Abstract
Local and remote complications can be observed in hip prosthesis failures associated with metallosis. Structural changes in the periprosthetic bone and soft tissues may not always be precisely assessed preoperatively due to metal artifacts. The unpredictability of the damage extension, potentially leading to complex and insidious surgeries, requires the availability of alternative surgical plan(s) for the reconstruction of the joint. The aim of the study is to present and analyze, with the literature data support, practical tips for the revision of the prosthetic components, the management of ARMD and of intraoperative complications in the unusual scenario of metallosis.
Keywords: Metallosis, Hip revision surgery complications, ARMD, Pseudotumor, Femoral stem revision, Acetabular cup revision
1. Introduction
Total hip arthroplasty is a widespread and highly successful orthopedic procedure. The constant increase in the number of total hip arthroplasties is associated with the substantial burden of revision total hip arthroplasty. The cause of a prosthetic hip failure influences the prognosis of revision surgery and, to some extent, can determine local and sometimes remote pathological manifestations. In hip prosthesis failures associated with metallosis, local complications of varying degrees can be observed, ranging from small asymptomatic soft tissue lesions to dramatic osteolysis, necrotic processes and solid or cystic pseudotumors, which can cause secondary pathological effects (often related to mass effect).1,2 Structural changes in the periprosthetic bone and soft tissues may not always be precisely assessed preoperatively because of the magnitude of metal artifacts in diagnostic imaging. The unpredictability of the damage extension requires the availability of alternative surgical plan(s) and extra implants for reconstruction on both the acetabular and femoral sides, potentially leading to unexpectedly complex and insidious surgeries even for experienced surgeons. This study aims to report and analyze the surgical strategies adopted in a case series of 15 hip prosthetic failures in metallosis.
2. Materials and methods
A retrospective study was conducted recruiting an original consecutive series of patients who underwent THA revision surgeries in the Orthopedic Unit of the University of Sassari, Italy, between May 2013 and May 2019. Initially, all revision procedures were considered.
From the total series of 196 THA revisions, the study was focused on 15 cases (both MoM and MoP bearings) in which the indication for revision was mainly due to metallosis. Thirteen cases were included on account of one symptomatic pseudotumor visible to instrumental images (MRI, CT, ultrasound) and later confirmed as an adverse reaction to metal debris (ARDM); two other MoM THA revision cases were included since an ARDM (confirmed on histological examination) located within the femoral canal and not extended in the periarticular soft tissues was intraoperatively highlighted. 181 patients were excluded from the study in the lack of metal debris production or macroscopic histological changes in the periprosthetic tissues found on the revision surgery. Five cases out of 181 were MoM THA revisions for causes other than metallosis (3 MoM THA revisions for traumatic non-pathological periprosthetic fracture and 2 revisions in early failure for aseptic loosening: 1 acetabular cup migration, 1 subsident undersized femoral stem; in none of these 5 cases macroscopic or microscopic signs of reaction to metals debris or radiographic signs of osteolysis were found, except for a periprosthetic radiolucent line around the subsident stem; no pathological levels of metal ions in the blood of these 5 patients were detected).
Patients, implants and surgical characteristics were collected from medical records. Data were reviewed by 3 investigators (F.E., A.F., R.M.) not involved in the original patient care. Patients' characteristics included first diagnosis, gender, age, BMI, and affected side. Implant characteristics collected were: implants’ model and bearing surface. The surgical assessment included indication for revision surgery, clinical signs and symptoms, radiographic assessment of component stability and positioning, bone loss/osteolytic lesions, intraoperative findings, complications, and solutions adopted.
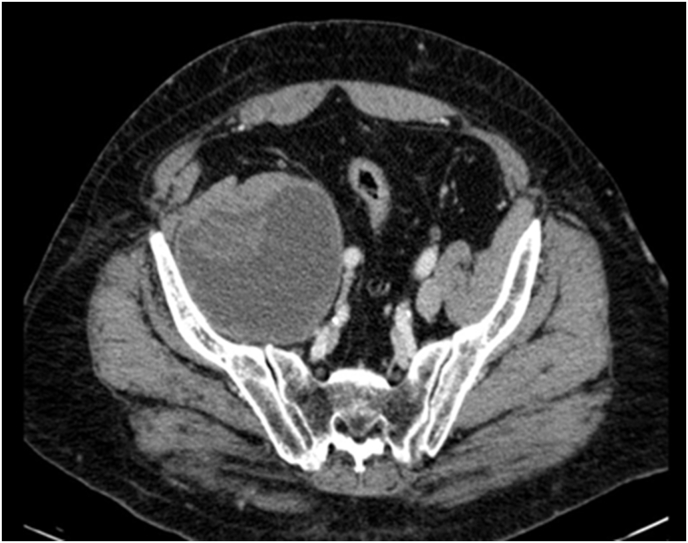
The radiologic evaluation was made through the systematic assessment of preoperative anteroposterior radiographs of the pelvis and frog-leg view; cross-sectional imaging (MRI and CT scan) were used to assess major osteolytic areas and soft tissue lesions to discriminate solid, cystic (Fig. 1) and multicystic pseudotumors; ultrasounds were mainly used to evaluate superficial inguinal and peritrochanteric region and deep intrapelvic lesions, but also to perform ultrasound-guided drainage from pelvic pseudotumors. Preoperative C-reactive protein (CRP) and white blood cell count (WBC) were used as a routine screening tool for infection in all patients. For postoperative assessment, anteroposterior pelvic radiographs were also digitally recorded. A widespread spreadsheet software (Microsoft Excel for Windows) was used to analyze images and measure leg length discrepancy and vertical and lateral offset from the hip joint center (HJC). The physiological HJC was determined in the geometrical center of the opposite unaffected hip; in patients with a bilateral pathological deviation of the rotational center (both hips affected or bilateral THA), the hip center was determined following Fessy's method.3 Component loosening and location of bone resorption and osteolysis were radiographically evaluated according to DeLee and Charnley4 for acetabular side and Gruen et al.5 for the femoral side. The acetabulum and femur abnormalities were described intraoperatively in accordance, respectively, with Paprosky6 et al. and D'antonio7 et al. classifications. Regarding surgical management, the type of revision prosthesis, the implants' additional fixation (screws, augments) and osteosynthesis systems (plates, cerclages), the use of bone substitutes or grafts, the duration of the surgery, the surgical procedure associated (e.g. pelvic drainage) and the intraoperative complications were recorded and evaluated.
Fig. 1.
Intrapelvic fluid collection displacing iliac vessels.
All acetabular screws were fixed in safe areas in accord with Wasielewski's acetabular-quadrant system theory.8
An ad hoc electronic form was used to collect demographic, epidemiological, and clinical variables. Qualitative variables were described with absolute and relative (percentage) frequencies, whereas quantitative variables were summarized with means and standard deviations (SD).
3. Results
Patients and first implants characteristics are summarized in Table 1, Table 2.
Table 1.
Patients’ characteristics.
| Male, n (%) | 6 (40) |
|---|---|
| Mean (SD) age (years) | 71.8 (7.5) |
| Mean (SD) BMI (Kg/m2) | 26.6 (4.6) |
| Side, n (%) | Right 11 (73.3) |
| Left 4 (26.7) |
Table 2.
Primary THA indications and implant features; AVN avascular necrosis.
| THA indication, n (%) | Coxarthrosis | 11 (73.3) |
| Post-traumatic coxarthrosis | 2 (13.3) | |
| Hip dysplasias | 1 (6.7) | |
| AVN of femoral head | 1 (6.7) | |
| Bearing surfaces, n (%) | MoM | 12 (80) |
| MoP | 3 (20) | |
| Mean (range) implant survivorship (years) | MoM | 6.9 (2–10) |
| MoP | 18.3 (14–22) | |
| Tot. | 9.2 (2–22) |
In all the selected cases, uncemented prosthetic components were used during primary total hip replacement. In 12 cases the coupling was MoM, in 3 cases MoP, in 1 of which the constrained tripolar cup presented a CoP inner coupling and a MoP outer coupling. In MoP implants, wear of polyethylene generated direct contact between metal components leading to a rapid worsening of the clinical symptoms related to the formation of large pseudotumors (in two cases with intrapelvic localization and in one with periarticular localization).
All patients complained of groin pain and coxalgia but in two cases remote signs predominated due to systemic cobalt intoxication, and mass effect producing constipation caused by an ALVAL with a large retroperitoneal cystic collection. In 15 out of 15 cases (100%) an ARMD was found with a pleomorphic pseudotumoral manifestation. Intraoperative cultures were negative for infection in all cases. At the time of revision surgery, 5 acetabular cups (including the 3 MoP implants) and 5 stems (2 MoP implants) were loosened; in all these cases severe periprosthetic osteolysis was evident. In one case, the periprosthetic osteolysis caused a spontaneous fracture of the greater trochanter and stem loosening. Bone loss locations in different Gruen regions and DeLee-Charnley areas, as well as D'Antonio's grading and Paprosky's classification, are shown in Table 3, Table 4.
