP) translation
The mean AP translation of femorotibial nearest point was shown in Fig. 4A for medial side and Fig. 4B for lateral side.
Fig. 4.
Anteroposterior translation. Femoral anteroposterior translations of the medial (A) and lateral (B) femorotibial nearest points during deep knee flexion.
In CR, the medial side of AP nearest point was −1.9 ± 2.4 mm (−5.0 to 3.0) at 0° flexion. The medial nearest point moved gradually 3.9 ± 1.7 mm (0.7–6.4) anteriorly from 0° to 100° flexion, then moved 1.5 ± 2.0 (−0.2 to 5.7) mm posteriorly until 120° flexion. The lateral side was −6.9 ± 2.1 mm (−9.0 to −3.3) at 0° flexion. The lateral nearest point moved 2.8 ± 2.4 mm (−1.7 to 5.9) posteriorly from 0° to 70° flexion, and then moved 2.1 ± 0.9 mm (0.8–3.7) anteriorly from 70° to 100° flexion, and afterward moved 2.1 ± 2.9 mm (0.1–7.2) posteriorly until 120° flexion.
In CS, the medial side of AP nearest point was −2.4 ± 0.7 mm (−3.4 to −1.4) at 0° flexion. The medial nearest point moved gradually 4.1 ± 1.8 mm (1.3–6.8) anteriorly from 0° to 100° flexion, then moved 0.4 ± 0.6 (−0.2 to 1.7) mm posteriorly until 120° flexion. The lateral side was −4.4 ± 2.5 mm (−2.0 to −8.9) at 0° flexion. The lateral nearest point moved 4.2 ± 2.1 mm (1.7–7.1) posteriorly from 0° to 70° flexion, and then moved 1.6 ± 0.8 mm (0.0–2.6) anteriorly from 70° to 100° flexion, and afterward moved 0.6 ± 0.9 mm (−0.5 to 2.3) posteriorly until 120° flexion.
No significant difference was observed in the amount of anterior translation between CR and CS (medial; p = 0.92, lateral; p = 0.46).
3.4. Kinematic pathway
From the results of bilateral nearest points at each flexion angle, patterns of kinematic pathways were determined (Fig. 5).
Fig. 5.
Kinematic pathway. From the results of bilateral nearest points at each flexion angle, patterns of kinematic pathways were determined (A: CR insert, B: CS insert).
From 0° to 70° knee flexion, the medial side moved forward continuously, whereas the lateral side moved backward continuously. There was no significant difference between the amount of movement in medial and lateral side until 70° flexion (CR; p = 0.17, CS; p = 0.10). Therefore, the kinematic pattern was central pivot in both CR and CS.
From 70° to 100° knee flexion, both sides moved anteriorly, then the kinematics changed into bicondylar rollback, which both sides moved backwards until 120° flexion. Both sides in CR moved more posteriorly than those in CS from 100° flexion, but there was no significant difference between the amount of posterior movement in CR and CS (medial; p = 0.29, lateral; p = 0.24) statistically.
4. Discussion
This study presented the detailed in vivo kinematics of sequential deep knee flexion and compared kinematics between the CR and CS inserts in the same single-radius CR TKA design. These kinematic results indicated that there was no significant difference between the inserts.
We hypothesized that there may be different knee kinematics between CR and CS inserts. Some authors have previously compared kinematics of CR and CS designs. However, CS designs represent posterior stabilized (PS) designs having the post-cam mechanism in most studies.24,25 Few studies have focused on a more dished tibial insert referred to as a cruciate sacrificing design, same as design used in this study. As far as we know, our study is the first to compare in vivo kinematics between the CR and CS inserts in detail.
With regard to femoral axial rotation, the kinematic pattern was central pivot with an external rotation that the medial condyle moved anteriorly and the lateral side moved posteriorly in both CR and CS. This is conceivable that the femoral component rotated along the shape of insert that has spherical rotary arc design.
Several in vivo kinematic studies have found that paradoxical anterior femoral movement of the medial femoral condyle during knee flexion can occur in conventional TKA.12,14, 15, 16 This is supported by our fluoroscopic data, showing that paradoxical anterior femoral movement was observed in both CR and CS TKAs.
The absence of the anterior cruciate ligament (ACL) allows the tibia to slide forward, putting the femur in a posterior position near full extension and then the femur will slide forward as a compensatory mechanism during knee flexion, which has been observed in ACL-deficient knees and in TKAs that sacrifice the ACL.26 Our results showing the posterior translated positions of the femur in extension and the paradoxical anterior femoral movement during mid-flexion could possibly be explained by the same mechanism.
Triathlon is designed to allow for ±10° of rotation in hyperextension and extension27 and to accommodate up to 20° of internal/external rotation in the deep flexion. The present result showed that range of axial rotation and rotational position were within an allowable range of its design concept in both CR and CS.
Also, we hypothesized that a raised anterior lip design would offer a potential minimization of the paradoxical movement and provide joint stability according to its design concept.
