Abstract
Objective
The current study examined the roles of constructive and dysfunctional problem-solving strategies in the relationships between illness uncertainty and adjustment outcomes (i.e., anxious, depressive, and posttraumatic stress symptoms) in caregivers of children newly diagnosed with cancer.
Methods
Two hundred thirty-eight caregivers of children (0–19 years of age) newly diagnosed with cancer (2–14 weeks since diagnosis) completed measures of illness uncertainty, problem-solving strategies, and symptoms of anxiety, depression, and posttraumatic stress.
Results
A mediation model path analysis assessed constructive and dysfunctional problem-solving strategies as mediators between illness uncertainty and caregiver anxious, depressive, and posttraumatic stress symptoms. Dysfunctional problem-solving scores partially mediated the relationships between illness uncertainty and anxious, depressive, and posttraumatic stress symptoms. Constructive problem-solving scores did not mediate these relationships.
Conclusions
The current findings suggest that illness uncertainty and dysfunctional problem-solving strategies, but not constructive problem-solving strategies, may play a key role in the adjustment of caregivers of children newly diagnosed with cancer. Interventions aimed at managing illness uncertainty and mitigating the impact of dysfunctional problem-solving strategies may promote psychological adjustment.
Keywords: cancer, caregiver, illness uncertainty, oncology, pediatric cancer, problem-solving, psychological adjustment
Introduction
Pediatric cancer diagnoses create a disruptive and distressful experience for families (Rodriguez et al., 2012). The majority of caregivers of children with cancer appear resilient and adapt over time; however, a consistent subset of caregivers are found to be at risk for psychosocial distress including anxiety, depression, and posttraumatic stress shortly after diagnosis (Katz et al., 2018; Patiño-Fernández et al., 2008). The duration of caregiver distress during pediatric cancer treatment varies but is consistently present immediately following the child’s diagnosis (Pai et al., 2007; Steele et al., 2003). This heightened distress coincides with the acute phase of treatment in which caregivers are presented with complex information and are required to make critical treatment decisions (Ruccione et al., 1991). Heightened levels of caregiver distress are of concern as it is a robust predictor of child psychosocial distress (Bakula et al., 2019; Pierce et al., 2017). Thus, understanding caregivers’ adjustment outcomes represents a key means of promoting better child adjustment in this population.
A construct often implicated in caregiver psychological adjustment in pediatric medical populations is illness uncertainty (Szulczewski et al., 2017). Illness uncertainty is a cognitive appraisal that occurs when one cannot discern an outcome based upon the available information (Mishel, 1988). Throughout pediatric cancer treatment, caregivers frequently and repeatedly experience situations with the hallmark characteristics of illness uncertainty including lack of information about the illness or treatment (e.g., effectiveness of an experimental treatment), ambiguity of symptoms (e.g., is bodily pain due to falling while playing or relapse of disease?), unpredictability of health outcomes (e.g., side-effects of chemotherapy, radiation, and medication), and complexity of the treatment (e.g., multimodal treatment plan consisting of surgery, radiation, and chemotherapy) (Mishel, 1984; 1990). Given the prevalence of situations eliciting illness uncertainty during pediatric cancer treatment, it is of concern that illness uncertainty has been linked to greater caregiver psychological distress as well as anxious, depressive, and posttraumatic stress symptoms (Mullins et al., 2012, 2016; Szulczewski et al., 2017). Thus, illness uncertainty appears to be a promising target to improve caregiver functioning within the pediatric cancer population. Clarifying the mechanism by which illness uncertainty and poor caregiver adjustment outcomes are associated is needed to inform these interventions.
Problem-solving strategies may represent one such mediating mechanism, as it has been consistently associated with caregiver adjustment in pediatric chronic illness populations (Iobst et al., 2009; Palermo et al., 2016; Phipps et al., 2020; Sahler et al., 2002). The social problem-solving skills model represents a multidimensional coping strategy to managing problems faced in everyday life by directing coping efforts to alter the situation or one’s cognitions (D’Zurilla et al., 2004; D’Zurilla & Goldfried 1971; D’Zurilla & Nezu, 1982). Based on D’Zurilla et al.’ (2004), social problem-solving model, problem-solving strategies fall into two broad dimensions: constructive versus dysfunctional problem-solving (Maydeu-Olivares & D’Zurilla, 1996). Constructive problem-solving is characterized by rational deductive thinking and positive problem orientation. In contrast, dysfunctional problem-solving is characterized by impulsivity/carelessness, avoidance, and negative problem orientation. It is important to note that problem-solving interventions for caregivers of children with chronic medical conditions that teach constructive problem-solving strategies have been effective at improving caregiver psychological adjustment, enhancing problem-solving skills, and reducing negative affect (Palermo et al., 2016; Phipps et al., 2020; Sahler et al., 2002). Interestingly, constructive problem-solving does not appear to be predictive of caregiver adjustment in other studies (Ko et al., 2005; Rivera et al., 2008; Shanmugham et al., 2009). Dysfunctional problem-solving, however, has been established as a robust predictor of poorer adjustment outcomes in caregivers of children and adults with chronic medical conditions (Ko et al., 2005; Rivera et al., 2008; Shanmugham et al., 2009). Thus, the mechanism through which problem-solving affects adjustment outcomes is unclear. Although problem-solving strategies and illness uncertainty are both linked to adjustment outcomes in caregivers of children with cancer, the interrelationship between illness uncertainty and problem-solving strategies in caregivers has not been directly examined.