Table 3.
Surgical management of femoral stem revision: cases (C) in alphabetical order. Femoral osteolysis refers to the radiographical assessment of femoral remodelling/osteolysis in Gruen zones, in brackets when bone loss is minimal. Fem Grad refers to femoral grading in accordance with the D'Antonio grading system. Stem revision cementless and monoblock unless otherwise stated, NO stem was not replaced, TFS long tapered fluted stem, SWS single wedge stem, M modular; revision stem length expressed in mm in brackets; bone filler * Mg-HA magnesium doped hydroxyapatite in granules or in paste. ETO extended trochanteric osteotomy.
| C | Femoral osteolysis | Fem Grad |
Stem Stability + (taper corrosion) | Stem revision Length (mm) |
Notes |
|---|---|---|---|---|---|
| 1 | (1),(7) | I | Well-fixed+ (no) | NO | Proximal stress shielding |
| 2 | 1,(6),7 | II | Loosened+ (yes) | TFS,(240) * | Intraoperative femoral cortex perforation |
| 3 | 1,2,6,7 | II | Loosened+ (yes) | TFS,(240) * | Intraoperative intertrochanteric fracture fixed with Ethibond and distal cortex perforation |
| 4 | 1,(7) | II | Loosened+ (yes) | TFS,(240) | |
| 5 | 1,7 | I | Well-fixed+ (yes) | TFS,(190) | Intraoperative isolated trochanteric fracture fixed with Ethibond; prophylactic femoral cerclage |
| 6 | 1,(2),(6),7 | II | Loosened+ (yes) | TFS,M,(240) | Preoperative spontaneous greater trochanter fracture |
| 7 | 1,(7) | I | Well-fixed+ (yes) | TFS,(190) | |
| 8 | 1,7 | I | Well-fixed+ (no) | NO | Proximal stress shielding |
| 9 | 1 | I | Well-fixed+ (no) | NO | |
| 10 | 1,2,(3),(5),6,7 | II | Loosened+ (yes) | TFS,(240) * | Femoral ectasia and strong pedestal |
| 11 | 1 | I | Well-fixed+ (yes) | TFS,M (235) | Pedestal |
| 12 | 1,2,(6),7 | II | Well-fixed+ (yes) | TFS,(240) | Intraoperative intertrochanteric fracture fixed with Ethibond |
| 13 | 1,2,(6),7 | II | Well-fixed+ (yes) | TFS,(190) | Intraoperative intertrochanteric fracture fixed with Ethibond |
| 14 | 1,2,(6),7 | II | Well-fixed+ (yes) | TFS,M,(240) | Femoral proximal stenosis and slight angular deformity, ETO + cable plate |
| 15 | 1,(7) | I | Well-fixed+ (yes) | SWS,(120) |
Table 4.
Surgical management of acetabular cup revision: cases (C) categorized accordingly with Paprosky classification. Bone loss: intraoperative assessment according to the Paprosky system. Gruen: radiographical assessment of periacetabular osteolysis according with Gruen zones, * retroacetabular stress-shielding. Cup stability and integrity: bearing surface damaged and MoM coupling unless otherwise stated, intact: mirror-polished bearing surface. Cup replacement: HC hemispherical cup, the difference in cup diameter (in millimeters) before and after revision; the number of screws is provided between brackets, screws are fixed in posterior quadrants unless otherwise stated, AI screw in the anterior-inferior quadrant. Bone substitutes: Mg-HA Magnesium doped hydroxyapatite, Coll-(Mg-HA) collagen-Mg-HA composite scaffold; struct structured, autolog autologous, homolog homologous. Notes: COR center of rotation. OL off-label.
| Bone loss | C | Gruen | Cup stability and integrity | Cup replacement (screws) | Bone substitutes | Notes |
|---|---|---|---|---|---|---|
| 1 | 5 | none | stable intact | / | / | OL: Primary cup + DMA |
| 6 | * | stable intact | / | / | OL: Primary cup + DMA | |
| 7 | * | stable | HC +6 (2) | / | Remarkable cup lateralisation before revision. | |
| 8 | * | stable intact | / | / | OL: Primary cup + DMA | |
| 11 | none | stable | HC+2 (3) | / | / | |
| 14 | none | stable intact | / | / | OL: Primary cup + DMA | |
| 2a | 1 | 1,3 | stable | HC +4(2) | / | Remarkable cup migration directed superiorly with intact superior acetabular rim |
| 2 | 1,3 | loosened MoP | HC -2 (5) | Coll-(Mg-HA) | Revision with undersized cup and COR elevation | |
| 2c | 4 | 1*,2,3 | stable | HC +0(3 + 1 AI) | Mg-HA granules, Coll-(Mg-HA) | / |
| 9 | 2,3 | loosened | HC +4 (3) | / | Coxa profunda | |
| 10 | 2,3 | stable | HC +2 (2) | Mg-HA granules, Coll-(Mg-HA) | / | |
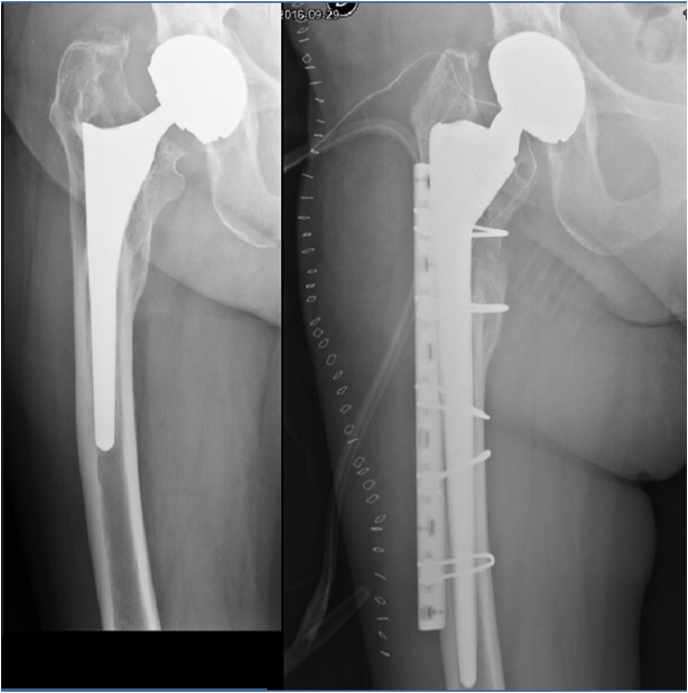
| 12 | 1,2 | loosened MoP | HC -10 (2) | Mg-HA granules, Coll-(Mg-HA) | Undersized cup with elevated COR was implanted (Fig. 4) | |
| 3a | 3 | 1,2,3 | loosened MoP | HC +0 (5) | struct autolog bone graft, Mg-HA granules | / |
| 13 | 1,2,3 | loosened | HC +4 (3) | struct autolog bone graft, Mg-HA granules, Coll-(Mg-HA) | Early failure of the structured graft. | |
| 15 | 1,2,3 | stable | HC +6, 3 iliac winglets and caudal hook (4) | struct and morcelized homolog bone graft | Hip dysplasia; intraoperative fracture of posterior column |
3.1. Femoral stem revision
Femoral abnormalities and surgical management of stem revision are summarized in Tab 3.
In 14/15 femurs (93,3%) an obvious proximal femoral area of bone resorption was found. One patient (early cup and prosthetic head revision) showed a minimal loss of bone density (compatible with stress shielding) in Gruen zones 1 and 7 (tab 3 case 1). In all cases, granulomatous tissue related to the ARMD filled the osteolytic areas. In three patients with minimal loss of bone density and no cavitary defects on the femoral side, a stable stem with taper not visibly damaged was not replaced and a partial revision was performed, changing only the cephalic component in 1 case (by switching to dual mobility), and replacing head and cup in two cases (and switch to a MoP coupling). In 12/15 cases the stem was revisioned. In 5 cases the stems were loosened (2 of these were osteointegrated at the very distal end, with the tip fixed in a strong pedestal).