With regard to AP translation of femorotibial nearest point, we did not observe knee kinematics, demonstrating that the anterior movement was statistically different between the two designs in mid-flexion. In other words, these results indicated that the increased anterior lip could not control medial anterior sliding in the CS insert.
This study also showed that there was no significant difference between the amount of femoral rollback in CR and CS during deep knee flexion. This could be related to the constraints of the prosthesis design which posterior part is not flat but rather has a raised posterior lip.
From the above kinematic results, the CR TKA could be converted to the CS TKA with PCL sacrifice because of insufficiency of PCL or difficulty of surgery without significantly changing the kinematics of the knee. Otherwise, the PS TKA would be the better option because it might be effective to reduce the paradoxical movement and provide stability in mid-flexion ranges.
This study has a number of limitations. First, the number of patients was relatively small. However, some previous reports have analyzed 10–20 knees.11, 12, 13, 14, 15, 16 Second, we have measured kinematics of only deep knee flexion motion. We are now undergoing analysis of many functional activities (e.g., walking, stair up and down, sitting on and rising from a chair, etc.) to investigate factors affecting kinematics of TKA. Additionally, the outcomes might be affected by other surgical factor such as components' alignment within the bones and soft-tissue balance. Future studies should examine surgical factors influencing the TKA kinematics.
In conclusion, this study presented the detailed in vivo kinematics of sequential deep knee flexion and compared kinematics between the CR and CS inserts in the same single-radius CR TKA design. Paradoxical anterior femoral movement was shown until 100° flexion in both CR and CS. These results indicated that the increased anterior lip could not control anterior sliding. Moreover, our kinematic results will support for surgeons to decide which to choose and suggest that the CR TKA could be converted to the CS or PS TKA with PCL sacrifice because of insufficiency of PCL or difficulty of surgery.
Declaration of competing interest
The authors have no conflicts of interest relevant to this article.
Acknowledgments
This work was supported by the JSPS KAKENHI Grant Number 18K10839 by Ministry of Education, Culture, Sports, Science and Technology, Japan.
References
- 1.Sloan M., Premkumar A., Sheth N.P. Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am. 2018;100(17):1455–1460. doi: 10.2106/JBJS.17.01617. [DOI] [PubMed] [Google Scholar]
- 2.NiemeläInen M.J., MäKelä K.T., Robertsson O. Different incidences of knee arthroplasty in the Nordic Countries. Acta Orthop. 2017;88(2):173–178. doi: 10.1080/17453674.2016.1275200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rodricks D.J., Patil S., Pulido P., Colwell C.W., Jr. Press-fit condylar design total knee arthroplasty. Fourteen to seventeen-year follow-up. J Bone Joint Surg Am. 2007;89(1):89–95. doi: 10.2106/JBJS.E.00492. [DOI] [PubMed] [Google Scholar]
- 4.Vessely M.B., Whaley A.L., Harmsen W.S., Schleck C.D., Berry D.J. The Chitranjan Ranawat Award: long-term survivorship and failure modes of 1000 cemented condylar total knee arthroplasties. Clin Orthop Relat Res. 2006;452:28–34. doi: 10.1097/01.blo.0000229356.81749.11. [DOI] [PubMed] [Google Scholar]
- 5.Bourne R.B., Chesworth B.M., Davis A.M., Mahomed N.N., Charron K.D. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468(1):57–63. doi: 10.1007/s11999-009-1119-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bourne R.B., Chesworth B., Davis A., Mahomed N., Charron K. Comparing patient outcomes after THA and TKA: is there a difference? Clin Orthop Relat Res. 2010;468(2):542–546. doi: 10.1007/s11999-009-1046-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nakahara H., Okazaki K., Mizu-Uchi H. Correlations between patient satisfaction and ability to perform daily activities after total knee arthroplasty: why aren't patients satisfied? J Orthop Sci. 2015;20(1):87–92. doi: 10.1007/s00776-014-0671-7. [DOI] [PubMed] [Google Scholar]
- 8.Andriacchi T.P., Galante J.O., Fermier R.W. The influence of total knee replacement design on walking and stair-climbing. J Bone Joint Surg Am. 1982;64(9):1328–1335. [PubMed] [Google Scholar]
- 9.Uvehammer J., Kärrholm J., Brandsson S. In vivo kinematics of total knee arthroplasty: flat compared with concave tibial joint surface. J Orthop Res. 2000;18(6):856–864. doi: 10.1002/jor.1100180603. [DOI] [PubMed] [Google Scholar]