The present study aimed to understand the roles of constructive and dysfunctional problem-solving strategies in the relationships between illness uncertainty and adjustment outcomes (i.e., anxious, depressive, and posttraumatic stress symptoms) in caregivers of children newly diagnosed with cancer. We hypothesized that both constructive and dysfunctional problem-solving would mediate the relationships between caregiver illness uncertainty and all three caregiver adjustment outcomes.
Methods
Participants
The current study sample included 238 caregivers, the majority of which were female (89.1%), non-Hispanic (94.5%), and White (85.7%). Mean caregiver age was 35.96 years (SD = 8.19). Median household income was $50,000–$59,000 and median educational attainment was “finished college/trade school.” Child age ranged from 0 to 19 years, with a mean of 7.63 years (SD = 5.53). Children were mostly male (58.0%), non-Hispanic (92.9%), and White (76.5%). Leukemias (42.4%) were the most prevalent cancer diagnosis followed by solid tumors (29.0%), brain tumors (15.1%), and then lymphomas (13.4%). Length of time since diagnosis ranged from 2.00 to 14.71 weeks, with a mean of 8.39 weeks (SD = 2.98). A detailed summary of demographic characteristics is provided in Table I. Of the 409 families approached between 2015 and 2019, 279 (68.2%) agreed to participate in the study. There were no significant differences between the ages and gender of children in families that participated compared to those that declined to participate. Forty caregivers withdrew before completing baseline questionnaires and one caregiver was excluded due to their child’s cancer diagnosis being a secondary malignancy. Common reasons for declining to participate and/or withdrawing included “lack of time” and desire to “focus attention on child.” This resulted in 238 caregivers (85.7%) that completed baseline questionnaires and were included in the following analyses. There was no significant difference between the genders of caregivers that withdrew prior to completing baseline questionnaires and those who completed baseline questionnaires.
Table I.
Descriptive Statistics and Demographics (N = 238)
| Variable | Frequency | Percent |
|---|---|---|
| Caregiver gender | ||
| Female | 212 | 89.1 |
| Male | 26 | 10.9 |
| Caregiver Ethnicity | ||
| Non-Latino/Hispanic | 225 | 94.5 |
| Latino/Hispanic | 13 | 5.5 |
| Caregiver Race | ||
| White | 204 | 85.7 |
| Black/African American | 10 | 4.2 |
| Asian | 7 | 2.9 |
| American Indian/Alaskan Native | 2 | 0.8 |
| Multiracial | 9 | 3.8 |
| Caregiver education | ||
| Started School but did not finish | 10 | 4.2 |
| Finished high school/got GED | 50 | 21.0 |
| Started college or trade school | 49 | 20.6 |
| Finished college or trade school | 99 | 41.6 |
| Started master’s or doctoral program | 4 | 1.7 |
| Finished master’s or doctoral program | 20 | 8.4 |
| Household income | ||
| <$19,999 | 42 | 17.6 |
| $20,000–$39,999 | 47 | 19.7 |
| $40,000–$79,999 | 61 | 25.6 |
| >$80,000 | 85 | 35.7 |
| Relationship to patient | ||
| Mother | 209 | 87.8 |
| Father | 25 | 10.5 |
| Other | 4 | 1.7 |
| Child gender | ||
| Female | 100 | 58.0 |
| Male | 138 | 42.0 |
| Child cancer diagnoses | ||
| Leukemia | 101 | 42.4 |
| Solid tumor | 69 | 29.0 |
| Brain tumor | 36 | 15.1 |
| Lymphoma | 32 | 13.4 |
Note. Descriptive statistics that do not sum to 238 are due to nonreported data.
Study Procedure
The current study utilized baseline data collected from caregivers of children newly diagnosed with cancer who were enrolled in a multi-site caregiver-based intervention to decrease psychological distress (ClinicalTrials.gov Identifier: NCT02505165). All data in the current study were collected before randomization occurred and analyzed prior to the completion of post-intervention data collection. The current study is a standalone analysis to examine the relationships between uncertainty, problem-solving strategies, and adjustment prior to any potential influence of the intervention condition or education and support control condition. This is the first study to report data from this cohort and is independent of outcome analyses conducted for the clinical trial intervention. Caregivers were recruited from three geographically diverse children’s hospitals. The Institutional Review Board at each hospital approved the study (IRB# 18, 158, and 5794) and all procedures adhered to American Psychological Association standards of ethical principles and codes of conduct. Families were eligible to participate if: (1) their child was diagnosed with cancer within the past 2–12 weeks; (2) their child was 18 years of age or younger at diagnosis; (3) caregiver was English proficient; and (4) caregiver had no serious intellectual impairments or psychiatric disorders that would preclude their ability to consent and be involved in the study. Families were ineligible if the child with cancer was determined to be in the terminal phase of illness and/or was not receiving curative therapy and if the diagnosis was determined to be a relapse or a secondary malignancy. Caregivers were invited to participate in the study during their child’s outpatient clinic visits and inpatient admissions. After informed consent and assent were obtained, caregivers were asked to complete questionnaires within three weeks of the date of consent. Caregivers were compensated for their time.