In all stem revisions except one, a long (190–240 mm) cementless tapered fluted stem (2 modular and 8 monoblock Redapt, Smith and Nephew; 1 modular Restoration Stryker) was used to bypass the proximal osteolytic area (Fig. 2). In one case a single wedge stem commonly used in primary surgery was implanted (Accolade Stryker). In all cases, an excellent meta-diaphyseal or diaphyseal stability was obtained. The proximal bone defects, in the presence of an evident metaphyseal-diaphyseal mismatch, were filled with biomimetic bone substitutes (Mg-doped hydroxyapatite in granules or in paste, SINTlife, Finceramica). In this series, all bone substitutes used in the femoral side had a filling function without providing any mechanical support.
Fig. 2.
Cementless tapered fluted stems monoblock (a) and modular (b, c) were used to bypass the proximal osteolytic area; bone substitutes used in the femoral side did not provide any mechanical support.
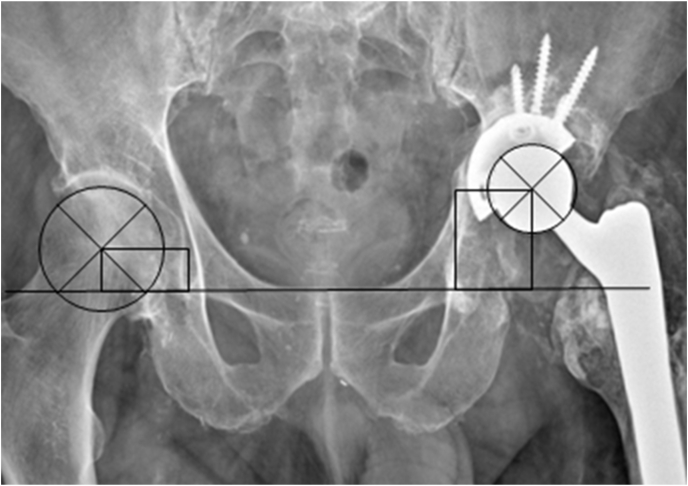
3.2. Acetabular CUP revision
Table 4 reports periacetabular bone loss assessment and surgical management of acetabular components. Patients are grouped according to bone loss as in Paprosky's classification. Among the 6 Paprosky's grade I patients, four stable cups with a mirror-polished internal surface were not replaced and a mixed THA was assembled with an off-label cup-dual mobility head (MDM/ADM, Stryker) coupling (in 3 cases in association with the femoral stem revision). A hemispherical cup (HC) fixed with screws (2–5) was implanted in all revisions of the acetabular component. As reported in Tab 4 one HC had iliac winglets and a caudal hook. All screws (except one fixed in the superior pubic ramus (Fig. 3)) were fixed in posterior quadrants.
Fig. 4.
Undersized cup with a center of rotation (COR) 5 mm medial and 25 mm proximal to ideal COR to get the full acetabular coverage in a severe periacetabular osteolysis (Paprosky 2c).
Fig. 3.
Hemispherical multihole cup fixed with 3 iliac and 1 pubic screws; a radiotransparent collagen-Mg-HA composite scaffold fills the gap and aims to facilitate the osteogenesis and osseointegration of the implant.
Synthetic bone grafts were used in all revisions of the acetabular component for Paprosky grade II bone defects (except in one case graded IIa, in which no graft was used). Structured bone grafts were used to augment acetabular defects in patients with a grade IIIa bone loss.
3.3. ARMD management
Macroscopic anatomy findings revealed unequivocal aspects of metallosis in all cases.
In 2/15 cases a friable collection mainly circumscribed inside the femur and minimally extended in the intra-articular space was found, not associated with an organized periarticular mass (Table 5). In 13 cases pseudotumors in different locations were observed: mainly intrapelvic localization in 3 cases, prevalent periarticular localization in 7 cases, and with both extensive intrapelvic and periarticular diffusion in 3 cases.
Table 5.
Surgical management of the pseudotumor: cases (C) listed by location of the ARMD. Site: A periarticular, B intrapelvic retroperitoneal, C mainly circumscribed inside the femur. An accurate debridement of the reactive and necrotic tissue, associated with fluid drainage when a cystic cavity was present, was performed in all cases.
| ARMD site | C | ARMD type | Perioperative and intraoperative notes |
|---|---|---|---|
| A | 1 | Solid + Cystic | |
| A | 2 | Solid | |
| A | 5 | Solid + Cystic | |
| A | 6 | Solid + Cystic | Aggressive granulomatosis, spontaneous greater trochanter fracture associated with apparent acute loosening of the stem (asymptomatic patient before fracture) |
| A | 7 | Solid + Cystic | |
| A | 9 | Cystic | Ultrasound guided percutaneous drainage from a relapsing aseptic fluid collection (3 months before revision surgery); widespread fibrosis and muscle-fascial scar adhesion. |
| A | 14 | Solid + Cystic | |
| A + B | 3 | Solid + Cystic | Retroperitoneal intrapelvic fluid collection spontaneously drained from acetabular bone defects |
| A + B | 11 | Solid + Cystic | Retroperitoneal intrapelvic fluid collection spontaneously drained from acetabular bone defects |
| A + B | 15 | Solid + Cystic | Severe degeneration and necrosis of abductors tendons; ilioinguinal approach to manage large retroperitoneal intrapelvic semi-cystic pseudotumor adherent to the left iliac vessels. |
| B | 8 | Solid + Cystic | Misleading clinical manifestations of abdominal pain; diagnostic ultrasound guided percutaneous drainage from an intrapelvic semi-cystic pseudotumor (ALVAL); ilioinguinal approach to manage the semi-cystic pseudotumor at time of partial THA revision. |
| B | 12 | Cystic | Retroperitoneal intrapelvic fluid collection spontaneously drained from acetabular bone defects |
| B | 13 | Solid + Cystic | Repeated ultrasound guided percutaneous drainage from an intrapelvic relapsing aseptic fluid collection before THA revision (being the correlation with ARMD unrecognized initially); ilioinguinal approach to manage the semi-cystic pseudotumor at time of THA revision. |
| C | 4 | (Solid) | |
| C | 10 | (Solid) |
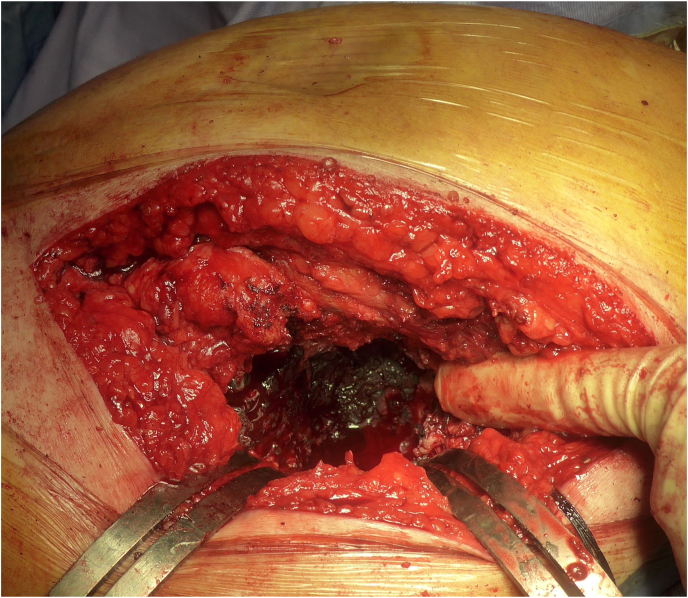
In most cases the liquid collections were drained through the surgical approach used for the prosthetic revision; in some cases, intrapelvic fluid collection spontaneously drained through bone defects after or during cup removal; in two cases, with a spreading lesion along the psoas sheath, additional ilioinguinal access was performed for drainage and curettage of large retroperitoneal pseudotumors adherent to the iliac vessels. Histological examination revealed a cellular infiltrate of macrophages and giant cells (foreign body granulomas-like) with several fibroblastic reactive zones in a context of altered connective tissues. The most frequent findings were: foam-like cytoplasmic histiocyte accumulations, widespread black pigmentation (hemosiderin-like), metal particles and extracellular metal deposits, intracytoplasmic debris in multinuclear giant cells. Less frequently a lymphocytic dominated reaction (ALVAL) depicted an immune-mediated type IV delayed hypersensitivity reaction. Fibrosis-surrounded necrotic tissue with lymphohistiocytic infiltrate and hemosiderin-like pigments deposits and small perivascular lymphocyte infiltrate was also found. In MoP THA revision, areas characterized by the infiltration of both metal and polyethylene have been described, with foamy histiocytes containing metallic debris and giant polynucleated cells containing threadlike particles, refractive under polarized light. In all cases, an accurate debridement of the peritrochanteric reactive and necrotic tissue was performed, as well as surgical removal of fibrosis and muscle-fascial scar adhesions (see Fig. 5, Fig. 6).
Fig. 5.