- 10.Dennis D.A., Komistek R.D., Scuderi G.R., Zingde S. Factors affecting flexion after total knee arthroplasty. Clin Orthop Relat Res. 2007;464:53–60. doi: 10.1097/BLO.0b013e31812f785d. [DOI] [PubMed] [Google Scholar]
- 11.Tamaki M., Tomita T., Watanabe T., Yamazaki T., Yoshikawa H., Sugamoto K. In vivo kinematic analysis of a high-flexion, posterior-stabilized, mobile-bearing knee prosthesis in deep knee bending motion. J Arthroplasty. 2009;24(6):972–978. doi: 10.1016/j.arth.2008.06.012. [DOI] [PubMed] [Google Scholar]
- 12.Okamoto N., Breslauer L., Hedley A.K., Mizuta H., Banks S.A. In vivo knee kinematics in patients with bilateral total knee arthroplasty of 2 designs. J Arthroplasty. 2011;26(6):914–918. doi: 10.1016/j.arth.2010.07.018. [DOI] [PubMed] [Google Scholar]
- 13.Shimizu N., Tomita T., Yamazaki T., Yoshikawa H., Sugamoto K. The effect of weight-bearing condition on kinematics of a high-flexion, posterior-stabilized knee prosthesis. J Arthroplasty. 2011;26(7):1031–1037. doi: 10.1016/j.arth.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 14.Yoshiya S., Matsui N., Komistek R.D., Dennis D.A., Mahfouz M., Kurosaka M. In vivo kinematic comparison of posterior cruciate-retaining and posterior stabilized total knee arthroplasties under passive and weight-bearing conditions. J Arthroplasty. 2005;20(6):777–783. doi: 10.1016/j.arth.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 15.Horiuchi H., Akizuki S., Tomita T., Sugamoto K., Yamazaki T., Shimizu N. In vivo kinematic analysis of cruciate-retaining total knee arthroplasty during weight-bearing and non-weight-bearing deep knee bending. J Arthroplasty. 2012;27(6):1196–1202. doi: 10.1016/j.arth.2012.01.017. [DOI] [PubMed] [Google Scholar]
- 16.Fujimoto E., Sasashige Y., Tomita T., Iwamoto K., Masuda Y., Hisatome T. Significant effect of the posterior tibial slope on the weight-bearing, midflexion in vivo kinematics after cruciate-retaining total knee arthroplasty. J Arthroplasty. 2014;29(12):2324–2330. doi: 10.1016/j.arth.2013.10.018. [DOI] [PubMed] [Google Scholar]
- 17.Nabeyama R., Matsuda S., Miura H. Changes in anteroposterior stability following total knee arthroplasty. J Orthop Sci. 2003;8(4):526–531. doi: 10.1007/s00776-003-0654-6. [DOI] [PubMed] [Google Scholar]
- 18.Dennis D.A., Komistek R.D., Mahfouz M.R., Haas B.D., Stiehl J.B. Multicenter determination of in vivo kinematics after total knee arthroplasty. Clin Orthop Relat Res. 2003;416:37–57. doi: 10.1097/01.blo.0000092986.12414.b5. [DOI] [PubMed] [Google Scholar]
- 19.Jacobs W.C., Clement D.J., Wymenga A.B. Retention versus removal of the posterior cruciate ligament in total knee replacement: a systematic literature review within the Cochrane framework. Acta Orthop. 2005;76(6):757–768. doi: 10.1080/17453670510045345. [DOI] [PubMed] [Google Scholar]
- 20.Zuffi S., Leardini A., Catani F., Fantozzi S., Cappello A. A model-based method for the reconstruction of total knee replacement kinematics. IEEE Trans Med Imag. 1999;18(10):981–991. doi: 10.1109/42.811310. [DOI] [PubMed] [Google Scholar]
- 21.Yamazaki T., Watanabe T., Nakajima Y. Improvement of depth position in 2-D/3-D registration of knee implants using single-plane fluoroscopy. IEEE Trans Med Imag. 2004;23(5):602–612. doi: 10.1109/tmi.2004.826051. [DOI] [PubMed] [Google Scholar]
- 22.Yamazaki T., Watanabe T., Nakajima Y. Visualization of femorotibial contact in total knee arthroplasty using X-ray fluoroscopy. Eur J Radiol. 2005;53(1):84–89. doi: 10.1016/j.ejrad.2003.09.018. [DOI] [PubMed] [Google Scholar]
- 23.Grood E.S., Suntay W.J. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng. 1983;105(2):136–144. doi: 10.1115/1.3138397. [DOI] [PubMed] [Google Scholar]
- 24.Victor J., Banks S., Bellemans J. Kinematics of posterior cruciate ligament-retaining and -substituting total knee arthroplasty: a prospective randomised outcome study. J Bone Joint Surg Br. 2005;87(5):646–655. doi: 10.1302/0301-620X.87B5.15602. [DOI] [PubMed] [Google Scholar]
- 25.Baier C., Springorum H.R., Götz J. Comparing navigation-based in vivo knee kinematics pre- and postoperatively between a cruciate-retaining and a cruciate-substituting implant. Int Orthop. 2013;37(3):407–414. doi: 10.1007/s00264-013-1798-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Victor J., Bellemans J. Physiologic kinematics as a concept for better flexion in TKA. Clin Orthop Relat Res. 2006;452:53–58. doi: 10.1097/01.blo.0000238792.36725.1e. [DOI] [PubMed] [Google Scholar]
- 27.Bhimji S., Kester M., Schmalzried T. Rotational constraint of posterior-stabilized total knee prostheses. J Knee Surg. 2008;21(4):315–319. doi: 10.1055/s-0030-1247838. [DOI] [PubMed] [Google Scholar]