Measures
Demographic Information
Caregivers provided demographic information for themselves and their child, including age, gender, race/ethnicity, household income, educational attainment, and child’s diagnosis.
Parent Perceptions of Uncertainty Scale (PPUS)
The Parent Perceptions of Uncertainty Scale (PPUS) is a 31-item self-report measure of caregiver perceptions of uncertainty related to their child’s illness (Mishel, 1983). Caregivers are asked to indicate the extent to which they agree with each statement on a 5-point Likert-type scale (Strongly Disagree to Strongly Agree). The PPUS consists of four subscales (ambiguity, lack of clarity, lack of information, and unpredictability) and a total score, which is the sum of the items. The current study used the PPUS total score, with higher scores reflecting greater levels of illness uncertainty. The PPUS has demonstrated excellent internal consistency among caregivers of children with cancer (Perez et al., 2020). Internal consistency for the PPUS in the current sample was excellent (α = .90).
Social Problem-Solving Inventory-Revised: Short Form (SPSI-R:SF)
The Social Problem-Solving Inventory-Revised: Short Form (SPSI-R:SF) is a 25-item self-report measure of adaptive and maladaptive problem-solving strategies across five subscales (D’Zurilla et al., 2002). Caregivers rated each the item on a 5-point Likert-type scale (0 = “Not at all true” to 4 = “Extremely true to me”). The current study utilized a robust two-factor structure of the SPSI-R:SF previously demonstrated in the literature (Ko et al., 2005; Sahler et al., 2002). Positive problem orientation and constructive problem-solving subscales were summed to create a constructive problem-solving score ranging from 0 to 40, with higher scores indicating greater use of constructive problem-solving skills. Negative problem orientation, avoidance problem-solving, and impulsive-careless problem-solving subscales were summed to create a dysfunctional problem-solving score ranging from 0 to 60. Higher scores indicated greater use of dysfunctional problem-solving strategies. The SPSI-R:SF has demonstrated good internal reliability in previous studies of caregivers of children with cancer (Sahler et al., 2005). Internal consistency was good for both constructive problem-solving (α = .88) and dysfunctional problem-solving (α = .86) subscales in this sample.
Symptom Checklist-90 Revised (SCL-90-R)
The Symptom Checklist-90 Revised (SCL-90-R) is a 90-item self-report measure designed to assess psychological symptoms and psychological distress on a 5-point Likert-type scale (1 = “Not at all” to 5 = “Extremely”) and comprises of nine total subscales and three global indices of distress (Derogatis, 1994). The current study used the Depression and Anxiety subscales. Raw scores were converted to t-scores based on normative data. The SCL-90-R has demonstrated good internal reliability in samples of caregivers of children with cancer (Mullins et al., 2012). In the current sample, internal consistency was excellent for the Depression subscale (α = .91) and good for the Anxiety subscale (α = .89).
Impact of Events Scale- Revised (IES-R)
The Impact of Events Scale-Revised (IES-R) is a 22-item self-report measure of posttraumatic stress symptoms in response to a specific distressing event (Weiss, 2007). Caregivers rated each item on a 5-point Likert-type scale (0 = “Not at all” to 4 = “Extremely”). For the current sample, the IES-R total score was summed with greater scores reflecting higher responses of intrusions. The IES-R has demonstrated good internal consistency in previous samples of caregivers of children with cancer (Sahler et al., 2013). Internal consistency was excellent for the IES-R in this sample (α = .94).
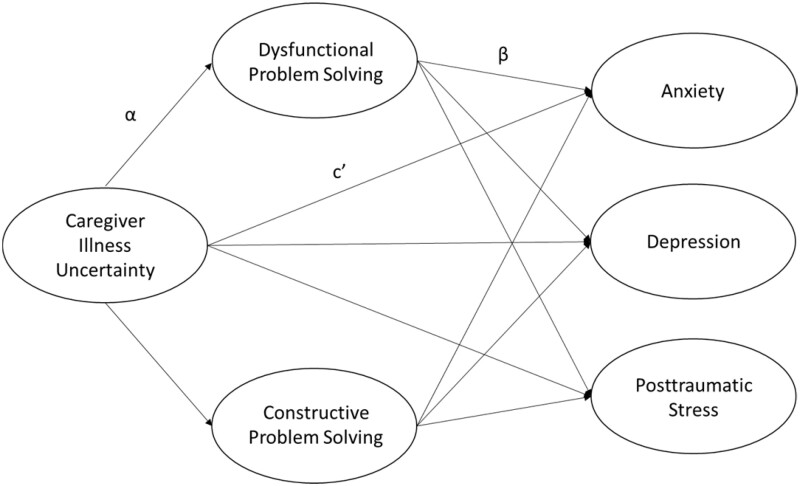
Data Analysis Plan
Descriptive statistics for demographic variables and key study variables were conducted in IBM SPSS Statistics 25. Bivariate correlations were also computed to characterize the relationships between caregiver illness uncertainty, constructive problem-solving, dysfunctional problem-solving, anxious symptoms, depressive symptoms, and posttraumatic stress symptoms. Mplus (Version 8.4) was used to construct a bootstrapped mediation path analysis model. This model consisted of one independent variable (caregiver illness uncertainty), two mediators (caregiver constructive and dysfunctional problem-solving), and three outcome variables (caregiver anxious, depressive, and posttraumatic stress symptoms). This model allowed us to evaluate the direct relationships between caregiver illness uncertainty with the three caregiver adjustment outcomes (anxious, depressive, and posttraumatic stress symptoms), as well as for the examination of six indirect effects of caregiver illness uncertainty on these three outcome variables via constructive problem-solving and dysfunctional problem-solving (see Figure 1). Significance of indirect pathways was assessed via 5,000 bias-corrected bootstrap-resampling draws. A 95% confidence interval for an indirect effect that does not include 0 indicates significant mediation. The R2 effect size statistic for significant indirect effects was calculated to estimate the amount of variance in the caregiver adjustment outcomes explained by the indirect effect. Participants for this study were recruited from three treatment sites; nesting of participants within treatment sites violates the assumption of independent responses. To address this, the three recruitment sites were dummy coded and included as additional predictors of the two mediators and three outcomes to model site variation in the analysis. Caregiver age and caregiver gender were also included as control covariates in the model given research linking these variables to caregiver adjustment outcomes. Overall model fit was suggested by the comparative fit index (0.98; Hu & Bentler, 1999) and the root mean square error of approximation (0.07; Hu & Bentler, 1999). Missing data was minimal (ranging from 0% to 5.5%) and was handled via maximum likelihood estimation.