Local aspects of metallosis: brownish fluid collection and dark-grayish granulomatous tissue.
Fig. 6.
Local aspects of metallosis: brownish fluid collection and dark-grayish granulomatous tissue.
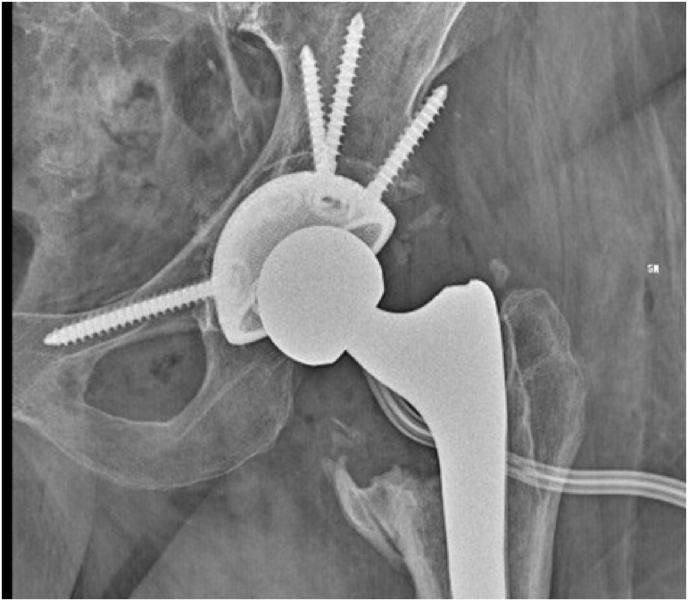
3.4. Intraoperative complications
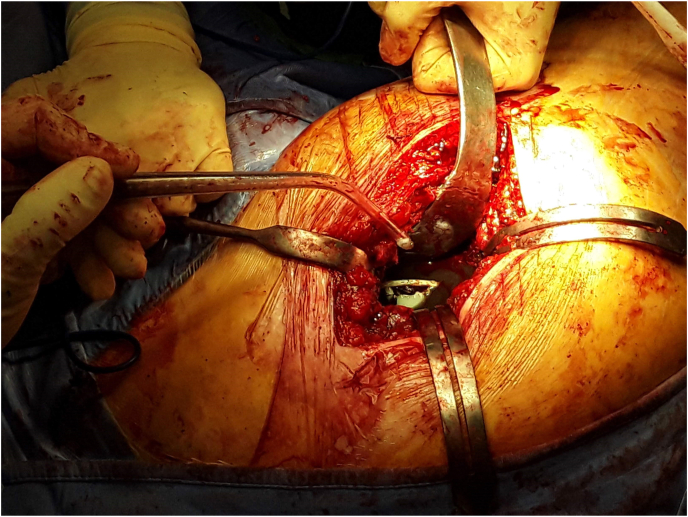
In one patient with proximal stenosis (due to an old fracture) and a slight angular deformity of the femur, an extended trochanteric osteotomy (ETO) was made to remove a well-fixed stem. Fixation of ETO was achieved with a cable-plate (Accord, Smith and Nephew 200 mm + 5 cerclage) and a long cementless modular tapered fluted stem (Redapt 16 × 240mm, high offset neck) was implanted (Fig. 7).
Fig. 7.
Proximal stenosis and slight angular deformity of the femur (a), cable-plate and long cementless modular tapered fluted stem (b).
An intraoperative intertrochanteric pathological fracture (associated with a cavitary or segmental-cavitary combined defect in the metaphyseal region) occurred during removal of the femoral stem in 3 cases (cases 3, 12, 13) and an isolated fracture of the greater trochanter occurred during femoral reaming in one more case. In all cases, after the implantation of the femoral stem, the fragments were reduced and fixed with a non-absorbable, braided Polyester Suture (Ethibond). When it was necessary to pass the sutures, holes were made with a K-wire on the fragments and the intact femur. The number of sutures varied according to the size and instability of the fracture fragments. In a single case of an iatrogenic trochanteric fracture produced during the reaming of the femur, before the stem implantation, a prophylactic cerclage was made to prevent crack propagation.
An intraoperative iatrogenic perforation of the femoral cortex occurred in 2 cases (during the removal of the stem in one case, and during the reaming through the bone pedestal in the second case); in both cases, no additional surgical solutions were used, as the long cementless stem bypassed the cortical defect.
A fracture of the posterior column of the acetabulum occurred during cup removal in 1 case (case 15: woman, 72 years old, Paprosky's grade IIIa, hip dysplasia); a hemispherical cup with 3 iliac winglets and caudal hook (Delta Revision TT cup, Lima) fixed with 4 screws in posterosuperior quadrant (3 extra-acetabular and 1 intra-acetabular iliac screws), was implanted after bone defects augmentation with homologous morselized and structured bone grafting.
In this series, although some acetabular screws crossed the far bone cortex, any neurovascular lesion was reported.
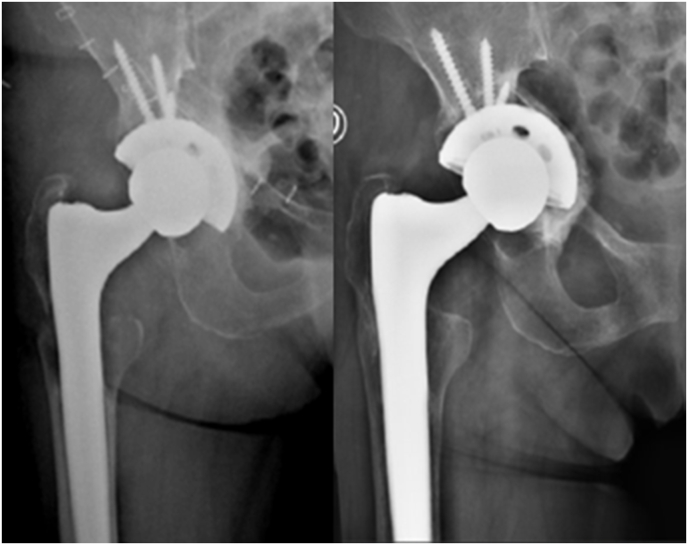
3.5. Outcomes
Radiographic and clinical assessment are summarized in Table 6. Following revision surgery, there were no cases of re-revision, recurrence of metallosis or ARMD related symptoms at the last follow-up (mean follow-up 3 years, range 1–9 years). All peri- and the intra-operative trochanteric fractures healed. The radiographic assessment showed in all cases a good bone graft incorporation but in two cases the bone substitutes partially invaded the intrapelvic pseudotumoral cystic cavity without further diffusion or complications. Two patients with massive bone deficit (Paprosky IIIa) and severe soft tissue degeneration reported major complications: one acute onset of nerve palsy, involving the peroneal division of the sciatic nerve, resulted in a permanent deficit (foot drop) on the treated limb; one early failure (within the first postoperative month) of the structured graft. The comparison of the radiographic control before and after weight-bearing showed a rotation of the acetabular cup around the sagittal axis with a cup inclination increase of about 16° (from 39° to 23°) (Fig. 8). In the latter case, after non-operative treatment and protected weight-bearing for 8 weeks, the acetabular inclination did not further change and the periacetabular bone appeared consolidated at the radiologic assessment at 6 and 12 months; at 2 years’ follow-up the patient complained of moderate pain but serious functional limitations (partially due to severe comorbidities, inter alia severe vascular dementia), being able to walk only in the house using a walker.
Table 6.
Radiographic and clinical assessment at mean 3 years follow-up: cup vertical and lateral offset report the distance of the prosthetic center of rotation from the physiological hip joint center, HHS Harris Hip Score.
| Mean (SD) cup abduction angle | Mean (SD) cup vertical offset (mm) | Mean (SD) cup lateral offset (mm) | Mean (SD) leg length discrepancy (mm) | Mean (SD) HHS |
|---|---|---|---|---|
| 47.1° (6.2) | 6.8 (9.3) | −1.8 (4.1) | 1.0 (14.9) | 75.9 (13.2) |
Fig. 8.
Rotation of the acetabular cup with a cup inclination increase of about 16°; after non-operative treatment and protected weight-bearing for 8 weeks, the acetabular inclination did not further change and the periacetabular bone appeared consolidated at the radiologic assessment at 6 and 12 months.
Last Harris hip score assessment showed: 3 poor (<70), 4 fair (70–79), 7 good (80–89) and 1 excellent result (90–100), with a mean (SD), score on HHS pain scale of 38.1 (5.3) (44 is the best possible pain score indicating no pain).
4. Discussion
In our revision series, we preferred the postero-lateral approach to the hip because of its familiarity and its extensile nature.
On the femoral side a granulomatous tissue related to the ARMD filled the osteolytic areas typically involving the great trochanter and the Gruen zones 1-7-2-6, progressing in an apparently centrifugal direction from the osteotomy site and the modular junctions. We hypothesize that the osteolytic process induced by metallic debris and the stress shielding can constantly amplify each other. ARMD related osteolysis can cause an alteration of the mechanical environment and a worsening of stress shielding which is determined by strain distribution. Anyway, due to the extreme fragility of the proximal femur, the decision was to perform a careful curettage of the bone and, in most of the cases, to bypass the proximal osteolytic area looking for diaphyseal stability by revisioning the femoral component with a long revision stem. The aim of the femoral implant revision was to obtain an adequate primary stability with a stem that “fixes as proximal as possible and as distal as necessary” to say it like Paul Böhm and Oliver Bischel.9 Surgical purpose was to bypass femoral defects, manage the leg length, the soft tissue tension, the neck orientation and the offset. According to the literature, in one case with minimal loss of bone density (Gruen 1–7, case 15) a single wedge stem was implanted.10 In 11/12 stem revisions a cementless tapered fluted stem (3 modular e 8 monoblock) was used to bypass the osteolytic area11; we preferred monoblock stems for the theoretical, although controversial, advantage of reducing the risk of stem fracture and fretting corrosion associated with modular junctions12,13 According to Bianchi et Al. we performed an impaction grafting technique (with magnesium doped hydroxyapatite in granules or paste) to improve bone stock in proximal femoral osteolytic cavitations without seeking any further mechanical supporting functions.14 Extreme caution is always necessary during the surgical dislocation of the replaced hip, the removal of the pseudotumoral mass and soft tissues, the removal of the stem and the preparation of the femoral canal because the creation of torque and high peak forces in a weak femur can cause an iatrogenic fracture. The bony pedestal drilling requires particular attention not to cause cortical perforations and is most safely performed with intraoperative fluoroscopy. The extended trochanteric osteotomy (ETO) is a safe and useful procedure for removing a fixed stem. The ETO does not appear to affect the outcomes of a tapered fluted distal fixation stem regardless of whether the osteotomy consolidates or not.15
In four patients of our series the acetabular cup was stable and with a mirror-polished internal surface, and in agreement with the literature a mixed THA was assembled with an off-label cup-dual mobility head (MDM/ADM, Stryker). Some Authors did not observe any significant difference between THAs treated with head and liner exchange, and those with the whole cup revised. Therefore, the head and liner revision may be still considered a viable option in a well fixed and positioned cup.16, 17, 18, 19
Various classifications based on acetabular bone loss can be used to help to choose the best management for cup revision. We used the Paprosky classification to plan the treatment, and focused on minimizing iatrogenic bone loss during implant removal and maximizing implant contact with host bone.20,21
In 11 cases (Table 4) a hemispherical cup fixed with screws was used. According to the literature, the main goal was to ensure good equatorial support and to fill bone defects.22 In Paprosky type 1 a press fit hemispherical cup fixed with 2–3 postero-superior screws was used. In Paprosky type 2 A, 2B a coated revision cup fixed with screws was used. In these cases medium sized chip bone grafts were impacted into cavitary defects. Holton et al. reported in their study23 that 10 mm3 size of bone chips provide better initial mechanical stability compared to smaller or larger bone chips. In Paprosky type 3 (case 13), we used structural graft (tricortical autologous graft from iliac tuberosity), a collagen Mg HA scaffold and Mg HA granules to fill the massive defect and a hemispherical cup was implanted. In this case an early failure of structural graft happened with an increase of acetabular inclination. The comparison of the radiographic control before and after weight bearing showed a rotation of the acetabular cup around the sagittal axis with a cup inclination increase of about 16° (from 39° to 23°). We attributed the failure to the poor bone quality, to the weak distal grip and to the configuration of screw placement. An oversized component was not an option due to the poor bone quality, and the 3 screws were all located close to each other in the superior central region of the cup and in the same near-sagittal plane. Such configuration of the screws placement only reduces micromotions locally without improving cup fixation in the rim edge far from the screws as proven by Hsu et al.24 A more widespread distribution of screws, while respecting safe areas, could be a more functional solution in such a scenario. In case 15 surgeons deal with a severe acetabular bone loss (Paprosky type 3a) (case 15) and an intraoperative fracture of the posterior column of the acetabulum; a good stability of the revision cup was obtained using a hemispherical cup with iliac winglets and a caudal hook, fixed with 6 screws to the supra-acetabular iliac bone. In this case a structural and morcelized homologous bone graft was used to restore the bone continuity. From literature analysis and clinical experience, considering not only the bone defects but also the poor quality of residual bone due to metallosis (comparable in many ways to a local metabolic bone disease), a viable option when dealing with a Paprosky type 3 defect, could be to prepare the acetabular bed with solid impaction of morcellized bone chips and autologous bone,22,25 to implant a oversized multihole revision cup, and to ensure a good primary stability to the construct with multiple screws in different quadrants and different directions.
Despite the extensive literature about metallosis, the patient's management is still controversial and challenging, especially regarding the pseudo tumoral mass removal technical aspects. The surgical indication is strongly given only in symptomatic patients with the presence of fluid or a mass on advanced imaging with or without elevated serum cobalt and chromium. In other cases, there is not a clear set management.26,27
Revision THA for MoM arthroplasty varies widely in complexity given the heterogeneous nature of ARMD.28 Surgical goals include excision of the soft tissues involved in metallosis and implantation of well-positioned components to optimise stability and reduce re-revisions but shared and univocal indications on the treatment of the pseudotumor, especially with a pelvic localization, do not exist.
The complete excision of the pseudotumoral lesion would theoretically reduce the infectious complication risk, since there is evidence of statistically higher risk of periprosthetic hip infection in MoM implants, with the pseudotumoral lesion probably acting as a culture medium for microorganisms in the development of infection.29 On the other hand, radical excision of the lesion may cause additional damage, depending on the location, the extent of tissue destruction, and the surgical gestures necessary for the purpose, with possible abductor insufficiency, iatrogenic femoral and acetabular fractures, nerve damage and bleeding to keep in mind. Especially in the case of invasion of less familiar anatomical areas (such as for the removal of an intrapelvic pseudotumor), a reasonable approach may include the assistance of a general or vascular surgeon and consider the possibility of a staged procedure. In our series, although complete removal of the pelvic tumor was not always performed (and often the collection was spontaneously drained through the acetabulum) no cases of infection or recurrence of symptoms in the follow-up period were reported.
The ilioinguinal approach may be necessary in the case of symptomatic neurovascular or ureteral compression caused by the mass effect of a solid pseudotumor, or as more frequently observed, a cystic one with fluid content, recurrent despite percutaneous drainage and not drained during the prosthetic revision.
According to the literature we have collected for every case a series of formal intraoperative photos, and we have taken and sent specimens for culture and histology.30,31 In our series the appearance of macroscopic intra-operative and laboratory microscopic findings in their variability and pleomorphism corresponds with the literature descriptions.32, 33, 34, 35
The location of a fluid collection, considered the most common subtype of pseudotumor, can depend on the surgical approach because the reactive fluid often dissects preferentially through the surgical tract.36 All patients of this series underwent THA through the posterolateral approach, and in this way, the capsular defect is posterior, and the reactive fluid can leak posteriorly to the great trochanter and accumulate all over. In our series the fluid collection was extended in periarticular spaces in 7 cases, mainly into the pelvis in 3 cases and in both spaces in other 3 cases. Ultrasounds were used to evaluate superficial inguinal and peritrochanteric regions and deep intrapelvic lesions. This technique is inexpensive, and generally quickly available, but it is operator-dependent and images can be less simple to interpret for a non-radiologist. In 3 cases echography was used to perform guided percutaneous drainage from a relapsing aseptic fluid collection before revision surgery. In 3 cases (8, 13 and 15) we found a pseudo tumoral mass large enough to compress and stretch the surrounding soft tissues, causing a mass effect. Especially in case 13, the spreading of the lesion in the pelvic area along the psoas causes neuro-vascular compression. In case 15 we found a large retroperitoneal intrapelvic semi-cystic pseudotumor adherent to the left iliac vessels; Algarni et al. reported a similar case of an iliopsoas bursal cystic lesion generating a venous obstruction and a unilateral lower limb swelling 5 years after a MoM total hip arthroplasty, and same surgical treatment: drainage of the cyst and THA revision.37
In literature intra or postoperative complication rates between 8% and 38% have been reported for revisions of MoM THAs.38, 39, 40, 41, 42 The most common intraoperative complications in the revision of MoM THAs were femoral fracture at the calcar region (3.5%), greater trochanter fracture (0.8%), sciatic nerve damage (0.6%) and acetabulum fracture (0.3%).43,44
Intraoperative periprosthetic femoral fractures (PFF) have received greater attention in the literature than acetabular fractures, possibly because it is more difficult to identify intraoperative acetabular fractures at the time of the surgery. Many studies collected and compared in 2019 Thaler's review have shown that the incidence of intraoperative PFF ranges between 1% in primary total hip arthroplasties to 7.8% in revision total hip arthroplasties procedures.45
According to the literature, in our series, in 3 cases an intraoperative intertrochanteric pathological fracture occurred during removal of the femoral stem. In 2 cases an intraoperative iatrogenic perforation of the femoral cortex occurred during the removal of the stem and the reaming. In one more case, an isolated fracture of the greater trochanter occurred during femoral reaming. Accidental cortical perforation is most likely to occur during channel preparation and drilling, so fractures during bone preparation can be due to torque generated by power reamers and forceful femoral preparation.46,47 Mainly in all of these cases, the fractures were associated with a cavitary or segmental-cavitary combined defect in the metaphyseal region. It's proven that patients with ARMD-like osteolysis at the greater trochanter or stem loosening are at the greatest risk of developing intraoperative and postoperative PFF.48,49
The surgery for PFF with the revision of the femoral component can be very demanding technically50 and is associated with a high rate of complications (18%) and reoperations (23%).45 In our series, neither of all femoral synthesis has failed in the follow-up period and no PFF has been missed.