Figure 1.
Proposed path analysis model examining the effects of problem-solving strategies on the relationship between caregiver illness uncertainty and outcomes of psychological adjustment.
Results
Preliminary Analyses
Descriptive statistics and bivariate correlations for key study variables can be found in Table II. Bivariate correlations revealed greater caregiver illness uncertainty was associated with lower constructive problem-solving scores, but with higher dysfunctional problem-solving scores, anxious symptoms, depressive symptoms, and posttraumatic stress symptoms (p < .01). Greater caregiver dysfunctional problem-solving was associated with worse caregiver anxious, depressive, and posttraumatic stress symptoms (p < .01). Constructive problem-solving was not significantly associated with any caregiver adjustment outcomes.
Table II.
Descriptive Statistics and Correlations for Key Study Variables
| 1 | 2 | 3 | 4 | 5 | 6 | Mean | SD | |
|---|---|---|---|---|---|---|---|---|
| 1. PPUS | — | 71.30 | 15.45 | |||||
| 2. SPSI—DPS | 0.44** | — | 12.38 | 8.29 | ||||
| 3. SPSI—CPS | −0.27** | −0.23** | — | 24.92 | 7.68 | |||
| 4. ANX | 0.44** | 0.36** | −0.04 | — | 55.56 | 11.79 | ||
| 5. DEP | 0.46** | 0.36** | −0.06 | 0.82** | — | 59.66 | 10.24 | |
| 6. IES-R | 0.45** | 0.38** | −0.06 | 0.70** | 0.64** | — | 28.03 | 18.79 |
Note. ANX = Symptom Checklist-90 Revised Anxiety subscale; DEP = Symptom Checklist-90 Revised Depression subscale; IES-R = Impact Events Scale-Revised total score; PPUS = Parent Perceptions of Uncertainty Scale—total score; SPSI-CPS = Social Problem-Solving Inventory-Revised: Short Form, Constructive Problem-Solving subscale; SPSI-DPS = Social Problem-Solving Inventory-Revised: Short Form, Dysfunctional Problem-Solving subscale.
p ≤ .001.
Mediation Analysis
Detailed results for the bootstrapped, mediated path analysis composed of one independent variable (caregiver illness uncertainty), two mediators (constructive and dysfunctional problem-solving), and three outcome variables (anxious, depressive, and posttraumatic stress symptoms) are included in Table III. Dummy-coded recruitment site, caregiver age, and caregiver gender were included as control covariates in the mediation model. Results are reported below by outcome variable.
Table III.