An intraoperative acetabular fracture of the posterior wall occurred in case 15, classified by Callaghan51 and by Della Valle as a type I-A.52 In line with the literature45 we used a revision cup with 3 iliac winglets and a caudal hook fixed with 4 screws in the posterosuperior quadrant (3 extra-acetabular and 1 intra-acetabular iliac screws), which was implanted after bone defects augmentation with homologous morselized and structured bone grafting. Thaler shows that a not identified acetabular fracture during total hip arthroplasty leads to a higher rate of early loosening. Identification of those fractures and adequate treatment is essential for the long-term survival of the prosthesis.
In this series, we did not observe neurovascular lesions due to the acetabular screws crossing the far bone cortex; we believe it is essential to be aware of and respect the safe areas for the trans acetabular placement of the screws described by Wasielewski8 to reduce the risk of such complications.
In our case series no infections were detected both in the preoperatory and in the intraoperative time.
Although generally speaking the good result of a surgical intervention cannot be evaluated only with the survival of the implant, in the complex prosthetic revision surgery the complication rate and the implant survival are the main outcomes reported in the literature.53
Initial outcomes following revision THA for ARMD in general literature were poor, with reported major complication rates of 38% including instability, deep infection, recurrence of ARMD, neurovascular injury, component loosening, and reoperation.38,54 Early studies reported catastrophic short-term outcomes following ARMD revision, with one-third of patients requiring re-operations.38,55,56 Differently, De Smet in 2011 has observed better outcomes with increased surgical experience,57 and Matharu reported a five-year implant rate of survival of 87.9% following ARMD revision.58 Nowadays Lainiala reported 7-year implant survivorship of 94% after revision of stemmed THAs and 91% after revision of hip resurfacings59. This is in line with our result: following revision surgery, there was no case of re-revision and there was no recurrence of metallosis or ARMD related symptoms at last follow-up (mean follow-up 3 years, range 1–7 years).
Many authors have described dislocation as a common issue after a revision of MoM hip replacement,38,39,41,42,55,57 a larger head size has been suggested to decrease the risk for poor outcome.58,59 In our series despite an average increase of 3.7 mm in cup diameter, we have often switched to a head with a smaller diameter than the previous MoM head (except when it was revised with a dual-mobility head) and we have observed one isolated case of dislocation (case 15) in a suboptimal anteversion of the acetabular cup associated with Paprosky type 3 acetabular defects, intraoperative fracture of the posterior column and hip dysplasia as the cause of primary hip replacement. In the same patient, we also recorded an acute onset of nerve palsy resulting in a permanent deficit with drop foot gait treated with specific rehabilitation and orthosis (AFO) with satisfactory functional results.60
Whyles and Stryker observed a higher-than-expected rate of infection after revision of MOM THAs.39,61 No post-revision infection was observed in our case series, probably because as the literature suggests, we have carefully removed necrotic tissue and metal debris. Incomplete elimination or multiple operations, and retention of primary MoM components are described as risk factors for infection.38,62
Routine follow-up with plain radiography and measurement of metal ion levels is necessary following revision surgery for ARMD. Serum cobalt and chromium ion levels typically decrease dramatically in the first 3 months of post-revision surgery63 but due to the number of complications and early failures careful followup seems desirable.64
Our study has many limitations related to the retrospective design, the lack of a control group, and the small number of the series limiting the scientific value while providing some suggestions for clinical practice through a careful analysis of case studies and literature. However, despite a vast and not always univocal scientific production regarding the etiopathogenesis and incidence of metallosis as a complication of hip prosthetic surgery, its local or systemic clinical manifestations, the recommendations regarding the frequency of check-ups and the timing and indications for the prosthetic revision (failure of the prosthesis, symptoms, serum levels of metal ions), little or nothing has been shared on the possible practical options in the management of these specific surgical challenges. Therefore, through the retrospective analysis of our experience and the review of the literature, we tried to describe the troubles and the complications that can be encountered, and the, albeit questionable, solutions that can be adopted in this infrequent scenario, hoping this could be a starting point for a constructive dialogue with those who have more experience than us, and a food for thought for all those who will face this insidious and challenging surgery.
Author statement
Francesco Pisanu: Conceptualization, Methodology, writing-Review & Editing, Supervision. Matteo Andreozzi: investigation, writing-original draft. Enrico Fiori: data curation, writing-original draft. Fabiana Altamore: data curation, writing-original draft. Marco Bartoli: investigation. Gianfilippo Caggiari: Review & Editing. Sebastiano Ortu: Review. Mario Rios: Editing. Andrea Fabio Manunta: supervision. Carlo Doria: conceptualization and supervision
Declaration of competing interest
All the authors have no conflict of interest to declare.
Contributor Information
Francesco Pisanu, Email: francesco.pisanu@aousassari.it.
Matteo Andreozzi, Email: matteo.andreozzi88@gmail.com.
Enrico Fiori, Email: efmfiori@hotmail.it.
Fabiana Altamore, Email: fabianaltamore@gmail.com.
Marco Bartoli, Email: marco.bartoli1987@gmail.com.
Gianfilippo Caggiari, Email: gianfilippocaggiari@gmail.com.
Sebastiano Ortu, Email: sebastiano.ortu10@gmail.com.
Mario Rios, Email: mr.rios2293@gmail.com.
Andrea Fabio Manunta, Email: andreafabio.manunta@aousassari.it.
Carlo Doria, Email: carlo.doria@aousassari.it.
References
- 1.Pisanu F., Doria C., Andreozzi M. Pleomorphic clinical spectrum of metallosis in total hip arthroplasty. Int Orthop. 2019 Jan;43(1):85–96. doi: 10.1007/s00264-018-4176-4. Epub 2018 Sep 29. PMID: 30269183. [DOI] [PubMed] [Google Scholar]
- 2.Manunta A.F., Zedde P., Pisanu F., Marras F. Sports-related changes of the synovial membrane. Joints. 2015;13(2):181–187 4. [PMC free article] [PubMed] [Google Scholar]
- 3.Fessy M.H., N'Diaye A., Carret J.P., Fischer L.P. Locating the center of rotation of the hip. Surg Radiol Anat. 1999;21(4):247–250. doi: 10.1007/BF01631394. PMID: 10549080. [DOI] [PubMed] [Google Scholar]
- 4.DeLee J.G., Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976 Nov-Dec;(121):20–32. PMID: 991504. [PubMed] [Google Scholar]
- 5.Gruen T.A., McNeice G.M., Amstutz H.C. Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979 Jun;141:17–27. PMID: 477100. [PubMed] [Google Scholar]
- 6.Paprosky W.G., Perona P.G., Lawrence J.M. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty. 1994 Feb;9(1):33–44. doi: 10.1016/0883-5403(94)90135-x. [DOI] [PubMed] [Google Scholar]
- 7.D'Antonio J., McCarthy J.C., Bargar W.L. Classification of femoral abnormalities in total hip arthroplasty. Clin Orthop Relat Res. 1993 Nov;(296):133–139. PMID: 8222415. [PubMed] [Google Scholar]
- 8.Wasielewski R.C., Cooperstein L.A., Kruger M.P., Rubash H.E. Acetabular anatomy and the transacetabular fixation of screws in total hip arthroplasty. J Bone Joint Surg Am. 1990 Apr;72(4):501–508. PMID: 2324135. [PubMed] [Google Scholar]
- 9.Böhm P., Bischel O. The use of tapered stems for femoral revision surgery. Clin Orthop Relat Res. 2004 Mar;(420):148–159. PMID: 15057091. [PubMed] [Google Scholar]
- 10.Cavagnaro L., Formica M., Basso M., Zanirato A., Divano S., Felli L. Femoral revision with primary cementless stems: a systematic review of the literature. Muscoloskelet Surg. 2018 Apr;102(1):1–9. doi: 10.1007/s12306-017-0487-7. [DOI] [PubMed] [Google Scholar]
- 11.Lopreite F., Perez Alamino L., Simesen de Bielke H., Garabano G., Del Sel H. Distal fixation stems for revision of total hip replacement. J Orthop. 2021 Feb 21;24:151–156. doi: 10.1016/j.jor.2021.02.031. PMID: 33716420; PMCID: PMC7932857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sheth N.P., Nelson C.L., Paprosky W.G. Femoral bone loss in revision total hip arthroplasty: evaluation and management. J Am Acad Orthop Surg. 2013 Oct;21(10):601–612. doi: 10.5435/JAAOS-21-10-601. [DOI] [PubMed] [Google Scholar]
- 13.Maniscalco P., Quattrini F., Ciatti C. Neck modularity in total hip arthroplasty: a retrospective study of nine hundred twenty-eight titanium neck implants with a maximum follow-up of eighteen years. Int Orthop. 2020;44:2261–2266. doi: 10.1007/s00264-020-04686-8. [DOI] [PubMed] [Google Scholar]
- 14.Bianchi L., Galante C., Zagra L. The management of femoral bone stock in THA revision: indications and techniques. Hip Int. 2014 Oct 2;24(Suppl 10):S37–S43. doi: 10.5301/hipint.5000174. PMID: 24970033. [DOI] [PubMed] [Google Scholar]
- 15.Garabano G., Gessara A.M., Pesciallo C.A., Alamino L.P., Del Sel H. Extended trochanteric osteotomy (ETO) and fluted tapered modular stems in revision hip arthroplasty. Does ETO integrity or consolidation, really matter? J Orthop. 2021 Feb 9;23:250–255. doi: 10.1016/j.jor.2021.02.001. PMID: 33664557; PMCID: PMC7890301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Colacchio N.D., Wooten C.J., Martin J.R., Masonis J.L., Fehring T.K. Dual mobility for monoblock metal-on-metal revision-is it safe? J Arthroplasty. 2020 Feb;35(2):508–512. doi: 10.1016/j.arth.2019.09.028. Epub 2019 Sep 26. PMID: 31662280. [DOI] [PubMed] [Google Scholar]
- 17.Plummer D.R., Botero H.G., Berend K.R., Pritchett J.W., Lombardi A.V., Della Valle C.J. Salvage of monoblock metal-on-metal acetabular components using a dual- mobility bearing. J Arthroplasty. 2016;31:846e9. doi: 10.1016/j.arth.2015.08.016. [DOI] [PubMed] [Google Scholar]
- 18.Figueras G., Planell R.V., Fernandez R.S., Biayna J.C. Revision of metal-on-metal hip arthroplasty with well fixed and positioned acetabular component using a dual-mobility head and review of literature. Open Orthop J. 2016;10:512e21. doi: 10.2174/1874325001610010512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pisecky L., Hipmair G., Schauer B., Böhler N. Osteolysis in total hip arthroplasty after head and inlay revision surgery. J Orthop. 2017 Jan 9;14(1):192–194. doi: 10.1016/j.jor.2016.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fryhofer G.W., Ramesh S., Sheth N.P. Acetabular reconstruction in revision total hip arthroplasty. J Clin Orthop Trauma. 2020 Jan-Feb;11(1):22–28. doi: 10.1016/j.jcot.2019.11.004. Epub 2019 Dec 2. PMID: 32001979; PMCID: PMC6985018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ahmad A.Q., Schwarzkopf R. Clinical evaluation and surgical options in acetabular reconstruction: a literature review. J Orthop. 2015 Nov 2;12(Suppl 2):S238–S243. doi: 10.1016/j.jor.2015.10.011. PMID: 27047229; PMCID: PMC4796576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee J.M., Kim T.H. Acetabular cup revision arthroplasty using morselized impaction allograft. Hip Pelvis. 2018 Jun;30(2):65–77. doi: 10.5371/hp.2018.30.2.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Holton C., Bobak P., Wilcox R., Jin Z. Impaction grafted bone chip size effect on initial stability in an acetabular model: mechanical evaluation. J Orthop. 2013 Nov 5;10(4):177–181. doi: 10.1016/j.jor.2013.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hsu J.T., Chang C.H., Huang H.L. The number of the screws, bone quality, and friction coefficient affect acetabular cup stability. Med Eng Phys. 2007 Dec;29(10):1089–1095. doi: 10.1016/medengphy.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 25.Kumar V., Ricks M., Abouel-Enin S., Dunlop D.G. Long term results of impaction Bone grafting using a synthetic graft (Apapore) in revision hip surgery. J Orthop. 2017 Apr 2;14(2):290–293. doi: 10.1016/j.jor.2017.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Berber R., Skinner J.A., Hart A.J. Management of metal-on-metal hip implant patients: who, when and how to revise? World J Orthoped. 2016 May 18;7(5):272–279. doi: 10.5312/wjo.v7.i5.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chang J.S., Haddad F.S. Revision total hip arthroplasty for metal-on-metal failure. J Clin Orthop Trauma. 2020 Jan-Feb;11(1):9–15. doi: 10.1016/j.jcot.2019.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Matharu G.S., Eskelinen A., Judge A., Pandit H.G., Murray D.W. Revision surgery of metal-on-metal hip arthroplasties for adverse reactions to metal debris. Acta Orthop. 2018;89(3):278e288. doi: 10.1080/17453674.2018.1440455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bordini B., Stea S., Castagnini F., Busanelli L., Giardina F., Toni A. The influence of bearing surfaces on periprosthetic hip infections: analysis of thirty nine thousand, two hundred and six cementless total hip arthroplasties. Int Orthop. 2019 Jan;43(1):103–109. doi: 10.1007/s00264-018-4097-2. [DOI] [PubMed] [Google Scholar]
- 30.Bolognesi M.P., Ledford C.K. Metal-on-Metal total hip arthroplasty: patient evaluation and treatment. J Am Acad Orthop Surg. 2015 Dec;23(12):724–731. doi: 10.5435/JAAOS-D-14-00183. [DOI] [PubMed] [Google Scholar]
- 31.Purudappa P.P., Sharma O.P., Priyavadana S., Sambandam S., Villafuerte J.A. Unexpected positive intraoperative cultures (UPIC) in revision Hip and knee arthroplasty- A review of the literature. J Orthop. 2019 Jul 2;17:1–6. doi: 10.1016/j.jor.2019.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hallab N.J., Mikecz K., Vermes C., Skipor A., Jacobs J.J. Orthopaedic implant related metal toxicity in terms of human lymphocyte reactivity to metal-protein complexes produced from cobalt-base and titanium-base implant alloy degradation. Mol Cell Biochem. 2001 Jun;222(1-2):127–136. PMID: 11678594. [PubMed] [Google Scholar]
- 33.Tkaczyk C., Huk O.L., Mwale F. Investigation of the binding of Cr(III) complexes to bovine and human serum proteins: a proteomic approach. J Biomed Mater Res. 2010 Jul;94(1):214–222. doi: 10.1002/jbm.a.32700. [DOI] [PubMed] [Google Scholar]