Caregiver Problem-Solving Strategies as Mediators of Their Illness Uncertainty and Adjustment
| IV on M (path a) |
M on DV (path b) |
Indirect effect (a × b) |
Direct effects (path c’) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| IV | M | DV | Est B (β) | SE | Est B (β) | SE | Est B (β) | 95% CI | Est B (β) |
| PPUS | SPSI—DPS | ANX | 0.23 | 0.04** | 0.29 | 0.09** | 0.07 | 0.03 to 0.12† | 0.29** |
| (0.44) | (0.20) | (0.09) | (0.38) | ||||||
| PPUS | SPSI—CPS | ANX | −0.14 | 0.03** | 0.17 | 0.10 | −0.02 | −0.05 to 0.00 | 0.29** |
| (−0.27) | (0.11) | (−0.03) | (0.38) | ||||||
| PPUS | SPSI—DPS | DEP | 0.23 | 0.04** | 0.23 | 0.08** | 0.06 | 0.02 to 0.10† | 0.26** |
| (0.44) | (0.19) | (0.09) | (0.39) | ||||||
| PPUS | SPSI—CPS | DEP | −0.14 | 0.03** | 0.12 | 0.10** | −0.02 | −0.04 to 0.01 | 0.26** |
| (−0.27) | (0.09) | (−0.03) | (0.39) | ||||||
| PPUS | SPSI—DPS | IES-R | 0.23 | 0.04** | 0.45 | 0.15** | 0.11 | 0.04 to 0.19† | 0.47** |
| (0.44) | (0.20) | (0.10) | (0.38) | ||||||
| PPUS | SPSI—CPS | IES-R | −0.14 | 0.03** | 0.22 | 0.16 | −0.03 | −0.08 to 0.01 | 0.47** |
| (−0.27) | (0.09) | (−0.03) | (0.38) | ||||||
Note. Caregiver age, caregiver gender, and dummy-coded recruitment site were included as covariates in this model. ANX = Symptom Checklist-90 Revised Anxiety subscale; CI = confidence interval; DEP = Symptom Checklist-90 Revised Depression subscale; DV = dependent variable; IES-R = Impact Events Scale-Revised total score; IV = independent variable; M = mediator variable; PPUS = Parent Perceptions of Uncertainty Scale—total score; SE = standard error; SPSI-CPS = Social Problem-Solving Inventory-Revised: Short Form, Constructive Problem-Solving subscale; SPSI-DPS = Social Problem-Solving Inventory-Revised: Short Form, Dysfunctional Problem-Solving subscale.
Statistically significant indirect effect.
p ≤ .001.
Anxious Symptoms
There was a significant indirect effect between caregiver illness uncertainty and anxious symptoms through dysfunctional problem-solving (αβ = 0.07; 95% confidence interval [CI], 0.03 to 0.12) when controlling for caregiver age, caregiver gender, and recruitment site. There was no indirect effect through constructive problem-solving (αβ = −0.02; 95% CI, −0.05 to 0.00). Dysfunctional problem-solving partially mediated the relationship between caregiver illness uncertainty and anxious symptoms as the direct relationship remained significant when controlling for the mediators and covariates (c’ = 0.29, p < 0.001). The indirect effect through dysfunctional problem-solving accounted for 19% of the variance in caregiver anxious symptoms.
Depressive Symptoms
Caregiver dysfunctional problem-solving was a significant mediator in the relationship between caregiver illness uncertainty and depressive symptoms (αβ = 0.06; 95% CI, 0.02 to 0.10) when controlling for caregiver age, caregiver gender, and recruitment site. This indirect effect accounted for 19% of the variance in caregiver depressive symptoms. There was no significant indirect effect between caregiver illness uncertainty and depressive symptoms through constructive problem-solving (αβ = −0.02; 95% CI, −0.04 to 0.01). The direct relationship between caregiver illness uncertainty and depressive symptoms remained significant in the presence of the mediators and covariates (c’ = 0.26, p < .001), reflecting dysfunctional problem-solving to have partially mediated this relationship.
Posttraumatic Stress Symptoms (IES-R)
The indirect path between caregiver illness uncertainty and posttraumatic stress symptoms was significant through dysfunctional problem-solving (αβ = 0.11; 95% CI, 0.04 to 0.19) but not through constructive problem-solving (αβ = −0.03; 95% CI, −0.08 to 0.01). The indirect effect through dysfunctional problem-solving accounted for 19% of the variance in caregiver posttraumatic stress symptoms. When controlling for the mediators and covariates, the direct relationships between caregiver illness uncertainty and posttraumatic stress symptoms remained significant (c’ = 0.47, p < .001) reflecting caregiver dysfunctional problem-solving partially mediated this relationship.
Discussion
The present study is the first to examine the roles of constructive and dysfunctional problem-solving strategies in the relationship between illness uncertainty and adjustment outcomes in caregivers of children newly diagnosed with cancer. Results showed that greater dysfunctional problem-solving strategies were associated with higher levels of both uncertainty and poorer adjustment outcomes. Furthermore, dysfunctional problem-solving strategies partially mediated the relationship between caregivers’ illness uncertainty and their anxious, depressive, and posttraumatic symptoms. Higher levels of constructive problem-solving strategies were associated with lower levels of uncertainty but not adjustment outcomes, consistent with other reports (Ko et al., 2005). However, constructive problem-solving strategies did not mediate this relationship. These results suggest the use of dysfunctional, but not constructive, problem-solving strategies (e.g., avoidance and impulsive/careless problem-solving, negative problem orientation) may contribute to the relationship between uncertainty and adjustment in caregivers.
These results are particularly interesting in light of recent randomized clinical trials with caregivers of children with a chronic medical condition. Problem-solving skills training interventions with caregivers of children newly diagnosed with cancer have led to significant reductions in negative affectivity of caregivers across multiple studies (Phipps et al., 2020; Sahler et al., 2002, 2005, 2013). Interestingly, Sahler et al. (2002) found that decreasing dysfunctional problem-solving strategies had a greater effect on improving mood than increasing constructive problem-solving strategies. This is consistent with our findings that showed dysfunctional problem-solving strategies partially mediated the relationship between uncertainty and adjustment, while constructive problem-solving strategies did not. Nezu et al. (2012) have suggested dysfunctional problem-solving strategies, specifically negative problem orientation, may interfere with effectively using constructive problem-solving strategies to manage a significant life stressor. Indeed, caregivers of adolescents with cancer have reported that they felt distressed and unable to play a role in the treatment decision-making process because they struggled to understand the large amount of information the medical team provided after diagnosis (Robertson et al., 2019). The current results suggest that negative cognitive appraisals of situations eliciting uncertainty could interfere with caregivers’ abilities to effectively problem-solve shortly after their child has been diagnosed with cancer. Future research exploring how information communicated to families by healthcare providers influences the relationship between uncertainty, problem-solving strategies, and psychosocial adjustment in caregivers of children newly diagnosed with cancer is warranted.