- 34.Hart A.J., Matthies A., Henckel J., Ilo K., Skinner J., Noble P.C. Understanding why metal-on-metal hip arthroplasties fail: a comparison between patients with well-functioning and revised birmingham hip resurfacing arthroplasties. AAOS exhibit selection. J Bone Joint Surg Am. 2012 Feb 15;94(4):e22. doi: 10.2106/JBJS.K.01266. [DOI] [PubMed] [Google Scholar]
- 35.Donell S.T., Darrah C., Nolan J.F. Norwich Metal-on-Metal Study Group. Early failure of the Ultima metal-on-metal total hip replacement in the presence of normal plain radiographs. J Bone Joint Surg Br. 2010 Nov;92(11):1501–1508. doi: 10.1302/0301-620X.92B11.24504. [DOI] [PubMed] [Google Scholar]
- 36.Sabah S.A., Mitchell A.W., Henckel J., Sandison A., Skinner J.A., Hart A.J. Magnetic resonance imaging findings in painful metal-on-metal hips: a prospective study. J Arthroplasty. 2011 Jan;26(1):71–76. doi: 10.1016/j.arth.2009.11.008. 76.e1-2. [DOI] [PubMed] [Google Scholar]
- 37.Algarni A.D., Huk O.L., Pelmus M. Metallosis-induced iliopsoas bursal cyst causing venous obstruction and lower-limb swelling after metal-on-metal THA. Orthopedics. 2012 Dec;35(12):e1811–e1814. doi: 10.3928/01477447-20121120-30. [DOI] [PubMed] [Google Scholar]
- 38.Munro J.T., Masri B.A., Duncan C.P., Garbuz D.S. High complication rate after revision of large-head metal-on-metal total hip arthroplasty. Clin Orthop Relat Res. 2014;472(2):523–528. doi: 10.1007/s11999-013-2979-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stryker L.S., Odum S.M., Fehring T.K., Springer B.D. Revisions of monoblock metal-on-metal THAs have high early complication rates. Clin Orthop Relat Res. 2015;473(2):469–474. doi: 10.1007/s11999-014-3791-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wyles C.C., Van Demark R.E., 3rd, Sierra R.J., Trousdale R.T. High rate of infection after aseptic revision of failed metal-on-metal total hip arthroplasty. Clin Orthop Relat Res. 2014 Feb;472(2):509–516. doi: 10.1007/s11999-013-3157-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.van Lingen C.P., Ettema H.B., Bosker B.H., Verheyen C.C. Revision of a single type of large metal head metal-on-metal hip prosthesis. Hip Int. 2015 May-Jun;25(3):221–226. doi: 10.5301/hipint.5000220. [DOI] [PubMed] [Google Scholar]
- 42.Jennings J.M.D.P.T., White S., Martin J.R., Yang C.C., Miner T.M., Dennis D.A. Revisions of modular metal-on-metal THA have a high risk of early complications. Clin Orthop Relat Res. 2019;477(2):344–350. doi: 10.1097/CORR.0000000000000363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Miettinen S.S.A., Mäkinen T.J., Mäkelä K., Huhtala H., Kettunen J.S., Remes V. Intraoperative complications and mid-term follow-up of large-diameter head metal-on-metal total hip arthroplasty and hip resurfacing arthroplasty. Scand J Surg. 2018 Jun;107(2):180–186. doi: 10.1177/1457496917748220. [DOI] [PubMed] [Google Scholar]
- 44.Matharu G.S., Judge A., Pandit H.G., Murray D.W. Which factors influence the rate of failure following metal-on-metal hip arthroplasty revision surgery performed for adverse reactions to metal debris? an analysis from the National Joint Registry for England and Wales. Bone Joint Lett J. 2017 Aug;99-B(8):1020–1027. doi: 10.1302/0301-620X.99B8.BJJ-2016-0889.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Thaler M., Lechneret R. Strategies for femoral, acetabular and trochanteric intraoperative fractures. G Ital Ortop Traumatol. 2019;45(Suppl. 1):S144–S146. [Google Scholar]
- 46.Sidler-Maier C.C., Waddell J.P. Incidence and predisposing factors of periprosthetic proximal femoral fractures: a literature review. Int Orthop. 2015 Sep;39(9):1673–1682. doi: 10.1007/s00264-015-2721-y. [DOI] [PubMed] [Google Scholar]
- 47.Egan K.J., Di Cesare P.E. Intraoperative complications of revision hip arthroplasty using a fully porous-coated straight cobalt-chrome femoral stem. J Arthroplasty. 1995 Nov;(10 Suppl):S45–S51. doi: 10.1016/s0883-5403(05)80230-x. [DOI] [PubMed] [Google Scholar]
- 48.Della Rocca G.J., Leung K.S., Pape H.C. Periprosthetic fractures: epidemiology and future projections. J Orthop Trauma. 2011 Jun;25(Suppl 2):S66–S70. doi: 10.1097/BOT.0b013e31821b8c28. [DOI] [PubMed] [Google Scholar]
- 49.Biberthaler P. Periprosthetic fractures. Unfallchirurg. 2016 Apr;119(4):262–263. doi: 10.1007/s00113-016-0157-5. [DOI] [PubMed] [Google Scholar]
- 50.Tsiridis E., Haddad F.S., Gie G.A. The management of periprosthetic femoral fractures around hip replacements. Injury. 2003 Feb;34(2):95–105. doi: 10.1016/s0020-1383(02)00257-7. [DOI] [PubMed] [Google Scholar]
- 51.Callaghan J.J. Periprosthetic fractures of the acetabulum during and following total hip arthroplasty. Instr Course Lect. 1998;47:231–235. [PubMed] [Google Scholar]
- 52.Della Valle C.J., Momberger N.G., Paprosky W.G. Periprosthetic fractures of the acetabulum associated with a total hip arthroplasty. Instr Course Lect. 2003;52:281–290. [PubMed] [Google Scholar]
- 53.Pisanu F., Andreozzi M., Costagli F. Resumption of physical activity and sport after knee replacement. J Orthop. 2020 Jan 25;20:247–250. doi: 10.1016/j.jor.2020.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Garfinkel J.H., Gladnick B.P., Pachter C.S., Cochrane N.H., Romness D.W. Perioperative factors associated with increased length of stay after revision of metal-on-metal total hip arthroplasty. J Orthop. 2019 Jan 17;16(2):109–112. doi: 10.1016/j.jor.2019.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Grammatopoulos G., Pandit H., Kwon Y.M. Hip resurfacings revised for inflammatory pseudotumour have a poor outcome. J Bone Joint Surg Br. 2009 Aug;91(8):1019–1024. doi: 10.1302/0301-620X.91B8.22562. [DOI] [PubMed] [Google Scholar]
- 56.Rajpura A., Porter M.L., Gambhir A.K., Freemont A.J., Board T.N. Clinical experience of revision of metal on metal hip arthroplasty for aseptic lymphocyte dominated vasculitis associated lesions (ALVAL) Hip Int. 2011 Jan-Mar;21(1):43–51. doi: 10.5301/hip.2011.6276. [DOI] [PubMed] [Google Scholar]
- 57.De Smet K.A., Van Der Straeten C., Van Orsouw M., Doubi R., Backers K., Grammatopoulos G. Revisions of metal-on-metal hip resurfacing: lessons learned and improved outcome. Orthop Clin N Am. 2011 Apr;42(2):259–269. doi: 10.1016/j.ocl.2011.01.003. ix. [DOI] [PubMed] [Google Scholar]
- 58.Matharu G.S., Pynsent P.B., Dunlop D.J. Revision of metal-on-metal hip replacements and resurfacings for adverse reaction to metal debris: a systematic review of outcomes. Hip Int. 2014 Jul-Aug;24(4):311–320. doi: 10.5301/hipint.5000140. [DOI] [PubMed] [Google Scholar]
- 59.Lainiala O., Reito A., Nieminen J., Eskelinen A. Complications and re-revisions after revisions of 528 metal-on-metal hips because of adverse reaction to metal debris. Acta Orthop. 2020 Aug;91(4):365–371. doi: 10.1080/17453674.2020.1748351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Manca A., Pisanu F., Ortu E. Isokinetic cross-training effect in foot drop following common peroneal nerve injury. Isokinet Exerc Sci. 2015;23:17–20. [Google Scholar]
- 61.Wyles C.C., Van Demark R.E., 3rd, Sierra R.J., Trousdale R.T. High rate of infection after aseptic revision of failed metal-on-metal total hip arthroplasty. Clin Orthop. 2014;472(2):509–516. doi: 10.1007/s11999-013-3157-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Liddle A.D., Satchithananda K., Henckel J. Revision of metal-on-metal hip arthroplasty in a tertiary center: a prospective study of 39 hips with between 1 and 4 years of follow-up. Acta Orthop. 2013 Jun;84(3):237–245. doi: 10.3109/17453674.2013.797313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ball S.T., Severns D., Linn M., Meyer R.S., Swenson F.C. What happens to serum metal ion levels after a metal-on-metal bearing is removed? J Arthroplasty. 2013 Sep;28(8 Suppl):53–55. doi: 10.1016/j.arth.2013.06.040. [DOI] [PubMed] [Google Scholar]
- 64.Slullitel P.A.I., Brandariz R., Oñativia J.I. Aggressive granulomatosis of the hip: a forgotten mode of aseptic failure. Int Orthop. 2019 Jun;43(6):1321–1328. doi: 10.1007/s00264-018-4252-9. [DOI] [PubMed] [Google Scholar]