Notably, illness uncertainty has been the target of two parent-based randomized controlled trials for caregivers of children, including one with parents of children newly diagnosed with diabetes (Hoff et al., 2005) and one with parents of youth with cancer (Mullins et al., 2012). Results of these trials demonstrated that teaching uncertainty management skills may effectively reduce parent distress, parent-rated child behavior problems, and posttraumatic stress symptoms (Hoff et al., 2005; Mullins et al., 2012). Both interventions incorporated problem-solving skills training that targeted illness uncertainty. Unfortunately, the unique impact of this problem-solving training could not be determined in these interventions as they did not directly measure participants’ problem-solving strategies. Based on the results of this current study and the literature, future uncertainty management interventions may benefit from measuring changes in problem-solving strategies reported by caregivers as a means to examine the potential mechanism of therapeutic change in order to maximize intervention effectiveness.
Pediatric cancer treatments require children and their caregivers to navigate complex situations that cause them to experience feelings of uncertainty. The current results suggest that early screening of caregivers for elevated illness uncertainty and dysfunctional problem-solving strategies may identify those at an increased risk for poor adjustment following their child being diagnosed with cancer. Brief interventions that teach problem-solving strategies to manage sources of uncertainty may facilitate positive caregiver adjustment. As caregivers experience uncertain situations throughout their child’s treatment, the use of dysfunctional problem-solving strategies to manage these situations may exacerbate anxious, depressive, and posttraumatic stress symptoms. Therefore, interventions aiming to improve caregivers’ ability to manage illness uncertainty and reduce their subsequent distress may benefit from identifying individuals who utilize dysfunctional problem-solving strategies and mitigating those strategies while also supporting and/or teaching constructive problem-solving strategies.
The following study limitations should be noted. First, the cross-sectional study design does not allow for examination of causality. As such, it cannot be claimed that caregivers experiencing illness uncertainty increases their use of dysfunctional problem-solving strategies, which in turn contributes to them developing anxious, depressive, or posttraumatic stress symptoms. The temporal relationship of problem-solving strategies with uncertainty and psychological adjustment should be further examined in longitudinal studies. Second, data were collected via self-report from a single informant which increases vulnerability to reporter bias. Third, caregivers were not assessed for a history of a mental health diagnosis prior to their child’s diagnosis. Therefore, the impact of a previous diagnosis on the current reports of symptoms could not be assessed. Fourth, although the study was conducted at geographically diverse pediatric hospitals and consisted of a large sample, the caregivers in our sample were primarily White mothers, decreasing the generalizability of our findings. Given research showing differences in social problem-solving strategies amongst a racially and ethnically diverse sample of caregivers of children with cancer (Isaac et al., 2020), examination of these associations within a more racially and ethnically diverse population that includes fathers is clearly needed.
Conclusions
In summary, the results of this study suggest that illness uncertainty and dysfunctional problem-solving strategies may play a key role in the early adjustment of caregivers of children newly diagnosed with cancer. Specifically, caregivers of children newly diagnosed with cancer who are experiencing elevated levels of illness uncertainty may benefit from learning problem-solving strategies targeting illness uncertainty sources and cognitions. Interventions should be developed and tested to determine if strategies to mitigate illness uncertainty and dysfunctional problem-solving strategies could incrementally increase the effectiveness of interventions to promote psychological adjustment of caregivers of children newly diagnosed with cancer.
Acknowledgments
We would like to thank the participants and research coordinators at each site who were involved in this project for their contributions and hard work.
Additional information: Coauthor Ayman El-Sheikh, MD, died February 3, 2021.
Funding
This work was supported by the NIH/National Institute of Nursing Research (5R01NR014248-05).
Conflicts of interest: None declared.
References
- Bakula D. M., Sharkey C. M., Perez M. N., Espeleta H. C., Gamwell K. L., Baudino M., Delozier A. M., Chaney J. M., Alderson M. R., Mullins L. L. (2019). Featured article: the relationship between parent and child distress in pediatric cancer: A meta-analysis. Journal of Pediatric Psychology, 44, 1121–1136. 10.1093/jpepsy/jsz051 [DOI] [PubMed] [Google Scholar]
- D’Zurilla T. J., Goldfried M. R. (1971). Problem solving and behavior modification. Journal of Abnormal Psychology, 78(1), 107–126. 10.1037/h0031360 [DOI] [PubMed] [Google Scholar]
- D’Zurilla T. J., Nezu A. (1982). Social problem solving in adults. In Kendall P.C. (Ed.), Advances in cognitive–behavioral research and therapy (pp. 201–274). Academic Press. [Google Scholar]
- D’Zurilla T. J., Nezu A. M., Maydeu-Olivares A. (2002). Social problem-solving inventory-revised: Technical manual. Multi-Health Systems. [Google Scholar]
- D’Zurilla T. J., Nezu A. M., Maydeu-Olivares A. (2004). Social problem solving: Theory and assessment. In Chang E. C., D'Zurilla T. J., Sanna L. J. (Eds.), Social problem solving: Theory, research, and training (pp. 11–27). American Psychological Association. 10.1037/10805-001 [DOI] [Google Scholar]
- Derogatis L. R. (1994). Symptom Checklist-90-Revised: Administration, scoring and procedures manual. National Computer Systems, Incorporated. [Google Scholar]
- Hoff A. L., Mullins L. L., Gillaspy S. R., Page M. C., Van Pelt J. C., Chaney J. M. (2005). An intervention to decrease uncertainty and distress among parents of children newly diagnosed with diabetes: a pilot study. Families, Systems, & Health, 23, 329–342. 10.1037/1091-7527.23.3.329 [DOI] [Google Scholar]
- Hu L. T., Bentler P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Iobst E. A., Alderfer M. A., Sahler O. J. Z., Askins M. A., Fairclough D. L., Katz E. R., Butler R. W., Dolgin M. J., Noll R. B. (2009). Brief report: Problem solving and maternal distress at the time of a child's diagnosis of cancer in two-parent versus lone-parent households. Journal of Pediatric Psychology, 34, 817–821. 10.1093/jpepsy/jsn140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isaac E. I., Sivagnanalingam U., Meisman A. R., Donewar C. W., Ewing L. J., Katz E. R., Muriel A. C., Rohan J. M. (2020). Longitudinal patterns of social problem-solving skills in an ethnically diverse sample of pediatric patients with cancer and their caregivers. International Journal of Environmental Research and Public Health, 17, 1581. 10.3390/ijerph17051581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz L. F., Fladeboe K., King K., Gurtovenko K., Kawamura J., Friedman D., Compas B., Gruhn M., Breiger D., Lengua L., Lavi I., Stettler N. (2018). Trajectories of child and caregiver psychological adjustment in families of children with cancer. Health Psychology, 37, 725–735. 10.1037/hea0000619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko C. M., Malcarne V. L., Varni J. W., Roesch S. C., Banthia R., Greenbergs H. L., Sadler G. R. (2005). Problem-solving and distress in prostate cancer patients and their spousal caregivers. Supportive Care in Cancer, 13, 367–374. 10.1007/s00520-004-0748-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maydeu-Olivares A., D’Zurilla T. J. (1996). A factor-analytic study of the Social Problem-Solving Inventory: An integration of theory and data. Cognitive Therapy and Research, 20, 115–133. 10.1007/BF02228030 [DOI] [Google Scholar]
- Mishel M. H. (1983). Parents' perception of uncertainty concerning their hospitalized child. Nursing Research, 32, 324–330. 10.1097/00006199-198311000-00002 [DOI] [PubMed] [Google Scholar]
- Mishel M. H. (1984). Perceived uncertainty and stress in illness. Research in Nursing & Health, 7, 163–171. 10.1002/nur.4770070304 [DOI] [PubMed] [Google Scholar]
- Mishel M. H. (1988). Uncertainty in illness. Image: The Journal of Nursing Scholarship, 20, 225–232. 10.1111/j.1547-5069.1988.tb00082.x [DOI] [PubMed] [Google Scholar]
- Mishel M. H. (1990). Reconceptualization of the uncertainty in illness theory. Image: The Journal of Nursing Scholarship, 22, 256–262. 10.1111/j.1547-5069.1990.tb00225.x [DOI] [PubMed] [Google Scholar]
- Mullins L. L., Cushing C. C., Suorsa K. I., Tackett A. P., Molzon E. S., Mayes S., McNall-Knapp R., Mullins A. J., Gamwell K. L., Chaney J. M. (2016). Parent illness appraisals, parent adjustment, and parent-reported child quality of life in pediatric cancer. Pediatric Hematology and Oncology, 33, 314–326. 10.1080/08880018.2016.1198443 [DOI] [PubMed] [Google Scholar]
- Mullins L. L., Fedele D. A., Chaffin M., Hullmann S. E., Kenner C., Eddington A. R., Phipps S., McNall-Knapp R. Y. (2012). A clinic-based interdisciplinary intervention for mothers of children newly diagnosed with cancer: A pilot study. Journal of Pediatric Psychology, 37, 1104–1115. 10.1093/jpepsy/jss093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nezu A. M., Nezu C. M., D'Zurilla T. (2012). Problem-solving therapy: A treatment manual. Springer Publishing Company. [Google Scholar]
- Pai A. L., Greenley R. N., Lewandowski A., Drotar D., Youngstrom E., Peterson C. C. (2007). A meta-analytic review of the influence of pediatric cancer on parent and family functioning. Journal of Family Psychology, 21, 407–415. 10.1037/0893-3200.21.3.407 [DOI] [PubMed] [Google Scholar]
- Palermo T. M., Law E. F., Bromberg M., Fales J., Eccleston C., Wilson A. C. (2016). Problem solving skills training for parents of children with chronic pain: A pilot randomized controlled trial. Pain, 157, 1213–1223. https://doi.org/10.1097%2Fj.pain.0000000000000508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patiño-Fernández A. M., Pai A. L., Alderfer M., Hwang W. T., Reilly A., Kazak A. E. (2008). Acute stress in parents of children newly diagnosed with cancer. Pediatric Blood & Cancer, 50, 289–292. 10.1002/pbc.21262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez M. N., Traino K. A., Bakula D. M., Sharkey C. M., Espeleta H. C., Delozier A. M., Mayes S., McNall R., Chaney J. M., Mullins L. L. (2020). Barriers to care in pediatric cancer: The role of illness uncertainty in relation to parent psychological distress. Psycho-oncology, 29, 304–310. 10.1002/pon.5248 [DOI] [PubMed] [Google Scholar]
- Phipps S., Fairclough D. L., Noll R. B., Devine K. A., Dolgin M. J., Schepers S. A., Askins M. A., Schneider N. M., Ingman K., Voll M., Katz E. R., McLaughlin J., Sahler O. J. Z. (2020). In-person vs. web-based administration of a problem-solving skills intervention for parents of children with cancer: Report of a randomized noninferiority trial. EClinicalMedicine, 24, 100428. 10.1016/j.eclinm.2020.100428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce L., Hocking M. C., Schwartz L. A., Alderfer M. A., Kazak A. E., Barakat L. P. (2017). Caregiver distress and patient health‐related quality of life: Psychosocial screening during pediatric cancer treatment. Psycho-oncology, 26, 1555–1561. 10.1002/pon.4171 [DOI] [PubMed] [Google Scholar]
- Rivera P. A., Elliott T. R., Berry J. W., Grant J. S. (2008). Problem-solving training for family caregivers of persons with traumatic brain injuries: A randomized controlled trial. Archives of Physical Medicine and Rehabilitation, 89, 931–941. 10.1016/j.apmr.2007.12.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson E. G., Wakefield C. E., Shaw J., Darlington A. S., McGill B. C., Cohn R. J., Fardell J. E. (2019). Decision-making in childhood cancer: Parents’ and adolescents’ views and perceptions. Supportive Care in Cancer, 27, 4331–4340. 10.1007/s00520-019-04728-x [DOI] [PubMed] [Google Scholar]
- Rodriguez E. M., Dunn M. J., Zuckerman T., Vannatta K., Gerhardt C. A., Compas B. E. (2012). Cancer-related sources of stress for children with cancer and their parents. Journal of Pediatric Psychology, 37, 185–197. 10.1093/jpepsy/jsr054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruccione K., Kramer R. F., Moore I. K., Perin G. (1991). Informed consent for treatment of childhood cancer: Factors affecting parents' decision making. Journal of Pediatric Oncology Nursing, 8, 112–121. https://doi.org/10.1177%2F104345429100800304 [DOI] [PubMed] [Google Scholar]
- Sahler O. J. Z., Dolgin M. J., Phipps S., Fairclough D. L., Askins M. A., Katz E. R., Noll R. B., Butler R. W. (2013). Specificity of problem-solving skills training in mothers of children newly diagnosed with cancer: Results of a multisite randomized clinical trial. Journal of Clinical Oncology, 31, 1329–1335. https://doi.org/10.1200%2FJCO.2011.39.1870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahler O. J. Z., Fairclough D. L., Phipps S., Mulhern R. K., Dolgin M. J., Noll R. B., Katz E. R., Varni J. W., Copeland D. R., Butler R. W. (2005). Using problem-solving skills training to reduce negative affectivity in mothers of children with newly diagnosed cancer: Report of a multisite randomized trial. Journal of Consulting and Clinical Psychology, 73, 272–283. 10.1037/0022-006X.73.2.272 [DOI] [PubMed] [Google Scholar]
- Sahler O. J. Z., Varni J. W., Fairclough D. L., Butler R. W., Noll R. B., Dolgin M. J., Phipps S., Copeland D. R., Katz E. R., Mulhern R. K. (2002). Problem-solving skills training for mothers of children with newly diagnosed cancer: A randomized trial. Journal of Developmental and Behavioral Pediatrics, 23, 77–86. [DOI] [PubMed] [Google Scholar]
- Shanmugham K., Cano M. A., Elliott T. R., Davis M. (2009). Social problem-solving abilities, relationship satisfaction and depression among family caregivers of stroke survivors. Brain Injury, 23, 92–100. 10.1080/02699050802657020 [DOI] [PubMed] [Google Scholar]
- Steele R. G., Long A., Reddy K. A., Luhr M., Phipps S. (2003). Changes in maternal distress and child-rearing strategies across treatment for pediatric cancer. Journal of Pediatric Psychology, 28, 447–452. 10.1093/jpepsy/jsg035 [DOI] [PubMed] [Google Scholar]
- Szulczewski L., Mullins L. L., Bidwell S. L., Eddington A. R., Pai A. L. (2017). Meta-analysis: Caregiver and youth uncertainty in pediatric chronic illness. Journal of Pediatric Psychology, 42, 395–421. 10.1093/jpepsy/jsw097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss D. S. (2007). The Impact of Event Scale-Revised. In Wilson J.P., Keane T.M. (Eds.), Assessing Psychological Trauma and PTSD: A Practitioner’s Handbook (2nd edn, pp. 168–189). Guilford Press. [Google Scholar]